Sign of labour pain
Signs that labour has begun
Know the signs
There are several signs that labour might be starting, including:
- contractions or tightenings
- a "show", when the plug of mucus from your cervix (entrance to your womb, or uterus) comes away
- backache
- an urge to go to the toilet, which is caused by your baby's head pressing on your bowel
- your waters breaking
The early (latent) stage of labour can take some time.
Urgent advice: Call your midwife or maternity unit if:
- your waters break
- you have vaginal bleeding
- your baby is moving less than usual
- you're less than 37 weeks pregnant and think you might be in labour
These signs mean you need to see a midwife or doctor.
Latent phase of labour
The start of labour is called the latent phase. This is when your cervix becomes soft and thin, and starts opening for your baby to be born. This can take hours or sometimes days.
You'll probably be advised to stay at home during this time. If you go to the hospital or maternity unit, they may suggest you go back home.
Find out more about the stages of labour and what you can do at home during the latent phase.
Call your midwife if you're unsure or worried about anything.
What do contractions feel like
When you have a contraction, your womb tightens and then relaxes. For some people, contractions may feel like extreme period pains.
You may have had contractions during your pregnancy, particularly towards the end. These tightenings are called Braxton Hicks contractions and are usually painless.
These tightenings are called Braxton Hicks contractions and are usually painless.
Your contractions tend to become longer, stronger and more frequent as your labour progresses. During a contraction, the muscles tighten and the pain increases. If you put your hand on your abdomen, you'll feel it getting harder; when the muscles relax, the pain fades and you will feel the hardness ease.
The contractions are pushing your baby down and opening the entrance to your womb (the cervix), ready for your baby to go through.
Your midwife will probably advise you to stay at home until your contractions become frequent.
Call your midwife or maternity unit for guidance when your contractions are in a regular pattern and:
- last at least 60 seconds
- come every 5 minutes or
- you think you are in labour
Read more information on when to go to hospital
Backache often comes on in labour
You may get backache or a heavy, aching feeling.
A "show" can signal the start of labour
During pregnancy, there's a plug of mucus in your cervix. This mucus comes away just before labour starts, or when in early labour, and it may pass out of your vagina. This sticky, jelly-like pink mucus is called a show.
It may come away in 1 blob or in several pieces. It's pink because it contains a small amount of blood.
If you're losing more blood, it may be a sign something is wrong, so phone your hospital or midwife straight away.
A show indicates that the cervix is starting to open. Labour may quickly follow or may take a few days. Sometimes there is no show.
What happens when my waters break
It's likely your waters will break during labour, but it can also happen before labour starts.
Your baby develops and grows inside a bag of fluid called the amniotic sac. When it's time for your baby to be born, the sac usually breaks and the amniotic fluid drains out through your vagina. This is your waters breaking. Sometimes when you're in labour, a midwife or doctor may offer to break your waters.
When it's time for your baby to be born, the sac usually breaks and the amniotic fluid drains out through your vagina. This is your waters breaking. Sometimes when you're in labour, a midwife or doctor may offer to break your waters.
If your waters break naturally, you may feel a slow trickle or a sudden gush of water you cannot control. To prepare for this, you could keep a sanitary towel (but not a tampon) handy if you're going out, and put a protective sheet on your bed.
Amniotic fluid is clear and pale. Sometimes it's difficult to tell amniotic fluid from urine. When your waters break, the water may be a little bloodstained to begin with.
Tell your midwife immediately if:
- the waters are smelly or coloured
- you're losing blood
This could mean you and your baby need urgent attention.
If your waters break before labour starts, call your midwife. Use a sanitary pad (not a tampon) so your midwife can check the colour of the waters.
Use a sanitary pad (not a tampon) so your midwife can check the colour of the waters.
If labour does not start after your waters break
It's usual to go into labour within 24 hours of the waters breaking. You'll be offered an induction if you do not because, without amniotic fluid, there's an increased risk of infection for your baby.
Until your induction, or if you choose to wait for labour to start naturally, tell your midwife immediately if:
- your baby moves less than usual
- there's any change in the colour or smell of any fluid coming from your vagina
You should take your temperature every 4 hours when you're awake, and tell your midwife if it's raised. A raised temperature is usually above 37.5C, but you may need to call before this – check with your midwife.
There's no evidence that having a bath or shower after your waters have broken increases your risk of infection, but having sex might.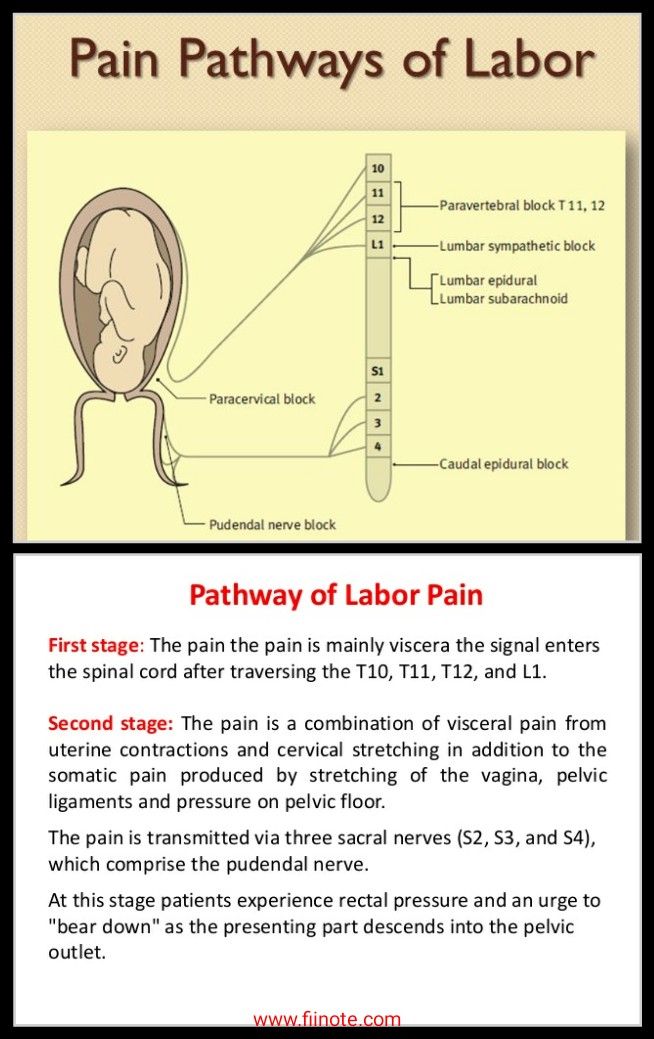
How to cope when labour begins
At the beginning of labour, you can:
- walk or move about, if you feel like it
- drink fluids – you may find sports (isotonic) drinks help keep your energy levels up
- have a snack, if you feel like it
- try any relaxation and breathing exercises you've learned to deal with contractions as they get stronger and more painful – your birth partner can help by doing these with you
- have your birth partner rub your back – this can help relieve pain
- take paracetamol according to the instructions on the packet – paracetamol is safe to take in labour
- have a warm bath
Find out what happens during labour and birth, and what you can do for pain relief in the early stages of labour.
Get Start4Life pregnancy and baby emails
For information and advice you can trust, sign up for weekly Start4Life pregnancy and baby emails.
Video: How will I know I am in labour?
In this video, a midwife describes the signs that mean labour may be starting.
Media last reviewed: 1 November 2019
Media review due: 1 November 2022
Contractions and signs of labor
Learning the signs of labor before your due date can help you feel ready for your baby’s birth.
Signs of labor include strong and regular contractions, pain in your belly and lower back, a bloody mucus discharge and your water breaking.
If you think you’re in labor, call your health care provider.
Not all contractions mean you're in true labor.
 Learning the difference between true and false labor can help you know when it’s the real thing.
Learning the difference between true and false labor can help you know when it’s the real thing.What is labor?
Labor (also called childbirth) is the process of your baby leaving the uterus (womb). You’re in labor when you have regular contractions that cause your cervix to change. Contractions are when the muscles of your uterus get tight and then relax. Contractions help push your baby out of your uterus. Your cervix is the opening to the uterus that sits at the top of the vagina. When labor starts, your cervix dilates (opens up).
As you get closer to your due date, learning the signs of labor can help you feel ready for labor and birth. If you have any signs of labor, call your health care provider.
What are the signs of labor?
You know you’re in true labor when:
- You have strong and regular contractions. A contraction is when the muscles of your uterus tighten up like a fist and then relax.
 Contractions help push your baby out. When you’re in true labor, your contractions last about 30 to 70 seconds and come about 5 to 10 minutes apart. They’re so strong that you can’t walk or talk during them. They get stronger and closer together over time.
Contractions help push your baby out. When you’re in true labor, your contractions last about 30 to 70 seconds and come about 5 to 10 minutes apart. They’re so strong that you can’t walk or talk during them. They get stronger and closer together over time. - You feel pain in your belly and lower back. This pain doesn't go away when you move or change positions.
- You have an increase in vaginal discharge that can be clear, pink or slightly bloody (brownish or reddish). This is called bloody show. It can happen a few days before labor or at the beginning of labor. If you have bright red bleeding or if the bleeding is heavy, tell your provider right away.
- Your water breaks. Your baby has been growing in amniotic fluid (the bag of waters) in your uterus. When the bag of waters breaks, you may feel a big rush of water. Or you may feel just a trickle.
If you think you’re in labor, call your health care provider, no matter what time of day or night. Your provider can tell you if it’s time to head for the hospital. To see for sure that you’re in labor, your health care provider measures your cervix.
Your provider can tell you if it’s time to head for the hospital. To see for sure that you’re in labor, your health care provider measures your cervix.
What are signs that you may be close to starting labor?
You may be close to starting labor if:
- Your baby drops or moves lower into your pelvis. This is called lightening. It means that your baby is getting ready to move into position for birth. It can happen a few weeks or even just a few hours before your labor begins.
- You have an increase in vaginal discharge that’s clear, pink or slightly bloody. This is called show or bloody show. It can happen a few days before labor starts or at the beginning of labor.
- At a prenatal checkup, your health care provider tells you that your cervix has begun to efface (thin) and dilate (open). Before labor, your cervix is about 3.5 to 4 centimeters long. When it’s fully dilated (open) for labor, it’s 10 centimeters.
 Once labor starts, contractions help open your cervix.
Once labor starts, contractions help open your cervix. - You have the nesting instinct. This is when you want to get things organized in your home to get ready for your baby. You may want to do things like cook meals or get the baby’s clothes and room ready. Doing these things is fine as long as you’re careful not to overdo it. You need your energy for labor and birth.
If you have any of these signs, you may start labor soon. Learn the signs of labor so you know when to call your provider.
What are false labor and Braxton-Hicks contractions?
Not all contractions mean you’re in labor. You may have contractions on and off before true labor starts. These contractions are called false labor or Braxton-Hicks contractions. They soften and thin the cervix to help your body get ready for labor and birth. You may feel them in the weeks right before your due date. Learning the differences between true labor contractions and false labor contractions can help you know when you’re really in labor.
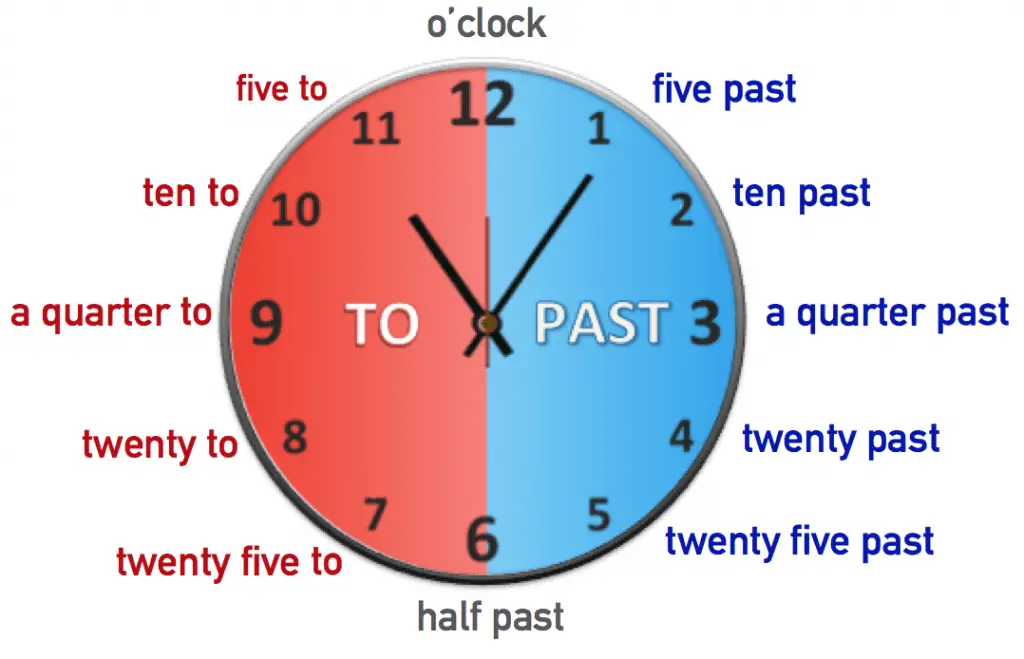
It can be hard to tell the difference between true labor and false labor. When you first feel contractions, time them. Write down how much time it takes from the start of one contraction to the start of the next. Make a note of how strong the contractions feel. Keep a record of your contractions for 1 hour. Walk or move around to see if the contractions stop when you change positions.
What is preterm labor?
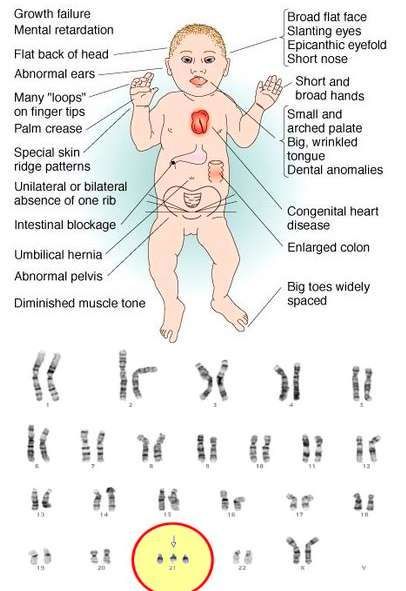
Preterm labor is labor that begins too early, before 37 weeks of pregnancy. Premature babies (born before 37 weeks of pregnancy) can have health problems at birth and later in life. If you’re not to 37 weeks of pregnancy and you have signs or symptoms of preterm labor, call your provider. Getting help quickly is the best thing you can do. Learn about risk factors for preterm labor and what you can do to help reduce your risk.
What are stages of labor?
Stages of labor include the whole process of labor, from your first contractions (stage 1) to pushing (stage 2) to delivery of the placenta (stage 3) after your baby is born. Learning about the stages of labor can help you know what to expect during labor and birth.
Learning about the stages of labor can help you know what to expect during labor and birth.
Last reviewed: December, 2018
Harbingers of childbirth - How to understand that it is time to go to the hospital?
January 10, 2017
Alekseeva Inna
Obstetrician-gynecologist, Doctor of the highest category
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.instagram.com/roddompravda/
Tips and opinions from leading children's specialists: https://www.instagram.com/emc.child/
Every pregnant woman with excitement and joy awaits the upcoming birth. The closer the cherished date, the more attentively the expectant mother listens to the changes taking place in her body and in the behavior of the baby. Of course, the expectant mother wants to know by what signs it is possible to understand that childbirth is just around the corner.
Of course, the expectant mother wants to know by what signs it is possible to understand that childbirth is just around the corner.
It is customary to call the harbingers of childbirth external, really tangible changes in the body, which are direct preparation for the onset of labor. The tissues of the birth canal - the cervix, vagina, vulva, perineum - become quite elastic, extensible, but at the same time - very strong and resistant to tearing. The cervix is located in the center of the vaginal vault, shortens by almost half its normal length and softens significantly. The cervical canal - the lumen of the cervix connecting the uterine cavity with the vagina - opens slightly, as a result, the diameter of the cervical canal is approximately 2-2.5 cm. Of course, such a significant "perestroika" takes more than one day.
Female sex hormones are responsible for preparing for childbirth. During the nine months of pregnancy, progesterone "reigns" in the body of the expectant mother. It ensures the normal tone of the uterus (relaxed state of the muscles), the production of cervical mucus - a mucous plug in the cervix that protects the fetus from infection. The amount of progesterone during pregnancy largely determines the normal development and growth of the fetus, the necessary concentration of nutrients and oxygen in the mother's blood, as well as their timely and uninterrupted delivery to the baby.
It ensures the normal tone of the uterus (relaxed state of the muscles), the production of cervical mucus - a mucous plug in the cervix that protects the fetus from infection. The amount of progesterone during pregnancy largely determines the normal development and growth of the fetus, the necessary concentration of nutrients and oxygen in the mother's blood, as well as their timely and uninterrupted delivery to the baby.
Shortly before childbirth, the production of progesterone decreases markedly, it is replaced by estrogens - female sex hormones. The increase in estrogen in the blood is caused by the need to prepare the body for the upcoming birth. It is these hormones that are responsible for the elasticity and patency of the birth canal. The rate of cervical dilatation in the first stage of labor depends on them. In the second period, when the cervix is fully opened and the fetus passes through the birth canal, it is also very important how elastic and extensible the walls of the vagina are - this will largely determine the duration of the straining period. Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation.
Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation.
These changes are normal and do not require an unscheduled visit to the doctor or hospitalization. Harbingers of childbirth are manifestations of a planned restructuring in the body of a future mother, the “finishing touches” of preparation for the upcoming joyful event.
The absence of clearly perceptible changes on the eve of the expected date of birth is also not a pathology. Not all expectant mothers note those changes in well-being that are commonly called harbingers. However, this does not mean that there is no preparation. In some cases, the “final preparations” go unnoticed by the pregnant woman. Therefore, do not worry or urgently contact a specialist.
The appearance of any of the "harbingers" indicates the likelihood of the development of regular labor activity over the next two hours - two weeks. None of the sensations described gives a 100% guarantee that a woman will become a mother within the next 24 hours. Hormonal changes before childbirth begin approximately two weeks before the expected birth. Theoretically, during these two weeks, at any time, a pregnant woman can notice certain changes in her state of health. Consequently, the absence of labor activity an hour, a day, or even a week after the first noted changes is not a pathology and does not require special medical advice.
None of the sensations described gives a 100% guarantee that a woman will become a mother within the next 24 hours. Hormonal changes before childbirth begin approximately two weeks before the expected birth. Theoretically, during these two weeks, at any time, a pregnant woman can notice certain changes in her state of health. Consequently, the absence of labor activity an hour, a day, or even a week after the first noted changes is not a pathology and does not require special medical advice.
- Scarlet discharge from the genital tract in any amount.
- Severe abdominal pain.
- Increased blood pressure (above 130/80 mmHg).
- An increase in body temperature to 37.5 ° C and above.
- Increased heart rate (more than 100 beats per minute).
- Severe headache, vomiting, blurred vision.
- Significant increase in edema.
- Absence, sharp decrease, sharp increase in fetal movements.
- Suspicion of amniotic fluid leakage.
Weight loss . Shortly before the expected date of delivery, the expectant mother may notice some “weight loss”. Weight loss during this period is associated with the removal of excess fluid from the body, that is, a general decrease in edema. The more pronounced the fluid retention during pregnancy, the more mass the pregnant woman will “lose” on the eve of childbirth. During pregnancy, water is retained in the body of all expectant mothers to a greater or lesser extent. The reason is progesterone - a hormone whose main function is to support the processes of pregnancy. Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg.
Change of stool. Increased frequency and change in the consistency of physiological functions on the eve of childbirth is also associated with an increase in estrogen levels and the removal of fluid from the body of the future mother.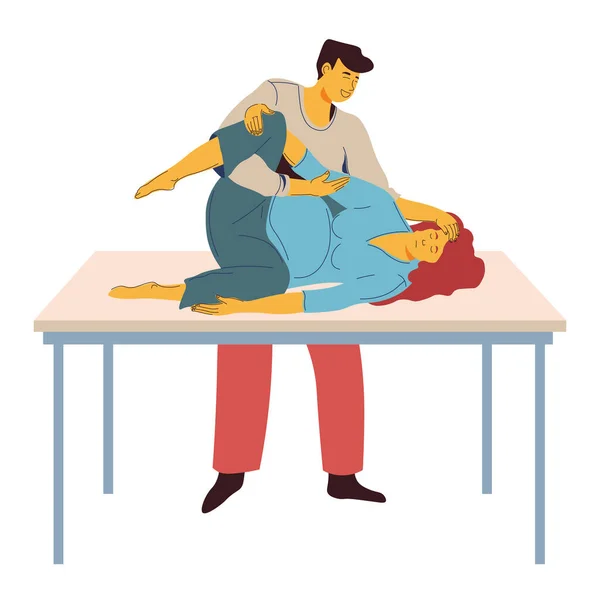 Similar changes in the body of a non-pregnant woman are observed during menstruation. The chair can become more frequent up to 2-3 times a day, at the same time there may be some liquefaction of the feces. More frequent urge to defecate, a sharp change in the color and smell of feces, combined with nausea and vomiting, is a reason for consulting a doctor - food poisoning can be masked under such "harbingers".
Similar changes in the body of a non-pregnant woman are observed during menstruation. The chair can become more frequent up to 2-3 times a day, at the same time there may be some liquefaction of the feces. More frequent urge to defecate, a sharp change in the color and smell of feces, combined with nausea and vomiting, is a reason for consulting a doctor - food poisoning can be masked under such "harbingers".
Fundal prolapse. Shortly before delivery, the baby presses the presenting part (most often the head) against the lower segment of the uterus and pulls it down, pressing against the entrance to the small pelvis. The fetus "groups", taking the most advantageous position for itself at the time of the onset of contractions. As a result of such "preparations" from the side of the fetus, the uterus "sags", and its upper part - the bottom - ceases to exert pressure on the internal organs. After lowering the bottom of the uterus, the pregnant woman has no shortness of breath (it becomes easier to breathe, there is a feeling of a full breath).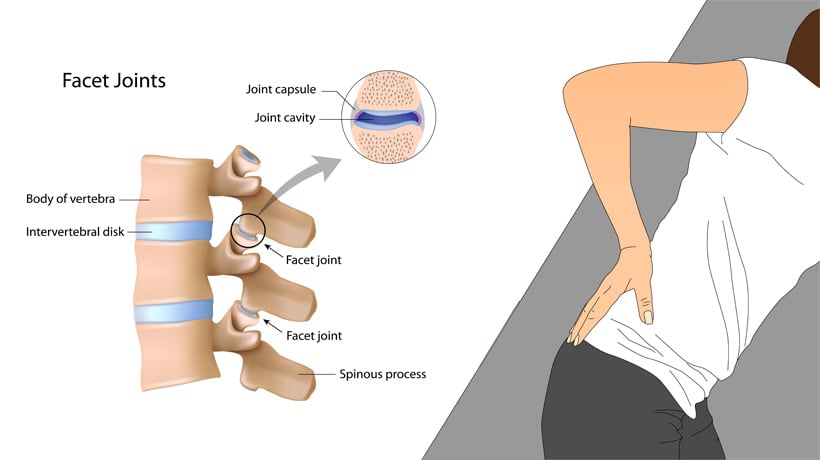 If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part. Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent.
If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part. Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent.
Isolation of the mucous plug. During pregnancy, the glands of the mucous membrane of the cervical canal (the lumen of the cervix) secrete a special secret. It is a thick, sticky, jelly-like mass that forms a kind of cork. The mucous plug completely fills the cervical canal, preventing the penetration of bacterial flora from the vagina into the uterine cavity. Thus, cervical mucus, or the mucous plug of the cervix, protects the fetus from ascending infection. Before childbirth, when the cervix begins to soften under the influence of estrogen, the cervical canal opens slightly and the cervical mucus contained in it can be released. In this case, the expectant mother may find small clots of yellowish-brownish mucus, transparent, jelly-like, odorless. The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases.
Thus, cervical mucus, or the mucous plug of the cervix, protects the fetus from ascending infection. Before childbirth, when the cervix begins to soften under the influence of estrogen, the cervical canal opens slightly and the cervical mucus contained in it can be released. In this case, the expectant mother may find small clots of yellowish-brownish mucus, transparent, jelly-like, odorless. The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases.
Training contractions. Training or false contractions are called such contractions that appear shortly before childbirth and are not actually labor activity, since they do not lead to the opening of the cervix. A contraction is essentially a single contraction of the uterine wall; this contraction usually lasts a few seconds. At the time of the contraction, the expectant mother feels a gradually increasing and then gradually decreasing tension in the abdomen. If at this moment you put your hand on your stomach, you can notice that the stomach becomes very hard, but after the contraction it completely relaxes and becomes soft again. In addition to involuntary tension of the uterus, other changes in the well-being of the expectant mother during false contractions are usually not noted. It is not difficult to distinguish training fights from real ones. In most cases, false contractions are weak, painless, irregular or alternating at a significant interval (30 minutes or more). Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization. False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days.
Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization. False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days.
Discomfort. In the last weeks before giving birth, many pregnant women report discomfort in the lower abdomen and in the area of the sacrum (the area slightly below the waist). Such changes in
the well-being of the expectant mother is caused by sprain of the pelvic ligaments and increased blood flow to the pelvic organs. Usually these minor sensations, described as a feeling of "light languor" in the lower abdomen, are comparable to similar phenomena in the period before or during menstruation.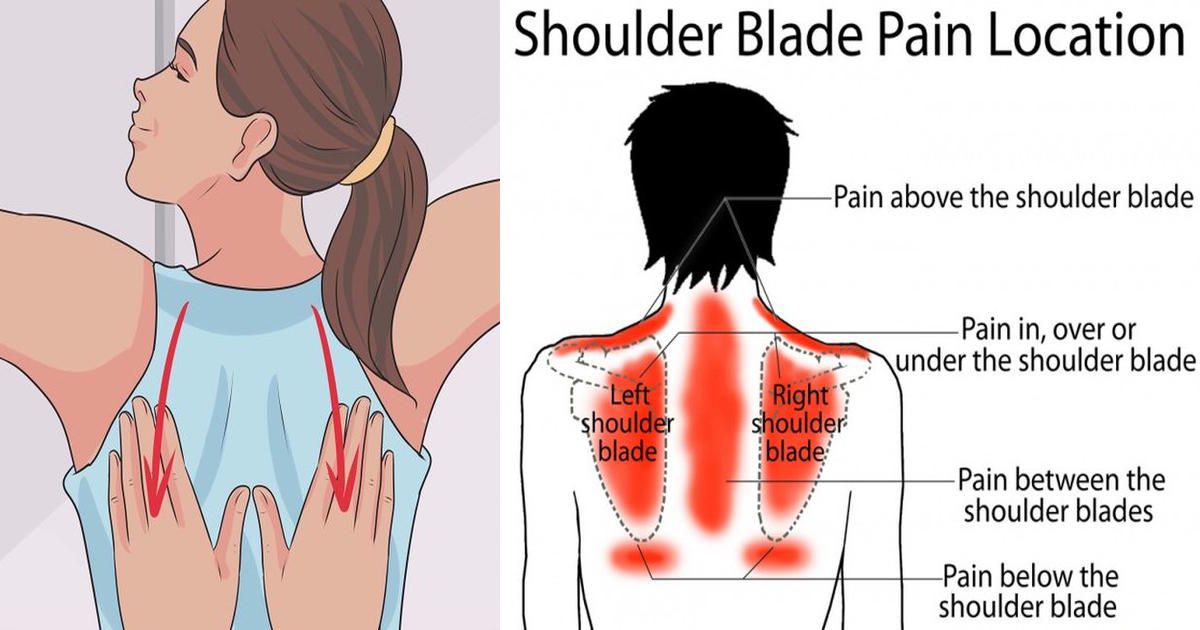 Discomfort, like training contractions, more often disturbs the expectant mother in the morning and evening hours. The level of discomfort is minimal, it should not worry the expectant mother and does not require medical intervention.
Discomfort, like training contractions, more often disturbs the expectant mother in the morning and evening hours. The level of discomfort is minimal, it should not worry the expectant mother and does not require medical intervention.
All harbingers of childbirth can appear during the last two weeks before childbirth, their presence, as well as their absence, is the norm and does not require a visit to a doctor. It is important to learn to listen to changes in your body, not to be afraid of changes in well-being associated with prenatal preparation, and most importantly, to have time to mentally and physically prepare for the most important event - the birth of a baby.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Pathophysiological basis of pain syndrome in childbirth
Pain as an integrative function of the body mobilizes a wide variety of functional systems to protect the body from the effects of harmful factors and includes emotional, motor-vegetative and humoral manifestations, generally identical stress responses to adverse effects [1, 2].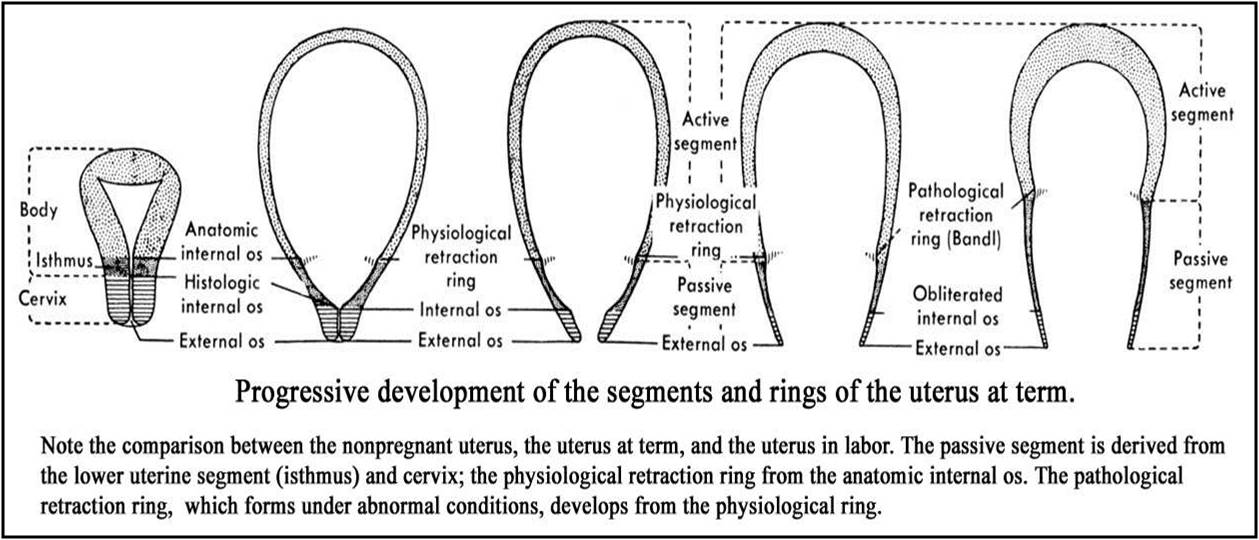 Disclosure of physiological links that provide a variety of signs of pain is carried out through the study of the central and peripheral structures of the nervous system involved in the perception, transmission and analysis of pain stimuli, as well as by studying the mechanisms that regulate the flow of pain impulses to the brain [3].
Disclosure of physiological links that provide a variety of signs of pain is carried out through the study of the central and peripheral structures of the nervous system involved in the perception, transmission and analysis of pain stimuli, as well as by studying the mechanisms that regulate the flow of pain impulses to the brain [3].
The neurophysiology of labor pain is represented by a complex multi-neuron reflex arc, the main links of which, like any other type of pain, can be represented by the following triad: impulsation resulting from irritation of peripheral nociceptors; the reaction of the central structures of the brain to receive the appropriate impulses; efferent response, which is a combination of emotional, vegetative and motor reactions. Thus, the nervous system, reacting to a damaging effect, is essentially a transport highway through which afferent information flows from the focus of damage to the centers of pain sensitivity of the spinal cord and brain, and each of its levels is characterized by a certain component of the pain reaction [4].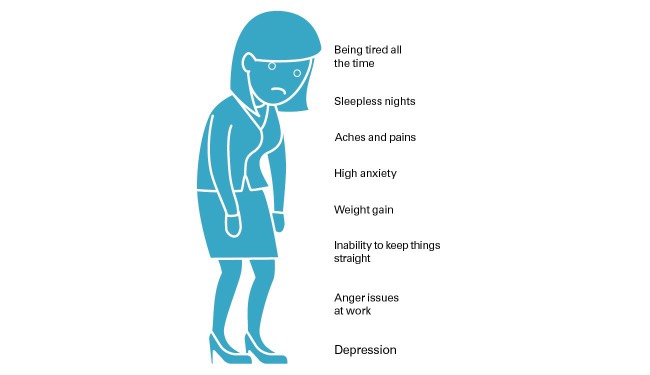 In the phenomenon of labor pain, two components of pain sensitivity are conventionally distinguished: visceral and somatic.
In the phenomenon of labor pain, two components of pain sensitivity are conventionally distinguished: visceral and somatic.
Visceral component of pain response
Visceral pain occurs early in the first and second stages of labour. The contractile activity of the uterus and the opening of the cervical canal play a leading role in the occurrence of visceral pain. There is evidence from J. Bonica and H. Chadwick [5] that manual palpation of the body of the uterus during caesarean section under local infiltration anesthesia was not accompanied by labor-like pain [5]. At the same time, manual impact on the cervix in women during caesarean section reproduced labor pain. It is possible that sensitization of cervical afferent fibers before and during childbirth can cause pain in the first stage of labor, in contrast to Bregston-Hicks contractions (false, rehearsal), which appear towards the end of pregnancy and are not accompanied by them [6, 7]. However, prior sensitization of these nociceptors appears to be necessary to make them sensitive to uterine contractions [8] and to increase signaling to the dorsal horn of the spinal cord [9]. An indicator of sensitization during childbirth is hyperalgesia, which occurs in response to mechanical stimulation of the skin of the lower abdomen, resulting in a total convergence of impulses coming from the ends of afferent fibers of both the skin of the lower abdomen and the cervix [10].
However, prior sensitization of these nociceptors appears to be necessary to make them sensitive to uterine contractions [8] and to increase signaling to the dorsal horn of the spinal cord [9]. An indicator of sensitization during childbirth is hyperalgesia, which occurs in response to mechanical stimulation of the skin of the lower abdomen, resulting in a total convergence of impulses coming from the ends of afferent fibers of both the skin of the lower abdomen and the cervix [10].
With each contraction of the uterus, pressure is transferred to the lower uterine segment and cervix, causing them to stretch and dilate, simultaneously activating baro- and mechanoreceptors [11]. Active labor activity is characterized by activation of baro- and mechanoreceptors with a high threshold of excitability. The increase in perceived pain intensity commonly seen with the progression of contractions may in part be due to the lowering of the nociceptor response threshold caused by repeated stimulation as a result of uterine contractions. In addition, a number of substances released during rupture of myometrial cells during repeated uterine contractions lead to stimulation of chemoreceptors. These released substances include bradykinin, histamine, serotonin, acetylcholine, potassium ions, and substance P [12]. Myometrial ischemia due to contraction of uterine arteries is another mechanism in these cellular responses [13, 14].
In addition, a number of substances released during rupture of myometrial cells during repeated uterine contractions lead to stimulation of chemoreceptors. These released substances include bradykinin, histamine, serotonin, acetylcholine, potassium ions, and substance P [12]. Myometrial ischemia due to contraction of uterine arteries is another mechanism in these cellular responses [13, 14].
The resulting afferent impulse is transmitted through thin unmyelinated C-fibers, which, as part of sympathetic fibers, pass through the paracervical zone, upper, middle, and lower hypogastric nerve plexuses, getting into the lower thoracic and lumbar sympathetic trunk [15, 16]. Pain fibers from the sympathetic trunk, passing through the white connecting branch associated with the spinal nerves from Th x to L I , as part of the posterior roots, are sent to the posterior horns of the spinal cord, ending in a synapse on the cells of the second neurons. Repeated afferent impulses cause increased sensitivity of the second neurons in the dorsal horn, central sensitization, which leads to an increase in signal transmission in the ascending pathways [17]. It is believed that the parasympathetic innervation of the uterus is of little importance in the transmission of uterocervical pain [11].
It is believed that the parasympathetic innervation of the uterus is of little importance in the transmission of uterocervical pain [11].
Irradiation of pain along C-fibers is ensured by the presence of a wide synaptic connection between the C-fibers themselves and the possibility of direct transmission of excitation to neighboring axons due to the crossing of some of the fibers at the level of the posterior horn. Such a wide diffusion during the conduction of a pain impulse is typical when it comes from the visceral organs (P.K. Anokhin, 1962). This phenomenon explains the fact that women in labor describe this pain as dull and poorly localized (diffuse feeling of pain) and not always sensitive to opioids.
At the beginning of the first stage of labor, pain correlates with dermatomes * Th XI and Th XII . By the end of the first period, the pain spreads to the dermatomes Th x to L I . Thus, pain sensations are localized in the lower abdomen, sacrum and back.
Somatic component of pain response
Somatic pain occurs in addition to visceral pain at the end of the first stage of labor, reaching a maximum in the second period. It is associated with irritation of the endings of the afferent nerves that innervate the vaginal part of the cervix, perineum and vagina, as a result of tension and stretching of the uterine ligaments and peritoneum, pressure on bone structures, ligaments of the pelvis, stretching, ischemia and trauma to the pelvic floor, perineum and vagina. In addition, contraction of the ganglia adjacent to the cervix and lower part of the uterus is believed to cause additional nociceptive input during the end of the first and beginning of the second stages of labor [18]. The somatic component manifests itself during the “lowering” of the presenting part of the fetus to the pelvic floor against the background of increasing regularity and intensity of contractions.
Somatic pain is transmitted by myelin Aδ fibers, which provide a high speed of nerve impulse conduction. The transmission of impulses occurs through the pudendal nerve and perineal branches of the posterior cutaneous nerve of the thigh to the spinal cord at the level of segments S II -S IV . Somatic fibers from the skin branches of the ilioinguinal and femoral-genital nerves also carry afferent impulses to segments L I and L II .
The transmission of impulses occurs through the pudendal nerve and perineal branches of the posterior cutaneous nerve of the thigh to the spinal cord at the level of segments S II -S IV . Somatic fibers from the skin branches of the ilioinguinal and femoral-genital nerves also carry afferent impulses to segments L I and L II .
In the second stage of labor, in addition to the areas already captured, the pain extends to the upper part of the lower extremities and is felt as pressure on the lower back and perineum. At the end of the second stage of labor, somatic pain is acute and clearly localized in the vagina, rectum, and perineum. It radiates to adjacent dermatomes Th x and L I and is more resistant to opioids compared to visceral pain.
One of the main substrates of intracentral interaction in the posterior horns of the spinal cord is the gelatinous substance (lamina II), which lies in the path of the afferent canals and receives collaterals from most afferent fibers (visceral and somatic). It is assumed that the neurons of the gelatinous substance control the interaction of visceral and skin afferent flows, which is directly related to the mechanism of referred pain [19].].
It is assumed that the neurons of the gelatinous substance control the interaction of visceral and skin afferent flows, which is directly related to the mechanism of referred pain [19].].
After initial processing in the gelatinous substance, the stimuli are transmitted by the interneurons of the spinothalamic tract to the thalamus, where all ascending nociceptive pathways form synapses as they move to the brain. In the thalamus, information is redistributed to the somatosensory cortex, which performs spatiotemporal and sensory-descriptive analysis of pain, taking into account its location, intensity, and duration [20]. An important role is played by the relationship of the thalamus with the limbic system involved in the implementation of the affective-emotional aspect of pain, and the prefrontal cortex of the brain, which is considered the most important area for the cognitive-rational assessment of pain (decision making, differentiation of conflicting thoughts and motives, differentiation and integration of objects and concepts , concentration of attention on the necessary objects) [21, 22]. Both the prefrontal and limbic regions are involved in the regulation of mood and anxiety symptoms, and activation of these regions may enhance the perception of pain [23]. The transmission of impulses through the spinoreticular tract to the reticular formation of the brain contributes to the activation of motor, autonomic and sensory functions, causing excitation and the emotional component of pain.
Both the prefrontal and limbic regions are involved in the regulation of mood and anxiety symptoms, and activation of these regions may enhance the perception of pain [23]. The transmission of impulses through the spinoreticular tract to the reticular formation of the brain contributes to the activation of motor, autonomic and sensory functions, causing excitation and the emotional component of pain.
The basis of the stated concept of pain are theories of specificity and intensity regimen. Nevertheless, pain remains a complex phenomenon, the definition and mechanisms of which have undergone various changes in medicine over the years [24].
Theories of pain
Thus, R. Melzack and P. Wall [25] put forward the theory of the "entrance gate", according to which an important role in the entry of pain impulses into the CNS through fibers of various types belongs to feedback mechanisms localized in the gelatinous substance of the dorsal horns of the spinal cord. Excitation of thick sensory fibers (Aα and Aß) during stimulation closes the “gates of pain”, while exposure to thin fibers (Aδ and C) opens the “gates” [25].
Excitation of thick sensory fibers (Aα and Aß) during stimulation closes the “gates of pain”, while exposure to thin fibers (Aδ and C) opens the “gates” [25].
Subsequently, R. Melzack [26, 27] transformed the concept of the "entrance gate" into the neuromatrix theory. Viewing the brain as the ultimate mechanism for evaluating certain characteristics of pain, it takes into account the confluence of multiple factors, including past experience, cultural background, emotional state, cognitive information, stress management, and the immune system, in addition to the most negative sensory input.
Numerous components of the neuromatrix that determine the perception of pain are produced by three parallel networks: sensory-descriptive (somatosensory components), affective-motivational (components of the limbic system) and evaluative-cognitive (thalamocortical components) [26]. The model also takes into account the additional influence of the neuroendocrine, autonomic nervous system and the modulation of the immune system. Synaptic inputs to these networks can be either phasic (short bursts such as cutaneous sensory input or attention span) or tonic (longer modulating signals such as cultural baggage and past experience). The summation of the three parallel processes forms a personal perception of pain and a "program of action", including conscious and unconscious strategies for dealing with pain, used by a woman in childbirth.
Synaptic inputs to these networks can be either phasic (short bursts such as cutaneous sensory input or attention span) or tonic (longer modulating signals such as cultural baggage and past experience). The summation of the three parallel processes forms a personal perception of pain and a "program of action", including conscious and unconscious strategies for dealing with pain, used by a woman in childbirth.
It should be noted that the contradictions in the mechanisms of pain have become the subject of research in several directions, not only by pathophysiologists, but also by clinicians who are constantly faced with the problem of pain in their daily work. Among the main directions, one can distinguish the development of neurochemical studies of the neurotransmitter mechanisms of pain, the study of the role of opioid receptors and endogenous morphines, as well as the central structures in the implementation of the pain response.
Pain control mechanisms
At present, there is no doubt about the polyneurochemistry of the nociceptive and antinociceptive systems of the brain, which can be considered as one of the leading factors that ensure the reliability of integral pain integration. An important role is played by neurotransmitters (acetylcholine, norepinephrine, serotonin), as well as calcitonin-gene-related peptide and substance P, each of which is associated with the provision of certain components of the psychophysiological phenomenon of pain [28, 29].
An important role is played by neurotransmitters (acetylcholine, norepinephrine, serotonin), as well as calcitonin-gene-related peptide and substance P, each of which is associated with the provision of certain components of the psychophysiological phenomenon of pain [28, 29].
Another important structure of pain modulation is the central periaqueductal gray matter of the brainstem (CPGR). Most of the opioid-induced antinociceptors originate from this structure, and the same site is the main one for descending inhibitory pathways [30]. Receiving nociceptive impulses from the posterior horns of the spinal cord, the CSVM is bilaterally connected to the hypothalamus, frontal cortex, and amygdala, areas responsible for the control of emotions, in particular, anxiety and fear, which may explain the effect of emotions on the modulation of pain perception [31].
Stimulation of the periwire gray matter activates enkephalin-releasing neurons located in the raphe nuclei of the brainstem. Serotonin released from the raphe nuclei, reaching the posterior horn of the spinal cord, forms synapses with "inhibitory interneurons" located in the II plate (gelatinous substance). When activated, these interneurons release endogenous opioid neurotransmitters that bind to μ-opioid receptors on the axons of C- and Aδ-fibers that carry pain signals from peripherally activated nociceptors. Activation of μ-opioid receptors inhibits the release of substance P from first-order neurons and, in turn, inhibits the activation of second-order neurons, which are responsible for the transmission of pain signals along the spinothalamic tract to the ventral posterolateral nucleus of the thalamus. Thus, the nociceptive signal is suppressed before it can reach the cortical areas that interpret the signals as "pain" [32].
Serotonin released from the raphe nuclei, reaching the posterior horn of the spinal cord, forms synapses with "inhibitory interneurons" located in the II plate (gelatinous substance). When activated, these interneurons release endogenous opioid neurotransmitters that bind to μ-opioid receptors on the axons of C- and Aδ-fibers that carry pain signals from peripherally activated nociceptors. Activation of μ-opioid receptors inhibits the release of substance P from first-order neurons and, in turn, inhibits the activation of second-order neurons, which are responsible for the transmission of pain signals along the spinothalamic tract to the ventral posterolateral nucleus of the thalamus. Thus, the nociceptive signal is suppressed before it can reach the cortical areas that interpret the signals as "pain" [32].
It is also necessary to note the significant role of opioid receptors and endogenous morphines in the regulation of pain sensitivity as neurotransmitters and neuromodulators of the nociceptive and antinociceptive systems of the brain. According to studies [33], receptive fields in posterior horn neurons are dynamic and can change the frequency of pain impulse transmission to the brain in response to changes in stimuli, neurotransmitters, and neuromodulators.
According to studies [33], receptive fields in posterior horn neurons are dynamic and can change the frequency of pain impulse transmission to the brain in response to changes in stimuli, neurotransmitters, and neuromodulators.
The analgesic properties of β-endorphins in the relief of labor pain were evaluated by T. Oyama et al. [34]. The study included 14 women in labor (7 primiparous and 7 multiparous), who, when the cervix was dilated by 3.5—5 cm, subdurally at the level of L III —L IV 1 mg of synthetic β-endorphin was administered. The authors demonstrated a fast (onset of action after 3.5±0.5 min) and long-term (mean duration 18.8±1.6 h) analgesic effect of the synthetic analog. At the same time, its administration did not affect labor activity and the intrauterine state of the fetus.
The results of studies have shown a progressive increase in the concentration of ß-lipotrophin, ß-endorphin and γ-lipotrophin in the mother's blood to a maximum by the 32nd week of pregnancy [35]. An increase in the concentration of endogenous peptides during pregnancy may be one of the factors responsible for the decrease in the sensitivity of pregnant women to local and general anesthetics. The minimum alveolar concentrations of halothane and isoflurane decrease in pregnant women by 25% and 40%, respectively [35]. Thus, an increase in the concentration of peptides should be considered as an endogenous protective mechanism that is activated against the background of progressing pregnancy and has a regulatory effect on pain during childbirth.
An increase in the concentration of endogenous peptides during pregnancy may be one of the factors responsible for the decrease in the sensitivity of pregnant women to local and general anesthetics. The minimum alveolar concentrations of halothane and isoflurane decrease in pregnant women by 25% and 40%, respectively [35]. Thus, an increase in the concentration of peptides should be considered as an endogenous protective mechanism that is activated against the background of progressing pregnancy and has a regulatory effect on pain during childbirth.
Currently, the ability of oxytocin to modulate pain and induce analgesia is of increasing scientific interest, which is confirmed by a number of clinical studies [36-38]. S. Gutierrez et al. [39] demonstrated that pain and hypersensitivity caused by peripheral nerve injury regress faster in rats if it occurs shortly before delivery, and subarachnoid administration of oxytocin (into the cerebrospinal fluid) induces antihypersensitization, which can be counteracted by an oxytocin receptor antagonist. The considered protective mechanism reflects the delay in oxytocin signaling at the level of the spinal cord in the postpartum period [39].
The considered protective mechanism reflects the delay in oxytocin signaling at the level of the spinal cord in the postpartum period [39].
Acting on the central and peripheral nervous system, oxytocin directly reduces the activity of spinal neurons that receive sensory information [40], excites interneurons in the spinal cord that inhibit gamma-aminobutyric acid (GABA-interneurons) [41, 42], reduces Aδ/C -afferent ascending nociceptive impulsation [42]. Additional mechanisms include the involvement of endogenous opioid [43] and cannabinoid [44] systems modulating pain perception. Subarachnoid injection of oxytocin in rats with symptoms of inflammation caused an antinociceptive effect by activating oxytocin receptors, as well as μ- and κ-opioid receptors involved in oxytocin-induced somatic analgesia at the spinal level [45]. In addition to somatic analgesia, subarachnoid administration of oxytocin can also be an effective pharmacological treatment for visceral pain by inhibiting nociceptive responses to acute bladder irritation [46].
In addition, Z. Tan et al. [47] revealed a biphasic effect of oxytocin: low doses of oxytocin increase GABA-activated fluxes leading to suppression of primary sensory transmission, while its higher doses decrease presynaptic inhibition of GABA interneurons. These results are consistent with a recent study by P. Juif and P. Poisbeau [48], which showed that intravenous injections of low doses of oxytocin induced oxytocin-mediated antinociception, while its higher doses induced vasopressin-V1A-mediated nociception in male rats.
The presented new data on the ability of oxytocin to modulate the pain response and induce oxytocin-induced analgesia seem to be a promising scientific direction that requires further study of specific mechanisms for the implementation of these effects both at the spinal and supraspinal levels, which may open up new possibilities for the use of low doses of oxytocin as an anesthetic.
Thus, the modern understanding of the neurophysiological mechanisms of pain is based on the existence of specific pain afferent systems in the brain, consisting of certain types of fibers and specialized groups of nerve cells in the spinal cord and brain stem.