Skin itchy after pregnancy
Causes and Treatments That Work
You’ve heard of new symptoms making their debut in the postpartum period, but did you know that one of them could be postpartum hives?
Hives happen when you get a bumpy skin rash, usually from an allergic reaction to something or a psychological cause like severe stress — and new parents know a little something about that.
Hives are a sign or symptom that your immune system isn’t quite in balance. They happen to about 20 percent of people (not just to new parents).
With postpartum hives, you can temporarily get this skin condition even if you’ve never had them before and even if you don’t have allergies. Don’t worry — hives normally go away as quickly as they appear. Here’s why you might have postpartum hives and what to do about it.
Hives can look like a red rash or raised bumps on the skin. They can sometimes look like other skin rashes such as eczema. Some people get an allergic rash that looks like hives at the end of their pregnancy or shortly after the birth of their baby.
If you have postpartum hives, you might have signs and symptoms like:
- skin rash on the face, neck, chest, stomach, arms, or legs (pretty much anywhere)
- single welts, large flat bumps, or patches on the skin
- skin bumps that are pink, red, or skin-colored
- skin bumps that blanche or turn white when you press on them
- flat, swollen bumps on the skin that can run together
- rough skin texture that looks like eczema
You might get postpartum hives or a skin rash for many reasons. If you don’t normally get hives, the cause could be linked to your pregnancy. You probably won’t get hives again once your body settles down post-baby.
Allergies
The most common cause of hives is an allergic reaction. No, you’re not allergic to your new baby: If you’ve never had allergies or only had very mild allergies before, you should know that pregnancy can make them worse. About a third of women have worsened asthma and allergy symptoms during pregnancy.
This might happen because the hormone rollercoaster ride you’re on while pregnant can tweak your immune system. All these changes in your body can lead to hives after pregnancy, too.
Changes in your diet during pregnancy (and after) might also change your gut health. This can sometimes trigger an overdrive in the immune system, causing allergies.
You might get postpartum hives because your body is more sensitive as it adapts to post-pregnancy changes. This can cause an allergic skin reaction if you’re around general allergens like:
- dust
- pollen
- mold and mildew
- animal fur and dander
- latex
- bug bites or stings
- chemicals, dyes, or perfumes
- medications such as aspirin, ibuprofen, and antibiotics (like amoxicillin and penicillin)
Infections
Infections from germs like bacteria and viruses can also temporarily throw your immune system out of whack. This might lead to postpartum hives and other allergy symptoms.
When you’re pregnant you’re more likely to catch a cold or flu. These germs might stay in your system, and will decide to annoy your immune system when it’s relaxed, right after the baby pops out.
You can also get infections down there, with so much going on during the birth! Infections that might trigger postpartum hives include:
- urinary tract infections
- strep throat
- other bacterial infections
- the common cold virus
- influenza virus
- hepatitis virus
- infectious mononucleosis (mono for short)
- other viral infections
Sluggish liver
Pregnancy can put your body into overdrive, especially the liver. This can make your liver slow down on its important work of filtering toxins and other junk from the blood. When this happens, liver enzymes might be temporary imbalanced or wastes might collect in your blood.
Both of these situations can lead to hives and other kinds of skin rashes. One medical case study found that this can happen near the end of pregnancy — around 36 weeks or right after delivery.
Liver causes of postpartum hives might lead to rashes on the face, stomach and legs. Along with hives, you might have other symptoms from a sluggish liver, like:
- fever
- swelling or bloating
- general itchiness
- fatigue (but that’s a given since you just had a baby!)
- high blood pressure (in rare cases)
Getting postpartum hives from a liver imbalance isn’t common. About 1 in every 200 pregnant or postpartum folks (0.5 percent) may get hives or a skin rash for this reason. You have a higher chance of getting this kind of skin rash if it’s your first pregnancy.
Other causes
Other causes of postpartum hives include physical, mental, and emotional aspects that might throw a wrench into your immune system. After all, there’s a lot to deal with and many changes to get used to right after your baby is born.
Other causes of postpartum hives may be linked to:
- not getting enough sleep
- sleeping at odd hours
- feeling anxious or depressed
- feeling stressed
- having a panic attack
- feeling cold or hot
- blood transfusions
- changes in your diet
- sun exposure
- exercising or other physical activity
- wearing tight clothing
How long postpartum hives last depends on the cause for this temporary skin condition. Hives that happen from most allergic reactions usually only last as long as your body takes to clear out the allergen. This might be a few minutes to hours or days.
Hives that happen from most allergic reactions usually only last as long as your body takes to clear out the allergen. This might be a few minutes to hours or days.
Your postpartum hives might return if you’re around the allergen again.
If you have postpartum hives from a liver imbalance it might clear up within a week of having your baby, or it may last as long as 6 weeks.
In most cases, you won’t need medical treatment for postpartum hives. Your doctor may prescribe medication to help control symptoms in serious cases. Treatment might include:
- skin steroid cream (like betamethasone valerate)
- an antihistamine (like pheniramine)
- anti-itch lotion or cream
- steroid medication (like prednisolone in cases of serious swelling and itching)
- an epinephrine (epi) pen
- allergy shots
- a medication called ursodeoxycholic acid (or Udiliv, only if the cause is a serious liver imbalance)
According to medical studies, steroid creams like betamethasone valerate and allergy medications like the antihistamine pheniramine are safe for people who are pregnant or breastfeeding.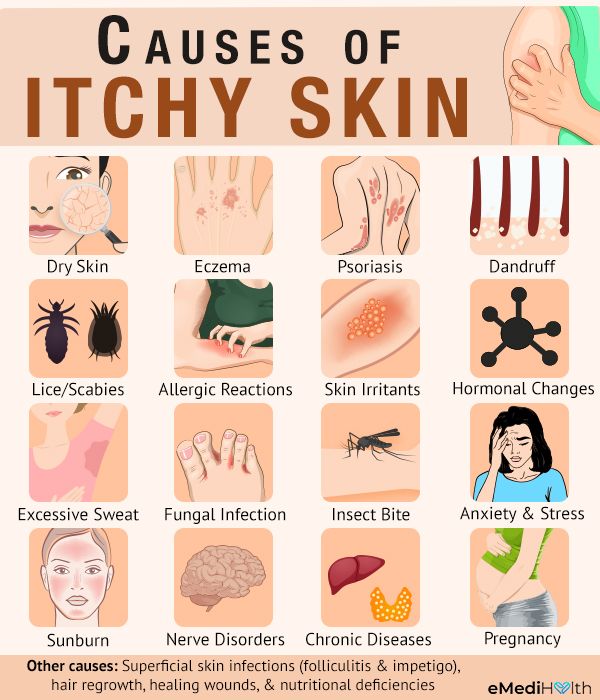 But if you have postpartum hives and you’re breastfeeding your baby, check with your doctor before applying or taking any kind of medication.
But if you have postpartum hives and you’re breastfeeding your baby, check with your doctor before applying or taking any kind of medication.
If you have allergies, you may need to see an allergy specialist to find out what you’re allergic to and find out if the allergies are here to stay.
Home remedies for postpartum hives help to soothe your skin and control itching. Try these tips to help slow down the scratching:
- have a cool (or lukewarm) bath
- take a nap or relax (after getting some help with your new little one!)
- apply pure aloe gel to help heal and soothe the area(s)
- apply a natural lotion like shea butter
- use wet wraps on the skin
- wear loose, breathable clothing (especially cotton fabrics)
- avoid allergens (if you know what you’re allergic to)
Tell your doctor if you get postpartum hives, even if it only happens once. Get urgent medical care if you have postpartum hives and other serious allergy symptoms, like:
- swelling of the face, lips, tongue, mouth, or throat
- difficulty breathing
- dizziness or lightheadedness
- fainting
- other anaphylaxis symptoms
See your doctor right away if you get hives more than once, if they don’t go away after a few days, or if you have serious itching. You might need medical treatment for the underlying cause of the postpartum hives.
You might need medical treatment for the underlying cause of the postpartum hives.
Also tell your doctor immediately if you get a skin rash and you’re not sure if it’s hives or something else.
Hives are a symptom of something else going on in your body, like allergies. Postpartum hives can happen for several reasons, even if you’ve never had allergies or other skin rashes before. They’re typically harmless to you and your baby.
However, you might need treatment if you have serious postpartum hives or if the cause of the hives is a chronic condition. Don’t take or apply any kind of medication for hives without checking with your doctor. This is especially important if you’re breastfeeding your baby.
7 Tips to Relieve Itchy Skin After Pregnancy
These tips to care for itchy skin after pregnancy are brought to you in collaboration with AmLactin® Skin Care.
It’s the postpartum side effect that literally drove me crazy, but no one warned me about it beforehand. I thought it would go away on its own, but two years later, I still deal with itchy skin after pregnancy.
I thought it would go away on its own, but two years later, I still deal with itchy skin after pregnancy.
Reading through pregnancy and childbirth forums on the web showed me just how common this is among new moms.
“I scratch in my sleep and don’t even know it.”
“I’ve scratched so hard that it left bruises.”
“Nothing seems to help! Not even allergy medicine!”
“My doctor doesn’t know what causes it.”
I poured over countless stories from other moms about how their lives were affected by itchy skin. And if you’ve experienced it too, then you know that I’m not just talking about a little annoyance like a mosquito bite.
Itchy skin after pregnancy is different. It feels like your skin is crawling. It feels like your skin is on fire. We’re adults and know better than to scratch, but sometimes you can’t help it.
This might not be a life-threatening condition, but it is excruciatingly irritating and embarrassing.
What causes itchy skin after pregnancy?
These are a few things that may cause postpartum rashes or skin issues:
- Changes in hormones
- Medications given during childbirth and recovery
- Thyroid issues
Often, however, there is no apparent culprit. And that makes it more difficult to find a solution, or even relief.
I’ve included affiliate links for your convenience; disclosure policy here.
What you can do to relieve itchy skin after pregnancy
If you’re not sure what is causing your skin irritation, you may consider visiting your healthcare provider. They can determine if there are any underlying serious medical conditions present.
If your doctor doesn’t have a clear answer, here are some tips that I used to finally find relief. Sometimes it is a process of elimination in finding the combination that works for you!
Read this next: 5 Surprisingly Easy Weight Loss Tricks for Breastfeeding Moms
1. Don’t use hot water to shower or bathe.
Hot water drys out skin, and can lead to irritation. Lukewarm or room temperature is gentler on sensitive skin.
2. Read the labels on your skincare products — it might be time to switch!
Pre-pregnancy, I could use pretty much any type of lotion with no ill effects. All that went out the window after the baby! If I am not extra careful about the lotion I use, my skin will feel worse than before.
Read the labels on all your products! Some ingredients to watch out for:
- Added fragrances
- Ethanol alcohol (labeled as Alcohol Denat.
 , SD Alcohol 3-A, SD Alcohol 30, SD Alcohol 39, SD Alcohol 39-B, SD Alcohol 39-C, SD Alcohol 40, SD Alcohol 40-B, SD Alcohol 40-C or alcohol.)
, SD Alcohol 3-A, SD Alcohol 30, SD Alcohol 39, SD Alcohol 39-B, SD Alcohol 39-C, SD Alcohol 40, SD Alcohol 40-B, SD Alcohol 40-C or alcohol.)
Note: There are actually good alcohols which function differently than those listed above. These so-called “fatty alcohols” have beneficial moisturizing properties: cetyl alcohol, cetearyl alcohol, stearyl alcohol, behenyl alcohol, arachidyl alcohol and myristyl alcohol.
After a long process of testing various lotions, I found one that worked so well that I had to share. AmLactin® Ultra Hydrating Cream far exceeded my expectations — it almost seemed like a miracle!
Where to buy: Find AmLactin Ultra Hydrating Cream on Amazon
The first time I tried AmLactin® Ultra Hydrating Cream, I experienced instant relief. No more itching! After a couple days, the embarrassing red bumps on my legs started to disappear.
After two years of worrying about itchy, bumpy skin, I finally could forget about my legs and just go about my day!
I apply AmLactin® Ultra Hydrating Cream immediately after showering — it’s thick and creamy, so a little bit goes a long way. Amazingly, I rarely need to reapply before my next shower, because my skin stays soft and hydrated for almost 24 hours.
3. Change your razor weekly and avoid those with “moisture or gel strips”
It didn’t occur to me for months that my razor could be part of the problem! Razors with gel or lotion strips definitely make for a smoother shave, but there is no telling what they’re made from. Choosing a razor free of additives that end up on your legs could help bring instant relief — it made a big difference for me!
You also want to be sure and change your razor regularly because blades dull over time, causing nicks and the dreaded “razor burn. ” Older cartridges may also be a breeding ground for nasty bacteria, putting your skin at greater risk for irritation or even infection. If you shave every day, consider swapping your blade after a week or two at most. And if your blade shows any signs of wearing or rusting, it’s time to toss it!
” Older cartridges may also be a breeding ground for nasty bacteria, putting your skin at greater risk for irritation or even infection. If you shave every day, consider swapping your blade after a week or two at most. And if your blade shows any signs of wearing or rusting, it’s time to toss it!
4. Wash clothes in a detergent free of perfumes and dyes
Perfumes, dyes, etc. in your laundry detergent can stay on clothes, irritating your skin when you wear them. Look for a detergent specifically designed for sensitive skin (baby detergent is an option too).
5. Use natural fabric softeners
For the same reason I use “free and clear” detergent, I avoid chemical-laden fabric softener sheets. I wrote a post about my easy trick to fluff pillows, and this is also what I use when drying clothes.
6. Hydrate on the inside and out
Dehydration can lead to skin issues, so make sure you’re drinking at least 8-10 glasses of water daily. (If you’re breastfeeding, you’ll want to increase your intake).
(If you’re breastfeeding, you’ll want to increase your intake).
If you live in an arid climate or spend a lot of time indoors with the heater on, a humidifier can help make sure that the air around you isn’t drying out your skin.
7. Lower your stress levels
This one is easier said than done, but it is SO important! Stress can cause our hormones to get out of whack, and hormone imbalances are a common culprit of skin issues.
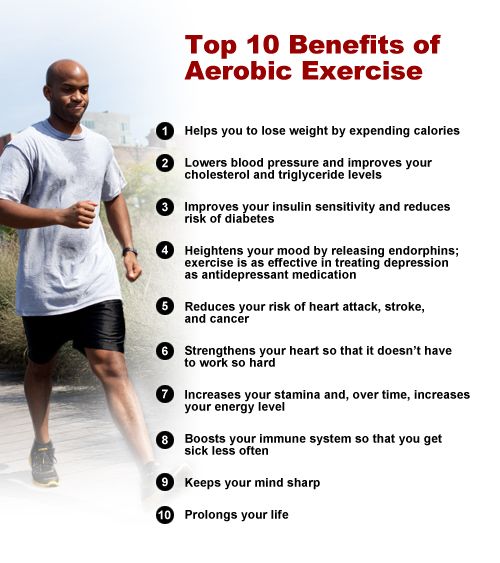
Exercise, a balanced diet, and getting the recommended amount of sleep are all key factors in balancing stress levels.
Related: 10 Ways to Improve Your Mood and Get out of the So-called “Mom Funk.”
More of our most popular posts on pregnancy and postpartum care
- The Best pregnancy pillow reviews for 2019 (sleep better and reduce pain)
- How to Get Your Body Confidence Back After Baby #2
- What is Postnatal Depletion and What Moms Can Do About it
- Do Postpartum Belly Bands Really Work?
- 18 Things You Should Do with a New Baby
- Don’t Call my C-Section a “Belly Birth”
- How to Lose Weight While Breastfeeding
Enter to win $100 of AmLactin Skin Care Products!
I can’t say enough about what a relief (literally!) AmLactin Ultra Hydrating Cream is for my skin and for my day-to-day life. If you’re suffering in silence from dry, itchy, or irritated skin, it’s absolutely worth a try!
If you’re suffering in silence from dry, itchy, or irritated skin, it’s absolutely worth a try!
Where to buy: Find AmLactin Ultra Hydrating Cream on Amazon
I’m also hooked on AmLactin® Foot Cream because it works wonders on my rough heels. Since I exercise daily, my feet take a bit of a beating. Even with regular exfoliation, I still find rough, dry patches that make me want to wear socks all day (not always a practical option in the Texas heat)! AmLactin® Foot Cream has made a huge difference and I finally treated myself to a pedicure since I’m not afraid to show my feet anymore!
GIVEAWAY CLOSED Thank you to everyone who entered!
On 10/28/16, I will randomly pick 1 commenter to win $100 worth of AmLactin products!
*Giveaway is open to United States residents only. Product and shipping provided by AmLactin Skin Care.
Product and shipping provided by AmLactin Skin Care.
Uncover smooth, radiant skin with AmLactin Alpha-Hydroxy Skin Care. Its unique exfoliating and hydrating alpha-hydroxy therapy gently removes dead skin cells to reveal soft, hydrated skin. It’s the difference between skin care and skin therapy. AmLactin moisturizers are available on Amazon.com and at your local Target, CVS, Walgreens, Costco, Walmart and Rite Aid.
This is a sponsored conversation written by me on behalf of AmLactin Skin Care. The opinions and text are all mine.
- Author
- Recent Posts
Stacey aka the Soccer Mom
Stacey is the creator of The Soccer Mom Blog, a Houston Texas mom blog that focuses on positive living for women and families. She loves to share real food recipes, money-saving tips, parenting encouragement, kids activities, DIY tutorials, home hacks, fitness, and so much more! To get to know Stacey even better, click here.
Latest posts by Stacey aka the Soccer Mom (see all)
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood. This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Itchy skin / Dermatology / Health Articles / Articles and Encyclopedia / madez.ru
Itchy skin is the most common symptom that comes from the skin, which is defined as “a special feeling of irritation that makes you want to scratch it”.
Pruritus is in most cases the first symptom encountered by the patient and his doctor.
Itching may be a symptom of a skin disease, and in 10-50% of cases, itching may be the first visible symptom of a systemic disease. Therefore, it is very important to consult a dermatologist in the presence of pruritus in order to determine the true cause of pruritus.
Pruritus may be localized, involving a limited area of the skin, but may also be generalized, involving most of the skin.
If left untreated, itching leads to secondary skin rashes in the form of: redness, scratching, bloody crusts, erosions. Very often, when combing, an infection joins and pyoderma occurs.
Very often, when combing, an infection joins and pyoderma occurs.
Pruritus can occur in different age groups and has its own characteristics of the course.
- Chronic itching in children can be caused by skin diseases such as:
- Lamellar and X-linked ichthyosis
- Epidermolysis bullosa
- Atopic dermatitis, the prevalence of which in pediatrics is up to 22%.
- Mild to moderate itching occurs in 13.8% of adolescents with acne.
The incidence of pruritus due to systemic diseases is lower in children than in adults.
- Itching in pregnant women occurs in about 18% of pregnant women and is the dominant symptom in specific dermatosis of pregnancy: polymorphic dermatosis of pregnancy, pemphigoid of pregnancy, intrahepatic cholestasis of pregnancy, atopic rashes in pregnancy.
- The prevalence of pruritus in the elderly ranges from 11.5 to 29%. The most common cause is xerosis of the skin.
 Patients note increased itching in winter and autumn.
Patients note increased itching in winter and autumn.
Skin itching, as one of the symptoms of a skin disease, is often observed in:
- Inflammatory dermatoses: atopic dermatitis, allergic, irritant contact dermatitis, pink lichen, seborrheic dermatitis, mastocytosis, miliaria, etc.
- Infectious dermatoses: mycoses, scabies, pediculosis, bacterial and viral infections, insect bites.
- Autoimmune dermatoses: bullous dermatoses, Dühring's dermatitis herpetiformis, bullous pemphigoid.
- Genodermatosis: Darier disease, Hailey-Hailey disease.
- Dermatosis of pregnancy: polymorphic exanthema of pregnancy, infectious vulvovaginitis, pemphigoid of pregnancy.
- Neoplasia: cutaneous T-cell lymphoma, cutaneous B-cell lymphoma, leukemic infiltrates.
Skin itching as one of the symptoms of a systemic disease can be observed in:
- Metabolic disorders (chronic renal morbidity, hepatopathy (cholestasis), hyper-, hypothyroidism, diabetes mellitus, malabsorption, celiac enteropathy, pruritus during menopause)
- Hematological diseases (iron deficiency, polycythemia vera, hypereosinophilia syndrome, Hodgkin's disease, non-Hodgkin's lymphoma, systemic mastocytosis)
- Malignant neoplasms (carcinoma of the cervix, prostate, colon)
- HIV/AIDS
- Complications of drug therapy
- Neuropsychiatric diseases (postherpetic neuralgia, multiple sclerosis; tumors, abscesses, infarctions of the central nervous system or spinal cord, stress, overwork; psychiatric diseases (depression, tactile hallucinosis, schizophrenia))
consult a dermatologist for the doctor to establish the true cause of the itching and prescribe the appropriate treatment.