Spontaneous abortion types
Threatened Abortion - StatPearls - NCBI Bookshelf
Continuing Education Activity
A threatened abortion is vaginal bleeding during pregnancy that does not meet diagnostic criteria for spontaneous abortion. In a threatened abortion, the cervical os remains closed. The World Health Organization (WHO) defines a threatened abortion as pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation. A threatened abortion can present during early pregnancy with lower abdominal pain, and/or vaginal bleeding. Nearly 25 percent of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50 percent of these progress to an actual abortion. The bleeding in a threatened abortion is mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. This activity examines when this condition should be considered on differential diagnosis and how to properly evaluate it. This activity highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
Outline threatened abortion.
Summarize the differences between threatened abortion and other abortion types including elective, inevitable, incomplete, complete, or missed.
Explain how to manage a patient presenting with a threatened abortion.
Describe how the facilitation of interprofessional team education and discussion can optimize the effective detection of a threatened abortion and inform the need for subsequent evaluations.
Access free multiple choice questions on this topic.
Introduction
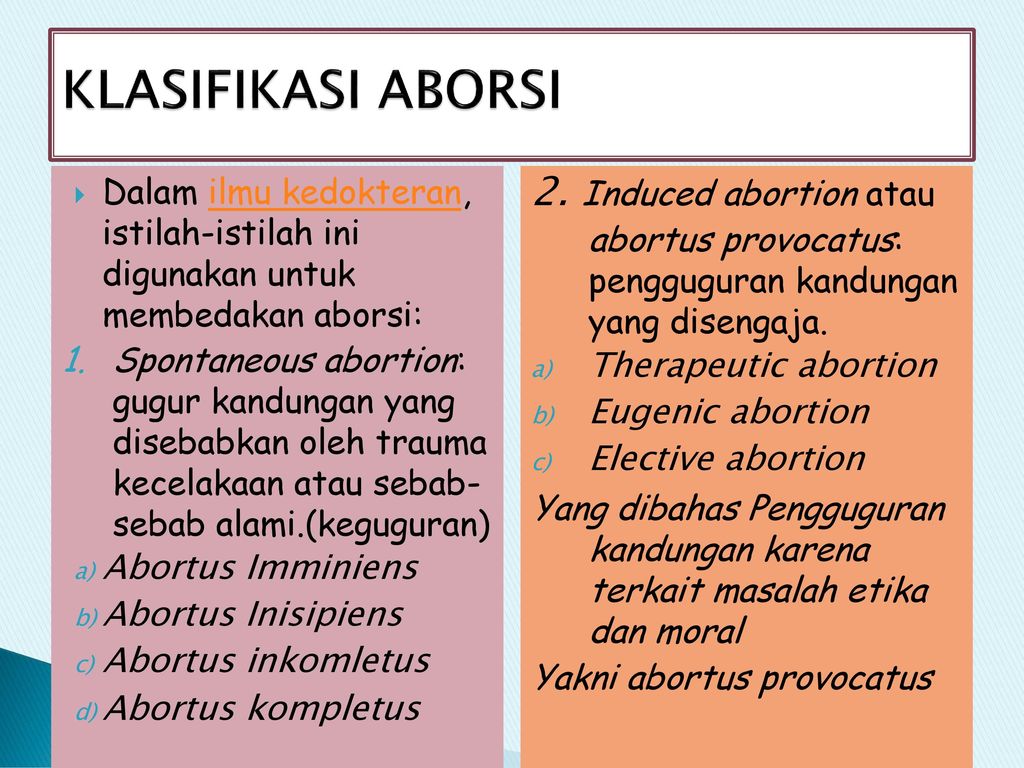
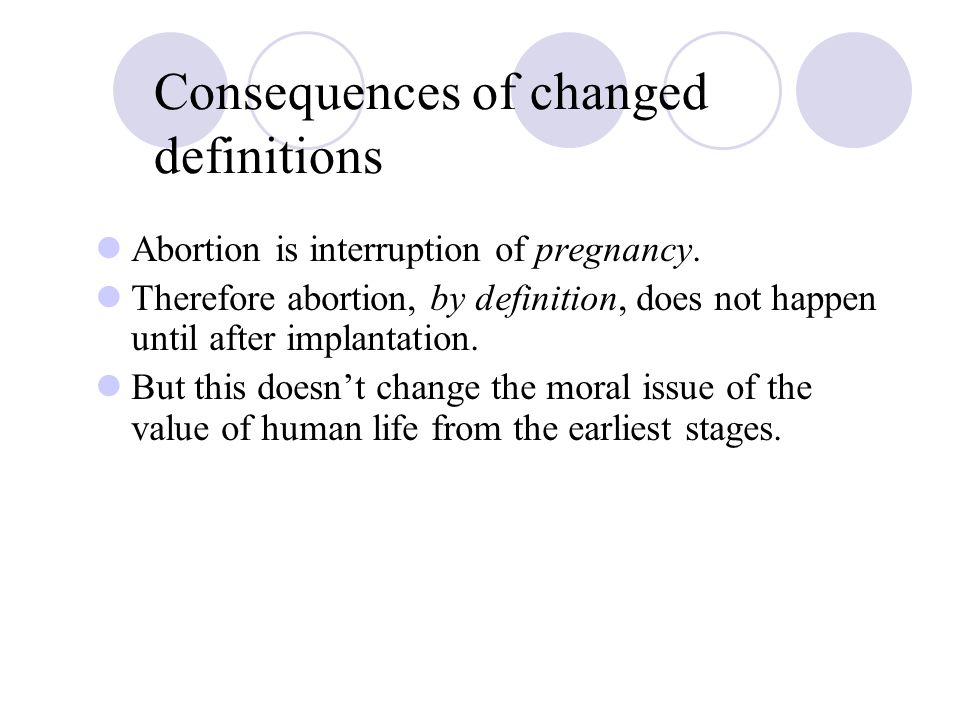
Abortion is the medical term for a pregnancy loss before 20 weeks of gestational age. The types of spontaneous abortion include threatened, inevitable, incomplete, complete, septic, and missed abortion[1].
A threatened abortion is defined as vaginal bleeding before 20 weeks gestational age in the setting of a positive urine and/or blood pregnancy test with a closed cervical os, without passage of products of conception and without evidence of a fetal or embryonic demise.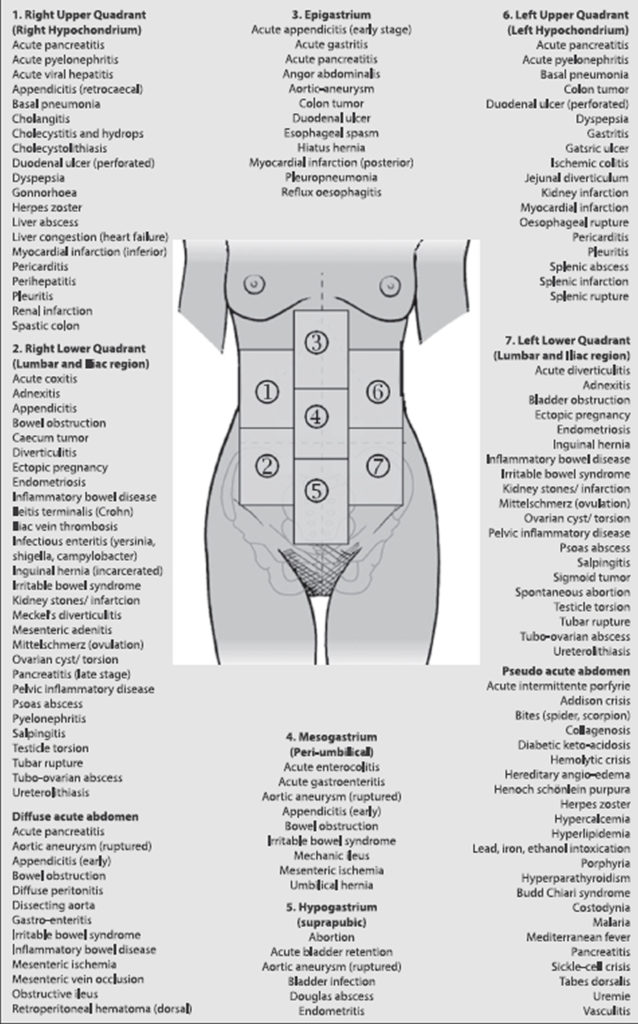 The definition of a threatened abortion by the World Health Organization (WHO) is pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation[2].
The definition of a threatened abortion by the World Health Organization (WHO) is pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation[2].
Other types of abortion should be considered if the cervical os is open, if there is determined to be an extrauterine pregnancy, if there is determined to be an intrauterine pregnancy without a fetal heartbeat, or if there is evidence of the passage of products of conception[3].
Nearly 25% of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50% of these progress to loss of the pregnancy. The bleeding during a threatened abortion is typically mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. [4][5][6][7]
Etiology
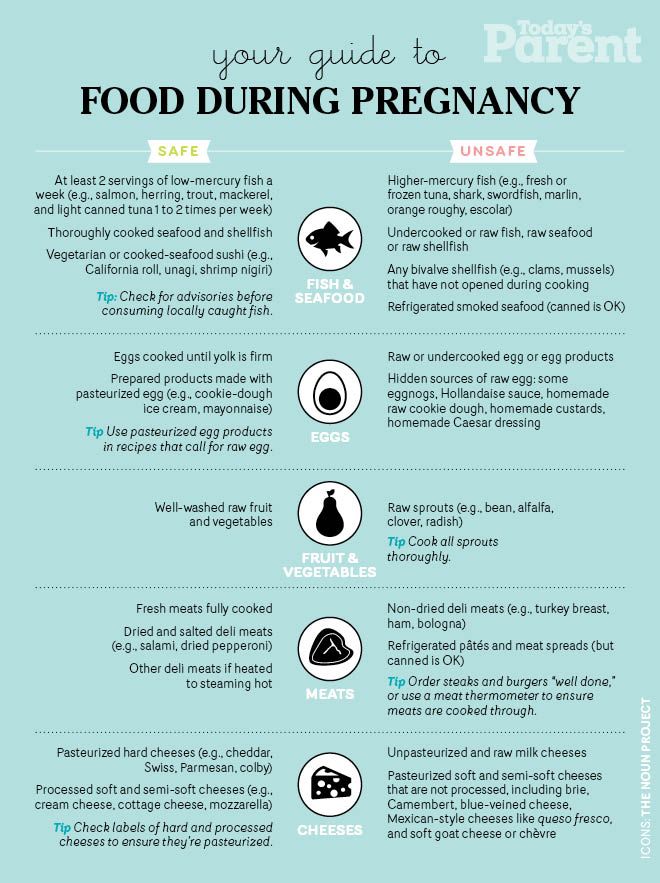
The exact etiology of a threatened or spontaneous abortion is not always known. It is widely accepted that the vast majority of spontaneous abortions cannot be prevented or modified likely because they are due to chromosomal abnormalities in at least half of all cases[8]. For pregnancy losses that are determined to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role[9]. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion[10]. When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence.
For pregnancy losses that are determined to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role[9]. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion[10]. When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence. It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
Epidemiology
Threatened abortion can occur in any pregnancy regardless of maternal age, race, comorbidities, lifestyle, or socioeconomic status[10]. If a woman has previously had bleeding in the first trimester of pregnancy, her risk of bleeding in the first trimester of subsequent pregnancies does appear to be increased. Risk factors for any type of miscarriage include advanced maternal age, advanced paternal age, prior history of pregnancy loss, TORCH infections, uncontrolled hyperglycemia, obesity, uncontrolled thyroid disease, significant stressors, use of teratogenic medications, and presence of a subchorionic hemorrhage[12].
Pathophysiology
A threatened abortion occurs when a pregnant patient at less than 20 weeks gestation presents with vaginal bleeding. The cervical os is closed on a physical exam. The patient may also experience abdominal cramping, pelvic pain, pelvic pressure, and/or back pain. Vaginal bleeding usually begins first followed by cramping abdominal pain hours to days later. Bleeding is the most predictive risk factor for pregnancy loss. More than half of threatened abortions will abort. The risk of spontaneous abortion, in a patient with threatened abortion, is less if fetal cardiac activity is present[1].
Vaginal bleeding usually begins first followed by cramping abdominal pain hours to days later. Bleeding is the most predictive risk factor for pregnancy loss. More than half of threatened abortions will abort. The risk of spontaneous abortion, in a patient with threatened abortion, is less if fetal cardiac activity is present[1].
Histopathology
It is strongly recommended that all products of conception from any type of abortion are considered for histopathological examination. For patients with repeat pregnancy loss, karyotyping should be given as an option for products of conception to rule in or rule out chromosomal abnormalities as likely cause of spontaneous abortion. This information can help patients determine the best options for moving forward if they desire future pregnancies[16].
History and Physical
A pelvic exam is mandatory to determine the type of abortion. Determining factors include the amount and site of bleeding, whether the cervix is dilated, and whether fetal tissue has passed. In a threatened abortion, the vaginal exam may reveal a closed cervical os with no tissue. There is usually no cervical motion tenderness[17]. In rare cases, the pelvic exam will reveal uterine and bilateral adnexal tenderness. It is important to note that in a threatened abortion there is no passage of tissue and the cervical os is, by definition, closed[2]. These observations differentiate the condition from an inevitable or incomplete abortion. Women with a threatened abortion usually have stable vital signs, but if hypovolemia is present, one should suspect bleeding or sepsis. The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
In a threatened abortion, the vaginal exam may reveal a closed cervical os with no tissue. There is usually no cervical motion tenderness[17]. In rare cases, the pelvic exam will reveal uterine and bilateral adnexal tenderness. It is important to note that in a threatened abortion there is no passage of tissue and the cervical os is, by definition, closed[2]. These observations differentiate the condition from an inevitable or incomplete abortion. Women with a threatened abortion usually have stable vital signs, but if hypovolemia is present, one should suspect bleeding or sepsis. The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
Evaluation
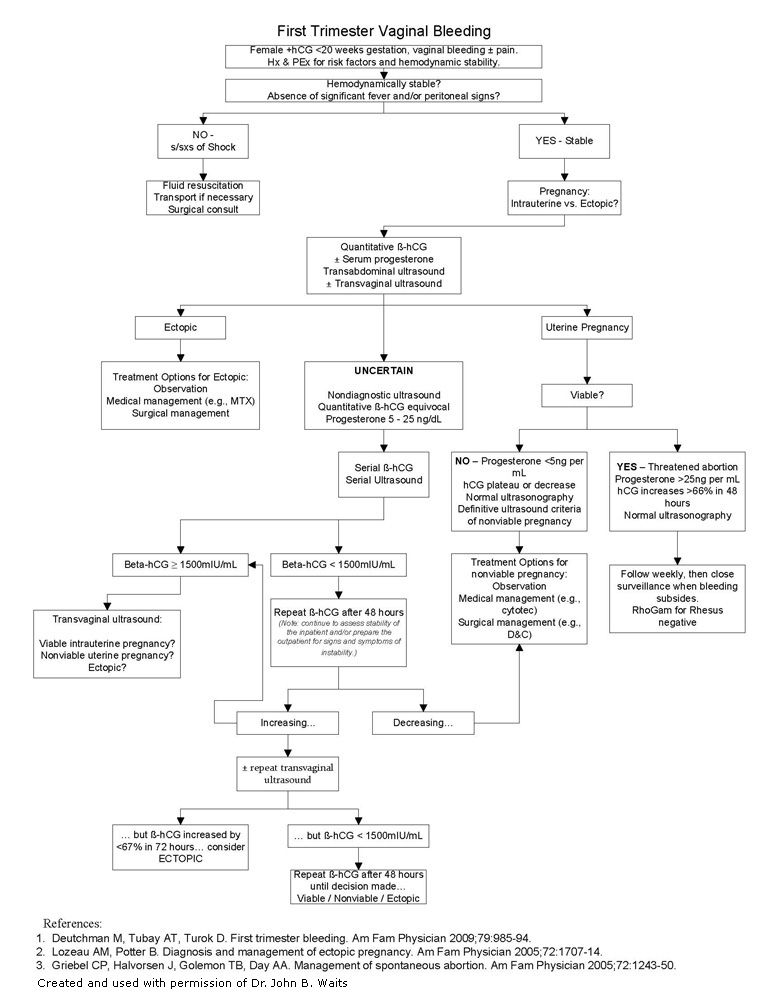
The diagnosis is made by history, physical exam, measurement of beta-human chorionic gonadotropin (beta-hCG), and an ultrasound[10].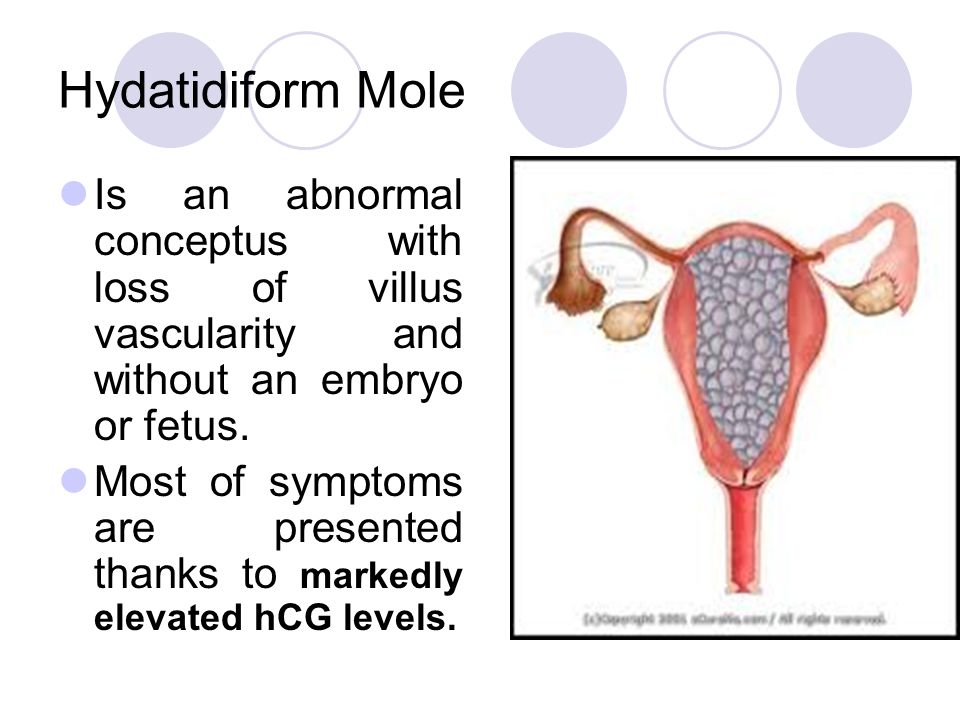
A thorough history should be obtained including pregnancy history, medical history, and history of present illness. History of present illness should include when and how symptoms/bleeding began, modifying factors, any treatments trialed up to the point of evaluation, and helping the patient to describe and quantify the bleeding[20][5].
Transvaginal ultrasound may be used to locate the pregnancy and determine if the fetus is viable. The ultrasound can also help rule out ectopic pregnancy and to evaluate for retained products of conception. A yolk sac is typically seen at 36 days, and a heartbeat is seen on ultrasound at approximately 45 days after the last menstruation[21].
A beta-hCG level of 1500 lU/mL to 2000 lU/mL is associated with a gestational sac on ultrasound. Beta-hCG doubles in 48 hours in 85% of intrauterine pregnancies. Beta-hCG is usually detectable the first nine to 11 days following ovulation and reaches 200 IU/mL at the expected time of menses[22].
Rh factor will also determine if Rhogam should be administered to prevent hemolytic disease of the newborn in this pregnancy and subsequent pregnancies[23].
Hemoglobin and hematocrit levels help monitor the degree of blood loss.
A urinalysis can also be obtained. Urinary tract infection (UTI) has been associated with signs and symptoms of threatened abortion[24].
During the pelvic exam, suction or cotton swabs may be needed to remove blood and products of conception to allow for better visualization of the cervix. Ringed forceps can also be used to remove tissue that may be protruding from the cervical os. All tissue must be examined to determine if it is a clot or products of conception. Evidence of products of conception protruding from the cervix or within the vagina changes the diagnosis from a threatened abortion to a complete or incomplete abortion. Evaluation of the amount of bleeding/blood loss should be performed through a thorough history, as well as during the pelvic examination[25].
Treatment / Management
Alloimmunization prevention by the administration of Rh(D) immunoglobulin should be considered for patients who have vaginal bleeding in the setting of pregnancy in a patient who is Rh-[26].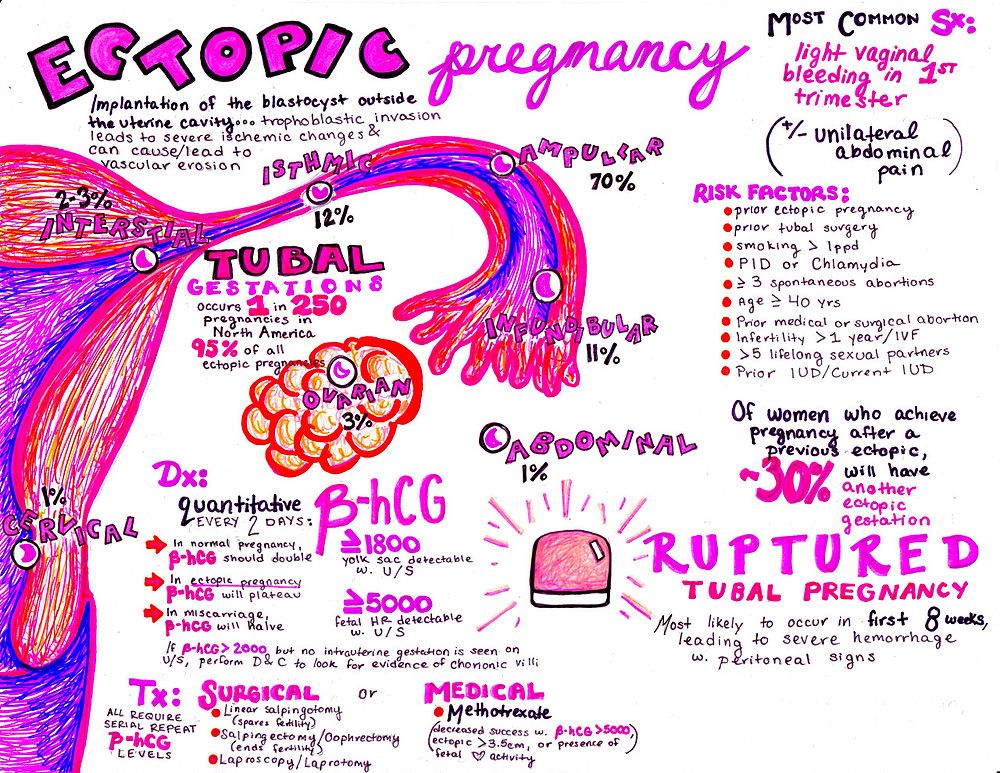 It has been determined that a 50 mcg dose of immunoglobulin is effective at alloimmunization prevention up to and through the 12th week of gestation, however, it is considered acceptable to give the standard 300 mcg dose due to availability or provider preference[23].
It has been determined that a 50 mcg dose of immunoglobulin is effective at alloimmunization prevention up to and through the 12th week of gestation, however, it is considered acceptable to give the standard 300 mcg dose due to availability or provider preference[23].
Patients with a threatened abortion should be managed expectantly without any medical or surgical interventions. However, patients should be given strict return precautions concerning excessive vaginal bleeding, abdominal pain, or fever and patients should be educated on the importance of follow-up. Analgesia can be provided to help relieve discomfort from cramping. NSAIDs should be avoided in the setting of a threatened abortion, as the pregnancy may continue to progress to viability[27]. Follow-up is recommended with serial transvaginal ultrasounds until a viable intrauterine pregnancy is confirmed or until progression to an inevitable, incomplete, or complete abortion occurs. Clinicians can consider serial quantitative beta hCG testing as recommended for a pregnancy of unknown origin to continue to monitor for the viability of the pregnancy, especially in the setting where an intrauterine pregnancy with cardiac activity has not been confirmed by ultrasound[28]. In these cases, it is possible that the pregnancy has not reached the gestational age by which cardiac activity would be expected on ultrasound or it is possible that the pregnancy will not be viable[22]. The patient should be counseled about the possibility of spontaneous abortion of the pregnancy, as well as the possibility that the pregnancy may continue to progress towards viability. Several trials have shown that progesterone supplementation does not improve outcomes for patients with threatened abortion and progesterone is not currently recommended as treatment or prevention for patients with threatened abortion.[29] Bedrest and other activity restrictions have not been found to be efficacious in the prevention of a threatened abortion progressing to spontaneous abortion and have been shown to increase the risk of other complications including deep vein thrombosis and/or pulmonary embolism and therefore should not be recommended[30]. Some providers do prefer to advise patients to avoid strenuous activities and to maintain pelvic rest at least until the cessation of vaginal bleeding.
In these cases, it is possible that the pregnancy has not reached the gestational age by which cardiac activity would be expected on ultrasound or it is possible that the pregnancy will not be viable[22]. The patient should be counseled about the possibility of spontaneous abortion of the pregnancy, as well as the possibility that the pregnancy may continue to progress towards viability. Several trials have shown that progesterone supplementation does not improve outcomes for patients with threatened abortion and progesterone is not currently recommended as treatment or prevention for patients with threatened abortion.[29] Bedrest and other activity restrictions have not been found to be efficacious in the prevention of a threatened abortion progressing to spontaneous abortion and have been shown to increase the risk of other complications including deep vein thrombosis and/or pulmonary embolism and therefore should not be recommended[30]. Some providers do prefer to advise patients to avoid strenuous activities and to maintain pelvic rest at least until the cessation of vaginal bleeding. Clinicians should recommend that patients start or continue to take prenatal vitamins with folic acid supplementation. [31][32][33][34]
Clinicians should recommend that patients start or continue to take prenatal vitamins with folic acid supplementation. [31][32][33][34]
Differential Diagnosis
Clinicians should consider several differential diagnoses when encountering vaginal bleeding in the setting of pregnancy. Vulvar, vaginal, cervical trauma should be ruled out during a pelvic examination. Cervical friability can lead to vaginal bleeding which can be caused by cervicitis from an infection or due to premalignant or malignant changes on the cervix. Clinical judgment should determine whether or not the patient should undergo a Pap smear and/or cultures for infection at the time of examination. Other types of abortion should be considered including elective, inevitable, incomplete, complete, septic, and missed abortion[25].
Prognosis
Studies have shown that about 20% of women experience vaginal bleeding before 20 weeks of pregnancy. Furthermore, about 50% of those patients who experience a threatened abortion progress to a pregnancy loss. Studies have shown that there may be an increased risk of adverse outcomes later in pregnancy if there was vaginal bleeding during the first trimester of that pregnancy. For example, there may be a greater risk of placenta previa, placental abruption, necessitation for manual removal of the placenta after delivery, cesarean delivery, preterm premature ruptured membranes, preterm birth, low-birthweight infant, fetal-growth restriction, and fetal or neonatal death. [2]
Studies have shown that there may be an increased risk of adverse outcomes later in pregnancy if there was vaginal bleeding during the first trimester of that pregnancy. For example, there may be a greater risk of placenta previa, placental abruption, necessitation for manual removal of the placenta after delivery, cesarean delivery, preterm premature ruptured membranes, preterm birth, low-birthweight infant, fetal-growth restriction, and fetal or neonatal death. [2]
Complications
Pregnancy loss (progression to inevitable, incomplete, complete, missed abortion)
Heavy bleeding
Retained products of conception
Endometritis
Septic abortion
Complications later in pregnancy as discussed in "Prognosis" [20]
Consultations
Patients with recurrent pregnancy loss or recurrent bleeding during pregnancy should be offered evaluation by a reproductive endocrinology and infertility specialist and/or by a maternal-fetal medicine specialist.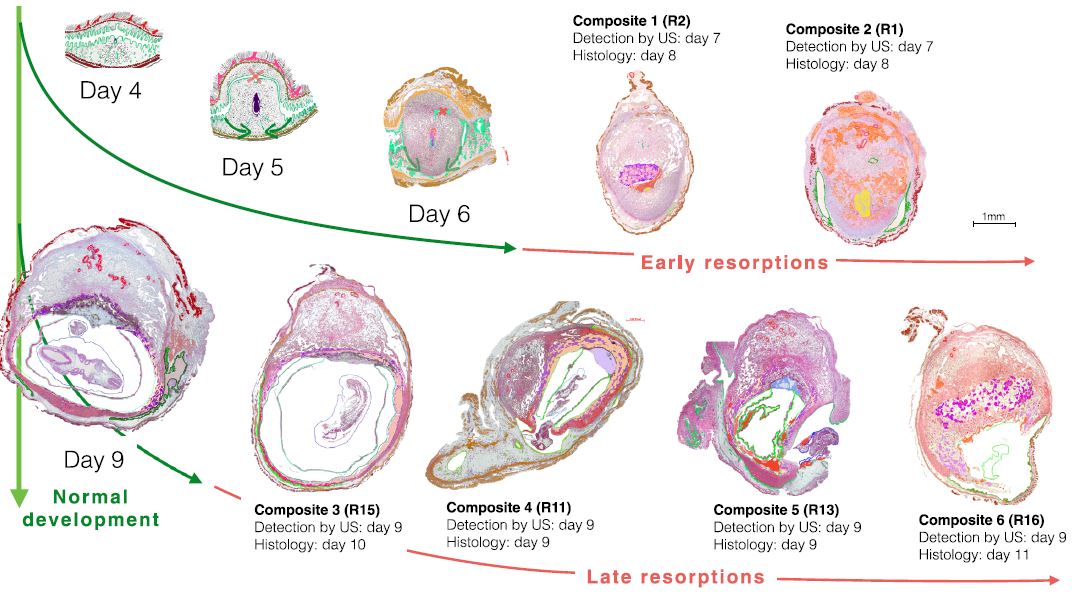 If a patient is determined to have a coagulopathy, a hematology consult should be considered[10].
If a patient is determined to have a coagulopathy, a hematology consult should be considered[10].
Deterrence and Patient Education
Patient education should be provided as both verbal and written explanations and instructions. It should be explained to the patient that it is possible her pregnancy will continue and it is also possible that she will undergo a miscarriage. The patient needs to understand that the vast majority of miscarriages are not preventable and that she is not at fault for the loss of the pregnancy if a loss does occur[35]. Providers should explain to the patient that mild to moderate bleeding and cramping can be expected, but uncontrolled pain or heavy bleeding should be evaluated by an obstetric care provider or in the emergency department. Many providers explain that saturating more than 1-2 pads per hour for 2 hours is considered to be heavy bleeding and should be promptly evaluated[36]. Patients can be instructed to take acetaminophen as directed for pain relief. Patients should avoid ibuprofen for pain control during a threatened abortion as it is contraindicated in pregnancy and the patient's pregnancy may progress to viability. Patients who undergo threatened abortion should be evaluated for mood disorders including depression and anxiety. Especially if a threatened abortion proceeds to pregnancy loss, the patient should be allowed to grieve as appropriate for each individual and should be offered grief counseling[37].
Patients should avoid ibuprofen for pain control during a threatened abortion as it is contraindicated in pregnancy and the patient's pregnancy may progress to viability. Patients who undergo threatened abortion should be evaluated for mood disorders including depression and anxiety. Especially if a threatened abortion proceeds to pregnancy loss, the patient should be allowed to grieve as appropriate for each individual and should be offered grief counseling[37].
Pearls and Other Issues
Most patients with a threatened abortion can be observed from home with close follow-up. Repeat ultrasounds and beta-hCG levels will help to determine progression to a viable pregnancy or to an inevitable, complete, incomplete, or missed abortion. Patients with increased vaginal bleeding require evaluation for hemorrhagic anemia and may be candidates for a blood transfusion or pregnancy evacuation[38].
Enhancing Healthcare Team Outcomes
The diagnosis and management of a threatened abortion involve an interprofessional team that can include an emergency department physician, obstetrician, radiologist, midlevel providers, and nursing staff. For patients to be safely monitored expectantly, good communication between clinicians and the patient is key. All members of the care team need to be on the same page regarding the possibility of pregnancy loss and the importance of return precautions[39].
For patients to be safely monitored expectantly, good communication between clinicians and the patient is key. All members of the care team need to be on the same page regarding the possibility of pregnancy loss and the importance of return precautions[39].
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Alves C, Rapp A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 18, 2022. Spontaneous Abortion. [PubMed: 32809356]
- 2.
Redinger A, Nguyen H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 27, 2022. Incomplete Abortions. [PubMed: 32644497]
- 3.
de Codt M, Balza C, Jadoul P, Forget P, Squifflet JL, Bernard P, Luyckx M. Hysteroscopic Resection for Missed Abortion: Feasibility, Operative Technique and Potential Benefit Compared to Curettage. Front Surg. 2020;7:64.
 [PMC free article: PMC7505996] [PubMed: 33102514]
[PMC free article: PMC7505996] [PubMed: 33102514]- 4.
Karataşlı V, Kanmaz AG, İnan AH, Budak A, Beyan E. Maternal and neonatal outcomes of adolescent pregnancy. J Gynecol Obstet Hum Reprod. 2019 May;48(5):347-350. [PubMed: 30794955]
- 5.
Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019 Feb 01;99(3):166-174. [PubMed: 30702252]
- 6.
Goodarzi P, Falahzadeh K, Aghayan H, Payab M, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Adibi H, Gilany K, Arjmand B. Therapeutic abortion and ectopic pregnancy: alternative sources for fetal stem cell research and therapy in Iran as an Islamic country. Cell Tissue Bank. 2019 Mar;20(1):11-24. [PubMed: 30535614]
- 7.
Boiko VI, Nikitina IM, Babar TV, Boiko AV. The problem of miscarriage in multiple pregnancy. Wiad Lek. 2018;71(7):1195-1199. [PubMed: 30448784]
- 8.
Yang J, Chen M, Ye X, Chen F, Li Y, Li N, Wu W, Sun J.
 A cross-sectional survey of pregnant women's knowledge of chromosomal aneuploidy and microdeletion and microduplication syndromes. Eur J Obstet Gynecol Reprod Biol. 2021 Jan;256:82-90. [PubMed: 33176246]
A cross-sectional survey of pregnant women's knowledge of chromosomal aneuploidy and microdeletion and microduplication syndromes. Eur J Obstet Gynecol Reprod Biol. 2021 Jan;256:82-90. [PubMed: 33176246]- 9.
Weghofer A, Barad DH, Darmon SK, Kushnir VA, Albertini DF, Gleicher N. Euploid miscarriage is associated with elevated serum C-reactive protein levels in infertile women: a pilot study. Arch Gynecol Obstet. 2020 Mar;301(3):831-836. [PMC free article: PMC7060953] [PubMed: 32107607]
- 10.
Devall AJ, Coomarasamy A. Sporadic pregnancy loss and recurrent miscarriage. Best Pract Res Clin Obstet Gynaecol. 2020 Nov;69:30-39. [PubMed: 32978069]
- 11.
Wierzejska R, Wojda B. Folic acid supplementation in pregnancy and prevention of fetal neural tube defects. Przegl Epidemiol. 2020;74(2):362-369. [PubMed: 33115226]
- 12.
du Fossé NA, van der Hoorn MP, van Lith JMM, le Cessie S, Lashley EELO. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: a systematic review and meta-analysis.
 Hum Reprod Update. 2020 Sep 01;26(5):650-669. [PMC free article: PMC7456349] [PubMed: 32358607]
Hum Reprod Update. 2020 Sep 01;26(5):650-669. [PMC free article: PMC7456349] [PubMed: 32358607]- 13.
Carp HJA. Progestogens and pregnancy loss. Climacteric. 2018 Aug;21(4):380-384. [PubMed: 29565684]
- 14.
Wahabi HA, Fayed AA, Esmaeil SA, Bahkali KH. Progestogen for treating threatened miscarriage. Cochrane Database Syst Rev. 2018 Aug 06;8(8):CD005943. [PMC free article: PMC6513446] [PubMed: 30081430]
- 15.
Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar N. Prediction of miscarriage in women with viable intrauterine pregnancy-A systematic review and diagnostic accuracy meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018 Jan;220:122-131. [PubMed: 29207325]
- 16.
Xu J, Chen M, Liu QY, Hu SQ, Li LR, Li J, Ma RM. Detecting trisomy in products of conception from first-trimester spontaneous miscarriages by next-generation sequencing (NGS). Medicine (Baltimore). 2020 Jan;99(5):e18731. [PMC free article: PMC7004681] [PubMed: 32000376]
- 17.
Curry A, Williams T, Penny ML. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Fam Physician. 2019 Sep 15;100(6):357-364. [PubMed: 31524362]
- 18.
Stewart KT, Lee JS, Pan K, Albert AY, Fisher S. Outcome of using vaginal misoprostol for treatment of retained products of conception after first trimester miscarriage: a retrospective cohort study. Eur J Contracept Reprod Health Care. 2020 Dec;25(6):474-479. [PubMed: 32869658]
- 19.
Long Y, Zhu H, Hu Y, Shen L, Fu J, Huang W. Interventions for non-tubal ectopic pregnancy. Cochrane Database Syst Rev. 2020 Jul 01;7(7):CD011174. [PMC free article: PMC7389314] [PubMed: 32609376]
- 20.
Storey A, White K, Treder K, Woodhams E, Bell S, Cannon R. First-Trimester Abortion Complications: Simulation Cases for OB/GYN Residents in Sepsis and Hemorrhage. MedEdPORTAL. 2020 Oct 16;16:10995. [PMC free article: PMC7566226] [PubMed: 33094159]
- 21.
Mj G, K B, R M, G D.
 Abdominal ectopic pregnancy with implantation on the rectum. Ulster Med J. 2020 Sep;89(2):101-102. [PMC free article: PMC7576386] [PubMed: 33093695]
Abdominal ectopic pregnancy with implantation on the rectum. Ulster Med J. 2020 Sep;89(2):101-102. [PMC free article: PMC7576386] [PubMed: 33093695]- 22.
Pereira PP, Cabar FR, Gomez ÚT, Francisco RPV. Pregnancy of unknown location. Clinics (Sao Paulo). 2019;74:e1111. [PMC free article: PMC6784610] [PubMed: 31618321]
- 23.
Yoham AL, Casadesus D. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 23, 2022. Rho(D) Immune Globulin. [PubMed: 32491807]
- 24.
Gágyor I, Strube-Plaschke S, Rentzsch K, Himmel W. Management of urinary tract infections: what do doctors recommend and patients do? An observational study in German primary care. BMC Infect Dis. 2020 Nov 09;20(1):813. [PMC free article: PMC7650164] [PubMed: 33167875]
- 25.
Milman T, Walker M, Thomas J. Pregnancy of unknown location. CMAJ. 2020 Sep 28;192(39):E1132. [PMC free article: PMC7532014] [PubMed: 32989026]
- 26.
Mayekar RV, Paradkar GV, Bhosale AA, Sachan R, Beeram S, Anand AR, Mundle SR, Trivedi Y, Md R, Patole KP, Sambarey PW, Daftary GV, John J, Divekar GH.
 Recombinant anti-D for prevention of maternal-foetal Rh(D) alloimmunization: a randomized multi-centre clinical trial. Obstet Gynecol Sci. 2020 May;63(3):315-322. [PMC free article: PMC7231934] [PubMed: 32489976]
Recombinant anti-D for prevention of maternal-foetal Rh(D) alloimmunization: a randomized multi-centre clinical trial. Obstet Gynecol Sci. 2020 May;63(3):315-322. [PMC free article: PMC7231934] [PubMed: 32489976]- 27.
Zafeiri A, Mitchell RT, Hay DC, Fowler PA. Over-the-counter analgesics during pregnancy: a comprehensive review of global prevalence and offspring safety. Hum Reprod Update. 2021 Jan 04;27(1):67-95. [PubMed: 33118024]
- 28.
Grenache DG. Current Practices When Reporting Quantitative Human Chorionic Gonadotropin Test Results. J Appl Lab Med. 2020 Sep 01;5(5):850-857. [PubMed: 32761058]
- 29.
Ali S, Majid S, Niamat Ali M, Taing S, El-Serehy HA, Al-Misned FA. Evaluation of etiology and pregnancy outcome in recurrent miscarriage patients. Saudi J Biol Sci. 2020 Oct;27(10):2809-2817. [PMC free article: PMC7499272] [PubMed: 32994741]
- 30.
Walsh CA. Maternal activity restriction to reduce preterm birth: Time to put this fallacy to bed.
 Aust N Z J Obstet Gynaecol. 2020 Oct;60(5):813-815. [PubMed: 32691407]
Aust N Z J Obstet Gynaecol. 2020 Oct;60(5):813-815. [PubMed: 32691407]- 31.
Morin L, Cargill YM, Glanc P. Ultrasound Evaluation of First Trimester Complications of Pregnancy. J Obstet Gynaecol Can. 2016 Oct;38(10):982-988. [PubMed: 27720100]
- 32.
Huchon C, Deffieux X, Beucher G, Capmas P, Carcopino X, Costedoat-Chalumeau N, Delabaere A, Gallot V, Iraola E, Lavoue V, Legendre G, Lejeune-Saada V, Leveque J, Nedellec S, Nizard J, Quibel T, Subtil D, Vialard F, Lemery D., Collège National des Gynécologues Obstétriciens Français. Pregnancy loss: French clinical practice guidelines. Eur J Obstet Gynecol Reprod Biol. 2016 Jun;201:18-26. [PubMed: 27039249]
- 33.
Mellerup N, Sørensen BL, Kuriigamba GK, Rudnicki M. Management of abortion complications at a rural hospital in Uganda: a quality assessment by a partially completed criterion-based audit. BMC Womens Health. 2015 Sep 20;15:76. [PMC free article: PMC4576397] [PubMed: 26388296]
- 34.
Schindler AE, Carp H, Druckmann R, Genazzani AR, Huber J, Pasqualini J, Schweppe KW, Szekeres-Bartho J. European Progestin Club Guidelines for prevention and treatment of threatened or recurrent (habitual) miscarriage with progestogens. Gynecol Endocrinol. 2015 Jun;31(6):447-9. [PubMed: 25976550]
- 35.
Diamanti A, Papadakis S, Schoretsaniti S, Rovina N, Vivilaki V, Gratziou C, Katsaounou PA. Smoking cessation in pregnancy: An update for maternity care practitioners. Tob Induc Dis. 2019;17:57. [PMC free article: PMC6770622] [PubMed: 31582946]
- 36.
Shamsi S, Mirza TT, Shejuti TR, Nigar K, Nahar S, Begum S, Sharmin T, Panna LK, Islam N, Jahan T. An Overview of Unsafe Abortion: Patterns and Outcomes in a Tertiary Level Hospital. Mymensingh Med J. 2020 Jul;29(3):523-529. [PubMed: 32844789]
- 37.
Smith C, Hashmi SS, Czerwinski J, Wagner VF, Promecene P, Milentijevic I, Ramdaney A. The impact of genetic counseling on women's grief and coping following termination of pregnancy for fetal anomaly.
 J Genet Couns. 2021 Apr;30(2):522-532. [PubMed: 33103308]
J Genet Couns. 2021 Apr;30(2):522-532. [PubMed: 33103308]- 38.
Bondick CP, M Das J, Fertel H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 3, 2022. Subchorionic Hemorrhage. [PubMed: 32644443]
- 39.
Ogunyemi D, Haltigin C, Vallie S, Ferrari TM. Evolution of an obstetrics and gynecology interprofessional simulation-based education session for medical and nursing students. Medicine (Baltimore). 2020 Oct 23;99(43):e22562. [PMC free article: PMC7581067] [PubMed: 33120744]
Spontaneous Abortion - StatPearls - NCBI Bookshelf
Continuing Education Activity
Spontaneous abortion is the loss of pregnancy naturally before twenty weeks of gestation. There are several different types of spontaneous abortion. Determining the type is essential to implementing the most appropriate management. This activity describes the evaluation and management of spontaneous abortion and highlights the role of the interprofessional team in evaluating and improving care for patients with this condition.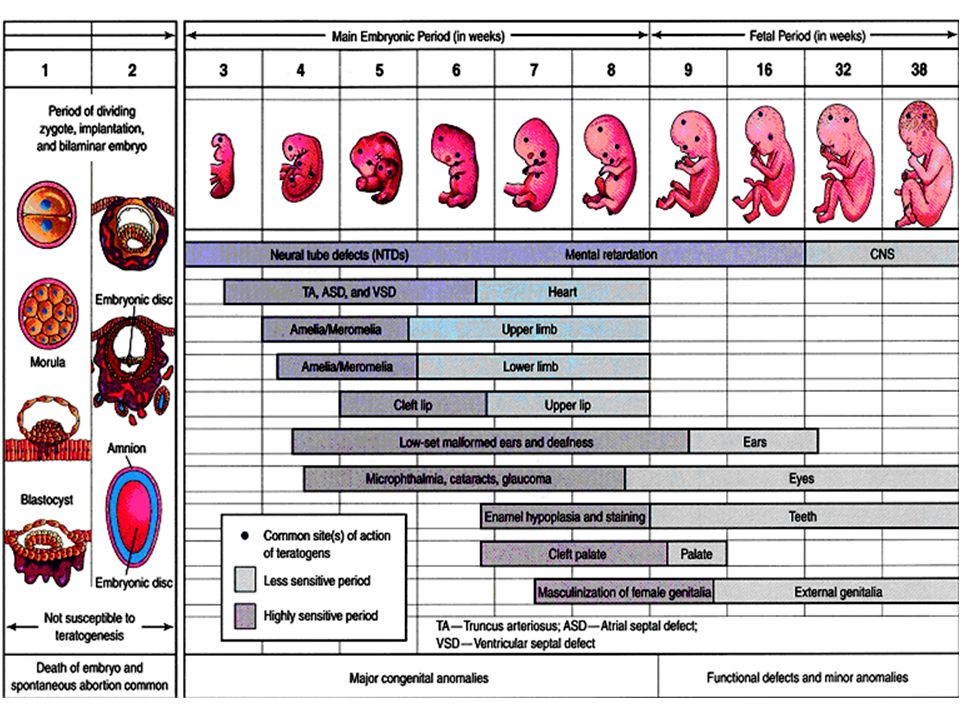
Objectives:
Describe the physical exam findings typically found in the various types of spontaneous abortion.
Explain the essential steps to diagnosing the type of spontaneous abortion a patient is experiencing.
Outline the most appropriate management options based on the type of spontaneous abortion.
Summarize the importance of collaboration and communication among the healthcare team for improving outcomes in patients affected by spontaneous abortion.
Access free multiple choice questions on this topic.
Introduction
Spontaneous abortion is the loss of pregnancy naturally before twenty weeks of gestation. Colloquially, spontaneous abortion is referred to as a ‘miscarriage’ to avoid association with induced abortion.[1] Early pregnancy loss refers only to spontaneous abortion in the first trimester. However, the first trimester is when most spontaneous abortions occur. [1][2] Therefore, in this article, these three terms will be used interchangeably.
[1][2] Therefore, in this article, these three terms will be used interchangeably.
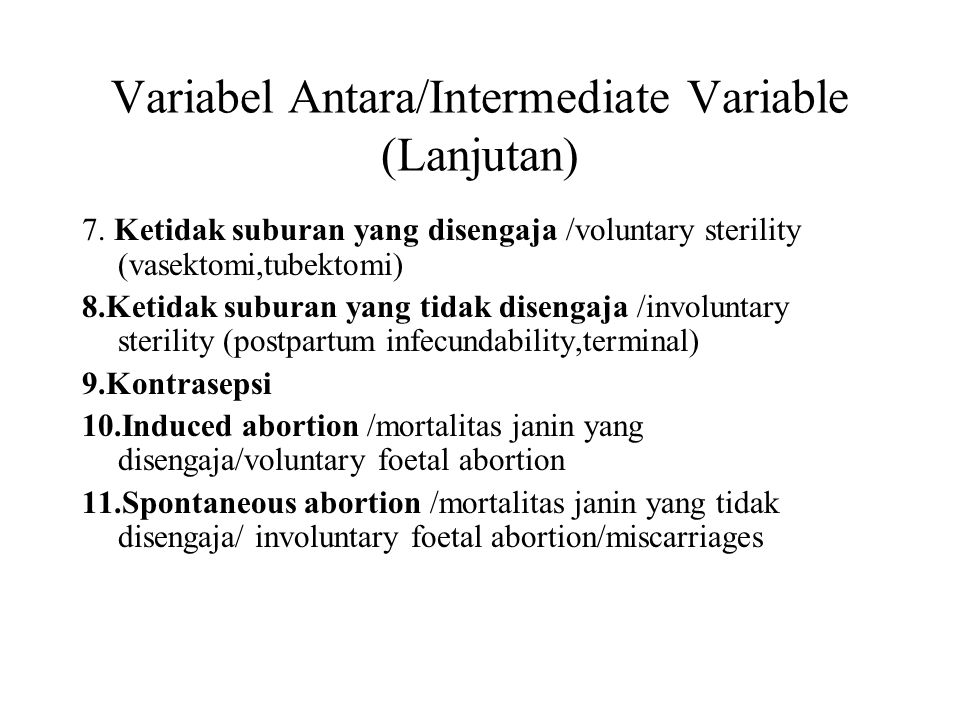
Early pregnancy loss takes many different forms. In missed abortion, there is asymptomatic or ‘missed’ death of the embryo or fetus without sufficient uterine contractions to push out the products of conception.[3] In contrast, threatened abortion is characterized by symptomatic, ‘threatened’ expulsion of the products of conception, yet the cervical os remains closed, and the embryo or fetus remains viable.[4] Inevitable abortion is distinguished from threatened abortion by the presence of an open cervical os, indicating the ‘inevitable’ passage of the conception products.[5] In incomplete abortion, there is an ‘incomplete’ passage of the products of conception through the cervical os.[6]
Complete abortion is defined as a ‘complete’ passage of all conception products.[5] Recurrent abortion is defined as three or more consecutive pregnancy losses.[1][5] Septic abortion can occur when retained products of conception become infected, which usually occurs in the setting of non-sterile induced abortion.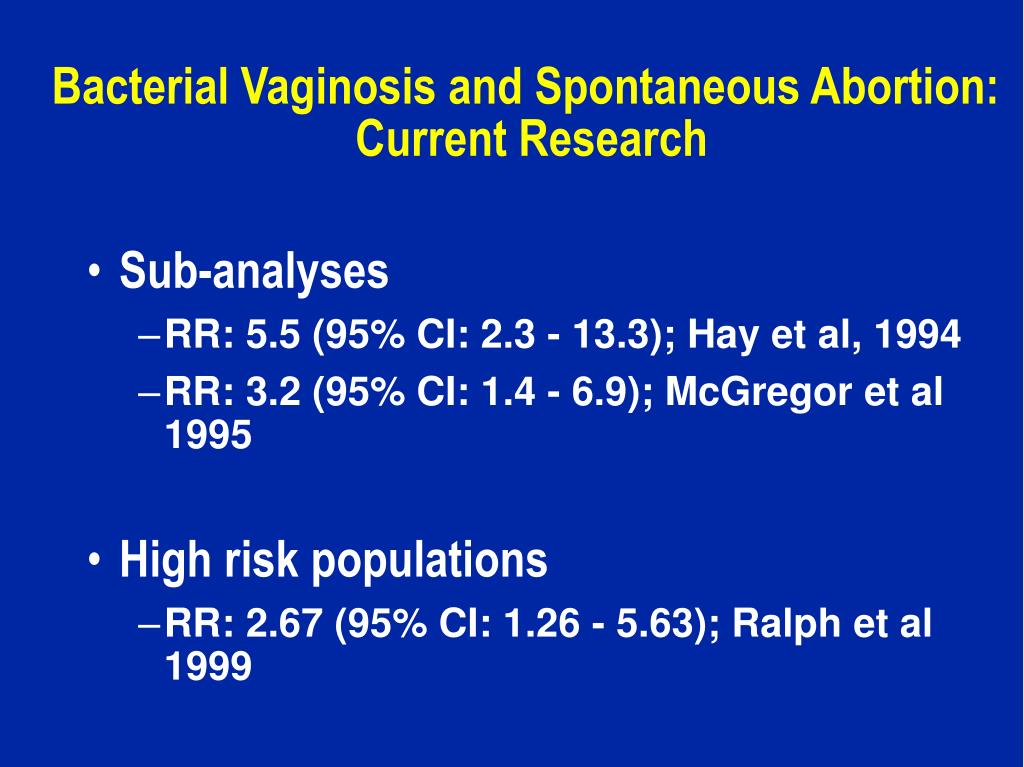 [7]
[7]
Etiology
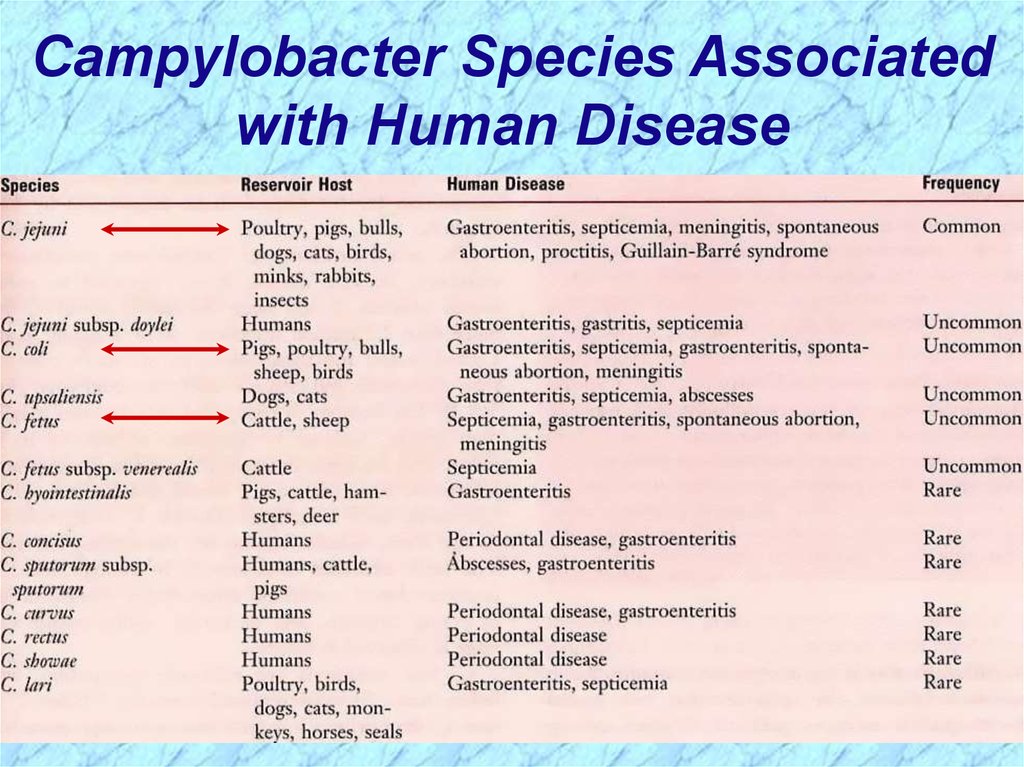
In 50% of cases, early pregnancy loss is believed to be due to fetal chromosomal abnormalities. Advanced maternal age and previous early pregnancy loss are the most common risk factors.[2] For example, the incidence of early pregnancy loss in women 20-30 years of age is only 9 to 17%, while the incidence at 45 years of maternal age is 80%.[8] Other risk factors include alcohol consumption, smoking, and cocaine use.
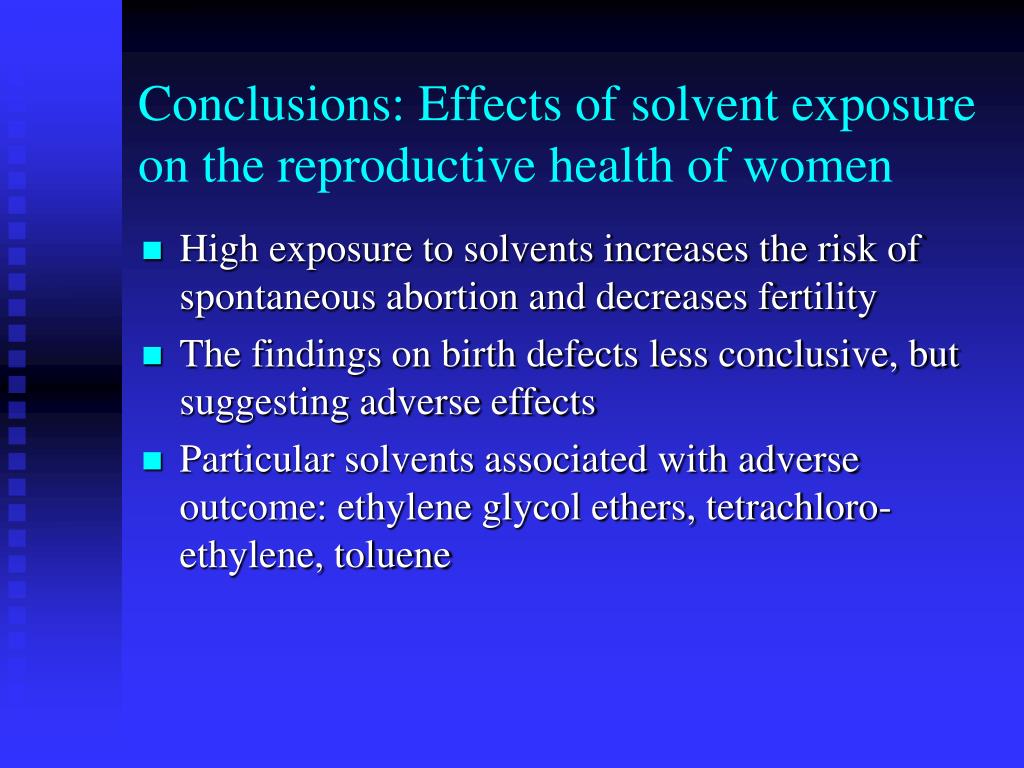
Several chronic diseases can precipitate spontaneous abortion, including diabetes, celiac disease, and autoimmune conditions, particularly anti-phospholipid antibody syndrome. Rapid conception after delivery and infections, such as cervicitis, vaginitis, HIV infection, syphilis, and malaria, are also common risk factors. Another important risk factor is exposure to environmental contaminants, including arsenic, lead, and organic solvents. Finally, structural uterine abnormalities, such as congenital anomalies, leiomyoma, and intrauterine adhesions, have been shown to increase the risk of spontaneous abortion.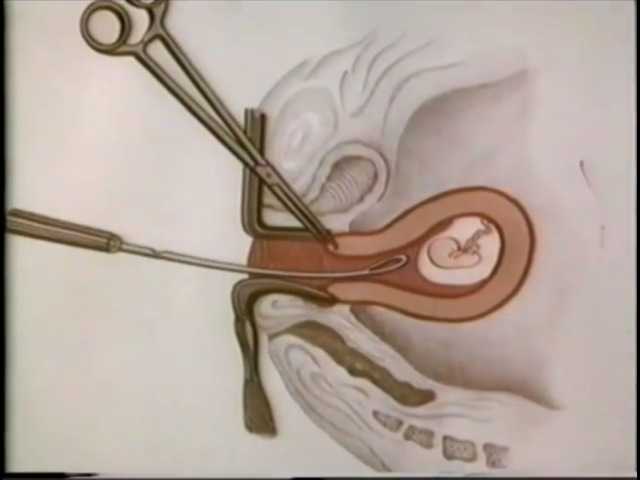 [1]
[1]
Epidemiology
Vaginal bleeding before twenty weeks of gestation occurs in up to 20% of pregnancies, and 50% of these cases will have a spontaneous abortion.[9] Overall, 10-20% of clinically recognized pregnancies will end in early pregnancy loss.[2][10] However, these statistics likely underestimate the true incidence of spontaneous abortion, as many miscarriages occur before a mother realizes she is pregnant and is simply mistaken as heavy, late menses. As a result, the true incidence of spontaneous abortion may be closer to 30%.[10]
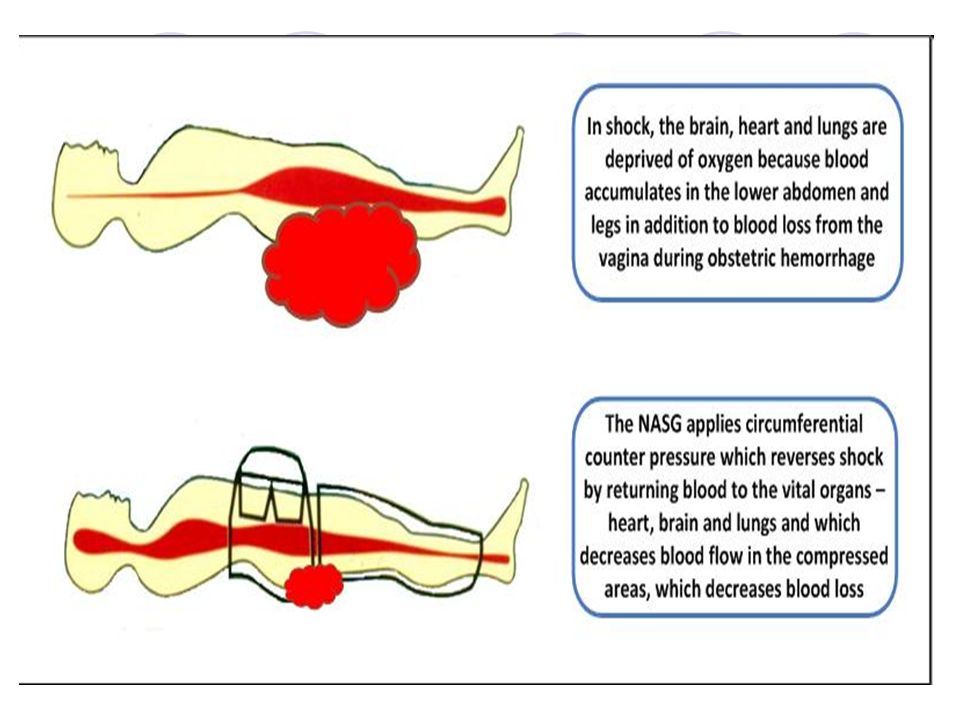
Complications of early pregnancy loss include hypovolemic shock due to excessive hemorrhage and septic abortion due to infection of retained conception products. Fortunately, these complications are rare, and complication rates are similar for expectant, medical, and surgical management.[2] As a result, the prognosis of spontaneous abortion is remarkably good. However, hemorrhage and infection due to miscarriage can contribute to maternal mortality, especially in low-income countries, where the social determinants of health decrease access to high-quality obstetrical care. [6]
[6]
History and Physical
Symptoms of spontaneous abortion depend on the type. A missed abortion is either asymptomatic or accompanied by a regression of the natural symptoms and signs of normal pregnancy.[1][3] Threatened, inevitable, incomplete, and complete abortions are all associated with abdominal-pelvic cramping and vaginal bleeding.[1][5] In addition to these symptoms, septic abortion is often accompanied by fever, purulent cervical or vaginal discharge, tachycardia, and hypotension.[7] An attempt should be made to quantify the amount of bleeding, as hemorrhage greater than typical menses often suggests early pregnancy loss. When there is significant bleeding, patients can exhibit symptoms and signs of hypovolemia, even in the absence of sepsis.
The first day of the last menstrual period and findings on any prior ultrasounds should be determined to establish the gestational age and location of the pregnancy. An abdominal exam should be performed to assess for peritoneal signs that might indicate a ruptured ectopic pregnancy or extra-uterine extension of a septic abortion.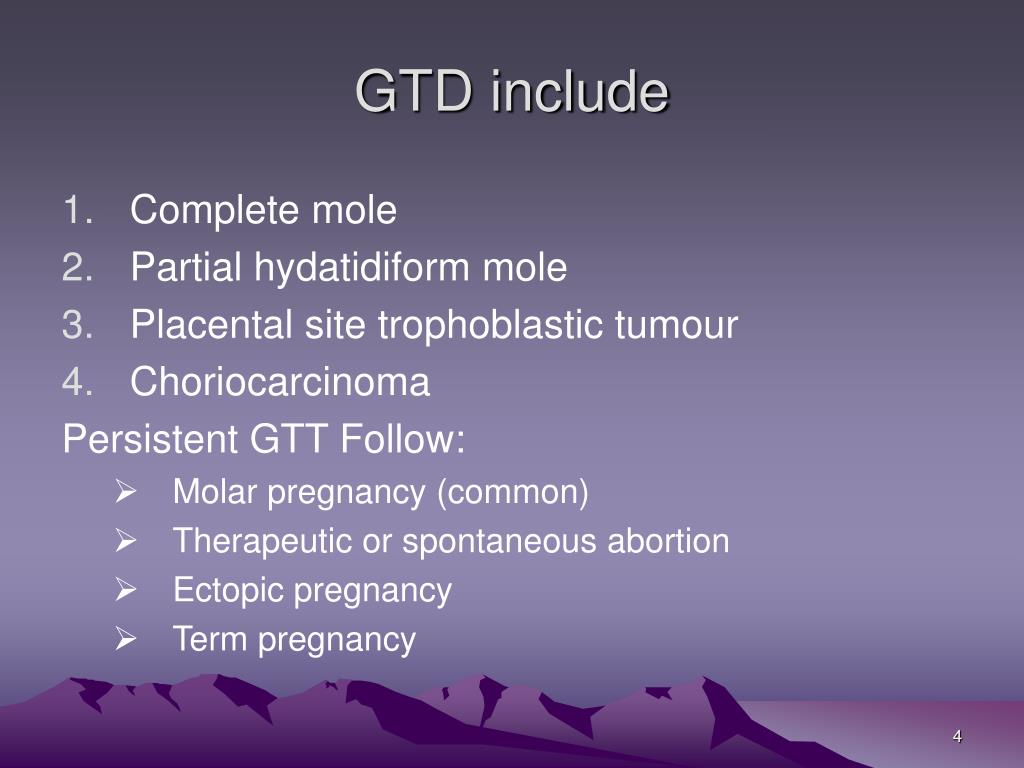 Lastly, a pelvic exam is central to the evaluation of suspected miscarriage. It should include both speculum-facilitated visualization of the cervix and a bimanual examination to assess for cervical motion tenderness that may indicate a septic abortion or an adnexal mass that may herald ectopic pregnancy.[5]
Lastly, a pelvic exam is central to the evaluation of suspected miscarriage. It should include both speculum-facilitated visualization of the cervix and a bimanual examination to assess for cervical motion tenderness that may indicate a septic abortion or an adnexal mass that may herald ectopic pregnancy.[5]
Evaluation
Further evaluation of miscarriage also depends on the type suspected based on history and physical exam. As a missed abortion has no reliable symptoms or signs, it can only be diagnosed by measurement of beta-human chorionic gonadotropin (beta-hCG) levels and pelvic ultrasound. A beta-hCG level is useful initially, as it helps determine the likelihood of intrauterine pregnancy. For example, when the beta-hCG level is more than 1,500-3,000 mIU/mL (the discriminatory level), intrauterine pregnancy should be evident on transvaginal ultrasound. If an intrauterine pregnancy is not seen on ultrasound with a beta-hCG above the discriminatory level, either early pregnancy loss or ectopic pregnancy should be suspected. [1][2][5][2][11][12]
[1][2][5][2][11][12]
In the setting of a viable pregnancy, beta-hCG levels increase at a relatively predictable rate. However, as the beta-hCG level increases, its rate of rising gradually decreases until reaching a plateau at ten weeks gestation. For example, an initial beta-hCG level of less than 1500 will increase by 50% over 48 hours, while an initial level greater than 3000 will only increase by 33% over the same period.[13]
The events of early pregnancy follow a predictable pattern and any variation from this sequence concerns spontaneous abortion. For example, a gestational sac with a mean diameter of at least 25 mm should contain a viable embryo, and an embryo with a crown-rump length of at least 7 mm should demonstrate detectable cardiac activity. Besides, the development of the yolk sac follows the appearance of the gestational sac and is usually accompanied by the presence of an embryo with cardiac activity.
Therefore, when there is evidence of prior intrauterine pregnancy, spontaneous abortion can be diagnosed if the mean gestational sac diameter is greater than or equal to 25 mm on pelvic ultrasound but contains no embryo or if the crown-rump length of the embryo is greater than or equal to 7 mm, but there is no cardiac activity.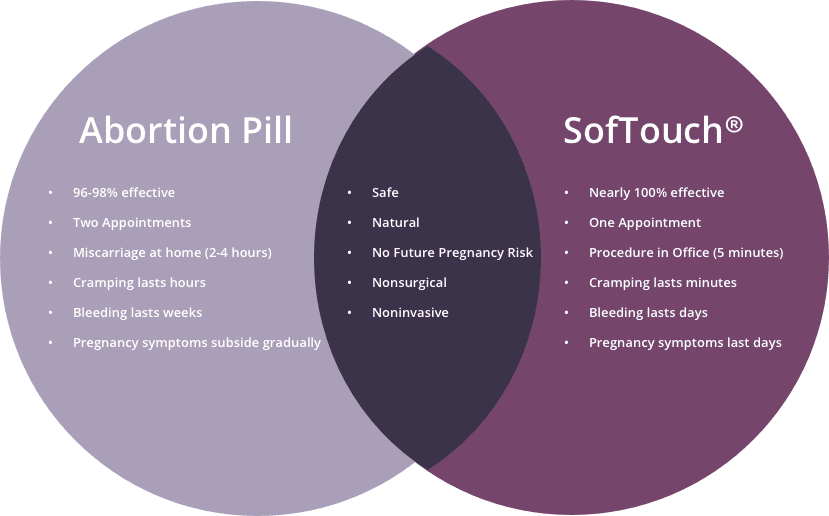 Early pregnancy loss can also be diagnosed if there is no embryo with cardiac activity at least 14 days after prior ultrasound demonstrated a gestational sac or at least 11 days after a previous ultrasound revealed a gestational sac with a yolk sac. However, some ultrasound findings, such as an embryonic heart rate of fewer than 85 beats per minute, are suspicious but not diagnostic for early pregnancy loss. When the diagnosis of spontaneous abortion is uncertain, trending beta-hCG levels every 48 to 72 hours and repeating the pelvic ultrasound in 7-10 days are recommended.[1][2][5][2][11][12]
Early pregnancy loss can also be diagnosed if there is no embryo with cardiac activity at least 14 days after prior ultrasound demonstrated a gestational sac or at least 11 days after a previous ultrasound revealed a gestational sac with a yolk sac. However, some ultrasound findings, such as an embryonic heart rate of fewer than 85 beats per minute, are suspicious but not diagnostic for early pregnancy loss. When the diagnosis of spontaneous abortion is uncertain, trending beta-hCG levels every 48 to 72 hours and repeating the pelvic ultrasound in 7-10 days are recommended.[1][2][5][2][11][12]
Threatened abortion can be diagnosed in the setting of cramping and vaginal bleeding but with a closed cervical os on exam and evidence of a viable intrauterine pregnancy on ultrasound. Inevitable abortion is diagnosed in the presence of cramping, vaginal bleeding, an open cervical os on the physical exam but no passage of the products of conception. The intrauterine pregnancy may be either viable or nonviable on ultrasound.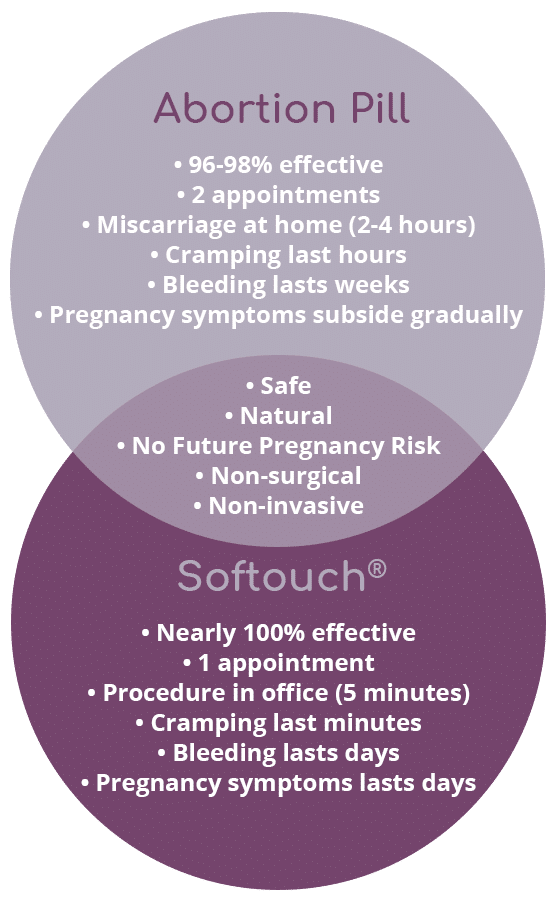 Incomplete abortion can be diagnosed in the instance of cramping, bleeding, an open cervical os, and partial passage of conception products. Retained products of a nonviable pregnancy will be evident on ultrasound. Complete abortion is diagnosed in the case of resolving cramp and bleeding, either an open or closed cervical os and no intrauterine conception products on ultrasound.[5][12][5]
Incomplete abortion can be diagnosed in the instance of cramping, bleeding, an open cervical os, and partial passage of conception products. Retained products of a nonviable pregnancy will be evident on ultrasound. Complete abortion is diagnosed in the case of resolving cramp and bleeding, either an open or closed cervical os and no intrauterine conception products on ultrasound.[5][12][5]
Septic abortion is diagnosed when cramping, and bleeding is followed by purulent cervical or vaginal discharge, fever, and an open or closed cervical os. If an induced abortion was performed with poor technique, then pelvic ultrasound may reveal retained conception products, exudative fluid, an extra-uterine extension of the infection, or uterine perforation.[7]
Besides beta-hCG measurement and ultrasound, a hemoglobin and hematocrit level should be obtained to rule out acute blood loss anemia. If unknown, maternal blood type and Rh status should be determined to prepare for possible blood transfusion or administration of Rh (D)-immune globulin. Since spontaneous abortion can be precipitated by infection, wet mount examination and screening for gonorrhea and chlamydia should also be considered.[2][5][12] This is especially important in septic abortion, where cultures of urine, blood, endocervical secretions, and evacuated conception products are recommended.[7]
Since spontaneous abortion can be precipitated by infection, wet mount examination and screening for gonorrhea and chlamydia should also be considered.[2][5][12] This is especially important in septic abortion, where cultures of urine, blood, endocervical secretions, and evacuated conception products are recommended.[7]
Treatment / Management
To some extent, the management of spontaneous abortion also depends on the type. However, expectant, medical, and surgical management is generally shown to be equally effective. Two notable exceptions are excessive bleeding and infection, in which case, surgical management is preferred.[1][2][5] Also, expectant management of missed abortion demonstrates a variable success rate of 25 to 76%. Therefore, surgical or even medical management of missed abortion is generally accepted as the preferred method of management.[3] Threatened and inevitable abortion can be managed expectantly unless the patient desires medical or surgical intervention. Incomplete abortion can also be managed expectantly.[1][2][5] However, it may take up to eight weeks for 80% of women to experience a complete abortion with expectant management alone. As a result, medical management of incomplete abortion is becoming more prevalent.[2]
Incomplete abortion can also be managed expectantly.[1][2][5] However, it may take up to eight weeks for 80% of women to experience a complete abortion with expectant management alone. As a result, medical management of incomplete abortion is becoming more prevalent.[2]
The conventionally accepted regimen for medical management consists of misoprostol 800 mcg vaginally, with a repeated dose if needed any time from three hours to seven days after the first dose. Premedication with mifepristone 200 mg orally 24 hours before the first dose of misoprostol may result in a higher success rate than misoprostol alone. Surgical management consists of dilation and suction curettage with sharp curettage, as needed, in either the operating room or office setting. There is evidence that suction curettage alone, without sharp curettage, is sufficient and decreases the risk of intrauterine adhesions, as long as there is reasonable certainty that the uterus is empty. Due to a lack of evidence on the safety of expectant management of second-trimester miscarriage, medical or surgical management is preferred beyond 12-13 weeks gestational age. [2]
[2]
Although there is a lack of consensus, complete abortion is often defined as the absence of a gestational sac on ultrasound with an endometrial stripe thickness of less than 30 mm. This ultrasound is usually performed 7-14 days after the initiation of medical management for spontaneous abortion. Patient-reported resolution of cramps and bleeding is also useful in confirming complete abortion.[2] Beta-hCG levels do not need to be followed to 0, unless the location of the pregnancy within the pelvis remains unknown, or if persistent bleeding and constitutional symptoms of malignancy raise suspicion for the gestational trophoblastic disease.[14] Regardless of the management approach, patients should be counseled on the level of bleeding that would warrant seeking care.[2] This is often defined as the soaking of two menstrual pads per hour for two consecutive hours.[2][5] Women who are Rh (D) negative and not yet sensitized to Rh (D) factor should be given Rh (D) immune-globulins within 72 hours of the onset of miscarriage. [2] A dose of 50-120 mcg is recommended in the first trimester and 300 mcg in the second trimester.[15]
[2] A dose of 50-120 mcg is recommended in the first trimester and 300 mcg in the second trimester.[15]
Hormonal contraception may be initiated immediately after the resolution of early pregnancy loss, including the placement of an intrauterine device, which is only contraindicated in the setting of septic abortion [2]. Attempting conception immediately is also safe, and couples who attempt conception within three months after miscarriage experience higher rates of successful pregnancy and live birth than those who postpone conception.[16][17] However, the weeks to months after a miscarriage are often accompanied by feelings of grief or even guilt, anxiety, and depression for both the woman and her partner. Although there is limited evidence for the effectiveness of psychological counseling, patients and their families will likely experience better outcomes if these emotions and feelings are addressed early.[1]
Differential Diagnosis
The differential diagnosis of spontaneous abortion can be constructed by considering the pelvic organs that could be responsible for vaginal bleeding early in pregnancy.
Ectopic pregnancy can also cause cramping, vaginal bleeding, and a plateau or decline in the natural rise of beta-hCG in early pregnancy.
Sub-chorionic hematoma is another common cause of vaginal bleeding in pregnancy.
Gestational trophoblastic disease, although rare, is a feared differential diagnosis of early pregnancy loss.
Cervical pathologies that should be considered include friability more than that typically encountered in pregnancy, infectious cervicitis, cervical polyps, ectropion, and dysplasia. These etiologies should be high on the differential in the setting of post-coital bleeding.
Implantation and idiopathic bleeding of pregnancy are other vital considerations.
Cervical and vaginal trauma must also be considered.
These differential diagnoses can usually be sufficiently evaluated through history, physical exam, and pelvic ultrasound.[1]
Complications
Complications of spontaneous abortion include:
Septic abortion
Retained products of conception
Cervical laceration
Disseminated intravascular coagulation
Post-abortion triad (i.
 e., low-grade fever, pain, bleeding)
e., low-grade fever, pain, bleeding)Hematometra
Deterrence and Patient Education
Expecting mothers should be counseled on the avoidance of the modifiable risk factors for miscarriage. However, there is limited evidence to support the use of any single prevention strategy. Pelvic rest, tocolytics, anticoagulants, and supplemental beta-hCG have not been shown to decrease the risk of early pregnancy loss. Aspirin has only been shown to reduce the rate of spontaneous abortion in women with anti-phospholipid antibody syndrome. Likewise, supplemental progesterone has only been shown to prevent early pregnancy loss in women with recurrent spontaneous abortion. Also, genetic testing for maternal and fetal chromosomal abnormalities or anti-phospholipid syndrome is only recommended in the setting of recurrent miscarriage.[2]
Pearls and Other Issues
Spontaneous abortion is a pregnancy loss before 20 weeks of gestational age.
Approximately half of the miscarriages are due to unknown genetic abnormalities.
Alcohol or drug use, infections, chronic disease, environmental exposures, and structural uterine abnormalities are other important risk factors.
Symptoms and signs of early pregnancy loss depend on the type.
Types include missed, threatened, inevitable, incomplete, complete, recurrent, and septic.
The evaluation usually involves a thorough history, physical exam, beta-HCG measurement, and pelvic ultrasound.
Although management also depends on the type, expectant, medical, and surgical approaches are generally equally effective.
Only aspirin in the setting of the anti-phospholipid syndrome and supplemental progesterone in the context of recurrent miscarriage have demonstrated the potential for prevention.
Testing for genetic abnormalities and anti-phospholipid syndrome should generally be reserved for cases of recurrent early pregnancy loss.
Enhancing Healthcare Team Outcomes
Since spontaneous abortion can occur across multiple settings, including home, clinic, and hospital, team-based care is essential.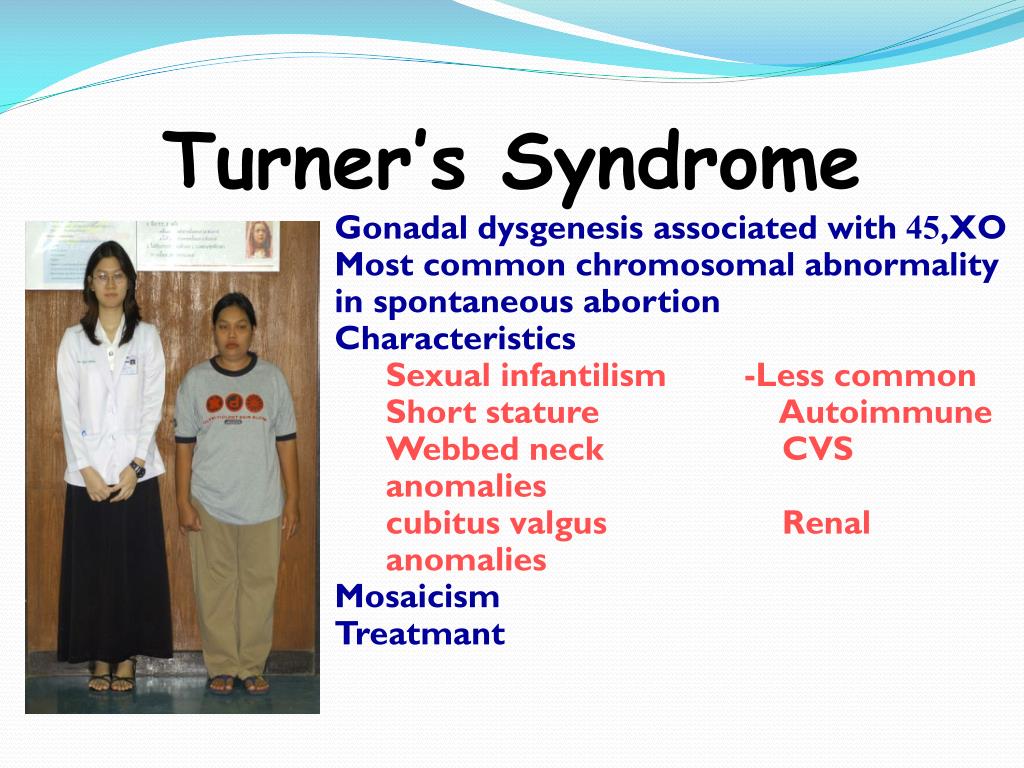 Emergency department providers must ensure the seamless transfer of medical records, including relevant labs and imaging, to outpatient clinics for appropriate follow-up. In the outpatient setting, convenient scheduling of frequent appointments is critical, as well as clear instructions for patients on when to present to the clinic versus emergency department for persistent symptoms. Finally, although the medical aspects of miscarriage management can be complicated, the psychological well being of the patient and her family cannot be neglected.
Emergency department providers must ensure the seamless transfer of medical records, including relevant labs and imaging, to outpatient clinics for appropriate follow-up. In the outpatient setting, convenient scheduling of frequent appointments is critical, as well as clear instructions for patients on when to present to the clinic versus emergency department for persistent symptoms. Finally, although the medical aspects of miscarriage management can be complicated, the psychological well being of the patient and her family cannot be neglected.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Griebel CP, Halvorsen J, Golemon TB, Day AA. Management of spontaneous abortion. Am Fam Physician. 2005 Oct 01;72(7):1243-50. [PubMed: 16225027]
- 2.
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Gynecology.
 ACOG Practice Bulletin No. 200: Early Pregnancy Loss. Obstet Gynecol. 2018 Nov;132(5):e197-e207. [PubMed: 30157093]
ACOG Practice Bulletin No. 200: Early Pregnancy Loss. Obstet Gynecol. 2018 Nov;132(5):e197-e207. [PubMed: 30157093]- 3.
Wu HL, Marwah S, Wang P, Wang QM, Chen XW. Misoprostol for medical treatment of missed abortion: a systematic review and network meta-analysis. Sci Rep. 2017 May 10;7(1):1664. [PMC free article: PMC5431938] [PubMed: 28490770]
- 4.
Zhou J, Huang Z, Pan X, Leung WT, Li C, Chen L, Zhang Y, Wang L, Sima Y, Zhang N, Qiu X, Li L, Wang L. New thoughts in exploring the pathogenesis, diagnosis, and treatment of threatened abortion. Biosci Trends. 2019;13(3):284-285. [PubMed: 31327799]
- 5.
Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019 Feb 01;99(3):166-174. [PubMed: 30702252]
- 6.
Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L. Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD007223.
 [PMC free article: PMC6464743] [PubMed: 28138973]
[PMC free article: PMC6464743] [PubMed: 28138973]- 7.
Udoh A, Effa EE, Oduwole O, Okusanya BO, Okafo O. Antibiotics for treating septic abortion. Cochrane Database Syst Rev. 2016 Jul 01;7(7):CD011528. [PMC free article: PMC6458041] [PubMed: 27364644]
- 8.
Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012 Nov;98(5):1103-11. [PubMed: 22835448]
- 9.
Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997 Jul 05;315(7099):32-4. [PMC free article: PMC2127042] [PubMed: 9233324]
- 10.
Hertz-Picciotto I, Samuels SJ. Incidence of early loss of pregnancy. N Engl J Med. 1988 Dec 01;319(22):1483-4. [PubMed: 3185669]
- 11.
Doubilet PM, Benson CB, Bourne T, Blaivas M, Society of Radiologists in Ultrasound Multispecialty Panel on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy.
 Barnhart KT, Benacerraf BR, Brown DL, Filly RA, Fox JC, Goldstein SR, Kendall JL, Lyons EA, Porter MB, Pretorius DH, Timor-Tritsch IE. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013 Oct 10;369(15):1443-51. [PubMed: 24106937]
Barnhart KT, Benacerraf BR, Brown DL, Filly RA, Fox JC, Goldstein SR, Kendall JL, Lyons EA, Porter MB, Pretorius DH, Timor-Tritsch IE. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013 Oct 10;369(15):1443-51. [PubMed: 24106937]- 12.
Bourne T. A missed opportunity for excellence: the NICE guideline on the diagnosis and initial management of ectopic pregnancy and miscarriage. J Fam Plann Reprod Health Care. 2015 Jan;41(1):13-9. [PubMed: 25512352]
- 13.
Barnhart KT, Guo W, Cary MS, Morse CB, Chung K, Takacs P, Senapati S, Sammel MD. Differences in Serum Human Chorionic Gonadotropin Rise in Early Pregnancy by Race and Value at Presentation. Obstet Gynecol. 2016 Sep;128(3):504-511. [PMC free article: PMC4993627] [PubMed: 27500326]
- 14.
Committee on Practice Bulletins-Gynecology, American College of Obstetricians and Gynecologists. ACOG Practice Bulletin #53. Diagnosis and treatment of gestational trophoblastic disease.
 Obstet Gynecol. 2004 Jun;103(6):1365-77. [PubMed: 15172880]
Obstet Gynecol. 2004 Jun;103(6):1365-77. [PubMed: 15172880]- 15.
Practice Bulletin No. 181: Prevention of Rh D Alloimmunization. Obstet Gynecol. 2017 Aug;130(2):e57-e70. [PubMed: 28742673]
- 16.
Schliep KC, Mitchell EM, Mumford SL, Radin RG, Zarek SM, Sjaarda L, Schisterman EF. Trying to Conceive After an Early Pregnancy Loss: An Assessment on How Long Couples Should Wait. Obstet Gynecol. 2016 Feb;127(2):204-12. [PMC free article: PMC4780347] [PubMed: 26942344]
- 17.
Sundermann AC, Hartmann KE, Jones SH, Torstenson ES, Velez Edwards DR. Interpregnancy Interval After Pregnancy Loss and Risk of Repeat Miscarriage. Obstet Gynecol. 2017 Dec;130(6):1312-1318. [PMC free article: PMC5709156] [PubMed: 29112656]
Spontaneous abortion - description, signs, treatment, prevention and diagnosis Spontaneous abortion is a spontaneous natural termination of pregnancy up to 22 weeks. This happens due to a violation of the development of the fetus or any pathologies in the mother.
 A spontaneous abortion is commonly referred to as a miscarriage. The difference between miscarriage and preterm birth is that in preterm birth, which occurs at 22-37 weeks of gestation, a viable baby (weighing at least 500 g) is born. nine0003
A spontaneous abortion is commonly referred to as a miscarriage. The difference between miscarriage and preterm birth is that in preterm birth, which occurs at 22-37 weeks of gestation, a viable baby (weighing at least 500 g) is born. nine0003 Features
The symptoms of a miscarriage depend on the duration of the pregnancy. So, if a spontaneous abortion occurs in the early stages, it begins with bleeding. Pain is either minor or non-existent.
With a miscarriage in the later stages, the first symptom is severe cramping pain, and bleeding begins later. Symptoms of spontaneous abortion can also be: pain in the sacrum, vomiting, rupture of amniotic fluid.
Description
Abortion is the termination of pregnancy, ending in the birth of an immature and unviable fetus. Sometimes it is planned, more often it happens spontaneously, without the desire of a woman. Such spontaneous abortions, according to statistics, end in 15-20% of pregnancies. Although there is an opinion that a significant number of spontaneous abortions occur at a very early stage and women do not notice them. Then the number of miscarriages increases to 50-78%. At the same time, 60% of them are due to some kind of chromosomal abnormalities, so many doctors qualify the majority of miscarriages that occur in the first trimester of pregnancy as a manifestation of natural selection. According to the stages of pregnancy, abortions are divided into:
Then the number of miscarriages increases to 50-78%. At the same time, 60% of them are due to some kind of chromosomal abnormalities, so many doctors qualify the majority of miscarriages that occur in the first trimester of pregnancy as a manifestation of natural selection. According to the stages of pregnancy, abortions are divided into:
- infraclinical abortion that occurred at a very early stage of pregnancy;
- abortion during the first trimester;
- abortion during the second trimester;
- repeated abortions.
Most often, spontaneous abortion occurs in the third month of pregnancy, in the second and fourth - much less often. And how many of them occur in the first month, it is very difficult to calculate. This can happen due to any past or current diseases (syphilis, toxoplasmosis, brucellosis, listeriosis), features of the constitution and development of a woman (anomalies in the development of the genital organs, infantilism), pathologies of the fetal egg and diseases of the second parent.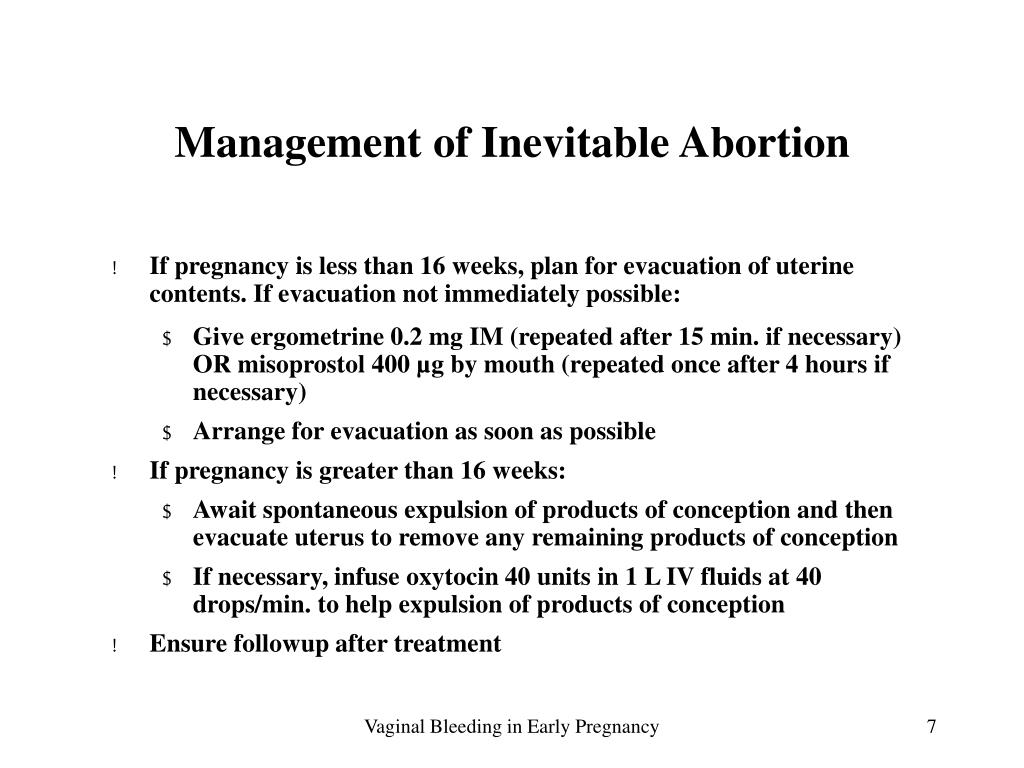 Also, the cause of spontaneous abortion can be previous abortions, a small interval between pregnancies, Rh conflict, hormonal disorders (excess male hormones, diabetes mellitus), smoking, alcohol and drug use, difficult or harmful working conditions, and even the quality of food. nine0003
Also, the cause of spontaneous abortion can be previous abortions, a small interval between pregnancies, Rh conflict, hormonal disorders (excess male hormones, diabetes mellitus), smoking, alcohol and drug use, difficult or harmful working conditions, and even the quality of food. nine0003
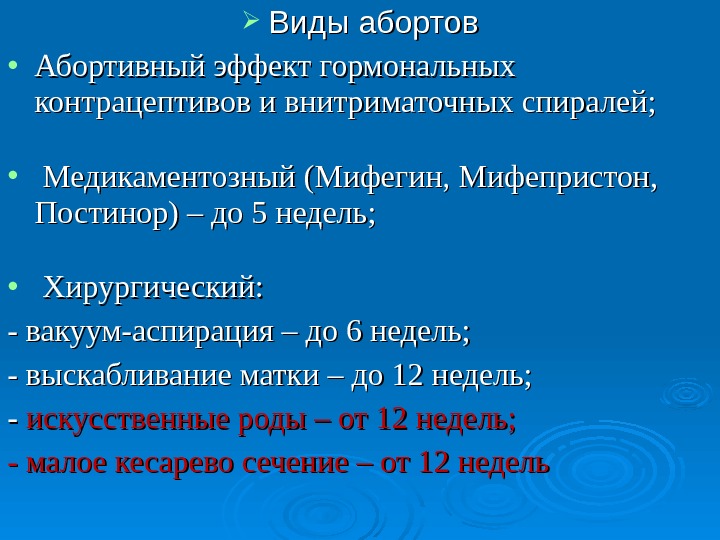
There are several types of spontaneous abortion, depending on the degree of detachment of the fetal egg and emptying of the uterine cavity:
- threatened miscarriage;
- a miscarriage that has begun;
- abortion in progress;
- incomplete abortion;
- complete abortion.
Now in more detail about each of them.
Threat of miscarriage occurs in 25% of pregnancies. Approximately half of them end in miscarriage. In this case, detachment of the ovum does not occur, there may not be bloody discharge, cramping pains in the lower abdomen are disturbing, it is possible to reduce signs of pregnancy - swelling of the mammary glands, nausea, frequent urination .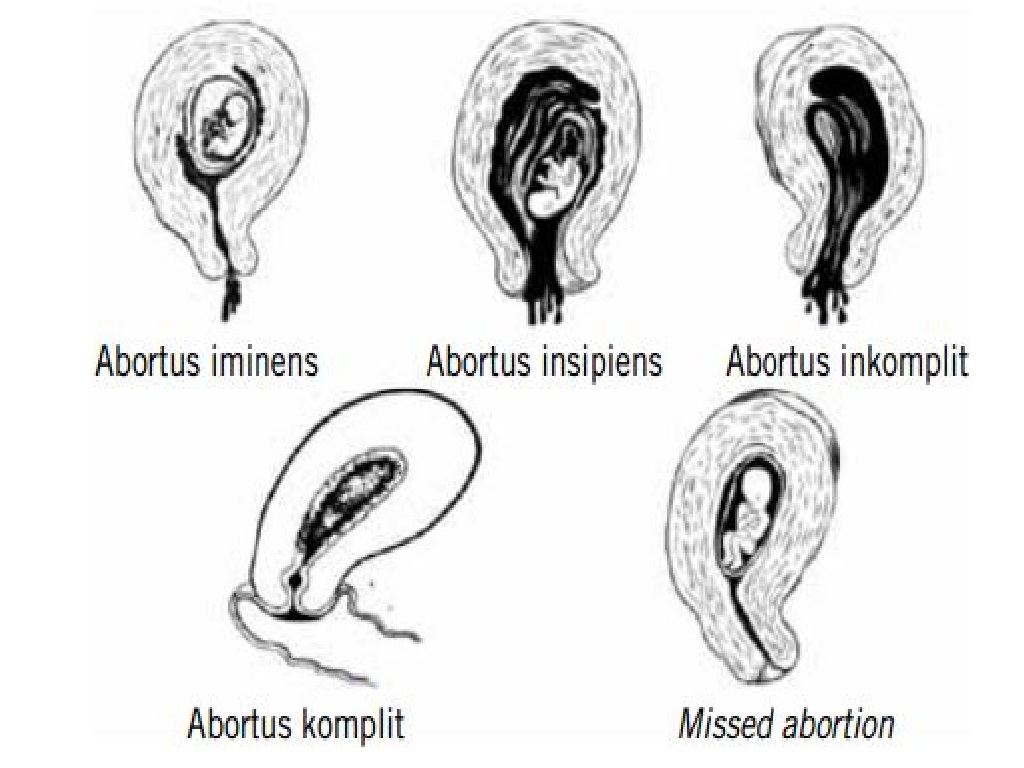 ..
..
With a miscarriage that has begun, bleeding and cramping pain intensify, the uterus is painful on palpation. The fertilized egg partially separates from the uterus.
With abortion in the course of , the detachment of the fetus intensifies, in addition to bleeding and cramping pain, there is also a feeling of compression of the rectum and the urge to defecate.
With incomplete abortion , a part of the fetal egg is usually born. And the part remaining in the uterus interferes with its contraction and hemostasis. Bleeding continues and can lead to hemorrhagic shock. Even if the fetal egg seems to have come out completely and the bleeding is insignificant, there is still a risk of renewed bleeding within 5-6 days due to the remaining particles of the fetal egg, the formation of a placental polyp and infection. nine0003
Complete abortion occurs more often in the later stages. The ovum is completely expelled, accompanied by cramping pain and bleeding. After expulsion, the uterus contracts and the bleeding stops.
After expulsion, the uterus contracts and the bleeding stops.
A failed abortion is also possible. In this case, the dead fetus is not expelled from the uterus.
If a spontaneous abortion occurs for a long time, an infection from the vagina can enter the uterus. Moreover, if inflammation occurs only in the uterus, this is an uncomplicated infected abortion, and if the infection spreads to all organs of the small pelvis, then a complicated infected abortion. It is also possible for the infection to spread throughout the body. This condition is called septic abortion. nine0003
Diagnostics
If a spontaneous abortion is suspected, a transvaginal ultrasound is mandatory to find out how the pregnancy is proceeding and whether the fetus has died, determine the level of human chorionic gonadotropin in the blood, do a general blood test and a general urine test. It is also necessary to determine the blood type and Rh factor of the mother and child. If this is not the first spontaneous abortion in a woman, the parents are examined for the carriage of chromosomal abnormalities, infections, the presence of any systemic diseases and anatomical abnormalities of the woman, which do not allow her to carry the pregnancy normally. nine0003
nine0003
A morphological study of the placenta preparation is also carried out. In some cases, diagnostic curettage of the uterus and cervical canal is necessary.
Treatment
As soon as it seems to a woman that “something is wrong” with her, she should immediately contact a gynecologist. On the one hand, not every bleeding during pregnancy is a sign of spontaneous abortion. On the other hand, it's better to play it safe. If there are no pathologies and the fetus is alive, if there is a threat of miscarriage, bed rest, vitamins, drugs to relax the myometrium, and a diet are prescribed. Sex in this state is not recommended. In Russia, usually with the threat of a miscarriage, a woman is put in a hospital, abroad - according to the condition, they can put a dropper and let her go home, after giving the necessary recommendations, or they can put her in the hospital. In many European countries, with the threat of miscarriage and the actual miscarriage at a gestational age of up to three to four months, nothing is done if it occurs less than three pregnancies in a row.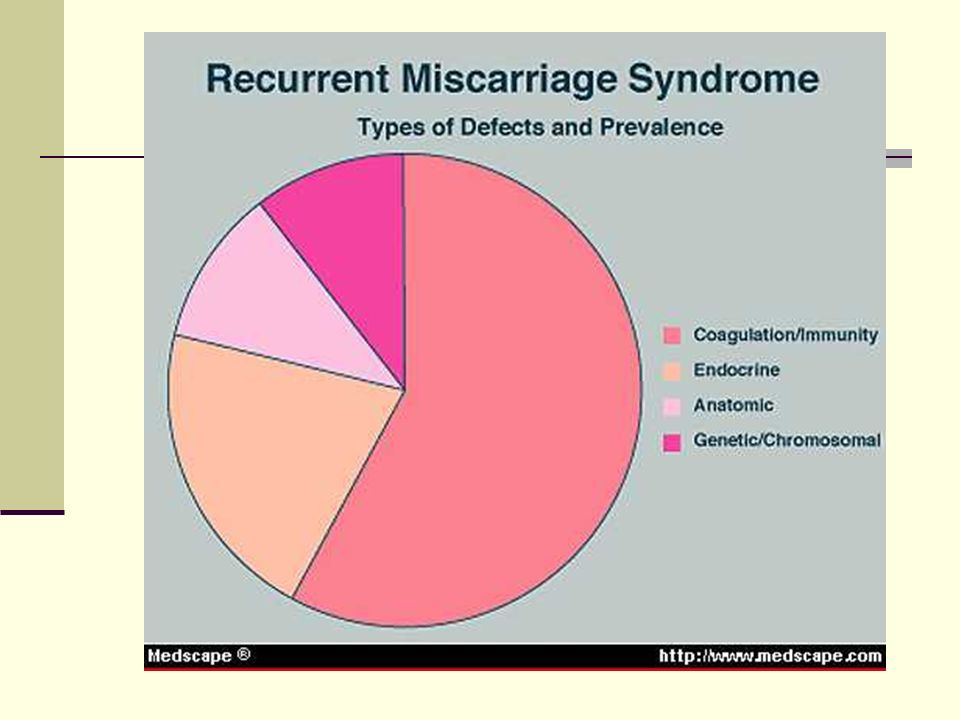 nine0003
nine0003
In some cases, with the threat of miscarriage, hormonal and antibacterial agents are prescribed. Sometimes surgery is also required.
If the fetus is dead, it must be removed from the uterus. The procedure is carried out in a hospital and until the completion of the abortion, and sometimes several days after, the woman should be under the supervision of a doctor. She is transfused with blood substitutes in case of large blood loss, and the uterus is scraped. In some cases, such as cervical pregnancy, the uterus may also be removed. nine0003
If necessary, analgesics, anti-Rhesus immunoglobulin are prescribed.
Unfortunately, in the event of a miscarriage, complications are possible. When scraping, this is perforation, infection of the uterus, uterine bleeding. Depression often occurs after a spontaneous abortion.
Prophylaxis
For most early abortions (before 12 weeks), there is no specific prophylaxis. Only vitamins, proper nutrition, lack of stress, limitation of physical activity. Also, pregnant women should not lift weights, as this can also cause spontaneous abortion. Some doctors believe that before the 8th week of pregnancy, hormone therapy is inappropriate, as it interferes with natural selection. nine0003
Also, pregnant women should not lift weights, as this can also cause spontaneous abortion. Some doctors believe that before the 8th week of pregnancy, hormone therapy is inappropriate, as it interferes with natural selection. nine0003
In general, therapeutic support for pregnancy is justified only if ultrasound has confirmed the viability of the fetus. It includes bed rest, antispasmodics and muscle relaxants (drugs that relax smooth muscles), hormone therapy.
If a woman has already had three miscarriages, she needs to do some research:
- genetic testing of both partners. It will help identify chromosomal abnormalities that may be the cause of the death of the embryo. nine0016
- hysterography. This study will help identify pathologies in the development of the uterus, for example, adhesions, septa, and other malformations.
- hormonal examination.
- tests for infections.
- immunological analysis. Sometimes the cause of a miscarriage can be a weak or, conversely, too strong immunity.
Depending on the results of the studies, the doctor will prescribe an effective treatment to solve this problem. nine0003
© Dr. Peter
Spontaneous abortion (miscarriage)
If the pregnancy ends naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor. nine0003
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.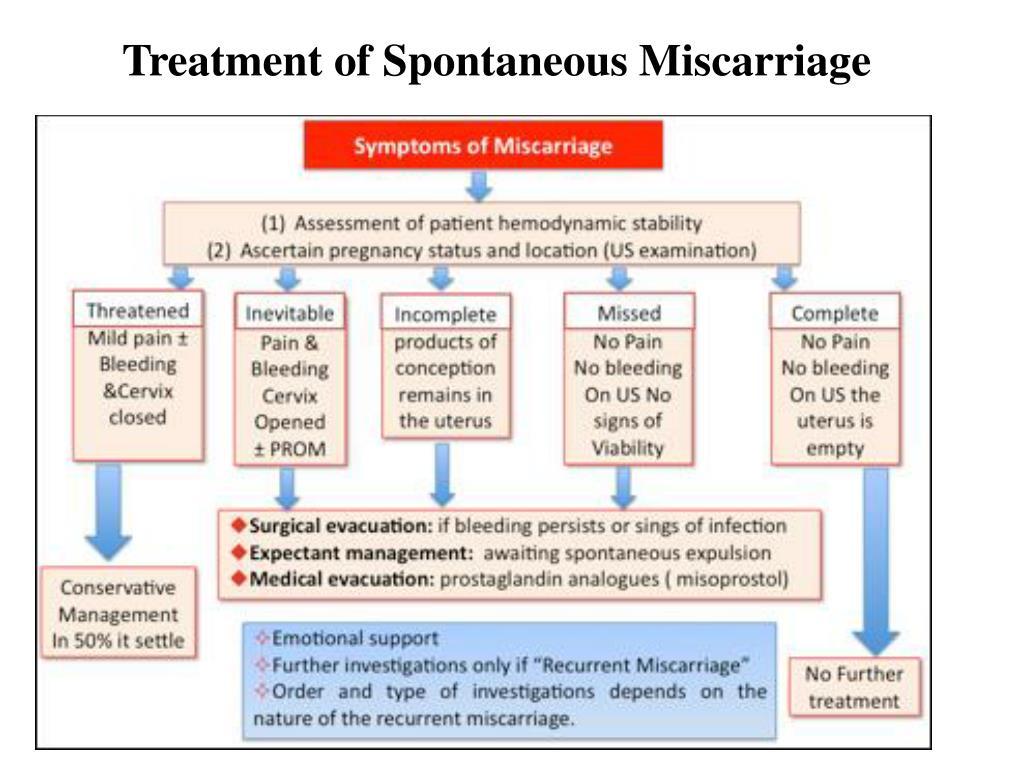
Types of spontaneous abortion
1. Threatened miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen. nine0003
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy; nine0003
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.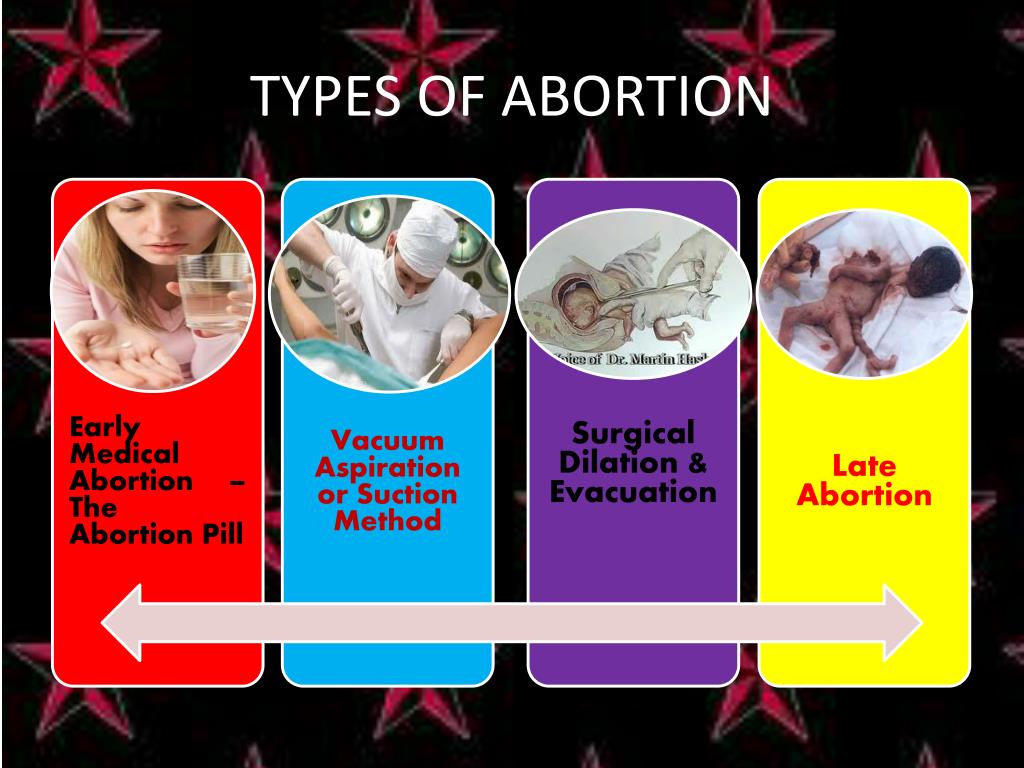
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, drawing pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization. nine0003
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin.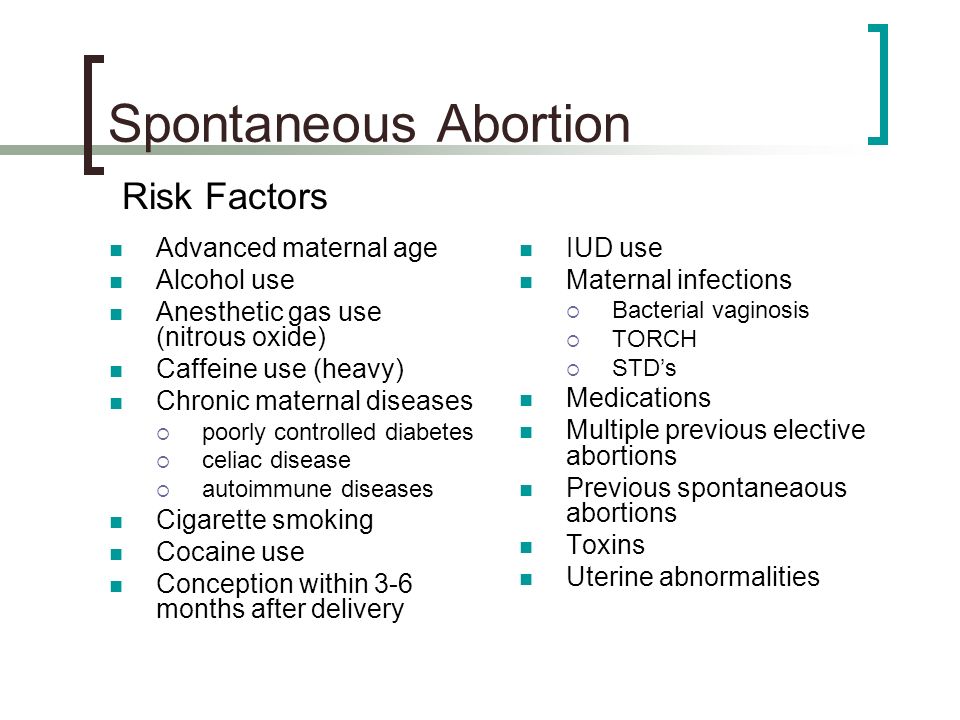 Pregnancy cannot be saved, cleaning is required; nine0003
Pregnancy cannot be saved, cleaning is required; nine0003
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them. nine0003
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.