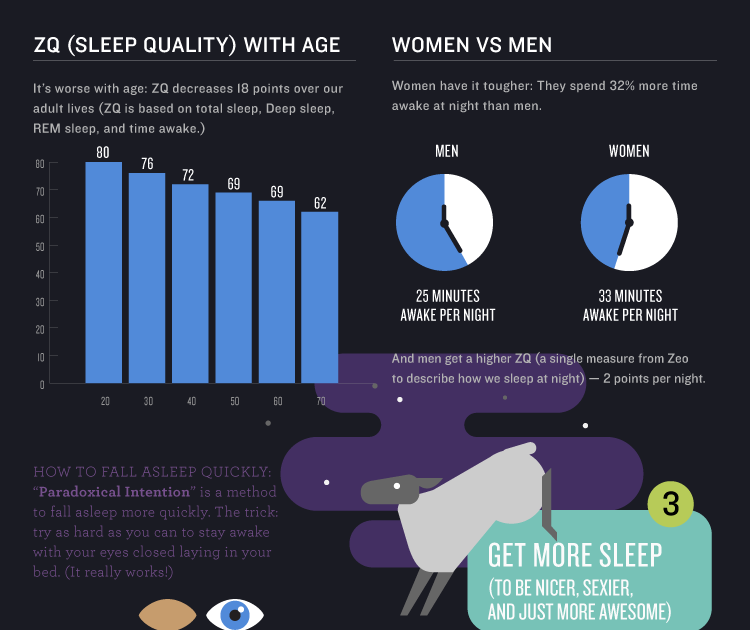
Sleep amount by age
Sleep Disorders – Common Types, Symptoms, Treatments
Sleep Disorders – Common Types, Symptoms, Treatments | Sleep Foundation Skip to contentWhat they are, their causes and symptoms, and how people with sleep disorders can get relief
Written by
Danielle Pacheco, Staff Writer Danielle Pacheco Staff Writer Danielle writes in-depth articles about sleep solutions and holds a psychology degree from the University of British Columbia. Read Full Bio Want to read more about all our experts in the field? Learn About The Editorial Team
Medically Reviewed by
Dr. Dr. Anis Rehman Endocrinologist Dr. Rehman, M.D., is a board-certified physician in Internal Medicine as well as Endocrinology, Diabetes, and Metabolism. Read Full Bio Want to read more about all our experts in the field? Learn About The Editorial Team Anis Rehman, Endocrinologist
The collective term sleep disorder refers to conditions that affect sleep quality, timing, or duration and impact a person’s ability to properly function while they are awake. These disorders can contribute to other medical problems, and some may also be symptoms for underlying mental health issues.
In 1979, the American Sleep Disorders Association published the first classification system dedicated to sleep disorders. Our knowledge and understanding of sleep health has evolved over the past four decades. More than 100 specific sleep disorders have been identified and today’s classifications use complex methodologies to categorize these disorders based on causes, symptoms, physiological and psychological effects, and other criteria. However, most sleep disorders can be characterized by one or more of the following four signs:
- You have trouble falling or remaining asleep
- You find it difficult to stay awake during the day
- There are imbalances in your circadian rhythm that interfere with a healthy sleep schedule
- You are prone to unusual behaviors that disrupt your sleep
Any of these signs could indicate a sleep disorder. We encourage people who experience any of these issues to consult with their doctor.
Visit the pages below to learn more about different sleep disorders.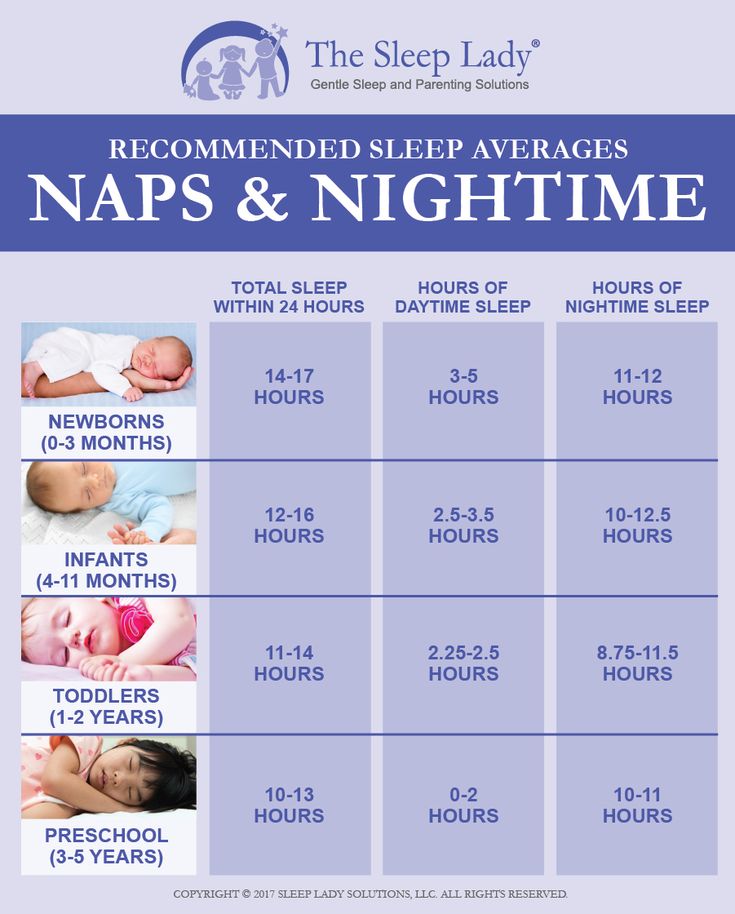 Our list of sleep disorders is based on categories in the American Academy of Sleep Medicine’s International Classification of Sleep Disorders – Third Edition (ICSD-3).
Our list of sleep disorders is based on categories in the American Academy of Sleep Medicine’s International Classification of Sleep Disorders – Third Edition (ICSD-3).
Most Researched Sleep Disorders
More Sleep DisordersInsomnia
Sleep Apnea
Narcolepsy
Restless Leg Syndrome (RLS)
Parasomnias
REM Sleep Behavior Disorder
Non-24-Hour Sleep Wake Disorder
Excessive Sleepiness
Shift Work Disorder
Periodic Limb Movement Disorder
Looking for Something Specific?
Learn More
Insomnia is characterized by the recurring difficulty to fall or remain asleep despite motivation and means to do so. People with insomnia also experience excessive daytime sleepiness and other cognitive impairments while they are awake. Insomnia is considered a chronic condition when patients exhibit symptoms at least three times per week for at least three months. Based on recent statistics, up to one-third of adults live with some form of insomnia.
Insomnia is considered a chronic condition when patients exhibit symptoms at least three times per week for at least three months. Based on recent statistics, up to one-third of adults live with some form of insomnia.
- Sleep-onset insomnia occurs when people have difficulty falling asleep, even when they are tired.
- Sleep maintenance insomnia refers to difficulty staying asleep during the night.
- Mixed insomnia is a hybrid condition characterized by sleep-onset and sleep maintenance insomnia symptoms.
Articles about Insomnia
Medically Reviewed by Dr. Abhinav Singh
Abhinav Singh
Medically Reviewed byAlex Dimitriu
Medically Reviewed byAlex Dimitriu
Insomnia
Treatments for Insomnia
Want to learn more about how to treat insomnia? Our insomnia treatment guide covers medications, cognitive behavioral therapy for insomnia,…
Learn More
Sleep apnea is a common sleep-related breathing disorder that occurs due to blockage of the upper airway. People with this condition often wake up choking or gasping for air. Heavy snoring is another common symptom. Like other sleep disorders, sleep apnea can cause excessive daytime sleepiness and fatigue, as well as various cognitive impairments. Most sleep apnea cases fall into one of the following two categories.
Like other sleep disorders, sleep apnea can cause excessive daytime sleepiness and fatigue, as well as various cognitive impairments. Most sleep apnea cases fall into one of the following two categories.
- Obstructive sleep apnea (OSA) is caused by a physical obstruction that blocks the upper airway. This obstruction may be attributed to large tonsils or adenoids, fluid buildup from advanced heart or kidney failure, or genetic syndromes that affect facial structure such as cleft palate. Obese people with fat deposits around their neck are also at higher risk of OSA, and back sleeping can lead to apnea episodes if the tongue falls back into the throat. For many patients, continuous positive air pressure (CPAP) therapy is the most effective treatment
- Central Sleep Apnea occurs when the brain stops sending signals to the muscles that control breathing, leading to choking episodes during the night.
 As with OSA, obesity is a common risk factor for CSA. The condition may also affect people who have experienced a stroke, brain infection, and other medical problems with the brain stem, as well as those who take narcotic painkillers and other sleep-inducing medications. CPAP therapy is often prescribed for CSA, though some patients find bi-level positive air pressure (BiPAP) therapy more effective.
As with OSA, obesity is a common risk factor for CSA. The condition may also affect people who have experienced a stroke, brain infection, and other medical problems with the brain stem, as well as those who take narcotic painkillers and other sleep-inducing medications. CPAP therapy is often prescribed for CSA, though some patients find bi-level positive air pressure (BiPAP) therapy more effective.
Articles about Sleep Apnea
Medically Reviewed by Dr. Abhinav Singh
CPAP Sleep Apnea Sleep Disorders Sleep Topics
How to Use a CPAP Machine for Better Sleep
Are you about to start using a CPAP machine for sleep apnea? We outline the steps for using your CPAP…
Medically Reviewed byKimberly Truong
Medically Reviewed byJohn DeBanto
Learn More
Narcolepsy is a sleep disorder that makes people feel excessively tired during the day despite getting an adequate amount of rest the previous night. This can lead to the irrepressible urge to sleep, culminating in “sleep attacks” that typically last for a few minutes. Over time, narcolepsy can also cause sleep-onset and sleep maintenance problems. The condition known as Narcolepsy Type 1 often includes cataplexy, or a sudden loss of muscle tone that causes people to fall or slump over as they nod off. Sleep attacks also occur with Narcolepsy Type 2, but cataplexy is not present. Narcolepsy affects roughly 1 in 2,000 people in the U.S. and Europe.
This can lead to the irrepressible urge to sleep, culminating in “sleep attacks” that typically last for a few minutes. Over time, narcolepsy can also cause sleep-onset and sleep maintenance problems. The condition known as Narcolepsy Type 1 often includes cataplexy, or a sudden loss of muscle tone that causes people to fall or slump over as they nod off. Sleep attacks also occur with Narcolepsy Type 2, but cataplexy is not present. Narcolepsy affects roughly 1 in 2,000 people in the U.S. and Europe.
Articles about Narcolepsy
Medically Reviewed by John DeBanto
How Sleep Works Narcolepsy Sleep Disorders Sleep Topics
Narcolepsy Treatment
Can narcolepsy be cured? Can its symptoms be improved? Learn about the different types of treatment for narcolepsy and their…
Medically Reviewed byDr.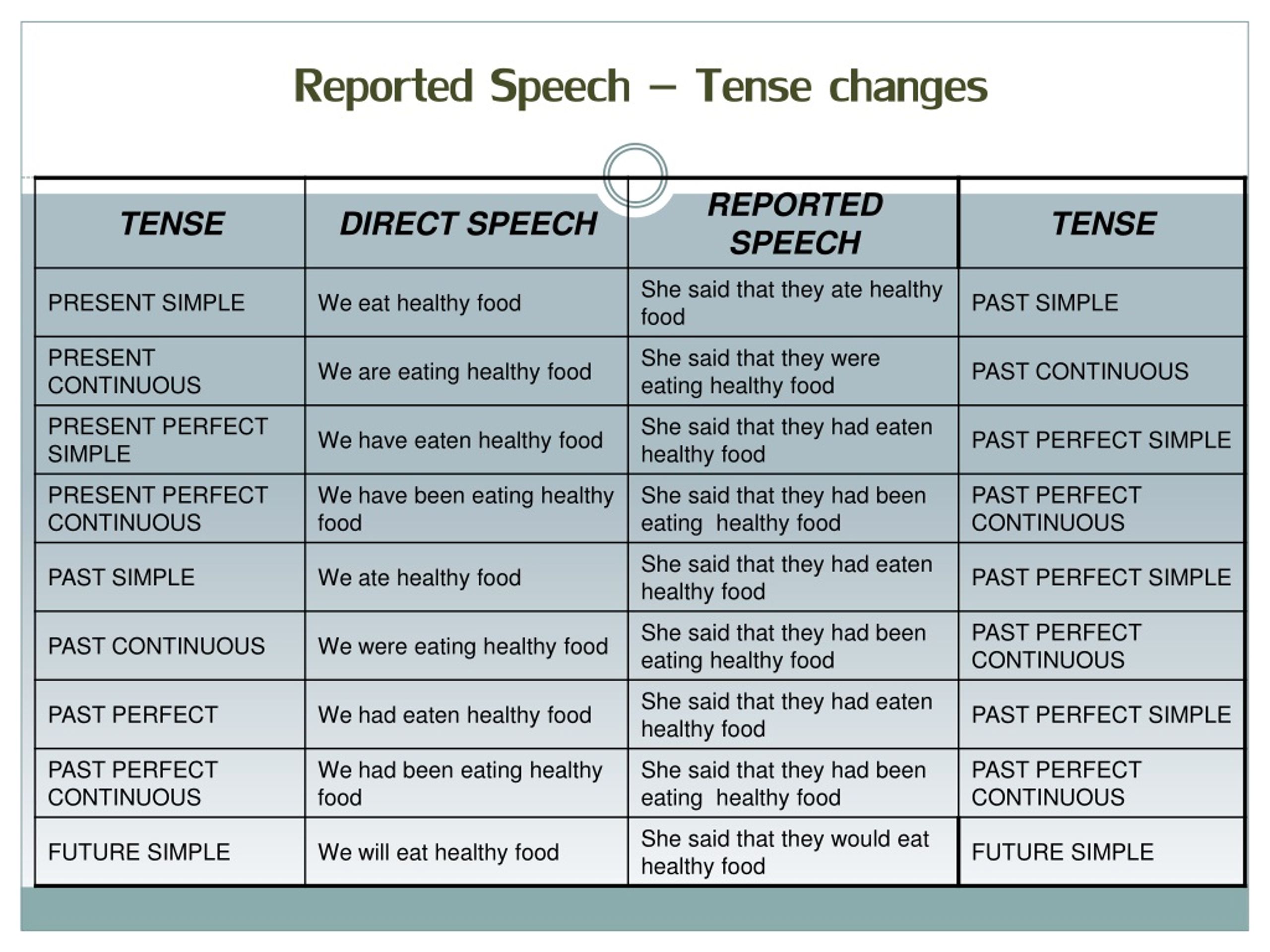 Anis Rehman
Anis Rehman
How Sleep Works Narcolepsy Sleep Disorders Sleep Topics
Diagnosing Narcolepsy
Concerned that you have symptoms of narcolepsy? Learn about the tests and criteria used to diagnose narcolepsy and how to…
Medically Reviewed byDr. Anis Rehman
How Sleep Works Narcolepsy Sleep Disorders Sleep Topics
Narcolepsy Symptoms
Our guide to the symptoms of narcolepsy explores the causes and impact of each symptom of this complex, chronic sleep…
Learn More
RLS is a type of sleep-related movement disorder that affects 7-10% of the U.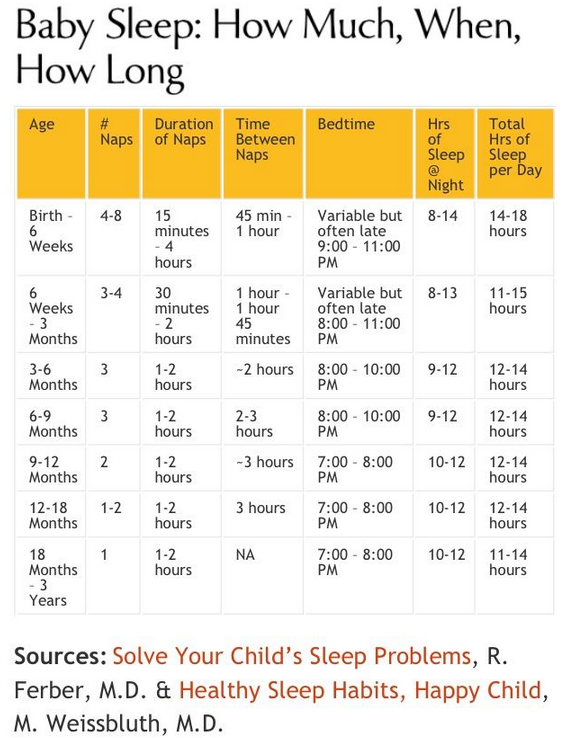 S. population. Also known as Willis-Ekbom Disease, RSL is characterized by throbbing, itching, and other painful sensations in the legs and powerful urges to move the legs while they are at rest. People with RLS typically experience the strongest symptoms in bed, putting them at an increased risk for sleep-onset and sleep maintenance problems. There is no cure for RLS, though lifestyle changes, moderate exercise, and nighttime stretching can help some patients manage their symptoms.
S. population. Also known as Willis-Ekbom Disease, RSL is characterized by throbbing, itching, and other painful sensations in the legs and powerful urges to move the legs while they are at rest. People with RLS typically experience the strongest symptoms in bed, putting them at an increased risk for sleep-onset and sleep maintenance problems. There is no cure for RLS, though lifestyle changes, moderate exercise, and nighttime stretching can help some patients manage their symptoms.
Articles about Restless Leg Syndrome
Medically Reviewed by Heather Wright
Medically Reviewed byHeather Wright
Medically Reviewed byHeather Wright
Learn More
EDS is defined by feelings of intense grogginess during the day that can compel people to sleep at inopportune times. People who feel excessively groggy during the day may also be more prone to errors and accidents. A wide range of medical and psychological conditions can lead to EDS, such as diabetes, hypothyroidism, chronic pain, depression, and anxiety. Other causes include certain sleep disorders like sleep apnea and periodic limb movement disorder. EDS is believed to affect up to 18% of the population.
People who feel excessively groggy during the day may also be more prone to errors and accidents. A wide range of medical and psychological conditions can lead to EDS, such as diabetes, hypothyroidism, chronic pain, depression, and anxiety. Other causes include certain sleep disorders like sleep apnea and periodic limb movement disorder. EDS is believed to affect up to 18% of the population.
Articles about Excessive Sleepiness
Medically Reviewed by Dr. Abhinav Singh
Medically Reviewed byDr. Abhinav Singh
Medically Reviewed byDr. Anis Rehman
Anis Rehman
Excessive Sleepiness How Sleep Works Sleep Disorders Sleep Topics
Causes of Excessive Sleepiness
Learn what may be causing your excessive sleepiness. It could be an underlying cause like a sleep disorder, psychiatric illness,…
Learn More
Shift work disorder primarily affects people whose jobs require them to work late at night or early in the morning. Sleeping during the day and working at night can cause misalignment between a person’s body and the circadian rhythms that guide their sleep-wake schedule based on natural light and darkness cycles. People with this condition often feel excessively tired at work and struggle to get enough sleep during their allotted daytime rest period.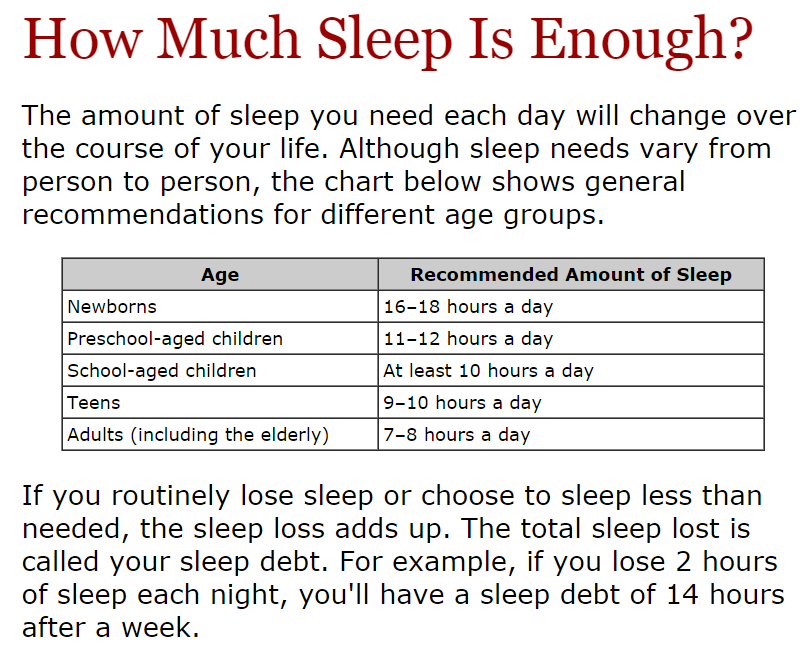 Up to 32% of night shift workers and 26% of rotating shift workers meet the diagnostic criteria for shift work disorder.
Up to 32% of night shift workers and 26% of rotating shift workers meet the diagnostic criteria for shift work disorder.
Articles about Shift Work Disorder
Medically Reviewed by Joshua Tal
Medically Reviewed byDr. Abhinav Singh
Learn More
Parasomnias are a group of unusual sleep behaviors that can occur before falling sleep, during sleep, or in the time between sleep and wakefulness. These are more commonly found in children, but some adults may experience them as well. These include sleepwalking, bedwetting, night terrors, and more unique ones like exploding head syndrome.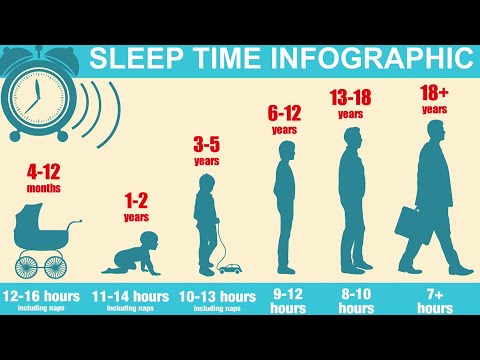 Parasomnias are broken down into three categories: NREM-related parasomnias, REM-related parasomnias, and other.
Parasomnias are broken down into three categories: NREM-related parasomnias, REM-related parasomnias, and other.
Articles about Parasomnias
Medically Reviewed by Dr. Nilong Vyas
Medically Reviewed byDr. Nilong Vyas
Medically Reviewed byAlex Dimitriu
Learn More
For most adults, the circadian rhythms that guide their sleep-wake cycle and other bodily processes will reset every 24 hours. The condition known as non 24-hours sleep wake disorder occurs when someone’s circadian cycle exceeds the 24-hour mark. These individuals often experience delays of one to two hours in their sleep-onset and waking times. This disorder primarily affects those who are totally blind and people with dementia.
These individuals often experience delays of one to two hours in their sleep-onset and waking times. This disorder primarily affects those who are totally blind and people with dementia.
Articles about Non 24-Hour Sleep Wake Disorder
Medically Reviewed by Dr. Abhinav Singh
Medically Reviewed byDr. Anis Rehman
Medically Reviewed byHeather Wright
Additional Information on Sleep Disorders
According to general estimates, 10-30% of adults live with some form of insomnia. The condition is defined by a persistent difficulty falling or remaining asleep despite the opportunity and motivation to do so, as daytime impairments associated with lack of sleep. Chronic insomnia occurs when sleepers experience symptoms at least three times per week for at least three months. Insomnia lasting less than three months is known as short-term insomnia.
The condition is defined by a persistent difficulty falling or remaining asleep despite the opportunity and motivation to do so, as daytime impairments associated with lack of sleep. Chronic insomnia occurs when sleepers experience symptoms at least three times per week for at least three months. Insomnia lasting less than three months is known as short-term insomnia.
- Confusional arousals: Those who experience confusional arousals will exhibit confused behavior in bed due to an incomplete arousal from deep sleep. They won’t react to other people who attempt to intervene, and they’ll have little to no memory of the event.
- Sleepwalking: Also known as somnambulism, sleepwalking occurs when people get out of bed and move about while still asleep. Sleepwalkers may remain in their bedrooms, but some travel to other areas in or outside of their residence. Attempting to wake up a sleepwalker can result in aggressive behavior.
- Night terrors: When someone experiences night terrors, they often cry or act out in their sleep but will have little to no memory of the incident after waking.
 Most night terror episodes are brief, but they can last for several minutes in some cases.
Most night terror episodes are brief, but they can last for several minutes in some cases. - Sleep-related sexual abnormal behaviors: People with this condition will display aggressive or uncharacteristic sexual behavior while asleep. As with other parasomnias, those with this condition – also known as “sexsomnia” – will remember very little, if any, of their behavior when they wake up
Parasomnia is a collective term for unusual behaviors that occur prior to sleep, while asleep, or during the transition period between sleep and waking. These behaviors can occur during different sleep cycle stages, as well. Parasomnias that are mostly isolated to the non-rapid eye movement (NREM) sleep stages include the following:
- Confusional arousals: Those who experience confusional arousals will exhibit confused behavior in bed due to an incomplete arousal from deep sleep. They won’t react to other people who attempt to intervene, and they’ll have little to no memory of the event.
- Sleepwalking: Also known as somnambulism, sleepwalking occurs when people get out of bed and move about while still asleep. Sleepwalkers may remain in their bedrooms, but some travel to other areas in or outside of their residence. Attempting to wake up a sleepwalker can result in aggressive behavior.
- Night terrors: When someone experiences night terrors, they often cry or act out in their sleep but will have little to no memory of the incident after waking. Most night terror episodes are brief, but they can last for several minutes in some cases.
- Sleep-related sexual abnormal behaviors: People with this condition will display aggressive or uncharacteristic sexual behavior while asleep. As with other parasomnias, those with this condition – also known as “sexsomnia” – will remember very little, if any, of their behavior when they wake up
Other parasomnias occur during the rapid-eye movement (REM) stage of the sleep cycle, when dreams are most likely to occur.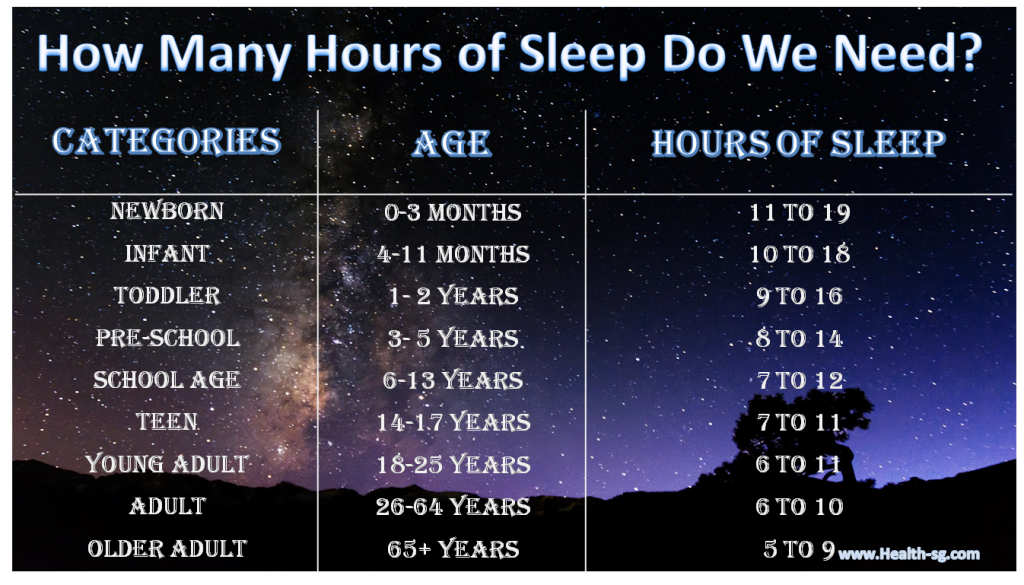 These include:
These include:
- REM sleep behavior disorder: Known as RSBD or RBD for short, REM sleep behavior disorder causes sleepers to physically or vocally act out on their dreams. The behaviors associated with this disorder can disrupt sleep for the individual and their partner, and also put people at higher risk of physical injury.
- Sleep paralysis: Sleep paralysis causes people to feel completely paralyzed as soon as they wake up. This may also occur during sleep onset. Paralysis episodes usually don’t last for more than a few minutes, but this condition can trigger sleep anxiety for some people.
- Nightmare disorder: While isolated nightmares are common for most people, nightmare disorder is defined by vivid, unpleasant dreams that disrupt sleep on a recurrent basis. For some, the nightmares become increasingly disturbing. People with nightmare disorder often experience anxiety about going to bed, as well as post-awakening anxiety when the dream ends.
Lastly, some parasomnias are not isolated to the NREM or REM stages. They may also occur during the transition between sleep and wakefulness
- Exploding head syndrome: As the name implies, people with this condition will imagine loud explosions in their head when they are aroused from sleep. People may physically or vocally act out toward the explosion, but they will not actually feel any pain.
- Sleep-related hallucinations: Some people experience hallucinations during sleep onset or the transition between sleep and waking. These hallucinations can be so vivid for sleepers that they will attempt to leave their bed, putting them at higher risk of injury. The hallucinations may persist for several minutes.
- Sleep enuresis: Also known as bedwetting, sleep enuresis is involuntary urination during sleep. This condition is quite common in young children. However, enuresis is considered a parasomnia for children and adults over the age of five who experience episodes at least twice a week for at least three months.
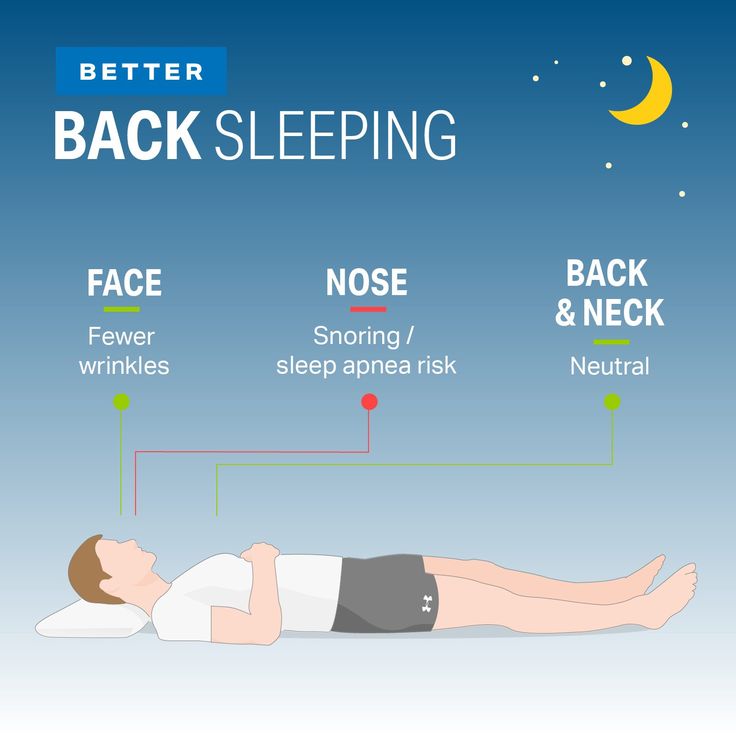
These disorders are characterized by abnormal breathing during sleep. For some, the individual will also experience abnormal breathing while they are awake. Some breathing disorders are highly disruptive for sleep and can lead to major daytime impairments. Sleep apnea, a common breathing disorder for children and adults, can also cause heavy snoring.
- Obstructive sleep apnea: Obstructive sleep apnea (OSA) is characterized by disordered breathing episodes, or apneas, during sleep. People with this condition will often wake up choking or gasping for air multiple times during the night, and report feelings of fatigue and non-restorative sleep during the day. OSA occurs when the airway is blocked due to certain physiological factors, such as a narrow throat, large tongue, smaller lower jaw, or obesity. Children may experience OSA if they have not had their tonsils or adenoids removed.
- Central sleep apnea: Much like OSA, central sleep apnea, or CSA, causes apnea breathing episodes during the night.
 The key difference is root cause. CSA occurs when the brain stops sending signals to muscles that regulate breathing, rather than a physical obstruction blocking the airway. Strokes and other medical conditions that affect the brain stem can cause CSA, as can obesity, heart failure, and some medications.
The key difference is root cause. CSA occurs when the brain stops sending signals to muscles that regulate breathing, rather than a physical obstruction blocking the airway. Strokes and other medical conditions that affect the brain stem can cause CSA, as can obesity, heart failure, and some medications. - Sleep-related hypoventilation disorders: These disorders occur when sleepers do not receive enough ventilation, causing the carbon dioxide levels in their blood to spike. Obesity, genetic abnormalities, certain drugs and medications, and underlying medical conditions can all lead to sleep-related hypoventilation.
- Sleep-related hypoxemia disorder: Hypoxemia refers to below-normal blood oxygen levels. For people with this condition, their blood oxygen levels decrease primarily during sleep. Sleep-related hypoxemia may be a symptom of an underlying medical condition such as pulmonary hypertension, chest wall disorders, or neurologic and neuromuscular disorders.

Hypersomnolence Disorders
Hypersomnolence refers to feelings of sleepiness and fatigue during the day despite a healthy circadian rhythm and an adequate amount of sleep the previous night. These feelings may lead to involuntary lapses into drowsiness or sleep, which in turn puts people at risk for accidents. Some people with hypersomnolence disorders feel the effects of daytime sleepiness before nodding off, while others will unknowingly fall asleep.
- Narcolepsy: Narcolepsy occurs when patients with normal sleep schedules either feel the irrepressible urge to sleep or involuntarily lapse into sleep on a daily basis for at least three months. This condition falls into two primary categories. Narcolepsy Type 1 includes cataplexy, a sudden muscle weakness or paralysis, whereas Narcolepsy Type 2 may include some muscle weakness but not to the same extent.
- Idiopathic Hypersomnia: This condition, like narcolepsy, is characterized by the strong urge to fall asleep or lapses into sleep despite an otherwise healthy sleep schedule.
 However, idiopathic hypersomnia does not include cataplexy. To qualify for a diagnosis, patients cannot have any sleep disorders or preexisting conditions that explain the hypersomnia.
However, idiopathic hypersomnia does not include cataplexy. To qualify for a diagnosis, patients cannot have any sleep disorders or preexisting conditions that explain the hypersomnia. - Kleine-Levin Syndrome: This rare disorder is defined by episodes of excessive sleep – up to 20 hours a day in some cases. The first episode often occurs in tandem with a bodily infection or excessive alcohol intake, and will usually occur every year or so. Episodes can persist for days, weeks, or even months. Common effects of Kleine-Levin Syndrome include cognitive dysfunction, altered perceptions, eating disorders, and disinhibited behaviors. Over the course of eight to 12 years, episodes of excessive sleepiness decrease in intensity and frequency.
Sleep-Wake Disorders
This category of circadian rhythm sleep disorders is tied to a person’s internal clock and the factors that regulate their 24-hour sleep cycle. Light plays a major role in the circadian rhythm.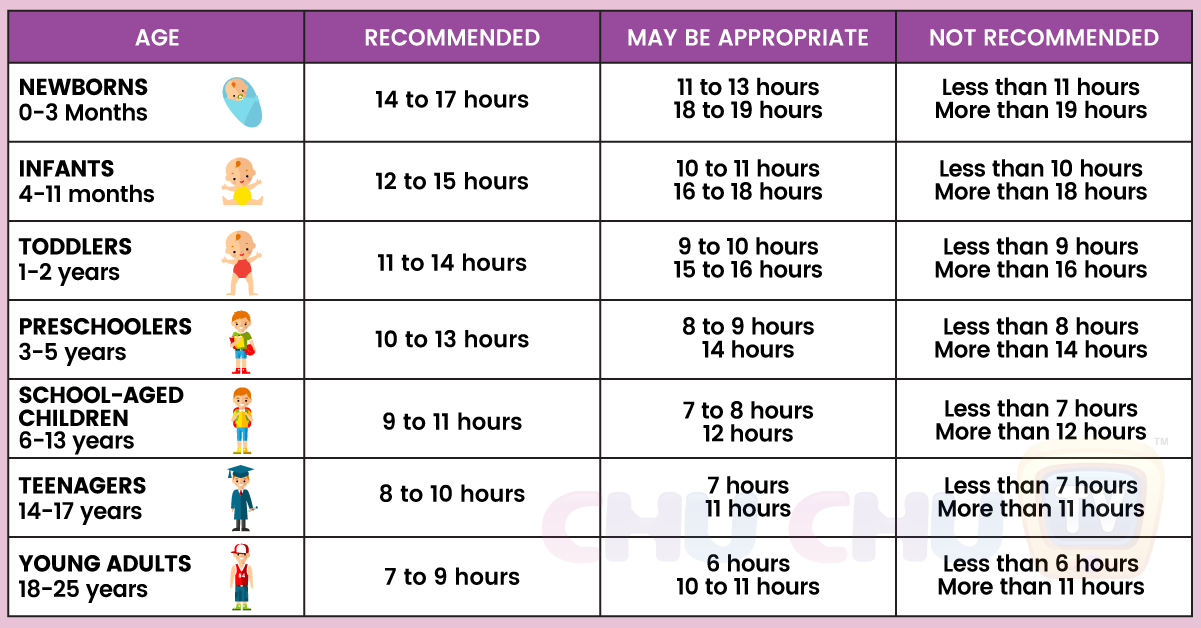 When our eyes are exposed to natural or artificial light, our body releases compounds that keep us awake and alert; when light disappears at night, the body produces different compounds to induce feelings of drowsiness and relaxation. Sleep-wake disorders occur in people whose circadian rhythms are misaligned, causing them to feel alert and tired at abnormal times of the day.
When our eyes are exposed to natural or artificial light, our body releases compounds that keep us awake and alert; when light disappears at night, the body produces different compounds to induce feelings of drowsiness and relaxation. Sleep-wake disorders occur in people whose circadian rhythms are misaligned, causing them to feel alert and tired at abnormal times of the day.
- Sleep-wake phase disorder: This disorder is defined by the inability to fall asleep and wake up at the intended times, and falls into two subcategories. Delayed sleep-wake phase disorder occurs when the patient’s sleep-wake cycle is delayed by at least two hours. For advanced sleep-wake phase disorder, patients fall asleep and wake up at least two hours ahead of schedule. Symptoms must persist for at least three months to warrant a diagnosis.
- Irregular rhythm sleep-wake disorder: This disorder is marked by irregular sleeping and waking episodes over a 24-hour period.
 Patients often experience insomnia symptoms when they are trying to sleep and excessive daytime sleepiness.
Patients often experience insomnia symptoms when they are trying to sleep and excessive daytime sleepiness. - Non-24 sleep-wake disorder: People with this disorder have internal clocks that do not follow a 24-hour schedule. Their sleep-wake cycle may be shorter or longer than 24 hours, depending on how their circadian rhythm is synchronized. Most patients with non-24 sleep-wake disorder are totally blind.
- Shift work sleep disorder: Most people with shift work sleep disorder have jobs that require shifts outside the typical 9-5 schedule, including evening and overnight shifts. They experience insomnia symptoms at night and excessive daytime sleepiness because their sleep schedule is not in sync with a normal 24-hour circadian rhythm, which is influenced by light and darkness. Shift work sleep disorder often deprives people of one to four hours of sleep every 24-hour period.
- Jet lag disorder: This temporary disorder occurs when travelers pass through multiple time zones during a single flight or series of successive flights, leaving their circadian rhythm out of sync with local time at their final destination.
 The severity of jet lag depends on the length of travel, as well as the direction – eastbound travelers tend to experience stronger jet lag than those heading west.
The severity of jet lag depends on the length of travel, as well as the direction – eastbound travelers tend to experience stronger jet lag than those heading west.
These disorders are characterized by abnormal movements during sleep that can be disruptive for the individual, as well as their sleep partner. They often cause excessive daytime sleepiness and fatigue due to sleep loss.
- Restless legs syndrome: Also known as Willis-Ekbom disease or simply RLS, this causes people to experience unpleasant or painful sensations in their legs. These sensations are usually more pronounced at night when the individual sits or lies down for prolonged periods. RLS creates strong urges to move the legs in order to alleviate the discomfort.
- Periodic limb movements disorder: People with this disorder – PLMS for short – will experience periodic bodily movements during the night that coincide with arousal and sleep disruptions. In most cases, movements are isolated to the lower limbs.
 Patients are often unaware of the movements or the sleep arousal.
Patients are often unaware of the movements or the sleep arousal. - Sleep-related bruxism: Sleep-related bruxism causes people to grind their teeth during sleep. Over time, this can cause excessive jaw pain, abnormal tooth wear, and other side effects. Many people with bruxism treat their condition with an anti-snoring mouthpiece or mouthguard, such as a mandibular advancement device that physically moves the jaw forward or a tongue retaining device that holds the tongue in place.
- Abnormal Sleep Behavior Disorders
- Bruxism
- Central Sleep Apnea
- Chronic Fatigue Syndrome
- Circadian Rhythm Sleep Disorders
- Excessive Sleepiness
- Hypersomnia
- Insomnia
- Narcolepsy
- Night Terrors
- Non-24-Hour Sleep Wake Disorder
- Obstructive Sleep Apnea
- Parasomnias
- Periodic Limb Movements Disorder
- REM Sleep Behavior Disorder
- Restless Leg Syndrome (RLS)
- Shift Work Disorder
- Sleepwalking
- Sleep Apnea
- Sleep-Related Breathing Disorders
- Sleep-Related Movement Disorders
- Sleep Paralysis
Recommended Hours of Sleep by Age Chart
demaerre/Getty Images/iStockphoto
Quick facts about how much sleep you need:
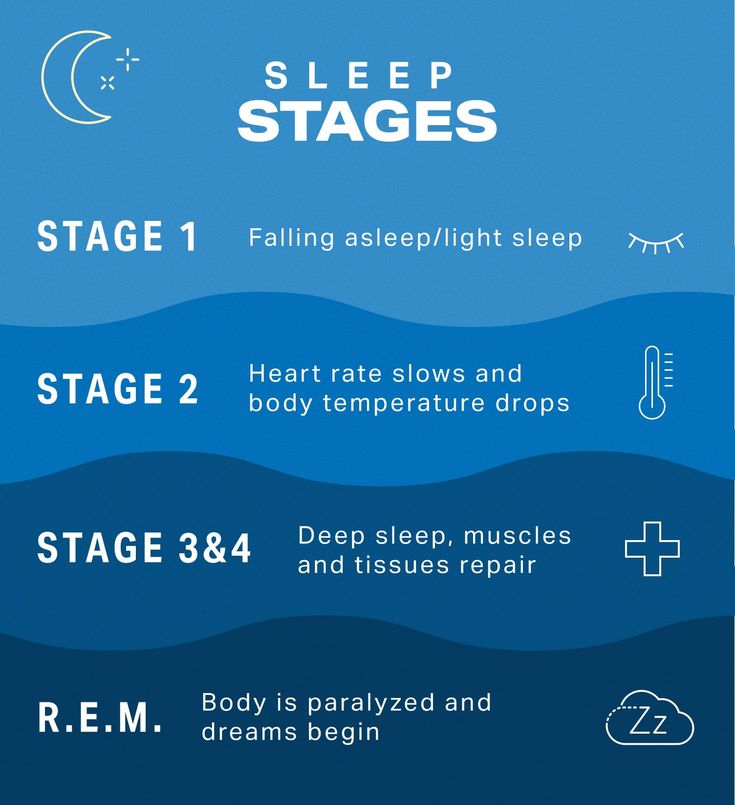
- For the average adult, you go through about 4 to 6 sleep cycles a night.
 To go through these cycles, you’ll need about 7 to 9 hours of sleep.
To go through these cycles, you’ll need about 7 to 9 hours of sleep. - Sleep recommendations are based on public health recommendations, which means you could need more, or less, to feel restored.
- Let your body sleep and wake without alarms for 10 to 14 days to find out how many hours you naturally need.
- Be careful of overestimating sleep. Awake time in bed shouldn’t count towards your total hours.
- Infants and children need their caregiver’s help to establish a healthy sleep schedule. Kids will also benefit from a 30-minute wind down routine before bed.
We’ve all experienced the benefits of good sleep before. You know that feeling when you wake up in the morning feeling refreshed, relaxed, and restored? Now think back to how much sleep that was — was it six hours of sleep or seven or eight? There is no single “right” answer because it varies from person to person. Age, environmental factors, daily sleep habits, and individual needs, from activity level to overall health, can all impact how many hours of sleep you need.
Keep reading for experts’ top tips to help you obtain an optimal amount of quality sleep. Hint: It starts with not obsessing over getting the recommended “normal” number of hours.
The average amount of sleep needed by adults and kids
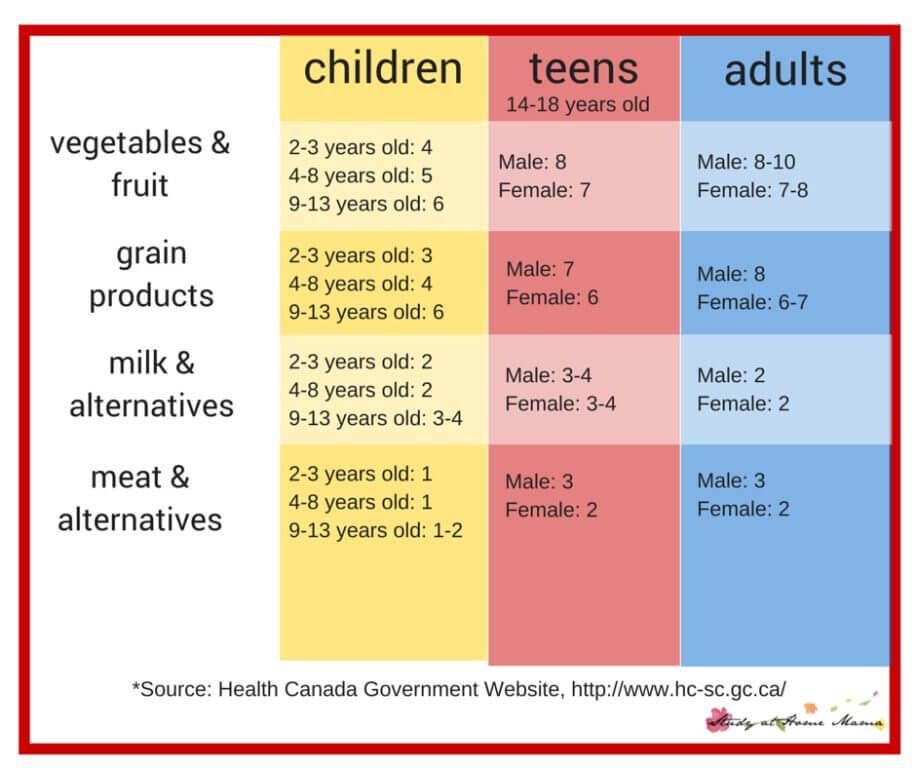
Before we dive into tips, it’s good to start with a baseline. According to the National Sleep Foundation, adults between 25 and 64 years of age need an average of 7 to 9 hours of sleep per night. Adults 65 and older need 7 to 8 hours per night. This is based on public health recommendations, but internal and external factors may change the number of hours you need.
Kids in particular need the most sleep, to promote growth and development. The amount of sleep needed varies, depending on their age, family schedules, and individual temperament.
See our chart below for how much sleep you might need by age:
| Age range | Recommended hours of sleep per day* | Ideal bedtime | |
| Newborn | 0-3 months | 14 to 17 | N/A |
| Infant | 4-11 months | 12 to 15 | 6 - 7 p. m. m. |
| Toddler | 1-2 years | 11 to 14 | 7 - 7:30 p.m. |
| Preschool | 3-5 years | 10 to 13 | 7 - 8 p.m. |
| School-age | 6-13 years | 9 to 11 | 8 - 9:30 p.m. |
| Teen | 14-17 years | 8 to 10 | 9 - 10:30 p.m. |
| Young adult | 18-25 years | 7 to 9 | 8 - 12 p.m. |
| Adult | 26-64 years | 7 to 9 | 8 - 12 p. m. m. |
| Older adult | 65 years and up | 7 to 8 | 8 - 12 p.m. |
*Per National Sleep Foundation guidelines
While determining your bedtime, consider sleep hygiene rules such as:
- Limiting screentime 1 hour before bed
- Avoiding caffeine 6 to 8 hours before bed
- Having a 30-minute bedtime routine to fully wind down and relax
Optimal bedtimes for kids to get enough sleep
Vera Livchak/Getty Images
“Newborns don’t really have well-organized sleep with a true bedtime until the 4- to 6-month mark,” says Lynelle Schneeberg, Psy.D., a pediatric sleep psychologist and author of “Become Your Child's Sleep Coach.”
“From the 4-to-6-month mark until the first birthday, most [experts] recommend a bedtime of 6 p.m. to 7 p.m. For toddlers, the bedtime could move a bit later, 7 p. m. to 7:30 p.m.,” she notes.
m. to 7:30 p.m.,” she notes.
Parents will need to factor in time for their child’s bedtime routine, about 15 to 30 minutes for babies six months and up and toddlers, depending on whether it is a bath night, Schneeberg says. Even if the child has historically taken longer to settle, Schneeberg recommends capping the routine at 30 minutes. “If the routines are too long or complicated, kids are more likely to stall and try to add things to the routine.”
For school-age children, Schneeberg recommends a bedtime between 8:00 p.m. and 9:30 p.m.; for teens, a 9:00 p.m. to 10:30 p.m. range is ideal.
How sleep quantity aids with sleep quality
Dr. Abhinav Singh, the medical director of the Indiana Sleep Center and clinical assistant professor at Marian University, explains that two kinds of sleep take place during the night, and you need to experience both for optimal rest. “Adults typically go through four to six sleep cycles a night,” explains Singh. “This adds up to roughly about 7 to 9 hours of sleep to accommodate the range.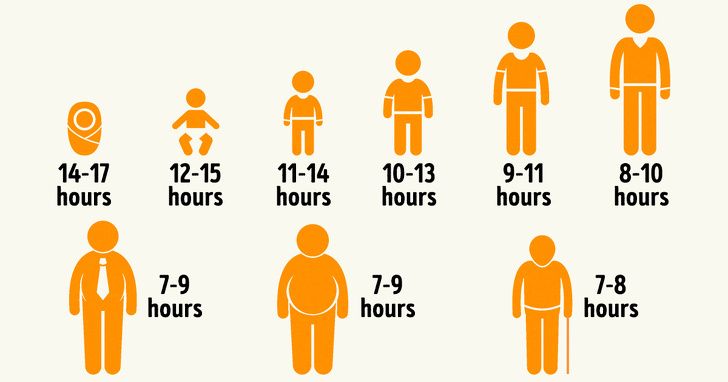 ”
”
The two types of sleep are:
- non-rapid eye movement sleep (NREM): NREM sleep consists of sleep stages 1 to 3, which is governed by homeostasis. Stages 1 and 2 are “light” stages because it’s easier to wake up during these stages. Most of your night will be in stage 2. Stage 3, also known as deep or slow wave sleep, is when the body takes care of housekeeping, including muscle repair, growth hormone release, brain toxin cleansing, and some types of memory functions.
- rapid eye movement (REM) sleep: REM sleep, also known as dream sleep, is governed by your circadian rhythms. This is the time your brain uses to sort through memories, emotions, and general comprehension.
While certain stages are considered lighter or deeper, you can still be woken up from each.
How to prioritize quality over quantity
Alberto Guglielmi/Blend Images/Getty Images/Tetra images RF
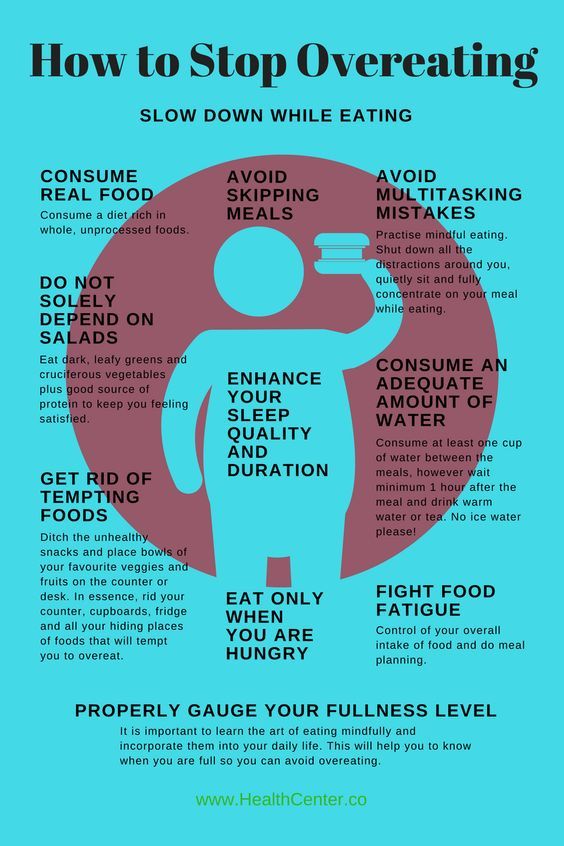
Have you ever gotten 8 or 9 hours of sleep and woken up feeling unrefreshed? When this happens, it indicates that the quality of sleep was insufficient, says Singh.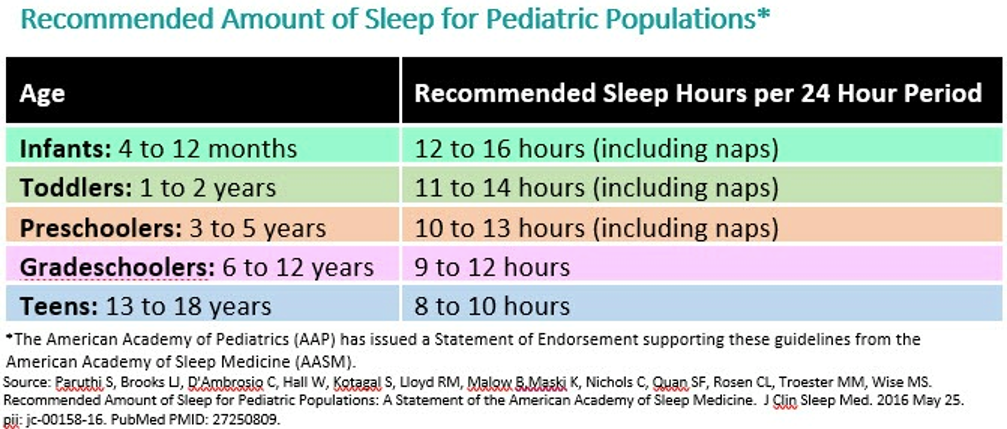 He says that a variety of intrinsic factors can be disrupting sleep, including a partner’s snoring, restless limbs, insomnia, or sleeping in an environment that’s too hot or too cold, has too much light, or is prone to noise.
He says that a variety of intrinsic factors can be disrupting sleep, including a partner’s snoring, restless limbs, insomnia, or sleeping in an environment that’s too hot or too cold, has too much light, or is prone to noise.
1. Figure out your natural sleep number
Instead of stressing about getting eight hours of sleep, let your body drive your sleep number. Singh cites an approach developed by his colleague Dr. Charles Joonghie Bae, an associate professor of clinical medicine at the University of Pennsylvania.
“Let your body naturally fall asleep and wake up and see where the number lands. At the end of 10 to 14 days of alarm-free sleep, you will know your natural sleep needs,” he says.
Some ways to track and discover your sleep number include using sleep diary. Or for an automated approach, try a fitness or app sleep tracker. Be wary of sleep debt, which can influence how much sleep you need at first.
2. Follow your natural circadian rhythm
Rather than defining sleep as bedtime, consider when you start to feel tired or relaxed — and what time the lights are out (literally and figuratively). Figuratively, it’s when the sun sets as less light exposure triggers your sleep–wake cycle so your body will produce melatonin, a sleep-promoting hormone.
Figuratively, it’s when the sun sets as less light exposure triggers your sleep–wake cycle so your body will produce melatonin, a sleep-promoting hormone.
“As the light fades, your sleep drive tends to rise,” says Singh. “As the light brightens, your sleep drive is repressed, and your wake drives are elevated.”
Literally speaking, turning off devices to avoid blue lights or switching bulbs to emit warm tones will also support your natural sleep-wake cycle. Adjusting your sleep schedule to your natural sleep-wake cycle will help you transition from falling asleep to being asleep much easier.
3. Choose your bedtime, based on your cycle
Now you know how many hours your body likes to sleep and around what time you start getting tired and want to relax. Take those numbers, determine what time you need to wake up, and work backwards from there. Singh says that an ideal bedtime range for adults is between 8 p.m. and midnight, though he acknowledges that individuals must consider their social and work responsibilities and intrinsic preferences, such as being a night owl versus a morning person.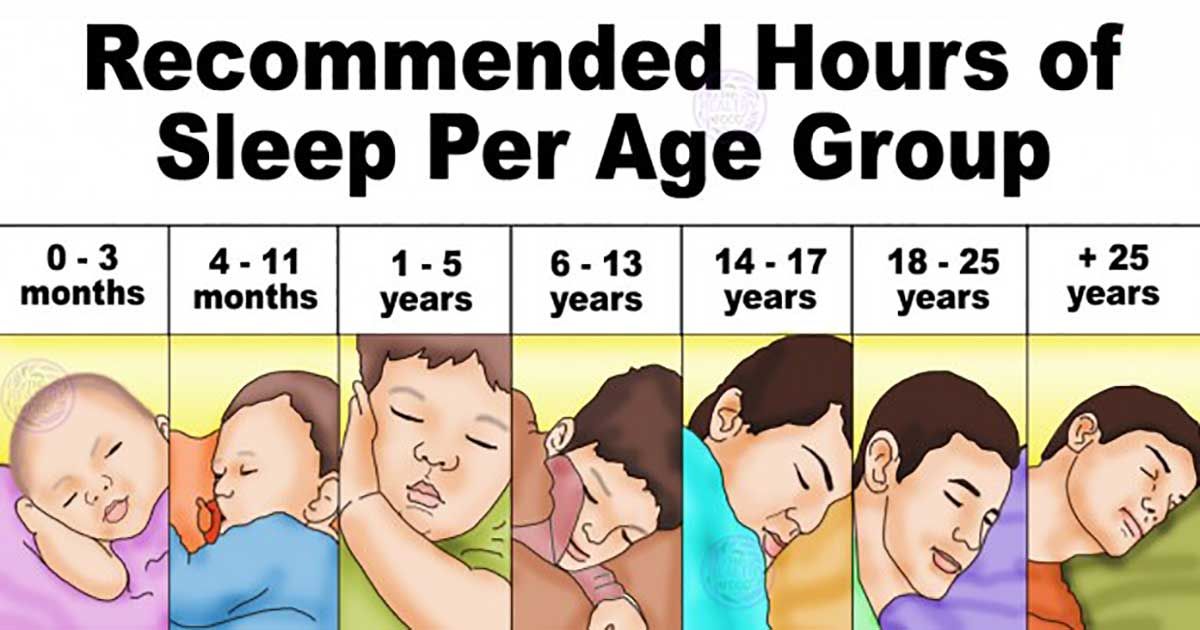
Let’s say that you need to wake up by 6 a.m. and that you need 8 hours of sleep. Your bedtime, that is, the time you need to fall asleep by, would be 10 p.m. However, it’s unlikely that you’ll fall asleep right away, so you factor in the 20 to 30 minutes it takes to settle in bed, which means: If you need 8 hours of sleep and need to be up by 6 a.m., you want to be in bed by 9:30 p.m.
Butterworth Collective
4. Don’t forget wind down time
Kids aren’t the only ones who benefit from a bedtime routine. Singh advises that adults give themselves 30 minutes to wind down before sleep.
He suggests what he’s dubbed the 4-Play Method: shower, journal, read, and breathe. “That becomes the routine so like a Pavlovian dog, it teaches the brain that this spells sleep,” Singh says.
- Shower or bath: This helps rev up your body temperature; as the skin dilates and loses heat, melatonin rises.
- Journal: Jot down your to-do list or thoughts, then put it away.

- Read: Spend 10 to 15 minutes listening to or reading an article or book.
- Breathe: Do a little bit of relaxed breathing with yoga or listen to a meditation.
If your bedtime was 9:30 p.m., after adding another 30 minutes for a wind-down routine, this means you’d want to start the process of getting to sleep by 9 p.m.
Of course, if you work from home or don’t have other morning commitments such as getting kids ready for school, you may be able to shift your bedtime routine later. If you are a morning person, Singh’s tip is to try and sleep before midnight. Sleeping before midnight, for most morning people, allows for adequate amounts of both non-REM and REM sleep in their natural circadian rhythm.
Be careful of overestimating how much sleep you’re getting
If you tend to toss and turn before sleep, be mindful of how much time it takes to sleep when you’re actually in bed. Overestimating sleep could lead to a chronic lack of sleep, which has been linked to health issues such as heart disease, Type 2 diabetes, obesity, and depression.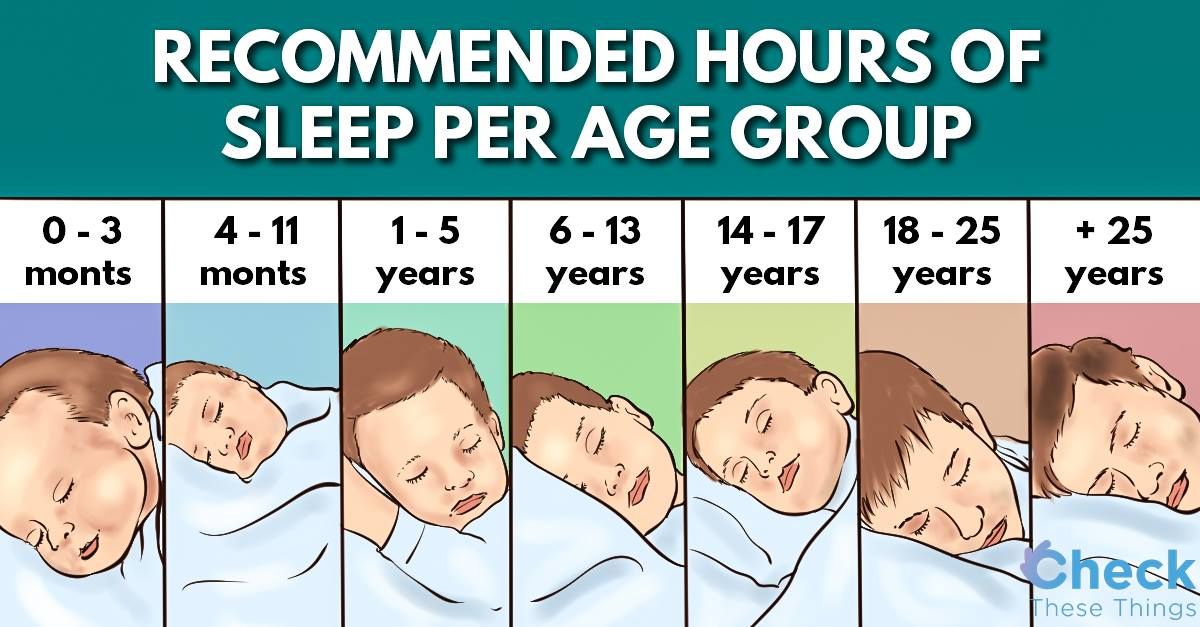
“[Many] think they’re getting 45 minutes to an hour more of sleep [than they actually are],” Singh says. “It takes 20 minutes after your eyes shut to get into restful, restorative sleep.” That time could take even longer, however, if you do other activities in bed like reading or scrolling on your phone.
If you’re not a sleep diary person and like your tracking automated, using a sleep tracker can help you figure out what time you’ve been going to bed. “[Sleep trackers] may be slightly better at estimating quantity rather than quality,” Singh says. But at the end of the day — or in the morning — trust your body to tell you how you feel about your sleep last night.
Layla Khoury-Hanold is a freelance journalist covering food, travel, and lifestyle stories. Her work has appeared online with Food Network, Refinery29, the Chicago Tribune, Saveur, and the James Beard Foundation, and in print with Drinks International, Our State, The Roanoker, and INDY Week.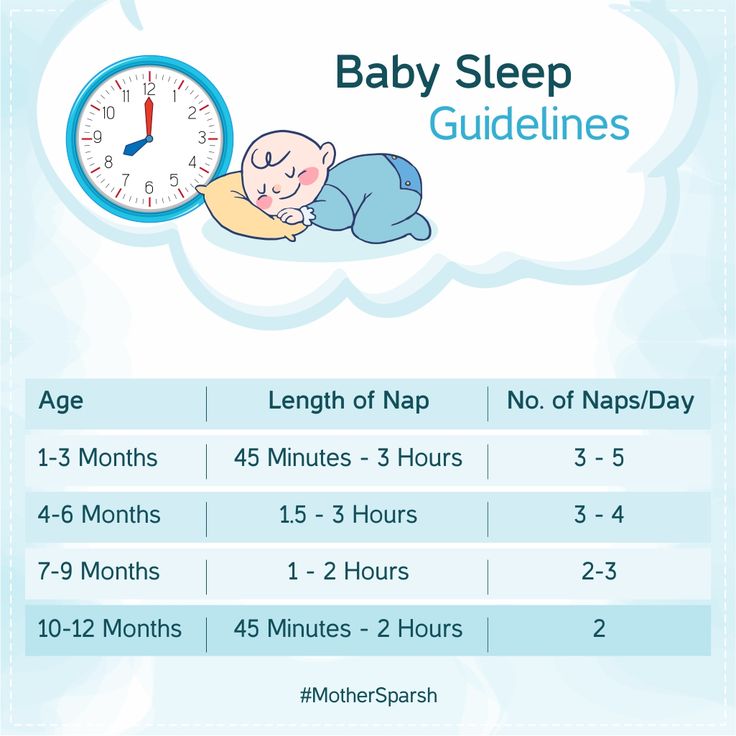 Follow her writing and food adventures on Instagram @words_with_layla.
Follow her writing and food adventures on Instagram @words_with_layla.
Child's sleep | How many hours a day are children from infants to 7.10 years old and older, table
08/25/2011
1783897
785
and sleep norms
Article
Elena Muradova
Elena Muradova
BabySleep Center, the first sleep consultant in Russia, author of the BabySleep methodology
Mother of three children
“As many as he needs,” is the answer. And in general, the child does not owe anything to anyone. Sleep is a natural process. Get tired - go to sleep. He does not fall asleep, which means that he is not yet tired enough and the body does not need rest. So?
Yes, if your child is over 7 years old (or 17). So, if a small child by nature has a so-called docile type of temperament. Such a baby really has a stable schedule of sleep and wakefulness almost from birth. He doesn't need help to fall asleep. Compliant children sleep long and soundly, not crying even during brief awakenings between sleep stages and cycles.
He doesn't need help to fall asleep. Compliant children sleep long and soundly, not crying even during brief awakenings between sleep stages and cycles.
But in most cases, it is desirable for parents to have at least an approximate idea of how much a child should / can stay awake and sleep per day at different ages.
What is it for:
- to avoid overwork;
- there was no accumulation of fatigue in the baby;
- the baby got enough sleep for brain development, growth, “recharging” of all body systems;
- improve the mood of the child during the day;
- don't expect the impossible.
Child crisis calendar
Sleep norms by age
Mothers know how much a child should eat, how much to gain weight. This information helps keep track of your baby's health. And doctors always control such parameters. But how many people know how much time a child should/can normally sleep? And worry about whether he gets this rate? But sleep, according to research, is of great importance for the development of the child.
The duration of sleep depends on age: the younger the body, the more sleep it needs. A newborn sleeps almost the whole day, a one-year-old needs 13 hours of total sleep, children aged 3–5 years need to sleep about 11–12 hours a day, elementary school students 10–11 hours, high school students 8.5–9 hours, adults 7 -9 hours.
Before dwelling on the sleep norms for each age in detail, let's figure out how to correctly calculate the amount of sleep.
4 sleep calculation rules:
- Write down all your dreams - in a notebook, notes on your phone or in the app - even if you have a perfect memory.
- Don't round up - even five minutes can play a role in the overall picture of sleep.
- Start the countdown in time: for example, if a baby suckles at the breast or a bottle with his eyes closed, then he is sleeping.
- Follow up for 5-7 days. And better 10-14 to get more accurate data.
How much sleep a newborn "should"
The neonatal period lasts 28 days.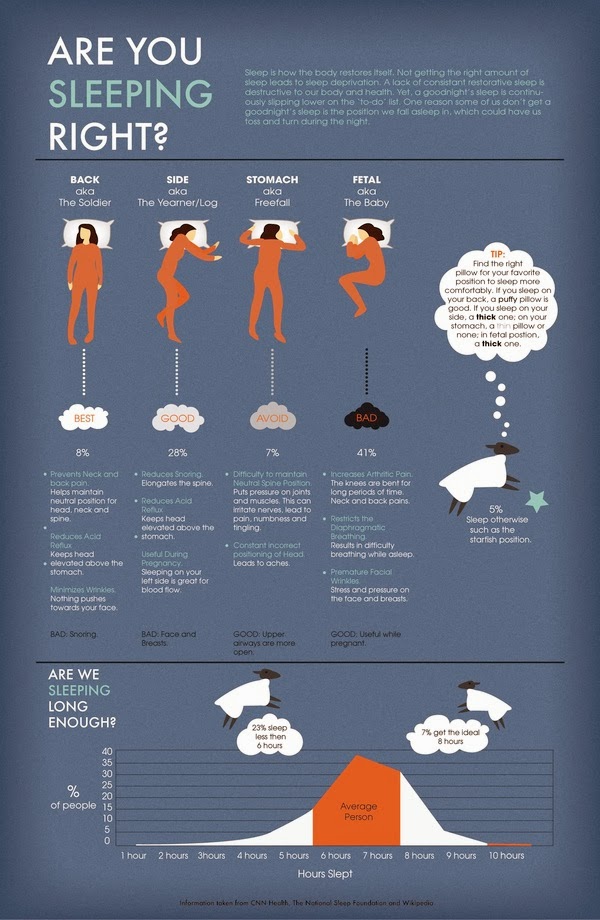 At this time, the baby is adapting to life in the outside world - first of all, this happens during sleep. Parents may think that the child sleeps around the clock. It's almost true: on average, a healthy newborn baby under the age of one month sleeps 16-19 hours, waking up every 1-3 hours during the day and at night to eat.
At this time, the baby is adapting to life in the outside world - first of all, this happens during sleep. Parents may think that the child sleeps around the clock. It's almost true: on average, a healthy newborn baby under the age of one month sleeps 16-19 hours, waking up every 1-3 hours during the day and at night to eat.
It is important to remember that all babies are different from birth, and newborns' daily sleep patterns may vary. One child at the age of 1 month may need 15 hours of sleep per night, while another at the same age will need all 22 hours. You can read more about the sleep of a newborn baby in this article.
How much a baby “should” sleep at 1-3 months
The baby is growing rapidly, the rhythm of his dreams often changes. You may notice a tendency to fall asleep earlier at night and increase the amount of uninterrupted sleep at night. This is due to physiological changes in the body - the process of consolidation of night sleep begins.
During this period, the first difficulties with sleep may begin - it is in your power to help the child overcome them more easily.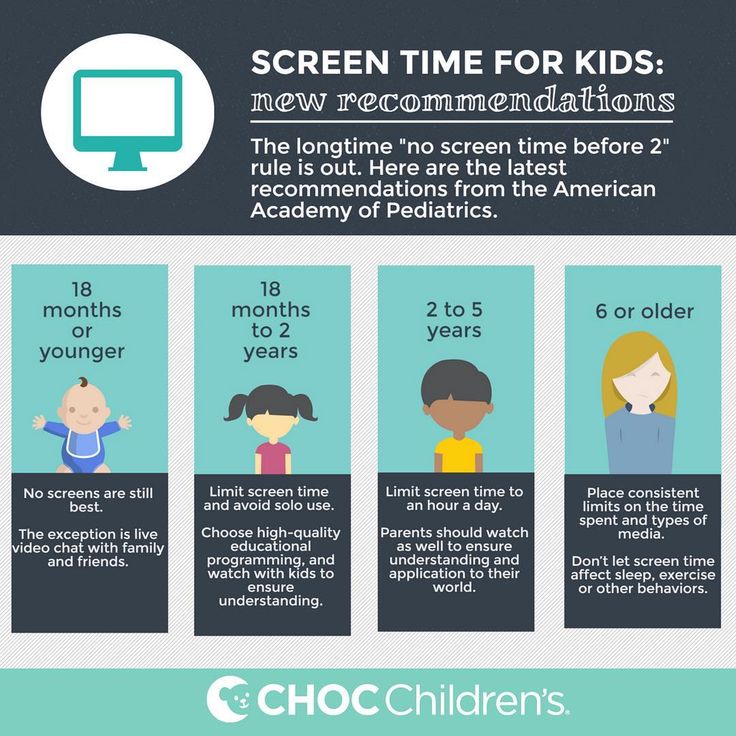
The features of a baby's sleep are largely determined by his temperament, but there are numbers that serve as a guide. At the age of 1-3 months, babies sleep an average of 14-17 hours per night. Of these, 5-7 hours fall on daytime sleep and 8-11 on night.
How much sleep "should" a child have at 3-5 months
The sleep of children aged 3-5 months is greatly affected by mental leaps that occur at about 3, 4 and 5.5 months. In addition, around 4 months, the structure of a child’s sleep completely changes, it becomes the same as in an adult. All this often causes sleep deprivation.
During this period, it is very important to ensure that the child sleeps enough in total per day. Babies aged 3-5 months need an average of 14-17 hours of sleep, of which 4-6 hours are during the day and 10-12 at night.
How much sleep children "should" at 6-8 months
Sleep for a child at 6-8 months is just as important as for a newborn. Now the baby is learning a lot of new skills. On the one hand, sleep is necessary for their assimilation, and on the other hand, the training of these new skills can also take place in a dream, interfering with proper rest. Help your little one get fit every day while awake, and don't lose sight of age-appropriate sleep patterns.
Now the baby is learning a lot of new skills. On the one hand, sleep is necessary for their assimilation, and on the other hand, the training of these new skills can also take place in a dream, interfering with proper rest. Help your little one get fit every day while awake, and don't lose sight of age-appropriate sleep patterns.
Typically, at 6-8 months, a child's body needs 13-15 hours of sleep per day. During the day, it is normal to have 2-3 sleeps with a total duration of 2-4 hours, and night sleep lasts 10-12 hours. Several awakenings per night is a variant of the norm. Children still do not live according to the regime, while this is a gradually changing rhythm of sleep and wakefulness, but it is already becoming quite predictable.
How much sleep a child "should" at 9-11 months
According to the average norms, at 9-11 months, children need 12-15 hours of sleep per day. Of these, 10–12 hours fall on night sleep, and 2–3 hours on daytime.
Approximately 70% of healthy children by the age of 9 months are physiologically able to sleep through the night without waking up.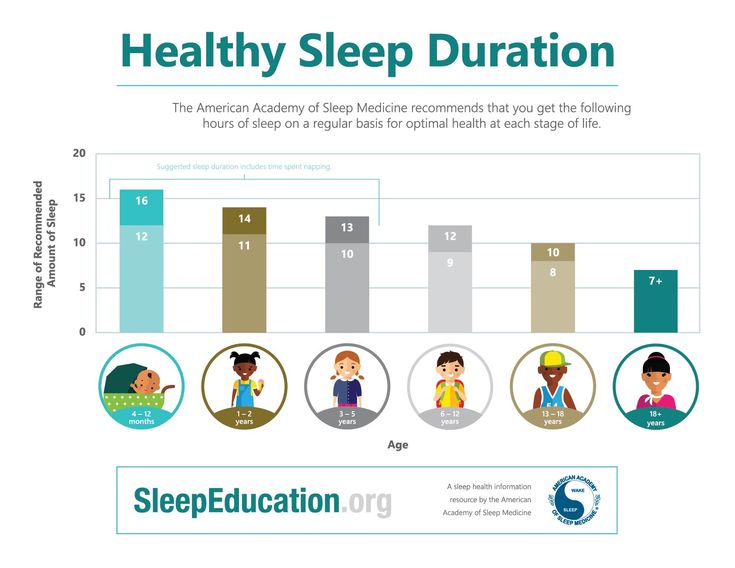 They can, but they don't have to. If your baby has already mastered falling asleep on his own, then most likely he can sleep through the night with a minimum number of awakenings (for example, breastfeeding at 5-7 am important for maintaining lactation) or without them at all.
They can, but they don't have to. If your baby has already mastered falling asleep on his own, then most likely he can sleep through the night with a minimum number of awakenings (for example, breastfeeding at 5-7 am important for maintaining lactation) or without them at all.
How much do children sleep at 1-1.5 years old
The second year of a child's life, as a rule, gives parents a long-awaited sense of stability: changes in sleep patterns become less rapid, and the daily routine is much more predictable.
Sleep continues to play a key role in your baby's development, growth and well-being. Children aged 1-1.5 years on average need 12-14 hours of sleep per day: 2-3 hours of daytime and 10-12 hours of sleep at night.
How much sleep children need at 2–3 years old
The total daily sleep time, which will provide children 2–3 years old with sufficient rest and recovery of the body, is normally 11–14 hours.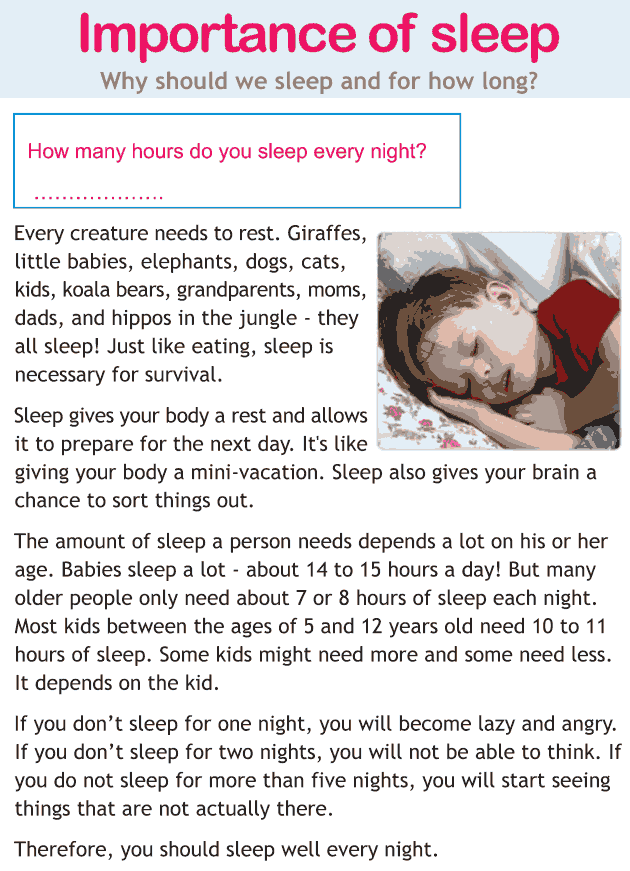 During this period, children usually have only one daytime nap lasting 1-3 hours. Some children may occasionally skip naps. On such days, it is important to put the child to sleep earlier than usual, so that the duration of night sleep is equal to the entire daily norm.
During this period, children usually have only one daytime nap lasting 1-3 hours. Some children may occasionally skip naps. On such days, it is important to put the child to sleep earlier than usual, so that the duration of night sleep is equal to the entire daily norm.
Many parents expect their child to sleep well by the time they are two years old. And often, indeed, this happens: the baby learns to connect sleep cycles and sleeps much better than in infancy. But it happens that a child’s sleep does not change for the better even at 2 years old. In this case, it is worth starting work on improving sleep with a BabySleep consultant.
How much do children sleep at 4–7 years old? It is probably even difficult for you to remember what he was like in infancy. But, as before, he still needs a lot of sleep: for children aged 4-7 years, this is an average of 10-13 hours a day.
Many children go to sleep for 1-2 hours in the afternoon until school. But there are those who, at the age of 3-6 years, finally refuse daytime sleep.
How much sleep do schoolchildren aged 7–17 years
When school life begins, the load on the child increases: lessons, homework, an endless stream of information, circles and sections, increased social activity - all this affects the emotional and physical state. For proper rest and recovery, children 7-10 years old need 10-11 hours of sleep, 10-12 years old - 9-11 hours, 12-14 years old - 9-10 hours. Adolescents 14-17 years old need not much less sleep - 8-10 hours a day.
The table shows how much a child should/can sleep approximately: newborn baby - in the first year of life - up to 3 years old - preschooler - secondary school student - high school student.
Table of norms for children's sleep (0-7 years)
Download the table of norms of sleep in pdf
These norms are average, some people need less time for sleep, some more. The child cannot be “fitted” to the clock. And you don't have to do it.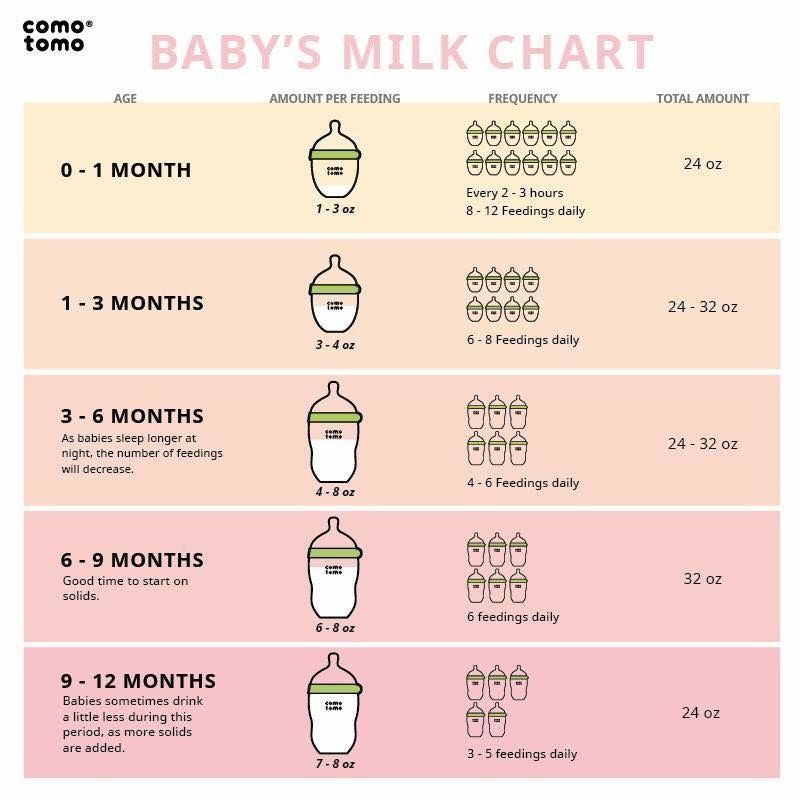 The main criterion of the "norm" is always good health, a childish smile and cheerfulness.
The main criterion of the "norm" is always good health, a childish smile and cheerfulness.
For a deeper understanding of the principles of working with norms, to stay calm and not fall into the “traps” of norms, be sure to read our article “Beware of norms!”
The duration and time of sleep depend on the individual characteristics of the child, his temperament. A “difficult” child may sleep less than a “flexible” child. There are also sleep deprived children. The baby's sleep is also affected by the phase of its development (stages of physical and psychological maturation), teething and other factors.
However, do not rush to classify your child as a sleepless one, and consider his whims as a feature of temperament or explain them by bad weather. First, gather information: think about whether he sleeps enough? Does he wake up in a good mood? Perhaps you should try to put him to bed earlier, choose a more suitable regimen, prolong short daytime naps.
Sleep should be sufficient to ensure a healthy and complete rest for the child. Sleep deprivation is harmful. Sooner or later, it leads to chronic overwork, to a disorder of the nervous system. Scientists have proven that children who sleep too little have an increased risk of behavior problems and attention deficit hyperactivity disorder (ADHD).
Be vigilant! For example, if a four-year-old goes to bed at 10 p.m., and at 7 a.m. you wake him up in the kindergarten, and he does not sleep during the day, then the daily duration of sleep is only 9hours (instead of 11 at this age). A child may behave normally for several days or even weeks, but as fatigue accumulates, whims will appear out of the blue, irritability, tears, sometimes the child may fall asleep unusually early (at 6–7 pm, for example) to compensate for the accumulated lack of sleep.
In this case, it is important to draw the right conclusions! Parents often think: “I have such an active, sleep-deprived child”, “we were covered by an age crisis” and the like, not realizing that the baby simply accumulated hours of lack of sleep. What to do? Going to bed early at night will noticeably improve the situation (move towards it gradually, shifting your bedtime by 15 minutes).
What to do? Going to bed early at night will noticeably improve the situation (move towards it gradually, shifting your bedtime by 15 minutes).
By the way, too much sleep is not good either. Children who sleep too long are lethargic, unfriendly; that's how illness starts. Keep track of the quantity and quality of sleep of your beloved children!
The How Much Sleep a Child Should/Can Sleep chart will help you set realistic expectations for how long a child sleeps at a given age. If parents tend to sleep too much, this can lead to problems and frequent awakenings. And if you do not control sleep at all, this often leads to overwork and the accumulation of fatigue in the child.
Your sleep rate is your approximate guideline. With a general positive mood of the baby, a consistently good mood, easy falling asleep and good sleep at night, deviations from the table values in any direction for an hour or a little more are normal (taking into account the characteristics of the child).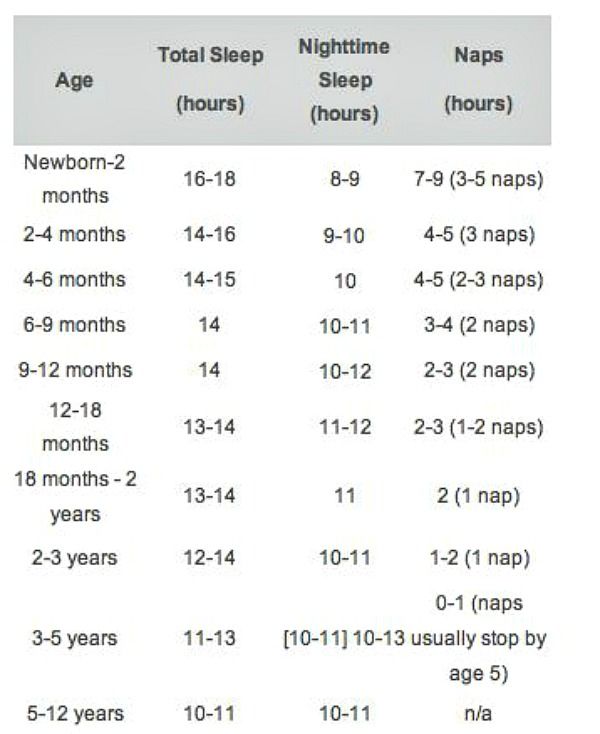 But remember: according to research, a regular lack of sleep reduces the efficiency of the child's brain functioning, attentiveness, and leads to increased fatigue in the evening. Try to pay attention to the quantity and quality of your baby's sleep.
But remember: according to research, a regular lack of sleep reduces the efficiency of the child's brain functioning, attentiveness, and leads to increased fatigue in the evening. Try to pay attention to the quantity and quality of your baby's sleep.
Listen to your child's signals, trust your feelings, monitor your children's sleep patterns.
P.S. Share in the comments: how much does your baby sleep? Be sure to include your age.
#sleepy#normal
1783897
', nextArrow: '', responsive: [{breakpoint: 1199, settings: {arrows: !1, infinite: !1, slidesToShow: 1}}] }) })How much sleep people of different ages need
February 9, 2015 Tips
Are you getting enough sleep? Find out how much sleep newborns, infants, toddlers, preschoolers, schoolchildren, teens, young adults, adults and seniors need. Employees of Harvard University share their scientifically verified opinion.
Let's sleep in the next world!
People's hope
Indeed, why spend about a third of your life sleeping if the "lost" time can be used for good purposes? For example, announce on the grid: “Go! I created! Or read the synopsis.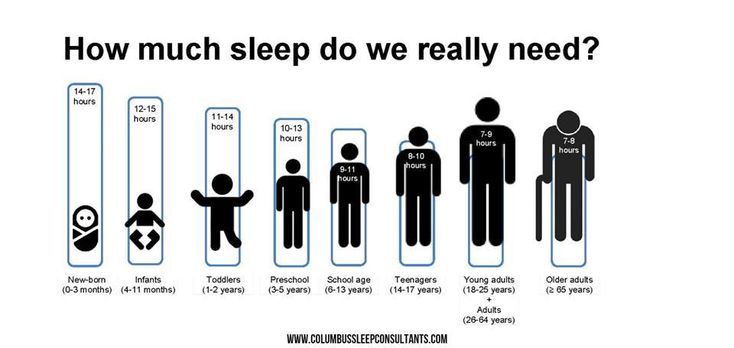 In the first case, we play and relax the brain, and in the second, we enrich it. Seemed like a profit! But the science of sleep says otherwise: lack of sleep does not give the brain proper rest and leads to cognitive decline, poor response and memory lapses.
In the first case, we play and relax the brain, and in the second, we enrich it. Seemed like a profit! But the science of sleep says otherwise: lack of sleep does not give the brain proper rest and leads to cognitive decline, poor response and memory lapses.
The situation is aggravated by the fact that people cannot soberly assess the weakening of their mental and physical abilities, believing that they are in an optimal state. Thus, a sleep-deprived person begins to lose a competitive advantage, at least over himself, but normally sleeping. Missed hours of sleep certainly have a negative impact on both professional and personal life of every person.
Surely you have heard that the norm of sleep for an adult varies around 7-8 hours a day. Is it really? Maybe you need to add a little or, conversely, take away? And how much sleep is needed in childhood, adolescence and adolescence? The answers to these questions are presented in a detailed study by the National Sleep Foundation (USA), a non-profit organization with a 25-year history of studying sleep-related phenomena.
A group of 18 researchers studied more than 300 (!) scientific papers in the field of sleep and made a number of conclusions about the rest rate based on them.
This is the first time that any professional body has developed age-specific sleep recommendations based on a rigorous systematic review of the world's scientific literature on the impact of sleep duration on health, performance and safety.
Charles Czeisler
Professor at Harvard Medical School
As expected, the younger the person, the more sleep their body needs to rest. So, newborns should sleep up to 2/3 of the day, while the elderly will be enough for seven hours.
| Age | Dream, h | ||||||
|---|---|---|---|---|---|---|---|
| Newborn (0-3 months) | 14–17 | ||||||
| 2 | infants (4-11 months) | 2 | 2 | 2 | 29204 29204 29204 29204 2 | 2 | |
| Toddlers (1-2 years old) | 11–14 | ||||||
| Preschoolers (3-5 years old) | 10–13 | ||||||
| Children of school age (6–13 years old) | 9–11 | ||||||
| adolescents (14–17 years) | 8–10 | ||||||
| Young adults (18–25 years old) | 7–9 | ||||||
| adults (26–64) | 7–9 | ||||||
| Elderly (older than 65 years) | 7–8 |
The report by Charles and his colleagues confirms the previously announced framework in 7–9hours of daily sleep.