How to make labor progress faster
How to dilate faster during labor: Safe methods
There are ways to induce labor medically, but a person can often encourage dilation by keeping the body relaxed and loose. This can help ease the delivery.
Dilation is a term that describes the widening of the cervical opening. Dilation of the cervix is one sign that a pregnant woman is going into labor.
During the final stages of pregnancy, doctors perform cervical exams to track the progress of the pregnancy and the extent of dilation of the cervix.
In the first stage of labor, the cervix will dilate to 10 centimeters (cm) in width.
Dilation is typically gradual, but the cervix can widen rapidly over 1 or 2 days. A few different factors can influence how quickly dilation occurs.
In this article, learn how to dilate more quickly before and during labor.
The following methods can help in dilation without using medication:
Move around
Getting up and moving around may help speed dilation by increasing blood flow.
Walking around the room, doing simple movements in bed or chair, or even changing positions may encourage dilation.
This is because the weight of the baby applies pressure to the cervix.
People may also find swaying or dancing to calming music effective.
Use an exercise ball
A large inflatable exercise ball, called a birthing ball in this case, may also help.
Sitting on the ball and rocking back and forth or moving in circles can help keep the muscles in the pelvis loose and relaxed for delivery.
Relax
It is easy to become tense during the last stages of pregnancy, but learning to relax can have a range of benefits.
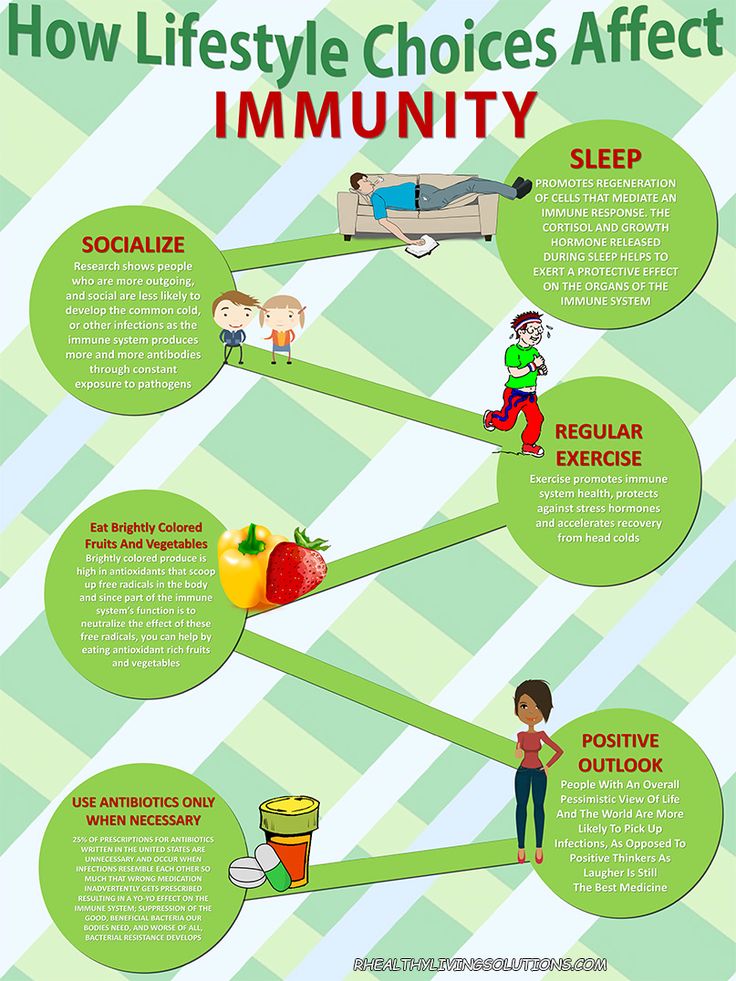
Stress and muscle tension and can delay labor by making it harder for the cervix to dilate. These issues can also keep the baby from descending.
Many women benefit from practicing breathing exercises or meditation before and during labor. Even dimming the lights can help.
Laugh
Laughing can keep stress and fear at bay. Even momentary relief can relax the body and aid dilation.
Even momentary relief can relax the body and aid dilation.
Joking around, or watching funny movies or stand-up comedy may help to keep spirits up before and during labor.
Have sex
Sexual stimulation can relax the body.
Also, a hormone called prostaglandin in semen can promote dilation.
Share on PinterestMedical intervention may be necessary during labor.
While labor is a natural process, there are times when a doctor needs to intervene.
Medical intervention may be necessary if:
- a woman has an infection in the uterus
- the baby is more than 2 weeks overdue, and active labor has not begun
- the water has broken, but there are no contractions
- underlying medical conditions will complicate delivery for the mother or baby
A doctor may apply a medication that contains prostaglandin to soften the cervix and promote dilation.
A process called membrane stripping may help. It involves a doctor or midwife rubbing their fingers against the membranes of the amniotic sac to release prostaglandin into the uterus and help the cervix dilate.
Women interested in unmedicated or “natural” birth may avoid medical intervention until it is necessary.
There are three distinct stages:
Stage one
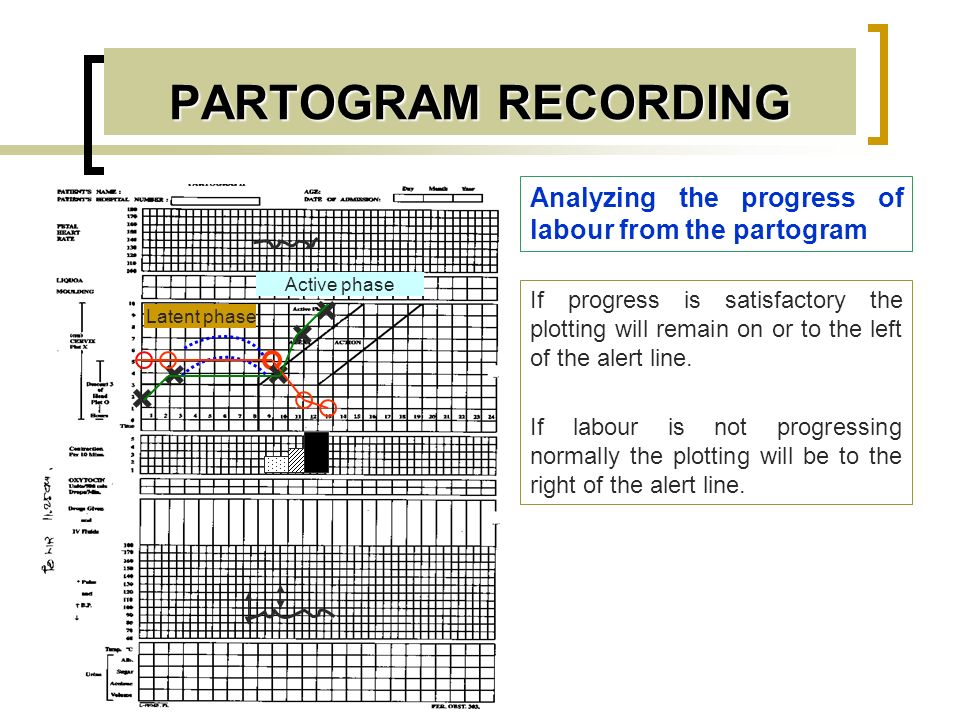
Share on PinterestThere are three distinct stages of labor.
This stage has three phases.
In the first phase, the cervix dilates to 3 cm. The baby drops lower into the pelvis, and this increases the levels of prostaglandin in the body, which stimulates dilation.
The mucus plug that has sealed the opening of the uterus during pregnancy will fall away.
Capillaries in the cervix can rupture during this stage and cause bloody discharge known as the bloody show. This is normal.
The next phase is active labor, when the cervix will dilate further. Some doctors mark the end of this phase when the width of the cervix reaches 7 cm. Others use contractions as a guideline.
The final step in this stage, called the transition phase, lasts until the cervix dilates to 10 cm.
Stage two
The second stage of labor begins when the cervix dilates to 10 cm and ends with delivery.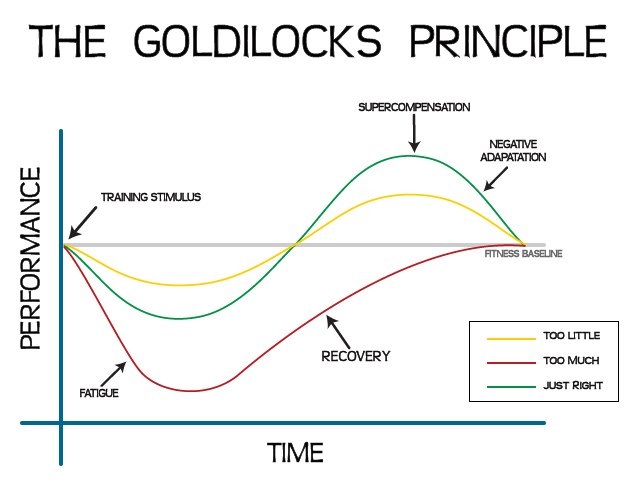 The length of time can vary from woman to woman, and a variety of factors influence it.
The length of time can vary from woman to woman, and a variety of factors influence it.
Stage three
In this stage, the doctor will deliver the placenta and cut the umbilical cord.
In some situations, a doctor may use medical methods to encourage dilation.
However, there are a number of natural ways to promote dilation before and during labor. It is often a good idea to find ways to relax.
Speeding up labour - BabyCentre UK
In this article
- When does active labour start?
- How long is a normal labour?
- What counts as a slow labour?
- Why might my labour be slow?
- How is labour speeded up?
- Can I speed up labour myself?
- What can help me to cope with a long labour?
When does active labour start?
Midwives and doctors say the active first stage of your labour starts when:
- you are having regular, powerful contractions and
- your cervix is dilating from 4cm (1.
 6in) onwards (NCCWCH 2014).
6in) onwards (NCCWCH 2014).
This may surprise you, as you may start to have strong tightenings well before reaching this point. You may have been awake all night and feeling as though labour has been under way for a while.
Pacing yourself in early labour may help you cope better when active labour gets under way (RCM 2018). Find out how to get through early labour at home.
How long is a normal labour?
Every labour is different, but there are average times that may help to guide you.
Early labour (before it gets active) often lasts about nine hours to 12 hours (Tilden et al 2019). It’s common for it to be longer for first-time mums, lasting 18 hours or more (Ängeby et al 2018).
The active first stage of labour (when your cervix is dilating from 4cm and you are having regular, powerful contractions) for a first baby is usually about eight hours, but it could be shorter or longer (NCCWCH 2014).
If this isn't your first baby, you may have a shorter labour, though this isn't guaranteed. For women who have given birth before, the active first stage of labour lasts, on average, for five hours (NCCWCH 2014). It's unlikely to last for more than 12 hours (NCCWCH 2014).
The pushing phase of labour (active second stage) shouldn't usually take more than three hours, or two hours if you've had a baby before (NCCWCH 2014).
Bear in mind that a quick labour isn't necessarily better either for you or your baby (Rimmer 2014). Very fast labours can be physically and emotionally challenging (Rimmer 2014). However, a very slow labour can leave you exhausted and unwell (Harper et al 2014).
What counts as a slow labour?
During active labour there may be an hour or so of slow or little progress, followed by periods of faster progress (Ehsanipoor and Satin 2019). What matters is how your labour progresses over several hours.
If your labour is straightforward, your midwife will assess your labour every four hours (NCCWCH 2014). With your permission, she'll carry out a vaginal examination to check how open your cervix is (NCCWCH 2014, RCM 2012a, RCN 2016). She'll also listen to your baby's heartbeat using a hand-held Doppler (a Sonicaid) or an ear trumpet (a Pinard stethoscope).
A four-hourly check gives your midwife a good overview of how you're doing. Assessing you more often than that won't necessarily help her to understand more, and can lead to unnecessary intervention in your labour (NCCWCH 2014).
However, if you've had any health concerns during this or a previous pregnancy you may need continuous monitoring.
Your doctor or midwife will also want to monitor you if you've developed complications, such as meconium (your baby’s first poo) in your waters, or fresh bleeding (NCCWCH 2014).
Your midwife will place two electronic sensors on your bump, one to measure contractions and one to measure your baby's heartbeat. The sensors will remain there throughout your labour. Your midwife will still only check your cervix every four hours, though.
The sensors will remain there throughout your labour. Your midwife will still only check your cervix every four hours, though.
If your cervix isn't dilating at a rate of at least 0.5cm (0.2in) an hour over a four-hour period, speeding up your labour may be an option (NCCWCH 2014). This is also called augmentation of labour. Your midwife will discuss whether or not to speed up your labour with you and your doctor.
Each woman's labour is unique. Your wishes should be taken into account, along with what your midwife and doctor recommend is best for you and your baby (Jackson et al 2014, NCCWCH 2014).
Why might my labour be slow?
Some labours are just slow for no particular reason. However, you may have a slow labour if:
- You're dehydrated or exhausted (NCCWCH 2014).
- The position of your baby is making it harder for your labour to progress (NCCWCH 2014).
- You feel particularly scared or anxious.
 These emotions tend to interfere with the release of the hormone oxytocin, which can help labour along (Aral et al 2014, Simkin and Ancheta 2011).
These emotions tend to interfere with the release of the hormone oxytocin, which can help labour along (Aral et al 2014, Simkin and Ancheta 2011). - Your contractions are infrequent, not very strong, or staying at the same intensity rather than getting stronger (NCCWCH 2014).
- You've had interventions that have slowed your contractions. These could include having to stay still for periods of time, or having an epidural (NCCWCH 2014).
Bear in mind that the first 5cm of cervix dilation nearly always takes much longer than the second 5cm (Ehsanipoor and Satin 2019, Jackson et al 2014, Simkin and Ancheta 2011). Your cervix opens more quickly as your contractions get stronger.
How is labour speeded up?
If your midwife asks whether you'd like to have your labour speeded up, take time to consider your options. If your baby is fine, and your cervix is gradually opening up, even if it's happening slowly, it may be best to leave things alone. You may be perfectly happy to take things gently, staying in tune with your body and your baby.
You may be perfectly happy to take things gently, staying in tune with your body and your baby.
Or you may be so exhausted that you really want your baby to be born quickly. If that's the case, your midwife can help to move things along in the following ways:
Breaking the waters
Your midwife may suggest breaking your waters to speed up your labour (NCCWCH 2014). This isn't usually recommended near the beginning of labour, as it could increase your risk of infection if labour doesn't start right away (NCCWCH 2008).
However, if the active stage of labour slows right down, breaking your waters can help to get things going again. It may shorten labour by about an hour (NCCWCH 2014).
If you agree to the procedure, here's how your midwife will do it. Once you're on the bed, she'll remove the last section of the bed so that your bottom is right at the end. She may ask you to put your legs up in stirrups, or just hold them apart.
Your midwife will then make a small break in the membranes around your baby. She'll use a long thin probe (amnihook) or a medical glove with a pricked end on one of the fingers (amnicot). She'll scratch the membrane until it bursts and the waters flow out into a tray placed underneath the bed.
This procedure isn't painful but it can be very uncomfortable. You'll probably be glad to get up again once it's over.
Your midwife will then check your baby's heartbeat using a Sonicaid or ear trumpet, to make sure that breaking the waters hasn't distressed him.
Your contractions may become much stronger after your waters have been broken (NCCWCH 2014). Be prepared to work hard with breathing and relaxation exercises. Or you can ask your midwife for some pain relief, such as gas and air, if you need extra help.
Hormone drip
If moving around or breaking your waters doesn't speed up your labour, your doctor may suggest a hormone drip to boost your contractions (NCCWCH 2014). This will contain Syntocinon, which is an artificial form of the labour hormone oxytocin.
This will contain Syntocinon, which is an artificial form of the labour hormone oxytocin.
If you have Syntocinon, your midwife will continuously monitor your baby's heartbeat by strapping electronic sensors to your tummy (NCCWCH 2014).
Your midwife may also recommend attaching a small clip to your baby's head. The clip is called a fetal scalp electrode and it may provide a more accurate reading than placing a sensor on your tummy. It also allows you to move around more easily.
Continuous monitoring is recommended because Syntocinon can over-stimulate your womb (uterus) (NCCWCH 2014). You may get very strong, frequent contractions, which could distress your baby.
You're also more likely to need help from pain-relieving drugs to cope with these artificially induced contractions. For this reason, your midwife should offer you an epidural before she starts a Syntocinon drip (NCCWCH 2014).
Can I speed up labour myself?
If you'd prefer not to have your waters broken, or a hormone drip, there are some natural techniques you could try to speed up your labour
- If you're lying on the bed, get up! Being upright and mobile may strengthen your contractions, while also helping you to cope with them (Lawrence et al 2013).
- Take a walk to the toilet. A full bladder may slow down your labour by getting in the way of your baby's head descending (Simkin and Ancheta 2011).
- If you have access to one, get into a warm bath or birth pool. This can reduce your need for an epidural or spinal pain relief (Cluett et al 2018).
- If your baby is lying back-to-back, an experienced midwife may advise you to lie on your side or try kneeling or standing lunge positions. This may help your baby to rotate to a better position for birth (Simkin and Ancheta 2011).
- Have some private time with your partner. Turn the lights down low and have a cuddle, with some nipple stroking or breast massage. This may help your body to release oxytocin, the hormone that strengthens your contractions (Simkin and Ancheta 2011).
You could also try acupuncture during your labour (Mollart et al 2015,Simkin and Ancheta 2011). Complementary therapies probably work best if used throughout labour. You may be able to request an acupuncturist if your labour has slowed down. In some areas of the UK, acupuncturists specialising in childbirth work in teams, meaning that a practitioner is always available.
You may be able to request an acupuncturist if your labour has slowed down. In some areas of the UK, acupuncturists specialising in childbirth work in teams, meaning that a practitioner is always available.
You can also ask your midwife whether she's certified in any complementary therapies, such as aromatherapy massage, that could help you.
How to help your baby be born
How can you speed up labour and make the birth easier? Discover how to help your baby be born more quickly.More preparing for birth videos
What can help me to cope with a long labour?
These methods may help you:
- Use breathing and relaxation techniques to help you stay calm and focused (NCCWCH 2014). If you've been taking hypnobirthing classes, this is the time to use everything you've learned!
- Ask your birth partner to massage your back, or your feet, if you're sitting in a chair (NCCWCH 2014, Smith et al 2018).
- Listen to your favourite music (NCCWCH 2014).
- Eat and drink when you need to. Have a small snack, such as toast, and water, or an isotonic drink, to stay hydrated (NCCWCH 2014).
- Change your position. Later in labour you may not feel like walking around, but your midwife can help you to find a comfortable position (NCCWCH 2014).
- Listen to your body and try different positions (Simkin and Ancheta 2011). Move around or adopt positions that feel most comfortable to you as labour progresses (NCCWCH 2014).
- Ask your midwife to explain what's going on. If you feel involved and in control of your labour, you'll probably feel less anxious and more relaxed. This may make your labour easier to cope with, and you may find it a more positive experience (NCCWCH 2014).
- If your midwife is caring for other women as well as you because the unit is busy, continuous support from a student midwife may help your labour to progress. Your birth partner could ask if there's any extra help available (Bolbol-Haghighi et al 2016).

Learn more about what to expect from each stage of labour.
References
Aral I, Koken G, Bozkurt M, et al. 2014. Evaluation of the effects of maternal anxiety on the duration of vaginal labour delivery. Clin Exp Obstet Gynecol 41(1):32-6
Bolbol-Haghighi N, Masoumi SZ, Kazemi F. 2016. Effect of continued support of midwifery students in labour on the childbirth and labour consequences: a randomized controlled clinical trial. J Clin Diagn Res 10(9): QC14–QC17. www.ncbi.nlm.nih.gov [Accessed September 2019]
Cluett ER, Burns E, Cuthbert A. 2018. Immersion in water during labour and birth. Cochrane Database of Systematic Reviews (5): CD000111. www.cochranelibrary.com [Accessed September 2019]
Ehsanipoor MD, Satin AJ. 2019. Normal and abnormal labor progression. UpToDate. www.uptodate.com [Accessed September 2019]
Harper LM, Caughey AB, Roehl KA, et al. 2014. Defining an abnormal first stage of labor based on maternal and neonatal outcomes. Am J Obstet Gynecol (210(6):536.e1-7. www.ncbi.nlm.nih.gov [Accessed September 2019]
2014. Defining an abnormal first stage of labor based on maternal and neonatal outcomes. Am J Obstet Gynecol (210(6):536.e1-7. www.ncbi.nlm.nih.gov [Accessed September 2019]
Jackson K, Marshall JE, Brydon S. 2014. Physiology and care during the first stage of labour. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 327-66
Lawrence A, Lewis L, Hofmeyr GJ, et al. 2013. Maternal positions and mobility during first stage labour. Cochrane Database of Systematic Reviews (10): CD003934. www.cochranelibrary.com [Accessed September 2019]
Mollart LJ, Adam J, Foureur M. 2015. Impact of acupressure on onset of labour and labour duration: a systematic review. Women Birth 28(3): 199-206
NCCWCH. 2014. Intrapartum care: care of healthy women and their babies during childbirth. National Collaborating Centre for Women's and Children's Health, Clinical guideline, 190. www.nice.org.uk [Accessed September 2019]
RCM.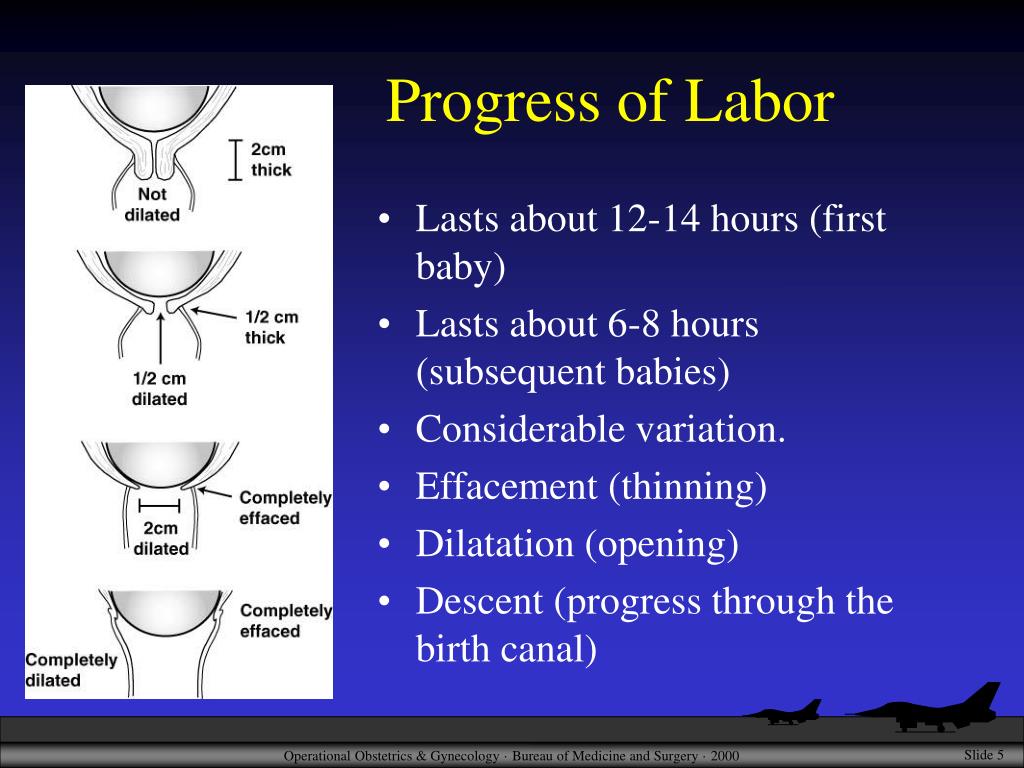 2012a. Assessing progress in labour. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
2012a. Assessing progress in labour. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
RCM. 2012b. Rupturing membranes. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
RCM. 2018. Midwifery care in labour guidance for all women in all settings. Royal College of Midwives, Midwifery Blue Top Guidance
RCN. 2016. Genital examination in women. Royal College of Nursing. www.rcn.org.uk [Accessed September 2019]
Rimmer A. 2014. Prolonged pregnancy and disorders of uterine action. In: Marshall JE, Raynor MD. eds. Myles textbook for midwives 16th ed. Edinburgh: Churchill Livingstone, 417-33
Simkin P, Ancheta R. 2011. The labor progress handbook: early interventions to prevent and treat dystocia. 3rd ed. Chichester: Wiley Blackwell
Smith CA, Levett KM, Collins CT, et al. 2018. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database of Systematic Reviews (3): CD009290. www.cochranelibrary.com [Accessed September 2019]
Cochrane Database of Systematic Reviews (3): CD009290. www.cochranelibrary.com [Accessed September 2019]
Smyth RMD, Markham C, Dowswell T. 2013. Amniotomy for shortening spontaneous labour. Cochrane Database of Systematic Reviews (6): CD006167. www.cochranelibrary.com [Accessed September 2019]
Thakar R, Sultan AH. 2014. The female pelvis and the reproductive organs. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 55-80
Show references Hide references
What will help in childbirth - articles from the specialists of the clinic "Mother and Child"
Vovk Lyudmila Anatolyevna
Reproductologist, Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
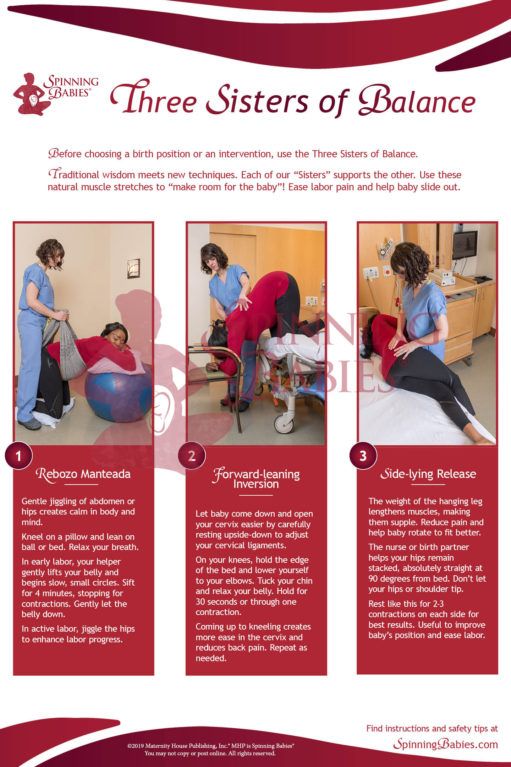
We walk and dance
If earlier in the maternity hospital, with the onset of labor, a woman was put to bed, now, on the contrary, obstetricians recommend that the expectant mother move . For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements.
For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements.
Showering and bathing
For many people, water is a great way to relieve fatigue and tension, and it also helps with painful contractions. You can just stand in the shower, or you can lie down in the bath. Warm water will warm the muscles of the back and abdomen, they will relax, and the birth canal will relax - as a result, the pain may decrease. Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions.
Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions.
Swinging on the ball
Until recently, fitball (rubber inflatable ball) in the rodblock was something outlandish, and today is found in many maternity hospitals. And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.
And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.
To be more comfortable, the ball should be soft, slightly deflated, and large, with a diameter of at least 75 cm.
We hang on a rope or wall bars
When the contractions become very strong and painful, you can take poses in which the stomach is, as it were, in a “suspended” state. Some advanced maternity hospitals have wall bars and ropes attached to the ceiling for this. During contraction, you can hang on them, as a result, the weight of the uterus will put less pressure on large blood vessels, and this will improve uteroplacental blood flow. In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain.
Do not hang on a rope or a wall only if there is a desire to push, and the cervix has not yet opened and the efforts must be restrained.
Lying comfortably
If during childbirth a woman wants not to move, but, on the contrary, to lie down, then, of course, she can lie down. In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control.
In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control.
We use everything we have
In any road block, even if it is minimally equipped, you can still find something useful. For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs.
If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs.
And don't be afraid to look stupid during childbirth. No one in the delivery room cares about how you move or lie down as long as it helps you get through your contractions, so calmly find your comfortable position.
Giving birth in an uncomfortable position is both difficult and inefficient. So memorize and rehearse some poses beforehand, and if there are any fixtures in the rodblock, try using them. Something of this will definitely help you to comfortably and easily survive childbirth.
When we move, take various postures, the blood supply to the uterus improves, as a result, it contracts better, and the cervix opens faster. In addition, uteroplacental blood flow improves, and therefore the baby does not suffer from hypoxia
strength to push
By clicking on the send button, I consent to the processing of personal data
WHO: Women in labor and physicians are increasingly opting for caesarean section
Modern surgical approaches, effective pain medications and antibiotics are reported by the World Health Organization to allow the operation to be performed with minimal risk to mother and child. A new WHO study in this area has shown that in countries where at least 10% of women undergo this operation, maternal and child mortality is reduced. However, caesarean section certainly has its downsides.
A new WHO study in this area has shown that in countries where at least 10% of women undergo this operation, maternal and child mortality is reduced. However, caesarean section certainly has its downsides.
“My doctor almost immediately recommended a caesarean section. He explained it by my age. Although this was the second birth for me, but I was already 44 years old. And when I came to the hospital at the appointed time, they said: why, actually, a caesarean? according to what evidence? But my doctor insisted, he didn't want to risk anything. And then, after the birth, he told me that the child had an entanglement of the umbilical cord, and during childbirth this loop could tighten around the child’s neck.
More and more women choose caesarean section as the most painless, quick and safe way to give birth. Caesarean section is especially popular in developed and developing countries. The numbers are impressive. For example, in Brazil, 45% of women choose a caesarean section. In European countries, this figure has increased from 15% to 22% over the past 20 years. WHO spokeswoman Dr. Marlene Temmerman says:
In European countries, this figure has increased from 15% to 22% over the past 20 years. WHO spokeswoman Dr. Marlene Temmerman says:
In Brazil, 45% of women opt for a caesarean section. In European countries, this figure has grown from 15% to 22% over the past 20 years
“In many developing and developed countries, there is a real epidemic of caesarean sections. A cesarean is done even when there is no medical need for it. You may be wondering: so what? If women choose caesarean section and it is safe, why not? Yes, in modern conditions it is really safe. But do not forget that this is still an operation, a surgical intervention.
A caesarean section can cause serious complications for both the baby and the mother. Marlene Temmerman explains:
“Women who have a cesarean are at a higher risk of bleeding. Also, do not forget about the scars that remain from previous births that have passed with the help of surgical intervention. Serious complications may arise. And even in some developed countries, where caesareans are often performed, a higher level of maternal mortality has been reported compared to other developed countries. Of course, this operation is not the main cause of death among women in childbirth, but the connection certainly exists.
Serious complications may arise. And even in some developed countries, where caesareans are often performed, a higher level of maternal mortality has been reported compared to other developed countries. Of course, this operation is not the main cause of death among women in childbirth, but the connection certainly exists.
However, the preference for caesarean is, of course, not only for women, but also for doctors. And they are partly understandable. It is better to perform a scheduled operation at a prearranged time than to receive a call from a patient in the middle of the night and then have to deal with this or that unforeseen situation during childbirth:
adjust your schedule. The doctor sees patients at a certain time. He can do two surgeries a day. No unexpected calls, no late night work, no emergencies, no added stress. The quality of life of doctors thanks to caesarean section is significantly improved.”
At the same time, experts emphasize that in many cases, caesarean section really saves lives.