Skin problems babies
Common Skin Conditions & Rashes in Children: Causes & Treatment
What are skin conditions in children?
Various skin conditions can affect babies, toddlers, children and adolescents throughout their lives. Healthcare providers receive more than 12 million office visits from children each year related to skin concerns. Skin conditions in kids may include hives, warts, acne, birthmarks and all sorts of rashes.
What are the different types of skin rashes in children?
Many different types of rashes can affect your child. Dermatitis, viral infections, bacterial infections, fungal infections and many other conditions may cause rashes.
Dermatitis
Dermatitis is an umbrella term for any condition that causes skin inflammation. These conditions may cause red rashes, itchiness and dry skin on your child and happen at any age. Types of dermatitis include diaper rash, cradle cap, eczema and contact dermatitis.
Diaper rash: Diaper rash is also called diaper dermatitis. It’s the most common skin condition seen in babies. Diaper rash occurs when moisture in your baby’s diaper area causes irritation or growth of fungi or bacteria that normally live in small amounts on the skin. To prevent or treat diaper rash, keep your baby’s diaper area clean and dry by changing diapers frequently. When changing your child's diaper, leave it off for a short while before putting it back on. You can also apply an ointment or cream that contains zinc oxide or petroleum jelly to protect your baby’s skin in the diaper.
Cradle cap: Cradle cap is also called infant seborrheic dermatitis. It’s a skin condition that looks like yellow scaly patches often surrounded by a red rash on your baby’s scalp. Overproduction of the oil-producing sebaceous glands on your baby’s scalp may cause cradle cap. You can treat cradle cap at home with mild baby shampoo and can also lightly rub the scale off if it doesn’t bother your baby.
Eczema: Eczema is also called atopic dermatitis. Eczema makes your child’s skin itchy and then it gets red, irritated and dry. Differences in your child’s skin barrier (compared to normal, healthy skin) and an immune system that tends toward allergies cause eczema. Issues with the barrier make your child’s skin more sensitive and prone to infections and dryness. Controlling your child’s symptoms is the goal of treatment. Often there are seasonal or allergic triggers that you should help your child avoid. Good skin care includes bathing in warm but not overly hot water and moisturizing regularly, especially immediately after baths or water exposure.
Eczema makes your child’s skin itchy and then it gets red, irritated and dry. Differences in your child’s skin barrier (compared to normal, healthy skin) and an immune system that tends toward allergies cause eczema. Issues with the barrier make your child’s skin more sensitive and prone to infections and dryness. Controlling your child’s symptoms is the goal of treatment. Often there are seasonal or allergic triggers that you should help your child avoid. Good skin care includes bathing in warm but not overly hot water and moisturizing regularly, especially immediately after baths or water exposure.
Contact dermatitis: Contact dermatitis can occur when kids have a reaction to an allergen or an irritant. Allergens may include poison ivy or medications. Irritants may include perfumes, soaps, cleaners and paints. Contact dermatitis causes an itchy skin rash that is sometimes also painful. Treatment includes moisturizers, anti-itch creams and topical (or sometimes oral) steroids.
Viral infections
Viral rashes in babies, toddlers and kids are caused by a variety of different viruses. These infections include fifth disease, roseola, chickenpox, measles, rubella, molluscum contagiosum and hand, foot and mouth disease.
Fifth disease: Fifth disease is also called slapped cheek (slap face) disease. It causes a bright red rash on your child’s cheeks. A specific virus, Parvovirus B19, causes fifth disease. Along with the rash, your child may have a fever and other nonspecific symptoms. After a few days, the facial rash will fade. But then pink patches may develop in a lacy pattern on your child’s arms and legs. Treatment includes comfort measures like non-steroidal anti-inflammatory drugs (NSAIDs) anti-itch creams or antihistamines.
Roseola: Roseola is also called sixth disease. Human herpesvirus 6 causes roseola. With roseola, your baby will suddenly develop a high fever that can last up to a week. Once the fever breaks, a slightly raised, spotty pink rash may appear on your baby’s chest or stomach. The rash may spread to your baby’s upper arms and neck, and then it will fade after about 24 hours. Treatment may include acetaminophen for your baby’s fever, but the rash doesn’t itch or cause pain.
Once the fever breaks, a slightly raised, spotty pink rash may appear on your baby’s chest or stomach. The rash may spread to your baby’s upper arms and neck, and then it will fade after about 24 hours. Treatment may include acetaminophen for your baby’s fever, but the rash doesn’t itch or cause pain.
Chickenpox: Varicella zoster virus causes chickenpox. Chickenpox generally causes a rash on your child’s face, chest and back first, but it may travel to their entire body. The rash turns into itchy, fluid-filled blisters, then blisters turn into scabs. Chickenpox usually goes away on its own in one to two weeks. You can treat your child’s symptoms with antihistamines and acetaminophen. They are contagious until all of the blisters are crusted over.
Measles: Morbillivirus causes measles. Measles is very contagious and prevented by the measles vaccine or MMR vaccine. It causes a rash that starts on your child’s face. It’s typically seen behind the ears or around your child’s mouth. Then it moves down over their body. The rash starts as flat red spots, but then smaller raised white spots may appear on top of the red spots. The spots may join together as it moves down your child’s body. Measles has to run its course. It will go away within about two weeks unless complications develop. You can treat your child’s symptoms of fever and achiness with acetaminophen or NSAIDs.
It’s typically seen behind the ears or around your child’s mouth. Then it moves down over their body. The rash starts as flat red spots, but then smaller raised white spots may appear on top of the red spots. The spots may join together as it moves down your child’s body. Measles has to run its course. It will go away within about two weeks unless complications develop. You can treat your child’s symptoms of fever and achiness with acetaminophen or NSAIDs.
Rubella: Rubella is also called German measles and can be prevented by a vaccine. It can look similar but is caused by a different virus than measles. Rubella causes a red or pink rash that starts on your baby’s face and neck. The rash then spreads to other parts of your baby’s body and lasts about three days unless complications develop. Your baby may have a fever, cough or runny nose before the rash appears. Rubella has to run its course. You can treat your child’s symptoms of fever and achiness with acetaminophen or NSAIDs.
Molluscum contagiosum: Molluscum contagiosum virus causes this benign but sometimes unpleasant rash. Molluscum contagiosum has raised bumps on your child’s skin. The bumps are usually flesh-colored, pink or pearly white with indentations in the center. The bumps will show up on your child’s face, chest, stomach, arms and legs. They’re painless but they may not go away for several months or years. Molluscum contagiosum will eventually go away on its own without treatment.
Hand, foot and mouth disease: A virus in the enterovirus family causes hand, foot and mouth disease. The disease causes a red rash to develop around your toddler’s mouth, and on the palms of their hands and soles of their feet. It may also affect other areas. The rash may turn into bumps or blisters on your baby’s skin and in their mouth, and they can be very painful. Hand, foot and mouth disease usually goes away on its own within one to two weeks. You can treat your toddler’s symptoms with acetaminophen or NSAIDs.
You can treat your toddler’s symptoms with acetaminophen or NSAIDs.
Bacterial infections
Types of baby rashes may also include bacterial infections such as scarlet fever and impetigo.
Scarlet fever: A bacteria called group A Streptococcus causes strep throat and scarlet fever. Scarlet fever usually starts with a fever, sore throat and headache, but the key symptom is a raised, red rash on your child’s neck and upper chest. The rash may then spread to other areas of your child’s body. Your child’s face may be red with a pale area left around their mouth. The rash feels rough like sandpaper and may look like your child has a sunburn. Treatment for scarlet fever includes antibiotics.
Impetigo: Group A Streptococcus or Staphylococcus aureus bacteria cause impetigo. It’s most common in kids aged 2 to 5 years old but can happen at any age. Impetigo causes red bumps, blisters or crusty spots to develop.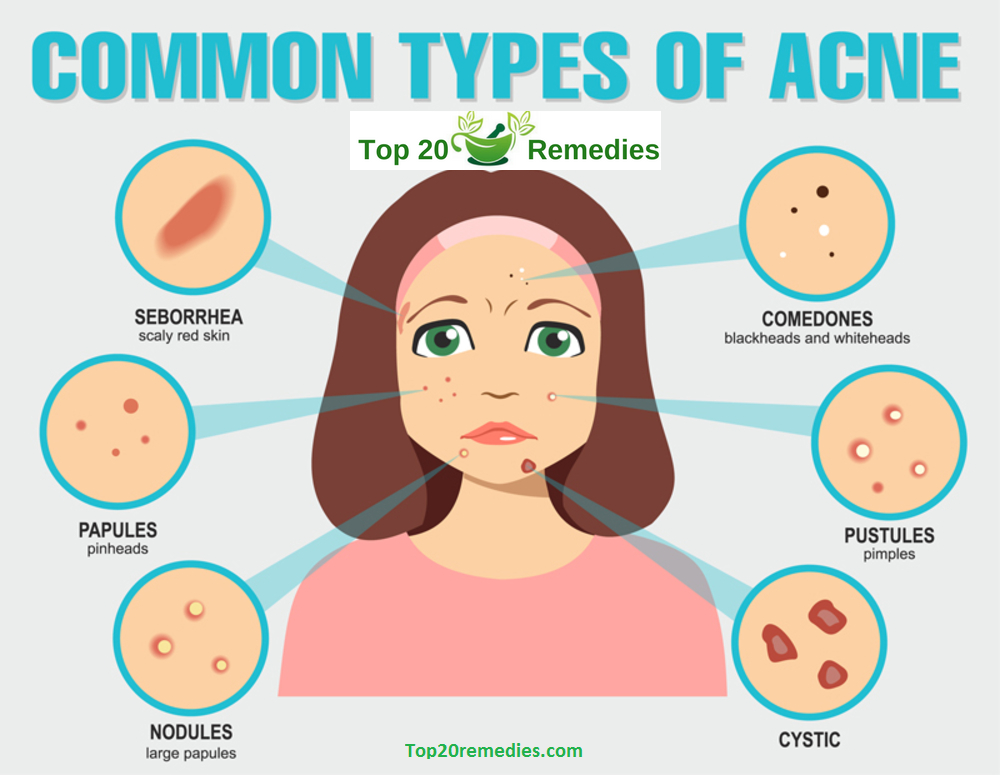 These are most common around your toddler’s mouth and nose and can be anywhere that skin gets repeatedly irritated. Treatment for impetigo usually includes antibiotics that may be oral or put directly onto the skin.
These are most common around your toddler’s mouth and nose and can be anywhere that skin gets repeatedly irritated. Treatment for impetigo usually includes antibiotics that may be oral or put directly onto the skin.
Fungal infections
Common skin rashes seen in babies, toddlers and children can also include fungal infections such as ringworm.
Ringworm: Despite its name, a fungus causes ringworm, not a worm. It causes round or oval patches to develop on your child’s skin. The patches have smooth centers and red, scaly borders and may not look like rings right away. But you’ll notice the rings when they get bigger. The patches may be itchy and painful and may become puffy and inflamed. You can treat your child’s ringworm with antifungal medicines either orally or put directly on the skin.
What is a teething rash?
When your baby’s teeth are starting to come in, they may drool a lot more than usual. Drool can irritate your baby’s skin. This can cause a harmless rash known as a teething rash. The rash causes tiny, red raised bumps on your baby’s face, neck or chest. Teething rashes may come and go as new teeth pop up or when your baby stops drooling as much.
This can cause a harmless rash known as a teething rash. The rash causes tiny, red raised bumps on your baby’s face, neck or chest. Teething rashes may come and go as new teeth pop up or when your baby stops drooling as much.
Teething rashes don’t cause fevers, so if your baby has a fever with a rash, talk with their healthcare provider. You can treat your baby’s teething rash by keeping the area clean and dry. You can also apply emollient cream to the affected area. This may prevent your baby’s drool from irritating their skin.
What causes hives in children?
Hives are also called urticaria. Hives are itchy pink, pale or red bumps on your baby’s skin. They may be small slightly raised spots or large welts of different shapes. Sometimes hives are ring-shaped or look like targets. The rings may have normal-looking skin in the center, or they may look pale, purple or blue. Hives can appear anywhere on your child’s body and may flatten out over several hours. But new bumps can keep showing up for days or weeks.
But new bumps can keep showing up for days or weeks.
Viral infections are a common cause of hives. But allergic reactions to foods, medicines and additives, or even cold temperature and stress may also cause hives. But many cases of hives have no known reason. The best treatment for hives is antihistamines.
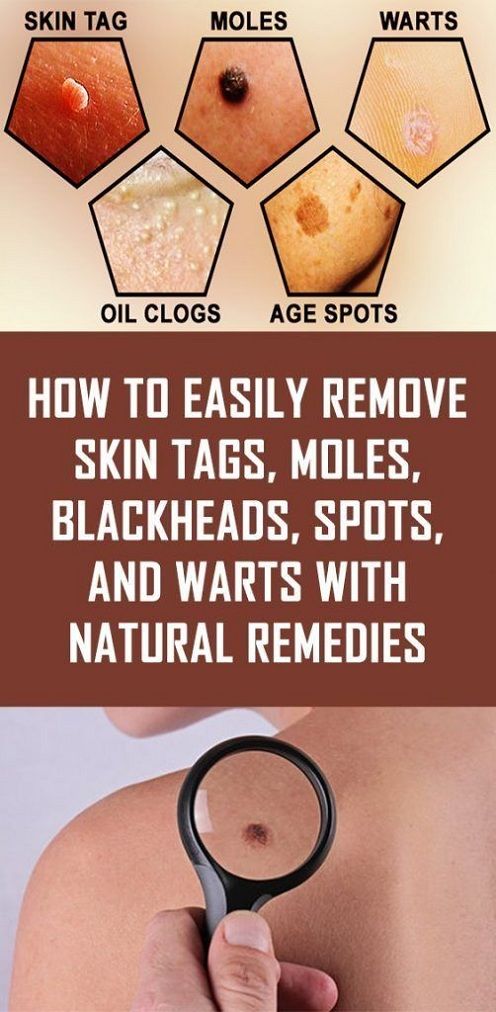
What causes warts in children?
Warts on kids are a type of skin infection caused by the human papillomavirus (HPV). There are multiple types of HPV that cause infections in different areas of skin. The infection causes hard bumps to form on your child’s skin. Warts most commonly appear on your child’s hands and fingers, but they can also appear on their feet, face, genitals and knees. Warts are common in children of all ages. Warts often go away on their own after your child’s immune system fights off the virus, but they can be painful and unpleasant in appearance.
What is baby acne?
Baby acne causes little white bumps and pink pimples to appear on your baby’s face including their forehead, cheeks, eyelids and chin. An inflammatory reaction to yeast on your baby’s skin may cause baby acne. Sometimes baby acne is seen on your baby’s chest or neck. Baby acne usually goes away on its own within your baby’s first three months of life.
An inflammatory reaction to yeast on your baby’s skin may cause baby acne. Sometimes baby acne is seen on your baby’s chest or neck. Baby acne usually goes away on its own within your baby’s first three months of life.
What are birthmarks in children?
There are two main types of birthmarks — red birthmarks and pigmented birthmarks. Red birthmarks are skin markings caused by a collection of blood vessels. Pigmented birthmarks are areas in which the color of your child’s birthmark is different from their skin color.
Red birthmarks
Strawberry hemangiomas: Strawberry hemangiomas can be found anywhere, but are most commonly found on your baby’s face, scalp, back or chest. They’re made up of small, closely packed blood vessels. Strawberry hemangiomas usually fade or go away as your child ages. Some minor discoloration or wrinkling of your child’s skin may remain at the site of the hemangioma.
Cavernous hemangiomas: Cavernous hemangiomas look sort of like strawberry hemangiomas.![]() But they’re deeper in your child’s skin and often darker in color. They look like reddish-blue spongy masses of tissue filled with blood. Cavernous hemangiomas usually go away on their own as your child ages.
But they’re deeper in your child’s skin and often darker in color. They look like reddish-blue spongy masses of tissue filled with blood. Cavernous hemangiomas usually go away on their own as your child ages.
Port-wine stains: Port-wine stains are flat, reddish-purple birthmarks. They’re made up of dilated blood capillaries. They’re commonly seen on your child’s face and they vary in size. Port-wine stains are permanent, without treatment. They might thicken or darken over time.
Salmon patches: Salmon patches are also called stork bites or angel’s kisses. Salmon patches are small blood vessels that are visible through your baby’s skin. They are frequently seen on your baby’s forehead, eyelids, upper lips, between their eyebrows and on the back of their neck. Salmon patches fade as your baby grows.
Pigmented birthmarks
Slate gray nevus or congenital dermal melanocytosis (previously called Mongolian spots): These birthmarks are typically bluish and may look like bruises.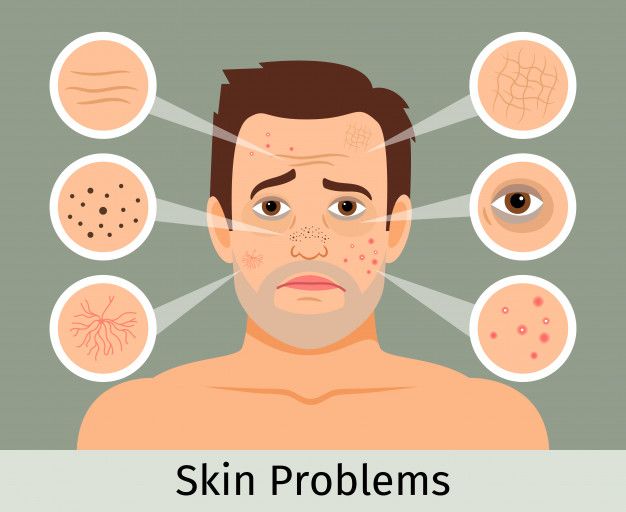 They’re often found on your baby’s buttocks and/or lower back. Sometimes they appear on your baby’s chest, back or arms. Mongolian spots are seen most often in babies with darker skin.
They’re often found on your baby’s buttocks and/or lower back. Sometimes they appear on your baby’s chest, back or arms. Mongolian spots are seen most often in babies with darker skin.
Pigmented nevi: Pigmented nevi are also called moles. Moles are growths on your baby’s skin that typically are flesh-colored, brown or black. Moles can appear anywhere on your baby’s skin. Your baby may have one mole or several in a group.
Congenital nevi: Congenital nevi are moles that your baby was born with. These moles have a slightly increased risk of becoming skin cancer. Larger congenital nevi have a greater risk than smaller congenital nevi do. Your baby’s healthcare provider should examine all congenital nevi and may refer you to dermatology.
Cafe-au-lait spots: Cafe-au-lait spots are light tan or brownish-colored spots. They’re usually oval-shaped. They commonly appear at birth but might develop in the first few years of your child’s life. Cafe-au-lait spots are usually harmless. But if your child has many cafe-au-lait spots, or if they are large, consult their healthcare provider. It may indicate a serious genetic condition.
Cafe-au-lait spots are usually harmless. But if your child has many cafe-au-lait spots, or if they are large, consult their healthcare provider. It may indicate a serious genetic condition.
A note from Cleveland Clinic
Finding a rash, bump, mark or other skin condition on your child’s body may be scary. But kids get tons of rashes, and most of the time, these rashes and other conditions shouldn’t cause too much worry. If you have any concerns, check in with your child’s healthcare provider. They can usually easily diagnose the skin condition and get your child started on any treatment, if necessary.
Common skin conditions in babies
Many parents expect their newborn’s skin to be flawless. But most babies are born with some bruising, and skin blotches and blemishes are common.
Young infants often have dry, peeling skin, especially on their hands and feet, for the first few weeks. Some blueness of the hands and feet is normal and may continue for a few weeks.
Rashes also are common, even into the toddler years. Most rashes and skin conditions are treated easily or clear up on their own. Here are some common skin conditions in babies.
MiliaMilia is the name for tiny white pimples or bumps that appear on the nose, chin and cheeks. Although they appear to be raised, they are nearly flat and smooth to the touch.
If your baby has milia, you can wash his or her face once a day with warm water and a mild baby soap, but avoid using lotion, oils or other products. It’s also important to leave the skin alone — never scrub or pinch the bumps. Milia disappear in time, often within a few weeks, and they don’t require treatment.
Baby acne
Baby acne (neonatal cephalic pustulosis) refers to small red and white bumps that are seen on the face, neck, upper chest and back of some newborns. The pimples are generally most noticeable within the first few weeks after birth.
To care for baby acne, place a soft, clean receiving blanket under baby’s head and wash his or her face gently once a day with mild baby soap. Avoid lotions, oils and other treatments and never scrub, squeeze or pinch the affected skin. The condition typically disappears without treatment within the first couple of months, without scarring. If it doesn’t clear up after a few months, talk with your child’s medical provider.
Avoid lotions, oils and other treatments and never scrub, squeeze or pinch the affected skin. The condition typically disappears without treatment within the first couple of months, without scarring. If it doesn’t clear up after a few months, talk with your child’s medical provider.
Erythema toxicum
Erythema toxicum is the medical term for a skin condition that’s typically present at birth or appears within the first few days after birth.
It’s characterized by small white or yellowish bumps surrounded by pink or reddish skin. The condition causes no discomfort and isn’t infectious. Erythema toxicum disappears in several days, although sometimes it flares and subsides before completely clearing up. Treatment isn’t necessary.
Pustular melanosis
These small spots look like yellowish-white sesame seeds that quickly dry and peel off.
They may look similar to skin infections (pustules), but pustular melanosis isn’t an infection and disappears without treatment.
The spots are commonly seen in the folds of the neck and on the shoulders and upper chest. They’re more common in babies with darker skin.
Cradle capCradle cap (infant seborrheic dermatitis) refers to a scaliness and redness that develops on a baby’s scalp. It results when oil-producing sebaceous glands produce too much oil.
Cradle cap is common in infants, usually beginning in the first weeks of life and clearing up over a period of weeks or months. It may be mild, with flaky, dry skin that looks like dandruff, or more severe, with thick, oily, yellowish scaling or crusty patches.
Shampooing with a mild baby shampoo can help with cradle cap. Don’t be afraid to wash your baby’s hair frequently. This, along with soft brushing, will help remove the scales. If the scales don’t loosen easily, rub a few drops of mineral oil onto your baby’s scalp. Let it soak into the scales for a few minutes, and then brush and shampoo your baby’s hair. If you leave the oil in your baby’s hair, the scales may accumulate and worsen cradle cap.
If cradle cap persists or spreads to other parts of your child’s body, especially in the creases at the elbow or behind the ears, contact your baby’s medical provider, who may suggest a medicated shampoo or lotion. Cradle cap isn’t usually uncomfortable or itchy for your baby, but sometimes a yeast infection can occur in the affected skin. In this case, the skin will become very red and itchy. If you notice this, mention it to your baby’s medical provider.
Eczema
Eczema, also known as atopic dermatitis, is marked by dry, itchy, scaly red patches of skin that are often found around babies’ and toddlers’ elbows or knees. Sometimes the affected area is small and doesn’t bother a baby much, and treatment isn’t necessary. Many children outgrow eczema.
In other cases, eczema can cover a lot of skin and be extremely itchy and uncomfortable. In these cases, talk with your child’s medical provider about whether treatment is needed. You can also try the following methods to prevent eczema from recurring:
- Use fragrance-free baby soaps to wash your child and laundry detergents that are free of fragrances, dye and deodorants.
 Even “mild” baby soaps may have a small amount of fragrance that can irritate sensitive skin.
Even “mild” baby soaps may have a small amount of fragrance that can irritate sensitive skin. - Dress your little one in soft, cotton clothing, and avoid synthetic fabrics and wool.
- Bathe your baby daily with a fragrance-free hypoallergenic bath oil. This can help moisturize your baby’s skin, in addition to helping prevent skin infections, which are more common in children with eczema.
- Use a fragrance-free moisturizer or ointment such as petroleum jelly right after patting baby dry following a bath. This helps lock moisture from the bath into baby’s skin.
- Keep your child away from environmental triggers for eczema, including heat and low humidity.
- Check your child’s sleeping conditions and ensure that the area is free
- of dust and upholstery that may contain dust mites.
Contact dermatitis is a kind of skin inflammation that occurs when substances touching your child’s skin cause irritation or an allergic reaction. The resulting red, itchy, dry or bumpy rash isn’t contagious or life-threatening, but it can be very uncomfortable.
Culprits for young children could include soaps, laundry detergent, rough fabric or even your baby’s own drool (sometimes referred to as drool rash).
If you can identify the offending agent and eliminate contact between it and your child, the contact dermatitis should clear up. Often, using an absorbent bib and changing it frequently, as well as applying a barrier cream such as petroleum jelly to the area of irritation, can help prevent the rash from worsening. In the meantime, a wet compress may help comfort your baby. Contact your child’s medical provider if the rash is severe or gets worse or if your baby’s skin is oozing or extremely itchy.
ImpetigoImpetigo is a highly contagious skin infection that mainly affects infants and children. It usually appears as red sores on the face, especially around a child’s nose and mouth.
The sores may be covered with a yellow brown scab or crust, or they may grow into blisters and pimples and ooze pus.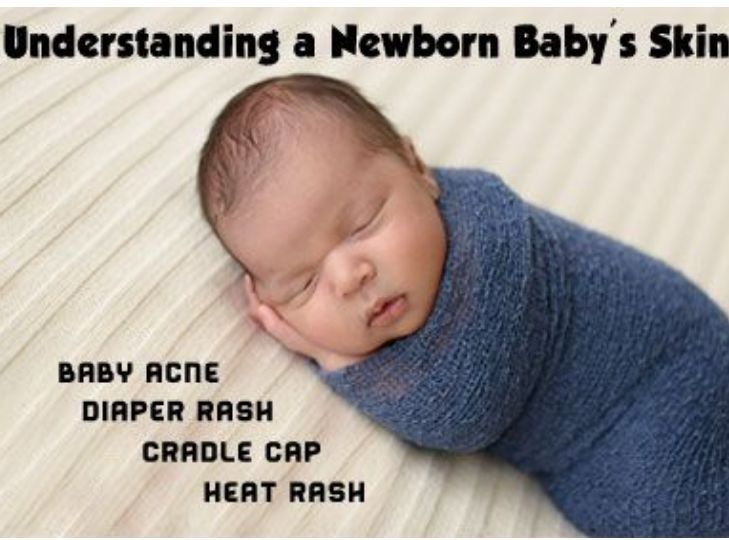
Although impetigo commonly occurs when bacteria enter the skin through cuts or insect bites, it can also develop in healthy skin. Because impetigo can sometimes lead to complications, your child’s medical provider may choose to treat impetigo with an antibiotic ointment or oral antibiotics.
Relevant reading
Mayo Clinic Guide to Your Baby’s First Years, Second Edition
Shop Now
Infant skin problems
When mothers go to the doctor's office, they are often concerned about the care of their babies' skin. In the first year of life, she is very thin and vulnerable. How to care for her, how to properly bathe a baby, how to deal with rashes? These questions are answered by the dermatovenereologist of the children's polyclinic No. 2 of the KGBUZ "KKTSOMD No. 2" L.P. Tretyakova.
I want to highlight some of the most common skin diseases in children of the first year of life.
Miliaria is a common problem in newborns. The appearance of prickly heat is due to overheating or insufficient skin care. On the skin of the neck, lower abdomen, upper chest, in the folds: axillary, inguinal, an abundance of small red nodules and spots appear.
The appearance of prickly heat is due to overheating or insufficient skin care. On the skin of the neck, lower abdomen, upper chest, in the folds: axillary, inguinal, an abundance of small red nodules and spots appear.
Skin irritation around the mouth (simple irritant contact dermatitis) . Saliva contains salt and digestive enzymes that irritate the baby's skin. Infants experience this phenomenon due to profuse salivation during teething at the age of 5-7 months, as well as sucking on a pacifier. For prevention, parents need to blot the skin in a timely manner with clean, dry wipes and wash the baby more often.
Diaper rash (diaper dermatitis). The appearance of diaper rash provokes the accumulation of moisture and friction. For example, excess moisture appears when a newborn overheats, stays in wet diapers for a long time. Friction occurs when using undershirts, diapers made of coarse fabric. On the skin, mainly in the buttocks, lower abdomen, genitals, inflammatory processes occur in the form of redness, irritation.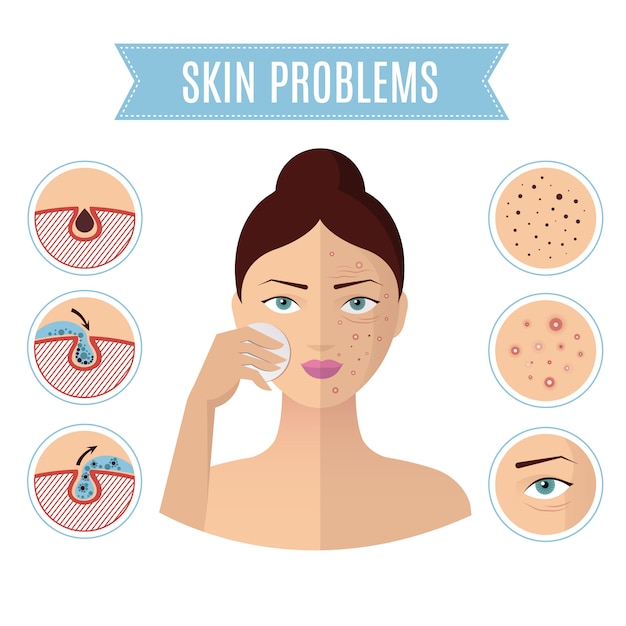 With a long process (more than 5 days), it is possible to attach a secondary infection (bacterial, fungal).
With a long process (more than 5 days), it is possible to attach a secondary infection (bacterial, fungal).
Proper home care will help eliminate and prevent skin problems.
1. Washing and bathing. Be sure to follow the daily care - keep the baby's skin dry and clean. It is necessary to immediately remove the remnants of the stool with a baby sanitary napkin, or, if possible, wash the child with warm water and lightly dry the skin with a towel. Never leave your baby's bottom wet or dirty. It is necessary to wash the child daily under a stream of warm water. Don't use soap frequently as it can dehydrate the skin and cause irritation. Detergents must be pH neutral and free from fragrances. Make sure that the room in which care is carried out after water procedures is warm.
2. Hydration.
Since baby's skin is very delicate, after washing, apply baby moisturizers (baby cream or emollients) to the baby's skin. Apply them with gentle light massaging movements, without rubbing. Repeat the procedure in the morning and evening, as well as after changing the diaper.
Repeat the procedure in the morning and evening, as well as after changing the diaper.
3. Diaper and diaper change.
With age, the parameters of the body and the nature of the bowel movements of your baby will change. When choosing diapers, you need to take these changes into account. Therefore, be guided by the age and weight of the child. And when the baby begins to actively move, we recommend switching to diaper panties. At the slightest irritation of the skin in the genital area, it is better to refuse diapers altogether (air baths).
When should you see a doctor?
If redness, itching, rashes appear on the skin, you should immediately consult a dermatologist or pediatrician, since the treatment of newborns and children of the first year of life requires special attention and an integrated approach. Self-medication is unacceptable.
Skin of a newborn baby [structure features, functions, care, overview of hygiene products]
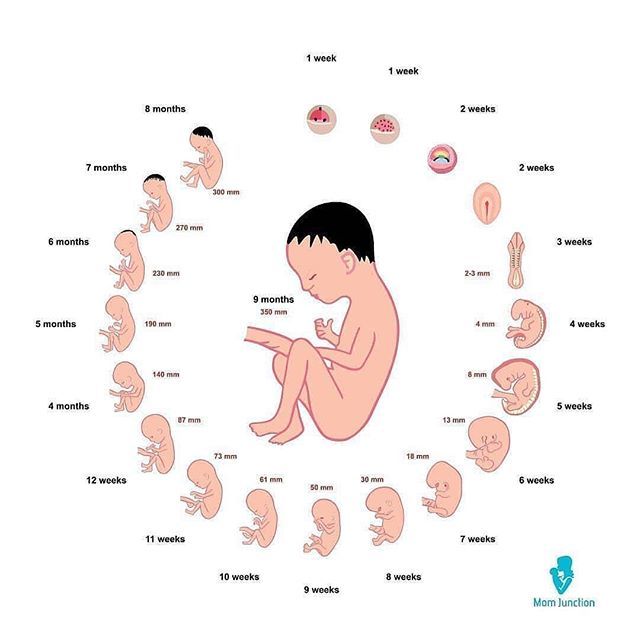
Newborn skin problems are common and every child will experience them to some extent. These problems are due to adaptation to the new environment. During fetal development, the child is in an aquatic environment with a constant temperature, and after birth, the body needs to adapt to an air environment saturated with microorganisms at a lower temperature.
These problems are due to adaptation to the new environment. During fetal development, the child is in an aquatic environment with a constant temperature, and after birth, the body needs to adapt to an air environment saturated with microorganisms at a lower temperature.
Consider the physiological characteristics of the skin of young children in more detail.
Features of the structure of the child's skin
Newborn skin consists of only 3 layers: basal, spiny and horny. The remaining layers are formed a little later.
Another physiological feature of the skin in infancy is its high water content and many vessels with thin permeable walls. Therefore, children's loose skin is so prone to allergic reactions.
It is the skin that is one of the first organs that undergoes structural changes. The most important changes that adapt the skin to the environment occur during the first 6-8 weeks of a child's life.
These include:
- increase in the density of cells in the stratum corneum of the skin,
- increase in the thickness of the epidermis and increase the barrier function of the skin of newborns,
- reducing the risk of pathogen entry
- maintaining optimal body temperature,
- as well as reducing transepidermal water loss.

These factors may influence the development of some skin conditions, but are not signs of any disease.
What is the skin pH of a newborn baby?
In the first days after birth, the skin of a newborn has a neutral pH - 7. But after 2-3 months it changes to a more acidic one - this significantly increases the protective properties of the epidermis.
Functions of the skin of a newborn
The skin of an infant, like the skin of an adult, performs several functions.
But there are differences:
- Protective function. Very poorly developed, because the dermis is very delicate, ph is neutral, and the lipid layer is insufficient.
- Suction function. Is at an excellent level for the same reasons as described above.
- Respiratory function. 10 times more oxygen penetrates through the skin into the baby's body than into the body of an adult.
- Excretory function.
 Practically absent. It develops only by 3 months, and the full sweat glands begin to work by 3 years.
Practically absent. It develops only by 3 months, and the full sweat glands begin to work by 3 years. - Temperature control function. Also poorly developed, because the sweat glands are not developed.
- Synthetic function of (eg formation of vitamin D). It starts working only by 3-4 weeks from birth.
- Tactile function. Normally developed.
Skin color of a newborn baby
What kind of skin should a newborn baby have normally? At birth, in the first hours of life, the epidermis may be dark - with a bluish or purple tint. This feature is due to the still weak blood circulation. In the future, hemoglobin in the blood rises, the baby's skin brightens and acquires a red tint. After 2-3 days, the redness disappears, the skin color changes again and may acquire a yellow tint. Normal pink or white skin color in the baby appears by the end of the first week of life.
Now let's look at the typical skin problems that parents face.
Erythema on the skin of newborns
This is a typical and very first reaction of a newborn to the outside world. Expressed by local redness, which may be accompanied by a small rash. It is a variant of the norm, passes within 1-2 days, treatment is not required.
Skin care for the umbilical wound of the baby
It concerns absolutely all parents, so it must be carried out carefully and correctly in order to avoid complications such as omphalitis (inflammation of the navel).
The umbilical cord and the umbilical wound must be cared for daily. Most often, the remnant of the umbilical cord falls off on days 4-5, and the navel is completely healed by about 10-14 days. In order for the healing process to occur quickly, and also to prevent infection, it is important to carefully care for the umbilical wound.
Keep your baby's navel dry and clean. With a cotton swab dipped in a solution of hydrogen peroxide, we carefully process all the folds of the umbilical ring. To dry the umbilical process and the umbilical wound, when it disappears, use a 5% solution of potassium permanganate or a solution of brilliant green, it is also possible to use solutions of chlorhexidine or chlorophyllipt.
To dry the umbilical process and the umbilical wound, when it disappears, use a 5% solution of potassium permanganate or a solution of brilliant green, it is also possible to use solutions of chlorhexidine or chlorophyllipt.
Navel care should be done 4-5 times a day. If there is swelling or redness of the skin around the navel, then you need to contact your pediatrician.
It is desirable to bathe a child already from the 2-3rd day of life, but it is necessary to refrain from water procedures on the day when the umbilical residue disappears, and the next day you can resume bathing.
Dryness and peeling of the skin in a newborn
Peeling of the skin in a newborn can be both a normal variant and the result of improper skin care for a child. Approximately every third baby is faced with physiological dryness of the skin. Let's see why a baby can peel off the skin and what to do in this case?
At birth, the baby's skin is covered with primordial cheesy grease.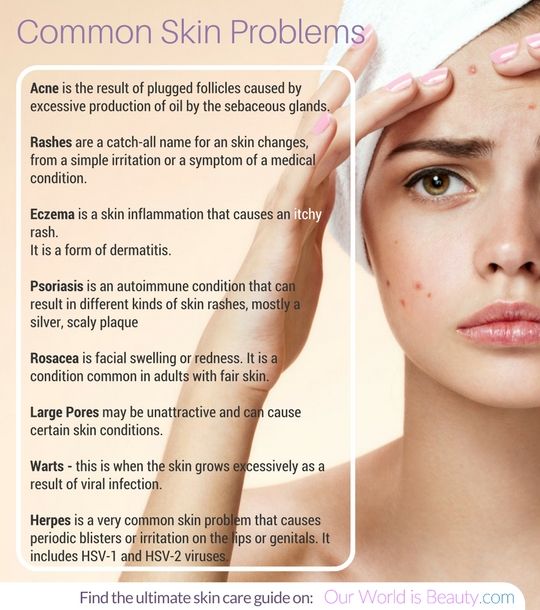 Its function is to protect the baby in the womb, help with the passage of the birth canal, and it also helps protect the skin during the transition from the aquatic environment to the air.
Its function is to protect the baby in the womb, help with the passage of the birth canal, and it also helps protect the skin during the transition from the aquatic environment to the air.
During the first 1-2 days of life, the original lubrication is completely absorbed into the skin, however, after birth, the baby is often cleansed of abundant lubrication, and if the baby is post-term (in this case, he is born practically without lubrication), the skin begins to peel off after a few days.
This is a natural process and this dryness can last up to a month. The skin of a newborn peels off both on the face and on the body. Particularly noticeable are small silvery scales on the arms and legs.
Baby's skin care in the period of physiological dryness
Peeling of the skin in a newborn cannot be prevented, but the restoration of the skin can be promoted by using moisturizing lipid-replenishing agents. It is only necessary to remember that the texture of such products should be very light (milk, emulsion, moisturizing lotion), they should be allowed to be used to care for the delicate skin of babies.
One such product is Lipikar Lait Milk for dry and very dry skin of babies, children and adults. Enriched with shea butter, cold cream and thermal water, the light texture of the products is instantly absorbed without leaving a sticky, greasy feeling on the skin.
Scabs on the head of a baby
This skin condition occurs in almost 50% of babies. It is sometimes called "gneiss", "baby cap" or "seborrheic crusts" because they resemble seborrhea. In infants, this is not a disease, but another of the adaptive responses. The reason for the appearance of crusts is the imperfect work of the sebaceous and sweat glands under the influence of transmitted maternal hormones during fetal development.
With age, the hormonal background of the child normalizes, the glands begin to work properly, and after a short period of time, this skin condition disappears. Crusts can appear regardless of whether the baby's hair is already growing or not. More often, crusts and greasy scales are not very pronounced and appear mainly in the region of the crown. Sometimes the crusts are large, yellowish-brown in color, located throughout the scalp and in the eyebrow area, and the baby may be disturbed by intense itching.
Sometimes the crusts are large, yellowish-brown in color, located throughout the scalp and in the eyebrow area, and the baby may be disturbed by intense itching.
Baby's skin care during gneiss
In no case do not try to mechanically tear off the crusts, there is a high risk of harm to health: you can easily injure the skin and cause an infection. In order to remove the crusts, you must first soften them, and then, while bathing, rinse gently so that they can be removed painlessly.
It is permissible to apply sterile oil (vaseline, olive, vegetable) to the scalp and put on a cotton cap for 1 hour - this will soften the crusts. After that, the cap can be removed and gently, gently massage the head with your fingertips. Then you need to bathe the baby and gently wash off the lagging crusts from the skin. Not all crusts may come off at one time, it will be necessary to repeat the procedure several times over several days.
For gentle gentle bathing, Lipikar AP+ Oil Lipid Replenishing Emollient Bath & Shower Oil can be used to gently cleanse and soothe dry skin in babies, children and adults. Shea butter included in the composition replenishes lipids. The oil does not irritate the baby's eyes, does not sting and the baby is comfortable.
Shea butter included in the composition replenishes lipids. The oil does not irritate the baby's eyes, does not sting and the baby is comfortable.
Neonatal acne
Also a fairly common skin problem in newborns that can be encountered. It occurs in about a third of babies. In appearance, it resembles adult acne, looks like red pimples with a white top. They can pop up on the skin of the face (cheeks, forehead, nose), sometimes on the ears, less often on the neck and back. The rashes do not itch and do not bother the child. The reason for their appearance are maternal hormones transmitted during fetal development. As the hormonal background normalizes, this problem on the skin is resolved. Sometimes a pediatrician may prescribe drying agents if there are a lot of rashes.
Prickly heat in infants
Another common problem in babies. It manifests itself as a multiple rash on the skin in the form of red “dots” and small pustules, localized on the face near the hairline, neck, upper chest and back. It appears as a result of overheating of the baby and insufficient hygiene (rare bathing), but it causes Staphylococcus aureus.
It appears as a result of overheating of the baby and insufficient hygiene (rare bathing), but it causes Staphylococcus aureus.
In order to prevent prickly heat on the skin, it is necessary to choose the right clothes, not to overheat the baby and observe hygiene. Indoors, it is recommended to maintain an air temperature of 20-22 degrees, and at night - about 18°C. Wear clothes made of natural cotton fabrics for your baby so that the skin “breathes”. With enough bathing, proper care, prickly heat usually goes away on its own. For prevention, use regular bathing and air baths.
For bathing it is recommended to use Lipikar Gel Lavant , it gently cleanses and protects the sensitive skin of babies, children and adults, soothes the skin, restores the natural protective barrier.
Diaper rash in newborns
Perhaps the most common and the most worrying problem for parents. Skin diaper rash is manifested by redness and the appearance of erosions on the skin. Most often, diaper rash occurs in places of natural folds: inguinal, cervical, axillary. And if you do not follow proper care, then infection is likely to join in places of diaper rash.
Most often, diaper rash occurs in places of natural folds: inguinal, cervical, axillary. And if you do not follow proper care, then infection is likely to join in places of diaper rash.
As with prickly heat, the causes are overheating of the skin, and in the buttocks and groin area, it is contact with urine and feces. Diaper rash in the groin has a special name - baby diaper dermatitis.
To avoid such problems with the skin of a newborn, it is necessary to wash the child after each toilet (if it is not possible, use wet wipes), as well as keep the skin open longer, carry out air baths so that the wrinkles are completely dry.
In case of redness and irritation, it is recommended to use healing repair products. Revitalizing and healing skin treatment for babies, children and adults Cicaplast balm B5 has a rich nourishing texture with Panthenol, which soothes dry, irritated skin, and [Copper-Zinc-Manganese] - a complex with recognized antibacterial properties.