Signs of infant hip dysplasia
Developmental Dysplasia of the Hip (for Parents)
What Is Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip (DDH) is a problem with the way a baby's hip joint forms. Sometimes the condition starts before the baby is born, and sometimes it happens after birth, as the child grows. It can affect one hip or both.
Most infants treated for DDH develop into active, healthy kids and have no hip problems.
What Happens in a Hip With Developmental Dysplasia?
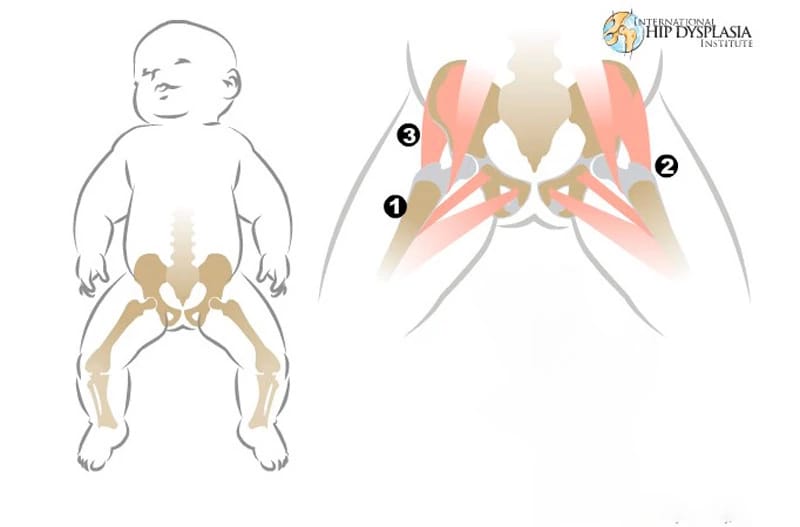
The hip joint is a ball and socket joint. The top part of the thighbone (the ball part of the hip) sits inside a socket that's part of the pelvic bone. The ball moves around in different directions, but always stays inside the socket. This lets us move our hips front, back, and side to side. It also supports our body weight for walking and running.
In DDH, the hip does not form well. The ball part of the joint may be completely, or partly, out of the socket. Sometimes the ball part may slide in and out of the socket. Often, the socket is shallow. If this is not fixed, the hip joint will not grow well. This can lead to pain with walking and hip arthritis at a young age.
What Are the Signs & Symptoms of Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip doesn't cause pain in babies, so can be hard to notice. Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Parents could notice:
- The baby's hips make a popping or clicking that is heard or felt.
- The baby's legs are not the same length.
- One hip or leg doesn't move the same as the other side.
- The skin folds under the buttocks or on the thighs don't line up.
- The child has a limp when starting to walk.
Babies with any of these signs should see a doctor to have their hips checked. Finding and treating DDH early usually means there's a better chance for a baby's hips to develop normally.
What Is Hip Laxity?
Many babies are born with hips that feel loose when moved around.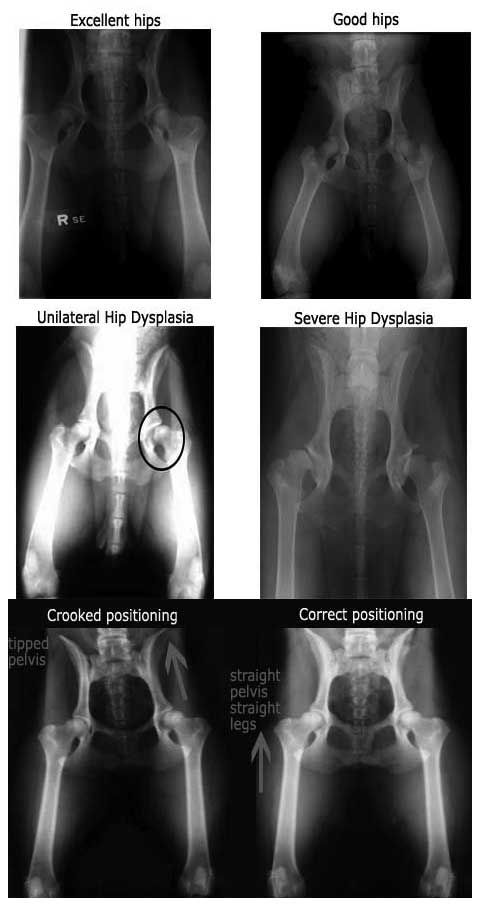 This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
A baby's whose hip ligaments are still loose after 6 weeks might need treatment. So follow-up doctor visits for babies with hip laxity are important.
Who Gets Developmental Dysplasia of the Hip?
Any baby can have DDH. But there's a higher chance of being born with it in babies who:
- are girls
- are first-born
- were breech babies (in the womb buttocks-down instead of head-down), especially during the third trimester of pregnancy
- have a family member with the condition, such as parent or sibling
Rarely, a baby isn't born with DDH, but develops it after birth. To prevent DDH in babies who aren't born with it, don't swaddle a newborn's hips or legs tightly together.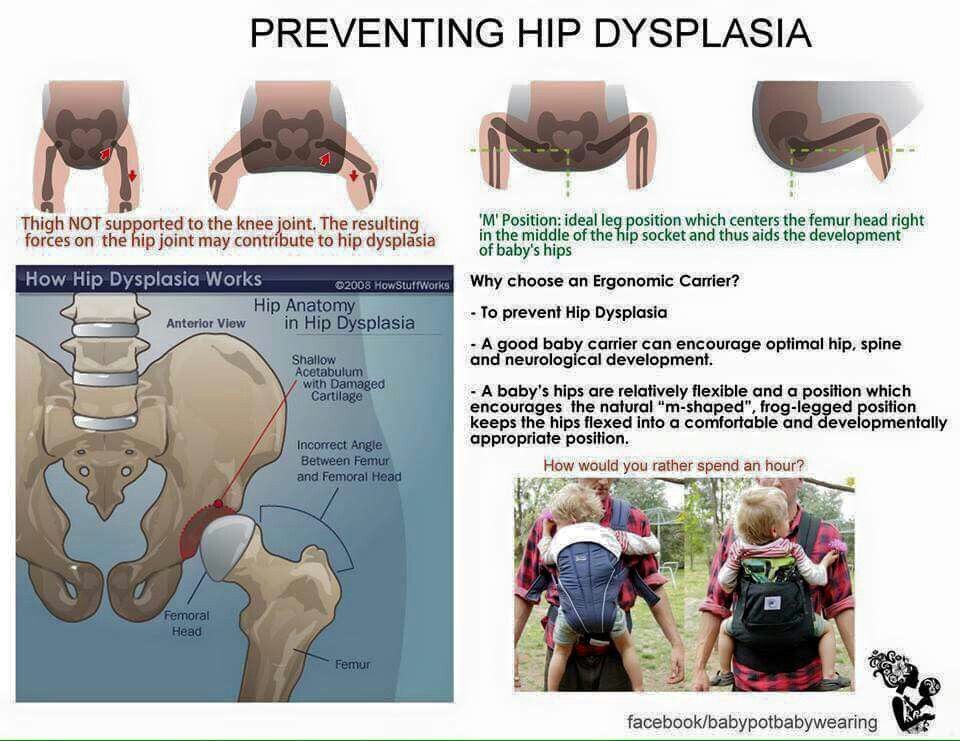 Always make sure a baby's legs have plenty of wiggle room.
Always make sure a baby's legs have plenty of wiggle room.
How Is Developmental Dysplasia of the Hip Diagnosed?
Doctors find most cases of DDH during well-child exams. If a baby has signs of DDH or has a higher risk for it, the doctor will order tests.
Two tests help doctors check for DDH:
- An ultrasound uses sound waves to make pictures of the baby's hip joint. This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray.
- An X-ray works best in babies older than 4–6 months. At that age, their bones have formed enough to see them on an X-ray.
How Is Developmental Dysplasia of the Hip Treated?
A pediatric orthopedic surgeon (a specialist in children's bone conditions) cares for babies and kids with DDH. The goal of care is to get the ball of the hip in the socket and keep it there, so the joint can grow normally.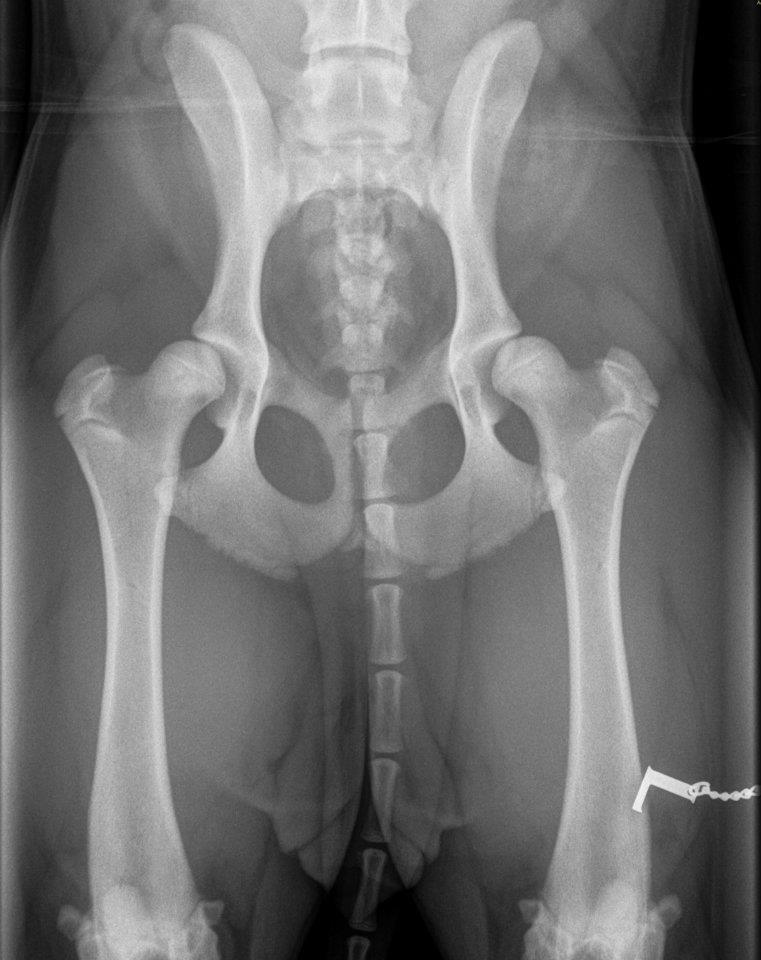
The orthopedic surgeon chooses the treatment based on the child's age. Options include:
- bracing
- a closed reduction and casting
- an open reduction (surgery) and casting
A brace or cast will hold the hip in place and will be on both sides, even if only one hip is affected.
Bracing
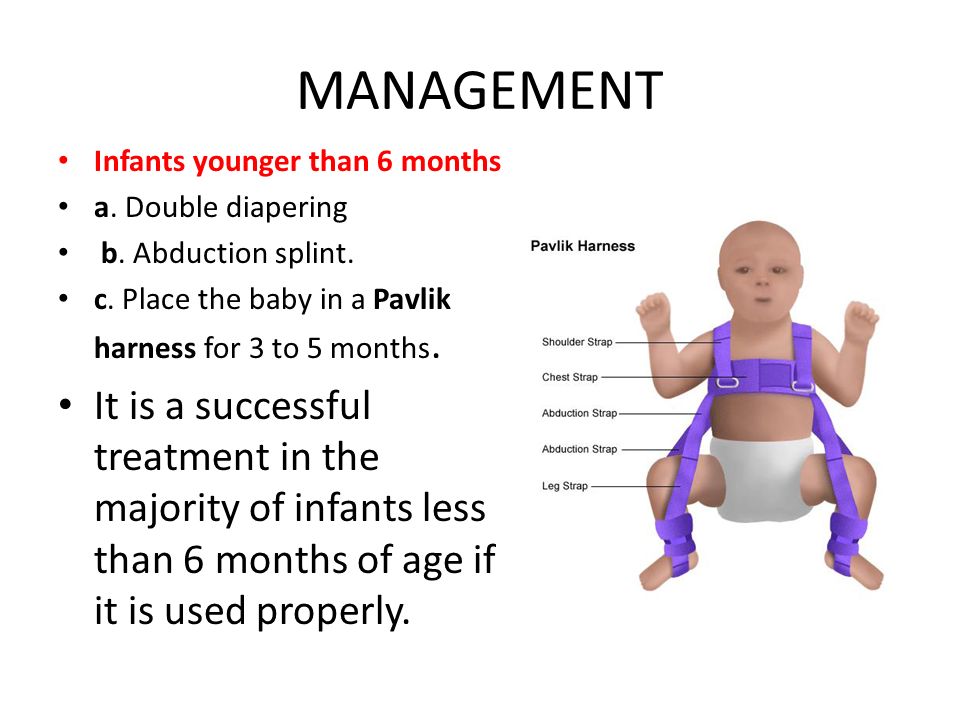
Treatment for babies younger than 6 months old usually is a brace. The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
Treatment with the Pavlik harness often lasts about 6–12 weeks. While wearing the harness, the baby has a checkup every 1–3 weeks with hip ultrasounds and exams. During the visit, the medical team can adjust the harness if needed.
The harness (brace) usually works well to keep the hips in position. Most babies won't need other treatment.
Rarely, the harness isn't able to keep the ball of the hip in the socket. Then, doctors might do either:
Then, doctors might do either:
- a closed reduction (manually moving the ball back into the socket) and casting
- an open reduction (surgery) and casting
Closed Reduction and Casting
A child might need a closed reduction if:
- The harness was not successful at keeping the ball of the hip in the socket.
- A baby starts care after age 6 months.
For a closed reduction, the baby gets medicine (general anesthesia) to sleep through the procedure and not feel pain. The surgeon:
- Injects contrast dye into the joint to see the cartilagepart of the ball.
- Moves the baby's thighbone so that the ball of the joint goes back into place in the socket.
- Puts on a hip spica cast to hold the hip in place. The baby wears the cast for 2–4 months.
Sometimes, the orthopedic surgeon also loosens the tight muscle in the groin during the closed reduction.
Open Reduction (Surgery) and Casting
A child might need surgery (an open reduction) if:
- The closed reduction was not successful at keeping the ball of the hip in the socket.

- The child is older than 18 months when starting treatment.
During an open reduction, the child is asleep under anesthesia. The surgeon:
- Makes a cut through the skin.
- Moves muscles out of the way to see the hip joint directly.
- Puts the ball back into place.
- Closes the surgical cut with stitches placed under the skin. These won't need to be removed.
- Puts on a hip spica cast to hold the hip in place. The child wears the cast for 6–12 weeks.
Sometimes, the orthopedic surgeon also does a surgery on the pelvic bone to deepen a very shallow hip socket, especially for a child older than 18 months.
What Else Should I Know?
Kids will have regular checkups with their orthopedic specialist until they're 16–18 years old and done growing. These help make sure the hip develops well.
Hip Dysplasia | Boston Children's Hospital
Listen
What is hip dysplasia?
The hip is a ball-and-socket joint.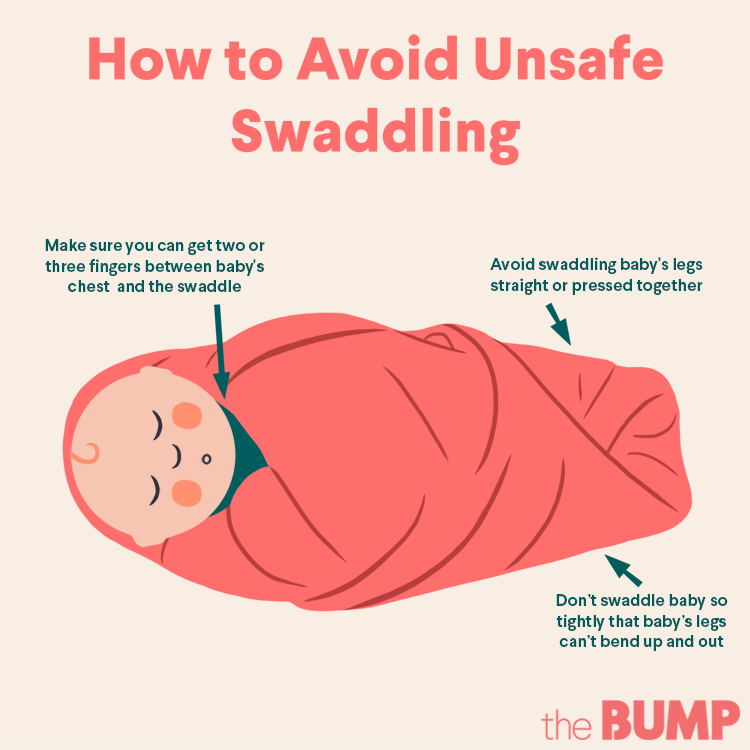 Normally, the ball at the top of the thigh bone fits into the hip socket. Hip dysplasia occurs when the hip joint has not developed properly and the socket (acetabulum) is too shallow. This allows the ball (femoral head) to slip partially or completely out of the joint. Hip dysplasia ranges from a mild abnormality to a complete dislocation of the hip.
Normally, the ball at the top of the thigh bone fits into the hip socket. Hip dysplasia occurs when the hip joint has not developed properly and the socket (acetabulum) is too shallow. This allows the ball (femoral head) to slip partially or completely out of the joint. Hip dysplasia ranges from a mild abnormality to a complete dislocation of the hip.
Severe cases of hip dysplasia are usually diagnosed during a routine screening within the first few months of a baby’s life. Other times, the problem may only become noticeable as a child grows and becomes more active.
Hip dysplasia is a treatable condition. However, if left untreated, it can cause irreversible damage that will cause pain and loss of function later in life. It is the leading cause of early arthritis of the hip before the age of 60. The severity of the condition and catching it late increase the risk of arthritis. Therefore, monitoring and early intervention are both important to reduce a child’s risk of pain and disability in adulthood.
Who is affected?
Hip dysplasia can affect anyone at any age. Although it is believed to develop around birth, a child with mild dysplasia may not have symptoms for years, or even decades.
- Hip dysplasia in babies is known as infant developmental dysplasia of the hip (DDH).
- When diagnosed in adolescents and young adults, it is sometimes called acetabular dysplasia.
The age at which older kids and young adults with hip dysplasia begin to notice symptoms depend on the severity of the condition and their activity level. Athletes who place a lot of load on their hips by participating in dance, hockey, football, soccer, or track and field may experience symptoms sooner.
Meet Louise
Undiagnosed hip dysplasia caused such severe knee pain, this former track star sometimes had trouble walking after competitions. With surgery behind her, and a degree in medicine in the works, she has returned to the sport she loves.
Read her story
Girls and women are two to four times more likely than boys to have hip dysplasia. It also tends to affect first-born children and those who have a close family member with hip problems. Some people with hip dysplasia are affected in only one hip while others have it in both hips.
In boys, the condition tends to be accompanied by other hip problems. These include acetabular retroversion (when the hip socket grows too far over the head of the femur) or CAM lesions (extra bone growth on the surface of the bone that causes extra friction and joint damage).
Hip dysplasia is sometimes confused with hip impingement, which occurs when extra bone grow on the acetabulum or femoral head. The irregular shape creates friction within the joint and wears down cartilage. Some patients have both conditions, both of which cause hip pain and are easy to confuse. However, they are different issues that require different treatments.
Image
Image
Generally speaking, treating hip dysplasia as early as possible can minimize joint damage and reduce the chance of early onset arthritis.
How we care for hip dysplasia
The Child and Young Adult Hip Preservation Program at Boston Children’s Hospital is at the forefront of research and innovation. We combine specialized expertise in non-surgical and surgical treatments with structured physical therapy to help children, adolescents, and young adults live healthy, active lives.
Our team has treated thousands of children with every level of complexity and severity of hip deformity. Our hip specialists have pioneered minimally invasive procedures as well as open surgical techniques to help treat patients of all ages. We perform more periacetabular osteotomy (PAO) procedures every year than any other hospital in the country and have helped hundreds of athletes return to the activities they love.
We have the experience to treat you or your child. Our goal is the same as yours: to help you get better so you can return to being healthy and pain-free.
Patient resources
Download these fact sheets to learn more about hip dysplasia and treatment options.
- fact sheet: developmental dysplasia of the hip (DDH)
- fact sheet: Pavlik harness
- fact sheet: hip dysplasia in adolescents and young adults
Hip Dysplasia | Hip Dysplasia in Adolescents
What is hip dysplasia in adolescents?
Hip dysplasia occurs when the hip socket (acetabulum) doesn't develop properly and is too shallow to cover the head of the thigh bone (femoral head) completely. Many adolescents and young adults with the condition were born with developmental dysplasia of the hip (DDH). In others, previously healthy hips did not develop properly as their bones and bodies grew.
Meet Alana and Nicole
A year and a half after hip surgery, Nicole still questioned her physical capabilities. That changed when she met Alana, another dancer who’d had the same surgery. This chance meeting became a turning point in both dancers' healing.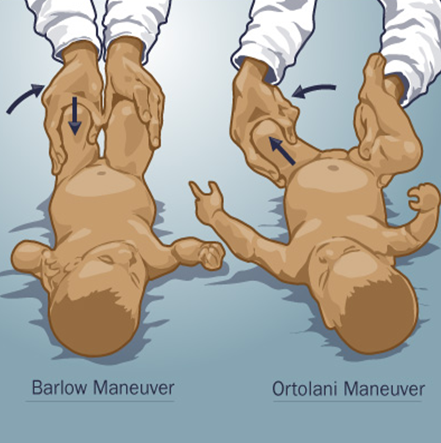
Read their story
The condition ranges from a mild abnormality of the hip socket to a complete dislocation of the hip. As children become more active and demand more of their legs, the ill-fitting hip joint becomes unstable. The instability damages cartilage inside the joint that becomes increasingly painful over time.
It is important not to ignore hip pain. Hip dysplasia is a treatable condition but early diagnosis and treatment are critical to preventing irreversible damage.
What are the symptoms of hip dysplasia in adolescents and young adults?
Teens or young adults may develop a limp or have hip pain in the front of the hip or groin. For others, the first sign is knee pain. You might hear a clicking sound in your hip. As the damage progresses, you may find it more and more painful to participate in sports and other activities. Without treatment, the pain will continue to become worse.
What causes hip dysplasia in adolescents and young adults?
Some teens and young adults are born with mild DDH that becomes symptomatic as they grow. However, the hip joint continues to develop throughout the teen years and sometimes does not develop properly, even if you were not born with DDH. Doctors are not sure why this happens but they do know that the condition affects girls two to four times as often as boys. People with a close relative with hip problems are also at higher risk.
However, the hip joint continues to develop throughout the teen years and sometimes does not develop properly, even if you were not born with DDH. Doctors are not sure why this happens but they do know that the condition affects girls two to four times as often as boys. People with a close relative with hip problems are also at higher risk.
Image
Image
How is hip dysplasia diagnosed in adolescents and young adults?
Doctors typically use variety of tests to determine if dysplasia is the source of hip pain in adolescents and young adults.
The first step is a thorough patient history and physical exam. The doctor will check your hip for range of motion. They may order imaging studies such as an x-ray, MRI, or CT scan to confirm the diagnosis. Ultrasound-guided diagnostic injection can help your doctor determine the location of your hip pain with greater precision.
How is hip dysplasia treated in adolescents and young adults?
The goal of treatment is to restore normal hip function and eliminate pain. Your treatment will depend on the severity of your condition.
Your treatment will depend on the severity of your condition.
Non-surgical treatment options for adolescents and young adults
Mild to moderate cases of hip dysplasia are often treated with physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDs). If you continue to be in pain after these treatments, your physician may suggest surgery.
Surgical options for adolescents and young adults
Periacetabular osteotomy (PAO) is the main surgical treatment for adolescents and young adults with hip dysplasia. PAO may serve as a lifelong treatment if performed before serious damage occurs within the joint.
The goals of PAO are to:
- reduce or eliminate pain
- maximize the function of your hip
- enable you to return to sport or other activity
Hip Dysplasia | Hip Dysplasia in Babies
What is hip dysplasia in babies?
Hip dysplasia in babies, also known as developmental dysplasia of the hip (DDH), occurs when a baby’s hip socket (acetabulum) is too shallow to cover the head of the thighbone (femoral head) to fit properly. DDH ranges in severity. Some babies have a minor looseness in one or both of their hip joints. For other babies, the ball easily comes completely out of the socket.
DDH ranges in severity. Some babies have a minor looseness in one or both of their hip joints. For other babies, the ball easily comes completely out of the socket.
Image
What are the symptoms of hip dysplasia in babies?
Many babies with DDH are diagnosed during their first few months of life.
Common symptoms of DDH in infants may include:
- The leg on the side of the affected hip may appear shorter.
- The folds in the skin of the thigh or buttocks may appear uneven.
- There may be a popping sensation with movement of the hip.
What causes hip dysplasia in babies?
The exact cause is unknown, but doctors believe several factors increase a child’s risk of hip dysplasia:
- a family history of DDH in a parent or other close relative
- gender — girls are two to four times more likely to have the condition
- first-born babies, whose fit in the uterus is tighter than in later babies
- breech position during pregnancy
- tight swaddling with legs extended
Breech position: Babies whose bottoms are below their heads while their mother is pregnant with them often end up with one or both legs extended in a partially straight position rather than folded in a fetal position.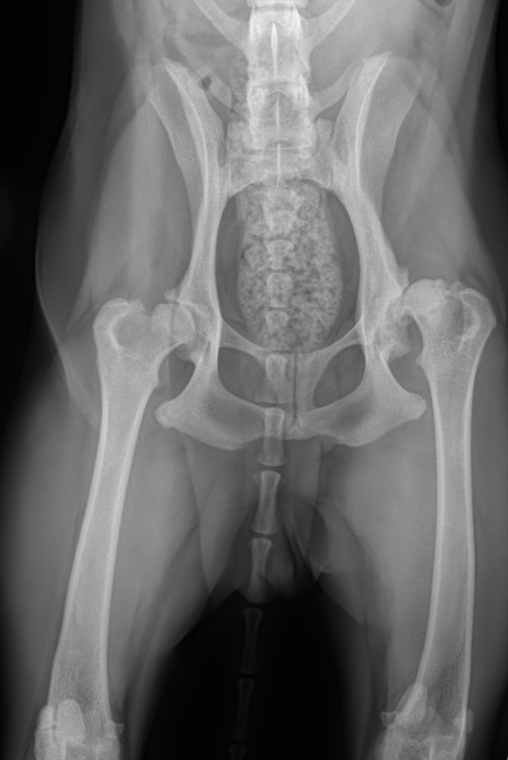 Unfortunately, this position can prevent a developing baby’s hip socket from developing properly.
Unfortunately, this position can prevent a developing baby’s hip socket from developing properly.
Tight swaddling: Wrapping a baby’s legs in a straight position may interfere with healthy development of the joint. If you swaddle your baby, you can wrap their arms and torso snugly, but be sure to leave room for their legs to bend and move.
Angela's story
Angela was 5 when her parents brought her to Boston Children’s Hospital, where she was diagnosed with hip dysplasia in both hips.
How is hip dysplasia diagnosed?
Infants in the U.S. are routinely screened for hip dysplasia. During the exam, the doctor will ask about your child’s history, including their position during pregnancy. They’ll also ask if there is any history of hip problems on either parent’s side.
The doctor will do a physical exam and order diagnostic tests to get detailed images of your child’s hip. Typical tests can include:
- Ultrasound (sonogram): Ultrasound uses high-frequency sound waves to create pictures of the femoral head (ball) and the acetabulum (socket).
 It is the preferred way to diagnose hip dysplasia in babies up to 6 months of age.
It is the preferred way to diagnose hip dysplasia in babies up to 6 months of age. - X-ray: After a child is 6 months old and bone starts to form on the head of the femur, x-rays are more reliable than ultrasounds.
How is hip dysplasia treated?
Your child’s treatment will depend on the severity of their condition. The goal of treatment is to restore normal hip function by correcting the position or structure of the joint.
Non-surgical treatment options
Observation
If your child is 3 months or younger and their hip is reasonably stable, their doctor may observe the acetabulum and femoral head as they develop. There’s a good possibility the joint will form normally on its own as your child grows.
Pavlik harness
If your child’s hip is unstable or sufficiently shallow, their doctor may recommend a Pavlik harness. The Pavlik harness is used on babies up to four months old to hold their hip in place while allowing their legs some movement. The baby usually wears the harness all day and night until their hip is stable and an ultrasound shows their hip is developing normally. Typically, this takes about eight to 12 weeks. Your child’s doctor will tell you how many hours a day your child should wear the harness. Typically, children wear the harness 24 hours a day.
The baby usually wears the harness all day and night until their hip is stable and an ultrasound shows their hip is developing normally. Typically, this takes about eight to 12 weeks. Your child’s doctor will tell you how many hours a day your child should wear the harness. Typically, children wear the harness 24 hours a day.
Image
While your child is wearing the harness, their doctor will frequently examine the hip and use imaging tests to monitor its development. After successful treatment, your child will need to continue to see the doctor regularly for the next few years to monitor the development and growth of their hip joint.
Typically, infants’ hips are successfully treated with the Pavlik harness. But some babies’ hips continue to be partially or completely dislocated. If this is the case, your child’s doctor may recommend another type of brace called an abduction brace. The abduction brace is made of lightweight material that supports your child’s hips and pelvis. If your child’s hip becomes stable with an abduction brace, they will wear the brace for about eight to 12 weeks. If the abduction brace does not stabilize the hip, your child may need surgery.
If your child’s hip becomes stable with an abduction brace, they will wear the brace for about eight to 12 weeks. If the abduction brace does not stabilize the hip, your child may need surgery.
Image
Surgical treatment options for babies
Closed reduction
If your child’s hip continues to be partially or completely dislocated despite the use of the Pavlik harness and bracing, they may need surgery. Under anesthesia, the doctor will insert a very fine needle in the baby’s hip and inject contrast so they can clearly view the ball and the socket. This test is called an arthrogram.
The process of setting the ball back into the socket after the arthrogram is known as a closed reduction. Once the hip is set in place, technicians will put your child in a spica cast. This cast extends from slightly below the armpits to the legs and holds the hip in place. Different casts cover differing amounts of the child’s legs, based on the condition of their hips. Children typically wear a spica cast for three to six months. The cast will be changed from time to time as your baby grows.
Children typically wear a spica cast for three to six months. The cast will be changed from time to time as your baby grows.
Open reduction
If a closed reduction does not work, your child’s doctor may recommend open-reduction surgery. For this, the surgeon makes an incision and repositions the hip so it can grow and function normally. The specifics of the procedure depend on your child’s condition but it may include reshaping the hip socket, redirecting the femoral head, or repairing a dislocation. After the surgery, your child will need to wear a spica cast while they heal.
Follow-up care
Any infant treated surgically for hip dysplasia must be followed periodically by an orthopedist until they have reached physical maturity. At regular visits, their orthopedic doctor will monitor their hip to ensure it develops normally as they grow. Diagnosing and treating any new abnormality early will increase the chance your child will grow up to be active free from hip pain throughout their childhood, the teen years, and adulthood.
Will treatment affect my child’s ability to walk?
Depending on their age during treatment, your child may start walking later than other kids. However, after successful treatment, children typically start walking as well as other kids. By contrast, children with untreated hip dysplasia often start walking later, and many walk with a limp.
Hip Dysplasia | Programs & Services
Departments
Centers
Programs
Hip Dysplasia | Contact Us
Hip dysplasia in young children
At an orthopedist's appointment in the first month of a child's life, an unpleasant detail may turn out: the baby has immaturity of the pelvic bones. Most often, at the same time, the pediatrician pronounces the words “hip dysplasia”, which instantly frighten all young parents without exception. But being scared is not the right thing to do in this situation.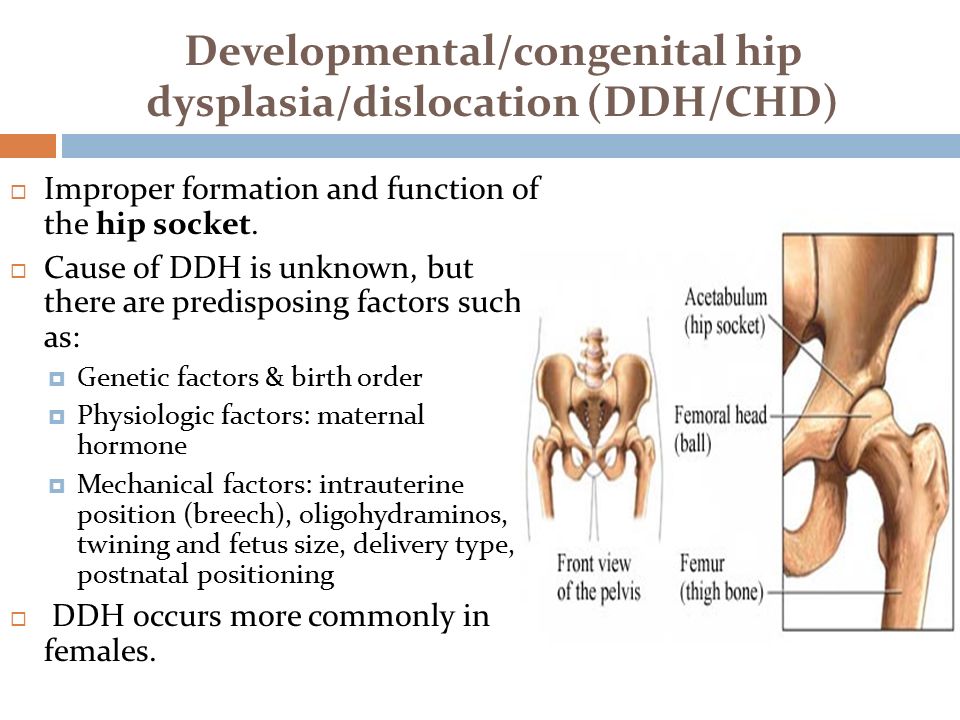 You need to be patient and strictly follow the recommendations of the attending physician. Nevertheless, all doctors will be right when they tell you that joint dysplasia, which was left without the attention of parents and doctors in the first year of a baby’s life, can form the most severe inflammatory processes in a child by the age of two or three, painful hip dislocation and in the future - lameness for life.
You need to be patient and strictly follow the recommendations of the attending physician. Nevertheless, all doctors will be right when they tell you that joint dysplasia, which was left without the attention of parents and doctors in the first year of a baby’s life, can form the most severe inflammatory processes in a child by the age of two or three, painful hip dislocation and in the future - lameness for life.
Hip dysplasia is a congenital disorder of the formation of the joint that can cause dislocation or subluxation of the femoral head. In this condition, either underdevelopment of the joint, or its increased mobility in combination with connective tissue deficiency, can be observed. Predisposing factors are unfavorable heredity, gynecological diseases of the mother and pathology of pregnancy. Hip dysplasia is 10 times more common in those children whose parents had signs of congenital hip dislocation and in those born with a breech presentation of the fetus, more often in the first birth. Often, dysplasia is detected during drug correction of pregnancy, during pregnancy complicated by toxicosis. The left hip joint is most often affected (60%), less often the right (20%) or both (20%). The relationship of morbidity with environmental problems has been noted. With untimely detection and lack of proper treatment, hip dysplasia can cause dysfunction of the lower limb and even disability. Therefore, this pathology must be identified and eliminated in the early period of the baby's life.
Often, dysplasia is detected during drug correction of pregnancy, during pregnancy complicated by toxicosis. The left hip joint is most often affected (60%), less often the right (20%) or both (20%). The relationship of morbidity with environmental problems has been noted. With untimely detection and lack of proper treatment, hip dysplasia can cause dysfunction of the lower limb and even disability. Therefore, this pathology must be identified and eliminated in the early period of the baby's life.
Hip dysplasia can present in a variety of ways. There are three main forms of dysplasia: acetabular dysplasia - acetabular dysplasia; dysplasia of the proximal femur; rotational dysplasia.
With timely detection and proper treatment, the prognosis is conditionally favorable.
Statistics say: up to 25% of newborn children have some form of hip dysplasia, in other words, they are born with subluxations. In most cases, under the constant supervision of an orthopedist, the joints “grow” on their own and return to the anatomical norm. For the rest, they just need a little help.
For the rest, they just need a little help.
A preliminary diagnosis can be made even in the maternity hospital. In this case, you need to contact a pediatric orthopedist within 3 weeks, who will conduct the necessary examination and draw up a treatment regimen. In addition, to exclude this pathology, all children are examined at the age of 1-4 months. Particular attention is paid to children who are at risk. This group includes all patients with a history of maternal toxicosis during pregnancy, a large fetus, breech presentation, as well as those whose parents also suffer from dysplasia. If signs of pathology are detected, the child is sent for additional studies.
To clarify the diagnosis, methods such as radiography and ultrasonography are used. In young children, a significant part of the joint is formed by cartilage, which is not displayed on radiographs, so this method is not used until the age of 2-3 months. Ultrasound diagnostics is a good alternative to X-ray examination in children during the first months of life. This technique is practically safe and quite informative.
This technique is practically safe and quite informative.
With dysplasia, the shape, relationship and size of the structures of the hip joint change significantly. The hip joint of a newborn, even in normal conditions, is an immature biomechanical structure. If the development of the joint is disturbed, the excessively elastic ligaments and the articular capsule are not able to hold the head of the femur in the articular cavity, it shifts upward and laterally (outwards). With certain movements, the femoral head can extend beyond the acetabulum. This condition of the joint is called "subluxation". In severe hip dysplasia, the head of the femur extends completely beyond the acetabulum, a condition called hip dislocation. Hip dysplasia can manifest itself not only as a violation of the acetabulum (acetabular dysplasia), but also as an abnormal development of the proximal femur.
Hip dysplasia is suspected in the presence of shortened hip, asymmetric skin folds, limited hip abduction, and Marx-Ortolani slipping. Asymmetry of the inguinal, popliteal and gluteal skin folds is usually better detected in children older than 2-3 months. During the inspection, they pay attention to the difference in the level of location, shape and depth of the folds. It should be borne in mind that the presence or absence of this symptom is not enough to make a diagnosis. With bilateral dysplasia, the folds may be symmetrical. In addition, the symptom is absent in half of the children with unilateral pathology. The asymmetry of the inguinal folds in children from birth to 2 months is of little information, since it sometimes occurs even in healthy infants. But the most important sign indicating congenital dislocation of the hip is the “click” or Marx-Ortolani symptom. Slowly abduct the hips evenly to both sides. With normal relations in the joints, both hips in the position of extreme abduction almost touch the outer surfaces of the table plane. With dislocation, the femoral head slips into the acetabulum at the moment of abduction, which is accompanied by a characteristic push - the moment when the femoral head from the dislocation position is reduced into the acetabulum.
Asymmetry of the inguinal, popliteal and gluteal skin folds is usually better detected in children older than 2-3 months. During the inspection, they pay attention to the difference in the level of location, shape and depth of the folds. It should be borne in mind that the presence or absence of this symptom is not enough to make a diagnosis. With bilateral dysplasia, the folds may be symmetrical. In addition, the symptom is absent in half of the children with unilateral pathology. The asymmetry of the inguinal folds in children from birth to 2 months is of little information, since it sometimes occurs even in healthy infants. But the most important sign indicating congenital dislocation of the hip is the “click” or Marx-Ortolani symptom. Slowly abduct the hips evenly to both sides. With normal relations in the joints, both hips in the position of extreme abduction almost touch the outer surfaces of the table plane. With dislocation, the femoral head slips into the acetabulum at the moment of abduction, which is accompanied by a characteristic push - the moment when the femoral head from the dislocation position is reduced into the acetabulum.
Another symptom that indicates the pathology of the joint is limitation of movement. In healthy newborns, the legs are retracted to a position of 80-90 ° and freely placed on the horizontal surface of the table. When the abduction is limited to 50-60°, there is reason to suspect a congenital pathology. In a healthy child of 7-8 months, each leg is retracted by 60-70°, in a baby with congenital dislocation - by 40-50°.
The main method of preventing hip dysplasia is wide swaddling. As soon as at 19In 1971, the national health program promoted wide swaddling; already a few years later, only 0.2% of children over the age of one year suffered from this disease. Orthopedic devices that securely fix the baby's legs in a bent and divorced form. These devices include all kinds of splints (a kind of spacers between the legs), plastic corsets and even plaster retainers. The most popular fixing device is the so-called Pavlik stirrups. Moreover, Pavlik here is not a boy who was the first to try a miracle unit on himself, but a talented Czech orthopedic doctor who came up with the idea of fixing a baby’s legs with a special harness.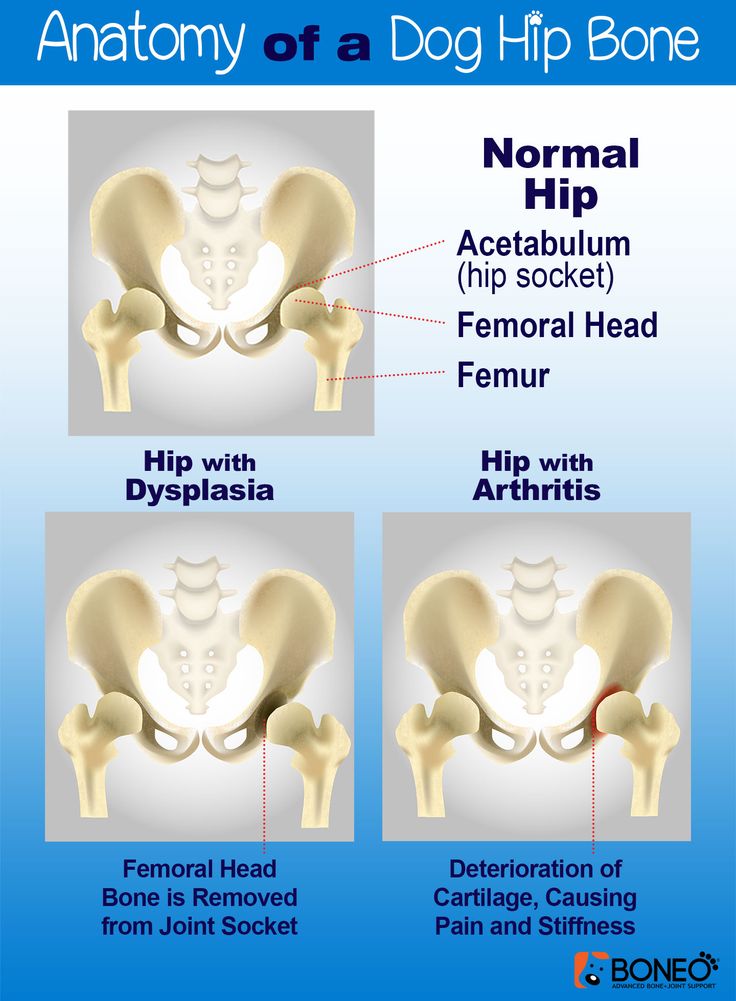 Massage and gymnastics. Your attending orthopedist will teach you specific exercises and techniques for daily massage and gymnastics, since the set of manipulations strictly depends on how the joint is under-formed. Use of carriers, slings, backpacks and car seats. But only those models that allow the baby to hold freely, legs wide apart. In the countries of Asia and Africa, where women have been carrying their babies on themselves since ancient times, tying them on their backs or on their stomachs (that is, the child spends all the time in a sitting position, with legs wide apart), there is no such phenomenon as hip dysplasia in children at all. exists.
Massage and gymnastics. Your attending orthopedist will teach you specific exercises and techniques for daily massage and gymnastics, since the set of manipulations strictly depends on how the joint is under-formed. Use of carriers, slings, backpacks and car seats. But only those models that allow the baby to hold freely, legs wide apart. In the countries of Asia and Africa, where women have been carrying their babies on themselves since ancient times, tying them on their backs or on their stomachs (that is, the child spends all the time in a sitting position, with legs wide apart), there is no such phenomenon as hip dysplasia in children at all. exists.
Treatment should begin as soon as possible. Alas, the treatment of dysplasia is not a quick matter. As a rule, it takes several months, sometimes - a year and a half. This is understandable: the hip joint cannot take the correct position and acquire reliable ligaments in a couple of days. But believe me, your efforts and patience are worth it! Of course, it’s not too pleasant to “hobble” your baby with orthopedic stirrups every day, and swaddle him with a pillow between his legs or “shackle” him in a plastic corset at night.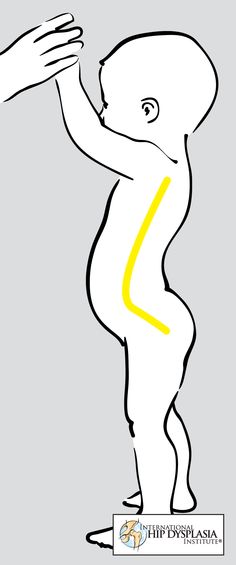 But it’s better to be a little sad before he is even a year old, so that later you can see how famously he dances at his 17-18 years old at the prom. The opposite is true: to be touched by crooked legs now and do nothing, and then reap the terrible consequences of your carelessness ... Isn't it?
But it’s better to be a little sad before he is even a year old, so that later you can see how famously he dances at his 17-18 years old at the prom. The opposite is true: to be touched by crooked legs now and do nothing, and then reap the terrible consequences of your carelessness ... Isn't it?
Radiologist of the 3rd City Children's Clinical Clinic
Vyacheslav Fedorovich Krasovsky
Hip dysplasia in children
G. I. Turner develop and apply modern methods for the treatment of pathologies of the hip joints in children. Specialists deal with the most non-standard and serious cases, treat children not only from all regions of the country, but also from foreign countries.
Surgical treatment is carried out according to federal quotas as part of the provision of specialized and high-tech medical care, which is free of charge for patients under 18 years of age from any regions of Russia.
Employees of the only specialized department of hip joint pathology of the N.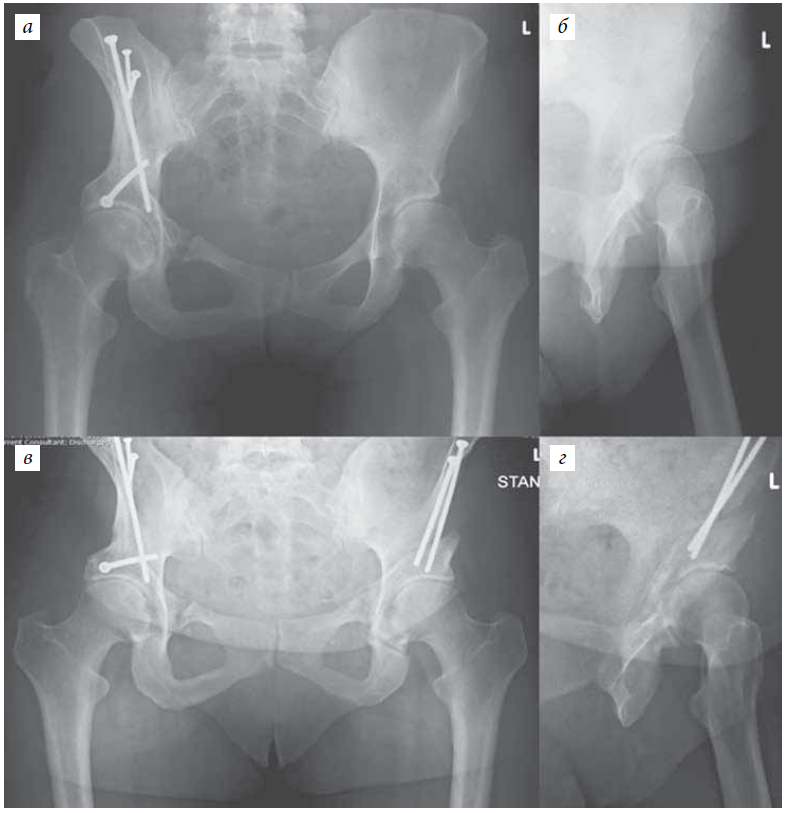 G.I. Turner successfully apply modern methods of conservative and surgical treatment of children with hip dysplasia of varying severity.
G.I. Turner successfully apply modern methods of conservative and surgical treatment of children with hip dysplasia of varying severity.
- According to international studies and statistics from our Center, 5-10 children per 1000 newborns suffer from this congenital pathology.
- The disease affects girls about 7 times more often than boys. Unilateral lesion occurs 1.5-2 times more often than bilateral.
- This pathology is the cause of every third case of coxarthrosis in adults.
What is hip dysplasia?
Hip dysplasia is a severe pathology characterized by underdevelopment of all elements of the hip joint (bones, ligaments, joint capsule, muscles, blood vessels, nerves).
Classification and assessment of the condition of the hip joint
The condition of the hip joints is assessed on the basis of ultrasound and x-ray data. Ultrasound screening is carried out according to the method of R.Graf (1984)
The main advantages of ultrasound screening:
- The earliest possible diagnosis of hip joint pathology (the “gold standard” of conducting is in the maternity hospital)
- Reduction of terms of conservative treatment!!!
- A significant reduction in the likelihood of surgical interventions!
- No exposure
There are several types of hip joint structure, according to R.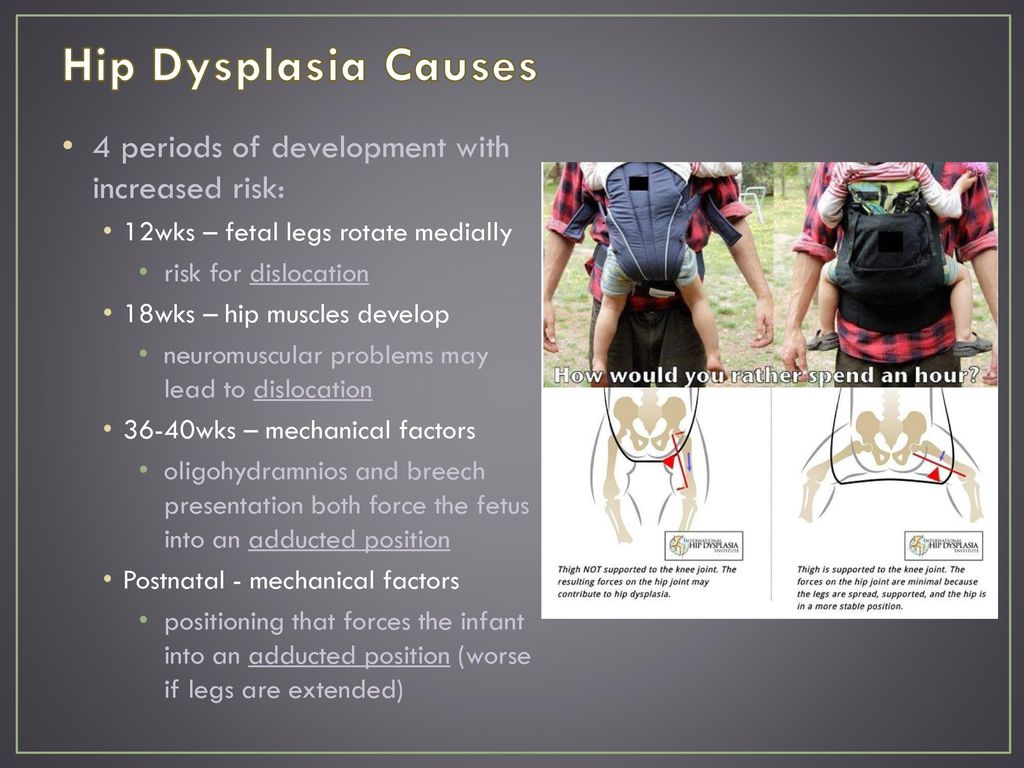 Graf evaluation criteria:
Graf evaluation criteria:
type 1a – mature hip joint
type 1b – transient – usually requires orthopedic treatment and does not require orthopedic treatment 903
2a type - immature hip joint. In children under 3 months of age, this type is regarded as functional immaturity and does not require orthopedic treatment; in children older than 3 months, such changes are considered pathological immaturity and require treatment, and the type itself is 2b
2c - hip subluxation
3 - hip subluxation
4 - hip dislocation
In children older than 3 months, X-ray examination is performed in addition to ultrasound examination. Before this age, radiological research methods are not informative, since there is no proper ossification of the bone structures of the hip joint and their adequate assessment is extremely difficult.
Today, in the world practice, the degree of hip dysplasia is determined according to the data of a radiation study according to the classification developed by the International Hip Dysplasia Institute, which is based on the relationship between the femoral head and the acetabulum.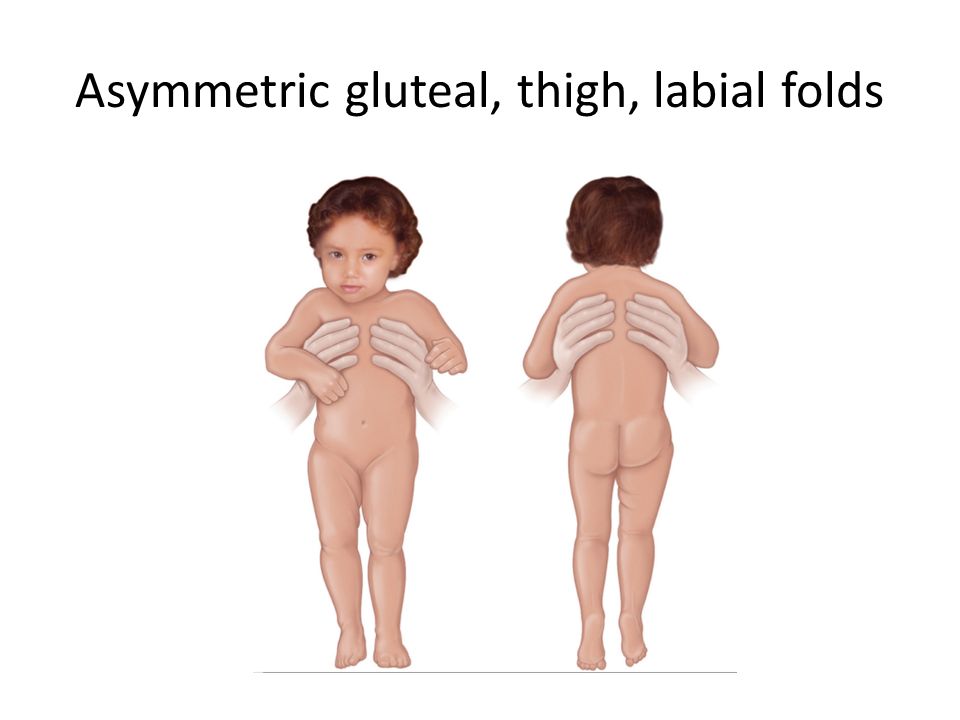
- First degree - hip joint without pathology
- Second degree (femoral subluxation) - the head of the femur is displaced cranially, but is below the upper-lateral edge of the true acetabulum
- Third degree (marginal dislocation of the hip) - the head of the femur is displaced cranially and is located at the level of the upper-lateral edge of the true acetabulum
- Fourth degree (supraacetabular dislocation of the hip) - the head of the femur is located above the upper-lateral edge of the true acetabulum
Main risk factors for occurrence:
- Heredity for congenital pathology of the hip joint
- Breech presentation
- Female
- First birth
- Large fruit (more than 4 kg)
- Viral or bacterial infection between 10 and 15 weeks of gestation
- Chronic diseases of the pelvic organs
Signs and symptoms of hip dysplasia
Symptoms of severe degrees of dysplasia (subluxation and dislocation) are pronounced in babies.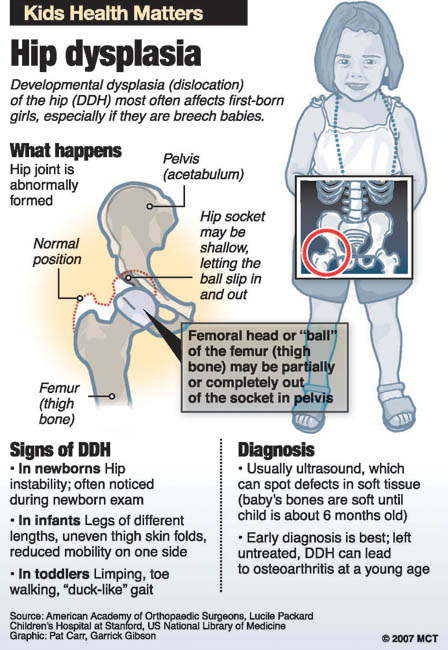 To exclude the diagnosis, the child should be examined by a pediatric orthopedist for the purpose of prevention. The “golden” standard for diagnosis is the maternity hospital! In the first year of life, an orthopedic examination is performed at 1, 3, 6 and 12 months.
To exclude the diagnosis, the child should be examined by a pediatric orthopedist for the purpose of prevention. The “golden” standard for diagnosis is the maternity hospital! In the first year of life, an orthopedic examination is performed at 1, 3, 6 and 12 months.
Main specific clinical signs in a child 1-2 months old
- Barlow test and Ortolani test
Additional (low specific) clinical signs
- Asymmetric skin folds on the thighs
- Asymmetric gluteal folds
- Excessive hip rotation
- External rotation of the feet
- Oblique location of the genital slit in girls.
- Shortening of the lower limb
- Palpation of the femoral head behind the posterior margin of the fossa
- Restriction of abduction of legs bent at right angles at the hip and knee joints
Diagnostics
Vissarionov Sergey ValentinovichVissarionov Sergey Valentinovich (Director of the National Research Center for Pediatric Traumatology and Orthopedics named after G.
I. Turner, Doctor of Medical Sciences, Professor, Corresponding Member of the Russian Academy of Sciences, laureate of the Prize of the Government of the Russian Federation)
We are currently focusing on the development of an innovative system for early diagnosis of hip dysplasia in infants and early functional conservative treatment. Our institution has developed a functional splint for the treatment of children with this pathological condition, which is being manufactured and is already used in the complex treatment of children with hip dysplasia.
Treatment of pathologies and dysplasia of the hip joints in newborns, children and adolescents is carried out by the Clinic of Hip Joint Pathology of our center.
A provisional diagnosis is often made during the stay in the maternity hospital. In such a situation, it is important to visit a pediatric orthopedist in the next three weeks. Necessary diagnostic procedures are radiography and ultrasonography.