Birth defect ultrasound
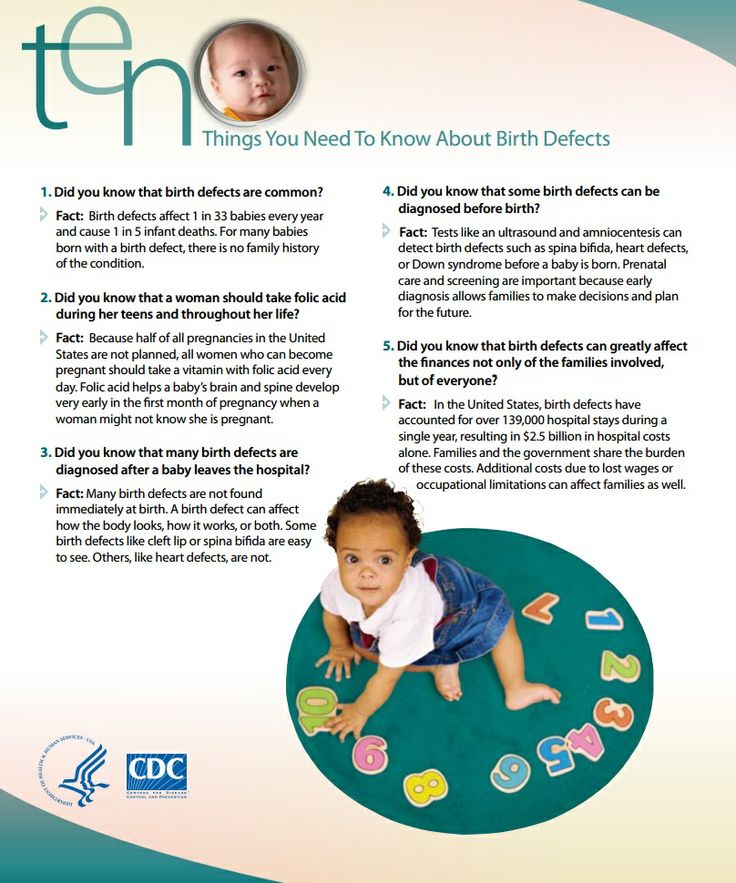
Diagnosis of Birth Defects | CDC
Birth defects can be diagnosed during pregnancy or after the baby is born, depending on the specific type of birth defect.
During Pregnancy: Prenatal Testing
Screening Tests
A screening test is a procedure or test that is done to see if a woman or her baby might have certain problems. A screening test does not provide a specific diagnosis—that requires a diagnostic test (see below). A screening test can sometimes give an abnormal result even when there is nothing wrong with the mother or her baby. Less often, a screening test result can be normal and miss a problem that does exist. During pregnancy, women are usually offered these screening tests to check for birth defects or other problems for the woman or her baby. Talk to your doctor about any concerns you have about prenatal testing.
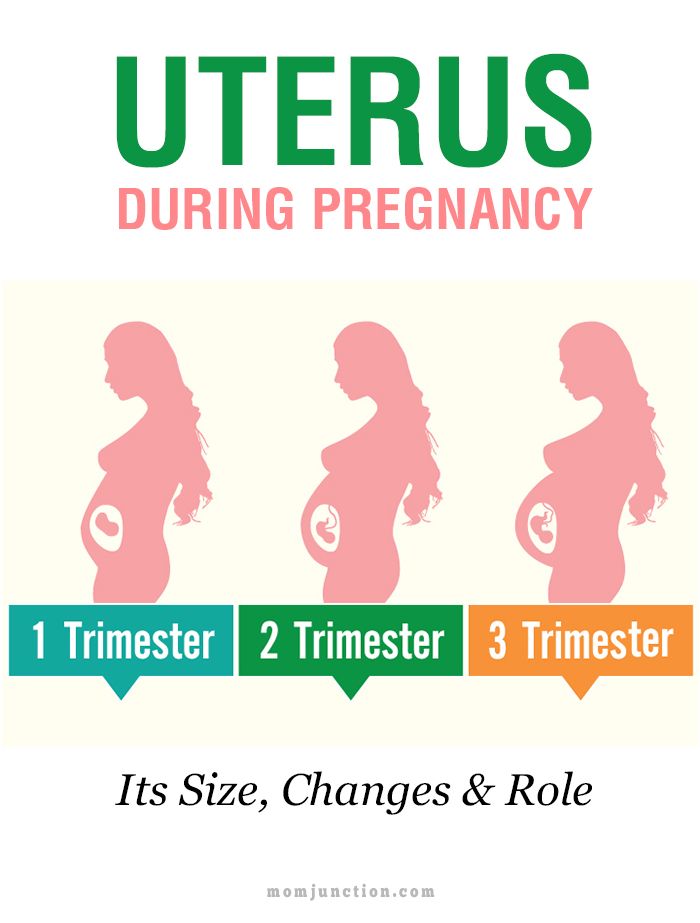
First Trimester Screening
First trimester screening is a combination of tests completed between weeks 11 and 13 of pregnancy. It is used to look for certain birth defects related to the baby’s heart or chromosomal disorders, such as Down syndrome. This screen includes a maternal blood test and an ultrasound.
- Maternal Blood Screen
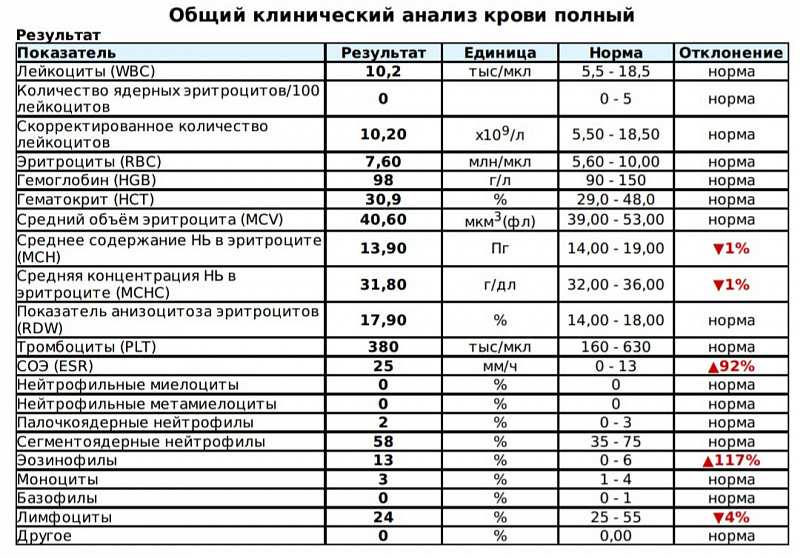
The maternal blood screen is a simple blood test. It measures the levels of two proteins, human chorionic gonadotropin (hCG) and pregnancy associated plasma protein A (PAPP-A). If the protein levels are abnormally high or low, there could be a chromosomal disorder in the baby.
- Ultrasound
An ultrasound creates pictures of the baby. The ultrasound for the first trimester screen looks for extra fluid behind the baby’s neck. If there is increased fluid found on the ultrasound, there could be a chromosomal disorder or heart defect in the baby.
Second Trimester Screening
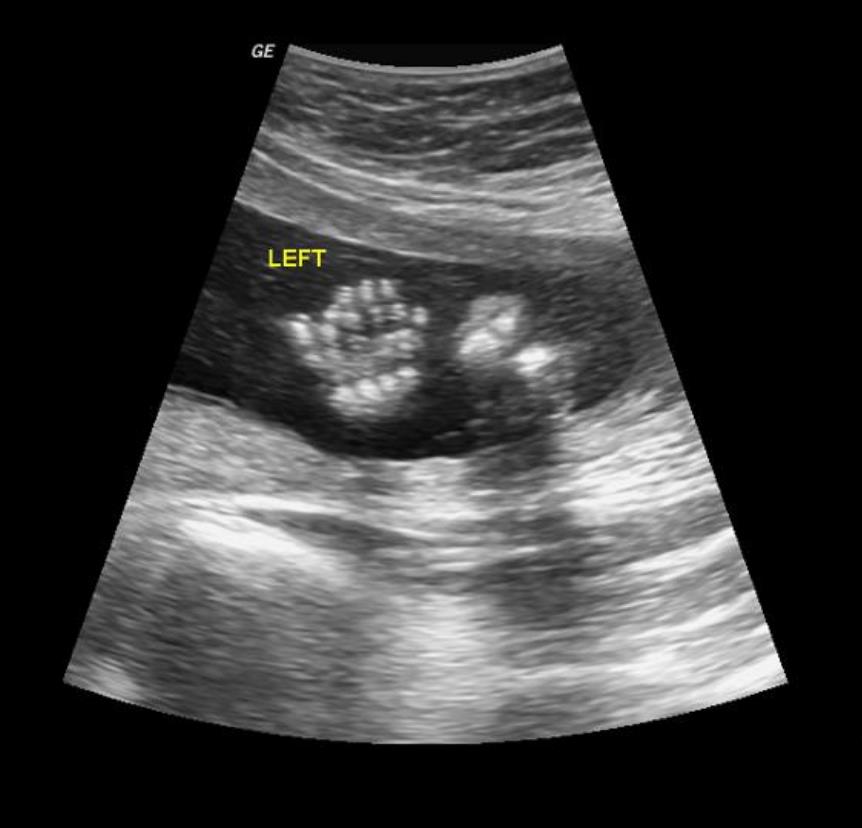
Second trimester screening tests are completed between weeks 15 and 20 of pregnancy. They are used to look for certain birth defects in the baby. Second trimester screening tests include a maternal serum screen and a comprehensive ultrasound evaluation of the baby looking for the presence of structural anomalies (also known as an anomaly ultrasound).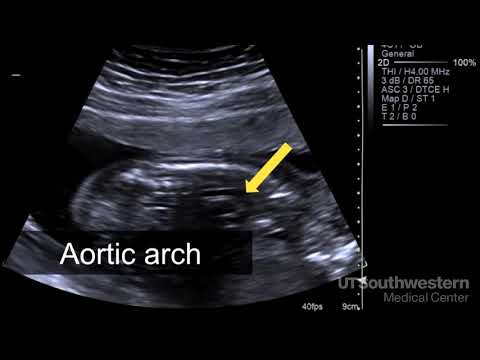
- Maternal Serum Screen
The maternal serum screen is a simple blood test used to identify if a woman is at increased risk for having a baby with certain birth defects, such as neural tube defects or chromosomal disorders such as Down syndrome. It is also known as a “triple screen” or “quad screen” depending on the number of proteins measured in the mother’s blood. For example, a quad screen tests the levels of 4 proteins AFP (alpha-fetoprotein), hCG, estriol, and inhibin-A. Generally, the maternal serum screen is completed during the second trimester.
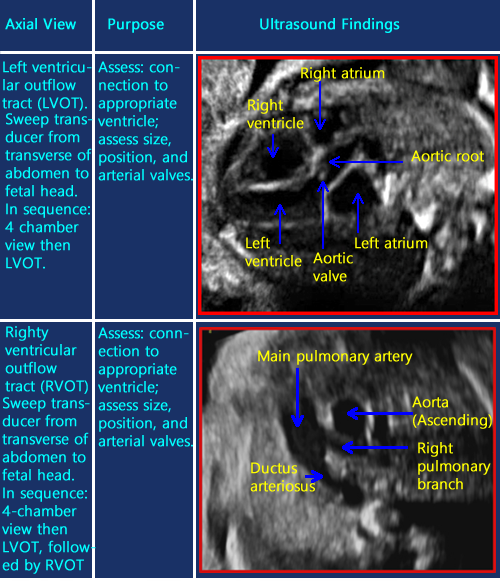
- Fetal Echocardiogram
A fetal echocardiogram is a test that uses sound waves to evaluate the baby’s heart for heart defects before birth. This test can provide a more detailed image of the baby’s heart than a regular pregnancy ultrasound. Some heart defects can’t be seen before birth, even with a fetal echocardiogram. If your healthcare provider finds a problem in the structure of the baby’s heart, a detailed ultrasound may be done to look for other problems with the developing baby.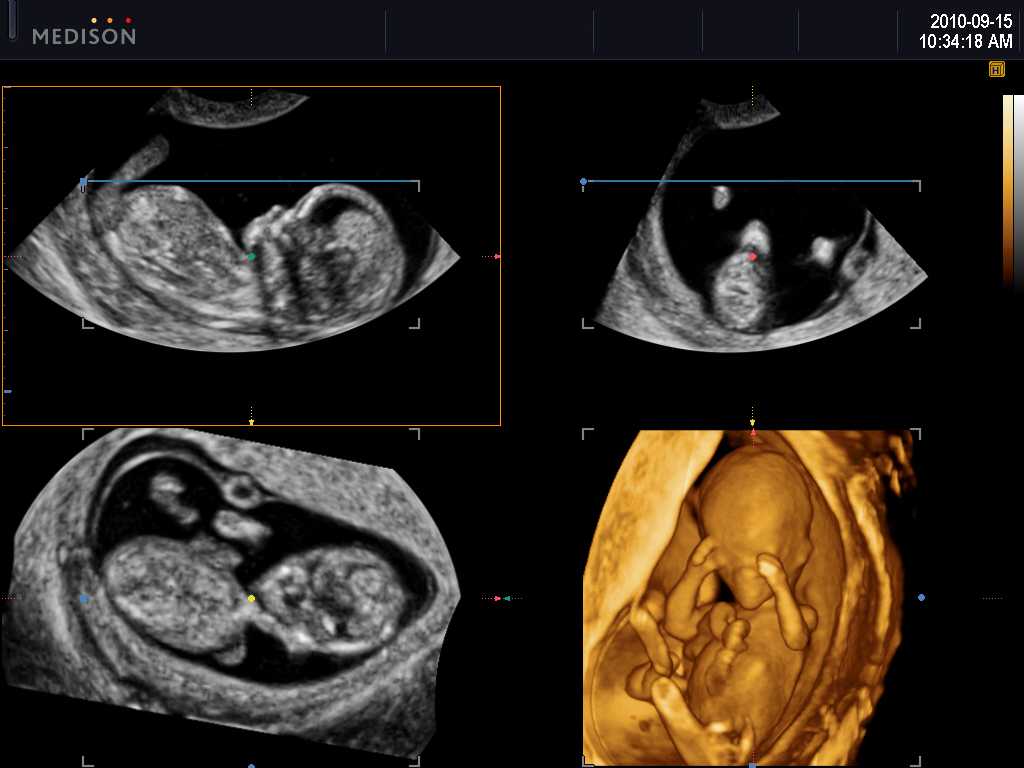
- Anomaly Ultrasound
An ultrasound creates pictures of the baby. This test is usually completed around 18–20 weeks of pregnancy. The ultrasound is used to check the size of the baby and looks for birth defects or other problems with the baby.
Diagnostic Tests
If the result of a screening test is abnormal, doctors usually offer further diagnostic tests to determine if birth defects or other possible problems with the baby are present. These diagnostic tests are also offered to women with higher risk pregnancies, which may include women who are 35 years of age or older; women who have had a previous pregnancy affected by a birth defect; women who have chronic diseases such as lupus, high blood pressure, diabetes, or epilepsy; or women who use certain medications.
High resolution Ultrasound
An ultrasound creates pictures of the baby. This ultrasound, also known as a level II ultrasound, is used to look in more detail for possible birth defects or other problems with the baby that were suggested in the previous screening tests.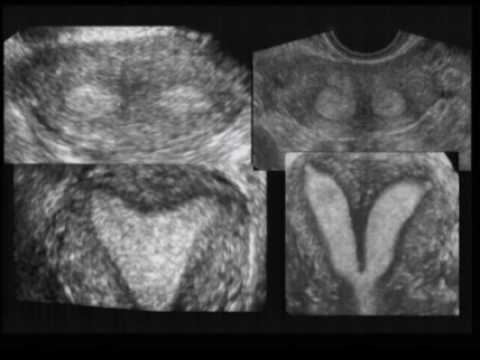 It is usually completed between weeks 18 and 22 of pregnancy.
It is usually completed between weeks 18 and 22 of pregnancy.
Chorionic Villus Sampling (CVS)
CVS is a test where the doctor collects a tiny piece of the placenta, called chorionic villus, which is then tested to check for chromosomal or genetic disorders in the baby. Generally, a CVS test is offered to women who received an abnormal result on a first trimester screening test or to women who could be at higher risk. It is completed between 10 and 12 weeks of pregnancy, earlier than an amniocentesis.
Amniocentesis
An amniocentesis is test where the doctor collects a small amount of amniotic fluid from the area surrounding the baby. The fluid is then tested to measure the baby’s protein levels, which might indicate certain birth defects. Cells in the amniotic fluid can be tested for chromosomal disorders, such as Down syndrome, and genetic problems, such as cystic fibrosis or Tay-Sachs disease. Generally, an amniocentesis is offered to women who received an abnormal result on a screening test or to women who might be at higher risk.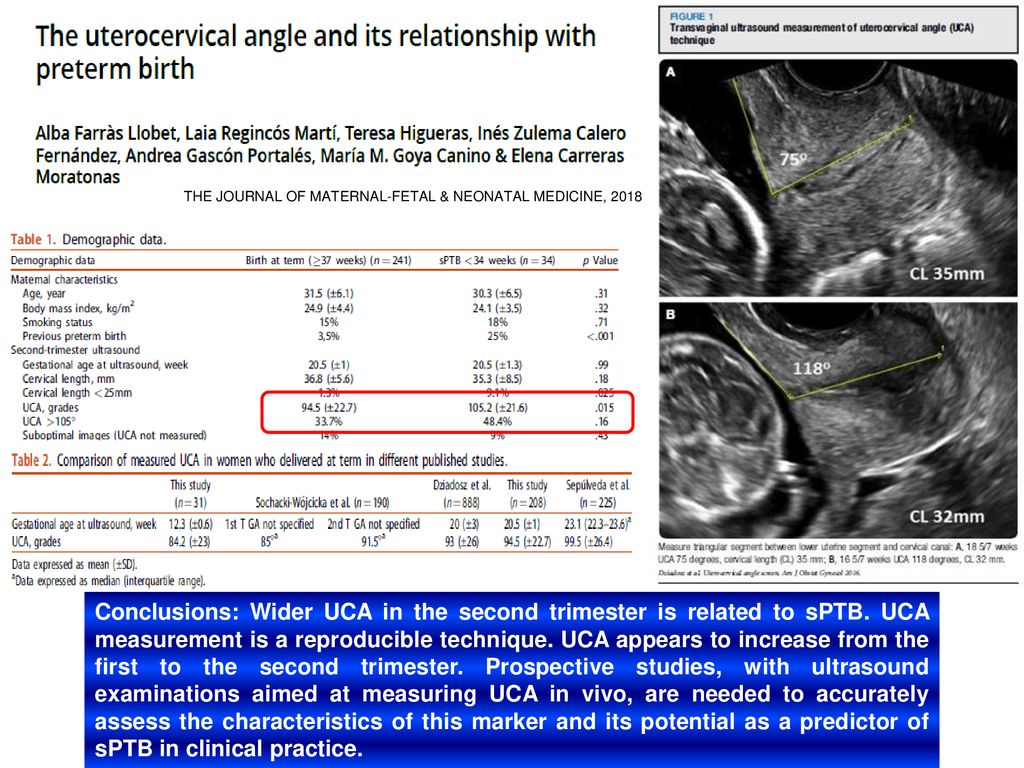 It is completed between 15 and 18 weeks of pregnancy. Below are some of the proteins for which an amniocentesis tests.
It is completed between 15 and 18 weeks of pregnancy. Below are some of the proteins for which an amniocentesis tests.
- AFP
AFP stands for alpha-fetoprotein, a protein the baby produces. A high level of AFP in the amniotic fluid might mean that the baby has a defect indicating an opening in the tissue, such as a neural tube defect (anencephaly or spina bifida), or a body wall defect, such as omphalocele or gastroschisis.
- AChE
AChE stands for acetylcholinesterase, an enzyme that the baby produces. This enzyme can pass from the baby to the fluid surrounding the baby if there is an opening in the neural tube.
After the Baby is Born
Certain birth defects might not be diagnosed until after the baby is born. Sometimes, the birth defect is immediately seen at birth. For other birth defects including some heart defects, the birth defect might not be diagnosed until later in life.
When there is a health problem with a child, the primary care provider might look for birth defects by taking a medical and family history, doing a physical exam, and sometimes recommending further tests.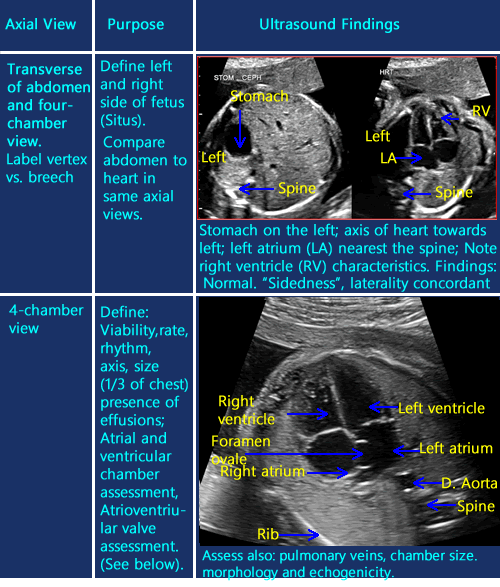 If a diagnosis cannot be made after the exam, the primary care provider might refer the child to a specialist in birth defects and genetics. A clinical geneticist is a doctor with special training to evaluate patients who may have genetic conditions or birth defects. Even if a child sees a specialist, an exact diagnosis might not be reached.
If a diagnosis cannot be made after the exam, the primary care provider might refer the child to a specialist in birth defects and genetics. A clinical geneticist is a doctor with special training to evaluate patients who may have genetic conditions or birth defects. Even if a child sees a specialist, an exact diagnosis might not be reached.
Preventing and Treating Birth Defects: What You Need to Know
If you’re thinking about becoming pregnant or are currently expecting, it’s important to understand the risk for birth defects. Birth defects cannot always be prevented, but there are many aspects of prenatal care that can protect your unborn baby. If your baby does have a birth defect or fetal condition, treatments are now available that have revolutionized an affected baby’s ability to survive and thrive after birth.
Learn more about prevention, diagnosis and available treatments for birth defects from Ahmet Baschat, M.D., director of the Johns Hopkins Center for Fetal Therapy, part of the Department of Gynecology and Obstetrics.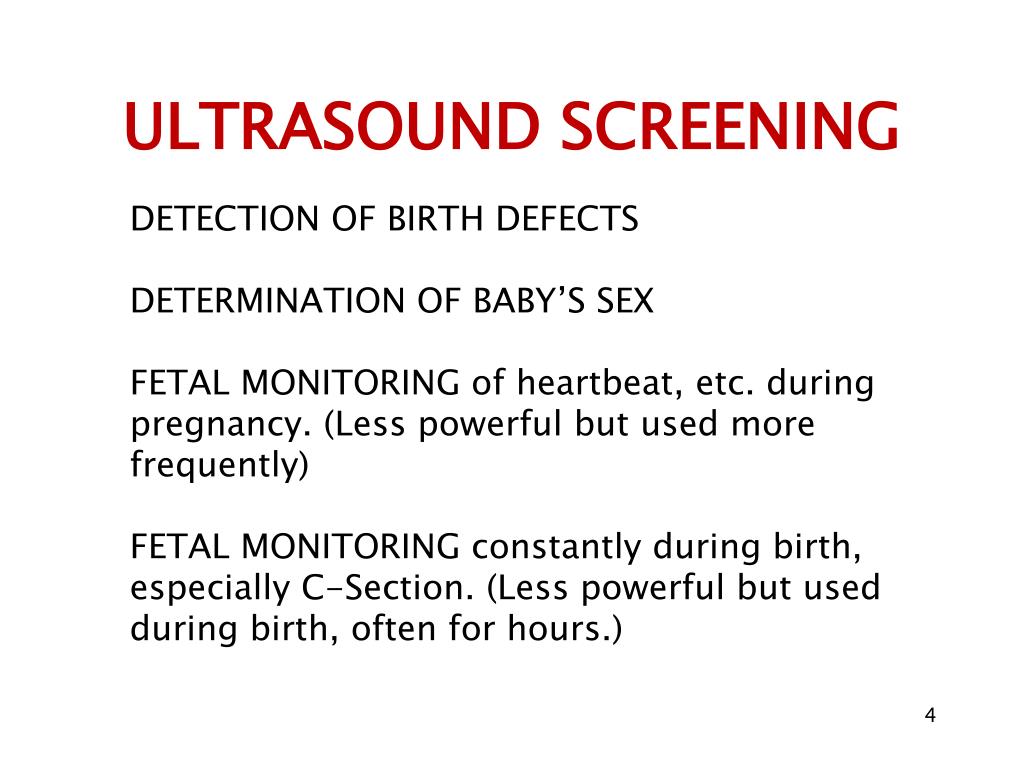
Can birth defects be prevented?
Though not all birth defects can be avoided, prenatal care and awareness of past or current conditions can help with prevention.
- Prenatal care. Taking a daily prenatal vitamin that includes at least 400 micrograms of folic acid can help prevent a variety of birth defects. You should be taking prenatal vitamins if you’re of reproductive age, when you’re actively trying to conceive and/or as soon as you find out you are pregnant. In addition to taking your prenatal vitamin, avoiding alcohol, tobacco and illegal drugs can significantly help prevent birth defects and pregnancy complications.
- Awareness of past or current conditions. If you previously had a pregnancy with a birth defect, it’s important to find out the most likely causes because it can help your physician plan preventive measures for your next pregnancy. For example, spina bifida is caused by a deficiency in folate, so if your previous pregnancy had spina bifida, you can take a high dose of folate to help prevent future spina bifida diagnoses.
Are all birth defects discovered before a baby is born?
It’s not always possible to detect all birth defects in utero. However, high-resolution ultrasounds done by certified prenatal ultrasound groups make it possible to diagnose defects that will cause a significant impact before birth.
Baschat says: “At the Center for Fetal Therapy, we recommend that pregnant women have the first-trimester nuchal translucency scan between 11 and 14 weeks and the anatomy scan between 18 and 20 weeks. These two ultrasounds provide us with the best opportunity for detecting birth defects.”
In recent years, some pregnant women have turned down the first-trimester ultrasound because a maternal screening blood test now exists for Down syndrome. The ultrasound is still strongly recommended, though, because there are many other serious birth defects that can be detected this early in pregnancy.
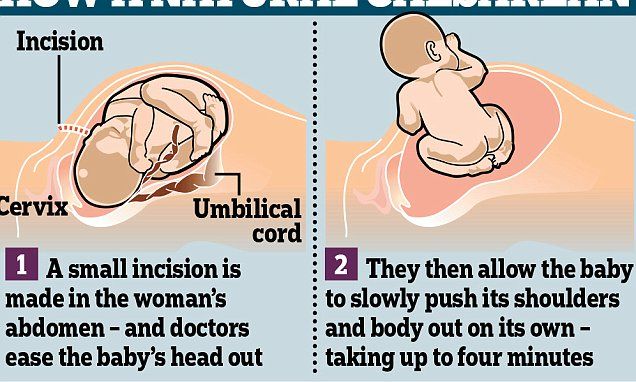
Is it possible to treat birth defects while a baby is in utero?
Absolutely.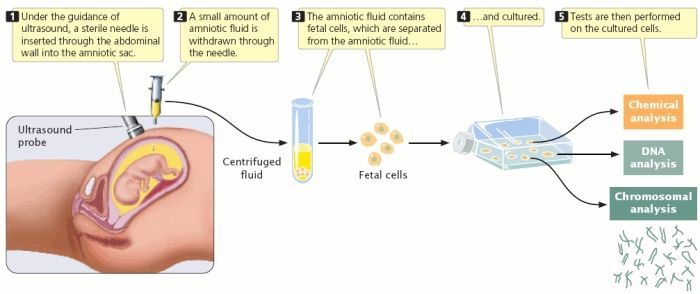 While there are many different types of birth defects, it’s extremely important to try to correct those that damage vital organs before the baby is born. The Center for Fetal Therapy specializes in treating several of these defects in utero, including:
While there are many different types of birth defects, it’s extremely important to try to correct those that damage vital organs before the baby is born. The Center for Fetal Therapy specializes in treating several of these defects in utero, including:
- Congenital diaphragmatic hernia. This condition, in which a hole in the diaphragm allows abdominal content to enter the chest and restrict lung development, can be significantly helped in utero through fetoscopic endotracheal occlusion, a surgery that improves lung function and significantly increases survival rates.
- Lower urinary tract obstruction. This occurs when the flow of urine is blocked from exiting the fetus’ body, leading to permanent kidney damage. Relieving this obstruction before birth protects the kidneys.
Fetal treatments also exist for conditions that make the baby unhealthy, even if they are not considered to be birth defects. For example, if a fetus has an irregular heartbeat, you can give the mother medication that will cross the placenta and treat the fetus.
How successful are in utero treatments for fetal conditions?
By treating fetal conditions in utero rather than waiting until after birth, fetuses are given significantly better chances of survival and a reduced need for major surgery after birth. For example, with a condition like twin-to-twin transfusion syndrome, in which identical twins develop a blood volume imbalance, both babies could die without any intervention. By performing laser surgery in utero, there is approximately a 95 percent chance that at least one baby will survive.
Explains Baschat, “Success rates vary depending on the condition, available treatments and the individual patient, but overall, where fetal interventions are available, we see a much higher rate of survival for affected fetuses.”
If a baby has fetal surgery, will he/she need different care after birth?
This will depend on the individual condition and type of surgery performed. For all fetal surgeries, your baby needs to be delivered at a hospital where pediatric subspecialties are in-house so the baby’s care can be managed after birth.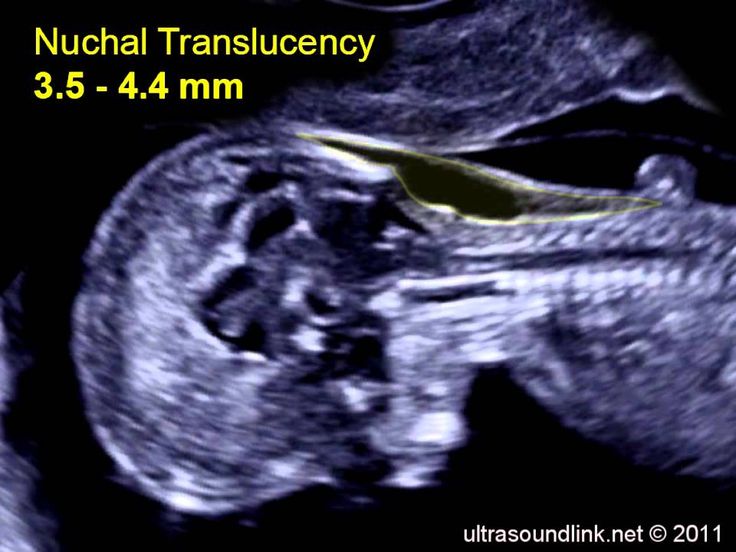 Baschat says: “Many of the treatments we perform require patients to deliver at the highest-level multispecialty hospital, like The Johns Hopkins Hospital. This way, all prenatal and postnatal care is available to you in one location.”
Baschat says: “Many of the treatments we perform require patients to deliver at the highest-level multispecialty hospital, like The Johns Hopkins Hospital. This way, all prenatal and postnatal care is available to you in one location.”
If you have one child affected by a birth defect, will all of your future children have that same condition?
All future children will not definitively be affected by the same birth defect, but it will depend on what the cause was. If the birth defect was caused by a genetic mutation, there may be a higher likelihood of recurrence, but if you seek care from a specialized center, maternal-fetal medicine specialists and genetic counselors can work with you to assess future risk.
The risk of some conditions can be determined before you become pregnant through genetic testing. If that doesn’t exist for the condition in question, maternal-fetal medicine specialists and genetic counselors can genetically test your fetus during pregnancy to see if she or he exhibits the mutation that affected your previous child.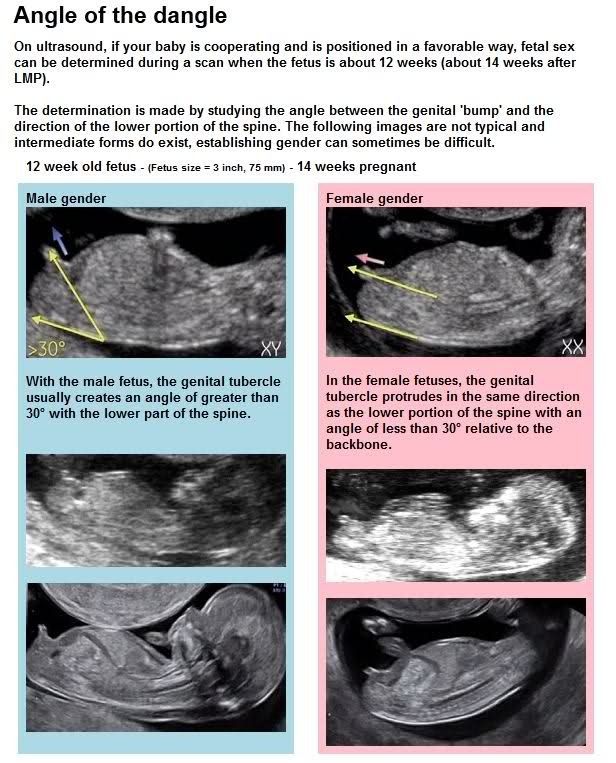
Are there communities in which you can speak with other families who have had children affected by birth defects?
There are many forums online, whether on the web or social media platforms, in which parents come together. “At our center, we reach out to previous patients to see if they are interested in communicating with new patients affected by the same condition,” Baschat explains. “They can empathize about the specific birth defect, but they can also provide guidance and advice about the experience of working with our center throughout the pregnancy and after the baby is born.”
In the future, what advances will take place in treating disease before birth?
Through prenatal diagnosis and understanding fetal disease better, physicians are learning more about what harms the fetus and what may be of benefit before birth. Additionally, new uses for minimally invasive surgical equipment are regularly being discovered.
There are also stem cell therapies, genomic medicine and a whole host of related treatments that are currently used for children and adults.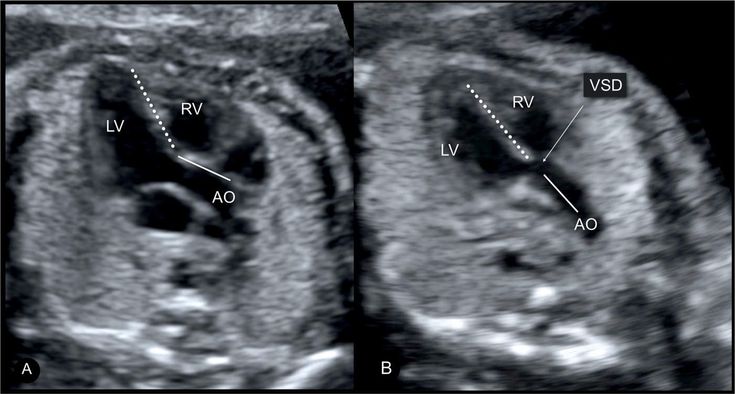 One day, these may also apply to the fetus. “While it’s hard to predict the future, we’re currently doing things we couldn’t have foreseen 10 years ago, so we’re very hopeful for continued advancements in fetal care,” says Baschat.
One day, these may also apply to the fetus. “While it’s hard to predict the future, we’re currently doing things we couldn’t have foreseen 10 years ago, so we’re very hopeful for continued advancements in fetal care,” says Baschat.
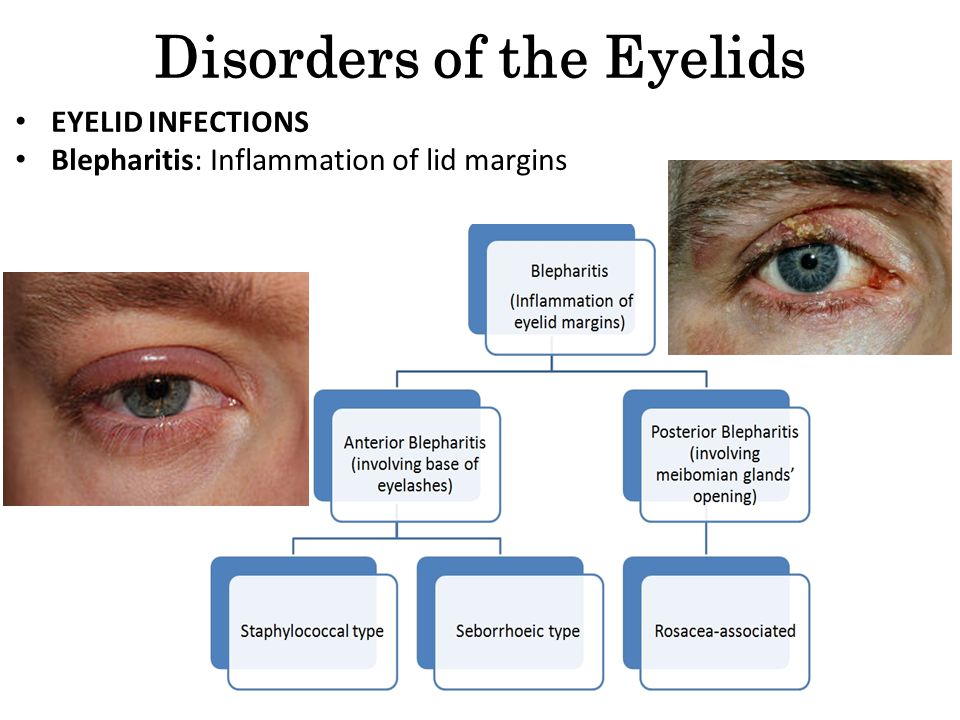
Fetal ultrasound reveals risk factors
Heart disease, despite all the achievements of modern medicine, remains one of the most common causes of infant mortality in the first year of life. According to statistics, the most common are defects of the interventricular septum, interatrial septum and patent ductus arteriosus.
Marina Bychkova, doctor of ultrasound diagnostics at the clinic "Mother and Child - IDK"
Predisposition to heart disease can be detected as early as the 3-8th week of fetal development. At this time, the formation of the cardiovascular system of the embryo takes place: the laying of partitions, heart chambers, main vessels. And not in all cases, bad heredity is to blame. Congenital heart defects can be promoted by viral diseases suffered by the expectant mother in the first three months of pregnancy.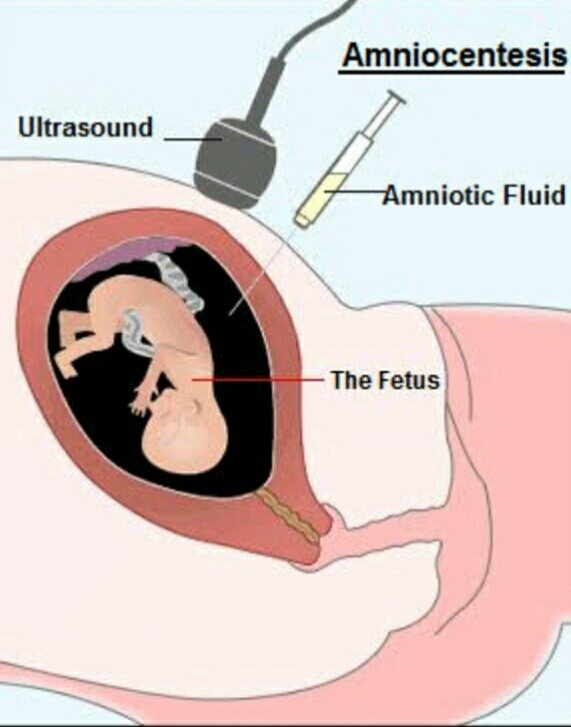 It has been scientifically proven that it is possible for influenza, ARVI and herpes simplex viruses to penetrate through the placenta that has not yet formed and their damaging effect on the baby's cardiovascular system.
It has been scientifically proven that it is possible for influenza, ARVI and herpes simplex viruses to penetrate through the placenta that has not yet formed and their damaging effect on the baby's cardiovascular system.
But many problems can be "seen" with the help of high-quality intrauterine diagnostics. About when and why it is needed, we were told by the doctor of ultrasound diagnostics of the clinic "Mother and Child - IDK" Marina Bychkova.
- Marina Vladimirovna, ultrasound did not exist before. Women have been carrying and giving birth to children for centuries without any diagnosis. Why do you need to do it during pregnancy?
- Since the early 1990s, diagnostic ultrasound has become an indispensable tool for obstetrician-gynecologists. Thanks to him, prenatal detection of congenital malformations increased, and maternal and infant mortality decreased. Ultrasound in obstetrics allows you to answer many questions that arise during pregnancy: is there a pregnancy, what is its duration, as well as to establish the number of fetuses, the presence of fetal developmental pathologies, including genetic ones, the location of the placenta and the baby in the uterus, the volume of amniotic fluid, etc. .
.
- There is a widespread opinion that ultrasound is not only not necessary, but also harmful to do, because. during the procedure, the fetus is "irradiated". What do you think about it?
- When conducting scientific research on the effect of ultrasound, no damaging and harmful effects on a woman and fetus were found. However, ultrasound is a physical phenomenon that, when passing through the tissues of the body, is converted into thermal and mechanical energy. In modern ultrasonic devices, these physical phenomena are so minimal that they do not have a biological effect. And yet, despite the fact that there is no evidence that ultrasound is harmful, doctors do not recommend doing it without appropriate indications. Especially in the first trimester of pregnancy, when all the organs of the baby are formed.
- How many times do you need to do an ultrasound during pregnancy?
- According to the recommendations of the World Health Organization, ultrasound diagnostics should be carried out at least three times: at 11-13.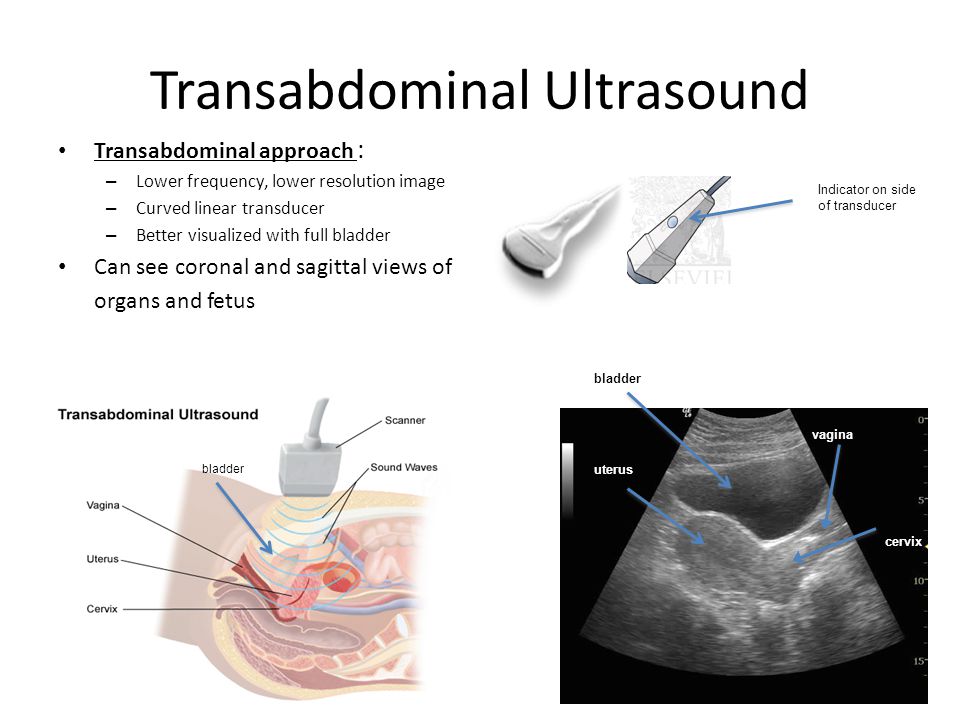 6 weeks, 18-22 and 30-34 weeks of pregnancy. In addition to mandatory ultrasound examinations, there are medical indications for urgent examinations at any time. But the decision on the need for additional research is made only by the attending physician.
6 weeks, 18-22 and 30-34 weeks of pregnancy. In addition to mandatory ultrasound examinations, there are medical indications for urgent examinations at any time. But the decision on the need for additional research is made only by the attending physician.
- From what gestational age can the sex of the baby be determined by ultrasound?
- The gender of the child is determined immediately after conception. But it can be established with 100% certainty only after 15-16 weeks of pregnancy. Until the 11th week of pregnancy, the genital tubercle is visualized in the embryo, which, under the action of hormones, is further formed into the female or male genital organs. It is possible to guess the sex of the unborn child from the 12th week of pregnancy, but the probability of error still remains high - up to 50%. Distinguishing a boy from a girl can be hindered by the position of the fetus, the amount of amniotic fluid, and even the thickness of the woman's abdominal wall. Although modern ultrasound in 3D format allows specialists to more accurately determine the sex of the fetus.
- From what period of pregnancy are pathologies of the child's development detected?
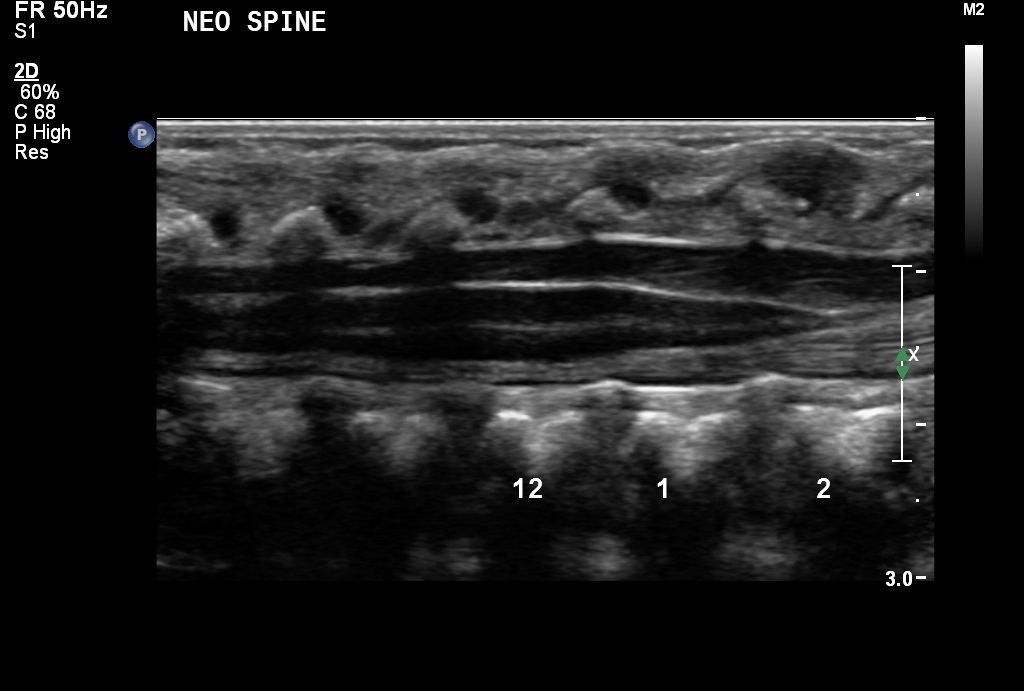
- Gross congenital malformations and chromosomal abnormalities are detected during the first ultrasound screening of pregnant women at 11-13 weeks of pregnancy. After the 18th week, with the help of ultrasound, most visible pathologies of the fetus can be detected. By this time, many internal organs and systems of the baby are already well formed. Diagnosis after 30 weeks is needed to identify late-appearing malformations in the fetus and delays in its development.
- What pathologies of fetal development can be detected on ultrasound?
- Ultrasound allows you to notice almost all deviations from the normal anatomical structure of the baby. The accuracy of diagnosis is about 95%, since there are defects that do not manifest themselves as changes in the anatomy or appear only after birth.
- What does intrauterine diagnosis of heart diseases give?
- First of all, it helps to correctly build the tactics of childbirth and provide specialized assistance to the baby immediately after birth. 97% of children born with heart defects who were operated on in the first months of life grow up absolutely healthy in the future: they study, work and go in for sports.
97% of children born with heart defects who were operated on in the first months of life grow up absolutely healthy in the future: they study, work and go in for sports.
- What should I do if a heart disease was detected in an ultrasound of a future baby?
- A pregnant woman is sent to a specialized institution of a cardiological profile. There, she will be registered and the child's diagnosis will be clarified. By the way, some forms of heart disease are amenable to surgical treatment even in utero. Others are operated on immediately after the baby is born. In any case, delivery should be carried out in the maternity ward of a cardiological hospital.
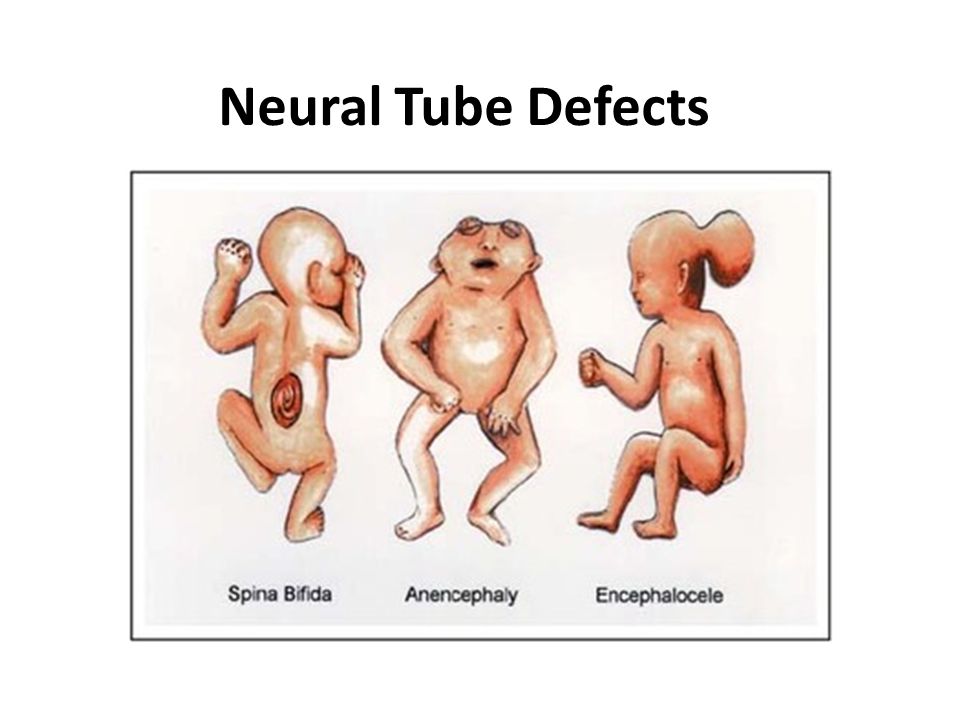
Diagnosis of congenital malformations of the fetus.
Diagnosis of congenital malformations of the fetus is included in the list of mandatory examinations conducted by a woman during pregnancy. And this is no coincidence, because intrauterine fetal malformations are one of the main causes of perinatal mortality and disability in children.
There can be many reasons for intrauterine development defects in a child. Pathology is sometimes hereditary, its causes can be negative external and internal factors. There is only one result - a terrible blow for the whole family, which not everyone manages to withstand with dignity, and this despite the fact that today in Russia 5 out of 100 children are born with similar problems.
What intrauterine fetal malformations can be detected already during pregnancy?
- Down syndrome or trisomy for the 21st pair of chromosomes, which subsequently leads to multiple malformations of internal organs and mental retardation.
- Edwards syndrome or trisomy for the 18th pair of chromosomes, characterized by malformations of many internal organs.
- Malformations of the neural tube, manifested by the absence of the brain (anencephaly), defects in the fusion of the spinal canal and the formation of a hernia of the spinal cord (spina bifida).
- Malformations of the heart and lungs.
- Malformations of limbs.
- Malformations of the facial part of the skull, e.g. cleft palate, cleft lip, etc.
Prenatal diagnosis of intrauterine malformations of a child is carried out in two main stages, including ultrasound and blood tests.
For the first time, a woman should visit an ultrasound room at 10-14 weeks of pregnancy, which allows you to confirm the presence of pregnancy; find out if the pregnancy is uterine or ectopic; determine the gestational age with an accuracy of 2-3 days; identify multiple pregnancies; exclude false pregnancy and pronounced anatomical abnormalities. And most importantly, there are signs of chromosomal anomalies of Down syndrome, which may not manifest themselves later, the definition of which largely depends on the qualifications of the doctor and the level of ultrasound equipment.
Blood test:
- b-hCG or free b-subunit of chorionic hormone.
- PAPP-A protein or pregnancy-associated plasma protein.
If deviations in the development of the fetus are detected, then at a period of 16-18 weeks of pregnancy, a triple biochemical test is performed, taking into account the results of the first screening and including:
- blood test for alpha-fetoprotein;
- blood test for free estriol;
- blood test for b-hCG.
Ultrasound examination at 20-24 weeks of gestation reveals the compliance of fetal development with the expected gestational age; diagnosis of fetal malformations; recommendations are given on the continuation of pregnancy (or its termination if severe anomalies in the development of the fetus are detected). In this period, all organs are fully formed, it is possible to assess their structure and, indirectly, function. Each organ of the fetus is examined in detail. When examining the head, the shape and thickness of the bones of the skull, the structure of the brain, its hemispheres, subcortical formations, the cerebellum and the ventricles of the brain are assessed. The structure of the facial skull and soft tissues of the face is analyzed. Vertebral defects (hernia and curvature, absence of vertebrae) are excluded. The shape and size of the chest, ribs, and shoulder blades are assessed. Examine the region of the anterior abdominal wall to exclude an umbilical hernia. Then the arms and legs of the unborn child are examined, assessing the movements in the joints, the length and thickness of the tubular bones. In this period of pregnancy, the heart of the fetus is especially carefully examined. At the same time, most serious heart defects are diagnosed, including those incompatible with life or requiring surgical treatment in the early stages after the birth of a child. Other internal organs of the fetus are being studied, which are already practically formed and available for research. These are the lungs, intestines, spleen, stomach, liver and gallbladder, kidneys and bladder. Again, chromosomal markers and the risk of chromosomal pathology are excluded.
The structure of the facial skull and soft tissues of the face is analyzed. Vertebral defects (hernia and curvature, absence of vertebrae) are excluded. The shape and size of the chest, ribs, and shoulder blades are assessed. Examine the region of the anterior abdominal wall to exclude an umbilical hernia. Then the arms and legs of the unborn child are examined, assessing the movements in the joints, the length and thickness of the tubular bones. In this period of pregnancy, the heart of the fetus is especially carefully examined. At the same time, most serious heart defects are diagnosed, including those incompatible with life or requiring surgical treatment in the early stages after the birth of a child. Other internal organs of the fetus are being studied, which are already practically formed and available for research. These are the lungs, intestines, spleen, stomach, liver and gallbladder, kidneys and bladder. Again, chromosomal markers and the risk of chromosomal pathology are excluded. An ultrasound examination of the placenta, umbilical cord, amniotic fluid is carried out, the features of the body, cervix and its appendages are evaluated.
An ultrasound examination of the placenta, umbilical cord, amniotic fluid is carried out, the features of the body, cervix and its appendages are evaluated.
Ultrasound at 30-34 weeks of gestation may reveal possible fetal growth retardation syndrome; to identify possible fetal pathologies that were not detected for one reason or another at earlier stages of pregnancy; determine the amount of amniotic fluid. The body parts of the fetus (head, chest, limbs) are measured to assess its height, weight and proportions. These measurements make it possible to exclude fetal growth retardation. By the 28th week, the cheeks of the fetus are rounded, the face becomes more formed, lips and nose are distinguishable. He can scratch his ear, fold his fists, yawn, make a grimace, smile.
In early pregnancy, uterine arterial blood flow is measured to identify pregnant women at high risk of preeclampsia in the second half of pregnancy and fetal growth retardation. This study also helps in the management of pregnant women with diabetes and vascular disorders.