Stds that affect pregnancy
Sexually transmitted infections, pregnancy, and breastfeeding
Sexually transmitted infections (STIs) are also called sexually transmitted diseases, or STDs. STIs include chlamydia, gonorrhea, trichomoniasis, genital herpes, genital warts, HIV, and syphilis. Some STIs can pass from mother to baby during pregnancy and through breastfeeding.
How do STIs affect pregnant women?
STIs can cause many of the same health problems in pregnant women as in women who are not pregnant. But having an STI also can hurt the unborn baby's health.
Having an STI during pregnancy can cause:
- Premature labor (labor before 37 weeks of pregnancy). Early (preterm) birth is the number one cause of infant death and can lead to long-term developmental and health problems in children.1
- Infection in the uterus (womb) after birth
Can I pass an STI to my baby?
Yes. Some STIs can be passed from a pregnant woman to the baby before and during the baby's birth.
- Some STIs, such as syphilis, cross the placenta and infect the baby in the womb.
- Other STIs, like gonorrhea, chlamydia, hepatitis B, and genital herpes, can pass from the mother to the baby as the baby passes through the birth canal.
- HIV can cross the placenta during pregnancy and infect the baby during delivery.
What are the harmful effects of passing an STI to a baby?
The harmful effects to babies may include:
- Low birth weight (less than 5 pounds)
- Eye infection
- Pneumonia
- Infection in the baby's blood
- Brain damage
- Lack of coordination in body movements
- Blindness
- Deafness
- Acute hepatitis
- Meningitis
- Chronic liver disease, which can lead to scarring of the liver (cirrhosis)
- Stillbirth
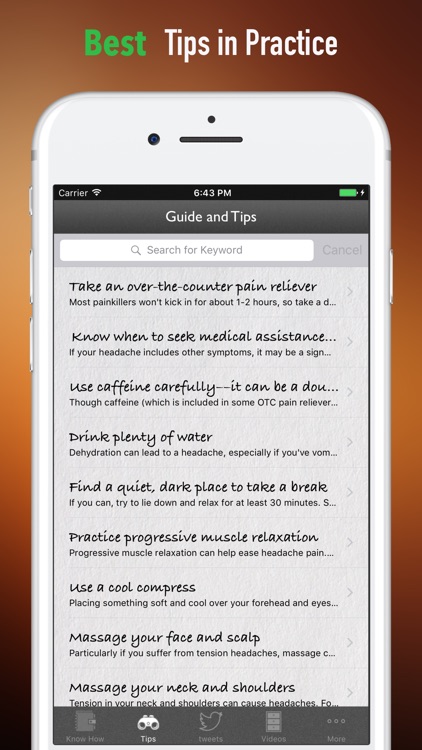
I'm pregnant. What can I do to prevent problems from STIs?
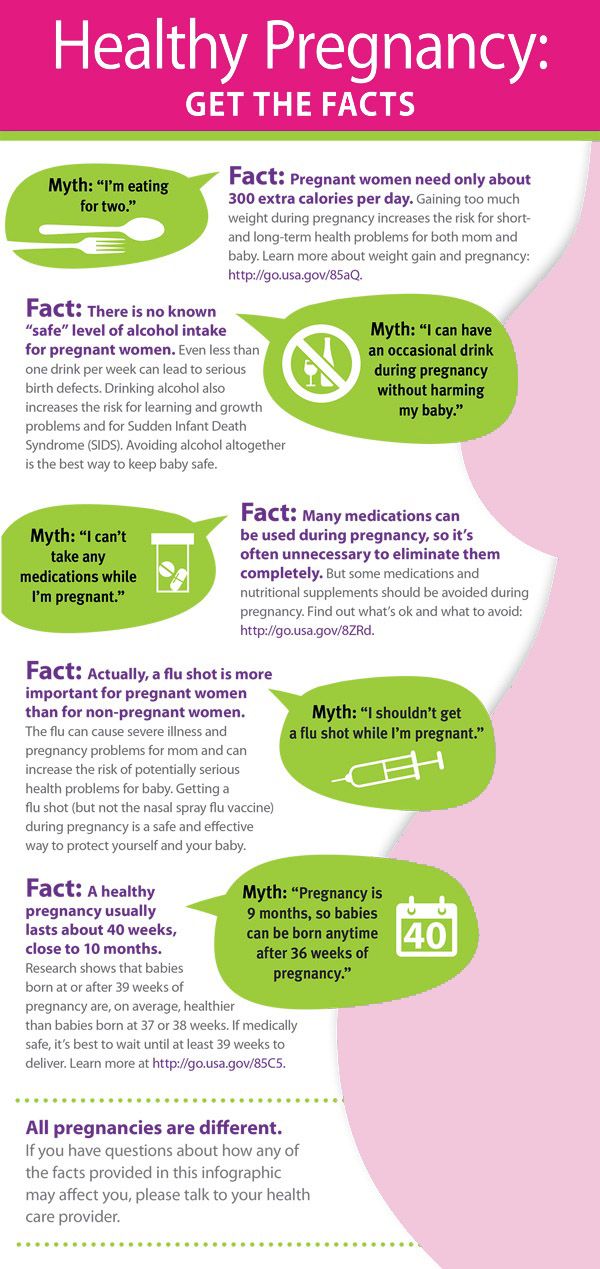
You can prevent some of the health problems caused by STIs and pregnancy with regular prenatal care.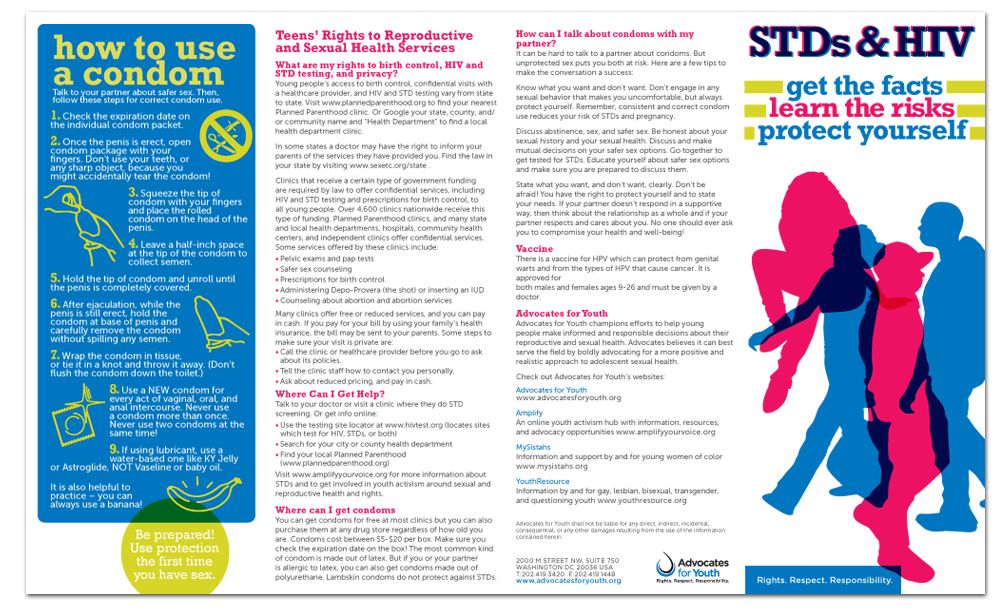 Your doctor will test you for STIs early in your pregnancy and again closer to childbirth, if needed.
Your doctor will test you for STIs early in your pregnancy and again closer to childbirth, if needed.
- STIs caused by bacteria, such as chlamydia and gonorrhea, can be cured with antibiotics. Some antibiotics are safe to take during pregnancy. Your doctor can prescribe antibiotics for chlamydia, gonorrhea, syphilis, and trichomoniasis during pregnancy.
- STIs caused by viruses, such as genital herpes and HIV, have no cure.
- If you have herpes, antiviral medicine may help reduce symptoms. If you have symptoms of herpes or active genital herpes sores at the start of labor, you may need a cesarean section (C-section). This can help lower the risk of passing the infection to your baby.
- If you have HIV, antiviral medicines can lower the risk of giving HIV to your baby to less than 1%.2 You also may need to have a C-section.
You also can take steps to lower your risk of getting an STI during pregnancy.
Can I breastfeed if I have an STI?
Maybe. Some STIs affect breastfeeding, and some don't. The following are some general guidelines, but talk to your doctor, nurse, or a lactation consultant about the risk of passing the STI to your baby while breastfeeding:
- If you have HIV, do not breastfeed. You can pass the virus to your baby. In countries like the United States where clean water is available, using a breastmilk substitute like formula is recommended.
- If you have chlamydia, gonorrhea, or HPV, you can breastfeed your baby.
- If you have trichomoniasis, you can take the antibiotic metronidazole if you are breastfeeding. You may need to wait 12 to 24 hours after taking the medicine to breastfeed.
- If you have syphilis or herpes, you can breastfeed as long as your baby or pumping equipment does not touch a sore. It is possible to spread syphilis or herpes to any part of your breast, including your nipple and areola.
 If you have sores on your breast, pump or hand-express your milk until the sores heal. Pumping will help keep up your milk supply and prevent your breast from getting overly full and painful. You can store your milk to give to your baby in a bottle for another feeding. But if parts of your breast pump also touch the sore(s) while pumping, you should throw the milk away.
If you have sores on your breast, pump or hand-express your milk until the sores heal. Pumping will help keep up your milk supply and prevent your breast from getting overly full and painful. You can store your milk to give to your baby in a bottle for another feeding. But if parts of your breast pump also touch the sore(s) while pumping, you should throw the milk away.
Are STI treatments safe to use while breastfeeding?
If you are being treated for an STI, ask your doctor about the possible effects of the medicine on your breastfeeding baby. Most treatments for STIs are safe to take while breastfeeding.
Did we answer your question about STIs, pregnancy, and breastfeeding?
For more information about STIs, pregnancy, and breastfeeding, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- Food and Drug Administration (FDA), HHS
Phone Number: 888-463-6332 - National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), CDC, HHS
Phone Number: 800-232-4636 - National Institute of Allergy and Infectious Diseases (NIAID), NIH, HHS
Phone Number: 866-284-4107 (TDD: 800-877-8339) - American Sexual Health Association
Phone Number: 800-227-8922
Sources
- Centers for Disease Control and Prevention.
 (2015). Preterm Birth.
(2015). Preterm Birth. - Centers for Disease Control and Prevention. (2015). HIV Among Pregnant Women, Infants, and Children.
The Office on Women's Health is grateful for the medical review by:
- Jill E. Long, M.D., M.P.H., FACOG, Commander, U.S. Public Health Service Commissioned Corps, Medical Officer, Sexually Transmitted Diseases Branch, Division of Microbiology and Infectious Diseases, National Institute of Allergy and Infectious Diseases
- Centers for Disease Control and Prevention (CDC) staff
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
STD Facts - STDs & Pregnancy
If you are pregnant, you can become infected with the same sexually transmitted diseases (STDs) as women who are not pregnant.
 Pregnant women should ask their doctors about getting tested for STDs, since some doctors do not routinely perform these tests. This fact sheet answers basic questions about STDs during pregnancy.
Pregnant women should ask their doctors about getting tested for STDs, since some doctors do not routinely perform these tests. This fact sheet answers basic questions about STDs during pregnancy.I’m pregnant. Can I get an STD?
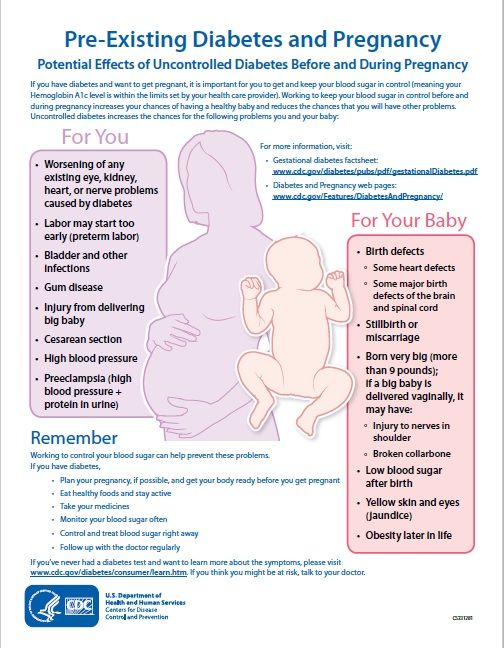
Yes, you can. Women who are pregnant can become infected with the same STDs as women who are not pregnant. Pregnancy does not provide women or their babies any additional protection against STDs. Many STDs are ‘silent,’ or have no symptoms, so you may not know if you are infected. If you are pregnant, you should be tested for STDs, including HIV (the virus that causes AIDS), as a part of your medical care during pregnancy. The results of an STD can be more serious, even life-threatening, for you and your baby if you become infected while pregnant. It is important that you are aware of the harmful effects of STDs and how to protect yourself and your unborn baby against infection. If you are diagnosed with an STD while pregnant, your sex partner(s) should also be tested and treated.
How can STDs affect me and my unborn baby?
STDs can complicate your pregnancy and may have serious effects on both you and your developing baby. Some of these problems may be seen at birth; others may not be discovered until months or years later. In addition, it is well known that infection with an STD can make it easier for a person to get infected with HIV. Most of these problems can be prevented if you receive regular medical care during pregnancy. This includes tests for STDs starting early in pregnancy and repeated close to delivery, as needed.
Should I be tested for STDs during my pregnancy?
Yes. Testing and treating pregnant women for STDs is a vital way to prevent serious health complications to both mother and baby that may otherwise happen with infection. The sooner you begin receiving medical care during pregnancy, the better the health outcomes will be for you and your unborn baby. The Centers for Disease Control and Prevention’s 2015 STD Treatment Guidelines recommend screening pregnant women for STDs. The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
Be sure to ask your doctor about getting tested for STDs. It is also important that you have an open, honest conversation with your provider and discuss any symptoms you are experiencing and any high-risk sexual behavior that you engage in, since some doctors do not routinely perform these tests. Even if you have been tested in the past, you should be tested again when you become pregnant.
Can I get treated for an STD while I’m pregnant?
It depends. STDs, such as chlamydia, gonorrhea, syphilis, trichomoniasis and BV can all be treated and cured with antibiotics that are safe to take during pregnancy. STDs that are caused by viruses, like genital herpes, hepatitis B, or HIV cannot be cured. However, in some cases these infections can be treated with antiviral medications or other preventive measures to reduce the risk of passing the infection to your baby. If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
How can I reduce my risk of getting an STD while pregnant?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting chlamydia:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
You can add this content to your website by syndicating.
STDs during Pregnancy - CDC Detailed Fact Sheet
Detailed fact sheets are intended for physicians and individuals with specific questions about sexually transmitted diseases. Detailed fact sheets include specific testing and treatment recommendations as well as citations so the reader can research the topic more in depth.
STIs and pregnancy - KVD №2
- home
- Articles
- STIs and pregnancy
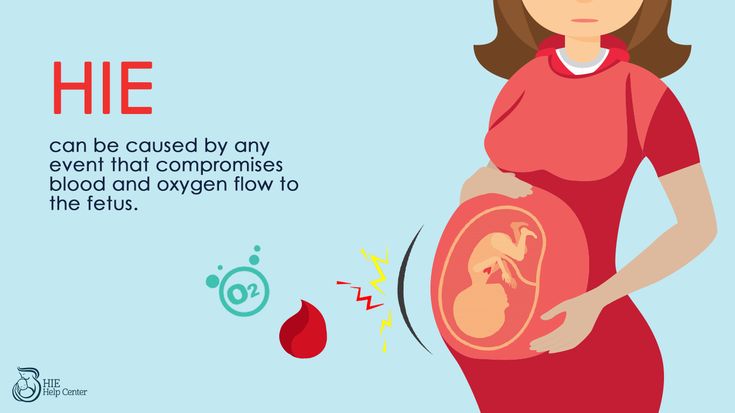
The presence of an STI in a pregnant woman can cause serious harm to the fetus. Untreated infections can lead to miscarriage, premature birth, stillbirth, underweight babies, blindness, hearing loss, chronic respiratory disease, mental retardation, and other serious developmental problems. Untreated syphilis can lead to the birth of a child with congenital syphilis. Activation of STIs during pregnancy is manifested by symptoms of intrauterine infection, leading to miscarriage and intrauterine lesions of the fetus up to its death. Infection of the placenta, according to histological studies, in half of the cases is associated with chlamydia, ureaplasmas, mycoplasmas and HSV (herpes simplex virus), CMV (cytomegalovirus). In newborns, STIs cause conjunctivitis, pneumonia, cerebrovascular accidents, intracranial hemorrhages (one of the causes of cerebral palsy), and sepsis.
Untreated infections can lead to miscarriage, premature birth, stillbirth, underweight babies, blindness, hearing loss, chronic respiratory disease, mental retardation, and other serious developmental problems. Untreated syphilis can lead to the birth of a child with congenital syphilis. Activation of STIs during pregnancy is manifested by symptoms of intrauterine infection, leading to miscarriage and intrauterine lesions of the fetus up to its death. Infection of the placenta, according to histological studies, in half of the cases is associated with chlamydia, ureaplasmas, mycoplasmas and HSV (herpes simplex virus), CMV (cytomegalovirus). In newborns, STIs cause conjunctivitis, pneumonia, cerebrovascular accidents, intracranial hemorrhages (one of the causes of cerebral palsy), and sepsis.
Untreated gonococcal infection often results in ectopic pregnancy or pelvic inflammatory disease. Chronic gonorrhea may worsen immediately after childbirth. At the same time, the risk of gonococcal sepsis is high. Women who become infected in the last 20 weeks of pregnancy or after childbirth are at high risk of gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth.
Women who become infected in the last 20 weeks of pregnancy or after childbirth are at high risk of gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth.
Infection of the fetus with gonorrhea occurs in utero or during childbirth. Intrauterine infection is manifested by gonococcal sepsis in the newborn and chorioamnionitis. Infection during childbirth can lead to gonococcal conjunctivitis, otitis externa, and vulvovaginitis. The most common complication in children born to gonorrhea mothers is a highly contagious eye disease (newborn ophthalmia) which, if left untreated, can lead to blindness. Rare complications in children born to gonorrhea mothers are childhood meningitis and arthritis.
Most doctors test women for gonorrhea at their first pregnancy visit, and many do another test in the third trimester. If your doctor has not given you the results of the tests, ask him what disease you were tested for.
Trichomoniasis, according to most doctors, does not belong to those diseases that can have a fatal effect on the fetus, but, of course, trichomoniasis during pregnancy is an extremely undesirable condition.
Trichomoniasis in a pregnant woman increases the risk of preterm labor and premature rupture of amniotic fluid.
Chlamydial infection in 80% of pregnant women is latent. The frequency of occurrence of urogenital chlamydia among pregnant women, according to various sources, is 6.0 - 8.0%. The most common consequences of untreated genital chlamydia during pregnancy are:
- missed pregnancy,
- spontaneous miscarriages,
- premature or delayed birth,
- untimely outpouring of waters,
- blood loss more than 300 ml,
- puerperal fever,
- endometritis,
- intrauterine infection of the fetus.
Transmission of the pathogen to the child is possible both in the presence and in the absence of obvious clinical manifestations of infection in the mother (the probability of its transmission is 50-70%).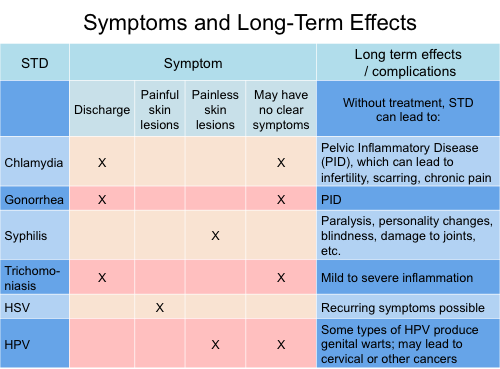 The fetus is infected both by direct contact with the mother's birth canal, and in utero: by ingestion or aspiration of amniotic fluid.
The fetus is infected both by direct contact with the mother's birth canal, and in utero: by ingestion or aspiration of amniotic fluid.
Conjunctivitis (inflammation of the mucous membrane of the eyes) is the most common manifestation of congenital chlamydial infection in infants, pneumonia develops in 10% of infected newborns, and otitis media is somewhat less common. In some children born to infected mothers, these microbes are isolated from the oropharynx, nasopharynx, and rectum. The total percentage of newborns infected with chlamydia reaches 9.8%.
Finally, what do you need to know about the impact of STIs on pregnancy, childbearing and breastfeeding?
A pregnant woman can pass on most STIs during pregnancy or childbirth to her children, and some diseases can be passed through breast milk (eg HIV). However, the chance of transmission can be drastically reduced if treatment is started on time.
Once you decide to become pregnant, visit your doctor and make sure that neither you nor your partner have an STI. If you are infected, take a course of treatment and get tested again before pregnancy.
If you are infected, take a course of treatment and get tested again before pregnancy.
If you are already pregnant, you will need a complete examination. At any time during your pregnancy, be sure to tell your doctor if you notice any symptoms of an STI or suspect you may have contracted it.
Sexually transmitted infections Medical On Group Khabarovsk
Sexually transmitted infections (STIs) are a group of diseases that are transmitted primarily through sexual contact. STIs are extremely common throughout the world. WHO experts (World Health Organization) have calculated that every sixth inhabitant of the globe suffers from any of the sexually transmitted diseases.
All STIs are caused by pathogens (bacteria, viruses, protozoa, parasites) and are transmitted primarily through sexual contact and through blood (mainly through syringes or instruments). But some infections, such as syphilis, herpetic, cytomegalovirus and papillomavirus infections, can be transmitted through skin-to-skin contact and through kissing.
Viral STIs, such as HIV infection, hepatitis, genital herpes and anogenital warts caused by the human papillomavirus, are not completely cured, and only in some cases the course of the disease and its manifestations can be controlled using various means and methods. Curable today are STDs caused by bacteria, protozoa and parasites: syphilis, gonorrhea, chlamydia, trichomoniasis and some others. However, in any case, an early visit to the doctor and the start of treatment will not only serve as a speedy recovery, but will also reduce the risk of developing numerous complications.
For men!
STI can be contracted by absolutely any of the men who have unprotected and promiscuous sex. It is very easy to get sick, but to be treated is much more difficult. Men, remember that the causes of infection with any of the sexually transmitted infections are neglect of your health!
The insidiousness of sexually transmitted infections lies in the fact that for infected men, the disease can occur without pronounced symptoms or completely unnoticed for a certain time. The lack of male attention to the appearance of some signs and symptoms of an incipient disease, as well as untimely or incorrect treatment, contribute to the fact that the disease becomes latent or chronic. The disease in men with a latent character is dangerous because the disease quickly acquires a chronic form, which is much more difficult to treat, and sometimes even impossible. The chronic nature of the disease caused by STIs can cause inflammation of the genitourinary system in men, leading to weakened erection, premature ejaculation, prostatitis, adenoma, impotence, infertility and other serious diseases of the male reproductive system. If in the male body the disease has acquired a chronic form, then it is no longer necessary to show symptoms, because the symptoms are an indicator of the body's active struggle with the infection.
The lack of male attention to the appearance of some signs and symptoms of an incipient disease, as well as untimely or incorrect treatment, contribute to the fact that the disease becomes latent or chronic. The disease in men with a latent character is dangerous because the disease quickly acquires a chronic form, which is much more difficult to treat, and sometimes even impossible. The chronic nature of the disease caused by STIs can cause inflammation of the genitourinary system in men, leading to weakened erection, premature ejaculation, prostatitis, adenoma, impotence, infertility and other serious diseases of the male reproductive system. If in the male body the disease has acquired a chronic form, then it is no longer necessary to show symptoms, because the symptoms are an indicator of the body's active struggle with the infection.
What symptoms should alert you?
-
Unusual white or yellow discharge from the penis, often with a foul odor.
-
Severe itching, burning, painful urination, frequent urge to urinate.
-
Pink or red rash, redness, spots on different parts of the body, for example, on the legs (soles), on the hands (palms).
-
Sharp or pulling pain in the lower abdomen and testicles.
-
Enlarged lymph nodes, especially in the groin.
-
Small vesicles, erosions, warts, ulcers around the mouth, lips and anus.
-
Abnormal tissue growth in the anus and directly on the penis.
Men with an STI may experience other, less common symptoms, such as pain during intimacy, impaired ejaculation, or fever.
The most common STIs in men are: chlamydia, trichomoniasis, mycoplasmosis, ureaplasmosis, gardnerellosis, gonorrhea, and syphilis.
For women!
The most frequent symptoms of STIs in women. What should alert?
-
Bad smell from the vagina.
-
An increase in the amount of secretions from the genital tract, a change in their color and structure.

-
The appearance of pain during urination.
-
Violent itching in the genital area.
-
Discomfort during sex.
-
Slight malaise, headache, lethargy, drowsiness.
-
Delayed menstruation or bleeding in the middle of the cycle.
Manifestations may vary depending on the disease:
-
With genital herpes, vesicles appear on the outer surface of the genital organs, which are very itchy, after a few days they burst and turn into sores. It is easy to get infected with such herpes, but it is difficult to cure this disease, you can only reduce the number of relapses.
-
Syphilis is a very insidious disease, the first symptoms appear after a few weeks. A small ulcer appears on the genitals. After about 2 weeks, it increases in size, there is a thickening of the lymph nodes. The symptoms of syphilis are the same in men and women.
 A primary ulcer (syphilitic chancre) may also occur outside of the genital area. Depending on the method of infection, chancres can appear anywhere on the skin or mucosa. Infection with syphilis can also occur non-sexually (for example, through a blood transfusion), in such cases there is no primary chancre and it may take longer to detect the disease.
A primary ulcer (syphilitic chancre) may also occur outside of the genital area. Depending on the method of infection, chancres can appear anywhere on the skin or mucosa. Infection with syphilis can also occur non-sexually (for example, through a blood transfusion), in such cases there is no primary chancre and it may take longer to detect the disease. -
With trichomoniasis, there is a change in the color of vaginal discharge. They become yellow or greenish, with an unpleasant odor.
-
Chlamydia is a disease that can be transmitted not only through sexual contact, but also through household contact. The first signs appear after a week. Characterized by frequent and painful urination, uterine bleeding, pain in the lower abdomen and back.
-
Gonorrhea (gonorrhea) can go on for a long time without any symptoms. In most cases, patients complain of yellow or green purulent discharge with an unpleasant odor, sharp pains in the lower abdomen.