Tens unit during pregnancy
TENS (Transcutaneous electrical nerve stimulation)
TENS (Transcutaneous electrical nerve stimulation) | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Key facts
- Transcutaneous electrical nerve stimulation, or TENS, is a form of pain relief without medicine that can be used during labour.
- It is not clear how TENS works to reduce pain. It is thought to reduce pain by stimulating different nerves in the spinal cord, blocking pain signals.
- There is not a lot of evidence that TENS works to reduce pain, but some people find it helpful.
- Most people can safely use TENS, but it’s a good idea to discuss it with your doctor or midwife before your labour begins.
- If you want to use TENS for pain relief during labour, ask your doctor, midwife or hospital in advance about where you can borrow or rent a machine.
What is TENS?
Transcutaneous electrical nerve stimulation, or TENS, is a form of pain relief without medicine. It can be used in labour to help with the pain.
Two electrodes are stuck to your skin and connected to a battery-powered machine. The machine delivers small pulses of electrical current to the body. You can adjust the amount of electricity delivered to your body. The pulses feel like tingling sensations on your skin.
How can I use TENS to relieve pain?
It is not clear how TENS works to relieve pain.
It's possible that it blocks pain signals by stimulating different nerves in your spinal cord. It might also cause the release of endorphins, the body's natural pain relievers.
There is not a lot of evidence to show that TENS works to reduce pain, but some people find it helpful.
What are the advantages of TENS in labour?
The advantages of TENS are that:
- it doesn't require medicines or injections
- it may give you some control over pain relief
- you are able to move around
- you can use other methods if TENS does not give you enough pain relief
- there is no harm to you or your baby
- it can be used at home during early labour
What are the disadvantages of TENS in labour?
TENS doesn’t work for everybody. It can be uncomfortable but shouldn’t be painful. You may experience skin irritation where the electrodes are stuck on. TENS can’t be used in the bath or shower.
It can be uncomfortable but shouldn’t be painful. You may experience skin irritation where the electrodes are stuck on. TENS can’t be used in the bath or shower.
When should I not use TENS?
TENS is thought to be very safe, but it shouldn't be used:
- if you are pregnant but not in labour
- before 37 weeks gestation
- by people who have a pacemaker
- by some people with epilepsy
Where can I get a TENS machine?
Not all hospitals and birthing centres have TENS machines. If you’re interested in using one, it's best to discuss it with your doctor or midwife before you go into labour. You may wish to ask about whether it is safe for you to use a TENS machine, where you can get one and about any costs involved.
You can find more information about other methods of pain relief during labour here.
Sources:
Cochrane Library (Transcutaneous electrical nerve stimulation (TENS) for pain management in labour), King Edward Memorial Hospital Obstetrics & Gynaecology (Clinical practice guideline, Pain management), SA Health (TENS in labour), Royal Women's Hospital (Managing pain in labour)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Giving birth - stages of labour
- Making a birth plan
- Pain relief during labour
- Non-medical pain relief during labour
- Gas (Entonox)
- Epidural
Need more information?
Pain Relief in Labour and Childbirth
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Pain relief during labour
Learn what options are available to you to relieve pain during labour pain, and how your birth support partner can help you.
Read more on Pregnancy, Birth & Baby website
Non-medical pain relief during labour
There are many ways to relieve labour pain without medicines. Each method has advantages and disadvantages. Learn about the different options to help choose one or more that suit you.
Each method has advantages and disadvantages. Learn about the different options to help choose one or more that suit you.
Read more on Pregnancy, Birth & Baby website
Childbirth - pain relief options - Better Health Channel
Understanding your pain relief options can help you cope better with the pain of childbirth.
Read more on Better Health Channel website
Pain during childbirth | HealthEngine Blog
Almost all women experience pain during childbirth which varies in severity. There are different pharmacological and non-pharmacological approaches to treatment of pain during childbirth.
Read more on HealthEngine website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Assisted Birth
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Going to hospital or birthing centre
Whether you're planning to have your baby at home, in hospital or at a midwifery-led birth centre, you should get a few things ready at least two weeks before your due date.
Read more on Pregnancy, Birth & Baby website
Having a baby in hospital
Both public and private hospitals provide high-quality care for you and your baby. They both have advantages and disadvantages – find out more here.
Read more on Pregnancy, Birth & Baby website
Pelvic Organ Prolapse
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Using a TENS Machine for Labor Pain: Is It For You?
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site.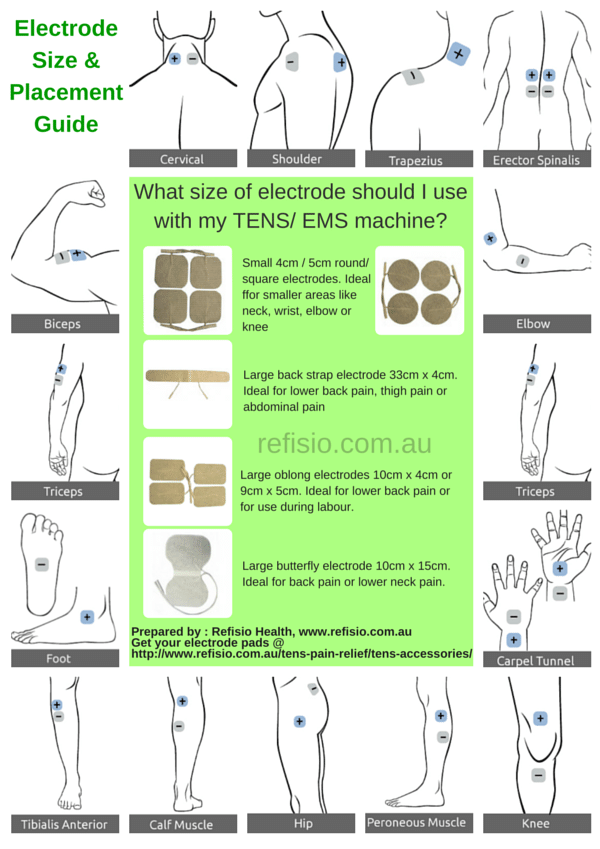 To establish that the product manufacturers addressed safety and efficacy standards, we:
To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Reducing pain during labor is a top priority for most moms-to-be. But given the limited options for managing pain, some pregnant people seek a more natural approach that doesn’t involve the use of medications.
And that’s why some parents-to-be are curious about the safety and effectiveness of a transcutaneous electrical nerve stimulation (TENS) unit.
A TENS machine or unit is a small device, often battery operated, that is used to manage both acute and chronic pain.
The unit has wires connected to electrodes that are placed on the skin. The electrodes deliver low voltage electrical currents to targeted body parts to control pain signals in the body.
A practitioner familiar with TENS therapy places the electrodes at or near the nerves where the pain is located. These electrical currents or impulses can create short-term or long-term relief from pain.
Experts say TENS therapy works in a couple of different ways. The first belief is that the electrical impulses affect the nervous system reducing its ability to transmit pain signals to the spinal cord and brain. But they also say that electrical impulses can stimulate the body to produce endorphins, a neurotransmitter that can help relieve pain.
“TENS unit use has been known to alleviate period, joint, back, endometriosis, arthritis, fibromyalgia, sports injuries, and postoperative pain,” says Sherry Ross, MD, OB-GYN and women’s health expert at Providence Saint John’s Health Center.
It’s essential that you do your homework when choosing a TENS unit. Ross recommends looking for one that has a reliable and good track record with a strong output intensity and with sufficient electrical impulses.
“The higher the numbers, the more helpful it will be to alleviate the pain,” Ross says.
Ideally, Ross says you’ll want to buy a pharmaceutical-grade TENS unit, going with a reputable brand. You can buy a TENS unit online through Amazon, at a CVS or Walgreens pharmacy, or through an online retailer that sells medical supplies and devices.
According to a review of the evidence, when using a TENS machine for labor pains, the electrodes are typically placed on your lower back, on specific acupuncture points, or on your head.
If you’re operating the unit yourself, you’ll regulate the intensity of the impulses during painful contractions. Most TENS units are small and battery operated, so you should be able to hold it in your hand or clip it to your clothing during contractions.
But if you’re not familiar with a TENS machine, it’s a good idea to consult with a physical therapist, midwife, or doctor who regularly uses this therapy. They’ll be able to show you how to place the electrodes on the skin as well as how to operate the machine to get the best results.
You can also hire a doula or midwife familiar with this method to operate the machine during labor. They’ll be able to place the electrodes and control the frequency of the currents coming from the TENS unit.
One of the main reasons parents-to-be consider a TENS machine is because it’s a drug-free alternative for pain management during labor.
According to Ross, the TENS unit’s ability to reduce pain sensation may be helpful in alleviating mild pain during labor. Some evidence points to the control it allows women to feel, which consequently reduces pain. It also provides a distraction from the contractions.
TENS therapy may also help reduce the dreaded low back pain that seems to strike so many women during the third trimester.
One 2012 study looked at the effectiveness of TENS in reducing low back pain during this period. Researchers divided 79 subjects into four groups: a control group and three treatment groups — one using acetaminophen, one using exercise, and the final group using TENS for pain management.
During the study period, researchers found that 57 percent of the control group experienced an increase in low back pain, while the TENS application reduced low back pain more effectively than exercise and acetaminophen.
In general, TENS therapy is considered mostly safe. That said, research involving the use of a TENS until during labor is minimal, at best.
Ross says some of the things you may notice when using the TENS unit in labor include:
- muscle twitching
- tingling
- buzzing sensation
- allergic reaction
- irritation and skin redness from the adhesive pads on the skin
- burn marks as a side effect from the electrode pads
- lower blood pressure
- muscle spasms
TENS units are used to manage pain for a variety of conditions, including painful contractions during labor. But if this is your first time receiving treatment from a TENS machine, and you plan on using it for labor pains, Ross says to proceed with caution.
“Women who have never used the TENS unit for other pain conditions should not use it during labor for the first time,” says Ross. However, she does say the TENS unit may be useful for pain relief for women in labor if they have had success in the past using it for other painful symptoms — just don’t use it in conjunction with water immersion.
For all women, Ross says that since there are inconsistent results for women using the TENS unit, it should not be the only relied upon method for labor pains.
In other words, you may need to use other forms of pain management in combination with a TENS unit. Techniques like massage, relaxation, and breath exercises are all proven ways to help moms-to-be move through labor and childbirth with less pain.
Using a TENS unit during labor may help to manage pain. The effectiveness of the currents depends on the placement of the pads and the frequency of the currents coming from the machine.
There is minimal research regarding the effectiveness of TENS during childbirth. That’s why it’s essential that you consult with your doctor and other healthcare professionals familiar with this protocol. They can help you decide if using a TENS machine during labor is right for you.
Drank a glass of wine while pregnant? It's OK
- Michelle Roberts
- BBC Health Columnist
Sign up for our Context Newsletter to help you understand what's going on.
Image copyright, Getty Images
Evidence that low alcohol consumption during pregnancy can harm the fetus is "surprisingly low", say British scientists.
They looked at all the available research on the subject since the 1950s and found no conclusive evidence that one or two small glasses of wine a week did any noticeable harm to the health of the mother or child.
However, this does not mean that it is completely safe, the team of scientists from the University of Bristol who conducted the study emphasizes and urges pregnant women not to drink at all just in case - as the official recommendations of the National Health Service prescribe.
At the same time, those women who drank a little during pregnancy should not worry about the fact that they harmed the health of the child.
76 milliliters
In 2016, the chief medical officer of the British National Health Service, Professor Sally Davies, revised the recommendations for pregnant women, urging them to completely abstain from alcohol throughout the entire period of pregnancy.
Similar recommendations in Western countries are usually expressed in conventional units of alcohol; one standard unit roughly corresponds to 76 ml of wine (less than half a glass in a restaurant) or 250 ml of beer.
Prior to this, pregnant women were advised that they could drink one to two conventional units per week.
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
It is not known how much drinking is "safe" for a pregnant woman, but it is well known what excessive drinking during pregnancy can lead to.
Alcohol intoxication or excessive drinking in this position increases the risk of miscarriage and premature birth, and can also lead to the development of fetal alcohol syndrome in a child, that is, a combination of congenital malformations, both mental and physical.
At the same time, the risks associated with infrequent moderate drinking are not so obvious.
Dr. Louise Zucollo and her colleagues found 26 studies on this subject.
After reviewing and analyzing all of the data, scientists found no clear evidence of the harm of moderate alcohol consumption, but in seven studies, moderate drinking was associated with an 8% increase in the likelihood that a child would be born with a low birth weight.
Also in their review, published in the scientific journal BMJ Open, scientists note that infrequent drinking may increase the risk of preterm birth.
"We still need to exercise caution, but there is hope that this will help alleviate guilt and anxiety in those women who occasionally indulge in a glass of wine during pregnancy," said Professor David Spiegelhalter of the University of Cambridge commenting on the results of a new study.
However, Professor Russell Weiner of the Royal College of Paediatrics and Child Health said: “My advice to women is that if you are trying to conceive or are already pregnant, it is best not to drink alcohol at all. Regular drinking, even in small amounts, can be harmful and should be avoided. , just as a precaution."
Tips for pregnant women
- If a woman drank small amounts of alcohol before she knew she was pregnant, or during the entire pregnancy, the risk that the fetus was harmed by this is very small
- Women who drink regularly in early pregnancy and suddenly find out they are pregnant should stop drinking alcohol; however, they should know that in most cases the health of their child will not be affected
- If you are worried about how much you drank during pregnancy, consult your doctor or midwife
PHARMATEKA Aggressive expansion in the drug market contributed to an increase in the number of registered side effects of pharmacotherapy, especially during pregnancy. The effect of drugs on the course of pregnancy is still a little-studied area, and opinions about the safety of their use are extremely controversial.
Key words: medicines, pharmacotherapy, side effects, pregnancy the registry is about 13 thousand, in Germany and the UK - more than 50 thousand drugs, and the total number of drugs available in different countries and their various combinations exceeds 200 thousand) [2].
The number of drugs used has increased particularly rapidly in recent years: it is noteworthy that even 20–30 years ago, 60–80% of currently used drugs were not known or did not find clinical use. It is reasonable to assume that such an aggressive expansion in the drug market contributed to an increase in the number of registered side effects of pharmacotherapy, especially during pregnancy.
At the same time, the effect of drugs on the course of pregnancy is still a poorly studied area, and opinions about the safety of their use are extremely controversial. It is not surprising that currently the study of the safety of drugs during pregnancy is considered as one of the priority areas of pharmacovigilance in the United States and the European Union [5]. The number of adverse reactions that occur in response to the treatment of expectant mothers is extremely important: at present, such effects are observed in a third of newborns. Strictly speaking, we are talking about a strict and clear justification for the pharmacotherapy of pregnant women, since almost any pharmacological drug can have a harmful effect on the fetus [2, 6].
Even more revealing are these arguments for modern Russian health care; which, in fact, is not at all surprising, since one of the global changes that have occurred in it over the past two decades can be considered, in fact, revolutionary changes in the field of drug circulation, which created the problem of a minimum of quality control of treatment. Commercial availability of almost any drugs that are in abundance on the pharmaceutical market; the aggressive policy of pharmaceutical companies, which until recently was not limited to legislative acts; a vicious feature in the psychology of the relationship between a doctor and a patient: if he does not prescribe a medicine - a bad doctor - all these factors do not at all contribute to a decrease in the consumption of drugs.
Contrary to one of the basic principles of perinatal medicine, proclaimed by the World Health Organization (1998), namely: demedicalization of care for pregnant women and women in childbirth, domestic physicians consider the appointment of many drugs as a manifestation of an attentive and qualified attitude towards a pregnant woman. To a large extent, this circumstance is facilitated by the fact that, unfortunately, the most common source of information in our country on the safety of drugs for pregnant women is still, unfortunately, the description of the drug in the drug reference books or the manufacturer's instructions for its use in pregnancy, while the use of modern medicines by clinicians advances in medicine based on the results of meta-analyses, Cochrane reviews on the effectiveness of methods of therapy and prevention of diseases in pregnant women, at the present stage are almost completely absent. On the other hand, the collection, analysis, systematization and wide dissemination of the results of clinical trials by independent, non-profit organizations (the most famous is the Cochrane Society with dozens of branches around the world) are an example of a reasonable approach to the use of one or another drug by pregnant women.
To be fair, it should be noted that the desire to maximally “secure” pregnancy and the fetus with the help of numerous achievements in pharmacology is an example not only from domestic practice [7, 9]. According to a survey of 5564 Brazilian women, 4614 (83.8%) of them took medication during pregnancy. In the US, 62% of women receive at least one drug during pregnancy, 25% use opiates, and 13% use psychotropic drugs. About 15% of women take drugs in the first 6 months of pregnancy, 75% of them - from 3 to 10 drugs.
The composition of drugs prescribed is also a concern: an analysis of 34,334 prescriptions for pregnant women in Denmark showed that 26. 6% of prescribed drugs were classified as potentially dangerous, and 28.7% were classified as unclassified, the risk of which during pregnancy is not determined [10]. Classifications of risk categories during pregnancy developed to indicate the potential danger of drugs, in particular the FDA (Food and Drug Administration), the risk categories of which are currently listed in the Russian State Register of Medicines, have their own objective inconveniences. Thus, the FDA classification, which is perhaps the only systematic source of information of this magnitude on the dangers of drugs during pregnancy, is rarely updated, simplified and more focused on teratogenic than on fetotoxic effects of drugs without taking into account the dose of the drug and clinical situations.
In addition, most of the drugs in it are characterized only by data obtained in experiments on animals, and belong to category C. A significant factor limiting its use in domestic conditions is that the mass of drugs that are not used in the United States is not included to the FDA classification. Unfortunately, we have to state that in the programs of pre- and postgraduate medical education, very little attention is paid to the pharmacological aspects of the use of drugs, while the issues of long-term use of this drug or drugs of a separate pharmacological group are not touched upon at all. The possibilities of self-education of a doctor in this area are quite limited; moreover, modern clinical pharmacology is not yet able to answer the vital questions of the compatibility of three or more drugs, especially during pregnancy.
The results of a multicenter pharmacoepidemiological study conducted in the Russian Federation show that the pharmacotherapy of pregnant women in Russia has its own specifics and is characterized by the following features:
• widespread use of drugs with unproven clinical efficacy and safety in pregnancy;
• frequent prescription of irrational drug combinations;
• use of outdated treatment regimens;
• polypharmacy;
• non-compliance with the dosing regimen and duration of therapy [4].
Declared by many authors, the expediency of controlling the prescription of drugs during pregnancy in order to optimize the safe and effective management of pregnancy and childbirth is a clearly justified urgent need at the present time.
Implementation of this postulate is possible if the basic principles of pharmacotherapy in pregnant women are observed, namely:
• prescribing drugs only for strict indications and after a thorough assessment of the potential benefits of the drug and its potential harm;
• refusal to use several drugs at the same time;
• use of the minimum effective dose of drugs for the shortest possible time;
• informing pregnant women about the need to consult a doctor about taking any drugs;
• monitoring the condition of the mother and fetus during drug therapy [6].
In our opinion, to achieve the desired result, it is necessary to overcome the conservatism of the majority of obstetrician-gynecologists who persist in prescribing certain drugs recommended by drug selection guidelines for the treatment of various complications of pregnancy, despite the lack of data obtained from high-quality clinical trials. methodological quality [1]. After all, it was possible, having reviewed the positions that seemed unshakable from the standpoint of evidence-based medicine, to exclude dozens of drugs used in the treatment of one or another nosological unit from the arsenal.
But this is clearly not enough: another point of joint efforts of progressive doctors and the society around them is the psychological readiness of pregnant women to take drugs that have been used in therapy regimens that have been traditional for domestic practice for many decades. The lack of evidence of their adverse effects on the fetus and the mother's body does not exclude them from the category of potentially hazardous to health. In addition, in addition to the positive effects of drugs on the course of pregnancy, both direct and indirect negative effects of drugs on the fetus are possible [3, 8]. Even more symptomatic is the fact that pregnant women ignore the requirements of a specialist who prescribes treatment regimens (58% of women use drugs without a doctor's prescription, 80% of pregnant women do not follow the doctor's recommendations for taking prescribed drugs) [6].
The problem of pharmacotherapy of pregnant women is very few years old. After all, until the early 1940s. humanity assumed that congenital malformations are hereditary pathology. And only in 1941, N. Gregg proved that when a mother becomes ill with rubella in the first trimester of pregnancy, various defects are detected in a newborn. This circumstance clearly revealed the influence of environmental factors on the development of the embryo. But before the thalidomide tragedy, when the possibility of drug penetration through the placenta, as well as their teratogenic effect on the development of organs and tissues, became obvious, a good two decades passed.
Opportunities to prevent or significantly reduce the negative effects of pharmacotherapy were already there. Thus, the United States was not affected by the tragedy associated with the occurrence of malformations of the limbs in the fetus as a result of taking a seemingly harmless sedative drug, due to the principled position of the FDA administration expert Francis O. Kelsey, who considered the results of preclinical studies of this drug insufficient. Thus, the understanding by each doctor of the basics of pharmacotherapy, the strict compliance of the use of drugs with the current level of knowledge, as well as the competent interpretation of the data of clinical monitoring of pregnant women, make it possible to avoid both diagnostic and therapeutic polypharmacy, and are guaranteed to comply with the rule formulated by the famous therapist and clinical pharmacologist B.E. Votchalom: "Less drugs: only what is absolutely necessary."
1. Ailamazyan E.K., Kulakov V.I., Radzinsky V.E., Savelyeva G.M. Obstetrics. National leadership. 2007. 1197 p. 2. Babanov S.A., Agarkova I.A. Features of the use of drugs during pregnancy and lactation // Gynecology 2010. No. 2. V. 12. 3. Sidelnikova V.M. Endocrinology of pregnancy in normal and pathological conditions. Moscow, 2007. 4. Strizhenok E. 5. Ushkalova E.A., Tkacheva O.N., Chukhareva N.A. Problems of the safety of the use of drugs during pregnancy and lactation // Obstetrics and Gynecology 2011. No. 2. P. 4–7. 6. Sheshukova N.A., Borovkova E.I. Pharmacotherapy for miscarriage // Questions of gynecology, obstetrics and perinatology 2009. V. 8. No. 6. P. 79–82. 7. Brucker MC. Top ten pharmacological considerations in pregnancy. Program and abstracts of the 5th Annual Conference of the National Association of Nurse Practitioners in Women’s Health; September 27–29, 2002; Scottsdale, Arizona. 8. Kalinka J, Szekers-Bartho J. The impact of dydrogesterone supplementation on hormonal profile and progesterone-induced blocking factor concentrations in women with threatened abortion Am J Reprod Immunol 2005;53:1–6. A., Gudkov I.V., Strachunsky L.S. The use of drugs during pregnancy: the results of a multicenter pharmacoepidemiological study // Klin. microbiology antimicro. chemother. 2007. Vol. 9. No. 2, pp. 162–75.