Stuffy during pregnancy
Relief for Ongoing Nasal Congestion Is Possible
If you're expecting a baby, you may be dealing with a stuffy nose that doesn’t seem to go away. This hassle is called pregnancy rhinitis. The cause of this condition isn’t really clear. However, it may be caused by hormonal changes.Having a history of allergies or asthma does not raise your risk of getting pregnancy rhinitis.
More than just a stuffy nose
Pregnancy rhinitis is an inflammation of the mucous membranes lining the nose. This causes nasal congestion. Increased blood flow to the nasal passages and enlargement of the nasal veins also play a role.
Symptoms occur during pregnancy. They can last for several weeks. On top of feeling uncomfortable, your sleep may be disrupted. This is because the congestion gets worse when you lie down. This may make you to feel more tired during the day. Long-lasting congestion also can lead to complications. These can include sinusitis and ear infections.
Be cautious when seeking treatment
Many women use non-prescription, over-the-counter (OTC) decongestant sprays to open up their nasal passages. Know that these medicines don’t work for pregnancy rhinitis. These medicines may give you temporary relief. However, they may actually make your symptoms worse and lead to a complete nasal blockage.
How can you get relief from pregnancy rhinitis? Experts say you can breathe easy with these measures:
-
Don’t use OTC nasal decongestants.
-
Drink plenty of fluids.
-
Increase the humidity levels in your home. Use a humidifier.
-
Don’t use nasal irritants, such as cigarette smoke.
-
Get moving. Regular, moderate-intensity exercise can reduce congestion. It can also help you sleep better. But first, check with your healthcare provider to see what exercises are safe for you.
-
When you go to sleep, raise the head of your bed. For instance, use an extra pillow or a wedge.

-
Ask your healthcare provider about using OTC nasal strips and saline sprays or drops.
The good news? Even if you don’t do anything, you can expect your stuffy nose to clear up soon after your baby is born. It often goes away within two weeks of childbirth.
Online Medical Reviewer: Bowers, Nancy, RN, BSN, MPH Foley, Maryann, RN, BSN
Date Last Reviewed: 4/12/2016
© 2000-2019 The StayWell Company, LLC. 800 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
© 2000-2019 The StayWell Company, LLC. 800 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Baby (and tissues!) on board: Tips for managing pregnancy rhinitis | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
October 6, 2020
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
When you think of side effects or symptoms brought on by pregnancy, nasal congestion and runny nose are not typically among the first to come to mind.
But maybe they should. Having a stuffy nose, difficulty breathing or sleeping, and snoring when pregnant can be alarming, especially amid the COVID-19 pandemic and the start of flu season.
Pregnancy rhinitis, also called gestational rhinitis, is a common ailment in the second and third trimesters, affecting approximately 20% of women. Characterized by inflammation and swelling of the mucous membranes in the nose, pregnancy rhinitis symptoms include congestion (nasal obstruction), sneezing, postnasal drip, and runny nose. These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
All these issues can dramatically affect your mood and quality of life. The good news is that, for most patients, pregnancy rhinitis is temporary and there are safe, effective treatments available.
I've invited my colleague, Ashleigh Halderman, M.D., an ear, nose, and throat specialist at UT Southwestern to explain in more detail the causes of pregnancy rhinitis and how patients can manage their symptoms.
What causes pregnancy rhinitis?
Dr. Ashleigh HaldermanThe root cause of rhinitis can be allergic (affected by environmental irritants) or non-allergic (caused by infection). However, we are still learning how rhinitis is related to pregnancy.
We know that smoking, as well as having chronic rhinitis before pregnancy, predisposes patients to developing pregnancy rhinitis. Research suggests a few more potential causes:
Research suggests a few more potential causes:
- Having extra fluid in the body: During pregnancy, the body makes more blood and fluids, which can cause swelling, even in unexpected places such as the nasal passages. Blood vessels in the nose can swell with this additional volume, causing stuffiness.
- Higher levels of estrogen: Estrogen in older formulations of birth control pills has been associated with a side effect of nasal obstruction. However, in studies of the menstrual cycle, we don't see congestion with fluctuating estrogen levels. So, the connection remains unclear for now.
- Creation of human growth hormone: The placenta creates a variant of the human growth hormone (HGH), which has been associated with nasal symptoms in other conditions. For example, tumors that grow on the pituitary glands secrete growth hormones, which can cause severe nasal congestion.
Gestational rhinitis is under-researched. Data to date suggest no known association of rhinitis with pre-existing asthma, maternal age, duration of pregnancy, or the number of times a patient has been pregnant. However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
Related reading: How to manage allergies and asthma during pregnancy
How long do symptoms last?
The annoying, uncomfortable symptoms of pregnancy rhinitis typically last six weeks or longer. For most patients, symptoms typically resolve two weeks after delivery.
Approximately a third of patients who had chronic rhinitis before pregnancy will have the same level of symptoms during, and a third will experience worsening of rhinitis symptoms. However, the remaining third will have less severe or no symptoms during pregnancy. I've had many women tell me they've felt the best, sinus-wise, when they were pregnant. However, there's no specific reason why this occurs.
Related reading: 5 weird pregnancy symptoms you might not know about
What treatments are available?
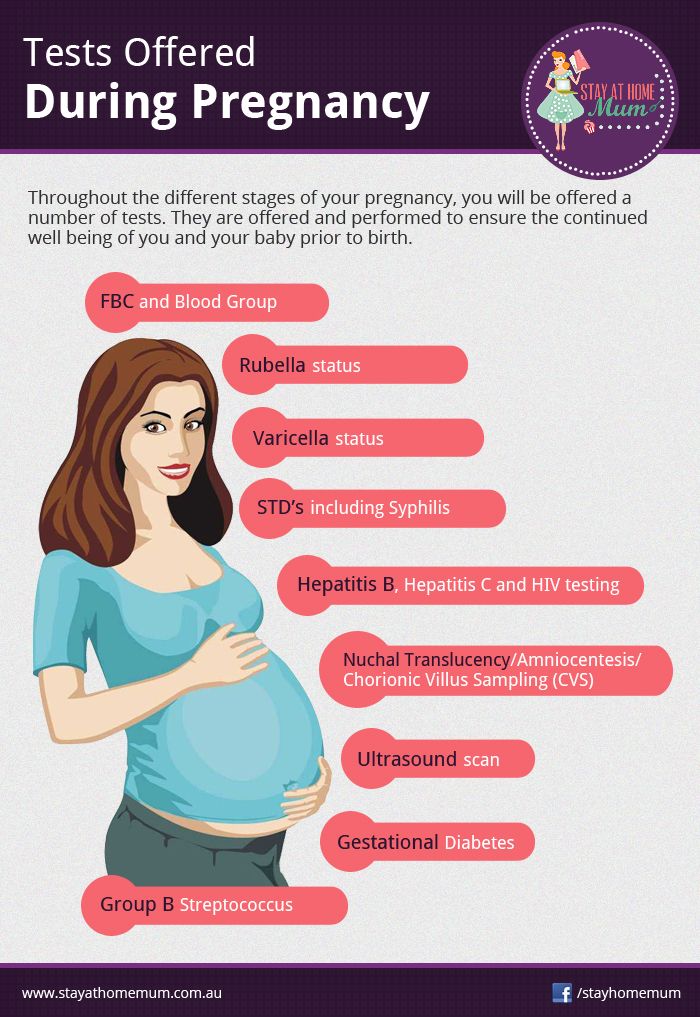
The first step toward relief is a visit with your doctor to rule out infection, such as COVID-19, influenza, or sinusitis. We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
From there, your doctor and Ob/Gyn may suggest:
- Getting regular exercise: Working out has been shown to significantly help relieve nasal congestion and regulate the sleep cycle. All the more reason to bust a move during pregnancy!
- Elevating your mattress: Try positioning the mattress so your whole body is situated at a 45-degree angle. While not widely studied, patients have reported that this helps clear the nasal passages enough to sleep.
- Using a humidifier: Adding a little moisture to the air can help alleviate nasal irritation. Many patients use them at night to wake up feeling less stuffy.
- Trying a sinus wash: Nasal saline sprays or sinus irrigation systems such as a neti pot can help clear the sinuses. Make sure to use distilled or boiled (and cooled) water – using water straight from the tap is not recommended.

Topical decongestants such as Afrin can be incredibly and immediately effective, but there is a risk of dependency. If you use this type of treatment more than once or twice a week, your nose can become "addicted" to it, which can lead to rhinitis medicamentosa – the spray will stop working as well, and your symptoms may get worse. Also, unlike gestational rhinitis, rhinitis medicamentosa won’t resolve after you deliver. It will only resolve when you stop using topical decongestants.
In general, pregnant patients can take decongestants that include pseudoephedrine as directed. However, we always recommend talking with your Ob/Gyn first, especially if you have high blood pressure.
Your Ob/Gyn might also recommend a steroid nasal spray, such as Flonase or Rhinocort, for severe symptoms. If you were using a spray to manage chronic rhinitis prior to pregnancy, your Ob/Gyn might advise you to keep using it during pregnancy. It is generally considered safe to use these products while breastfeeding, under your Ob/Gyn's guidance.
Your body will change in interesting ways during pregnancy. If you have new or unusual symptoms, call your doctor. We'll help you sort out what's normal from what could be a sinus infection or respiratory illness.
To talk with a doctor about nasal symptoms during pregnancy, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
Your Pregnancy Matters
- Emily Adhikari, M.
 D.
D.
August 2, 2022
More Articles
Shortness of breath and shortness of breath during pregnancy In addition to positive emotions from waiting for the baby, the “interesting position” also brings a number of inconveniences. A common problem during pregnancy is lack of air, resulting in shortness of breath. What is this state? Is it so dangerous and is there a way to alleviate it? Let's figure it out together.
Causes of shortness of breath in pregnant women
There are several main reasons why it is difficult to breathe during pregnancy:
- as the fetus grows, the pressure in the abdominal cavity begins to increase. This causes the diaphragm to move upward, therefore, a woman has a feeling of lack of air,
- hormonal changes in the body - pregnant women actively produce estrogen and progesterone.
 Last sends a signal to the respiratory center in the brain, so the woman begins to breathe deeper and more often,
Last sends a signal to the respiratory center in the brain, so the woman begins to breathe deeper and more often, - additional factors - wearing uncomfortable clothing, taking the wrong posture (for example, many pregnant women find it difficult to breathe when lying on their backs), chronic respiratory disease systems that can become aggravated during pregnancy, overweight, systematic overeating.
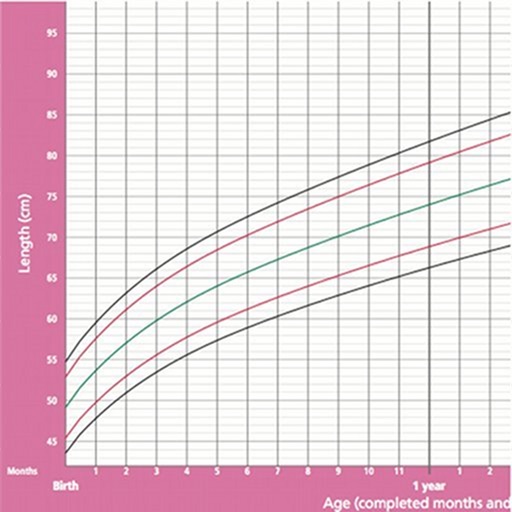
In most cases, breathing becomes difficult during pregnancy around the third trimester. In that period, the fetus already reaches a significant size (up to 44-46 cm in length) and exerts pressure on many organs, including the respiratory system.
Is there any reason for concern?
Every expectant mother is interested in the question - can the appearance of shortness of breath lead to a lack of air in a child?
The answer to this question is unambiguously negative. The appearance of shortness of breath in a healthy woman in position is regarded as normal physiological phenomenon. Therefore, in most cases there is no cause for concern.
The appearance of shortness of breath in a healthy woman in position is regarded as normal physiological phenomenon. Therefore, in most cases there is no cause for concern.
On the contrary, actively produced progesterone contributes to an increase in the concentration of oxygen in the blood of a pregnant woman women.
There are several main factors provoking difficulty in breathing in an expectant mother:
- physical activity (shortness of breath may appear when walking, bending over, climbing stairs, etc.),
- if a woman is expecting twins or triplets (in this case, the pressure on the diaphragm is even greater than with a singleton pregnancy),
- in certain positions (for example, if the woman is lying straight on her back),
- in cases where the body is experiencing general fatigue.
Although the occurrence of dyspnea is not considered abnormal, it is necessary to assess the situation in in general. The following factors are taken into account: at what stage of pregnancy it is difficult to breathe, whether women chronic pathologies of the respiratory system, whether there were any additional complications, etc. Only after studying the totality of these factors, it is possible to give an accurate answer to the question of whether this condition is dangerous or not in specific case.
The following factors are taken into account: at what stage of pregnancy it is difficult to breathe, whether women chronic pathologies of the respiratory system, whether there were any additional complications, etc. Only after studying the totality of these factors, it is possible to give an accurate answer to the question of whether this condition is dangerous or not in specific case.
When is shortness of breath a danger to the woman and the fetus?
Shortness of breath during early or late pregnancy is not always safe for mother and baby. Sometimes she is signaling the presence of a particular threat.
There are several signs that should definitely alert:
- shortness of breath accompanied by rapid heartbeat,
- difficulty in breathing occurs spontaneously, while the woman's lips turn blue, weakness and sweating appear,
- severe chest pain and arrhythmia,
- exacerbated bronchial asthma.

The appearance of such symptoms may indicate the development of pathologies of the cardiovascular system, anemia (low hemoglobin in the blood), respiratory diseases. In this case, you should immediately seek advice to the doctor. The specialist will listen to complaints, prescribe the necessary examinations (for example, a laboratory blood test, ECG, etc.) and establish an accurate diagnosis.
Remember - ignoring the above symptoms can lead to fetal hypoxia. This is very dangerous a condition with many severe consequences. Therefore, it is better to play it safe and spend everything necessary examinations.
How to alleviate the condition of a pregnant woman: effective ways
If, apart from shortness of breath, a pregnant woman no longer has any symptoms indicating the development of serious pathologies, then the only task is to alleviate this condition.
There are quite a few ways that will make the signs of shortness of breath less pronounced:
- Performing breathing exercises - a few simple exercises will help to quickly relieve an attack of shortness of breath.
 What can Do: Raise your arms above your head and take 3 deep breaths in and out. Another option is to take a deep breath, hold for 5 seconds, and then exhale slowly, Another exercise according to the "4/7/8" method: you need to take a breath, (counting to 4), hold your breath (counting to 7) and exhale slowly (counting 8 seconds). This exercise can be done 10-12 times with short pauses.
What can Do: Raise your arms above your head and take 3 deep breaths in and out. Another option is to take a deep breath, hold for 5 seconds, and then exhale slowly, Another exercise according to the "4/7/8" method: you need to take a breath, (counting to 4), hold your breath (counting to 7) and exhale slowly (counting 8 seconds). This exercise can be done 10-12 times with short pauses. - If an attack of shortness of breath appeared while taking a certain position, then it should be changed. For pregnant women the most A comfortable resting position is to lie on your side. You can buy yourself a special pillow that will allow you to take comfortable position.
- Drink a sedative - women during the period of bearing a child become very vulnerable and vulnerable. As a result hormonal adjustment, pregnant women are regularly nervous. Being under stress often causes rapid breathing. The drug will help you relax slight soothing effect.
 About which remedy is better to choose, be sure to consult with your doctor.
About which remedy is better to choose, be sure to consult with your doctor. - Ventilate the room well - sudden shortness of breath may occur due to lack of oxygen, high concentration carbon dioxide. For the most comfortable ventilation, get yourself a breather.
This is a compact supply air unit with a triple effect:- purification of incoming air from gases, odors, dust and other harmful impurities,
- outdoor air heating to a comfortable temperature,
- recycling.
Preventive actions
The fight against shortness of breath during pregnancy should not only be reduced to the removal of an already existing acute condition. There are also certain preventive measures. They may not completely eliminate shortness of breath, but they will significantly reduce its intensity.
These are the following preventive measures:
- control your weight - during pregnancy, a woman gains weight, but you can monitor it, not exceeding the norm.
 Large numbers on the scales - an additional burden on all organs, including the respiratory system,
Large numbers on the scales - an additional burden on all organs, including the respiratory system, - do not overeat - very often shortness of breath occurs due to the fact that the stomach is full. Remember he's already under a lot of pressure,
- as your belly grows, periodically review your wardrobe - clothes should be light, free and not restricting movement,
- ventilate the room regularly,
- Reduce your time outside during hot weather and stay in the shade if possible. It is better to walk in cloudy or cool weather,
- in the fight against shortness of breath during pregnancy, yoga and swimming have proven themselves. These exercises allow you to learn how to breathe correctly and train the respiratory system well.
Separately, it should be emphasized that if you are allergic, then during pregnancy you should be especially careful to ensure that any contact with the allergen is excluded. If symptoms of seasonal pollinosis are added to shortness of breath, then the condition of the pregnant woman will be even worse.
Buying a Tion 4S breather will be the way out. Thanks to special filters, the air will be cleaned of all types of allergens (plant pollen, fluff, animal hair).
The main thing is not to dwell on temporary ailments (in the form of shortness of breath, weight gain, etc.). Let this wonderful period of life be remembered only by pleasant moments!
Early pregnancy | Shchelkovsky perinatal center
Pregnancy is a wonderful period! However, the changes taking place in the body at this time can greatly frighten you. The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
1. Frequent urination.
Frequent, painless (!) urge to urinate is one of the signs of pregnancy. This is due to increased secretion of progesterone (pregnancy hormone), changes in metabolism and pressure from the growing uterus on the bladder.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg)
Be sure to see a doctor if:
- urination is painful (this may be a sign of an infection)
- urine of strange color (stained with blood, brown)
- the amount of urine excreted per day is much less than the liquid drunk per day
Life hack! In no case should you limit your fluid intake! To alleviate the condition and reduce the frequent urge to urinate, it is necessary to exclude products that have a diuretic effect: tea, coffee, zucchini, watermelon; as well as salty, spicy and fried foods. It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
2. Nausea, vomiting, heartburn, increased susceptibility to odors.
Nausea is one of the common symptoms of early pregnancy. The range of issues related to nausea and vomiting during pregnancy is quite wide. From "it's good, I don't even feel sick" (with relief), "I don't feel sick, what's wrong with me?" (with anxiety) to "when will this nausea pass" (with hope). Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Life hack! For nausea, eat before feeling hungry. Solid, non-hot food and drinks at a cool temperature are best. With heartburn, you should eat small portions of food and often, and most importantly, sit, stand or walk for at least 30 minutes after eating, but do not lie down.
You should definitely consult a doctor if:
- vomiting occurs even after drinking water
- vomiting is exhausting, accompanied by dizziness, weakness
- dryness, jaundice and flaking of the skin appear
- Nausea and vomiting interfere with proper nutrition, accompanied by weight loss
To reduce nausea and vomiting in the morning, try eating something before you get out of bed. It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
3. Pain or cramps in the lower abdomen, constipation, pain in the lumbar region.
The simplest and most easily controlled cause of pain is delayed and incomplete bowel movements. An increase in the concentration of progesterone relaxes the smooth muscles, which are located not only in the uterus, but also in other hollow organs. In this case, the correction of the diet and the restoration of the passage of feces will help. If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
You should definitely consult a doctor if:
- pain is accompanied by spotting bloody discharge from the external genitalia
- increasing duration and intensity of pain
- abdominal pain accompanied by dizziness, fever, loss of consciousness
Life hack! To improve bowel movements, eat more vegetables and fruits, drink water and move more during the day. Try to eat often and in small portions.
Try to eat often and in small portions.
4. Enlargement and soreness of the mammary glands.
Hormonal restructuring of the body during gestation is accompanied, among other things, by an increase in the size of the mammary glands and an increase in their sensitivity. By the end of the first trimester, the soreness usually disappears, no additional methods of treatment are needed.
Life hack! Choose comfortable supportive underwear (it should not leave marks on the skin at the end of the day). You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You should definitely see a doctor if:
- the pain is severe
- mammary glands are very dense with redness and body temperature is increased
- there is discharge from the nipples (purulent, bloody)
5. Increased body temperature.
In early pregnancy, an increase in body temperature to 37.5 ° C is not necessary, but is possible due to the peculiarities of the action of progesterone. Because of this, it is difficult for pregnant women to endure stuffy, hot rooms. Self-medication is dangerous: an attempt to bring down the temperature even with a seemingly harmless folk method - tea with raspberries - can mask the true cause of hyperthermia and delay the diagnosis. Due to the increased body temperature, pregnant women should dress in layers and avoid stuffy and hot rooms and spaces so that they can always “adjust” their temperature on their own.
- temperature above 37.5 °C
- along with fever, any pain occurs
- runny nose, cough, body aches appear
6. Nasal congestion, shortness of breath, nosebleeds.
These symptoms can be explained by the individual reaction of the vascular system to the increase in blood volume that occurs during pregnancy. Another possible reason is dry air in the room, the operation of central heating batteries.
Another possible reason is dry air in the room, the operation of central heating batteries.
Life hack! The easiest way to deal with nasal congestion is to use a humidifier. If you don't have one, you can put a damp towel on the battery - less effective, but better than nothing. It is possible to use sprays with sea salt, but you need to carefully read the instructions and especially the "Indications" section, it should contain information about the safety of the product during pregnancy.
Be sure to see a doctor if:
- symptoms of a cold occur
- nasal congestion accompanied by ear congestion
- These symptoms appeared after exposure to the allergen known to you
7. Blood pressure fluctuations.
The ideal option for any pregnancy is the stability of blood pressure throughout the gestation. However, this is extremely rare. A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels.![]() Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130-139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress.
Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130-139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress.
Life hack! If you are experiencing high normal blood pressure for the first time, repeat the measurement after 15 minutes. If the pressure remains elevated, see a doctor.
Be sure to see a doctor if:
- your blood pressure is above 140/90 mmHg
- pressure increased by more than 10 mm Hg.
 relative to your usual
relative to your usual - an increase in the pressure indicator is accompanied by edema, the appearance of "flies" before the eyes
NB! You should also pay attention to lowering blood pressure. Numbers less than 90/60 mmHg - an excuse to see a doctor.
Life hack! Keep a blood pressure diary, especially if you are prone to hypertension. Show your diary to your doctor at every appointment.
8. Heaviness and pain in the legs.
Heaviness and pain in the legs, especially in the evening, are frequent companions of pregnancy. There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
Life hack! Ask your partner/husband to give you a foot massage, relax with your limbs elevated (not too much!) A therapeutic pedicure, dousing the legs with cool water, a contrast shower, a cream or gel for legs with cooling components (menthol, essential oils), as well as compression stockings or stockings of the lightest degree of compression will help.
Be sure to see a doctor if:
- one or both legs are severely swollen or discolored
- previously diagnosed varicose veins, family history of thrombosis
9. Skin changes.
During pregnancy, you may notice dark spots on your skin. Especially often such darkening (hyperpigmentation) is observed in the nipple area, along the white line of the abdomen. Stretch marks (stretch marks) may appear on the skin of the abdomen and thighs. These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
Life hack! Oils and moisturizing creams to increase skin elasticity, contrast showers, massage with a hard brush will help reduce the likelihood of skin changes.
You should definitely consult a doctor if:
- along with itching there are areas of redness, spots, peeling
- itching increases
10. Bleeding gums.
Changes in the characteristics of blood circulation in the body of a pregnant woman can cause bleeding gums. The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
You should definitely consult a doctor if:
- you have loose teeth, sore gums, bad breath
- bleeding in the gum area increases
11.