Sleeping positions during 8th month of pregnancy
Best Sleeping Positions While Pregnant
The best sleep position during pregnancy is “SOS” (sleep on side) because it provides the best circulation for you and your baby. It also places the least pressure on your veins and internal organs. Sleeping on your left side will increase the amount of blood and nutrients that reach the placenta and your baby. Plus good circulation helps reduce potential swelling, varicose veins in your legs and hemorrhoids.
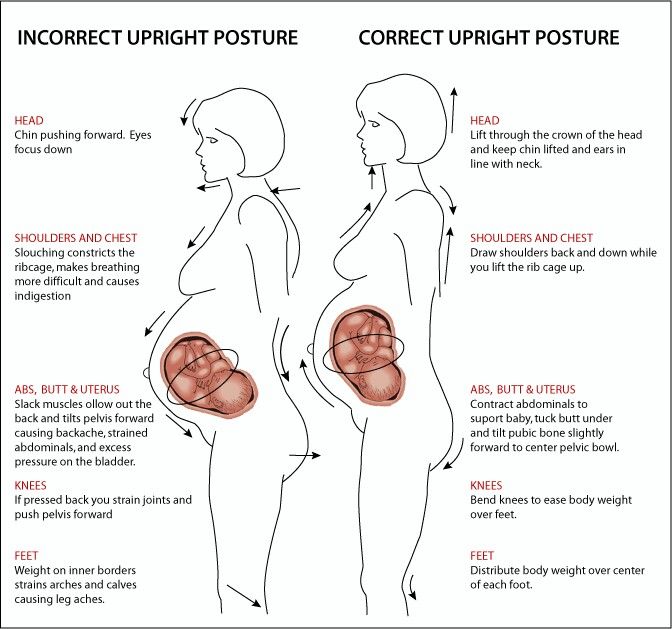
How Can I Sleep More Comfortably During Pregnancy?
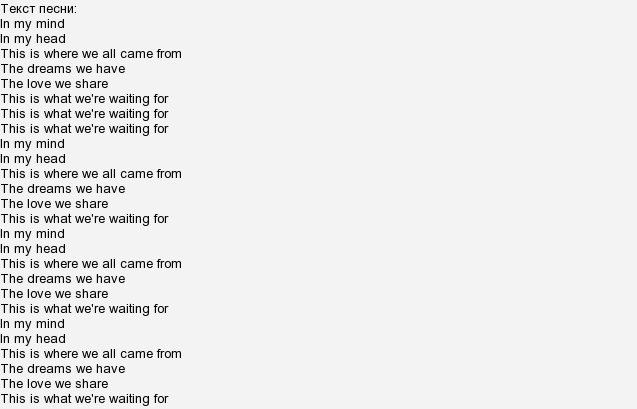
Keep your legs and knees bent, and put a pillow between your legs to relieve the stress on your back.
- If you find that you are having problems with back pain, use the “SOS” position, and try placing a pillow under your abdomen as well.
- If you are experiencing heartburn during the night, you may want to try propping your upper body with pillows.
- In late pregnancy, you may experience shortness of breath. Try lying on your side or propped up with pillows.
These suggestions may not sound completely comfortable, especially if you are used to sleeping on your back or stomach, but try them out. You may find that they work. Keep in mind that you may not stay in one position all night, and rotating positions is fine.
What Sleep Positions During Pregnancy Should I Avoid?
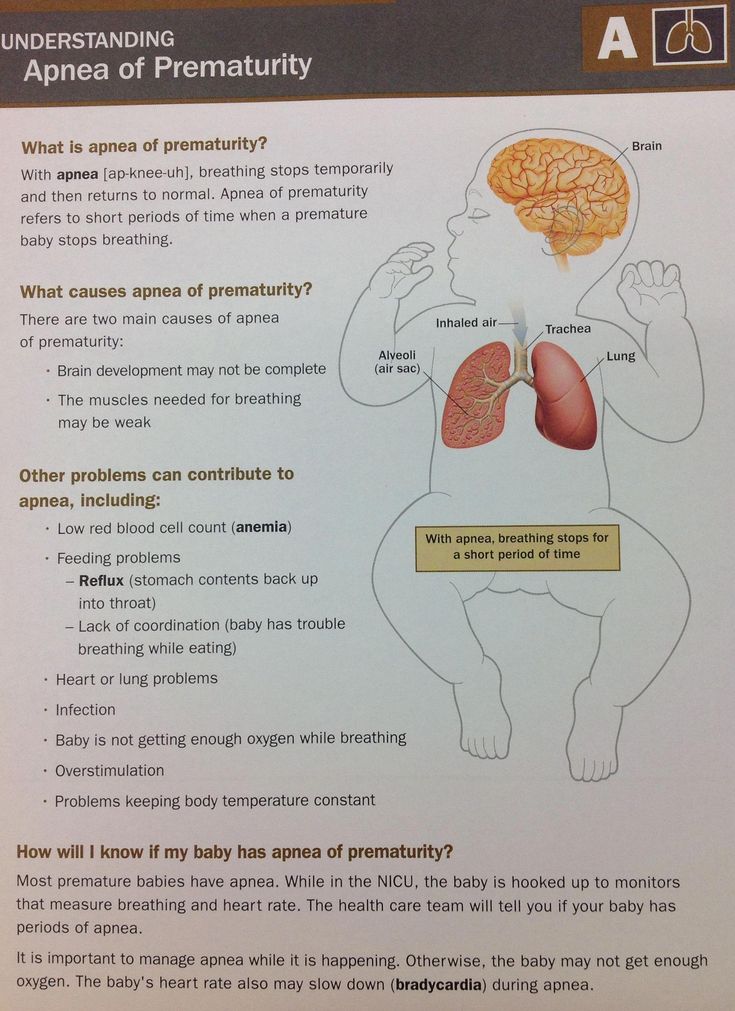
Sleeping on your back: This can cause problems with backaches, breathing, the digestive system, hemorrhoids, low blood pressure and cause a decrease in circulation to your heart and your baby. This is a result of your growing abdomen resting on your intestines and major blood vessels (the aorta and vena cava). You can also develop sleep apnea as you put on weight.
Sleeping on your stomach: When you are farther along in your pregnancy, your breasts become more tender and your abdomen continues to grow, both making sleeping on your tummy uncomfortable. Using a donut-shaped pillow (with a hole in the middle) may help you sleep comfortably on your stomach.
Reasons for your discomfort may include:
During pregnancy, you may find yourself wrestling in bed trying to get comfortable before falling asleep. When you are pregnant your body goes through a variety of changes causing your regular sleeping positions to no longer work for you.
- Increased size of the abdomen
- Back pain
- Heartburn
- Shortness of breath
- Insomnia
More Steps to Sleeping Better While Pregnant
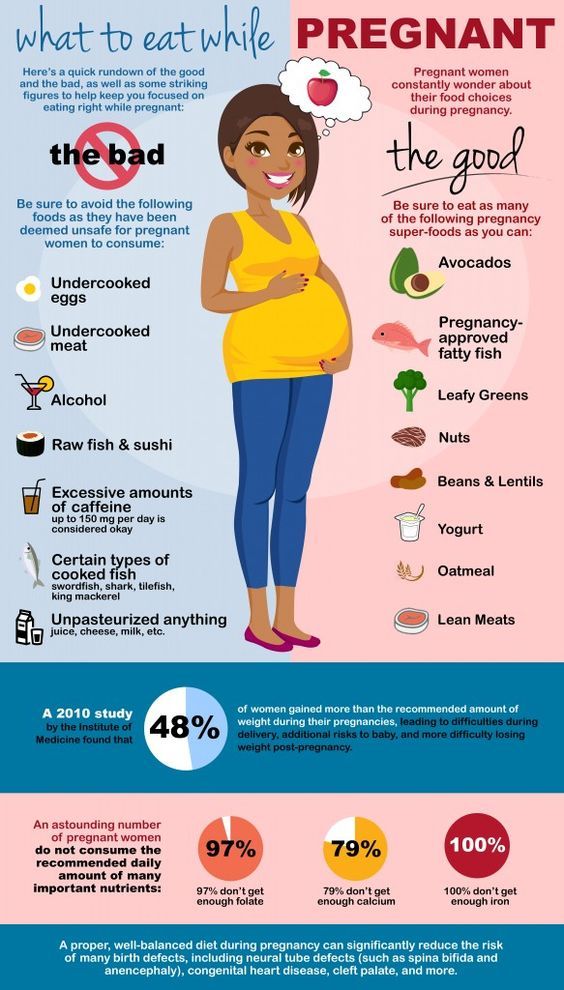
- Limit caffeine. Try not to drink coffee or caffeinated tea after 3 p.m.
- Brink plenty of water. Drink lot of water through out the day, but limit intake a couple of hours before bedtime so you don’t have to wake up and go to the bathroom.
- Exercise for 30 minutes. Exercise helps you sleep better, but don’t exercise within four hours of bedtime.
- Relaxing activities. A warm bath, foot or shoulder massage will help you relax.
- Peaceful bedroom. Keeping your bedroom dark, quiet and cool at night will help to drift off to sleep and stay asleep.
- 7 Discomforts of Pregnancy
- Nighfood Nighttime Ice Cream
- Pregnancy Week 15
Compiled using information from the following sources:
1. Nemours Foundation
https://www.kidshealth.org
1. Your Pregnancy Week by Week Fifth Ed. Curtis, Glade B., OB/GYN, et al. Week 16
Sleeping During Your Third Trimester
1.
Sedov, I. D., Cameron, E. E., Madigan, S., & Tomfohr-Madsen, L. M. (2018). Sleep quality during pregnancy: A meta-analysis. Sleep medicine reviews, 38, 168–176. https://www.sciencedirect.com/science/article/abs/pii/S1087079217300291?via%3Dihub
2.
Mindell, J. A., Cook, R. A., & Nikolovski, J. (2015). Sleep patterns and sleep disturbances across pregnancy.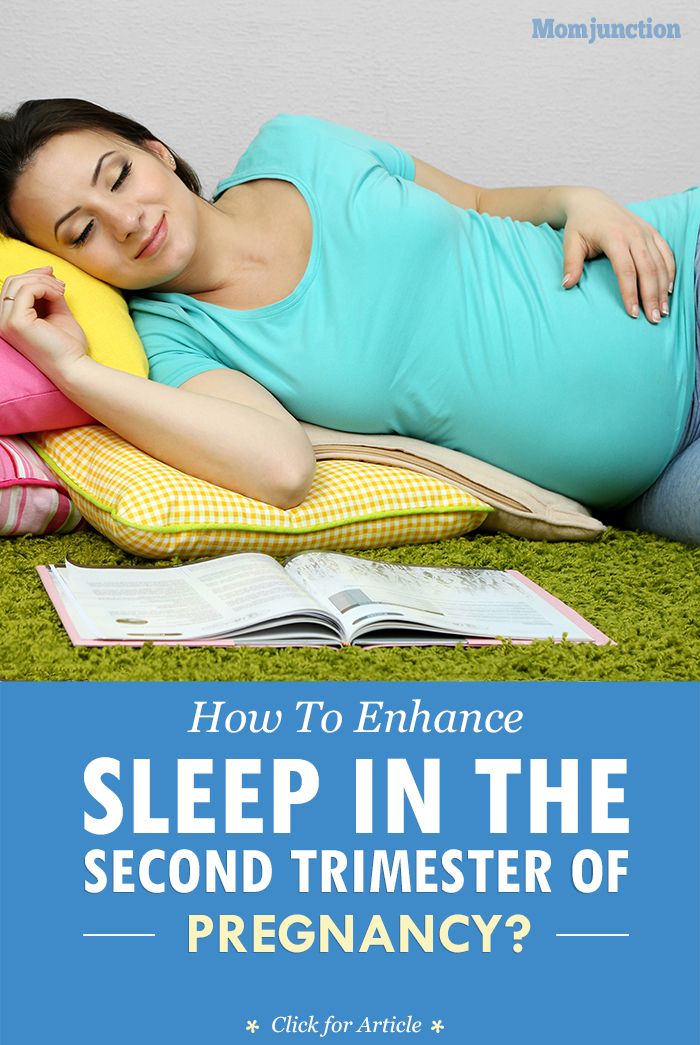 Sleep medicine, 16(4), 483–488. https://www.sciencedirect.com/science/article/abs/pii/S1389945714004997?via%3Dihub
Sleep medicine, 16(4), 483–488. https://www.sciencedirect.com/science/article/abs/pii/S1389945714004997?via%3Dihub
3.
Virgara, R., Maher, C., & Van Kessel, G. (2018). The comorbidity of low back pelvic pain and risk of depression and anxiety in pregnancy in primiparous women. BMC pregnancy and childbirth, 18(1), 288. https://doi.org/10.1097/01.AOG.0000129403.54061.0e
4.
Virgara, R., Maher, C., & Van Kessel, G. (2018). The comorbidity of low back pelvic pain and risk of depression and anxiety in pregnancy in primiparous women. BMC pregnancy and childbirth, 18(1), 288. https://doi.org/10.1186/s12884-018-1929-4
5.
Román-Gálvez, R. M., Amezcua-Prieto, C., Salcedo-Bellido, I., Martínez-Galiano, J. M., Khan, K. S., & Bueno-Cavanillas, A. (2018). Factors associated with insomnia in pregnancy: A prospective Cohort Study. European journal of obstetrics, gynecology, and reproductive biology, 221, 70–75. https://doi. org/10.1016/j.ejogrb.2017.12.007
org/10.1016/j.ejogrb.2017.12.007
6.
Reichner C. A. (2015). Insomnia and sleep deficiency in pregnancy. Obstetric medicine, 8(4), 168–171. https://doi.org/10.1177/1753495X15600572
7.
Ruiz-Robledillo, N., Canário, C., Dias, C. C., Moya-Albiol, L., & Figueiredo, B. (2015). Sleep during the third trimester of pregnancy: the role of depression and anxiety. Psychology, health & medicine, 20(8), 927–932. https://doi.org/10.1080/13548506.2015.1017508
8.
Lara-Carrasco, J., Simard, V., Saint-Onge, K., Lamoureux-Tremblay, V., & Nielsen, T. (2014). Disturbed dreaming during the third trimester of pregnancy. Sleep medicine, 15(6), 694–700. https://doi.org/10.1016/j.sleep.2014.01.026
9.
Neau, J. P., Texier, B., & Ingrand, P. (2009). Sleep and vigilance disorders in pregnancy. European neurology, 62(1), 23–29. https://doi.org/10.1159/000215877
10.
Hutchison, B. L., Stone, P. R., McCowan, L. M., Stewart, A. W., Thompson, J. M., & Mitchell, E. A. (2012). A postal survey of maternal sleep in late pregnancy. BMC pregnancy and childbirth, 12, 144. https://doi.org/10.1186/1471-2393-12-144
L., Stone, P. R., McCowan, L. M., Stewart, A. W., Thompson, J. M., & Mitchell, E. A. (2012). A postal survey of maternal sleep in late pregnancy. BMC pregnancy and childbirth, 12, 144. https://doi.org/10.1186/1471-2393-12-144
11.
Medical Encyclopedia: A.D.A.M Medical Encyclopedia. (2018, September 25). Common symptoms during pregnancy. Retrieved August 22, 2020. https://medlineplus.gov/ency/patientinstructions/000583.htm
12.
Tsai, S. Y., Lee, P. L., & Lee, C. N. (2018). Snoring and Blood Pressure in Third-Trimester Normotensive Pregnant Women. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing, 50(5), 522–529. https://doi.org/10.1111/jnu.12416
13.
Facco, F. L., Parker, C. B., Reddy, U. M., Silver, R. M., Koch, M. A., Louis, J. M., Basner, R. C., Chung, J. H., Nhan-Chang, C. L., Pien, G. W., Redline, S., Grobman, W. A., Wing, D. A., Simhan, H. N., Haas, D. M., Mercer, B. M., Parry, S., Mobley, D., Hunter, S., Saade, G. R., … Zee, P. C. (2017). Association Between Sleep-Disordered Breathing and Hypertensive Disorders of Pregnancy and Gestational Diabetes Mellitus. Obstetrics and gynecology, 129(1), 31–41. https://doi.org/10.1097/AOG.0000000000001805
N., Haas, D. M., Mercer, B. M., Parry, S., Mobley, D., Hunter, S., Saade, G. R., … Zee, P. C. (2017). Association Between Sleep-Disordered Breathing and Hypertensive Disorders of Pregnancy and Gestational Diabetes Mellitus. Obstetrics and gynecology, 129(1), 31–41. https://doi.org/10.1097/AOG.0000000000001805
14.
Louis, J. M., Mogos, M. F., Salemi, J. L., Redline, S., & Salihu, H. M. (2014). Obstructive sleep apnea and severe maternal-infant morbidity/mortality in the United States, 1998-2009. Sleep, 37(5), 843–849. https://doi.org/10.5665/sleep.3644
15.
Reutrakul, S., Zaidi, N., Wroblewski, K., Kay, H. H., Ismail, M., Ehrmann, D. A., & Van Cauter, E. (2013). Interactions between pregnancy, obstructive sleep apnea, and gestational diabetes mellitus. The Journal of clinical endocrinology and metabolism, 98(10), 4195–4202. https://doi.org/10.1210/jc.2013-2348
16.
Dunietz, G. L., Lisabeth, L. D., Shedden, K.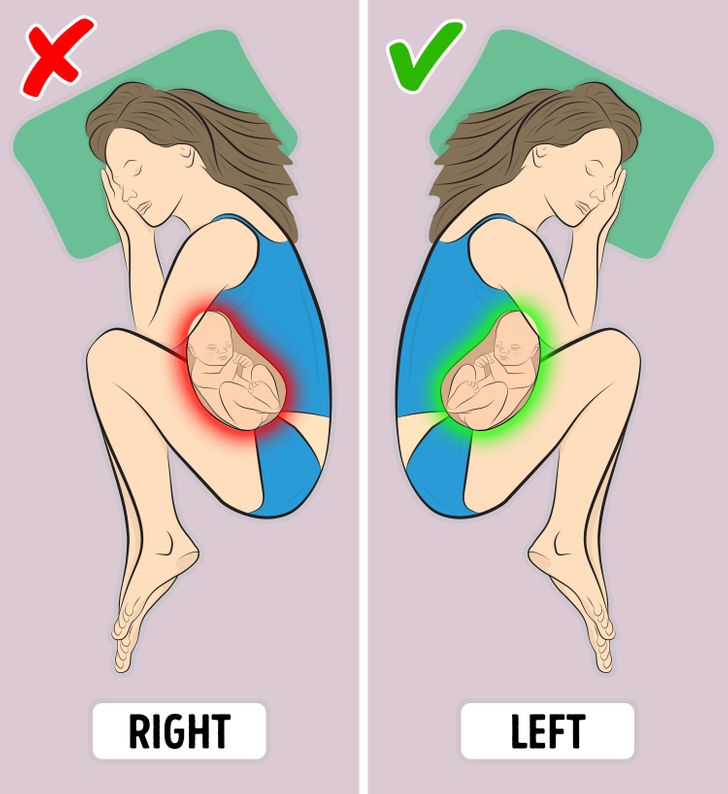 , Shamim-Uzzaman, Q. A., Bullough, A. S., Chames, M. C., Bowden, M. F., & O'Brien, L. M. (2017). Restless Legs Syndrome and Sleep-Wake Disturbances in Pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 13(7), 863–870. https://doi.org/10.5664/jcsm.6654
, Shamim-Uzzaman, Q. A., Bullough, A. S., Chames, M. C., Bowden, M. F., & O'Brien, L. M. (2017). Restless Legs Syndrome and Sleep-Wake Disturbances in Pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 13(7), 863–870. https://doi.org/10.5664/jcsm.6654
17.
Hall, H., Lauche, R., Adams, J., Steel, A., Broom, A., & Sibbritt, D. (2016). Healthcare utilisation of pregnant women who experience sciatica, leg cramps and/or varicose veins: A cross-sectional survey of 1835 pregnant women. Women and birth : journal of the Australian College of Midwives, 29(1), 35–40. https://doi.org/10.1016/j.wombi.2015.07.184
18.
Felder, J. N., Baer, R. J., Rand, L., Jelliffe-Pawlowski, L. L., & Prather, A. A. (2017). Sleep Disorder Diagnosis During Pregnancy and Risk of Preterm Birth. Obstetrics and gynecology, 130(3), 573–581. https://doi.org/10.1097/AOG.0000000000002132
19.
Okun, M. L., & O'Brien, L. M. (2018). Concurrent insomnia and habitual snoring are associated with adverse pregnancy outcomes. Sleep medicine, 46, 12–19. https://doi.org/10.1016/j.sleep.2018.03.004
20.
Liu, H., Li, H., Li, C., Chen, L., Zhang, C., Liu, Z., Wu, Y., & Huang, H. (2019). Associations between Maternal Sleep Quality Throughout Pregnancy and Newborn Birth Weight. Behavioral sleep medicine, 1–13. Advance online publication. https://doi.org/10.1080/15402002.2019.1702551
21.
Lee, K. A., & Gay, C. L. (2004). Sleep in late pregnancy predicts length of labor and type of delivery. American journal of obstetrics and gynecology, 191(6), 2041–2046. https://doi.org/10.1016/j.ajog.2004.05.086
22.
Cai, S., Tan, S., Gluckman, P. D., Godfrey, K. M., Saw, S. M., Teoh, O. H., Chong, Y. S., Meaney, M. J., Kramer, M. S., Gooley, J. J., & GUSTO study group (2017). Sleep Quality and Nocturnal Sleep Duration in Pregnancy and Risk of Gestational Diabetes Mellitus. Sleep, 40(2), 10.1093/sleep/zsw058. https://doi.org/10.1093/sleep/zsw058
Sleep, 40(2), 10.1093/sleep/zsw058. https://doi.org/10.1093/sleep/zsw058
23.
Casey, T., Sun, H., Burgess, H. J., Crodian, J., Dowden, S., Cummings, S., Plaut, K., Haas, D., Zhang, L., & Ahmed, A. (2019). Delayed Lactogenesis II is Associated With Lower Sleep Efficiency and Greater Variation in Nightly Sleep Duration in the Third Trimester. Journal of human lactation : official journal of International Lactation Consultant Association, 35(4), 713–724. https://doi.org/10.1177/0890334419830991
24.
Tsai, S. Y., Lin, J. W., Wu, W. W., Lee, C. N., & Lee, P. L. (2016). Sleep Disturbances and Symptoms of Depression and Daytime Sleepiness in Pregnant Women. Birth (Berkeley, Calif.), 43(2), 176–183. https://doi.org/10.1111/birt.12215
25.
Wu, M., Li, X., Feng, B., Wu, H., Qiu, C., & Zhang, W. (2014). Poor sleep quality of third-trimester pregnancy is a risk factor for postpartum depression. Medical science monitor : international medical journal of experimental and clinical research, 20, 2740–2745. https://doi.org/10.12659/MSM.891222
https://doi.org/10.12659/MSM.891222
26.
Rossi, A., Cornette, J., Johnson, M. R., Karamermer, Y., Springeling, T., Opic, P., Moelker, A., Krestin, G. P., Steegers, E., Roos-Hesselink, J., & van Geuns, R. J. (2011). Quantitative cardiovascular magnetic resonance in pregnant women: cross-sectional analysis of physiological parameters throughout pregnancy and the impact of the supine position. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance, 13(1), 31. https://doi.org/10.1186/1532-429X-13-31
27.
Warland, J., Dorrian, J., Kember, A. J., Phillips, C., Borazjani, A., Morrison, J. L., & O'Brien, L. M. (2018). Modifying Maternal Sleep Position in Late Pregnancy Through Positional Therapy: A Feasibility Study. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 14(8), 1387–1397. https://doi.org/10.5664/jcsm.7280
28.
Effati-Daryani, F., Mohammad-Alizadeh-Charandabi, S., Mirghafourvand, M., Taghizadeh, M., Bekhradi, R., & Zarei, S. (2018). Effect of Lavender cream with or without footbath on sleep quality and fatigue in pregnancy and postpartum: a randomized controlled trial. Women & health, 58(10), 1179–1191. https://doi.org/10.1080/03630242.2017.1414101
29.
Lee, K. A., Zaffke, M. E., & Baratte-Beebe, K. (2001). Restless legs syndrome and sleep disturbance during pregnancy: the role of folate and iron. Journal of women's health & gender-based medicine, 10(4), 335–341. https://doi.org/10.1089/152460901750269652
30.
Quach, D. T., Le, Y. T., Mai, L. H., Hoang, A. T., & Nguyen, T. T. (2020). Short Meal-to-Bed Time Is a Predominant Risk Factor of Gastroesophageal Reflux Disease in Pregnancy. Journal of clinical gastroenterology, 10.1097/MCG.0000000000001399. Advance online publication. https://doi.org/10.1097/MCG.0000000000001399
31.
Carnelio, S., Morton, A., & McIntyre, H. D. (2017). Sleep disordered breathing in pregnancy: the maternal and fetal implications. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology, 37(2), 170–178. https://doi.org/10.1080/01443615.2016.1229273
32.
The American College of Obstetricians and Gynecologists. (2019, July). Exercise During Pregnancy. Retrieved August 22, 2020. https://www.acog.org/patient-resources/faqs/pregnancy/exercise-during-pregnancy
33.
Bei, B., Milgrom, J., Ericksen, J., & Trinder, J. (2010). Subjective perception of sleep, but not its objective quality, is associated with immediate postpartum mood disturbances in healthy women. Sleep, 33(4), 531–538. https://doi.org/10.1093/sleep/33.4.531
34.
Lee, K. A., & Gay, C. L. (2017). Improving Sleep for Hospitalized Antepartum Patients: A Non-Randomized Controlled Pilot Study. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 13(12), 1445–1453.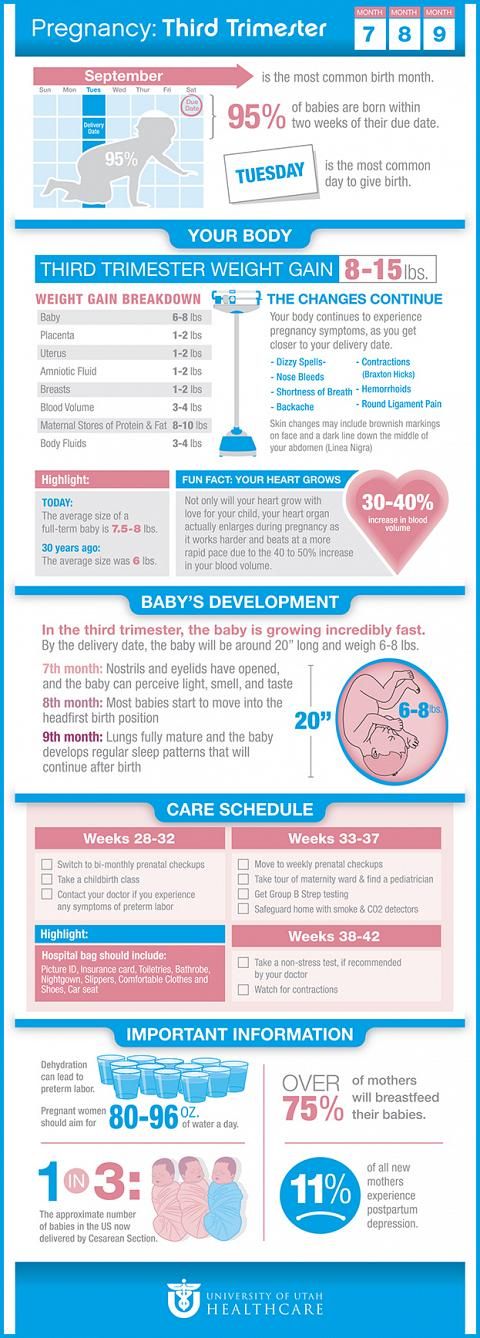 https://doi.org/10.5664/jcsm.6846
https://doi.org/10.5664/jcsm.6846
How to sleep during pregnancy
It is difficult to overestimate the role of sleep in the life of every person. A complete healthy rest allows you to fully restore the functioning of the nervous system, relieve stress, improve performance and increase activity. Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
The cause of insomnia can be :
- Anxiety;
- Frequent urination;
- Fears and phobias before a new stage of one's life;
- Nervousness and irritability;
- Digestive disorder;
- Toxicosis;
- Physical indisposition;
- Uncomfortable posture.

During the period of bearing a child, the female body experiences an extraordinary load, especially in the last trimester. The need for more sleep increases, because the body expends much more energy. Therefore, healthy sleep and pregnancy are inextricably linked.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
Let's try to figure out how to sleep during pregnancy, so as not only not to harm the health of your unborn baby, but to sleep well.
Looking for a comfortable sleeping position
Each person has his own favorite position, in which it is easy to fall asleep and sleep. Many do not imagine a comfortable rest on their backs, accustomed to sleeping on their stomachs. This habit will have to be sacrificed, as it is unsafe for the normal development of the fetus.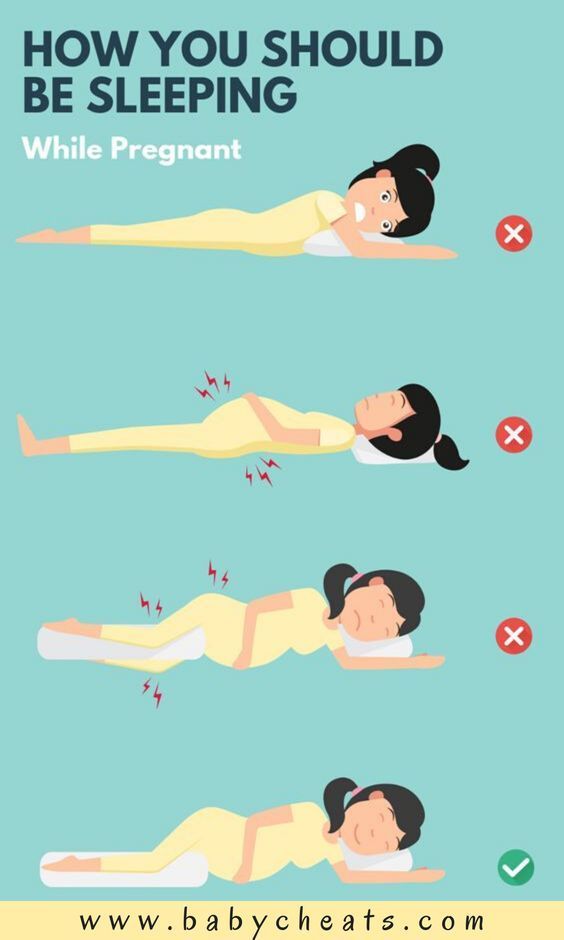 If in the first three months of pregnancy a woman can still sleep in the position in which she is used to and feels comfortable, then after the first trimester the growing belly will not allow her to lie safely in this position. Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
If in the first three months of pregnancy a woman can still sleep in the position in which she is used to and feels comfortable, then after the first trimester the growing belly will not allow her to lie safely in this position. Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
Back position
Even if you are used to sleeping in a Spartan position, on your back, with your arms spread wide, from the 28th week you will have to radically change your lifestyle. The fact is that as the fetus grows, the load on the intestines and vena cava will increase significantly, blocking the access of oxygen to the baby.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
If you sleep on your back during pregnancy, you may experience the following problems:
- Dizziness;
- Nausea;
- Convulsions;
- Numb limbs;
- Pressure reduction;
- Hemorrhoids;
- Heaviness of breathing.
If you feel these symptoms or the baby gives persistent signals, you need to urgently change your position, so squeezing the vena cava is fraught not only with poor health for the mother, but also with a lack of oxygen supply to the fetus.
Stomach position
One of the most beloved positions for many people, which allows you to quickly fall asleep while hugging a pillow. Many women, as soon as they find out about the change in their lives, are interested in the question, is it possible to sleep on your stomach during pregnancy? Doctors recommend abandoning this position already in the first weeks, even before the enlarged belly makes it impossible to fall asleep peacefully.
If you are afraid during sleep, without controlling your movements, to arbitrarily roll over on your stomach, you can put a large pillow that does not allow you to change position.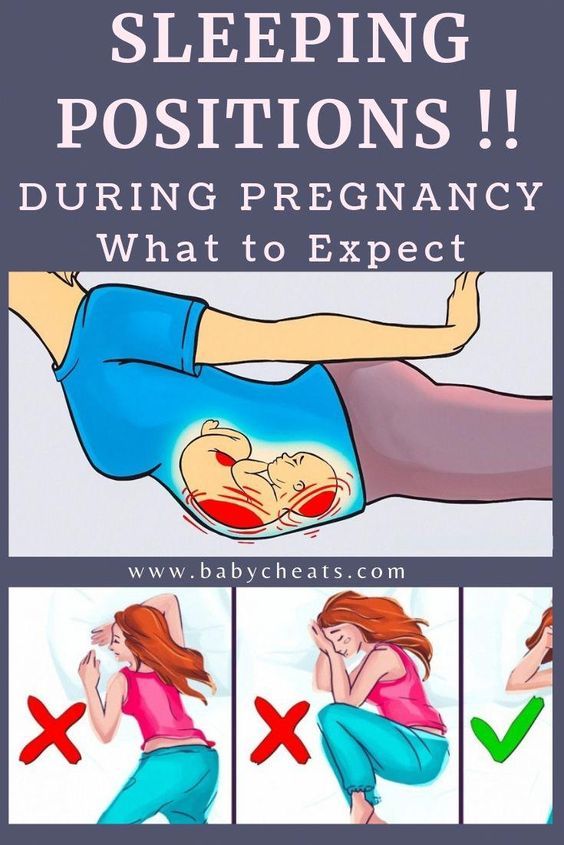
Side position
In order to normalize your sleep and not harm the health of the baby, experts recommend sleeping on your side during pregnancy. And if at first this option seems unacceptable to many, after the second trimester, lying on your side is the only possible one. But here the question arises, on which side to sleep in order to ensure the safety of the fetus?
Sleeping on the right side can cause squeezing of the kidney, which can have dire consequences. The ideal posture is lying on the left side. Thus, you not only do not injure the unborn baby, but also improve blood flow along with oxygen to the placenta.
But one should not ignore the individual characteristics of each organism and the position of the fetus in the uterus. When the baby is in a transverse position, choose the side where the baby's head is. And with a breech presentation, doctors recommend changing the position several times a night.
If you still cannot improve your sleep, you feel unwell and you are tormented by insomnia, then it is better to consult a specialist.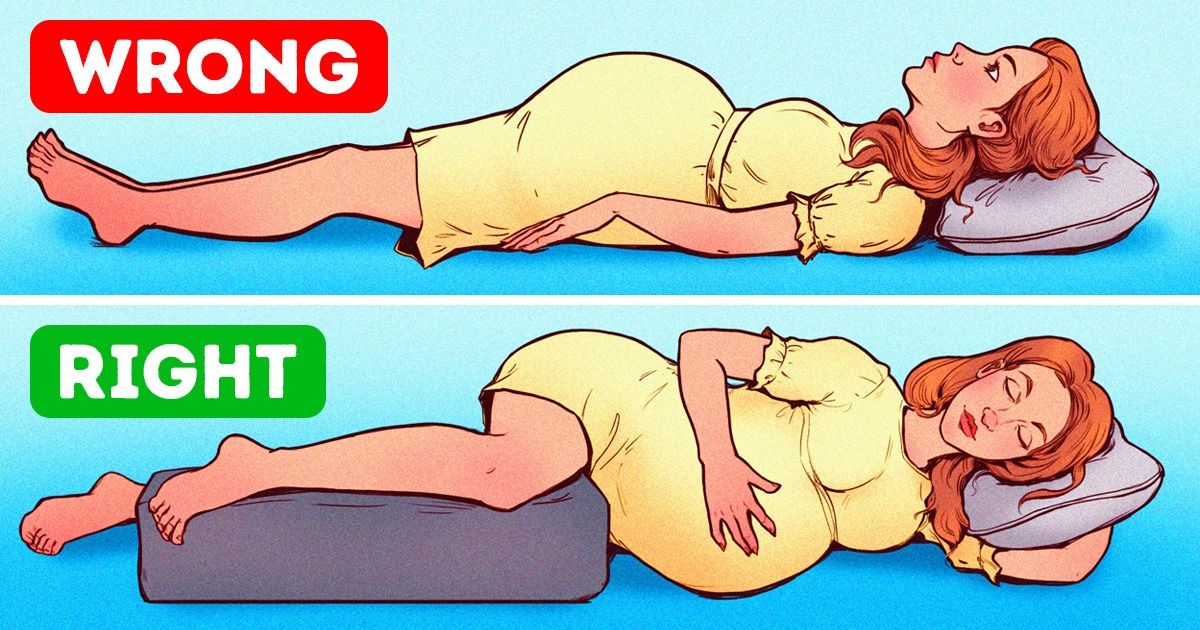 A good gynecologist will analyze the situation and help solve the problem. If necessary, he will prescribe a safe sedative that stabilizes the emotional state and helps to fall asleep calmly, resting and restoring the nervous system in a dream.
A good gynecologist will analyze the situation and help solve the problem. If necessary, he will prescribe a safe sedative that stabilizes the emotional state and helps to fall asleep calmly, resting and restoring the nervous system in a dream.
Help pillow
Fortunately, now modern manufacturers help women survive the pregnancy period with great comfort by offering special pillows. They are made taking into account the physiological characteristics of a woman in this period and allow you to find a comfortable position for relaxation.
You can buy two pillows and put one under your stomach and the other under your knees, looking for your best option. And you can buy a long banana-shaped pillow, which allows you to throw your leg on it while sleeping, which improves well-being and relieves the main load from the lower back and abdomen. Already in the last weeks of pregnancy, when the growing belly does not allow you to breathe normally, the pillow will allow you to take a comfortable half-sitting position.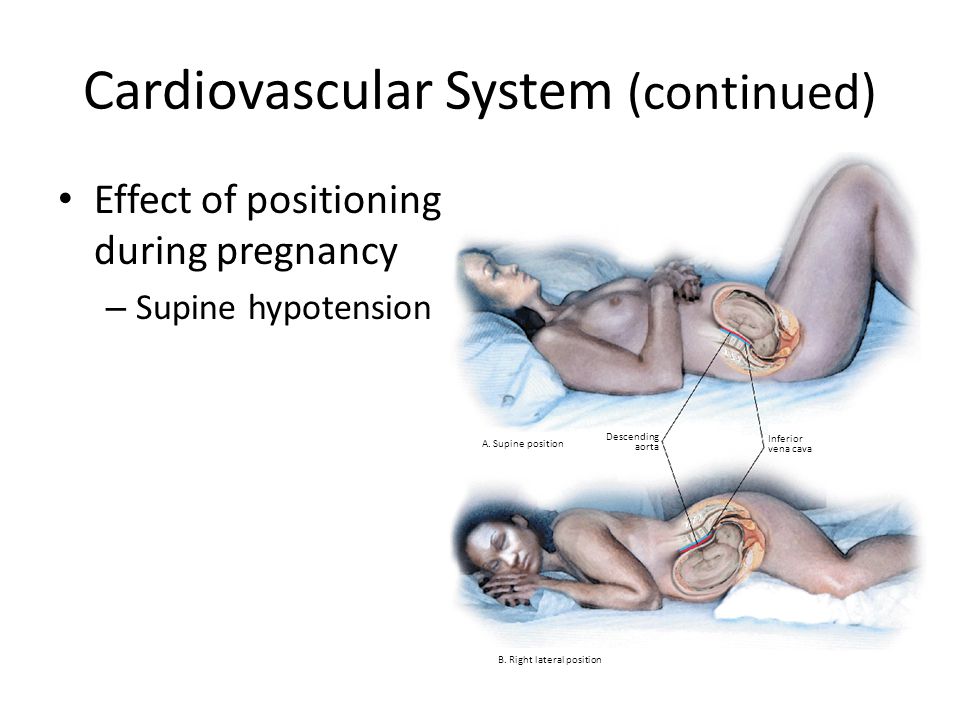
Remember that pregnancy is your opportunity to gain strength and fully relax before the most crucial period in your life. Childbirth and the first weeks of caring for your baby will require a lot of energy from you, so good luck and sound sleep!
Comfortable Sleep Positions During Pregnancy
Pregnant women often have difficulty falling asleep. Firstly, because of the state of health, which is far from always normal. Secondly, because of the restlessness of the child, who is increasingly making itself felt. And thirdly, the stomach grows and it becomes more and more difficult to find a comfortable position for sleeping. There are special pillows for pregnant women, which are designed to help women in this situation. Do they really help? Maybe ordinary pillows are also suitable? Let's figure it out.
For those who like to sleep on their stomach, the difficulties will begin already in the first trimester. At this time, the chest begins to increase significantly in size and makes it difficult to sleep in the usual position.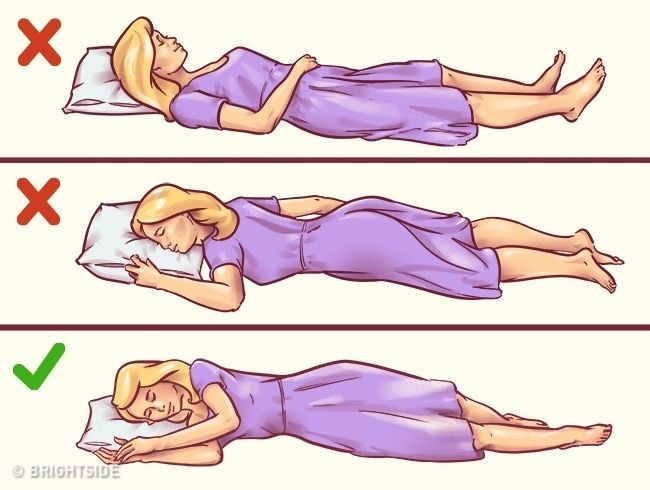 In the second trimester, it's time to get used to sleeping on your side, otherwise an enlarged and heavier belly can negatively affect blood circulation. The ideal position is to sleep on your left side. But in the third trimester, a woman will still have a hard time, even if she always sleeps on her left side, because the considerable weight of the abdomen, combined with the weakness of the joints - because the body is preparing for the process of childbirth - is likely to provoke great inconvenience and pain.
In the second trimester, it's time to get used to sleeping on your side, otherwise an enlarged and heavier belly can negatively affect blood circulation. The ideal position is to sleep on your left side. But in the third trimester, a woman will still have a hard time, even if she always sleeps on her left side, because the considerable weight of the abdomen, combined with the weakness of the joints - because the body is preparing for the process of childbirth - is likely to provoke great inconvenience and pain.
It is during this period that many people think about a special pillow for pregnant women and the question of choice arises. But how do you know which of them can really provide convenience for you?
How to choose the right maternity pillow before buying it online
To start with, we recommend experimenting with regular pillows you have at home. Place them under your head and neck, as well as between your knees, lying on your left side. You can also adjust the pillow under the stomach to support the weight and ease the load on the spine.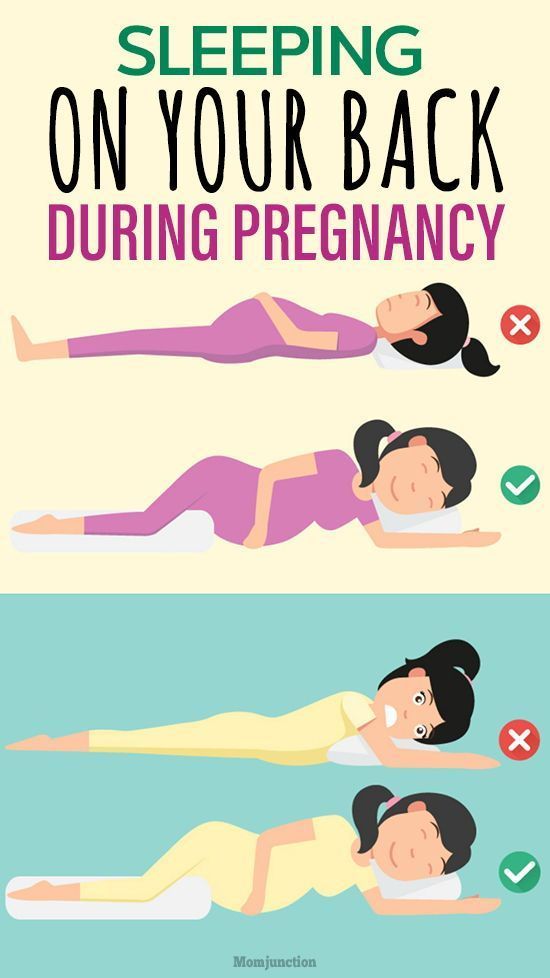 If you find it difficult to get used to sleeping on your left side, put a pillow under your back as well, it will serve as a barrier if you want to roll over in a dream. It is possible that the pillows available at home will do the job perfectly, and you do not have to buy a special one.
If you find it difficult to get used to sleeping on your left side, put a pillow under your back as well, it will serve as a barrier if you want to roll over in a dream. It is possible that the pillows available at home will do the job perfectly, and you do not have to buy a special one.
If regular pillows aren't comfortable, you'll be surprised at the variety of maternity bedding options. Some women like large square pillows that can be placed between the legs and support the stomach. Others prefer small wedge-shaped ones that are placed just under the stomach and thus flatten the entire body. And there are huge pillows-rollers in the form of a semicircle that cover the entire body. They simultaneously serve as a support for the back and abdomen, are conveniently located between the knees and support the head. They look the most comfortable of all, but still take your time with the purchase.
Things to consider before choosing a pregnancy pillow
Your own body will help you make the right choice.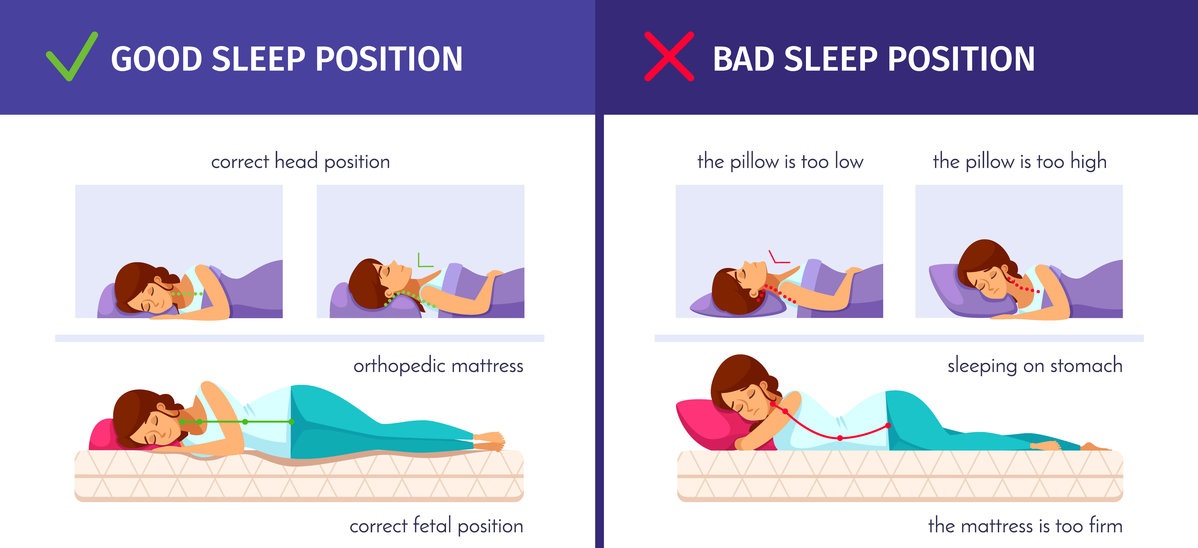 Think about how you usually sleep and what, in fact, you have difficulty. For example, if you usually lie on your back, then the same cushion-roller that supports both your back and stomach will suit you. But if you do not like the abundance of blankets and pillows on the bed, such a huge pillow will annoy you. Pay attention to smaller items. The advice of friends who have passed this period will be very useful. Perhaps one of them has used one or another pregnancy pillow, and you can try it out before buying.
Think about how you usually sleep and what, in fact, you have difficulty. For example, if you usually lie on your back, then the same cushion-roller that supports both your back and stomach will suit you. But if you do not like the abundance of blankets and pillows on the bed, such a huge pillow will annoy you. Pay attention to smaller items. The advice of friends who have passed this period will be very useful. Perhaps one of them has used one or another pregnancy pillow, and you can try it out before buying.
Now let's talk about sleeping positions. For a pregnant woman, this is a very relevant issue, because her task is not only to get enough sleep herself, but also not to harm the child. First of all, avoid sleeping on your back from the beginning of your pregnancy. In the first trimester, it is safe, but it is better to start weaning this habit now, because in the future, the increasing weight of the abdomen will put pressure on the blood vessels and interfere with blood circulation, you will wake up with dizziness.