Birth of baby by operation
C-Section (Cesarean Section): Procedure, Risks & Recovery
Overview
What is a C-section?
A C-section, also called a cesarean section or cesarean delivery, is a surgical procedure in which a baby is delivered through incisions in your abdomen and uterus. They're performed when a vaginal delivery is not possible or safe, or when the health of you or your baby is at risk.
When would I need a C-section?
You may need a C-section if you have certain medical conditions or if complications occur during labor in a vaginal delivery. A planned C-section happens when any of the following conditions exist:
- Cephalopelvic disproportion (CPD): CPD is a term that means that your baby's head or body is too large to pass safely through your pelvis, or your pelvis is too small to deliver an average-sized baby.
- Previous C-section: Although it’s possible to have a vaginal birth after a previous C-section, it’s not an option for everyone.
Factors that can affect this include type of uterine incision used in the previous C-section and the risk of uterine rupture.
- Expecting multiples: Although twins can often be delivered vaginally, two or more babies might require a C-section.
- Placenta previa: In this condition, the placenta is attached too low in your uterus and blocks your baby's exit through your cervix.
- Transverse lie: The baby is in a horizontal, or sideways, position in your uterus.
- Breech presentation: In a breech presentation, your baby's feet- or bottom-first in your uterus. Some providers may attempt to turn your baby, but a C-section will be necessary if that's unsuccessful.
- Health conditions: Conditions like heart disease could worsen with labor during a vaginal birth. A C-section is necessary if you have genital herpes at the time of delivery.
- Obstruction: A large uterine fibroid, a pelvic fracture or you're expecting a baby with certain congenital anomalies may also be reasons for a C-section.

An unplanned C-section delivery might be necessary if any of the following conditions arise during your labor:
- Labor isn't progressing: Also called prolonged labor, this means your cervix dilates and stops, doesn't efface (or thin) or your baby stops moving down the birth canal.
- Umbilical cord compression: The umbilical cord is looped around your baby's neck or body or caught between your baby's head and your pelvis.
- Umbilical cord prolapse: The umbilical cord comes out of your cervix before your baby does.
- Placental abruption: The placenta separates from the wall of your uterus before your baby is born.
- Fetal distress: Your baby might develop problems that cause an irregular heart rate during labor. Your obstetrician might decide that the baby can no longer tolerate labor and that a C-section is necessary.
How common are C-sections?
According to the Centers for Disease Control (CDC), C-sections account for about 30% of all deliveries in the United States.
Procedure Details
What can I expect before a C-section?
If you have a planned C-section, the following procedures will take place:
- You'll sign consent forms for the procedure.
- The anesthesiologist will discuss options for anesthesia. Most often, it's an epidural (or spinal block) that numbs you from your breasts down to your feet.
- The hair in the area around the incision will be clipped or shaved.
- A catheter will be inserted to keep your bladder empty.
- You will have heart and blood pressure monitors applied.
- You'll get an IV in your hand or arm to give you medicine and fluid.
- You'll discuss the procedure and what to expect with your obstetrician (if you haven't already).
If you need an emergency C-section, your obstetrician delivers your baby quickly because either the health of you or your baby is at risk. However, there's typically not much time to prepare, and you may need general anesthesia because it works faster.
What actually happens during a C-section?
The first step in a C-section procedure is preparing you for anesthesia. Most planned C-sections use an epidural, so you are awake for the delivery. However, in some cases, you're asleep under general anesthesia.
Your abdomen will be cleaned with an antiseptic, and you might have an oxygen mask placed over your mouth and nose to increase oxygen to your baby. Next, your provider places a sterile drape around the incision site and over your legs and chest. Finally, your providers raise a sterile curtain or drape between your head and your lower body.
The obstetrician will then make an incision through your skin and into the wall of your abdomen. They might use either a vertical or transverse incision. A horizontal incision is also called a bikini incision.
Next, your provider cuts a 3- to 4-inch incision into the wall of your uterus. This incision can also be transverse or vertical. Finally, the obstetrician removes your baby through the incisions.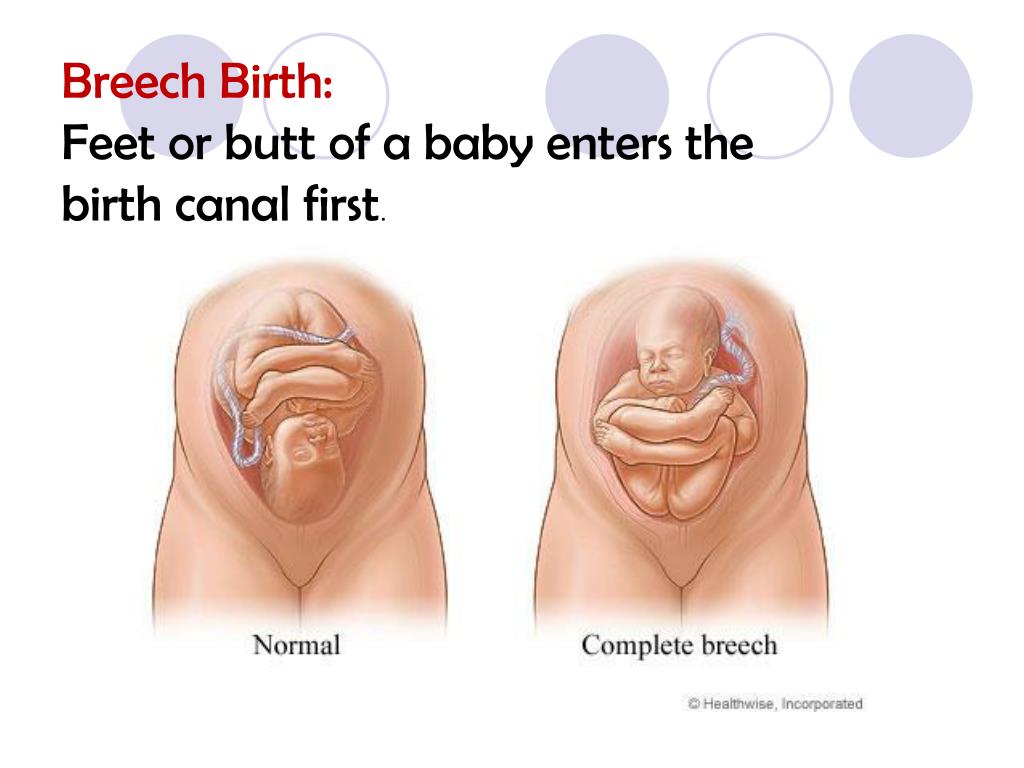 The umbilical cord is cut, the placenta is removed and the incisions are closed with stitches and staples.
The umbilical cord is cut, the placenta is removed and the incisions are closed with stitches and staples.
Emergency C-sections follow the same steps; however, the speed at which your baby is removed is different. During a planned C-section, the delivery takes about 10 to 15 minutes. Your provider removes your baby in only a few minutes in an emergency C-section.
If you're awake for your C-section surgery, you will be able to see and hold your baby shortly after it's born.
What does a C-section feel like?
You'll be under anesthesia, which should prevent you from feeling any pain. Most people report feeling a tug or pull when their baby is removed from their abdomen.
Are C-sections safe?
Vaginal births are usually preferred, but in some cases, a C-section is the only safe option. For example, a C-section is the safer option when your baby is breech or you have placenta previa (placenta covers part of the cervix). A C-section carries risks and benefits, which should be discussed with your pregnancy care provider.
How long does a C-section surgery take?
The typical C-section takes about 45 minutes from start to finish. After your provider delivers your baby, they'll stitch your uterus and close the incision in your abdomen. Different types of emergencies can arise during a delivery. In some cases, the delivery will happen very quickly, with your baby being delivered in as little as 15 minutes. This is an emergency C-section.
What happens after a C-section?
Like vaginal births, your obstetrician will deliver the placenta after your baby is born. Next, your provider will stitch your uterus and stitch or staple your abdominal muscles. Stitches should dissolve, but staples are removed at the hospital about one week later. Your abdomen will be sore for several days or weeks. In some cases, your provider may prescribe stronger pain medication.
You can expect to limit your activities, take it easy and rely on family and friends once you go home. A typical C-section surgery requires at least two to three days in the hospital.
Risks / Benefits
What are the benefits of a C-section?
The advantages of a C-section depend on your pregnancy. In most cases, the biggest benefit of a C-section is that it's safer for both you and your baby. When a vaginal birth is risky or could hurt your baby, most providers will turn to a C-section to minimize risks. Sometimes C-sections are unplanned. For example, if your baby's heart rate drops to an unsafe level, an emergency C-section is safer than letting your baby's heart rate decline further.
What are the risks involved in a C-section?
Like any surgery, a C-section involves some risks. The risks of complications are slightly higher with C-sections than with vaginal delivery. These might include:
- Infection.
- Loss of blood (hemorrhage).
- A blood clot that may break off and enter your bloodstream (embolism).
- Injury to the bowel or bladder.
- A cut that might weaken the uterine wall.
- Abnormalities of the placenta in future pregnancies.

- Risks from general anesthesia.
- Fetal injury.
Other disadvantages of having a C-section are:
- Recovering from a C-section may be more difficult than a vaginal delivery.
- C-sections are more likely to cause chronic pelvic pain.
- You're more likely to have a C-section in future pregnancies.
- Your baby may have trouble breastfeeding.
- Your baby may be at greater risk for breathing problems.
Recovery and Outlook
How long does a C-section recovery take?
Once the anesthesia wears off, you’ll begin to feel the pain from the incisions. You might also experience gas pains and have trouble taking deep breaths. Make sure an adult is there to help you get up from bed the first several days following C-section surgery. Most people stay in the hospital between two and three days.
A full recovery can take between four and six weeks. Ask your healthcare provider what you can expect during recovery. Most providers recommend avoiding steps, lifting, exercise and other strenuous activities for several weeks. Ask your friends or partner for help with errands, cooking and cleaning so you can rest and recover. Your provider may put restrictions on driving until you're able to turn your body and apply pressure to the pedals with ease.
Most providers recommend avoiding steps, lifting, exercise and other strenuous activities for several weeks. Ask your friends or partner for help with errands, cooking and cleaning so you can rest and recover. Your provider may put restrictions on driving until you're able to turn your body and apply pressure to the pedals with ease.
You can expect cramping and bleeding for up to six weeks, as well as some discomfort around the incision. Taking over-the-counter pain relievers such as acetaminophen or ibuprofen for pain may help. Avoid sex for at least six weeks or until your healthcare provider gives you the OK.
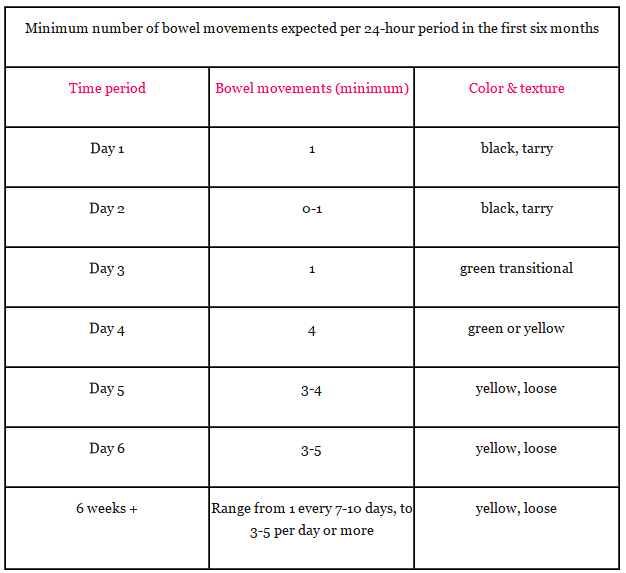
You will also have a vaginal discharge after the surgery due to the shedding of your uterine lining. The discharge, called lochia, will be red at first and then gradually change to yellow. Be sure to call your healthcare provider if you experience heavy bleeding or a foul odor from the vaginal discharge. Use sanitary pads, not tampons, until you're completely done bleeding.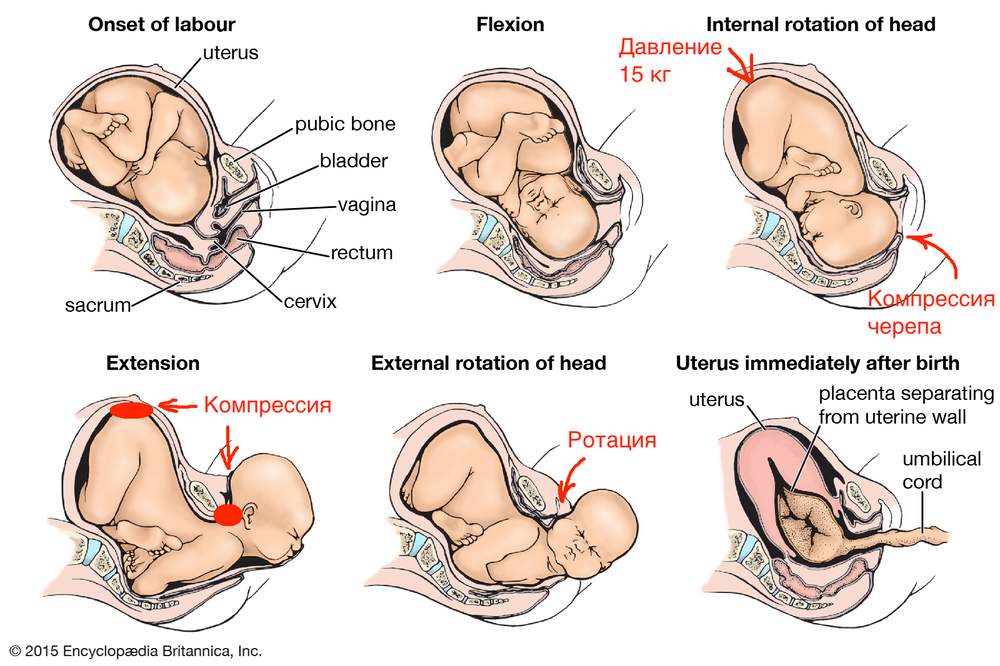
Can I have a baby vaginally after a C-section?
The majority of people who had a C-section can consider a vaginal delivery in future pregnancies. If you meet the following criteria, your chances of vaginal birth after cesarean (VBAC) are significantly increased:
- Your provider used a low transverse incision.
- Your pelvis is not too small to accommodate an average-sized baby.
- You're not expecting multiples.
- Your first C-section was only performed because your baby was breech.
When to Call the Doctor
When should I see my healthcare provider?
If you have an infection at your C-section incision, contact your healthcare provider. Watch for signs of infection such as:
- Red or swollen incision.
- Pus or leaking discharge from the incision.
- Fever or worsening pain.
Other signs of a problem include heavy bleeding or severe pelvic pain and cramping.
Additional Details
What is more painful: a C-section or natural birth?
The level of pain you experience during childbirth is unique. For example, if you opt for an unmedicated vaginal birth, you can expect more pain than someone who had an epidural before a vaginal birth. During a C-section delivery, you won't feel much pain. However, recovering from a C-section may be more painful and take longer than recovering from a natural birth. There isn't a right or wrong answer as to what is more painful because every birth is different.
For example, if you opt for an unmedicated vaginal birth, you can expect more pain than someone who had an epidural before a vaginal birth. During a C-section delivery, you won't feel much pain. However, recovering from a C-section may be more painful and take longer than recovering from a natural birth. There isn't a right or wrong answer as to what is more painful because every birth is different.
How many C-sections can you have?
The number of C-sections you can have is unique to your medical history and pregnancy. An exact number hasn't been agreed on. The surgery may be slightly more complicated each time due to prior incisions or scarring.
A note from Cleveland Clinic
C-sections are often necessary for the health of you and your baby. If you know you're having a C-section, your obstetrician can walk you through the procedure and discuss the recovery process with you in advance. In the cases where a C-section is unexpected, you may end up feeling upset that your birth plan didn't go as expected. Just know that most providers prefer a vaginal delivery and that the decision to proceed with a C-section was made for you or your baby's wellbeing. The best thing you can do after a C-section delivery is rest and allow others to help you recover.
Just know that most providers prefer a vaginal delivery and that the decision to proceed with a C-section was made for you or your baby's wellbeing. The best thing you can do after a C-section delivery is rest and allow others to help you recover.
Caesarean (C-section) | Pregnancy Birth and Baby
Caesarean (C-section) | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is caesarean birth (C-section)?
A caesarean section (C-section or caesarean) is an operation to deliver a baby through a cut in the abdomen (tummy) and uterus (womb).
There are several reasons why you might plan for a caesarean, or your medical team might recommend you have a caesarean after labour begins.
Why might I need a C-section?
The most common reasons for having a caesarean are:
- concerns for the safety of you or your baby
- your baby is in the breech position (bottom first) and your doctor doesn’t recommend a vaginal breech birth
- your baby is transverse (lying sideways) and can’t be turned
- you have twins and the first one is in the breech position
- your placenta is covering the cervix (opening to the womb)
- you have had several previous caesareans
- there are complications such as severe bleeding
- your labour is not progressing
Around 1 in 3 babies in Australia are born by caesarean.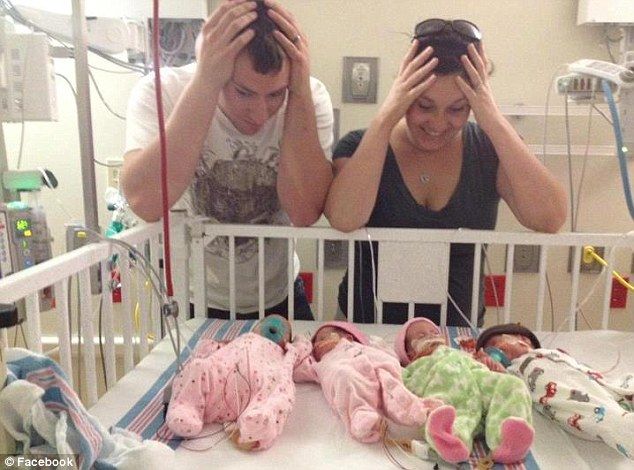 This is higher than the rate in many other developed countries. This rate is also increasing, both in private and in public hospitals, although you are more likely to have a caesarean in the private sector.
This is higher than the rate in many other developed countries. This rate is also increasing, both in private and in public hospitals, although you are more likely to have a caesarean in the private sector.
A caesarean might be planned (elective) if there is a reason preventing your baby been born by a vaginal birth. Sometimes before or during your labour, complications develop, and a C-section delivery needs to be done quickly. This is called an emergency caesarean.
Your doctor will discuss the reason you may need a caesarean based on your individual situation and, in some cases, your preferences.
What to expect if you have a caesarean birth
You may be in the operating theatre for one hour or more. The operation takes about 30 to 40 minutes. The baby is usually born in the first 10 minutes. The doctors will talk to you during the operation and tell you what is happening.
In most cases your partner or support person can be with you. You will also usually have a midwife with you. They will look after you and your baby in the theatre and recovery area.
They will look after you and your baby in the theatre and recovery area.
You will usually receive an epidural or spinal anaesthetic. This numbs the lower part of your body and lets you be awake throughout your caesarean birth. Sometimes emergency caesareans must be done under general anaesthetic which means you will be asleep during the birth.
A catheter (a thin flexible tube) will be placed into your bladder to collect urine. This is because you will not be able to get up to use the bathroom. You will have intravenous (IV) lines inserted into your arm to give you fluid and medicines.
Your tummy will be cleaned, and the obstetrician (doctor) will make a cut through the wall of your tummy near the pubic hair line. The doctor will cut through layers of fat and muscle and then through your uterus. Your baby is birthed through your tummy this way. If your baby needs to be delivered very quickly, the cut may be made from just below the belly button to above the pubic bone.
Diagram showing how a baby is born during a C-section
The doctor will remove the placenta and close the cut with stitches or staples. You will feel tugging and pulling if you are awake but not pain. You will also hear fluid being suctioned. A screen is usually put across your chest so you cannot see what is happening.
If you are awake, you can usually hold your baby straight after your caesarean birth and begin skin-to-skin contact and breastfeeding. Sometimes the baby’s nose and mouth need to be cleared of fluids or the baby may need additional treatment from the medical team.
Who will be in the room?
Your partner or support person will usually be able to be with you during your caesarean. There may also be a lot of medical staff, including:
- obstetrician — doctor who performs the operation and delivers the baby
- anaesthetist — doctor who administers the anaesthetic
- scrub nurse — passes instruments to the obstetrician
- scout nurse — assists the scrub nurse
- anaesthetic nurse — assists the anaesthetist
- paediatrician — doctor who looks after the baby after the birth
- midwife — nurse who looks after the baby until you return to the ward
- theatre technician — looks after the operating theatre and helps you on and off the table
What are the pain relief options?
The types of anaesthetic used in caesareans differ. Your doctor will choose the most appropriate for you.
Your doctor will choose the most appropriate for you.
Epidural
When you get an epidural, you receive a local anaesthetic then a hollow needle and a small, flexible tube (catheter) are inserted near the spinal cord in your back. The needle is removed, leaving the catheter in place. Anaesthetic medicine is injected through the catheter and can be topped up later.
Spinal block
Similar to an epidural, a spinal block injects a single dose of anaesthetic directly into the fluid around the spinal cord. You will go numb very quickly, but the amount of anaesthetic cannot be topped up.
General anaesthetic
You might be given a general anaesthetic if
- a spinal block or epidural anaesthetic doesn’t work
- there isn’t time for a spinal block or epidural anaesthetic to be used
- there are concerns for your health or your baby’s health
- you request a general anaesthetic
What are the risks and complications of C-sections?
A caesarean is major surgery. Complications are rare but they can be serious. The risks include:
Complications are rare but they can be serious. The risks include:
- blood loss
- wound infection
- blood clots
- possible damage to organs near the operation site, such as your bladder
- risks from the anaesthetic
The risk of complications increases if you are overweight.
If you have a caesarean, your future pregnancies will be considered higher risk and there are more risks with future caesareans.
Sometimes babies born by C-section can have temporary trouble breathing. The midwife and paediatrician will take care of your baby. There is a very small chance your baby can be cut during the operation. This is usually a small cut that isn’t deep and will heal on its own.
What should I expect when recovering from a caesarean birth?
There is usually a slower recovery after a caesarean birth compared with vaginal birth. You may feel pain for a few days, but this can usually be treated with pain-relief medication. Usually, you will stay in hospital for three to five days.
Usually, you will stay in hospital for three to five days.
Your obstetrician and midwife will provide advice about your recovery.
Sources:
The Royal Women's Hospital (Caesarean birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Caesarean section)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2022
Back To Top
Related pages
- Vaginal birth after caesarean (VBAC)
- Recovery after a caesarean
- Planned or elective caesarean
- Emergency caesarean
Need more information?
Caesarean Section
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Caesarean Section - Birth Trauma
Being abdominal surgery, pain in the early months is very common after a caesarean section (C-section) and needs to be managed with rest, pain relief, and
Read more on Australasian Birth Trauma Association website
Vaginal Birth after Caesarean Section
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Caesarean section - Better Health Channel
A caesarean section is usually performed when it is safer for the mother or the baby than a vaginal birth.
Read more on Better Health Channel website
Your Next Birth after Caesarean Section - Maternal, child and family health
Consumer brochure with information on birth options available to women planning their next birth after caesarean section.
Read more on NSW Health website
Elective caesarean birth: what to expect | Raising Children Network
Having a planned or elective caesarean birth? As with any major surgery, it helps to know what to expect during a caesarean section. Our guide explains.
Read more on raisingchildren.net.au website
Recovery after caesarean: first six weeks | Raising Children Network
This guide to recovery after caesarean section has tips for wound care, pain relief, practical help, physical and emotional recovery, and breastfeeding.
Read more on raisingchildren.net.au website
Recovery after a caesarean
Recovery after a caesarean section - whether it's an emergency or planned - will take several weeks. Find out what to expect after you have had your baby.
Read more on Pregnancy, Birth & Baby website
Vaginal birth after caesarean (VBAC)
If you've delivered a baby by caesarean (C-section), you may have a choice with your next pregnancy - a vaginal birth after caesarean (VBAC) or a planned (elective) caesarean.
Read more on Pregnancy, Birth & Baby website
Planned or elective caesarean
There are important things to consider if you are having a planned, or elective, caesarean.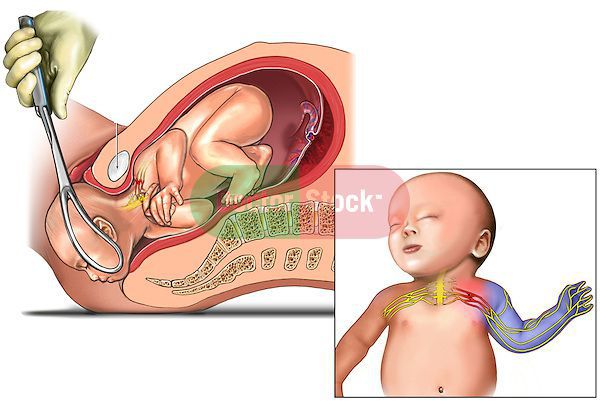
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.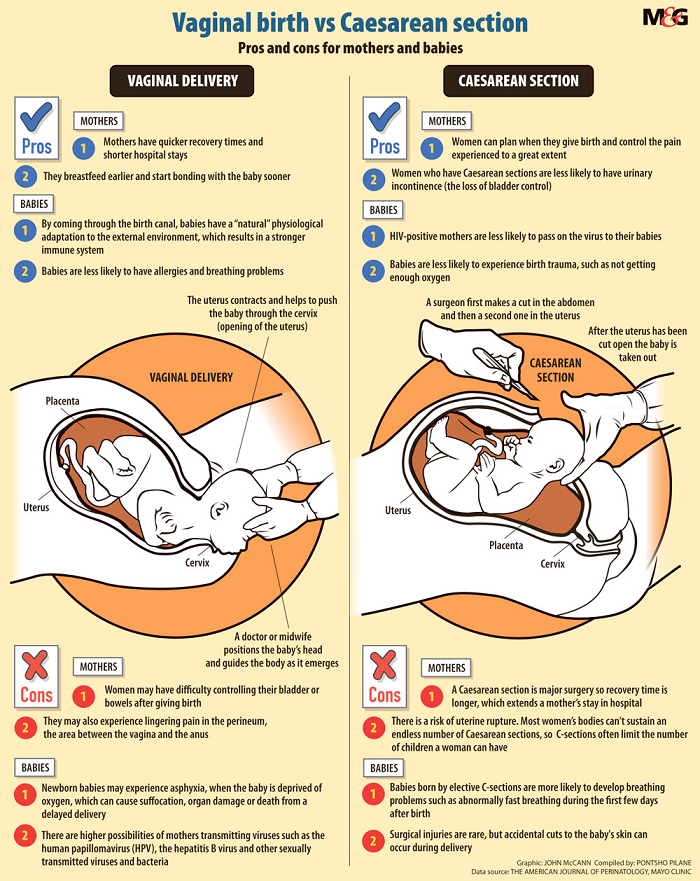
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Birth of a child by caesarean section
Main page / Interesting video
Views: 113
What progress has come to.
How can this be? The person is conscious, he talks, while behind the screen they take out the baby from the stomach, carry out manipulations in the cavity, and you do not feel anything exactly half of the body.
This is the merit of the anesthesiologist. Less than a minute and the expectant mother is ready for surgery. But what is the responsibility?
Yuri Svyatoslavovich Raspopin, PhD, anesthesiologist-resuscitator of the highest qualification category, head of the department of anesthesiology and resuscitation No. 2, says “isn’t it a miracle when a mother is conscious and hears the first cry of her child and sees him with first seconds of birth? This is where the maternal instinct comes in.
Anesthesia begins with a preoperative examination and selection of the anesthesia method. In obstetrics, the gold standard is to perform neuraxial anesthesia techniques, preventing the risk of many fatal complications. The place where the anesthetic will be injected is treated with an antiseptic. After that, the medicine is injected with a special needle into the spinal space at the level of the lumbar spine. nine0003
After the injection of an anesthetic, the woman feels numbness in her legs, they become like cotton wool, heavy.
The numbness gradually spreads up the body. The anesthesiologist checks how wide the area of anesthesia has spread, and whether the patient is ready for surgery.
Before the operation, a special curtain is installed to delimit the patient's face from the intervention area. In this case, the anesthesiologist will be next to the woman at all times. The mother-to-be hears the preparations for the operation as the OB/GYNs work as a team with the midwives and anesthesia team. nine0003
The skin incision is usually made just below the bikini line. When they begin to do the operation, you can feel pressure or tension, but there will be no feeling of pain. The anesthesiologist continuously assesses the general condition of the expectant mother during the operation, and, if necessary, corrects the main parameters of hemodynamics and respiration, and can also perform additional anesthesia or sedation of the mother. The time from the start of the operation to the removal of the baby is usually less than five minutes. Immediately after birth, the midwife and pediatrician examine the newborn. The operations team will take approximately half an hour to complete the operation. nine0003
Immediately after birth, the midwife and pediatrician examine the newborn. The operations team will take approximately half an hour to complete the operation. nine0003
When the operation is completed
After the end of the operation, the patient is transferred to the recovery room for observation in the near future and early rehabilitation for a quick recovery after the operation. It is allowed to take with you a telephone, water without gas, personal hygiene products, all other things are transferred to the midwife. The child will be in the children's department for this time, the neonatologist informs the mother about his condition. Several times a day, the child is brought in for feeding. In the awakening ward, drugs administered during anesthesia gradually cease to have their effect, and tingling sensations may appear in the legs, their sensitivity and strength are restored. After a few hours, the woman will be able to move her legs again. Six hours after the operation, you can get up and walk around the ward on your own under the supervision of medical staff. If there are no contraindications, the mother is immediately allowed to eat. nine0003
If there are no contraindications, the mother is immediately allowed to eat. nine0003
Having a baby by caesarean section is safe, and staying conscious allows the mother to control the process and recover faster in order to reunite with the baby as soon as possible and be together in the same room. The institution implements the tasks of the national project "Healthcare" in terms of tasks for the protection of motherhood and childhood. The mission of the Krasnoyarsk Regional Clinical Center for Maternal and Child Health: "Professional assistance, careful care and sincere care for every child, mother and family." nine0003
Natural birth or caesarean section?
16/03/2018 - 13:35
Expectant mothers often face a dilemma: what will be better for her and the baby - natural childbirth or caesarean section. Both methods of obstetrics have their pros and cons, their indications and contraindications.
Aleksey Sherstobitov, head of the obstetric department of the Chelyabinsk Regional Perinatal Center, obstetrician-gynecologist of the highest category, helped the Ural-press-inform agency to dispel the fears and unnecessary fears of women.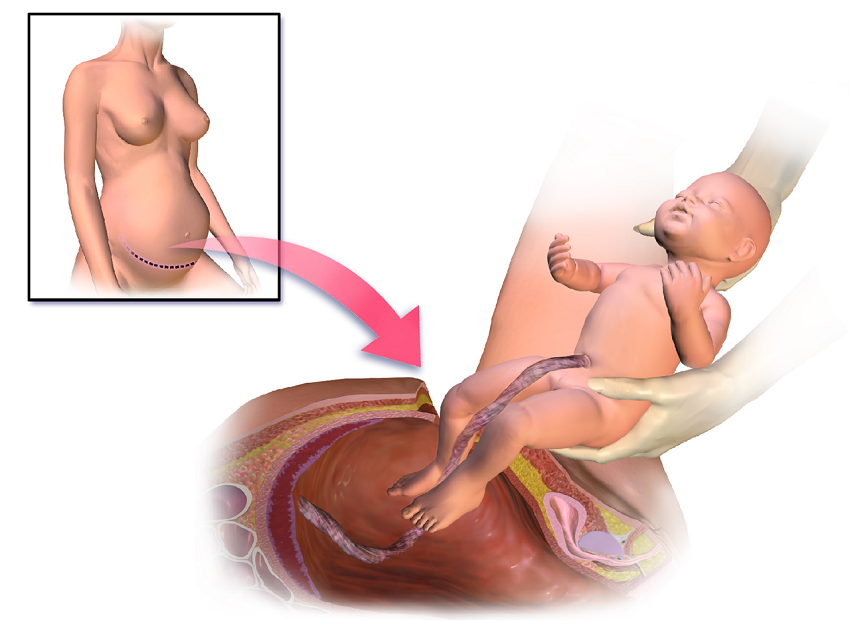 nine0003
nine0003
- Alexey Vasilyevich, in your opinion, as a professional, what choice should I make (natural birth or caesarean section), based on the benefits for mother and child?
- Until about the 1980s, the percentage of caesarean sections was about 2-4 percent of the total volume of deliveries. And we are all alive and well. And everything is fine with our grandmothers and mothers.
- What are the advantages of natural childbirth?
- In case of childbirth through natural birth canal, there is no pain syndrome in the postoperative period. The recovery process for the female body as a result of natural childbirth is much faster than after a cesarean section. There are fewer complications. Accordingly, the time of stay of a woman in labor in a hospital is reduced. The woman goes home on the third or fourth day. After caesarean section - only for 4-5 days. In addition, during natural childbirth, the baby is immediately brought to the mother's breast, which is good for the health of the newborn and for the mother's lactation. nine0003
nine0003
- When is natural childbirth contraindicated?
- For certain medical conditions in a woman (eg, somatic, eye, cardiovascular disease), vaginal delivery is more of a risk than a benefit. For some women, a caesarean section is performed according to indications that occur during childbirth (acute fetal hypoxia and others). There are also relative indications - breech or foot presentation, large fetus.
- Is the woman's age an indication for caesarean section?
- Now women are increasingly giving birth at a late reproductive age. Previously, a woman aged 33 years and older was written late. And that was an indication for a caesarean section. Now there is no such term, and women at this age also give birth through the natural birth canal. We have several women who are 44-47 years old sometimes pass through us in a week.
- How old was your oldest woman in labor?
- 51 years old (her first daughter was already 31 years old).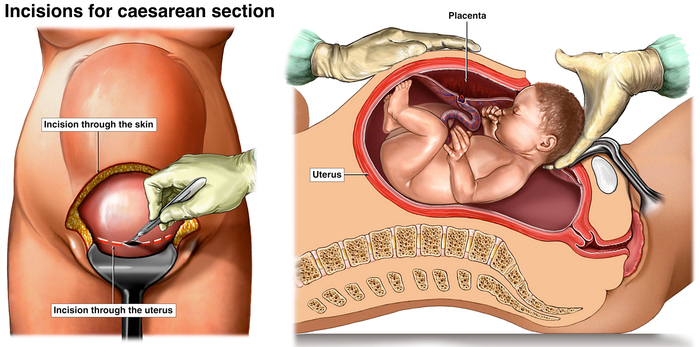 There was also a woman who had her first pregnancy at the age of 49.
There was also a woman who had her first pregnancy at the age of 49.
- Can a woman in labor be an indication for a caesarean section?
- There are several countries in the world where the indication of a woman's desire to have a caesarean section is legislated. The Russian Federation is not included in this list of countries. Therefore, we do not perform cesarean at the request of a woman without medical indications. Indications for a caesarean section are clearly regulated by the order of the Ministry of Health of the Russian Federation. They are divided into a number of groups: planned and emergency indications during pregnancy, as well as emergency during childbirth. And there is no such indication as the desire of a woman. nine0003
- Currently, the number of deliveries by caesarean section has increased dramatically. Why did this happen?
- Perinatal focus of medicine has expanded the range of indications for operative delivery. For example, earlier women with heart defects were strictly forbidden to give birth. At the moment, these defects are being corrected. For a woman, therapy is selected, and she becomes pregnant. Subject to certain rules, a favorable outcome is guaranteed. The method of delivery is chosen in each case individually, depending on the degree of compensation of the defect by the time of delivery. nine0003
For example, earlier women with heart defects were strictly forbidden to give birth. At the moment, these defects are being corrected. For a woman, therapy is selected, and she becomes pregnant. Subject to certain rules, a favorable outcome is guaranteed. The method of delivery is chosen in each case individually, depending on the degree of compensation of the defect by the time of delivery. nine0003
- Have caesarean sections become more advanced today?
- Yes. The technique of performing caesarean section operations is being improved, more modern suture material is used, when sutured, the lower uterine segment is better restored, less scar tissue is formed.
- Previously, if a woman had a caesarean section during her first birth, then only a caesarean section during her second and subsequent births ...
- Absolutely right. But for the fourth year in our perinatal center, women with a scar on the uterus give birth through the natural birth canal.
- And now, after the first cesarean, a woman, having become pregnant for the second time, can choose - to give birth through the birth canal or she will have a cesarean section?
- Yes. If a woman with a scar on the uterus wants to give birth through the birth canal, she must sign up for a planned hospitalization with us. She will need to submit the protocol of the previous operation - a caesarean section. We will see how it was performed, we will find out from the woman if there were any complications in the postoperative period. Doctors working in the ultrasound department will assess the condition of the lower uterine segment, the obstetrician - the viability of the scar. nine0003
Then the woman in labor enters the department of pathology of pregnant women, where a consultation is held with the participation of the chief physician, the head of the department, and employees of the department of the Chelyabinsk State Medical Academy. And we determine whether a woman can give birth through the natural birth canal or not.