Swollen vagina while pregnant
How to Ease Vaginal Swelling During Pregnancy
Swelling is a common side effect of pregnancy, especially when it comes to your feet and hands. But there’s one area that can also swell during pregnancy that doesn’t get a lot of attention: Your vagina. If you notice you have a swollen vagina during pregnancy, know you’re not the only woman going through this! Still, we’re guessing you might have questions about why this is happening. Here’s what you need to know, plus how to minimize the swelling and ease any discomfort.
In this article:
Symptoms of vaginal swelling during pregnancy
What causes vaginal swelling during pregnancy?
How to reduce vaginal swelling during pregnancy
How to prevent vaginal swelling during pregnancy
Symptoms of Vaginal Swelling During Pregnancy
Every woman and every pregnancy is different—which means the symptoms of vaginal swelling during pregnancy can differ from person to person. In general, though, you might experience the following:
• Noticeable swelling. You’re probably familiar on at least some level with what your vulva and vaginal area usually feels like. If it’s swollen, it can feel noticeably bigger or puffier, says Frederick Friedman, Jr., MD, associate professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai in New York City. “There may just be a general feeling of swelling or fullness in the vaginal area,” adds Julie Lamppa, APRN, CNM, a certified nurse midwife at Mayo Clinic, which can lead to overall discomfort.
• Bumps. Some women who experience vaginal swelling during pregnancy can have varicose veins surface in their vulvar area, which can cause swelling and a bumpy feel down there, Lamppa says.
• Itchiness. This isn’t the case for every woman, but itchiness can sometimes accompany vaginal swelling, Lamppa says.
What Causes Vaginal Swelling During Pregnancy?
There are several reasons why you might develop vaginal swelling in pregnancy.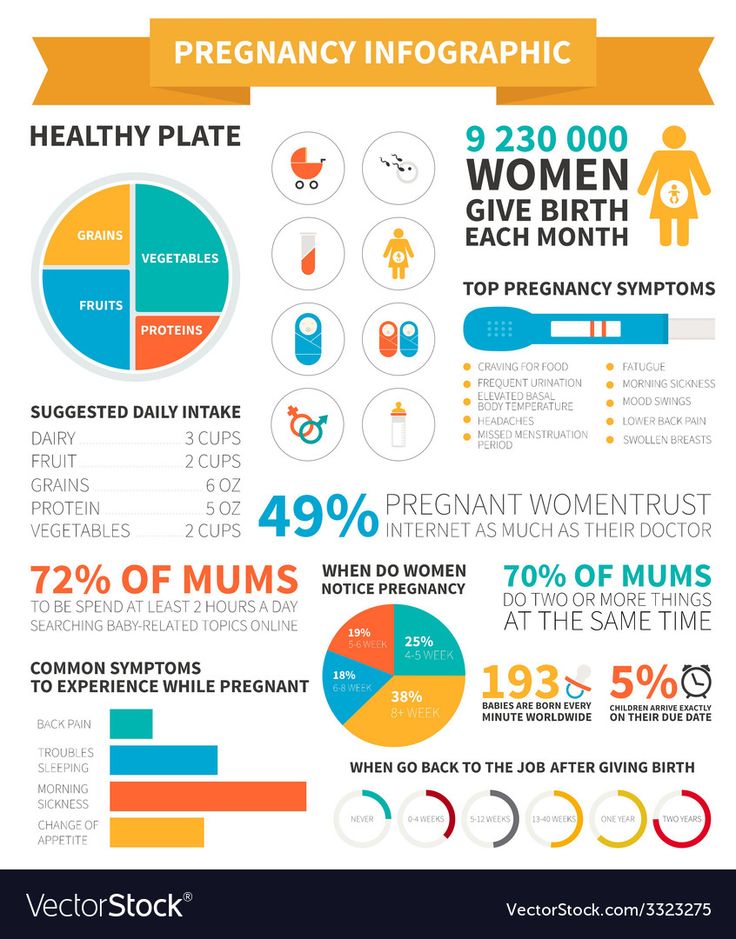 Here are some of the most common ones:
Here are some of the most common ones:
• An increase in blood volume. Your blood volume increases during pregnancy to help support the growing baby. As your uterus grows, there’s also an increase in pressure of the blood vessels in your pelvis, Lamppa explains. The combination of these two things can lead to swelling.
• Varicose veins in your vulva. Varicose veins are swollen, bumpy veins that develop when valves let blood pool in one spot or flow backward. Just like you can develop varicose veins in your legs, you can also develop these in your vulva during pregnancy, Lamppa says. “These aren’t dangerous, but they can be alarming to women when they suddenly show up.”
• A yeast infection. Yeast infections are common among moms-to-be, and they can also lead to a swollen vagina during pregnancy, Friedman says. “The inflammation that results from the infection can cause more swelling,” he explains.
• Excess fluid. Excess fluid can get trapped in your body’s tissues during pregnancy, and that can cause swelling down there, Friedman says.
Excess fluid can get trapped in your body’s tissues during pregnancy, and that can cause swelling down there, Friedman says.
How to Reduce Vaginal Swelling During Pregnancy
If you suspect that your vaginal swelling is due to excess fluid, compression or support stockings might help. “There are products on the market that you can buy that give vulvar support,” Lamppa says. (Just check in with your doctor first to make sure it’s okay for you to use.)
For direct relief, Lamppa recommends applying a cool pack directly to your vulva. That should help with discomfort as well as cut down on some of the swelling.
If you’re experiencing vaginal swelling along with symptoms of a yeast infection—such as an itchy vaginal area during pregnancy, accompanied by white vaginal discharge—Lamppa recommends seeing your doctor for an evaluation. If they determine that you do, in fact, have a yeast infection, your care provider will likely recommend that you use an over-the-counter cream.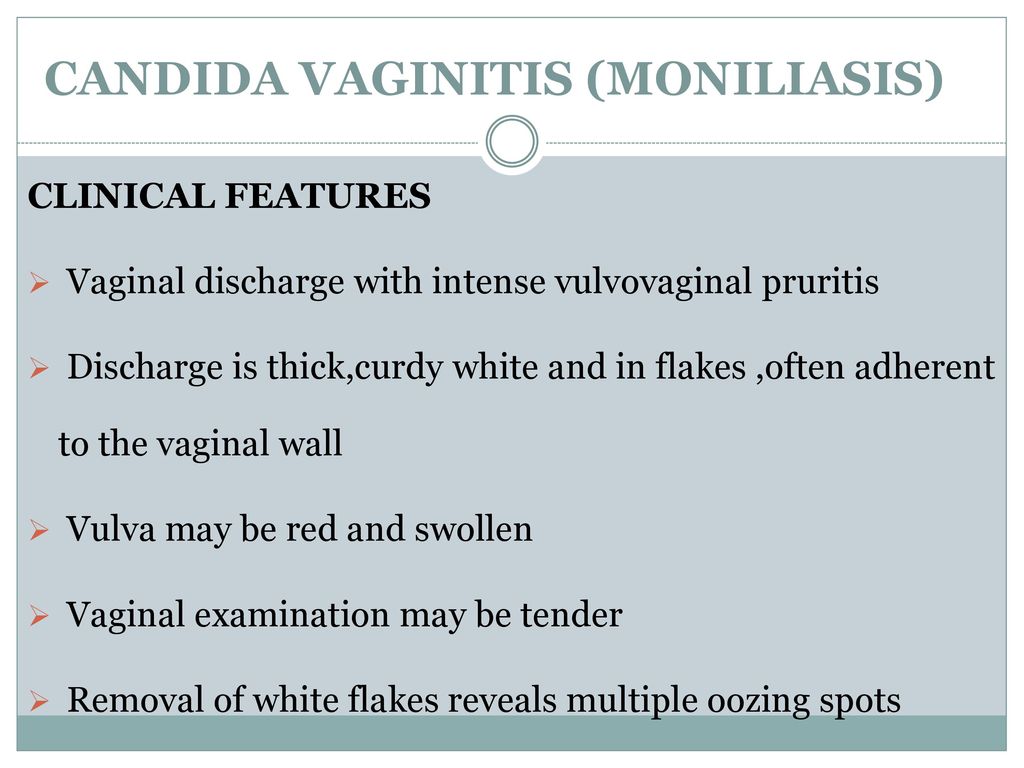
How to Prevent Vaginal Swelling During Pregnancy
Sorry, but there isn’t a ton you can do to lower the odds you’ll experience vaginal swelling during pregnancy, given that it’s a normal side effect of being pregnant, Lamppa says. However, doing your best to avoid sitting or standing for long periods of time may be helpful, Friedman suggests.
While it’s pretty common, it’s a good idea to flag any vaginal swelling during pregnancy for your care provider so they can help pinpoint the cause and get you sweet relief ASAP.
Updated January 2020
Expert bios:
Frederick Friedman, Jr., MD, is an associate professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai. He also serves as director for both the division of obstetrics and the division of generalists in the department of obstetrics, gynecology and reproductive science at the Mount Sinai Health System, and maintains a clinical practice in general obstetrics and gynecology.
Julie Lamppa, APRN, CNM, is a certified nurse midwife and medical editor at Mayo Clinic, and maintains a midwifery practice in Rochester, New York.
*Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances. *
Plus, more from The Bump:
Swelling in Pregnancy: Why It Happens and How to Deal
How Your Vaginal Discharge Can Change During Pregnancy
10 Surprising Pregnancy Symptoms No One Warned You About
How to Treat a Swollen Perineum During Pregnancy
Your perineum is the small area of skin and muscle located between the vagina and the anus.
By the third trimester of pregnancy, your baby is gaining weight and dropping lower in your pelvis. The added pressure can lead to swelling of the genitals and perineum. At the same time, your perineum is starting to stretch in preparation for childbirth.
At the same time, your perineum is starting to stretch in preparation for childbirth.
A sore perineum due to pregnancy is a temporary condition, though it can be uncomfortable.
The perineum is stretched even more during childbirth. It’s not uncommon for the perineum to tear as your baby passes through.
According to the American College of Nurse-Midwives (ACNM), anywhere from 40 to 85 percent of women have a tear during vaginal delivery. About two-thirds of them require stitches to repair the damage.
To decrease the chances of a ragged tear, your doctor may cut the perineum. This procedure is called an episiotomy. This gives baby more room to pass through without causing severe tears.
Whether you experience a tear or have an episiotomy, your perineum is a delicate area. Even tiny tears can cause swelling, burning, and itching. A large tear can be quite painful. Episiotomy stitches can feel sore and uncomfortable.
The symptoms can last a few days to several months. During that time, it may be difficult to sit or walk comfortably.
During that time, it may be difficult to sit or walk comfortably.
Pregnancy and childbirth are the most common causes of a sore perineum. Other things can lead to a sore perineum, but it’s not always easy to find the cause.
Something as simple as tight pants or sitting in an uncomfortable position for too long can cause soreness of the vulvar area or perineum. Intercourse without sufficient lubrication can also cause a sore perineum.
Generalized vulvodynia refers to a chronic pain in the vulvar area without an obvious cause. The pain can affect the entire area, including the labia, clitoris, and perineum.
Descending perineum syndrome occurs when the perineum balloons beyond its standard positioning. This might happen if you have an ongoing problem defecating or urinating and you strain too hard. If you have a descending perineum, the first step is to determine the cause.
It could also be referred pain. If you have unexplained pain, a healthcare professional will likely begin with a complete gynecological examination to diagnose the concern.
A 2013 study indicated that some women have a higher risk for certain types of perineal tearing during childbirth. Risk factors include:
- delivering a baby when you’re an adolescent
- being 27 years old or over
- having a baby with a high birth weight
- having an instrumental delivery
Having more than one of these risk factors makes a perineal tear significantly more likely. In this case, your doctor may consider an episiotomy to try and prevent a tear.
If you have a sore perineum, sitting can make it worse. One simple and inexpensive fix is a hemorrhoid or donut cushion to keep your weight off of your perineum when you sit.
Massaging the area during pregnancy may help relieve soreness and prepare the perineum for childbirth.
Some women find that using an ice or a cold pack relieves symptoms such as swelling, itching, and burning of the perineum. However, a 2007 paper, updated in 2019, concluded that there’s only a small amount of evidence that cooling treatments are safe and effective in relieving perineal pain.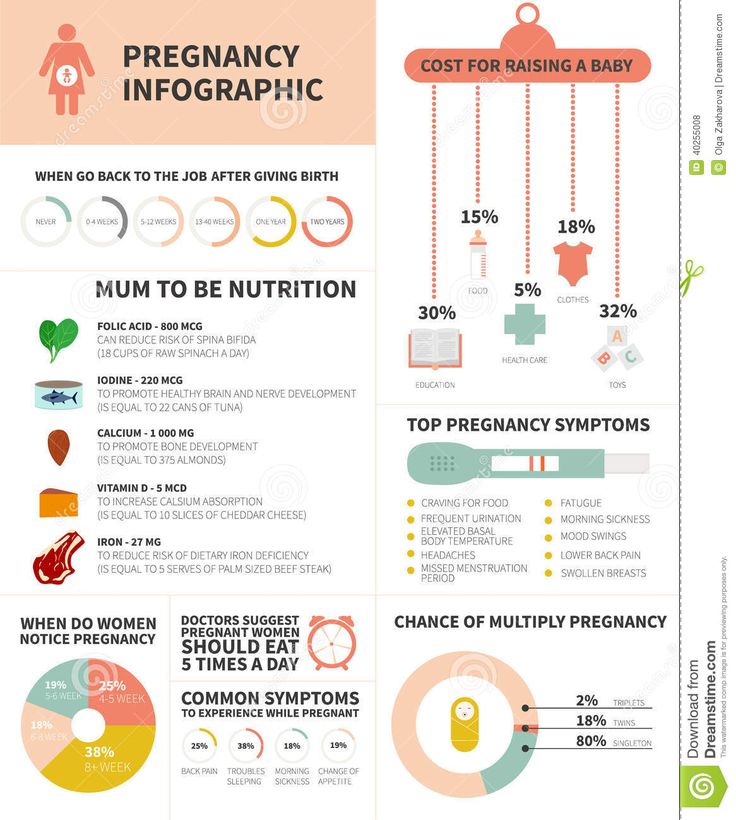
If you’ve experienced a tear or an episiotomy, your doctor will provide aftercare instructions. It’s important that you follow them carefully.
They’ll probably give you a perineal irrigation bottle. You can use it to squirt warm water on the area to clean and soothe it, especially after going to the bathroom.
To help prevent infection, you’ll need to keep the area very clean. A warm, shallow bath may help temporarily relieve discomfort. Use a clean towel to pat yourself dry rather than rubbing the area. You shouldn’t have a bubble bath or use other products with harsh ingredients until it’s completely healed.
Taking care of vaginal tears: Are you missing a step?
Will the soreness eventually get better?
How much soreness you have and how long it will last can vary depending on the person. It has a lot to do with the cause. If you’ve had extensive tearing and swelling, it may take longer to heal.
For most people, childbirth-related soreness of the perineum subsides within a few days to a few weeks.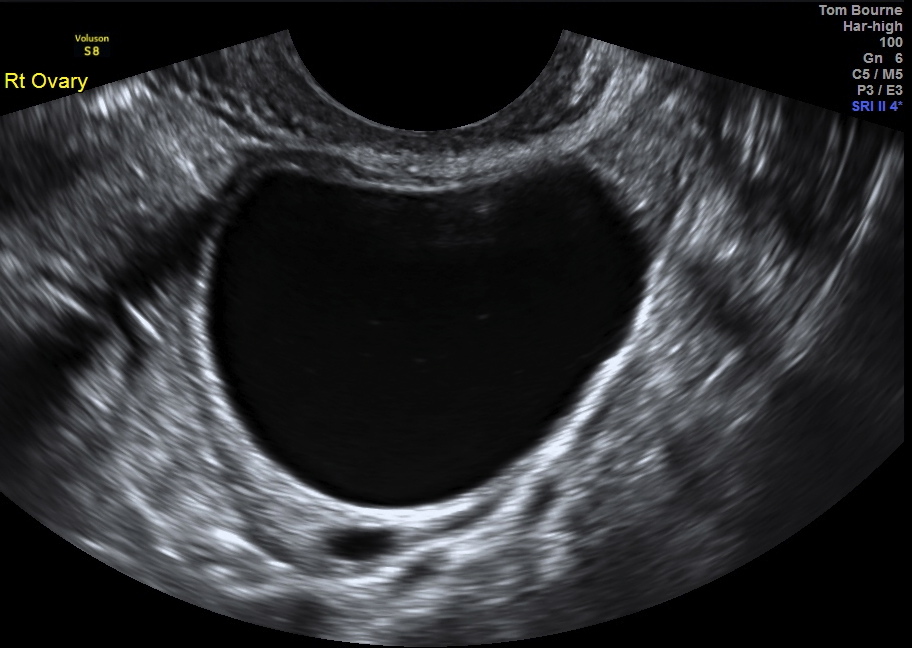 There are usually no long-term effects.
There are usually no long-term effects.
Reach out to a doctor if the soreness doesn’t seem to be improving or it’s getting worse. You should also call a doctor if you have:
- a fever
- foul-smelling discharge
- perineal bleeding
- difficulty urinating
- severe pain
- swelling
- problems with perineal stitches
If you’re prone to perineal soreness, try to avoid wearing pants that are too tight. You should also make sure you’re well lubricated before having intercourse.
If you’re pregnant, you might benefit from a perineal massage. According to Brighton and Sussex University Hospitals, studies show that in a first pregnancy, perineal massage after the 34th week can reduce perineal tearing.
To prepare for self-massage, the ACNM suggests you cut your fingernails short and wash your hands well. Relax, with your knees bent. Use pillows for added comfort.
You’ll need to lubricate your thumbs as well as the perineum. You can use vitamin E oil, almond oil, or vegetable oil. If you prefer, you can use a water-soluble jelly. Don’t use baby oil, mineral oil, or petroleum jelly.
You can use vitamin E oil, almond oil, or vegetable oil. If you prefer, you can use a water-soluble jelly. Don’t use baby oil, mineral oil, or petroleum jelly.
To massage:
- Insert your thumbs about 1 to 1.5 inches into your vagina.
- Press down and to the sides until you feel it stretch.
- Hold for 1 or 2 minutes.
- Use your thumbs to slowly massage the lower part of your vagina in a U shape.
- Concentrate on keeping your muscles relaxed.
- Massage the perineum this way for about 10 minutes per day.
If you’re not comfortable doing it yourself, a partner can do it for you. Partners should use the same technique, but with index fingers instead of thumbs.
Do perineal massages make labor less painful?
COLPITIS DURING PREGNANCY
During pregnancy, a woman, as a rule, takes special care of her health and reacts anxiously to every unusual symptom.
Unusual discharge and discomfort in the genital area are often the cause of the expectant mother's panic.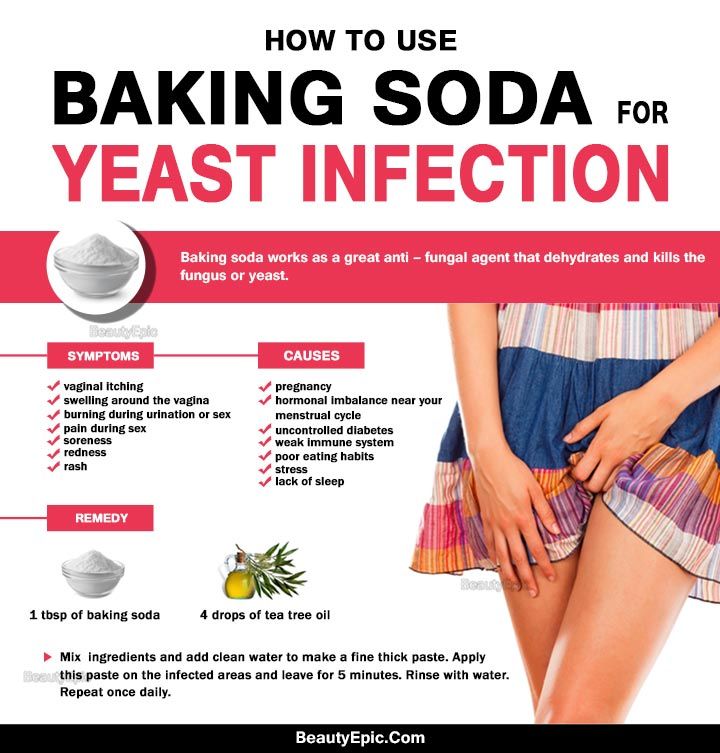 Such a complex of symptoms most likely indicates the development of a pathological process, which in medicine is called vaginitis or colpitis. In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman.
Such a complex of symptoms most likely indicates the development of a pathological process, which in medicine is called vaginitis or colpitis. In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman.
Vaginitis during pregnancy is a good reason to immediately contact a gynecologist and start treating this dangerous pathology. Diagnose the disease and determine how to treat colpitis during pregnancy without harming the mother and baby, qualified gynecologists will prompt.
Symptoms of colpitis during pregnancy
First of all, it should be determined that vaginitis or colpitis is an inflammatory disease that involves the mucous membranes of the vagina. The inflamed walls of the vagina swell and undergo hyperemia. Also, single hemorrhages are noted on the surface of the vaginal tissues. If the inflammation does not spread beyond the vagina, the woman does not notice visual manifestations of the disease, while in some cases the pathological process affects the external genitalia.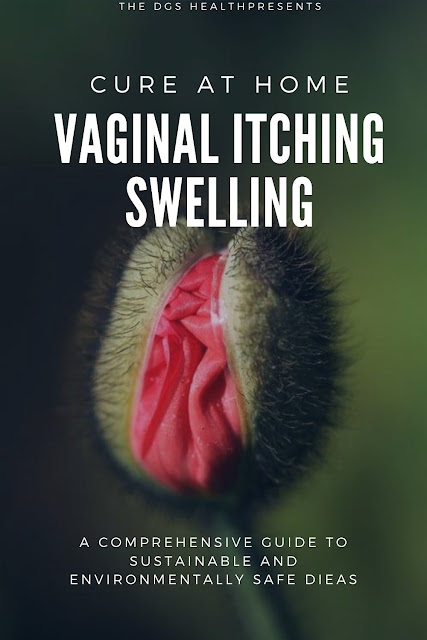 In this case, inflammation can be seen with the naked eye.
In this case, inflammation can be seen with the naked eye.
The characteristic signs of colpitis during pregnancy do not differ from the symptoms of a non-pregnant woman:
- itching and burning in the vaginal area - the inflammatory process irritates the delicate mucous membranes, which causes discomfort and sometimes pain in the vaginal walls;
- pain in the lower abdomen - this symptom is especially frightening for pregnant women, but it is not associated with the tone of the uterus, as many assume, but with inflammation of the tissues;
- the appearance of specific discharge - the discharge during colpitis during pregnancy is very abundant and may have a different color and consistency. Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
- swelling and redness of the genital organs - patients often notice hyperemia and swelling of the labia and clitoris, which become more sensitive and cause discomfort to the woman.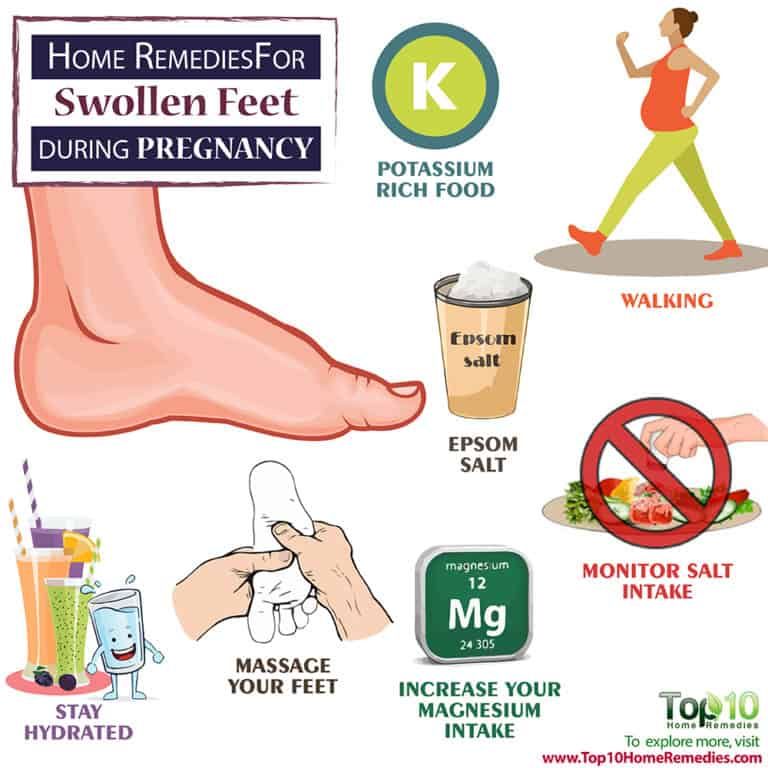
Acute vaginitis during pregnancy is accompanied by severe symptoms, which should make the patient seek professional help. This will help protect the child from possible negative consequences.
Causes and types of vaginitis during pregnancy
Inflammation of the mucous membranes of the vagina is usually of an infectious nature. This becomes possible due to vaginal dysbacteriosis, which often accompanies the period of pregnancy. Hormonal changes and high loads on all organs of the expectant mother cause a decrease in the body's defenses, which provokes an infectious and inflammatory process. In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.
It is interesting that depending on the cause of the development of the disease, its symptoms and manifestations may differ:
- candidal colpitis - accompanied by abundant cheesy discharge and severe itching of the genital organs, which manifests itself even at rest;
- emphysematous colpitis - a very common type of vaginitis in pregnant women. Pathology is accompanied by the formation of small watery vesicles on the surface of the mucous membranes of the genital organs. This form of colpitis resolves on its own in 2-3 weeks after childbirth;
- Trichomonas colpitis is a very dangerous form of pathology that develops when Trichomonas enters the vaginal environment. Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Concomitant conditions for the development of colpitis in a pregnant woman, in addition to a decrease in immunity, may be allergic reactions, microtrauma of the vagina, non-observance of personal hygiene, the presence of chronic diseases.
Colpitis during pregnancy: consequences for the child
Inflammation of the mucous membranes of the vagina poses a threat not only to the health of the expectant mother, but also to the baby. The ascending route of infection can lead to pregnancy abnormalities such as polyhydramnios, premature birth, and infection of the amniotic fluid. Vaginitis is especially dangerous during childbirth, when the baby passes through an infected maternal birth canal. In at this moment there is a high probability of infection newborn.
Interestingly, colpitis after pregnancy can go away on its own, but this happens relatively rarely. The development of colpitis after childbirth is most often provoked by trauma to the vaginal membranes during delivery. In connection with this fact, doctors recommend abstaining from sexual activity for the first weeks after childbirth. Violating this prohibition, a woman increases the risk of developing colpitis after childbirth.
Treatment of colpitis during pregnancy
Diagnosis of the disease involves a standard gynecological examination and colposcopy. This research method makes it possible to visualize the surface of the mucous membrane of the walls of the vagina and assess their condition. During the examination, the doctor takes a smear for analysis. The study of biological material is carried out by bacterioscopic and bacteriological methods.
Treatment of colpitis in pregnant women requires a rational approach to prescribing antibiotics. The doctor selects an antibacterial drug that can suppress the pathogen detected in the smear, and at the same time does not have a negative effect on the fetus. Often preference is given to local forms of antibiotics - suppositories, ointments and tampons. Treatment is supplemented with general strengthening therapy and safe physiotherapy procedures.
Changes in a woman's body during pregnancy
From the very first days of pregnancy, the body of a pregnant woman undergoes profound transformations. These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body.
These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body.
During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth. Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy.
The respiratory system during pregnancy works hard. The respiratory rate increases. This is due to an increase in the need of the mother and fetus for oxygen, as well as in the limitation of the respiratory movements of the diaphragm due to an increase in the size of the uterus, which occupies a significant space of the abdominal cavity.
Cardio The mother's vascular system has to pump more blood during pregnancy to ensure an adequate supply of nutrients and oxygen to the fetus. In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of the blood vessels during pregnancy decreases, which creates favorable conditions for enhanced
In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of the blood vessels during pregnancy decreases, which creates favorable conditions for enhanced
to supply tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. and changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
Kidneys work hard during pregnancy. They secrete decay products of substances from the body of the mother and fetus (the waste products of the fetus pass through the placenta into the mother's blood).
Changes in the digestive system are represented by increased appetite (in most cases), craving for salty and sour foods. In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur.
The most significant changes, however, occur in the genitals of pregnant women. These changes prepare the woman's reproductive system for childbirth and breastfeeding.
These changes prepare the woman's reproductive system for childbirth and breastfeeding.
The uterus of a pregnant woman increases significantly in size. Its mass increases from 50 g - at the beginning of pregnancy to 1200 g - at the end of pregnancy. The volume of the uterine cavity by the end of pregnancy increases by more than 500 times! The blood supply to the uterus is greatly increased. In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy.
The walls of the vagina will loosen and become more elastic.
External genitalia (labia minor and major), also increase in size and become more elastic. The tissues of the perineum are loosened. In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
Skin in the genital area and in the midline of the abdomen usually becomes darker in color. Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Mammary glands increase in size, become more elastic, tense. When pressing on the nipple, colostrum (first milk) is released. Changes of the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This accomplishes two goals. On the one hand, this helps to reduce the rigidity of the joints between the pelvic bones (especially the pubic joint) and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
It should be noted that calcium compounds are washed out of all bones of the maternal skeleton (including the bones of the foot and spine). As shown earlier, a woman's weight increases during pregnancy by 10 -12 kg. This additional load against the background of a decrease in bone stiffness can cause foot deformity and the development of flat feet. A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
Changes in the nervous system . In the first months of pregnancy and at the end of it, there is a decrease in the excitability of the cerebral cortex, which reaches its greatest degree by the time of the onset of childbirth. By the same period, the excitability of the receptors of the pregnant uterus increases. At the beginning of pregnancy, there is an increase in the tone of the vagus nerve, in connection with which various phenomena often occur: changes in taste and smell, nausea, increased salivation, etc.
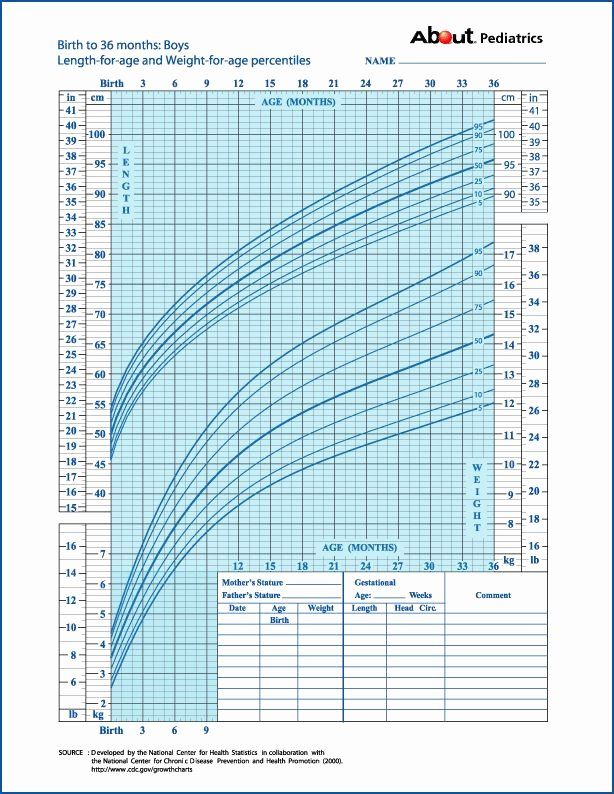
Active endocrine glands there are significant changes that contribute to the proper course of pregnancy and childbirth. Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.
Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.
Conclusion. Summarizing the facts concerning changes in a woman's body during pregnancy, it is worth emphasizing that these changes reflect the processes of physiological adaptation of the mother's body to the process of intrauterine development of the fetus. Therefore, measures aimed at preventing the pathology of pregnancy should be, first of all, natural, physiological. This is a proper and balanced diet, smoking cessation, a sufficient level of physical activity and fluid intake. In a healthy woman, such approaches ensure the normal course of pregnancy and adequate preparation of the mother's body for childbirth and breastfeeding.