Tens unit stimulation
TENS (transcutaneous electrical nerve stimulation)
Transcutaneous electrical nerve stimulation (TENS) is a method of pain relief involving the use of a mild electrical current.
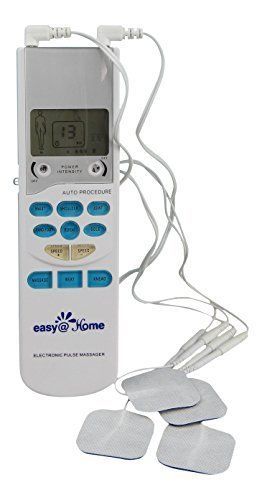
A TENS machine is a small, battery-operated device that has leads connected to sticky pads called electrodes.
Credit:
FAYE NORMAN / SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/282593/view
You attach the pads directly to your skin. When the machine is switched on, small electrical impulses are delivered to the affected area of your body, which you feel as a tingling sensation.
The electrical impulses can reduce the pain signals going to the spinal cord and brain, which may help relieve pain and relax muscles. They may also stimulate the production of endorphins, which are the body's natural painkillers.
What TENS is used for
TENS may be able to help reduce pain and muscle spasms caused by a wide range of conditions including:
- arthritis
- period pain
- pelvic pain caused by endometriosis
- knee pain
- sports injuries
It's also sometimes used as a method of pain relief during labour.
Does TENS work?
There's not enough good-quality scientific evidence to say for sure whether TENS is a reliable method of pain relief. More research is needed and clinical trials are ongoing.
Healthcare professionals have reported that it seems to help some people, although how well it works depends on the individual and the condition being treated.
TENS is not a cure for pain and often only provides short-term relief while the TENS machine is being used.
However, the treatment is generally very safe and you may feel it's worth trying instead of, or in addition to, the usual medical treatments.
Trying TENS
If you're thinking about trying TENS, it's a good idea to speak to a GP about a referral to a physiotherapist or pain clinic.
A physiotherapist or pain specialist may be able to loan you a TENS machine for a short period if they think it could help.
You can choose to buy your own TENS machine without getting medical advice, but it's generally better to have a proper assessment first, so you can find out whether a TENS machine is appropriate for you and be taught how to use it properly.
To get the most benefit from TENS, it's important that the settings are adjusted correctly for you and your individual condition.
If you find TENS effective, you can buy a TENS machine from a pharmacy. They range in price from about £20 to £100. More expensive machines are not necessarily any better than lower-priced ones, so it's best to do some research before you buy.
How to use TENS
This is a general guide on how to use a TENS machine. Always follow the manufacturer's specific instructions.
TENS machines are small and lightweight, so you can use them while working or on the move. You can put it in your pocket, clip it to your belt or hold it in your hand.
You can use TENS throughout the day for as long as you like, although it should not be used while you're driving, operating machinery, or in the bath or shower.
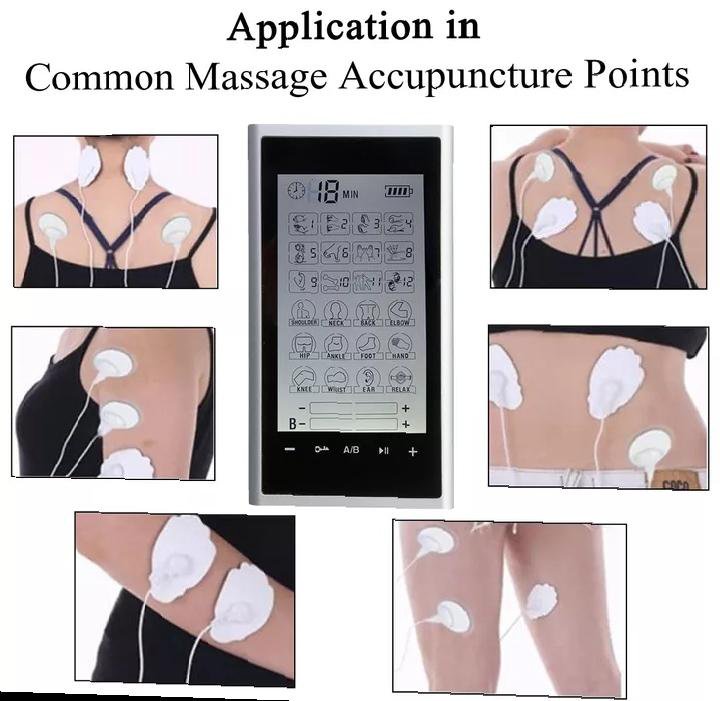
Positioning the pads
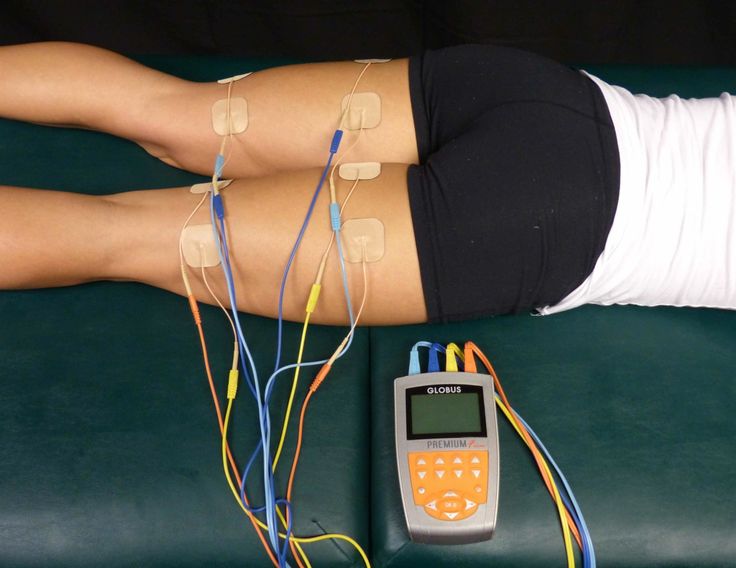
Make sure the machine is switched off before you attach the pads to your skin. Position the pads either side of the painful area, at least 2.5cm (1 inch) apart.
Position the pads either side of the painful area, at least 2.5cm (1 inch) apart.
Never place the pads over:
- the front or sides of your neck
- your temples
- your mouth or eyes
- your chest and upper back at the same time
- irritated, infected or broken skin
- varicose veins
- numb areas
Turning it on and adjusting the strength
Turn on the TENS machine when the pads are attached in the correct places. You'll feel a slight tingling sensation pass through your skin.
The machine has a dial that allows you to control the strength of the electrical impulses.
Start on a low setting and gradually increase it until the sensation feels strong but comfortable. If the tingling sensation starts to feel painful or uncomfortable, reduce it slightly.
If the tingling sensation starts to feel painful or uncomfortable, reduce it slightly.
Switch the TENS machine off after you've finished using it and remove the electrodes from your skin.
Are there any risks of side effects?
For most people, TENS is a safe treatment with no side effects.
Some people may be allergic to the pads and their skin may become red and irritated. Speak to your GP, physiotherapist or pharmacist if you have concerns. You may need to take a short break from using TENS. Special pads are available for people with allergies.
TENS is not safe for everyone to use. Do not use it without first getting medical advice if:
- you have a pacemaker or another type of electrical or metal implant in your body
- you're pregnant, or there's a chance you might be pregnant – TENS may not be recommended early in pregnancy
- you have epilepsy or a heart problem
- you have an overactive bladder
Page last reviewed: 13 April 2022
Next review due: 13 April 2025
Transcutaneous Electrical Nerve Stimulation - StatPearls
Dac Teoli; Jason An.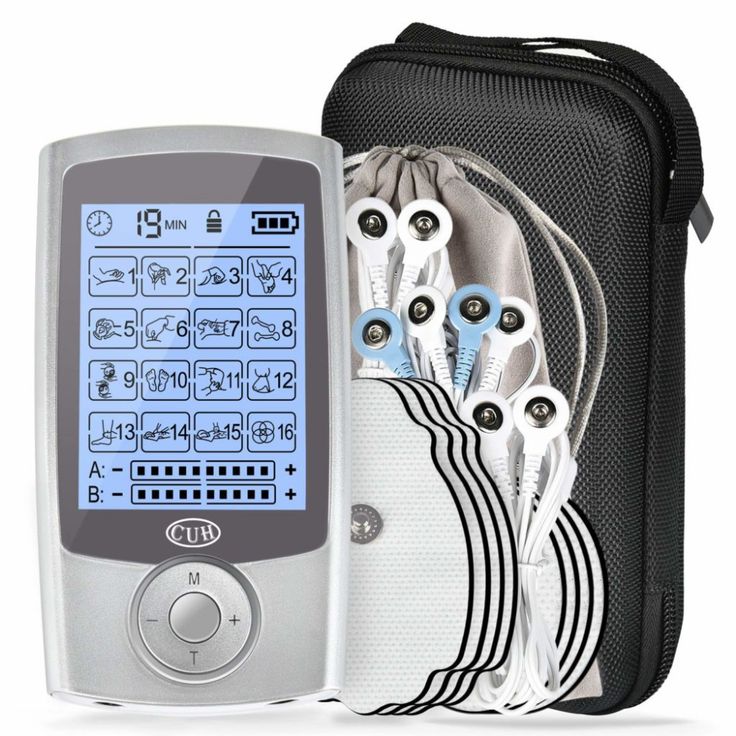
Author Information and Affiliations
Last Update: October 31, 2022.
Continuing Education Activity
Transcutaneous electrical nerve stimulation, known by its acronym TENS, is a modality that uses electric current to activate nerves in order to decrease pain. The TENS unit is a small device, often battery-operated, which can sometimes even fit into a pocket. It utilizes electrodes placed on the skin and which connect to the unit via wires to address pain in a target region. Pregnancy, epilepsy, and pacemaker are all contraindications for TENS. This activity describes the indications, contraindications, and clinical significance of transcutaneous electrical nerve stimulation and highlights the role of the interprofessional team in the management of pain.
Objectives:
Summarize the indications for transcutaneous electrical nerve stimulation.
Explain how transcutaneous electrical nerve stimulation reduces pain.
Recall the complications of transcutaneous electrical nerve stimulation.
Discuss interprofessional team strategies for improving care coordination and communication to advance the control of pain and improve outcomes.
Access free multiple choice questions on this topic.
Introduction
Transcutaneous electrical nerve stimulation, known by its acronym TENS, is a modality that uses electric current to activate nerves for therapeutic reasons. The TENS unit is a small device, often battery-operated, which can sometimes even fit into a pocket. It utilizes electrodes placed on the skin and which connect to the unit via wires to address a targeted therapeutic goal. The units are said to be titratable, permitting for a high degree of user tolerance with few side effects. Compared to many medications, the device is free from the risk of overdose. TENS units are often highly adjustable, allowing the user to control pulse width, intensity, and frequency. Low frequency of < 10Hz in conjunction with high intensity is used to produce muscle contractions. High frequencies of > 50 Hz are used with low intensity to produce paresthesia without muscle contractions. Overall, the concept of TENS throughout history has been the topic of vigorous debate within scientific circles in regards to efficacy. However, while this modality of pain management has proven itself in clinical investigations, there remains to this day disagreement over which pain syndromes and conditions TENS is appropriate.
Low frequency of < 10Hz in conjunction with high intensity is used to produce muscle contractions. High frequencies of > 50 Hz are used with low intensity to produce paresthesia without muscle contractions. Overall, the concept of TENS throughout history has been the topic of vigorous debate within scientific circles in regards to efficacy. However, while this modality of pain management has proven itself in clinical investigations, there remains to this day disagreement over which pain syndromes and conditions TENS is appropriate.
TENS, in its earliest conceptual form, is believed to date back to approximately 60 A.D. The Roman physician Scribonius Largus proposed symptomatic relief to patients by having the patient be exposed and in contact with an "electric fish" from the ocean. There are also ancient records of the use of electric eels for their pain management benefits — the use of electricity in managing human ailments propagated over time. By the 18th century, there were numerous devices developed to deliver electrostatic exposures with the belief of treating a wide array of conditions, from headaches to cancer, with even Benjamin Franklin being an eventual supporter.
The 19th century started with one particular machine, the "Electreat," leading the way in clinical therapeutic usage of electricity in managing patient disease. However, it had several constraints including large size and limited adjustments. It has been long since abandoned.
The TENS units and functionality as we think of it today are credited to American neurosurgeon Dr. C. Norman Shealy. After completing medical school at Duke University in North Carolina, he had additional training out of Barnes-Jewish Hospital and Massachusetts General Hospital. He spent several years subsequently researching spinal cord stimulators and transcutaneous electrical nerve stimulation, developing what developed into today's TENS units. His early work was an effort to arrive at an impactful therapy for several types of pain including migraines, back pain, and gout.
As the study of transcutaneous electrical nerve stimulation advanced, there came new techniques inherent to the modality, such as intense TENS, acupuncture TENS, and conventional TENS.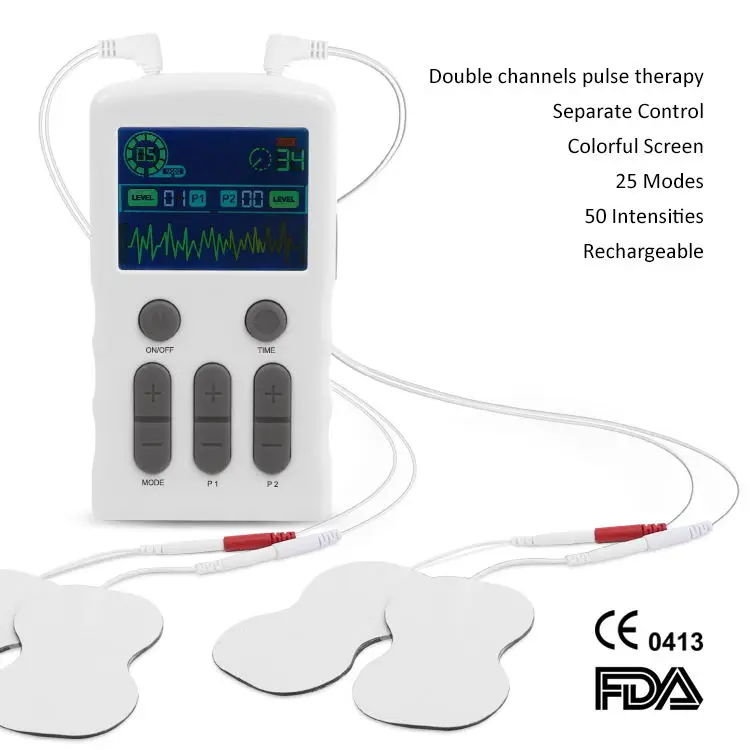 [1][2][3][4]
[1][2][3][4]
Anatomy and Physiology
TENS is believed to be effective by selectively delivering an activating stimuli to large diameter non-noxious afferents (A-beta) which subsequently reduces pain (via decreased nociceptor activity) and unwanted sensation.[5][6]
Indications
The fundamental indication for TENS is seeking to manage pain, both acute and chronic. There is an overall divide across scientific literature regarding the efficacy of TENS application for particular types of pain or pain conditions. While a significant body of work exists which suggests that TENS is effective for neuropathic, nociceptive, and musculoskeletal pain, a notable portion of these studies were noted for methodological concerns.
A look at the three types of TENS is outlined below along with their conceptual indications.
Intense TENS is used primarily as a "counter-irritant." Aiming to target small diameter, high threshold cutaneous afferent (A-delta), this type of TENS specifically seeks to block transmission of nociceptive information in nerves while stimulating other analgesic mechanisms. Both high frequencies and intensities are used for short periods of time.
Both high frequencies and intensities are used for short periods of time.
Acupuncture-like TENS (AL-TENS) is an approach at hyperstimulation and often used in patients that do not respond to conventional TENS. Titration is to low-frequency, higher intensity, longer pulse width. AL-TENS aims to stimulate small diameter, high threshold peripheral afferent (A-delta).
Conventional TENS utilizes high-frequency, low-intensity, small pulse width. The goal is to stimulate selectively large diameter, low threshold non-noxious afferent (A-beta). This approach enjoys use in the treatment of dermatomal pain distributions.[5][7][8]
Contraindications
Pregnancy, epilepsy, and pacemaker are all contraindications for TENS. Additionally, contraindications exist to the placement of the electrode pads in certain areas. Some of these placements include: over the eyes, trans-cerebrally, the front of the neck, simultaneously positioned anterior and posterior chest electrodes, internally, over broken skin or lesions, over tumors, directly over the spine, regions of severe paresthesia where the user might not recognize skin irritation. [6][9]
[6][9]
Technique
It is imperative to read the manufacturer's instruction booklet, as each unit might have slight variances in recommendations. TENS units are now small and lightweight. Patients can place them in their pocket, on a desk, or hold them. Treatment sessions can take place at the convenience of the patient except while operating heavy machinery, driving, bathing, showering, or swimming. The unit should be powered off before placing the pads. Electrode pad placement is at least 1 inch apart in the appropriate dermatomal region of the targeted pain. The skin underlying pad placement must have intact sensation. After powering on the unit, the setting titration is to manufacturer recommendations. Red and black lead placement have little impact on clinical outcomes.[8]
Complications
Overall, for the vast majority of people, TENS is believed to be safe and well-tolerated with little to no side effects. However, manufacturers of TENS units universally warn individuals with pacemakers, epilepsy, or are pregnant that these conditions are contraindications to use as they can lead to potential complications.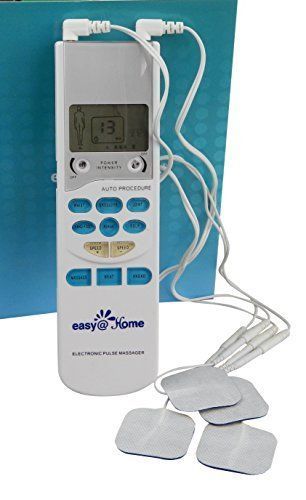 Nevertheless, this has been viewed as more of a medicolegal maneuver in high-risk populations, and TENS units are actually usable in these groups assuming close medical supervision and electrode placement is not in close vicinity to the chest, neck, or abdomen.
Nevertheless, this has been viewed as more of a medicolegal maneuver in high-risk populations, and TENS units are actually usable in these groups assuming close medical supervision and electrode placement is not in close vicinity to the chest, neck, or abdomen.
Furthermore, there have been some complications with impacting transdermal drug delivery systems if drug application is close to the TENS electrodes.
There have been documented dermatologic complications from using TENS units — the most of these cases relate to either allergic reactions to the electrode pads or contact dermatitis. Special hypoallergenic electrode pads are available for this population. Additionally, syncope and nausea have both been documented as complications of transcutaneous electrical nerve stimulation.
Lastly, there are theoretical risks with using TENS units while driving or operating heavy machinery, so it is therefore recommended to avoid TENS during those activities to avoid the risk of further complication. [9][10]
[9][10]
Clinical Significance
There is no universal consensus concerning the efficacy of TENS in managing pain. However, there are indeed a number of studies which have found a positive impact on patients with an overall low risk of complications/side effects when using TENS appropriately and according to manufacturer instructions. As such, combining TENS with pharmacotherapy remains a worthwhile endeavor for interested patients willing to try the modality. More research needs to take place to arrive at a definitive position on the place of TENS in pain management. One characteristic that has universal agreement, however, is that if TENS does provide results, those are short-term in nature and rapid in onset and offset. TENS is not a cure for pain conditions or syndromes.
The positive impact in which TENS has on an individual might diminish over time. Habituation might even lead to a worsening of pain. Recommendations are that patients take breaks from treatment and vary their placement of electrode pads over time. [8][11]
[8][11]
Enhancing Healthcare Team Outcomes
TENS units are available in many different clinical settings. Practitioners utilize them in hospice and palliative care, pain management, orthopedic surgery, neurology, dentistry, chiropractic, and physical therapy. Units have found use in hospitals, clinics, and homes alike. However, before the first TENS treatment, individuals should have a formal pain assessment by an experienced and qualified professionals, as well as given full and clear instructions on how to use the TENS unit. It is just as important to review the medical conditions and contraindicated electrode pad placements. Instructions should be thorough, but easy to understand. The patient should undergo a monitored session of TENS therapy by a trained provider so that they can evaluate for adherence to and comprehension of directions, placement, and titrating the machine. Conventional TENS is the approach first used in individuals new to the modality, often with a continuous pulse pattern of midrange frequencies and durations. [12][6] An interprofessional team approach involving the nurse, allied health professional, and clinician in educating the patient and family and providing follow up will elicit the best results. [Level V]
[12][6] An interprofessional team approach involving the nurse, allied health professional, and clinician in educating the patient and family and providing follow up will elicit the best results. [Level V]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
TENS (Transcutaneous Electrical Nerve Stimulator). Contributed by Wikimedia Commons (CC by 2.0) https://creativecommons.org/licenses/by/2.0/
References
- 1.
Francis J, Dingley J. Electroanaesthesia--from torpedo fish to TENS. Anaesthesia. 2015 Jan;70(1):93-103. [PubMed: 25348076]
- 2.
Kasat V, Gupta A, Ladda R, Kathariya M, Saluja H, Farooqui AA. Transcutaneous electric nerve stimulation (TENS) in dentistry- A review. J Clin Exp Dent. 2014 Dec;6(5):e562-8. [PMC free article: PMC4312687] [PubMed: 25674327]
- 3.
Slavin KV. History of peripheral nerve stimulation.
 Prog Neurol Surg. 2011;24:1-15. [PubMed: 21422772]
Prog Neurol Surg. 2011;24:1-15. [PubMed: 21422772]- 4.
Johnson MI, Jones G. Transcutaneous electrical nerve stimulation: current status of evidence. Pain Manag. 2017 Jan;7(1):1-4. [PubMed: 27641909]
- 5.
Gibson W, Wand BM, O'Connell NE. Transcutaneous electrical nerve stimulation (TENS) for neuropathic pain in adults. Cochrane Database Syst Rev. 2017 Sep 14;9(9):CD011976. [PMC free article: PMC6426434] [PubMed: 28905362]
- 6.
Sluka KA, Walsh D. Transcutaneous electrical nerve stimulation: basic science mechanisms and clinical effectiveness. J Pain. 2003 Apr;4(3):109-21. [PubMed: 14622708]
- 7.
Johnson M. Transcutaneous electrical nerve stimulation: review of effectiveness. Nurs Stand. 2014 Jun 10;28(40):44-53. [PubMed: 24894255]
- 8.
Johnson MI, Paley CA, Howe TE, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database Syst Rev. 2015 Jun 15;2015(6):CD006142.
 [PMC free article: PMC8094447] [PubMed: 26075732]
[PMC free article: PMC8094447] [PubMed: 26075732]- 9.
Miller MA, Palaniswamy C, Sharma D, Reddy VY. Inappropriate shock from a subcutaneous implantable cardioverter-defibrillator due to transcutaneous electrical nerve stimulation. Heart Rhythm. 2015 Jul;12(7):1702-3. [PubMed: 25889810]
- 10.
Jauregui JJ, Cherian JJ, Gwam CU, Chughtai M, Mistry JB, Elmallah RK, Harwin SF, Bhave A, Mont MA. A Meta-Analysis of Transcutaneous Electrical Nerve Stimulation for Chronic Low Back Pain. Surg Technol Int. 2016 Apr;28:296-302. [PubMed: 27042787]
- 11.
Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Syst Rev. 2008 Oct 08;2008(4):CD003008. [PMC free article: PMC7138213] [PubMed: 18843638]
- 12.
Young JD, Spence AJ, Power G, Behm DG. The Addition of Transcutaneous Electrical Nerve Stimulation with Roller Massage Alone or in Combination Did Not Increase Pain Tolerance or Range of Motion.
 J Sports Sci Med. 2018 Dec;17(4):525-532. [PMC free article: PMC6243624] [PubMed: 30479519]
J Sports Sci Med. 2018 Dec;17(4):525-532. [PMC free article: PMC6243624] [PubMed: 30479519]
Osito Tens Unit Muscular stimulator Electronic impulse massager User Manual
Osito Tens Unit stimulator Electronic impulse massager
Characteristics
- : 7.01 x 3.98 x 2.6 inch; 15.52 oz
- BRAND: Osito
Introduction
To activate the body's natural pain medications, a transcutaneous electrical nerve stimulator (TENS) transmits electrical impulses through the skin. Endorphins and other chemicals can be released with electrical impulses to block pain signals in the brain. nine0007
RELIEVING THE PAIN OF TENS
The tenth block of the muscle stimulator has 50 intensity levels and 25 settings. reduces severe chronic pain and effectively treats muscle tension and pain. HSA or FSA approved product.
STRONG MASSAGER
Shiatsu/deep tissue, low intensity, kneading/tapping, acupuncture and tapping are some of the dozens of modes available.
ADJUSTABLE TIME AND INTENSITY
The 50 strength levels of the EMS massager allow you to experiment with a unique experience, and the default time can be easily changed from 5 to 60 minutes.
4 REUSED ELECTRODE PADS
The pads use multi-layer technology and have good conductivity with hydrogels. When properly used, they can be used repeatedly 70 to 110 times, and once fully charged, they can be used continuously for 10 hours.
The TENS device has 25 modes, 50 intensity levels and a 5 to 60 minute timer for pain relief.
- No children using this TENS unit; it is used for adults only.
- Switching modes will turn off the device.
(If the strength varies in different modes, adjust the level as needed. )
)
Using electricity to stimulate the nerve, pain relief therapy can be applied to the shoulder, waist, back, neck, arm, leg, and foot that have been strained as a result of physical exercise or regular household chores. Use it whenever you need; it is safe! nine0007
Guard
- Do not use on patients with hypertension or in labour.
- Never use electrode pads on broken or broken skin.
- Be careful around delicate parts of the body such as the mouth, heart and brain.
Easy to use
- Attach the electrodes and connecting line to the TENS block; (Fully charged before use.)
- Do not overlap pads when applying each set of pads to clean, dry and healthy skin (free of sweat or oil) around the painful area;
- Press the switch button to turn on the TENS unit for about 3 seconds;
- Set time; 30 minute timer by default. Each press results in an additional five minutes;
- Choose from 25 available modes.
 (Techniques similar to massage include kneading, tapping, pressing, shiatsu, manipulation, rubbing, tapping, and masseur circulation.)
(Techniques similar to massage include kneading, tapping, pressing, shiatsu, manipulation, rubbing, tapping, and masseur circulation.) - Set individual intensity of channels P1 and P2 when using two channels.
Effective Tens Unit Pain Therapy
Unit of Tens provides low volume tag sends impulses to the skin for muscle stimulation, reduces the sensation of physical pain from sciatica, arthritis or inflammation of the discs/joints, stiff shoulders, legs and back muscles, relieves chronic pain and helps with body stress and rehabilitation after pain, so that the user can feel more healthy and energetic. nine0007
Frequently Asked Questions
Ems and tens are two different things. is this device a combo box (tens and ems) or is it actually a tens box?
There are several moods for this car, you can choose from dozens of which I use most often.
Will the pads stick to hairy skin or does it need to be shaved?
They are likely to stick, but may cause pain to come off. nine0007
nine0007
Is it necessary to use all 6 electrode pads in every session?
No. I only use 2 at a time.
Is the mat reusable or disposable?
Normal use of our pillow can be used 70-110 times, but you won't have sweat or lotion on your body for pads.
Replacement pads are not currently available. Will other brands fit?
YES FITS.
Is there a "static" or "steady" mode? one that continues and stays at the selected level.
Yes, there is!
What are these 25 modes?
Massage-like modes: kneading, beating, pressing, shiatsu, manipulating, rubbing, tapping, massager circulation, etc.
Is there a replacement pad and where can I buy it?
This is our replacement unit of tens. nine0007
nine0007
What are dual channels?
Like two dozen separate cars at once. You can massage 2 body parts with 2 different modes and intensity.
How many modes can be selected?
Our tens unit has 25 modes and 50 intensity modes. Video0190 Posted in OSITO Tags: Electronic, massager, OSITO, OSITO TENS Unit Muscle stimulator Electronic pulse massager, Impulse, stimulator, TENS, Muscle Unit
HCG Injection. Pregnancy after an injection of hCG
Today, unfortunately, many couples of reproductive age face the problem of infertility. As you know, infertility is a consequence of any disease that is currently present in the body or was previously. Therefore, in order to eliminate infertility, a couple must undergo a series of examinations to help identify the cause of this condition. Based on the results of the examination, the attending physician will prescribe measures to eliminate infertility, which include stimulation of ovulation with an injection of hCG. nine0007
nine0007
When ovulation induction is indicated
Ovulation induction is one of the treatments for infertility. It can be shown with regular anovulatory cycles, as well as when performing assisted reproductive technologies.
Ovulation stimulation can be performed for conception in a natural way, with artificial insemination, as well as during in vitro fertilization. Before ovulation stimulation, a couple must be prescribed examinations to identify the causes of infertility. Since problems with the reproductive system can affect both women and men, both partners are examined. During the diagnosis, the causes of anovulatory cycles can be identified, which are sufficient to eliminate to restore natural ovulation (endocrine system disorders, inflammatory or infectious diseases, etc.). It is also important to check the "capacity" of male germ cells. Sometimes pregnancy may not occur not only because of anovulatory cycles, but also due to impaired spermatogenesis. nine0007
In order to detect anovulation, the following examinations will be assigned to a woman during several cycles:
- measurement of basal body temperature;
- ultrasound examinations;
- blood tests for hormone levels.

Without normalization of the level of prolactin, thyroid hormones, and male sex hormones, ovulation stimulation is not carried out.
Stimulation of ovulation with an injection of hCG
Stimulation of ovulation begins with non-steroidal antiestrogen or gonadotropic drugs. The choice of drug will depend on the method of eliminating infertility, during which stimulation occurs. On average, drugs are prescribed for up to 12 days. This will depend on the response of the ovaries to the ongoing therapy. During the period of ovulation stimulation, to control the growth of follicles, a woman will undergo ultrasound every 3-4 days until the follicles reach the required size of 18-20 mm. nine0007
Next, the patient is given an injection of hCG. HCG completes the process of maturation of follicles and "turns on" the mechanisms of ovulation. HCG also prevents the regression of follicles and the appearance of follicular cysts, which can be formed due to non-disclosure of a mature follicle.
After an injection of hCG, ovulation occurs within 24-36 hours. Next, the patient is assigned a schedule of sexual intercourse (in the case of natural fertilization), insemination or the date of ovarian puncture (during IVF).
Artificial insemination
Artificial insemination is the intrauterine introduction of partner or donor spermatozoa to effect a pregnancy. Artificial insemination, in most cases, is carried out for women with immunological infertility, when antisperm antibodies that destroy spermatozoa are present in the secret of the cervical canal. Also, artificial insemination can be performed on women without a husband or partner who decide to have a child. The artificial insemination procedure can be carried out with ovulation stimulation and in the natural cycle. nine0007
In vitro fertilization
During in vitro fertilization, ovulation is stimulated to obtain the maximum number of mature eggs. This process is called superovulation. There are several methods (protocols) for IVF.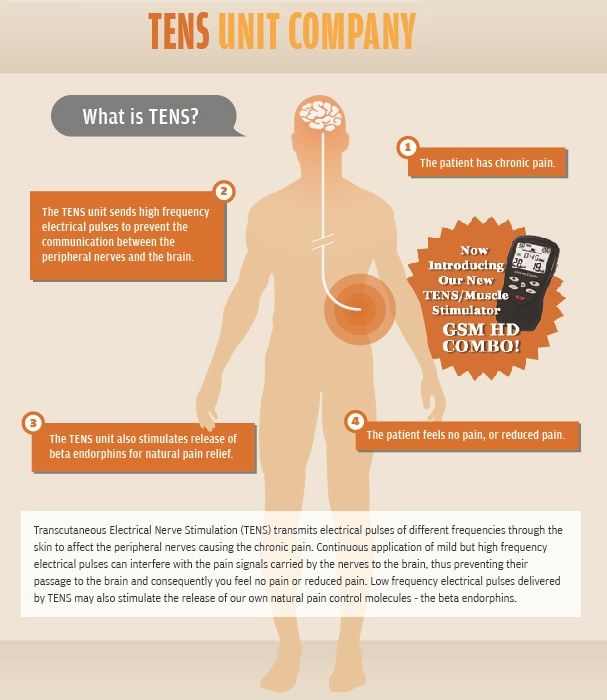 However, any of them use gonadotropic drugs that stimulate the growth of follicles and eggs, as well as an injection of hCG. Methods for IVF will differ in duration and dosage of drugs. The choice of the necessary IVF protocol is carried out by the attending physician based on the patient's health status. nine0007
However, any of them use gonadotropic drugs that stimulate the growth of follicles and eggs, as well as an injection of hCG. Methods for IVF will differ in duration and dosage of drugs. The choice of the necessary IVF protocol is carried out by the attending physician based on the patient's health status. nine0007
A long IVF protocol begins with the introduction of pituitary blockers - preparations of gonadotropin-releasing hormones. This is necessary to control the natural hormonal background of a woman.
From the 3rd-5th day of the menstrual cycle, gonadotropic drugs are prescribed that stimulate the growth of follicles. These drugs will contain synthetic analogues of follicle-stimulating hormone, which is normally produced by the pituitary gland. Additionally, luteinizing hormone may be prescribed, which is necessary to prevent premature ovulation. nine0007
When the follicles are mature (determined by ultrasound), the woman is given an injection of hCG. After an injection of hCG, an ovarian puncture is performed approximately 36 hours later (more precise terms are determined by the attending physician in each individual case). Ovarian puncture is a minimally invasive procedure that collects eggs. During IVF, it is important to obtain the eggs before they are directly released into the abdominal cavity, otherwise it is almost impossible to collect them in the future and the stimulation will have to be repeated again. The procedure is carried out under general anesthesia, so you can’t eat (6-8 hours before) and drink (2 hours before). During the puncture, a special needle is inserted into the ovaries through the vagina under the control of ultrasound. When the needle reaches the mature follicle, the eggs are taken with the follicular fluid. The manipulation is repeated with each mature follicle. nine0007
Ovarian puncture is a minimally invasive procedure that collects eggs. During IVF, it is important to obtain the eggs before they are directly released into the abdominal cavity, otherwise it is almost impossible to collect them in the future and the stimulation will have to be repeated again. The procedure is carried out under general anesthesia, so you can’t eat (6-8 hours before) and drink (2 hours before). During the puncture, a special needle is inserted into the ovaries through the vagina under the control of ultrasound. When the needle reaches the mature follicle, the eggs are taken with the follicular fluid. The manipulation is repeated with each mature follicle. nine0007
For further IVF, a man must provide sperm that was obtained on the day of the puncture. If donor sperm is used, it must be ready for use on the same day.
Selected oocytes and specially processed ejaculate are placed on the medium in a Petri dish for fertilization. The environment in the Petri dish is as close as possible in composition to the natural environment of the fallopian tubes, where conception should take place.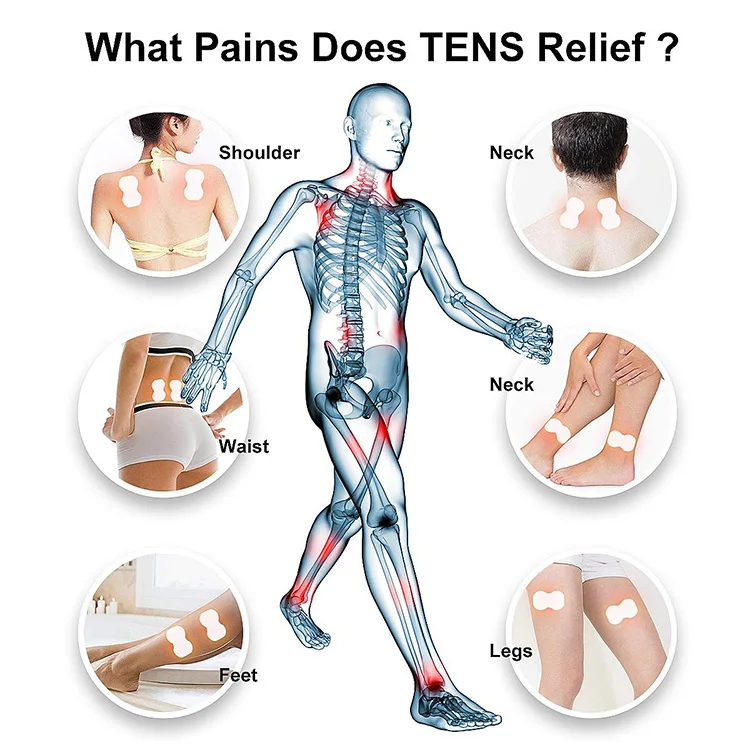 After fertilization, the highest quality zygotes continue to be cultured until they reach the blastocyst stage. Cultivation lasts 3-5 days. Next, the embryos are transplanted into the woman's uterus for further implantation and development. Usually 1-2 embryos are transplanted, which increases the likelihood of a positive outcome of IVF. nine0007
After fertilization, the highest quality zygotes continue to be cultured until they reach the blastocyst stage. Cultivation lasts 3-5 days. Next, the embryos are transplanted into the woman's uterus for further implantation and development. Usually 1-2 embryos are transplanted, which increases the likelihood of a positive outcome of IVF. nine0007
In Kaliningrad, IVF and other methods of reproductive technologies can be done at the IVF Center clinic, whose specialists successfully eliminate infertility of any etiology.
Pregnancy after hCG injection
In order to check whether pregnancy has occurred, appropriate tests after a hCG injection are prescribed after a certain time:
- 2-3 weeks from ovulation - with natural fertilization;
- 2 weeks from sperm injection - with artificial insemination; nine0016
- 14 days - after embryo transfer after IVF.
You can find out if you are pregnant with a "homemade" cavity test, which reacts to an increase in hCG in the urine. However, the most informative is the analysis of the level of hCG in the blood, which is monitored over time. With the help of a blood test for the level of hCG, you can determine the quality of the course of pregnancy, its fertility, and also identify the threat of ectopic pregnancy or miscarriage.
However, the most informative is the analysis of the level of hCG in the blood, which is monitored over time. With the help of a blood test for the level of hCG, you can determine the quality of the course of pregnancy, its fertility, and also identify the threat of ectopic pregnancy or miscarriage.
During pregnancy, hCG levels will continuously increase tens of thousands of times, reaching a maximum peak of approximately 200,000 mIU/ml by the 12th week. Further, hCG will gradually subside, while its level will still be high compared to the norms for a non-pregnant woman (0-25 mIU / ml). A sharp decrease in the level of hCG in the first trimester may signal a threat of miscarriage, ectopic pregnancy, or pregnancy fading. nine0007
In a multiple pregnancy, the level of hCG will increase depending on the number of fetuses: two times for twins, three times for triplets, etc.
HCG injections during pregnancy
In some cases, with a history of threatened miscarriage or after IVF, hCG tablets or injections are prescribed to support pregnancy directly during pregnancy (in the first trimester).