Spotting in 15 week of pregnancy
The Second Trimester of Pregnancy: Pain, Bleeding, and Discharge
Pain, bleeding, and discharge
Some pain or discomfort is normal during the second trimester of pregnancy. Spotting and very small amounts of blood may also be harmless. However, there are certain types of pain, bleeding, and vaginal discharge that you shouldn’t ignore.
Learn how to tell the difference between normal pregnancy problems and serious medical concerns.
Emergency medical symptoms during the second trimester
There are a number of situations during pregnancy that demand medical attention. If you experience the symptoms below, don’t hesitate to call your doctor or seek emergency care.
When to seek emergency medical attention
Always seek emergency care if you are experiencing the symptoms of a miscarriage. Symptoms of a miscarriage include:
- enough vaginal bleeding to soak more than one menstrual pad
- severe pain in the abdomen or pelvic region
- clots or clumps of tissue (typically gray or pink in color) passed from the vagina
If you pass clots or clumps from the vagina, try to save the tissue in a jar or plastic bag to give to the doctor for analysis. They may then determine the cause of the problem.
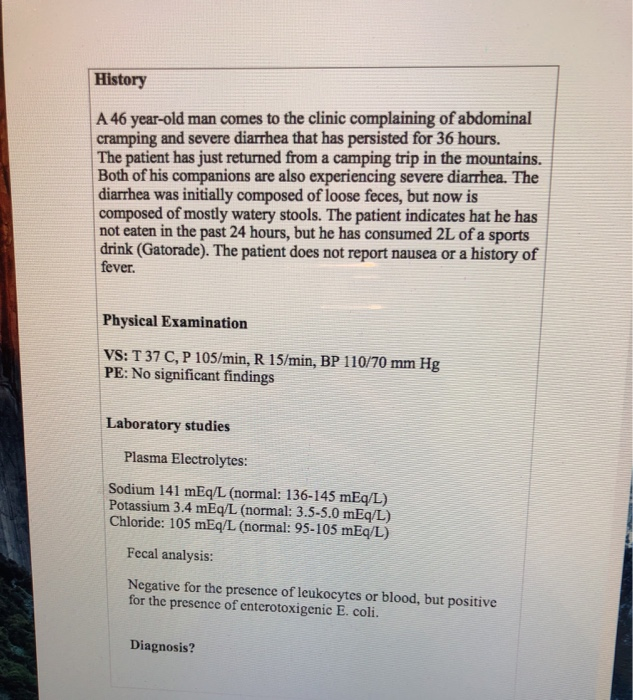
There are three types of miscarriage.
If a miscarriage has been threatened, there was bleeding before 20 weeks of pregnancy with no cervical dilation and no expulsion of any of the fetal parts.
If a miscarriage has been completed, there was complete expulsion of fetal parts from your body.
If a miscarriage has happened incompletely, there was partial expulsion of the fetal parts before 20 weeks. In the case of incomplete miscarriages, the next step may be to allow the remaining products of pregnancy to pass naturally or perform a dilation and curettage.
Note: If you have miscarried before and notice bleeding or cramping, you should seek emergency medical attention.
Always seek emergency care if you are experiencing the symptoms of an ectopic pregnancy (a pregnancy outside the uterus). Symptoms of an ectopic pregnancy include:
- cramps and colicky (spasmodic) pain with associated tenderness
- pain that starts on one side and spreads across the belly
- pain that worsens with taking a bowel movement or coughing
- light bleeding or spotting that is brown in color, is either constant or intermittent, and precedes the pain by weeks
- one of the above symptoms combined with nausea and vomiting, pain in the shoulder, weakness or lightheadedness, or rectal pressure
- rapid and weak pulse, clamminess, fainting, and sharp pain (these symptoms may arise if the ectopic pregnancy is in the fallopian tube and the tube ruptures, causing septic shock)
When to call your doctor
Emergency care isn’t always necessary.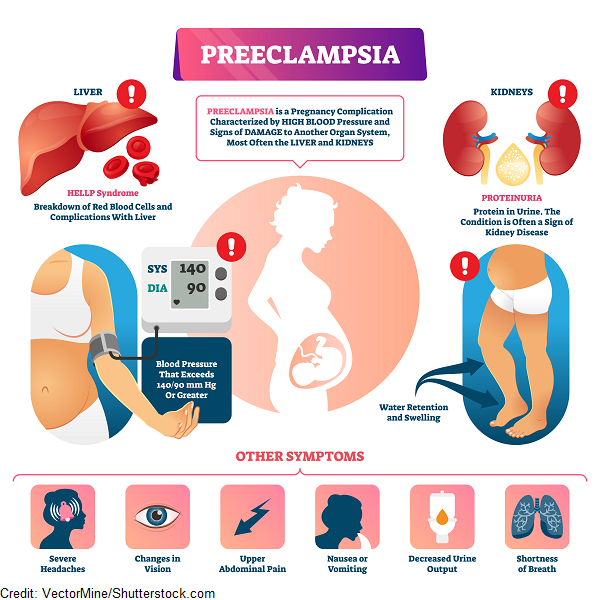 However, some signs require a doctor’s evaluation. Always call your doctor for advice if you’re experiencing signs of miscarriage. Early signs of miscarriage include:
However, some signs require a doctor’s evaluation. Always call your doctor for advice if you’re experiencing signs of miscarriage. Early signs of miscarriage include:
- cramps and pain in the center of the abdomen with vaginal bleeding
- severe pain or pain that lasts for more than a day (even without bleeding)
- bleeding that is as heavy as a period
- spotting or staining that lasts for three days or longer
Pain
Although you may not experience an emergency, there will probably be times during your pregnancy when you’re uncomfortable or in pain. Many women have pain during the second trimester even when nothing is medically wrong.
Abdominal pain, back pain, headaches, leg cramps, and hand pain don’t always signal a problem. Learning to identify and relieve these normal discomforts will help you throughout your pregnancy.
Abdominal pain
Abdominal pain can either be a normal symptom of pregnancy or a sign of something serious, like preterm labor or ectopic pregnancy. It’s important to tell your doctor when you feel any type of abdominal pain, because of the potential for a serious complication.
It’s important to tell your doctor when you feel any type of abdominal pain, because of the potential for a serious complication.
When you feel pain in your abdomen during the second trimester, it’s usually related to the tension on the ligaments and muscles in the pelvis. These get stretched as the uterus expands to hold the growing baby.
If you move quickly, you can “pull” a ligament or muscle. This may feel like a painful pang in your pelvis or a cramp down your side that can last for several minutes. This kind of pain isn’t harmful to you or your baby.
Sometimes abdominal pain is related to past pregnancies or surgeries. If you’ve had surgery for infertility or other types of abdominal surgery, you may experience pain from the pulling of the remnants of scar tissue (adhesions).
Pregnant women can also have the same types of abdominal infections that other women develop. Infections that can cause abdominal pain include:
- cholecystitis (inflamed gallbladder)
- appendicitis (inflamed appendix)
- hepatitis (inflamed liver)
- pyelonephritis (kidney infection)
- pneumonia (lung infection)
Sometimes these diseases are harder to diagnose during pregnancy because the location of pain characteristic to each has been shifted.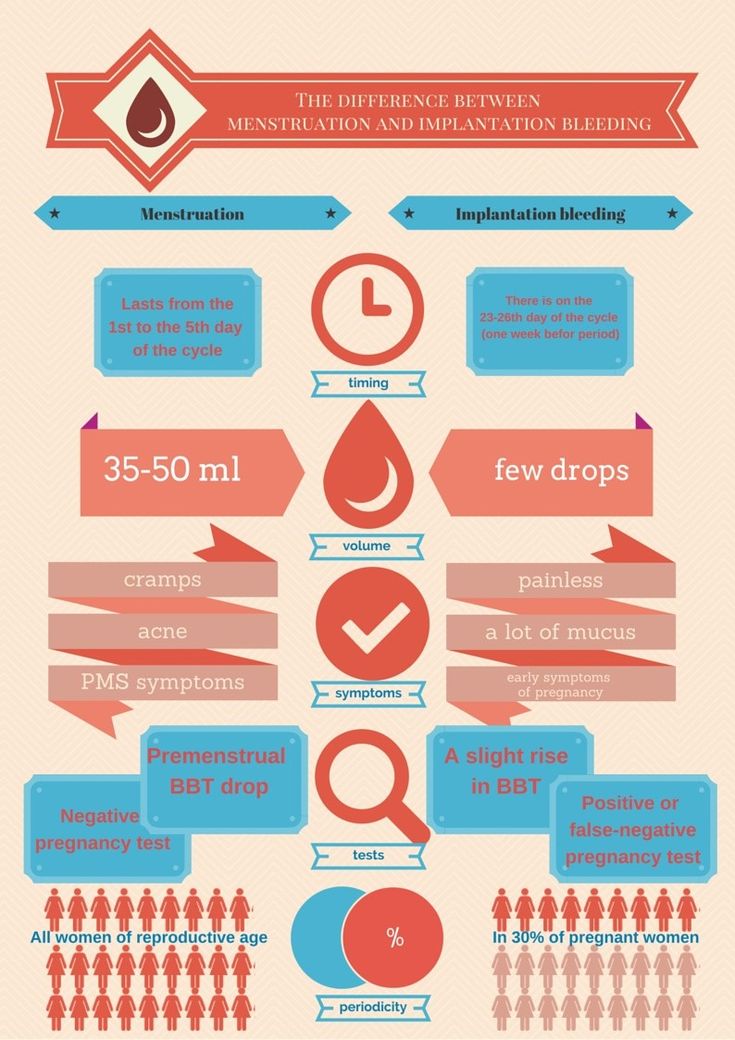 This happens when the growing uterus pushes nearby organs out of its way.
This happens when the growing uterus pushes nearby organs out of its way.
If you’re experiencing serious pain that doesn’t feel like it’s in your uterus, show or tell your doctor exactly where the pain is located. If you have one of the above infections, you may need antibiotics or surgery to fix the problem.
Warning: If you’re experiencing regular or painful contractions in the pelvis or abdomen, call a doctor immediately. These may be a sign of preterm labor.
Back pain
Back pain is very common during pregnancy. Pregnancy hormones cause the joints in the pelvis to become soft and lax in preparation for childbirth. As your uterus gets bigger in the second trimester, your center of gravity changes.
You begin to carry yourself differently to accommodate the weight. In addition, your abdominal muscles may separate as the uterus presses up against them, weakening the abdominal wall. All of these factors can contribute to back pain, strain, and discomfort.
Here’s how you can improve back pain:
- Practice good posture while standing (shoulders back, pelvis in) and sitting (elevate feet slightly and try to avoid crossing your legs).
- Get up every once in a while when you’re sitting for long periods.
- Lift heavy objects by bending at the knees, rather than the waist.
- Try not to reach for things over your head.
- Sleep on your left side, bending at your hips and knees, and place a pillow between your legs to reduce pressure on your back.
- Strengthen your stomach muscles. One of the keys to a strong back is a strong abdomen.
- Talk to your doctor. You may need to use a back brace or some other form of support to relieve the pressure on your back.
Warning: If you’re experiencing lower back pain accompanied by painful urination, you may have a bladder or kidney infection. Low, dull, consistent back pain may be a sign of preterm labor. Severe back pain coupled with vaginal bleeding or discharge may also indicate a serious problem. Call your doctor immediately if you experience any of these symptoms.
Severe back pain coupled with vaginal bleeding or discharge may also indicate a serious problem. Call your doctor immediately if you experience any of these symptoms.
Headaches
Many women experience frequent headaches during pregnancy. You still may be experiencing headaches that started during the first trimester, or they may be just beginning now.
Hormonal changes, tension, fatigue, hunger, and stress are all culprits. Try to relax, stay rested, and eat regularly. You can also try to relieve headaches in the following ways:
- If you have a sinus headache, apply warm compresses to aches in the sinus areas of your head. These include both sides of the nose, the middle of the forehead, and the temples.
- If the headache is due to tension, try applying cold compresses to aches along the back of your neck.
- Learn relaxation exercises, like closing your eyes and imagining yourself in a peaceful place. Reducing stress is a key component of a healthy pregnancy.
 Consider calling a counselor or a therapist if needed.
Consider calling a counselor or a therapist if needed.
Speak with a physician before you begin using pain relievers. This is important even if you took over-the-counter medications for pain before you were pregnant.
Common headache medicines include ibuprofen (Motrin), aspirin (Bufferin), acetaminophen (Tylenol), and naproxen sodium (Aleve).
Acetaminophen is probably the safest option during pregnancy, but don’t take pills during pregnancy unless your doctor has specifically told you to do so.
Warning: Call your doctor if the headache is particularly severe or lasts for more than a few hours. Also note whether your headache comes with a fever, swelling in the face and hands, dizziness, nausea, or changes in vision. These may be signs of preeclampsia or another serious complication.
Leg cramps
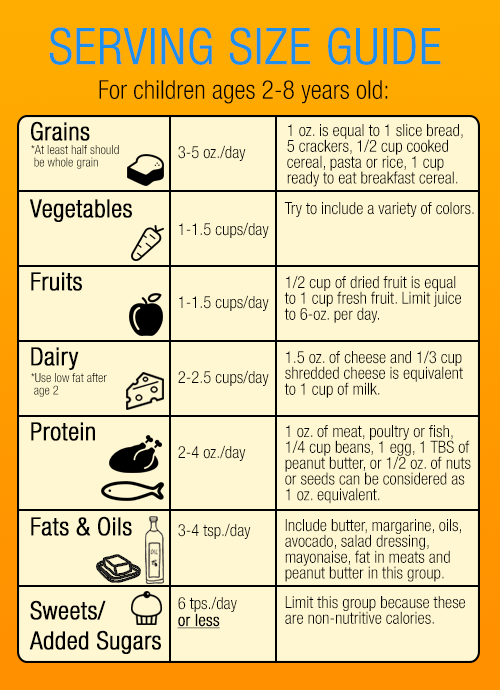
Although no one knows exactly what causes them, leg cramps are common in the second and third trimester. Possible causes may be that you don’t consume enough calcium, have too much phosphorous in your diet, or are tired.
Possible causes may be that you don’t consume enough calcium, have too much phosphorous in your diet, or are tired.
It may be that the uterus is pressing on the nerves that go to the legs. Regardless of the cause, you may wake up in the middle of the night with bothersome cramps.
You can avoid or get rid of cramps by:
- exercising your calves
- staying hydrated
- alternating between sitting and standing
- wearing support hose
- wearing comfortable, supportive shoes
- flexing the ankle and toes upward with a straightened knee to stop the cramping
- massaging or applying a warm compress to the leg that is cramping
- talking to your doctor about reducing the amount of phosphorous in your diet by cutting down on foods like milk or meat
- making sure you get enough calcium (by eating fortified cereal or spinach) and magnesium (by eating beans or semisweet chocolate)
Warning: Tell your doctor if the cramps feel particularly painful, fail to go away, cause swelling, feel warm to the touch, or change the skin color of your leg (to white, red, or blue).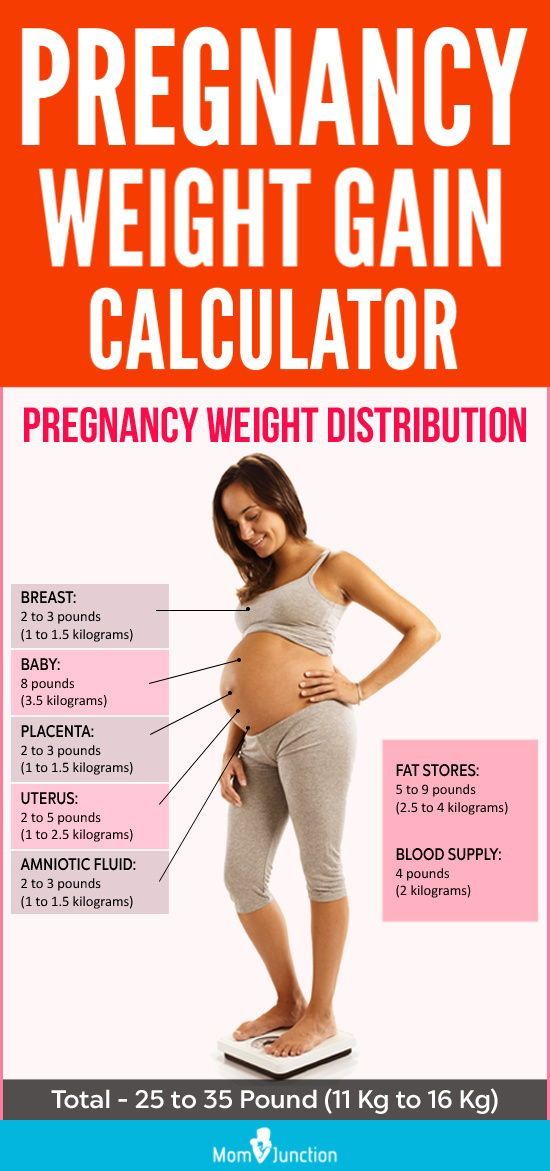 You may have a blood clot in a leg vein that needs to be treated. This is known as deep vein thrombosis, and without treatment it can be deadly. Consult a doctor immediately.
You may have a blood clot in a leg vein that needs to be treated. This is known as deep vein thrombosis, and without treatment it can be deadly. Consult a doctor immediately.
Pain and numbness in the hand
Numbness and pain in the thumb, index finger, middle finger, and half of the ring finger can be a sign of carpal tunnel syndrome.
Usually this condition is diagnosed in people who regularly perform repetitive tasks such as typing or piano playing, but it’s also common in pregnant women.
During pregnancy, the tunnel that surrounds the nerve to these fingers can become swollen, causing tingling, numbness, and pain. In the evening, after your arm has been dangling by your side all day, your symptoms may worsen due to gravity.
Shaking out your arm when you experience the carpal tunnel symptoms may help. Alternatively, you may want to talk to your doctor about splinting your wrist or taking vitamin B-6.
Numbness and tingling in the hand can also be caused by poor posture. If your shoulders droop and your head is thrust forward, you put pressure on the nerves under your arms, causing tingling.
If your shoulders droop and your head is thrust forward, you put pressure on the nerves under your arms, causing tingling.
Practice standing up straight with your head and spine erect. A supportive bra and proper bed rest are also important.
Bleeding
Bleeding can be a scary symptom during pregnancy. In some cases, bleeding can be harmless. It can happen when pregnancy hormones cause you to develop more sensitive, expanded blood vessels.
In other cases, bleeding can indicate a serious problem with the pregnancy. If you experience any bleeding, call a doctor for advice.
Vaginal bleeding
Light bleeding or spotting (which can be brown, pink, or red) during the second and third trimester isn’t usually cause for concern. It typically occurs as a result of interference with the cervix during sex or a vaginal exam.
Pink mucus or brownish discharge may both occur during the second trimester. It’s caused by small amounts of blood leaving your body with normal discharge.
Vaginal bleeding that’s like a period, however, can be a worrisome sign that needs immediate medical attention. Clots of blood or clumps of tissue in the blood may be symptoms of a miscarriage.
For this reason, you should never be the judge of what is normal or abnormal bleeding. Instead, call your doctor.
If the bleeding is heavy or if it’s accompanied by pain, call your doctor immediately. If it’s spotty, you can make the call sometime that day. Serious bleeding is most commonly caused by placenta previa, premature labor, or late miscarriage.
Rectal bleeding and hemorrhoids
Rectal bleeding isn’t as worrisome as vaginal bleeding and is generally a sign of either hemorrhoids or anal fissure. Rectal bleeding could also be a sign of something more serious. You should speak with your doctor if you’re experiencing this symptom.
Rectal bleeding may mean you have hemorrhoids, either external or, less commonly, internal. Hemorrhoids occur in up to half of all pregnant women. They are varicose veins of the rectum and can cause pain, itching, and bleeding, often made worse by constipation.
They are varicose veins of the rectum and can cause pain, itching, and bleeding, often made worse by constipation.
Hemorrhoids are caused by progesterone acting on the walls of the rectal veins, causing them to relax and expand. As you advance in your pregnancy and the uterus presses on these veins, blood flow slows down and the veins dilate even more.
Squeezing and constipation can make hemorrhoids worse. Laughing, coughing, straining, and going to the bathroom may cause hemorrhoids to bleed.
If rectal bleeding isn’t caused by hemorrhoids, it may be caused by an anal fissure — a crack in the skin that lines the anal canal. Anal fissures are usually caused by constipation. Fissures are very painful, particularly during the strain of taking a bowel movement.
Hemorrhoids and anal fissures can cause brown, pink, or red bloodstains to appear on your underwear or toilet paper. If the bleeding is heavy or continuous, call a doctor for advice.
If you’re diagnosed with hemorrhoids or an anal fissure, you should do the following:
- Try to avoid constipation by remaining well hydrated and eating a diet high in fiber.
- Try to alleviate pressure on the veins in the rectum by sleeping on your side, not standing or sitting for long periods of time, and not taking too long or straining when going to the bathroom.
- Take warm sitz baths up to two times a day. Sitz baths are basins that fit on your toilet and are filled with warm water in which you can soak your anus.
- Soothe the hemorrhoids with ice packs or witch hazel, and only use topical medications if your doctor prescribes them. Your doctor may also prescribe stool softeners or a laxative.
- Practice good hygiene by wiping thoroughly after bowel movements (from front to back) and keeping yourself clean.
- Use only white, unscented toilet paper.
- Perform Kegel exercises to improve the circulation to the area.
Warning: Massive rectal bleeding can be a serious problem. It can be caused by ectopic pregnancies or serious internal problems. Seek medical care immediately if you’re bleeding heavily from the anus.
Nosebleeds and nasal congestion
Like many of the complaints of pregnancy, nasal stuffiness and nosebleeds are believed to be due in large part to estrogen and progesterone. These hormones cause increased blood flow and swelling of the blood vessels in the mucus membranes.
Particularly in cold, dry weather, this can mean that you feel more congested than normal. You may also experience nosebleeds more often than you did before getting pregnant.
You may want to try the following to ease your nasal symptoms:
- Use a humidifier to help with the dryness that can make symptoms worse.
- Blow your nose gently by closing one nostril while you blow through the other.
- Curb nosebleeds by leaning forward and applying gentle pressure to the nose. Try squeezing it with the thumb and forefinger for five minutes. Repeat if necessary.
- Call your doctor if the bleeding doesn’t stop, or is heavy or frequent.
- Seek emergency medical care if nasal congestion makes it hard to breathe.

The same changes in hormones and blood vessels that cause nasal bleeding can cause sensitive gums. If you experience bleeding when flossing or brushing your teeth, try using a softer toothbrush.
Visit a dentist if you bleed a lot or have a lot of pain when flossing or brushing your teeth. Serious dental problems can be a sign of other health concerns that can complicate pregnancy.
Discharge
Many women experience different types of discharge during the second trimester. Pay attention to the color, smell, amount, and frequency of vaginal or anal discharge. Some types of discharge may indicate an infection that needs medical attention or treatment.
Vaginal discharge
As the pregnancy progresses, you may notice increasing vaginal discharge. Typically, it looks like egg whites and is milky and a bit odorous. It may remind you of premenstrual discharge, only a bit heavier and more frequent.
This discharge is totally normal and is just another change your body goes through in response to the pregnancy hormones and the increased blood flow to the area.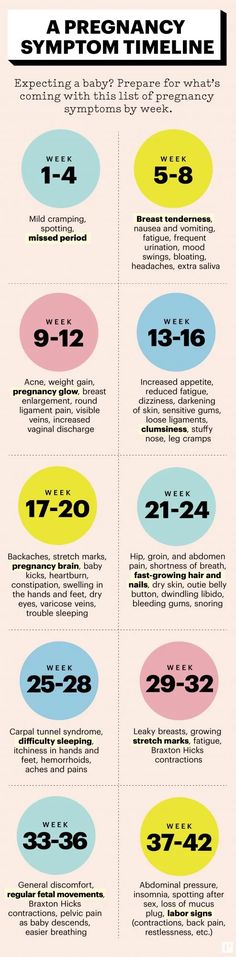 You can wear panty liners or change your underwear more often than usual if you find the discharge bothersome.
You can wear panty liners or change your underwear more often than usual if you find the discharge bothersome.
Though the kind of discharge described above is normal, there are some types of discharge that may mean you have an infection.
Vulvovaginal candidiasis, or yeast infection, is very common during pregnancy. Signs include a thick, cottage cheese-like discharge accompanied by itching, redness, and burning, as well as painful intercourse and urination.
Sexually transmitted infections (STIs) may also occur during pregnancy, and because many of them can affect the fetus, it’s important that they be treated.
You may have a condition that requires treatment if any of the following is true:
- The discharge looks like pus.
- The discharge is yellow, green, or has a foul odor.
- You notice a burning sensation when you urinate.
- Your labia are red, swollen, or itchy.
Unlike signs of infection, clear or pinkish watery discharge may be a sign of premature rupture of the amniotic sac.
Rupture of the sac may cause a trickle of watery discharge or a rush of lots of watery fluid from the vagina. This is commonly known as having the water break before labor begins.
Warning: If you experience a steady trickle or a rush of watery discharge during the second trimester, call a doctor immediately. It may be a sign of premature labor or a tear in the amniotic sac.
Rectal discharge
In addition to bleeding from the rectum, some women may experience anal discharge during pregnancy. Rectal discharge may be caused by STIs, bowel and gastrointestinal problems, or physical wounds in the rectum. If you’re experiencing rectal discharge, consult a doctor.
Gonorrhea, chlamydia, and other infections that can be transmitted through sexual contact can cause an infection in the anus. These infections can cause lesions or sores that bleed. In addition, they may lead to discharge that’s foul-smelling, green or yellow, and thick.
In addition, they may lead to discharge that’s foul-smelling, green or yellow, and thick.
It may be painful to wipe or go to the bathroom. If you have these symptoms, discuss them with a doctor. Left untreated, they may cause serious problems for the baby. Most STIs can be treated with antibiotics.
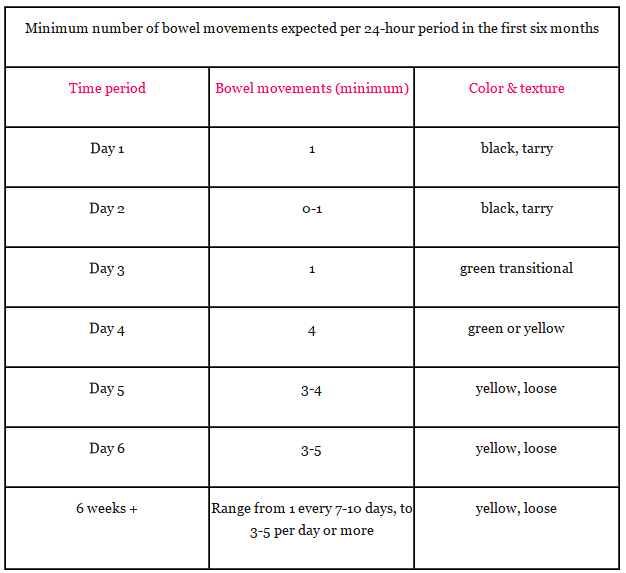
Some pregnant women may experience anal discharge due to bowel problems or gastrointestinal disorders. These may result in mucus or watery discharge from the anus.
Certain gastrointestinal problems or food poisoning may also cause frequent diarrhea or fecal matter with unusual colors or textures. Tell your doctor about any unusual characteristics of your bowel movements. Some conditions require immediate treatment.
Finally, if you have a hemorrhoid or anal fissure that has become infected, you may notice unusual rectal discharge. Infected wounds may cause brown, yellow, green, or white discharge.
Such a wound may or may not have a foul smell. Infected sores are often very painful and require medical attention. Consult a doctor for treatment if you experience anal discharge of this nature.
Consult a doctor for treatment if you experience anal discharge of this nature.
Nipple discharge
Many women experience discharge from one or both nipples during the second trimester of pregnancy. Breast tenderness and changes in nipple color are also common during pregnancy.
Discharge is most common in women who have previously given birth. Nipple discharge is often clear, milky, or yellowish in color.
Discharge from the nipples is normally not a sign of a problem, unless the following symptoms are present:
- The nipple changes in size or becomes inverted.
- The nipple is dry, cracked, or painful.
- The nipple has a rash or new bumps.
- The discharge is foul-smelling, bloody, green, or brown.
If you aren’t sure whether your nipple discharge is normal, call a doctor to discuss your symptoms.
How much pain, bleeding, and discharge is normal?
Some pain and a small amount of spotting are normal during the second trimester.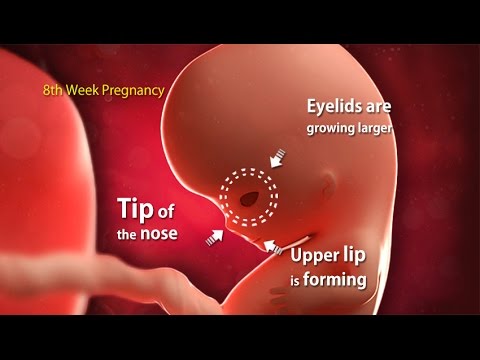 However, it is essential to know when to see a doctor.
However, it is essential to know when to see a doctor.
For many people, the second trimester marks a moment of calm in pregnancy. The intense symptoms of the first trimester often dissipate, and the exhaustion, muscle pain, and anxiety about birth that are common during the third trimester may not have appeared.
Small amounts of bleeding during the second trimester are typical and may not signal a problem, though it is important to get checked if something feels wrong. In this article, we look at the possible causes and when to see a doctor.
Bleeding is common during the first trimester of pregnancy, affecting 15 to 25 percent of pregnant women.
Bleeding in the second trimester is less usual, with heavier bleeding being a more serious sign than light bleeding. Causes can range from mild inflammation to problems with the placenta or cervix.
Bleeding does not usually mean a woman is going into labor or having a miscarriage.
Women who experience mild bleeding, spotting, or unusual discharge should contact their healthcare providers. When bleeding is heavy or painful, it is a medical emergency.
When bleeding is heavy or painful, it is a medical emergency.
Possible causes of bleeding in the second trimester include:
Minor cervical irritation
Light spotting does not usually mean that there is a serious problem with the pregnancy, especially if the spotting goes away on its own within a day or two.
During pregnancy, the blood vessels in the cervix may become inflamed, especially when the weight of the uterus puts pressure on them. Some women can experience light bleeding after a pelvic exam or sex.
Cervical growths
Cervical polyps are benign, or non-cancerous, growths on the cervix. They are common and rarely cause any problems.
During pregnancy, cervical polyps may swell or become irritated, causing them to bleed. A doctor can often carry out a quick exam to identify whether a cervical growth is a reason for a person’s bleeding
Placenta issues
The placenta is an organ that nourishes and protects the developing baby. Problems with this organ are a leading cause of bleeding during birth.
Problems with this organ are a leading cause of bleeding during birth.
Anyone who suspects problems with the placenta must seek immediate treatment, as issues with the placenta can injure the baby and cause dangerous bleeding in the pregnant woman.
Some placenta issues that may cause bleeding in the second trimester include:
- Placenta previa: This is when the placenta is very low in the uterus. It may fully or partially cover the cervix, causing bleeding throughout pregnancy. In severe cases, doctors may recommend extra monitoring or a cesarean delivery.
- Placenta accreta: Placenta accreta causes the placenta to grow much deeper into the uterus than usual. It is more likely to cause bleeding during the third trimester than the second, however. During delivery, the bleeding may become life-threatening, so healthcare professionals will monitor the pregnancy carefully, often in a setting with emergency medical care, which may be critical to the mother’s safety.

- Placenta abruption: Sometimes the placenta detaches from the uterus too early. It can cause bleeding, back pain, and intense stomach cramps. Early diagnosis can prevent severe complications to the woman and the baby.
Preterm labor
Bleeding can be an early sign of labor. Some women may also notice an unusual discharge, called a mucous plug. A mucous plug looks like a combination of vaginal discharge, mucous, and blood.
When labor begins before 37 weeks, it is more likely that the baby will need to stay in the intensive care unit and may also experience other problems. During the second trimester, preterm labor endangers the baby’s life.
Bleeding can be a risk factor for preterm labor. Women who have a history of bleeding during the second trimester can talk to their doctors about whether they are at risk of preterm labor and how best to minimize that risk.
Vasa previa
Vasa previa is a problem with the baby’s blood vessels.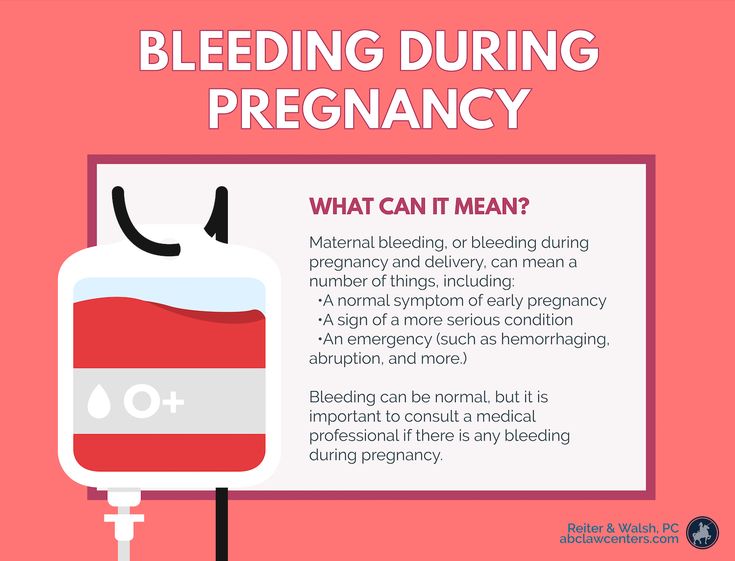 It causes some of the baby’s blood vessels to run parallel to the cervix, left unprotected by the umbilical cord or placenta. These blood vessels may cause unusual bleeding, especially late in pregnancy or during preterm labor.
It causes some of the baby’s blood vessels to run parallel to the cervix, left unprotected by the umbilical cord or placenta. These blood vessels may cause unusual bleeding, especially late in pregnancy or during preterm labor.
When the membranes burst, these vessels may also burst. Women with vasa previa usually have a cesarean delivery. A woman with a history of preterm labor or bleeding who has contractions or other intense pain should go to the emergency room.
Uterine rupture
Uterine rupture happens when the uterus tears. This can endanger the mother and the baby by causing severe bleeding and depriving the baby of oxygen. It can also trigger labor.
A woman who experiences bleeding, pain, a fever, or who has recently suffered an injury to the stomach or uterus may be experiencing a uterine rupture and should go to the emergency room.
Gestational trophoblastic disease
Gestational trophoblastic disease (GTD) is a group of rare diseases that causes abnormal cells to grow in the uterus during and after pregnancy. These cells can form tumors and masses. Sometimes these masses turn cancerous, though most forms of GTD are benign.
These cells can form tumors and masses. Sometimes these masses turn cancerous, though most forms of GTD are benign.
Women with GTD may have bleeding and an unusually large uterus.
Treatment depends on the type of GTD, how large the growth is, and other factors. A surgeon may need to remove the mass during or after pregnancy.
Not all bleeding during the second trimester is an emergency. In many cases, the woman and the baby are fine.
Nevertheless, it is important to be cautious. Prompt intervention in emergencies can save the life of both the woman and the baby. Anyone who is uncertain should go to the emergency room.
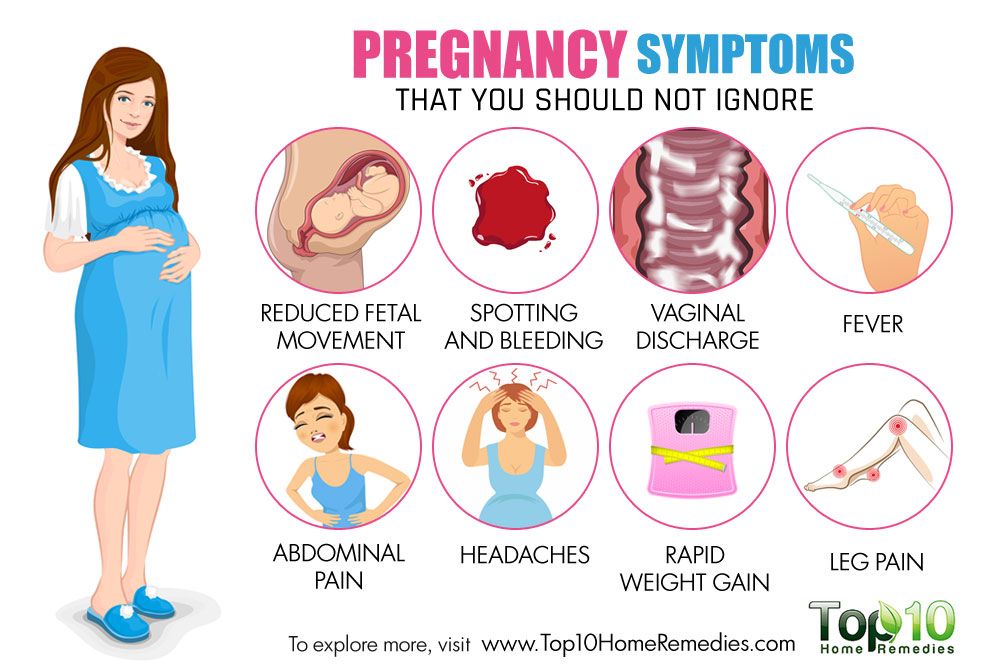
Some symptoms that warrant emergency treatment include:
- bleeding after an injury, such as a car accident or fall
- sudden heavy bleeding
- bleeding that is getting progressively heavier
- bleeding that includes blood clots
- bleeding along with pain or contractions
- dizziness or weakness along with bleeding
- bleeding in a person with placenta accreta, placenta previa, or a history of preterm labor
Tell a doctor about any bleeding episodes to ensure a prompt and accurate diagnosis.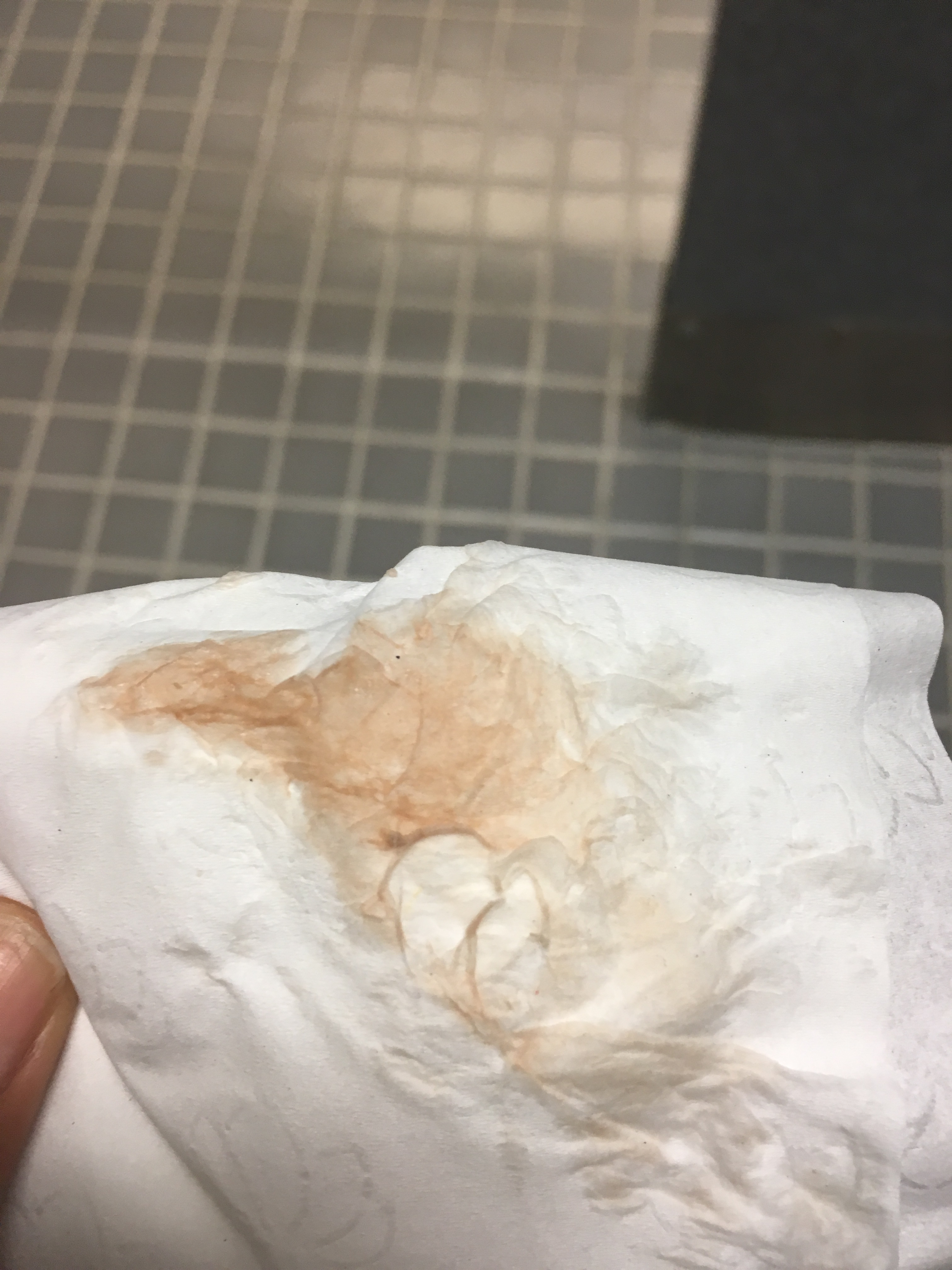 Anyone who is uncertain about their bleeding should call right away.
Anyone who is uncertain about their bleeding should call right away.
Bleeding during the second trimester can be worrying. However, even when the bleeding is due to a serious complication, most women go on to have healthy pregnancies and babies.
Prompt medical care can prevent complications and save lives, so always talk to a provider about any bleeding, even if it seems minor.
Bloody discharge during pregnancy ᐈ Blood during early pregnancy
Seeing bloody discharge, a pregnant woman is always frightened. They are considered a symptom of miscarriage and other equally serious pathologies. At the same time, in some cases, the appearance of a small amount of blood is considered the norm and does not pose a threat to the life and health of the fetus or the expectant mother.
In early pregnancy, bloody discharge occurs in 25% of women. In most cases, they are associated with the implantation of the fetal egg to the wall of the uterus. Also, scanty spotting may appear on the dates of the expected menstruation.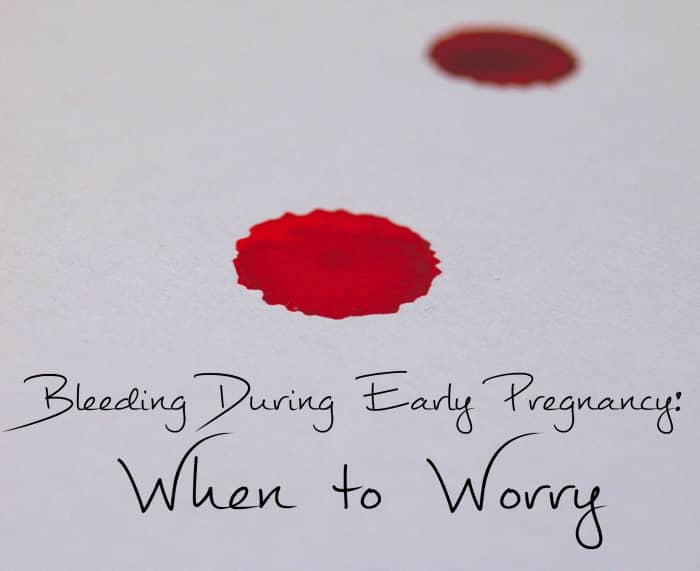 If they end quickly, are not accompanied by pain, and the woman has not had miscarriages or pregnancy complications before, most likely she has nothing to worry about. However, it is necessary to consult an obstetrician-gynecologist and undergo an examination. nine0003
If they end quickly, are not accompanied by pain, and the woman has not had miscarriages or pregnancy complications before, most likely she has nothing to worry about. However, it is necessary to consult an obstetrician-gynecologist and undergo an examination. nine0003
Why bloody discharge can appear and when it is dangerous, said Elena Petrovna Domnich, obstetrician-gynecologist of the highest category, gynecologist-endocrinologist, ultrasound specialist of the ADONIS medical center.
Elena Nikolaevna, tell me, can a woman have periods during pregnancy?
- Sometimes during pregnancy, a woman may experience spotting, but this should not be interpreted as menstruation. Menstruation occurs at the end of the menstrual cycle, during which the endometrium changes, first proliferative, then secretory. During the cycle, the endometrium prepares for pregnancy, and if it does not occur, then menstruation begins. nine0003
In the event of pregnancy, menstruation is not possible, although bleeding may occur at the expected time. Because of this, some women do not immediately know that they are pregnant. However, when the obstetrician-gynecologist at the reception asks them about the nature of the discharge, it always turns out that they are different from menstrual. As a rule, they are more scarce, pass faster and are not accompanied by other symptoms. Sometimes a woman says that her period was very recent, but at the time of examination and examination, we find that she is already 8 or 12 weeks pregnant. nine0003
Because of this, some women do not immediately know that they are pregnant. However, when the obstetrician-gynecologist at the reception asks them about the nature of the discharge, it always turns out that they are different from menstrual. As a rule, they are more scarce, pass faster and are not accompanied by other symptoms. Sometimes a woman says that her period was very recent, but at the time of examination and examination, we find that she is already 8 or 12 weeks pregnant. nine0003
How often does this happen? Is spotting during pregnancy an exception or a fairly common occurrence?
- Bloody discharge is not common in pregnant women, but still it cannot be said that these are exceptional cases.
Tell me, if a woman is planning to conceive a child, and during the expected period she has atypical discharge, should she take a pregnancy test? nine0012
– Yes, but it is better to visit an obstetrician-gynecologist.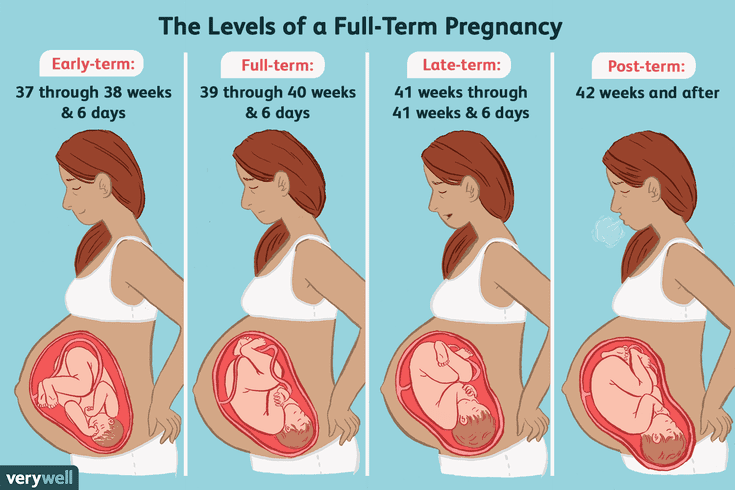 There are cases when a woman is pregnant, but the test strip shows a negative result. To accurately determine whether there is a pregnancy, allows a blood test for the level of hCG.
There are cases when a woman is pregnant, but the test strip shows a negative result. To accurately determine whether there is a pregnancy, allows a blood test for the level of hCG.
So bleeding during pregnancy is not menstruation, but bleeding? Why can it appear and why is it dangerous?
- Yes, that's right. This is bleeding, not menstruation. It can be a symptom of a miscarriage, ectopic pregnancy, or other pathology. For diagnosis, you must consult a doctor. nine0003
Tell me more, if a woman has a discharge and thinks she is menstruating, but a previous pregnancy test came back positive, could it be wrong?
- A pregnancy test is sometimes positive even if it is not. This happens if a woman has formed luteal cysts or developed a thyroid disease.
Bloody discharge during pregnancy requires contacting the antenatal clinic or the medical center where the woman was registered for pregnancy management. Sometimes they may not be dangerous, but without diagnosis, it cannot be ruled out that this is a symptom of a serious disorder. nine0003
Sometimes they may not be dangerous, but without diagnosis, it cannot be ruled out that this is a symptom of a serious disorder. nine0003
Bleeding may occur with:
- threatened miscarriage;
- ectopic pregnancy;
- infectious diseases of the reproductive system;
- cysts;
- myomas;
- cervical erosion;
- placental abruption;
- threatened preterm birth.
You can watch the video version of Elena Petrovna Domnich's interview here. More helpful videos on our YouTube channel. nine0003
Pregnancy discharge | What are the discharge during pregnancy? | Blog
In the absence of menstruation, girls usually suspect that conception has occurred. However, during pregnancy, the female body may continue to secrete a secret of a different color and character. We recommend that you keep a close eye on everything that happens so as not to miss the development of adverse events.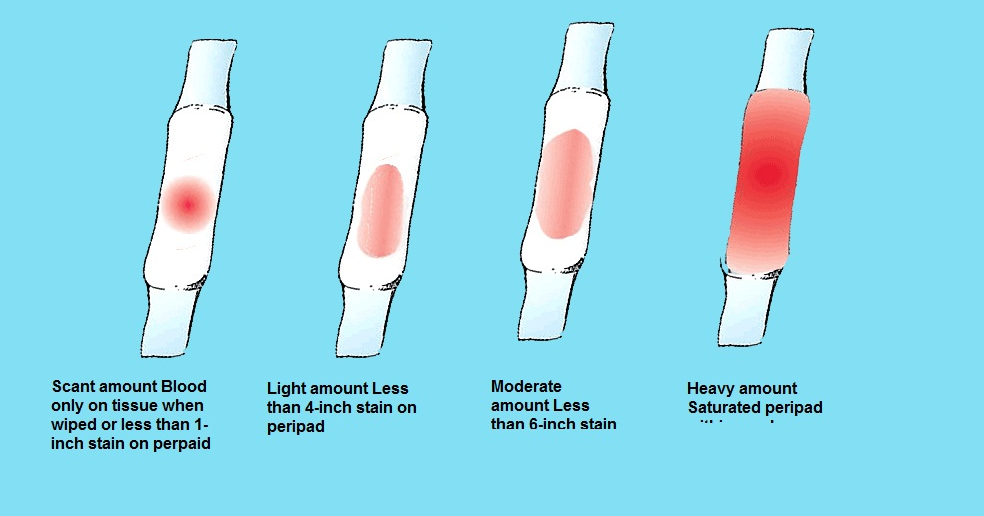 We will talk about how to recognize problem situations during pregnancy in the article.
We will talk about how to recognize problem situations during pregnancy in the article.
What discharge can occur during conception
Many women note that immediately after the delay and in the later stages, the nature of secretion changes. It can be:
- With or without scent.
- Depending on the color - transparent, white, cream, yellow, greenish, bloody.
- By consistency - thick, liquid, cheesy.
- As a symptom for assessing the state of health - threatening, safe.
During ovulation, the egg is released from the ovary, its membrane is deflated, a small amount of fluid is released - so it becomes ready for fertilization. At this time, the thick mucus that fills the cervical canal of the cervix becomes less viscous. This makes it easier for the spermatozoa to penetrate and move further into the tubes for fertilization. At this time, you may notice an abundance of clear mucous secretion. nine0003
After the fusion of the egg with the spermatozoon, movement into the uterus begins, which should end with implantation in the inner layer. During penetration, its slight detachment may occur - this causes damage to the blood vessels that abundantly penetrate the muscular layer of the uterus. You may see light brown discharge, which is common during pregnancy. The color is due to the fact that the blood has time to clot.
During penetration, its slight detachment may occur - this causes damage to the blood vessels that abundantly penetrate the muscular layer of the uterus. You may see light brown discharge, which is common during pregnancy. The color is due to the fact that the blood has time to clot.
Sometimes the discharge is brightly colored and some women mistake it for a period that has started too early. But in this case, a short duration is characteristic, a different shade (dark or scarlet), a slight mark on the linen. nine0003
With some features of the structure of the female genital organs (for example, with a bicornuate uterus), after implantation of the embryo in one part, rejection of the endometrium may begin in the other, as usually occurs during menstruation. This rarely happens.
Characteristics of discharge in the event of a threatened miscarriage
Spontaneous abortion is the rejection of an embryo in the early stages after conception. If at the first signs of pregnancy, you notice spotting, there is a high probability that a miscarriage begins.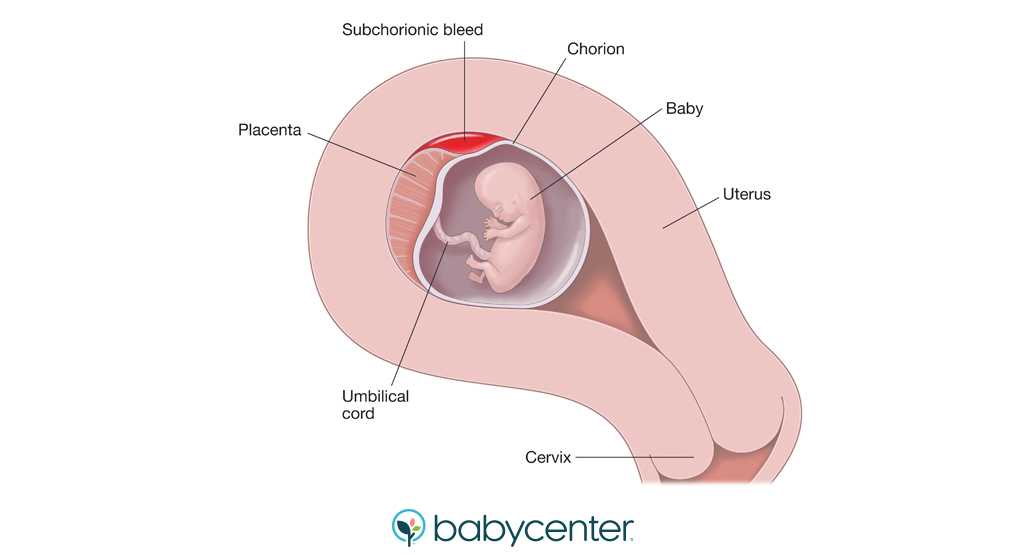 nine0003
nine0003
Also, miscarriage symptoms include:
- pulling or pressing on the lower abdomen, sacrum, lower back;
- the muscles of the uterus are tense.
The woman may experience cramps. This continues all the time or intermittently. From the vagina there are scarlet or brown discharge during pregnancy, which was previously confirmed. Sometimes the period may be still small, and the first signs did not have time to appear.
After 22 weeks, this phenomenon is called preterm labor. The child in this case is still weak, the organs are not sufficiently developed, and there is little chance of survival. nine0003
The following factors increase the risk of miscarriage:
- various diseases;
- progesterone deficiency;
- nervous and physical strain;
- pathologies in the genitals;
- fetal developmental defects.
To confirm the diagnosis, the doctor prescribes an ultrasound scan. If it shows that the fetal heart rate is disturbed, the tone of the uterus is increased, its size differs from normal for this period, hospitalization will be recommended to maintain pregnancy. nine0003
If it shows that the fetal heart rate is disturbed, the tone of the uterus is increased, its size differs from normal for this period, hospitalization will be recommended to maintain pregnancy. nine0003
What discharge during pregnancy is considered normal
This secretion does not pose a threat to health:
- transparent;
- whitish;
- yellowish;
- odor free;
- mucous;
- without itching, burning, redness of the genitals.
Clear fluid on underwear is a symptom of ovulation. During pregnancy, the activity of ongoing processes in the body increases, so the amount of secretion secreted may increase. However, a violation of the norm is the leakage of amniotic fluid. You can determine the problem with the help of special diagnostic tests that the doctor will prescribe if he has suspicions. nine0003
White color, small amount, homogeneous structure should also not cause concern. The increased volume of fluid in this case is associated with increased hormonal activity.
One of the variants of the norm is mucous discharge, which smells of slight sourness. If there is no pain, discomfort, there is nothing to worry about.
Yellow discharge, there are signs of pregnancy, there is no unpleasant odor - you are all right. Some women had this color before conception, only they did not pay attention. Now there are more of them, therefore more noticeable. nine0003
Sometimes a woman observes that the laundry gets wet and there is a smell of urine. This may indicate incontinence due to the constant pressure of the growing uterus. In this case, it is recommended to go to the toilet more often, change underpants twice a day.
What discharge during pregnancy is considered a sign of infection?
White discharge during pregnancy with a cheesy texture is a symptom of thrush (candidiasis). In pregnant women, it is diagnosed quite often - the reason is a change in hormonal levels. The disease is accompanied by itching, redness of the vulva, a strong sour smell. Sometimes external manifestations are not detected, then treatment is not carried out. nine0003
Sometimes external manifestations are not detected, then treatment is not carried out. nine0003
Infection is indicated by pain, pain, skin irritation, ulcers, smell of rot or fish, gray or green color, frothy discharge, increased nervousness, large inguinal lymph nodes. The reason may lie in sexually transmitted infections. This includes syphilis, gonorrhea, trichomoniasis, chlamydia and others. They are dangerous because they cause premature birth and fetal developmental defects.
Which discharge during pregnancy should be paid special attention to and should I consult a doctor? nine0013
The following indicates that pregnancy is at risk:
- Severe pain in the perineum, bleeding, difficulty defecation, convulsions - these can be injuries to the vaginal mucosa.
- Nausea, profuse vomiting, swelling, headaches, cough, hypertension, bright red secretion are symptoms of hydatidiform mole (abnormal development of the embryo).
- A drop in blood pressure, pallor, weakness, sweating, pulling sensations, bleeding during pregnancy against the background of a lack of growth of hCG in the blood - this is how ectopic attachment manifests itself.
 nine0068
nine0068 - Isolation of clots, sharp pain, vomiting, diarrhea may indicate a frozen fetus.
If you experience any of these symptoms, contact your doctor immediately.
It is also necessary to go to the clinic if you have been physically abused, had rough sex, had an accident, fell, hit. The likelihood that the situation will be resolved successfully is much higher if you do not delay the visit, listen to the symptoms and take good care of your health. nine0003
Remember, despite the fact that pregnancy is a normal state of health of the female body, the diagnosis and treatment tactics are still different, due to the many restrictions on manipulations and medications during pregnancy. That is why diagnosis and treatment during pregnancy should take place only under the supervision of a doctor. By ignoring the symptoms or self-medicating, a pregnant woman risks not only her health, but also the health of her child.
Doctors of the Leleka maternity hospital manage pregnancies of any complexity, including those aggravated by infections, pathologies, and the threat of miscarriage.