Take laxative while pregnant
Causes, treatments, and home remedies
Constipation is a very common symptom that many women experience during pregnancy.
Some women have constipation at an early stage of their pregnancy, while it does not affect other women until much later on.
In this article, we explain why constipation is common in pregnancy and discuss safe treatments and home remedies that women can use to relieve the discomfort.
The cause of constipation during pregnancy depends on the stage at which it occurs. Possible causes include:
- Hormones: Changing hormone levels in early pregnancy cause the intestines to slow down the movement of stool through the bowel. This delay increases the amount of water that the colon absorbs from the stool, which makes it more solid and difficult to pass.
- Prenatal vitamins: Prenatal vitamins are chock-full of iron, a crucial mineral that can sometimes be deficient during pregnancy. Iron can cause constipation and hard, black stools.
- Pressure from the uterus: In later pregnancy, the growing uterus can put pressure on the bowel, making it harder to move stool through the intestines.
In addition to infrequent bowel movements, constipation can cause bloating, stomach discomfort, and hard, dry stools that are painful to pass. It can also result in a feeling that not all the stool has passed.
Constipation can be particularly uncomfortable during pregnancy.
During pregnancy, women can often relieve constipation using gentle, safe home remedies:
- Fiber: Taking fiber supplements or eating more fibrous foods, such as fruits, vegetables, and whole grains, can increase the number of stools and facilitate their passage through the intestines. Adults should eat between 28 and 34 grams of fiber each day.
- Fluid: Drinking enough water is important to keep stool soft and easy to pass. If a person feels that water is not helping, they can try adding clear soups, teas, and naturally sweetened fruit or vegetable juices to their diet.

- Activity: Being active helps stool move through the intestines. Getting regular exercise, with a doctor’s approval, can help relieve constipation. If exercising is not a priority or possibility, try to fit in a gentle walk each day.
- Probiotics: Millions of healthy bacteria live in the gut and help it function correctly. Probiotics may help repopulate the gut bacteria with healthy strains that encourage normal and regular bowel movements. Foods high in probiotics include yogurt, sauerkraut, and kimchi.
If the home remedies above do not work, it may be time to discuss other options with a doctor.
For women taking prenatal vitamins that are high in iron, doctors may recommend trying a vitamin that contains less iron.
The primary medical treatment for constipation in pregnancy is a medication called a laxative, which makes it easier and more comfortable to go to the bathroom.
It is generally safe to use gentle laxatives, but it is best to avoid stimulant laxatives because they can induce uterine contractions.
Although many laxatives are available over the counter, it is important to check with a doctor which one is safe to use. Limited information is available about using some of these medications during pregnancy.
Women can usually safely use the following types of laxative during pregnancy:
Bulk-forming agents
Bulk-forming agents mimic fiber by adding material to the stool and helping it absorb more water. By doing this, they make the stool larger, softer, and easier to pass.
These types of laxative can cause some cramping or discomfort, so people should start with the lowest dosage and ensure that they drink lots of water.
Examples of bulk-forming agents include psyllium, methylcellulose, and polycarbophil.
Stool softeners
Stool softeners add water to the stool to help make it softer and more comfortable to pass.
The stool softener that doctors most commonly recommend to pregnant women is docusate (Colace).
Lubricant laxatives
Lubricant laxatives add a slippery coating to either the stool or the inside of the intestinal tract to aid the passage of stool out of the body.
Glycerin suppositories are one type of lubricant laxative. It is essential to always speak to a healthcare professional before using suppositories, especially when pregnant.
Osmotic laxatives
By drawing more water into the intestines, these laxatives help soften the stool. They also allow the bowel to contract more to move the stool along. These types of laxative can also cause cramping and bloating in the abdomen.
Examples of osmotic laxatives include polyethylene glycol and magnesium hydroxide.
In most cases, constipation in pregnancy is short-lived and resolves with no or minimal treatment. In rare cases, however, prolonged constipation can cause fecal impaction, which may need removal by a doctor.
Continued use of certain types of laxative can cause the bowel to “forget” how to push stool through the intestines.
These drugs can also cause electrolyte or fluid imbalances in some people. Such issues usually affect people who have other health problems, such as diabetes or kidney disease.
It is best to speak to a doctor about the types of laxative to take and how often to take them.
It is vital that pregnant women speak with their doctor before taking any medication, including laxatives or other constipation remedies.
Seeing a doctor is also advisable if any additional symptoms occur, including:
- nausea
- stomach pain
- vomiting
- constipation that lasts for longer than 1–2 weeks
- bleeding from the rectum
- no relief after using a laxative
As always, mention any other symptoms or concerns to the doctor for more specific information and advice.
Can You Take Laxatives During Pregnancy? Their Side Effects
Mild laxatives are safe but only provide temporary relief from constipation.
Research-backed
MomJunction believes in providing reliable, research-backed information to you. As per our strong editorial policy requirements, we base our health articles on references (citations) taken from authority sites, international journals, and research studies. However, if you find any incongruencies, feel free to write to us.
However, if you find any incongruencies, feel free to write to us.
Image: Shutterstock
Constipation is a common pregnancy complication. Most women can relieve it by staying active and increasing their fiber and water intake. However, if it persists, the doctor may prescribe laxatives. But is it safe to take laxatives during pregnancy?
Laxatives or purgatives are medicines used to treat constipation. You can get them over-the-counter (OTC) under different brand names. However, medical guidance is vital to select a safe laxative to avert any side effects and complications.
Keep reading as we tell you about laxatives, their safety during pregnancy, their possible side effects, and some safe laxatives you may try after consulting your doctor.
What Are Laxatives?
Image: Shutterstock
Laxatives are drugs that help relieve constipation by inducing a bowel movement or bulking the stools. They contain chemicals that help stool motility, frequency, and bulk.
The laxatives are available in the form of pills, capsules, foods, gums, and liquids for oral consumption or through the rectum in the form of enemas and suppositories (1).
Experts say
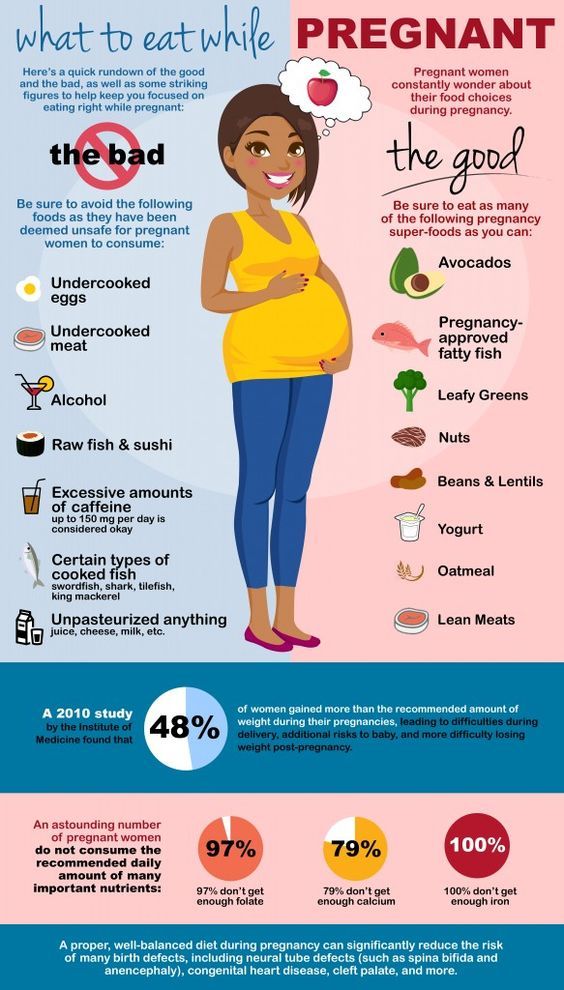
The American College of Obstetricians and Gynecologists (ACOG) recommends a fiber-rich diet to pregnant women to prevent constipation. Fruits, veggies, nuts, whole grains, and seeds are packed with fiber (2).
Related: 26 Foods To Avoid During Pregnancy
Is It Safe To Take Laxatives During Pregnancy?
Usually, doctors advise natural remedies and probiotics to improve bowel function. If these remedies seem ineffective, the doctor will prescribe mild laxatives as the second line of treatment (3).
Among the various mild laxatives, bulk-forming laxatives such as Metamucil (psyllium hydrophilic mucilloid) are not absorbed and are not known to increase the risk of malformations in the fetus. Therefore, these are considered safer than the others.
Emollient laxatives like mineral oil and stimulant laxatives like castor oil must be avoided during pregnancy due to their potential for maternal and fetal morbidity (4).
It must be noted that these laxatives only help temporarily relieve constipation; your doctor will advise you to change your diet and lifestyle to retain your natural bowel movements.
Image: Shutterstock
Prolonged usage of laxatives can result in dehydration and create an imbalance of mineral and salt levels in your body.
Quick tip
Practice regular physical activity and drink more water when you follow a fiber-rich diet to avoid bloating and abdominal discomfort (5).
Related: Fetal Growth Restriction: Reasons, Diagnosis And Risks Involved
Laxatives Safe To Take During Pregnancy
Let us take a look at the different types of laxatives that doctors usually prescribe during pregnancy (3) (6).
1. Bulk-forming laxatives
Also called fiber supplements, they work similar to fiber in your diet. They add bulk to the stools by helping them retain liquid for an easy bowel movement. They take around 12 to 24 hours to work and are unlikely to cause any harm to your pregnancy since they do not get into the blood.
Psyllium (Metamucil), methylcellulose (Citrucel), carboxymethyl-cellulose, and sterculia are some bulk-forming laxatives.
2. Stool softener laxatives
They cause water and fats to penetrate the stools, thus encouraging it to move quickly through the gastrointestinal tract. They take 12 to 72 hours to work. Multiple studies have shown no harmful effects, and thus, these laxatives are considered safe during pregnancy.
Docusate sodium (Colace) and Dicoto are such medications.
Related: Bloating And Gas During Pregnancy: Causes And Home Remedies
3. Stimulant laxatives
Image: Shutterstock
They stimulate the intestinal wall lining to speed up the bowel movements. They give quick relief within 6 to 12 hours. There is no risk to the baby as the absorption is minimal. However, long-term use can have some side effects such as electrolyte imbalances on the mother.
Senna (Senokot) and Bisacodyl (Correctol) are considered safe in small doses.
4. Osmotic laxatives
They soften the stools by drawing fluid into the gastrointestinal tract from the surrounding tissues. They take around 30 minutes to six hours to be effective. Their use is not associated with any adverse effects on the baby. Long-term use might affect the mother in the same way as stimulant laxatives do.
Sodium bisphosphate (OsmoPrep), magnesium hydroxide (milk of magnesia), sugars including polyethylene glycol (Miralax) and lactulose are some effective osmotics.
In spite of their effectiveness, laxatives are prescribed only as a second option because of some side effects.
Related: Milk Of Magnesia During Pregnancy: Safety, Benefits And Side Effects
What Could Be The Side Effects Of Laxatives During Pregnancy?
Like any other medications, laxatives also have some side effects, which usually depend on the type of laxative you are taking.
The common side effects include (3):
Image: Shutterstock
- Abdominal cramps
- Flatulence
- Bloating
- Dehydration
- Lightheadedness
- Dark urine
Excessive or prolonged intake of laxatives could result in the following side effects.
- Reduced absorption of nutrition and other medicines into the blood as laxatives increase the rate of food passage through the intestinal tract.
- Lower levels of magnesium salt in the blood. One study has found that mothers who had docusate sodium when pregnant had babies with low magnesium levels and suffered temporary jitteriness (7).
Therefore, talk to your doctor before using laxatives during pregnancy.
Next, we answer a few commonly raised queries.
1. Can laxatives cause miscarriage?
There are not enough studies to show that laxatives cause a miscarriage. However, castor oil which is a natural laxative (8) could cause fetal morbidity (4).
2. Can the use of laxatives during pregnancy cause birth defects?
Laxatives are not known to increase the probability of birth defects or other major pregnancy issues.
Before using laxatives during pregnancy, it is advised that you consult your doctor or gynecologist and ensure that it will not bring about any complications in the pregnancy. Try incorporating fiber-rich food into your diet, and bring specific changes in your lifestyle to help improve your bowel functions and reduce the chances of constipation. However, if these remedies do not work, try using laxatives that are safe to be used during pregnancy for the recommended number of days so that they will not harm you or your baby.
This post is for informational purposes only and is not a replacement for a doctor’s consultation. Do not use any medication without talking to your doctor.
References:
MomJunction's articles are written after analyzing the research works of expert authors and institutions. Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
- Erin Larowe; Laxative information; C. S. Mott Children’s Hospital (2013)
http://www.med.umich.edu/1libr/PedSurgery/ColorectalProgram/Laxatives.pdf - What can help with constipation during pregnancy?; American College of Obstetricians and Gynecologists
https://www.acog.org/womens-health/experts-and-stories/ask-acog/what-can-help-with-constipation-during-pregnancy - Magan Trottier MSc Aida Erebara MD and Pina Bozzo; Treating constipation during pregnancy; The College of Family Physicians of Canada
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3418980/ - Jessica Servey Jennifer Chang; Over-the-counter medications in pregnancy; American Family Physician.
https://www.aafp.org/afp/2014/1015/p548.pdf - Laxatives; National Health Services
https://www. nhs.uk/conditions/laxatives/#:~:text=Self%2Dhelp%20alternatives%20to%20laxatives&text=add%20bulking%20agents%2C%20such%20as
nhs.uk/conditions/laxatives/#:~:text=Self%2Dhelp%20alternatives%20to%20laxatives&text=add%20bulking%20agents%2C%20such%20as - Meredith Portalatin & Nathaniel Winstead; Medical management of constipation (2012)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3348737/ - Prescribing in Pregnancy Fourth edition; Perpustakaan Pusat Universitas Pancasila; Organization of Teratology Information Specialists (2013)
http://perpus.univpancasila.ac.id/repository/EBUPT181056.pdf - Gulsah Gurol Arslan Ismet Eser; An examination of the effect of castor oil packs on constipation in the elderly; Complementary Therapies In Clinical Practice (2011)
https://www.sciencedirect.com/science/article/pii/S1744388110000320?via%3Dihub
The following two tabs change content below.
- Reviewer
- Author
Shreeja holds a postgraduate degree in Chemistry and diploma in Drug Regulatory Affairs from the University of Mumbai. Before joining MomJunction, she worked as a research analyst with a leading multinational pharmaceutical company. Her interest in the field of medical research has developed her passion for writing research-based articles. As a writer, she aims at providing informative articles on health...
Before joining MomJunction, she worked as a research analyst with a leading multinational pharmaceutical company. Her interest in the field of medical research has developed her passion for writing research-based articles. As a writer, she aims at providing informative articles on health...
View Profile ›
Dr. Mona Hardas is a practicing Ob/Gyn from Flint, Michigan, with over 20 years of experience in private practice. She is also actively involved in teaching medical students and residents as an associate clinical professor from MSU College of Human Medicine. Dr. Hardas is interested in minimally invasive gynecology procedures, including laparoscopic hysterectomy, myomectomy, removal of adnexal masses, etc. Having...
View Profile ›
Tubal Ligation: What It Is, Procedure, Benefits And Risks
Tubal Ligation: What It Is, Procedure, Benefits And Risks
Cellulite During Pregnancy: How To Control?
Cellulite During Pregnancy: How To Control?
Safe Sleeping Positions During Second Trimester Of Pregnancy
Safe Sleeping Positions During Second Trimester Of Pregnancy
5 Amazing Benefits Of Dancing During Pregnancy
5 Amazing Benefits Of Dancing During Pregnancy
Is It Safe To Take Antacids During Pregnancy?
Is It Safe To Take Antacids During Pregnancy?
Sticky Eyes In Babies: Causes, Treatment, Remedies And Prevention
Sticky Eyes In Babies: Causes, Treatment, Remedies And Prevention
Benefits Of Baby Pacifiers And Tips To Stop Using Them
Benefits Of Baby Pacifiers And Tips To Stop Using Them
Baby Banging Head: Is this Normal, Causes And How To Respond
Baby Banging Head: Is this Normal, Causes And How To Respond
Bronchitis During Pregnancy: Causes, Prevention And Treatment
Bronchitis During Pregnancy: Causes, Prevention And Treatment
Treatment of constipation in pregnant women: what's new?
Constipation is a violation of bowel function, manifested by a delay in its emptying for more than 2 days with difficulty defecation.![]() Normally, food taken within 8 hours after a bowel movement is evacuated within the next 24 hours. In patients with chronic constipation, the transit time of food through the gastrointestinal tract is 60-120 hours or more.
Normally, food taken within 8 hours after a bowel movement is evacuated within the next 24 hours. In patients with chronic constipation, the transit time of food through the gastrointestinal tract is 60-120 hours or more.
Constipation affects 5-7% of healthy people, mostly over the age of 60 years. Among children, the frequency of this pathology is 1.5%. Recently, there has been an increase in the prevalence of constipation. Constipation can be divided into: primary and secondary.
Constipation during pregnancy is secondary. In the first half of pregnancy, constipation is caused by increased production of progesterone. In later periods - mechanical compression of the colon by the growing uterus, leading to congestion and decreased peristalsis. The prevalence of constipation during pregnancy reaches 50%.
The diagnosis of functional constipation according to the diagnostic criteria formulated in 1999 at the World Congress of Gastroenterology in Rome (Rome II criteria) is based on the presence of the following:
• less than 3 bowel movements per week;
• straining that takes up more than 25% of the time of defecation;
• fragmented stools, hard in consistency, in small volume, occupying more than 25% of the act of defecation;
• sensation of incomplete emptying in more than 25% of bowel movements;
• sensation of anorectal obstruction in more than 25% of bowel movements;
• manual methods to facilitate the evacuation of contents in more than 25% of bowel movements (eg, finger evacuation, pelvic floor support).
The treatment of constipation during pregnancy is a rather difficult task, because. there are restrictions associated with the use of laxatives, which can provoke a threat of termination of pregnancy.
The high incidence of constipation in pregnant women is due to a number of reasons.
During pregnancy, the amount of progesterone increases, which has an inhibitory effect on the smooth muscles of the intestine, which leads to the development of hypotonic dyskinesia, segmental spasm of the intestine, and inhibition of motility of the gastrointestinal tract. There is a violation of the spatial relationship between the organs of the abdominal cavity, an increase in intra-abdominal pressure, compression of the intestine by an enlarged uterus as pregnancy develops. The pathology of the anorectal region (anal fissure, hemorrhoids) that is common during pregnancy also exacerbates the problem. Predisposing factors may be a decrease in physical activity and the prescription of bed rest in case of a threatened abortion. In addition, a number of drugs used during pregnancy can cause or exacerbate existing constipation: drotaverine, papaverine, hexoprenaline, calcium channel blockers, iron preparations, aluminum and calcium-containing antacids.
In addition, a number of drugs used during pregnancy can cause or exacerbate existing constipation: drotaverine, papaverine, hexoprenaline, calcium channel blockers, iron preparations, aluminum and calcium-containing antacids.
Treatment of constipation in pregnant women should begin with non-pharmacological methods. First of all, it is recommended to change the diet, add dietary fiber in the form of bran or wheat to the diet, increase fluid intake (at least 1.5-2 liters per day), as well as increase physical activity. A high-fiber diet and dietary fiber supplementation in the form of bran have been shown to be effective in constipation in a number of studies, but experts say these interventions should not be used in severe cases, as they may exacerbate symptoms such as flatulence and cramping. .
In case of ineffectiveness of non-drug methods, laxatives are prescribed. When choosing medicines for pregnant women, first of all, it is necessary to consider their safety for the fetus.
In population-based case-control studies, no association between congenital malformations of the fetus and chronic constipation, as well as laxatives used to treat it, was found. However, the use of laxatives during pregnancy is associated with the risk of other complications. For example, castor oil is absolutely contraindicated in pregnancy, as it stimulates labor and its use has been associated with uterine rupture. The use of petroleum jelly and other mineral oils should also be avoided, as they may impair the absorption of fat-soluble vitamins and, as a result, lead to the development of coagulopathy and bleeding in newborns. Stimulant laxatives (senna and bisacodyl preparations) can increase the tone and contractile activity of the myometrium, so during pregnancy only their short-term use is permissible. Long-term use of saline osmotic laxatives, such as magnesium citrate and sodium phosphate, is not recommended, since hypermagnesemia, hyperphosphatemia and dehydration may develop. When using laxatives containing psyllium (psyllium oval seed coat), allergic reactions, up to anaphylactic shock, have been reported.
When using laxatives containing psyllium (psyllium oval seed coat), allergic reactions, up to anaphylactic shock, have been reported.
Comparative clinical studies on the efficacy and safety of laxatives of different groups in pregnant women have been few. Only 2 randomized clinical trials were included in the meta-analysis. According to his results, laxatives that have a stimulating effect on intestinal motility are more effective than drugs that increase the volume of intestinal contents, but they have more side effects.
The American Gastroenterological Association recommends osmotic laxatives for the treatment of constipation in pregnant women. The drugs of choice for chronic constipation during gestation include polyethylene glycol and lactulose. It is possible to use the drug with a softening effect on the stool sodium docusate in low doses.
Lactulose is one of the safest and most well-researched laxatives in pregnancy. It has laxative and prebiotic properties. The lactulose molecule is not destroyed by the enzymes of the small intestine, it reaches the large intestine unchanged, where it undergoes hydrolysis with the formation of lactic acid (mainly) and partially formic and acetic acids. As a result, there is a decrease in intra-intestinal pH, an increase in osmotic pressure in the intestine, liquefaction and an increase in the volume of feces and activation of intestinal peristalsis. The drug promotes the growth of Lactobacillus acidophilus, Lactobacillus bifidus in the intestine, while inhibiting the growth of ammoniogenic microorganisms, especially Esherihia coli.
As a result, there is a decrease in intra-intestinal pH, an increase in osmotic pressure in the intestine, liquefaction and an increase in the volume of feces and activation of intestinal peristalsis. The drug promotes the growth of Lactobacillus acidophilus, Lactobacillus bifidus in the intestine, while inhibiting the growth of ammoniogenic microorganisms, especially Esherihia coli.
The acidic environment of the intestine reduces the ionization and absorption of ammonia, amines and other toxic nitrogen-containing compounds in the proximal colon. Absorption of the drug is low, excreted by the kidneys (3%). Lactulose does not irritate the mucous membrane, gives a mild and physiological effect, which allows you to prescribe it even with the threat of miscarriage or premature birth. In clinical studies, it has been proven that lactulose does not penetrate the fetoplacental barrier, does not have a teratogenic and toxic effect and a negative effect on myometrial tone.
The action of lactulose occurs 24-48 hours after administration (the delay of the effect is due to the passage of the drug through the gastrointestinal tract). At the beginning of treatment, slight transient flatulence is possible, which disappears on its own on the 2nd-3rd day of treatment or is stopped by changing the dose.
At the beginning of treatment, slight transient flatulence is possible, which disappears on its own on the 2nd-3rd day of treatment or is stopped by changing the dose.
The high efficacy and safety of lactulose was also proven in another study including 62 pregnant women with constipation. Already in the second week of treatment, the frequency of defecation increased from 2.5 to 6 times a week. When using the drug at a daily dose of 20 g, the therapeutic effect was achieved faster than when used at a dose of 10 g. 84% of doctors and 81% of patients rated the effectiveness of treatment as "good" and "very good". Tolerability of treatment was rated by 87% of patients and 84% of physicians as "very good"; the main side effect was a slight transient flatulence.
Enterosorbents contribute to the elimination of flatulence when using lactulose. The most studied and safe in this category of patients is enterosgel.
In the study of pregnant rats and their fetuses, no signs of embryotoxicity and teratogenicity were found. The safety of the drug in terms of mutagenic activity was shown in tests for the induction of chromosome aberration in bone marrow cells, in a culture of human peripheral blood lymphocytes, as well as in the Ames test for the induction of reverse gene mutations in Salmonella typhimurium. It has been proven that enterosgel is safe when used in pregnant women and does not affect the fetus.
The safety of the drug in terms of mutagenic activity was shown in tests for the induction of chromosome aberration in bone marrow cells, in a culture of human peripheral blood lymphocytes, as well as in the Ames test for the induction of reverse gene mutations in Salmonella typhimurium. It has been proven that enterosgel is safe when used in pregnant women and does not affect the fetus.
Enterosorbents are widely prescribed to patients to reduce the severity of toxicosis. Their mechanism of action is connected with the accelerated release of metabolites (most often immune complexes) through the gastrointestinal tract. However, the use of almost all enterosorbents is fraught with the development of constipation, which in pregnant women would not only be undesirable, but also exacerbate the manifestations of toxicosis.
The combination of sorbents with lactulose eliminates, in fact, two problems: firstly, the severity of metiorism associated with the use of lactulose itself decreases due to the action of the sorbent, and secondly, the constipation effect of the sorbent is eliminated due to the influence of lactulose.
In pharmacy, the combination of two substances that eliminate each other's side effects is not only rational, but also an approach to creating new products. An example of such an approach is LactobioEnterosgel, which is a combination of the well-known enterosgel sorbent and the reference prebiotic lactulose.
Reprinted from Obstetrics and Gynecology No 3/2011
Treatment of constipation in pregnant women in a private clinic
This is one of the most common, but at the same time the most delicate problems that occur in at least 50% of pregnant women. In a normal state, bowel movements should be daily and in sufficient volume. Any deviations in this process require attention and adjustment of the diet, lifestyle and even psychological attitude. From a physiological point of view, problems in the work of the gastrointestinal tract are explained by hormonal changes and the physiological characteristics of the body of a pregnant woman (under the influence of various processes in different phases of pregnancy, the contraction of the smooth muscles of the intestine is weakened, in addition, the enlarged uterus compresses the intestines, etc. ).
).
Among other - non-medical reasons - the most common are the features of a woman's lifestyle: systematic stress; lack of mobility; lack of fiber; low water intake (not liquids!) and/or high intake of refined foods and foods with a high composition of sugar, homogenized fats and salt (fast food). “Refined foods are refined oils, polished rice, white flour and all the familiar white refined sugar, plus fast food with a high composition of sugar, homogenized fats and salt, which slow down the absorption of nutrients by the body and the passage of food in the intestines” (Laima Lankmane, naturopath, herbalist).
Homeopaths say that constipation is not only a “problem” of the rectum, “it is a problem of the whole organism as a whole and it must be solved in a complex way” (D.V. Arkhipova, Ph.D., homeopath): for example, this may be an allergic reaction to certain foods. Therefore, constipation is, in principle, an individual problem, and an individual approach will be the most effective solution to the problem: “Even equally pregnant women do not have 2 identical constipations: some had them before pregnancy, others did not eat properly, others did not move. All good wishes for real constipation will work only in 10% of cases. The only right decision is a full-fledged visit to a homeopath, who will approach the solution of the disharmony that has arisen, taking into account all the individual characteristics of a woman, looking at her as an integral unique system ”(A.S. Gavrilenko, obstetrician-gynecologist, Ph.D., homeopath , reflexologist).
All good wishes for real constipation will work only in 10% of cases. The only right decision is a full-fledged visit to a homeopath, who will approach the solution of the disharmony that has arisen, taking into account all the individual characteristics of a woman, looking at her as an integral unique system ”(A.S. Gavrilenko, obstetrician-gynecologist, Ph.D., homeopath , reflexologist).
First, about how NOT to solve the problem of constipation: classic laxatives such as hay, aloe vera and castor oil are contraindicated for pregnant women - they can cause premature contractions.
Now about what is POSSIBLE and NEEDED.
DIET
- Need to temporarily eliminate dairy products. “The main milk protein, casein, is one of the most difficult to digest proteins and is also a strong allergen. The fact that cottage cheese itself is capable of causing constipation is probably known to everyone. If you solve the problem with constipation in this way, then carefully introduce natural fermented milk products into the diet (preferably without flavorings and sugar) ”(D.
 V. Arkhipova, Ph.D., homeopath). It’s not worth worrying that the baby won’t get enough of something - he will take everything he needs from “mother’s reserves”, and the question is not in the amount eaten, but in the amount absorbed by the mother’s body. From the point of view of homeopathy, if you want - eat, no - you don’t need to force yourself, because. food likes and aversions are in accordance with our constitution, and therefore our needs (naturally, this applies to healthy and healthy eating habits).
V. Arkhipova, Ph.D., homeopath). It’s not worth worrying that the baby won’t get enough of something - he will take everything he needs from “mother’s reserves”, and the question is not in the amount eaten, but in the amount absorbed by the mother’s body. From the point of view of homeopathy, if you want - eat, no - you don’t need to force yourself, because. food likes and aversions are in accordance with our constitution, and therefore our needs (naturally, this applies to healthy and healthy eating habits). - It is necessary to monitor the liquid used - or rather, drink enough clean water. Volume - from one to three liters per day, if desired, but not less than a liter. “If you don’t feel like drinking water, you need to remove sweet drinks and teas from the diet and compensate for this with clean water (preferably raw, of artesian origin, pleasant to the taste, and even better thawed).” (T.G. Sadovaya, obstetrician, author of the lecture “Nutrition during pregnancy”).
- “Dried fruits are obligatory (you can pour prunes with water at night and drink an infusion in the morning), and / or drink a glass of water in the morning on an empty stomach (you can add a little lemon juice there) and a glass of water with honey at night” (I.
 S. Arefyeva, obstetrician gynecologist).
S. Arefyeva, obstetrician gynecologist). - The diet should have a sufficient amount of fiber: at least 50% of the diet of natural plant foods in raw and processed form (fiber stimulates peristalsis). It can be whole grain cereals, products made from wholemeal flour, fruits before meals or in between, vegetables, berries (the same cranberries help with constipation).
- A daily intake of 1 to 3 tablespoons of unrefined oils has a good effect on the body. “Sweet almond oil (food) has a pronounced laxative effect and does not irritate the intestinal wall. Olive and linseed oils, as well as walnut oil, also have a mild laxative effect. Do not forget that unrefined oils should be stored in the refrigerator (with the exception of olive oil), and flaxseed should be eaten within a month after opening the bottle. (O.L. Bannikova, obstetrician).
- Add magnesium-rich foods to your diet, such as green leafy vegetables, walnuts and almonds, sunflower seeds (unroasted and preferably pre-soaked for 5-7 hours), green buckwheat and spinach.
 “You can try this recipe - soak 1 teaspoon of flax seeds in ½ cup of warm water and leave for several hours. Then eat it just like that or add it to porridge, soup” (L. Lankmane, naturopath, phytotherapeutist).
“You can try this recipe - soak 1 teaspoon of flax seeds in ½ cup of warm water and leave for several hours. Then eat it just like that or add it to porridge, soup” (L. Lankmane, naturopath, phytotherapeutist). - You can try to consume more foods that normalize the balance of intestinal flora - such as kefir (preferably homemade), miso soup, sauerkraut.
- You should not get carried away with strong tea, black coffee, cocoa, chocolate, white bread, flour and slimy soups, semolina, blueberries. All these products, like dry food, have a fixing effect. For the time of problems with the gastrointestinal tract, it is better to observe separate fractional meals, drink liquid 15 minutes before meals or some time later, etc. - that is, to facilitate the assimilation of the food consumed as much as possible. Make sure that there are no distortions - the daily diet should be balanced.
HOW TO HELP
- You can drink enzymatic preparations for a short time.
 If these are preparations of animal origin - no more than 7 days, plant enzymes can be taken longer. You can take probiotics, beneficial gut bacteria that aid digestion. Long-term use of these biological products not only normalizes the intestinal flora, but also contributes to a less pronounced manifestation of dysbacteriosis in a newborn child. (D.V. Arkhipova, homeopath, PhD, pediatrician)
If these are preparations of animal origin - no more than 7 days, plant enzymes can be taken longer. You can take probiotics, beneficial gut bacteria that aid digestion. Long-term use of these biological products not only normalizes the intestinal flora, but also contributes to a less pronounced manifestation of dysbacteriosis in a newborn child. (D.V. Arkhipova, homeopath, PhD, pediatrician) - Check the level of iron with a doctor - against the background of its deficiency, there may also be disturbances in the work of the intestines. “But keep in mind that some iron-containing dietary supplements, unfortunately, can only worsen this condition (not to mention dosage forms). It is better to add foods rich in iron, such as almonds, pine nuts, apricots, avocados, sunflower and pumpkin seeds, wheat germ ”(L. Lankmane, naturopath, herbalist).
- Freshly squeezed juices, diluted 1 to 1 with water 15 minutes before meals, stimulate the production of pancreatic enzymes and aid digestion in the most natural way.
 (D.V. Arkhipova, homeopath, PhD, pediatrician)
(D.V. Arkhipova, homeopath, PhD, pediatrician) - Drink hot - as far as possible - water on an empty stomach, a little later, eat half a banana, chewing it for a long time and macerating it with saliva to a liquid slurry (the banana must be ripe!). (O.L. Bannikova, obstetrician).
- Starting from the second trimester, you can use essential oils: exotic basil (Ocimum basilicum in Latin), seaside pine (Pinus Pinaster), saro (Cinnamosma fragrans, Saro), rosewood (Aniba rosaeodora). “Oils should be only edible, of good quality! It is not recommended to use essential oils during the first 3 months of pregnancy. 1st composition - take 1 drop of basil, 2 drops of pine on a small piece of sugar or honey and suck under the tongue in the morning on an empty stomach. 2nd composition - basil 30 drops, rosewood 20 drops, saro 10 drops and 40 drops of apricot kernel oil or any other unrefined food oil. Mix. Take 3 drops of this mixture under the tongue on sugar or honey morning and evening before meals for 5-7 days or as needed.
 When buying aroma oils, be sure to check whether there is information on the packaging that this oil can be eaten. (O.L. Bannikova, obstetrician)
When buying aroma oils, be sure to check whether there is information on the packaging that this oil can be eaten. (O.L. Bannikova, obstetrician) - If this does not help, you can try to use "Duphalac" for a short time.
LIFESTYLE
Enough physical activity, swimming in the pool. Walking for at least one hour. But the load should be increased gradually. To begin with, one lesson should be no more than 30 minutes. The step should be slow, the shoes are comfortable, and the route should be laid away from the roads. Gymnastics for pregnant women for at least 30 minutes daily. As gymnastics, our yoga instructor for pregnant women Svetlana Shnyrova recommends a few simple exercises:
- backbends in cat pose (standing on all fours),
- alternating leg raises from a sitting position on the floor with support on the hands,
- certain types of soft twists of the spine from a sitting or lying position,
- Breathing exercises such as a few deep belly breaths can also help.