Severe sickness during pregnancy
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 12 to 20, although for some women it can last longer.
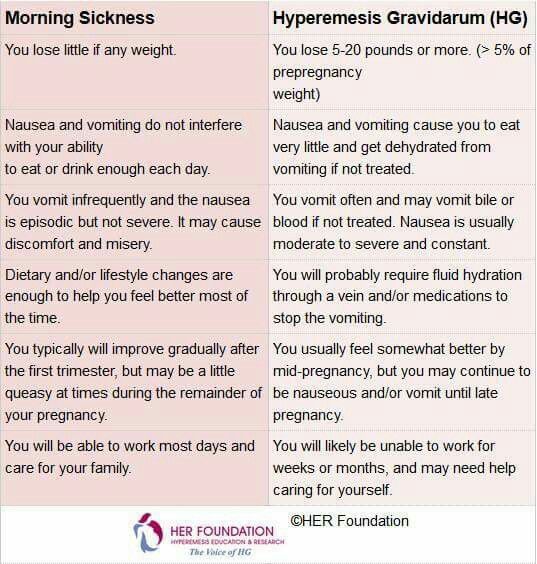
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
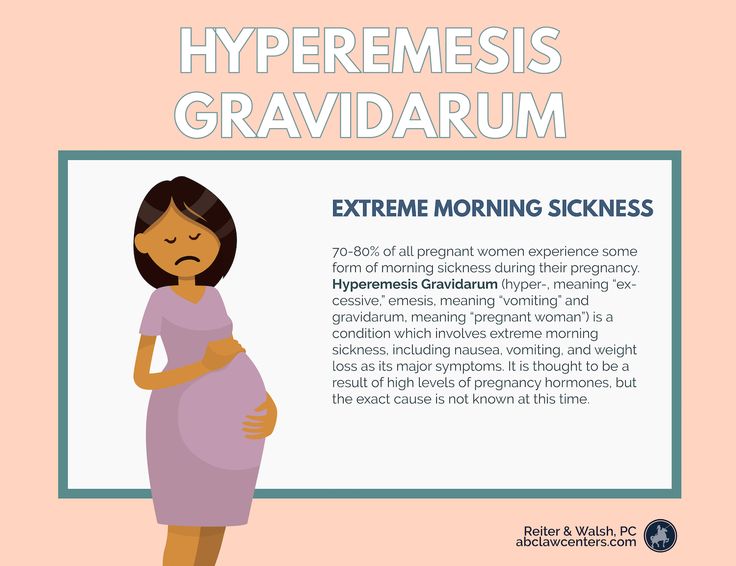
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- dehydration – symptoms include feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See videos and written interviews of women talking about their experiences of hyperemesis gravidarum on the healthtalk website.
What causes hyperemesis gravidarum?
It's not known exactly what causes HG, or why some women get it and others do not. There is evidence that it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, steroids, or a combination of these.
These include anti-sickness (anti-emetic) drugs, steroids, or a combination of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given into a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself. Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to a partner, family members and friends if you want to.
Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to a partner, family members and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Severe Morning Sickness (Hyperemesis Gravidarum) (for Parents)
What's Morning Sickness?
During the first trimester of pregnancy, many women have the bouts of nausea and vomiting known as morning sickness.
Despite its name, morning sickness can happen day or night. It usually starts around the 6th week of pregnancy, is at its worst around week 9, and stops by weeks 16 to 18. Although unpleasant, morning sickness is considered a normal part of a healthy pregnancy.
What’s Severe Morning Sickness?
Severe morning sickness is when nausea and vomiting get so serious that a pregnant woman vomits several times a day, loses weight, and gets dehydrated or is at risk for dehydration.
If this rare pregnancy-related condition isn’t treated, it can affect a woman's health and her baby's ability to thrive.
The medical term for severe morning sickness is "hyperemesis gravidarum" (hi-per-EM-eh-sis grav-ih-DARE-um), which means "excessive vomiting during pregnancy." It usually follows a similar timeline to normal morning sickness. But it can go longer, sometimes lasting for the whole pregnancy. Often, the symptoms get less severe as the pregnancy continues.
Most cases of hyperemesis gravidarum affect a woman's first pregnancy. But women who have it in one pregnancy are more likely to have it in future pregnancies.
What Causes Severe Morning Sickness?
The cause of severe morning sickness isn’t known. But it might be related to the hormone changes of pregnancy. A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
Severe morning sickness also might run in families. It’s more common in women whose close family members (such as mothers and sisters) have had it.
Other things that can increase a woman's chances of having severe morning sickness include:
- carrying multiples (twins, triplets, etc.)
- history of motion sickness
- migraine headaches with nausea or vomiting
What Problems Can Happen?
The nausea and vomiting that happen in severe morning sickness are so extreme that they can harm the mother and the baby. Not being able to keep down food makes it hard for the mom to meet her nutritional needs. So she might lose weight. And a loss of fluids, combined with the loss of stomach acid from vomiting, can cause dehydration and electrolyte imbalances.
If severe morning sickness isn’t treated, it can cause many problems, including organ failure and the early birth of her baby.
When Should I Call the Doctor?
Call the doctor right away if you’re pregnant and have any of these symptoms:
- nausea that lasts throughout the day, making it impossible to eat or drink
- vomiting three to four times per day or not being to keep anything in the stomach
- brownish vomit or vomit with blood or streaks of blood in it
- weight loss
- fainting or dizziness
- peeing less than usual
- a fast heart rate
- a lot of headaches
- unpleasant, fruity mouth or body odor
- extreme tiredness
- confusion
How Is Severe Morning Sickness Treated?
Treatments used for morning sickness, such as eating dry crackers in the morning or a bland diet, may be recommended for women with extreme morning sickness. But these might not help with severe symptoms.
Medical treatment can include:
- a short period of not eating to rest the gastrointestinal system
- intravenous (IV) fluids
- vitamin and nutritional supplements
Some women might get medicine to stop the vomiting, either by mouth or through an IV.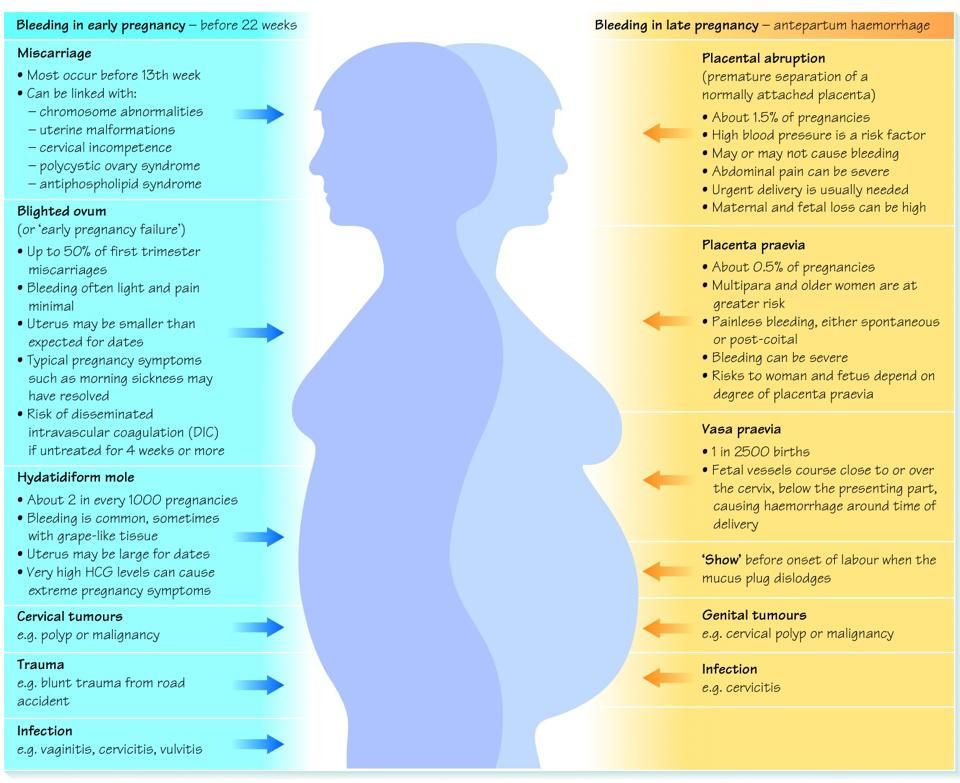 The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
- Eat a bland diet.
- Eat frequent small meals.
- Drink plenty of liquids when not feeling nauseated.
- Avoid spicy and fatty foods.
- Eat high-protein snacks.
- Avoid sensory stimuli that can act as triggers (like specific smells or noises).
If a woman feels anxious or depressed about her condition, talking to a therapist or counselor might help her cope with her feelings.
What Else Should I Know?
With treatment, women with severe morning sickness can feel better and get the nourishment they need so they and their babies thrive. And lifestyle changes can help ease nausea and vomiting and make the pregnancy more enjoyable.
With time, symptoms usually do improve. And, of course, they stop by the time a woman's next journey starts: parenthood.
» 10 DANGEROUS DIAGNOSIS DURING PREGNANCY!
from Down syndrome to the heart , from light to the kidneys . ..
..
without a doubt, the dream of each parent is the capture of his healthy child, but not always everything happens the way we want it to. A potential problem can change from feelings of joy and excitement to sadness and anxiety. Fortunately, the latest technologies and the rapid development of medicine are becoming assistants in this situation. The disease of the child that occurs in the womb can now be diagnosed at an early stage through constant examination and observation, as a result of which immediate actions are taken to restore the health of the child. Specialist-perinatologist of the Department of Obstetrics and Gynecology of the Acibadem Maslak Clinic Assoc. Dr. Julia Dede noted: “There is a 3-5 percent chance of developing pathologies during pregnancy. For the detection of which constant surveys and observations are carried out. New generation high resolution ultrasound equipment and obtaining baby DNA from maternal blood sampling are some of the new screening methods. ” An innovation that has been successfully practiced in recent years, the method of extracting the DNA of a child from the mother’s blood can be carried out as early as 8 weeks of pregnancy, Dr. Julija Dede added: “A small amount of blood, 20 cc, obtained from the mother, is sufficient to determine the DNA child and risk assessment of Down syndrome at 99 percent." The doctor explained some of the problems that can be found in the womb and made important warnings and suggestions.
” An innovation that has been successfully practiced in recent years, the method of extracting the DNA of a child from the mother’s blood can be carried out as early as 8 weeks of pregnancy, Dr. Julija Dede added: “A small amount of blood, 20 cc, obtained from the mother, is sufficient to determine the DNA child and risk assessment of Down syndrome at 99 percent." The doctor explained some of the problems that can be found in the womb and made important warnings and suggestions.
- Kidney disorders
Kidney disorders may be included in the examination of fetal pathologies. There are many pathologies of the kidneys from small to no kidneys at all and kidneys that are out of place. Although most of the kidney pathologies are not life threatening, they can cause kidney disease in later years. Today, many kidney pathologies can be cured.
- Lung diseases
Lung diseases are congenital diseases. For example, diseases such as cysts in the lungs, incomplete formation of the lungs, connections of the esophagus with the respiratory tract can develop. These diseases are asymptomatic in the mother and can only be diagnosed by careful ultrasonographic examination. Treatment is carried out after childbirth.
These diseases are asymptomatic in the mother and can only be diagnosed by careful ultrasonographic examination. Treatment is carried out after childbirth.
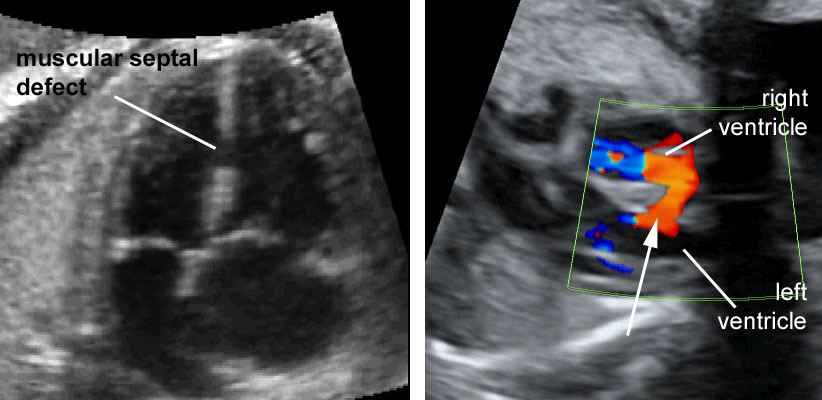
- Heart disease
The 20th week of pregnancy is important for the development of the heart. Therefore, the period from 19to 22 weeks of gestation is ideal for examining fetal pathologies. Many genetic or environmental factors cause cardiac abnormalities. Maternal use of risky diabetes medications during pregnancy, exposure to measles and rubella may be causes. The most common among cardiac pathologies are tetralogy of fallot (“blue” heart disease), transposition of the great vessels of the heart, large holes in the heart, or underdevelopment of one side of the heart due to severe stenosis. Today, many cardiac disorders can be detected during pregnancy.
- Cleft lip ( Cleft palate or lip )
The pathology of cleft palate or lip, commonly known as cleft lip, occurs in 1 in 1,000 newborns. The cause of occurrence is still unknown. Drugs taken by the mother during pregnancy, X-rays, consanguineous marriages, some injuries, the use of harmful substances, and trauma during pregnancy can cause this disease. After birth, two plastic surgeries are performed: surgery on the lips in the first months after birth, on the palate - before the end of infancy.
The cause of occurrence is still unknown. Drugs taken by the mother during pregnancy, X-rays, consanguineous marriages, some injuries, the use of harmful substances, and trauma during pregnancy can cause this disease. After birth, two plastic surgeries are performed: surgery on the lips in the first months after birth, on the palate - before the end of infancy.
- Dwarfism and clubfoot
Problems such as fusion of the child's toes, more or no limbs, limbs that are too long or short, can be detected while still in the womb and corrected with surgery and prostheses. Dislocation of the hip, crooked legs, bowed neck, dwarfism, and severe developmental disorders of the limbs and spine are some of the most serious skeletal pathologies.
- Skeletal abnormalities
Skeletal abnormalities in the baby that occur during pregnancy can be detected during a fetal scan, but their causes have not yet been determined. It is believed that they occur due to a vitamin deficiency in the mother. Smoking, alcohol and drug use by the mother during pregnancy can also cause skeletal pathologies, and the influence of genetics is not excluded. In this case, it is necessary to inform the family by the attending physician and take appropriate measures.
It is believed that they occur due to a vitamin deficiency in the mother. Smoking, alcohol and drug use by the mother during pregnancy can also cause skeletal pathologies, and the influence of genetics is not excluded. In this case, it is necessary to inform the family by the attending physician and take appropriate measures.
- Head and brain pathologies
Head and brain pathologies are among the most common pathologies that can be detected at an early stage using ultrasound diagnostics. Some of the most common problems are underdevelopment of the skull, lack of brain tissue, lack of brain tissue, over-expansion of fluid-filled sacs, and underdevelopment of brain tissue. An important part of these pathologies is lost soon after the birth of the child. In this case, depending on the outcome and severity of the disease, the choice is given to the family within the principles of treatment and ethics.
- Abdominal wall problems
Some types of abdominal wall problems can be treated with surgery after the baby is born. The formation of a hernia on the navel, intestines or other organs of the abdominal cavity (and sometimes even the heart) or the protrusion of the intestines or liver due to the absence of the abdominal wall are the most common types of pathologies of the abdominal cavity.
The formation of a hernia on the navel, intestines or other organs of the abdominal cavity (and sometimes even the heart) or the protrusion of the intestines or liver due to the absence of the abdominal wall are the most common types of pathologies of the abdominal cavity.
- Neural tube defect
It implies a non-closure of the tubular structure of the formation of the brain and spinal cord in the womb. Many of the children with neural tube defects do not survive, and the survivors become paralyzed or unable to perform vital functions such as bladder and bowel control. The most obvious cause of the defect is the lack of folic acid in the mother's body, which should be taken before and after pregnancy.
- Down syndrome
Assoc. . dr . Julie Dede explained: “It is not a disease, Down syndrome is a genetic feature that can be detected at an early stage. The potential risk can be determined between the 11th and 14th weeks of pregnancy, with the help of ultrasound, the formation of the nasal bone and the thickness of the child's collar space are determined, and then some parameters taken from the mother's blood are considered. Or, the likelihood of the syndrome can be determined by ultrasound data and some hormonal parameters in the mother's blood according to her age, smoking, medical history. We can also contribute by examining some echographic markers.”
The potential risk can be determined between the 11th and 14th weeks of pregnancy, with the help of ultrasound, the formation of the nasal bone and the thickness of the child's collar space are determined, and then some parameters taken from the mother's blood are considered. Or, the likelihood of the syndrome can be determined by ultrasound data and some hormonal parameters in the mother's blood according to her age, smoking, medical history. We can also contribute by examining some echographic markers.”
Complications of pregnancy. What are Pregnancy Complications?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Complications of pregnancy are pathological conditions in obstetric practice that have arisen in connection with gestation and violate its natural course. At the initial stages, they may not be accompanied by clinical symptoms, later they manifest pain in the lower abdomen, vaginal discharge, impaired fetal movement, headaches, and edema. For diagnosis, ultrasound of the uterus and fetus, MRI pelvimetry, laboratory tests, invasive prenatal methods, CTG and other methods are used. Depending on the condition of the woman and the unborn child, treatment may be aimed at maintaining or terminating the pregnancy.
At the initial stages, they may not be accompanied by clinical symptoms, later they manifest pain in the lower abdomen, vaginal discharge, impaired fetal movement, headaches, and edema. For diagnosis, ultrasound of the uterus and fetus, MRI pelvimetry, laboratory tests, invasive prenatal methods, CTG and other methods are used. Depending on the condition of the woman and the unborn child, treatment may be aimed at maintaining or terminating the pregnancy.
- Causes of pregnancy complications
- Classification
- Symptoms of pregnancy complications
- Diagnostics
- Treatment of pregnancy complications
- Prognosis and prevention
- Prices for treatment
General
According to experts in the field of obstetrics and gynecology, only about 30-50% of pregnancies proceed physiologically, and this percentage is constantly decreasing. The most common complications of the gestational period, apart from early toxicosis, are miscarriages, which end up to 15-20% of pregnancies, and premature births (6-10%). At the same time, 30-80% of very premature babies suffer from disabling diseases. Approximately 8% of pregnant women develop oligohydramnios, 3-8% - preeclampsia and eclampsia, 2-14% - gestational diabetes mellitus. Every fiftieth pregnancy is ectopic, and every two hundredth placenta previa occurs. Other types of complications in pregnant women are less common.
At the same time, 30-80% of very premature babies suffer from disabling diseases. Approximately 8% of pregnant women develop oligohydramnios, 3-8% - preeclampsia and eclampsia, 2-14% - gestational diabetes mellitus. Every fiftieth pregnancy is ectopic, and every two hundredth placenta previa occurs. Other types of complications in pregnant women are less common.
Complications of pregnancy
Causes of pregnancy complications
The complicated course of the gestational period can be triggered by many factors on the part of the mother or fetus. The most common causes of pregnancy complications are:
- Extragenital somatic pathology. With cardiovascular diseases (hypertension, heart defects, arrhythmias) and urological diseases (glomerulonephritis, pyelonephritis), the risk of late preeclampsia increases. Gestation can also lead to decompensation of almost any chronic disease.
- Endocrinopathy.
 With violations of the hypothalamic-pituitary regulation and endocrine function of the ovaries, the process of implantation of a fertilized egg suffers, and the contractile activity of the myometrium changes. Diabetes mellitus provokes microcirculatory disturbances both in the woman's body and in the fetoplacental system.
With violations of the hypothalamic-pituitary regulation and endocrine function of the ovaries, the process of implantation of a fertilized egg suffers, and the contractile activity of the myometrium changes. Diabetes mellitus provokes microcirculatory disturbances both in the woman's body and in the fetoplacental system. - Inflammatory gynecological diseases. With salpingitis, adnexitis, endometritis, the likelihood of ectopic tubal and cervical pregnancy increases. Chronic cervicitis can provoke isthmic-cervical insufficiency. With inflammation, intrauterine infection of the fetus is possible.
- Anomalies in the development of the uterus. In women with an intrauterine septum, a bicornuate, saddle-shaped or infantile uterus, spontaneous abortions, premature births, fetoplacental insufficiency, placental abruption and fetal hypoxia are more often diagnosed.
- Pathological pregnancy and childbirth in the past. Past miscarriages and preterm births increase the likelihood of recurrent miscarriage.
 Cicatricial deformity of the neck after its rupture is the main cause of isthmic-cervical insufficiency. After a uterine rupture in childbirth, it is likely to rupture in the later stages of the next pregnancy, especially multiples.
Cicatricial deformity of the neck after its rupture is the main cause of isthmic-cervical insufficiency. After a uterine rupture in childbirth, it is likely to rupture in the later stages of the next pregnancy, especially multiples. - Multiple pregnancy. If there are two or more fetuses in the uterus, chronic extragenital pathology is more often exacerbated, late toxicosis is observed, polyhydramnios occurs, leakage of amniotic fluid, and the threat of premature termination of pregnancy.
- Infectious diseases. Viral and bacterial infections can provoke miscarriage, premature birth, aggravate the course of preeclampsia, chronic somatic and endocrine diseases, and cause complications in the form of inflammation of the membranes. Some pathogens can infect the fetus in utero.
- Immunological factors. Habitual miscarriage is more often observed when the blood of the mother and fetus is incompatible according to the AB0 system or the Rh factor, and the patient has antiphospholipid syndrome.

- Genetic abnormalities of the fetus. The most common cause of pregnancy termination by early miscarriage is fetal developmental defects incompatible with life.
- Iatrogenic complications. Performing amnioscopy, amniocentesis, cordocentesis and chorion biopsy, suturing the cervix increases the risk of high rupture of the amniotic bladder, infection and early termination of pregnancy.
Additional provoking factors, in which complications of pregnancy are more often observed, are addictions (nicotine, alcohol, drugs), an asocial lifestyle. The risk group also includes pregnant women under 18 and over 35 years of age, patients with poor nutrition and obesity, women who lead an inactive lifestyle, experience excessive physical and psychological stress.
Classification
The clinical classification of pregnancy complications takes into account who and at what level pathological changes have occurred - in the mother, fetus, in the mother-fetus system or in embryonic structures.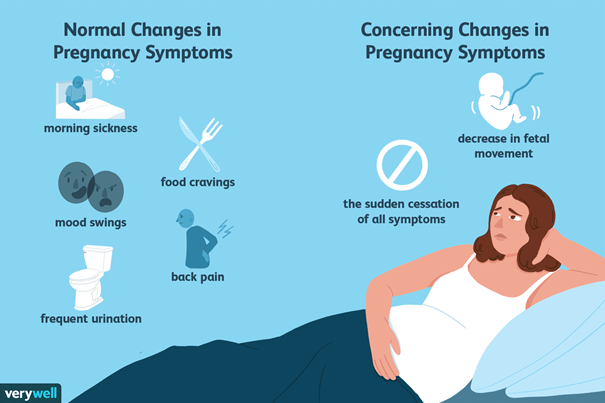 The main complications in women are:
The main complications in women are:
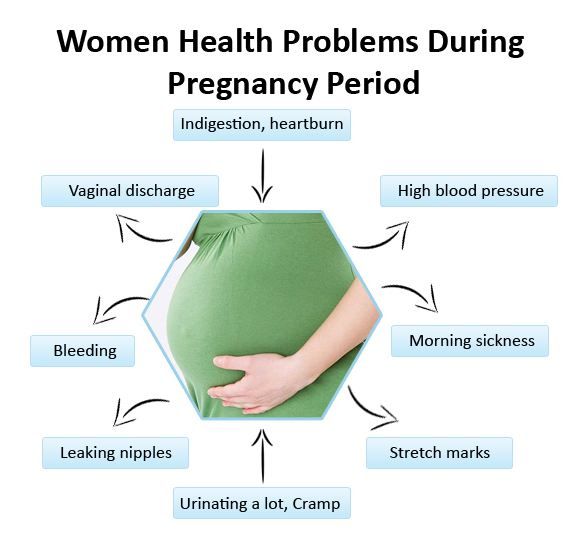
- Conditions and diseases associated with pregnancy. The patient may experience early toxicosis, late gestosis, anemia, gestational diabetes and thyrotoxicosis, varicose veins. Functional changes in the pyelocaliceal system contribute to the rapid development of inflammatory urological diseases.
- Complications of existing diseases. Loads on the body of a pregnant woman provoke decompensation of chronic endocrine and somatic pathology - thyrotoxicosis, hypothyroidism, diabetes mellitus, cardiomyopathy, hypertension, gastrointestinal diseases. Violation of the function of organs and systems sometimes reaches the degree of insufficiency (cardiovascular, renal, hepatic).
- Threatened miscarriage and miscarriage. Gestation can end prematurely with early or late spontaneous abortion (up to 22 weeks inclusive) or preterm birth (from 23 to 37 full weeks).
- Ectopic pregnancy. When a fetal egg is attached outside the uterine cavity, an ectopic pregnancy is observed.
 Currently, this condition in 100% of cases ends with the death of the fetus and the occurrence of severe complications in a woman (internal bleeding, hypovolemic shock, acute pain syndrome).
Currently, this condition in 100% of cases ends with the death of the fetus and the occurrence of severe complications in a woman (internal bleeding, hypovolemic shock, acute pain syndrome).
In some cases, the main pathological changes occur in the body of the fetus. This group of complications includes:
- Genetic anomalies. Malformations caused by genetic defects cause miscarriages, and during pregnancy - severe neurological, mental and somatic disorders in a child.
- Intrauterine infection. Infection can be caused by bacteria, mycoplasmas, chlamydia, fungi, viruses. Its complications are violation of fetal maturation, early termination of pregnancy, multiple malformations, fetal death, pathological course of childbirth.
- Fetal hypoxia. This condition is noted with insufficient oxygen supply, can cause ischemia and necrosis in various organs. The result of prolonged hypoxia is a congenital pathology of the newborn or antenatal fetal death.
- Hypotrophy. With a pronounced lag in fetal development from the gestational age, birth hypoxia, problems with spontaneous breathing, meconium aspiration with the subsequent development of pneumonia, thermoregulation disorders, hyperbilirubinemia, and brain damage may occur.
- Incorrect position and presentation. With pelvic and oblique presentation, the likelihood of complications in childbirth is high, with transverse independent childbirth becoming impossible.
- Frozen pregnancy. Intrauterine death of a child with its preservation in the uterine cavity leads to the development of severe inflammatory complications - purulent endometritis, peritonitis, sepsis, which pose a threat to the health and life of a woman.
With complications from the embryonic structures that provide nutrition and protection for the fetus, the unborn child most often suffers, which can develop inflammatory diseases, hypoxia, malnutrition, leading to congenital pathology or antenatal death. In addition, such complications provoke premature and pathological births. Depending on the level of damage, there are:
In addition, such complications provoke premature and pathological births. Depending on the level of damage, there are:
- Pathology of the placenta. Cysts and tumors can appear in the placental tissue, infectious and inflammatory processes (deciduitis, villitis, intervillezitis) can develop. Anomalies of the placental disc, violations in the attachment of the placenta to the uterine wall are possible - tight attachment, increment, ingrowth and germination. Serious complications are low location, presentation and premature detachment of the placenta.
- Pathology of the umbilical cord. When the inflammatory process spreads to the tissues of the umbilical cord, funiculitis occurs. The main anomalies in the development of the umbilical cord are its shortening, elongation, sheath attachment, the formation of false and true nodes, cysts, hematomas, teratomas, hemangiomas.
- Pathology of the membranes. The most common complications from the side of the fetal sac are low and polyhydramnios, premature rupture and leakage of water, the formation of amniotic bands, chorioamnionitis.
A separate group of complications is represented by disorders in the system of interaction between mother and fetus. The main ones are:
- Rh conflict. The condition is accompanied by the destruction of fetal red blood cells and the development of various complications, from hemolytic jaundice to the death of the child.
- Fetoplacental insufficiency. Violation of the morphological structure and functionality of the placenta, caused by various reasons, leads to hypoxia, malnutrition, and in severe cases, fetal death.
When classifying complications, it is equally important to take into account the time of their occurrence. There are early complications, often leading to abortion, and late ones, affecting the development of the fetus and the course of childbirth.
Symptoms of pregnancy complications
Despite the relationship between certain pathological conditions and gestational age, there are a number of common signs that indicate a complicated pregnancy. The first one is abdominal pain. Usually they are localized in the lower part of the abdominal cavity, they can give to the groin and lower back. Less often, the pain begins in the epigastrium, and then goes to the lower abdomen. Pain syndrome occurs with ectopic pregnancy, the threat of miscarriage and premature birth, threatening rupture of the uterus (in pregnant women with a scar on the uterus). In such cases, weakness, dizziness, and sometimes loss of consciousness are observed. Pain in inflammatory diseases is often combined with fever.
The first one is abdominal pain. Usually they are localized in the lower part of the abdominal cavity, they can give to the groin and lower back. Less often, the pain begins in the epigastrium, and then goes to the lower abdomen. Pain syndrome occurs with ectopic pregnancy, the threat of miscarriage and premature birth, threatening rupture of the uterus (in pregnant women with a scar on the uterus). In such cases, weakness, dizziness, and sometimes loss of consciousness are observed. Pain in inflammatory diseases is often combined with fever.
Vaginal discharge indicates a complication of pregnancy. Miscarriage, premature birth, abruption or placenta previa are accompanied by spotting. Purulent and mucopurulent leucorrhoea are observed in inflammatory processes. The watery nature of the discharge is characteristic of premature outflow or leakage of amniotic fluid.
Almost any change in a woman's general well-being can be a sign of possible complications.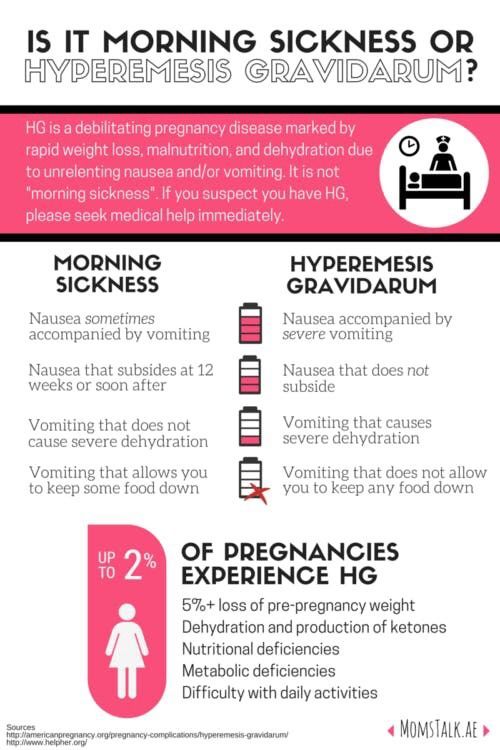 In the first trimester, pregnant women are worried about nausea, vomiting and other signs of early toxicosis. With late gestosis, dizziness, pain in the occipital region, the appearance of "flies" before the eyes, swelling in the legs, nausea, and vomiting occur. A sudden increase in temperature can be observed with the development of inflammatory complications or with an infectious disease. A pregnant woman may notice the appearance or intensification of symptoms characteristic of extragenital pathology - dry mouth, palpitations, shortness of breath, heartburn, varicose veins, etc.
In the first trimester, pregnant women are worried about nausea, vomiting and other signs of early toxicosis. With late gestosis, dizziness, pain in the occipital region, the appearance of "flies" before the eyes, swelling in the legs, nausea, and vomiting occur. A sudden increase in temperature can be observed with the development of inflammatory complications or with an infectious disease. A pregnant woman may notice the appearance or intensification of symptoms characteristic of extragenital pathology - dry mouth, palpitations, shortness of breath, heartburn, varicose veins, etc.
Complications of pregnancy from the side of the fetus are often detected by a change in the frequency of movements. If movements are not felt for more than 4 hours, there is no reaction to the usual stimuli (stroking the abdomen, music, food), you should urgently contact an obstetrician-gynecologist. Hypoxia is characterized by active stirring and a feeling of fetal hiccups.
Diagnostics
If a pregnancy complication is suspected, in the process of collecting an anamnesis, provoking factors are identified, an examination is prescribed to determine the type and degree of violations. Recommended for diagnosis:
Recommended for diagnosis:
- External obstetric examination. The size and shape of the uterus, the tone of its muscles, and areas of pain are determined.
- Inspection in mirrors. Allows you to detect discharge, assess the condition of the vaginal mucosa and cervix.
- Microscopy and culture of a vaginal smear. Indicated for assessing the state of the vaginal secretion, identifying pathogens of infectious diseases.
- Ultrasound of the pelvic organs. It is aimed at determining the size of the uterus, the state of its wall and scar (if any), assessing the size and condition of the fetus, placenta, umbilical cord, and the volume of amniotic fluid.
- MRI pelvimetry. Effectively detects anomalies in the development of the fetus and embryonic membranes, suspected by ultrasound.
- Invasive prenatal diagnosis. With the help of amnioscopy, amniocentesis, chorion biopsy, cordocentesis, placentocentesis and fetoscopy, congenital chromosomal abnormalities are excluded, the condition of the fetal membranes, the amount and color of the amniotic fluid are assessed.
- Non-invasive rapid tests. The determination of specific markers allows, in doubtful cases, to diagnose an ectopic pregnancy, to establish leakage of amniotic fluid, to confirm the premature onset of labor.
- Laboratory monitoring of pregnancy. Determination of the level of hormones - hCG, free beta-hCG and estriol, PAPP-A, placental lactogen and alpha-fetoprotein - is indicative of placental disorders, the presence of fetal pathologies and the complication of the gestation process.
- TORCH complex. In the course of a serological study, infectious diseases that affect the fetus in utero are diagnosed - toxoplasmosis, rubella, cytomegalovirus, herpes, hepatitis B and C, chlamydia, syphilis, gonorrhea, listeriosis, HIV, chickenpox, enterovirus.
- Dopplerography of uteroplacental blood flow. Provides an objective assessment of transplacental hemodynamics.
- Cardiotocography. It is prescribed to assess the fetal heartbeat, timely detection of bradycardia and tachycardia, indicating hypoxia and other complications that are critical for the child.
For dynamic control over the condition of the pregnant woman and fetus, identification of additional risk factors, general blood and urine tests, blood pressure and temperature control, ECG, and other instrumental and laboratory research methods can be used. Differential diagnosis of pregnancy complications is carried out with concomitant diseases (hypertension, renal colic, glomerulo- and pyelonephritis), acute surgical pathology (appendicitis, acute cholecystitis), inflammatory and non-inflammatory gynecological diseases. In difficult cases, a urologist, surgeon, therapist, anesthesiologist-resuscitator, infectious disease specialist, immunologist and other narrow specialists are involved in the diagnosis.
Treatment of pregnancy complications
The tactics of managing a pregnant woman in the presence of complications depends on their nature, severity, and the degree of risk to the fetus and mother. In the normal state of the child and pathological disorders that do not pose a serious threat to the life of a woman, drug therapy is prescribed to prolong pregnancy. The treatment plan may include:
The treatment plan may include:
- Hormonal preparations. Normalize the endocrine balance in the body.
- Tocolytics. Reduce the contractile activity of the myometrium.
- Antibacterial agents. Destroy pathogenic flora or prevent the development of infection.
- Anti-inflammatory drugs. Reduce the severity of the inflammatory process and pain syndrome.
- Glucocorticoids. Promote the maturation of lung tissue and accelerate the synthesis of surfactant.
- Sedatives. Relieve emotional stress.
According to indications, a woman is given symptomatic therapy for extragenital pathology, vitamin-mineral complexes, infusions of solutions are used. If necessary, suture the neck or install an obstetric pessary in the vagina. When certain types of pathology of the fetus, placenta and amniotic fluid are detected, fetal drainage and fetoscopic operations, intrauterine transfusions and infusions are indicated.
For the treatment of placental insufficiency, drugs that improve microcirculation and uteroplacental blood flow are used - antiplatelet agents and anticoagulants.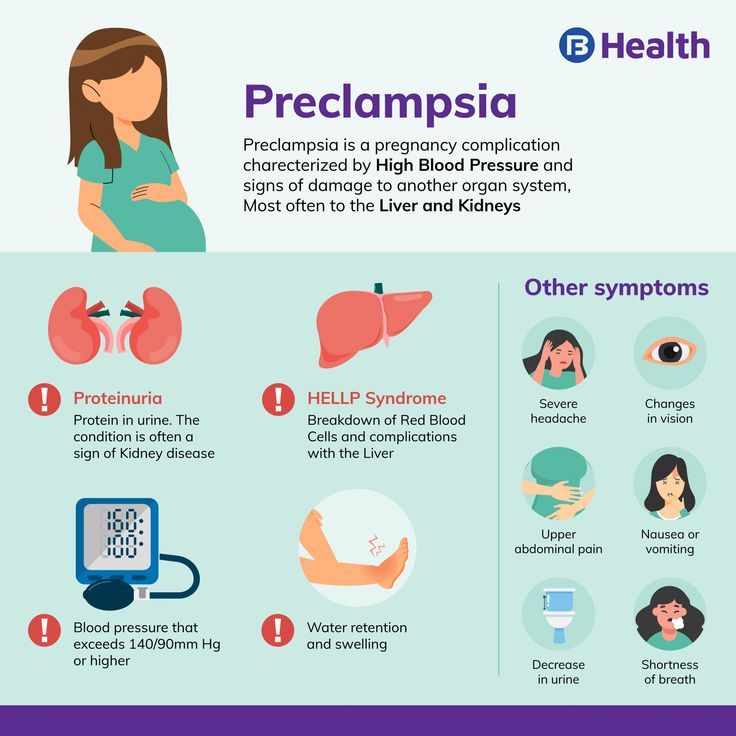 With Rhesus conflict, the administration of anti-Rhesus immunoglobulin is effective. The detection of gross malformations, the death of a child, an abortion that has begun, and conditions that threaten the life of the mother are indications for abortion and intensive care. Taking into account the term, a drug, mini- or medical abortion or artificial birth is performed.
With Rhesus conflict, the administration of anti-Rhesus immunoglobulin is effective. The detection of gross malformations, the death of a child, an abortion that has begun, and conditions that threaten the life of the mother are indications for abortion and intensive care. Taking into account the term, a drug, mini- or medical abortion or artificial birth is performed.
Prognosis and prevention
The prognosis of a complicated pregnancy depends on the nature of the pathology. With genetic defects, ectopic pregnancy and miscarriage, the fetus cannot be saved. In other cases, the probability of term pregnancy and the birth of a healthy child is determined by the time of detection and the degree of pathological disorders, as well as the correctness of obstetric tactics. To prevent pregnancy complications, women who plan to conceive a child are advised to treat concomitant diseases, give up bad habits, timely registration at the antenatal clinic and regular visits to the doctor, especially if there are risk factors.