P c o s medical terms
Polycystic ovary syndrome (PCOS) - Care at Mayo Clinic
Polycystic ovary syndrome (PCOS) care at Mayo Clinic
Your Mayo Clinic care team
Mayo Clinic's care team for PCOS includes specialists trained in female reproductive medicine (gynecologists), hormone disorders (endocrinologists) and infertility (reproductive endocrinologists).
Specialists in the division of Reproductive Endocrinology and Infertility are frequently involved in care. Every staff doctor in that division is board certified in obstetrics and gynecology as well as reproductive endocrinology and infertility. These reproductive and infertility specialists work frequently with other specialists in endocrinology, metabolism and nutrition.
Mayo Clinic also has registered dietitians and certified diabetes care and education specialists to help with weight loss or diabetes prevention and treatment.
Having all of this expertise in a single place, focused on you, means that you're not just getting one opinion. Your care is discussed among the team, appointments are scheduled in coordination, and highly specialized PCOS experts work together to determine what's best for you.
Advanced diagnosis and treatment
Mayo Clinic has comprehensive diagnostic testing to identify PCOS. The disorder requires lifelong management to avoid complications such as diabetes and cardiovascular disease. Mayo Clinic has the multispecialty expertise to treat all of your health concerns, including infertility.
Many Mayo Clinic doctors who treat PCOS are also active researchers. They are working to improve treatment of PCOS. When you seek care at Mayo Clinic, you have access to the expertise of these Mayo Clinic care providers and researchers.
Nationally recognized expertise
Mayo Clinic in Rochester, Minnesota, ranks among the Best Hospitals for gynecology in the U. S. News & World Report Best Hospitals rankings.
S. News & World Report Best Hospitals rankings.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.
Collaboration that changes lives
Elyn Simmons was 31 years old and eager to start a family with her husband, Guy. But in 2016, she was diagnosed with a hormonal disorder — PCOS, or polycystic ovary syndrome — that causes fertility problems. Then Elyn began experiencing other symptoms, including unexplained weight gain, increased body hair, migraines, and severe fatigue. Teamwork by Mayo Clinic clinicians and specialists in Mayo’s Department of Laboratory Medicine and Pathology found the source of Elyn's problem. In 2018, she was…
Expertise and rankings
- Experience. Mayo Clinic experts care for more than 2,100 women who have PCOS every year, using research-based treatments and teaching helpful lifestyle changes.

- Teamwork. Managing PCOS can require expertise in infertility, hirsutism, diabetes and cardiovascular care. Mayo Clinic experts work together closely to address all of your health concerns.
- Research. Mayo Clinic experts are continually studying how to improve the diagnosis and treatment of PCOS.
Learn more about Mayo Clinic's obstetrics and gynecology and endocrinology departments' expertise and rankings.
Locations, travel and lodging
Mayo Clinic has major campuses in Phoenix and Scottsdale, Arizona; Jacksonville, Florida; and Rochester, Minnesota. The Mayo Clinic Health System has dozens of locations in several states.
For more information on visiting Mayo Clinic, choose your location below:
Mayo Clinic's campus in Arizona
Mayo Clinic's campus in Florida
Mayo Clinic's campus in Minnesota
Mayo Clinic Health System
Costs and insurance
Mayo Clinic works with hundreds of insurance companies and is an in-network provider for millions of people.
In most cases, Mayo Clinic doesn't require a physician referral. Some insurers require referrals, or may have additional requirements for certain medical care. All appointments are prioritized on the basis of medical need.
Learn more about appointments at Mayo Clinic.
Please contact your insurance company to verify medical coverage and to obtain any needed authorization prior to your visit. Often, your insurer's customer service number is printed on the back of your insurance card.
More information about billing and insurance:
Mayo Clinic in Arizona, Florida and Minnesota
Mayo Clinic Health System
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Polycystic Ovary Syndrome (PCOS) | Johns Hopkins Medicine
Polycystic ovary syndrome (PCOS) is a condition in which the ovaries produce an abnormal amount of androgens, male sex hormones that are usually present in women in small amounts. The name polycystic ovary syndrome describes the numerous small cysts (fluid-filled sacs) that form in the ovaries. However, some women with this disorder do not have cysts, while some women without the disorder do develop cysts.
However, some women with this disorder do not have cysts, while some women without the disorder do develop cysts.
Ovulation occurs when a mature egg is released from an ovary. This happens so it can be fertilized by a male sperm. If the egg is not fertilized, it is sent out of the body during your period.
In some cases, a woman doesn’t make enough of the hormones needed to ovulate. When ovulation doesn’t happen, the ovaries can develop many small cysts. These cysts make hormones called androgens. Women with PCOS often have high levels of androgens. This can cause more problems with a woman’s menstrual cycle. And it can cause many of the symptoms of PCOS.
Treatment for PCOS is often done with medication. This can’t cure PCOS, but it helps reduce symptoms and prevent some health problems.
What causes PCOS?
The exact cause of PCOS is not clear. Many women with PCOS have insulin resistance. This means the body can't use insulin well. Insulin levels build up in the body and may cause higher androgen levels. Obesity can also increase insulin levels and make PCOS symptoms worse.
Obesity can also increase insulin levels and make PCOS symptoms worse.
PCOS may also run in families. It's common for sisters or a mother and daughter to have PCOS.
What are the risks for PCOS?
You may be more likely to have PCOS if your mother or sister has it. You may also be more likely to have it if you have insulin resistance or are obese.
What are the symptoms of PCOS?
The symptoms of PCOS may include:
-
Missed periods, irregular periods, or very light periods
-
Ovaries that are large or have many cysts
-
Excess body hair, including the chest, stomach, and back (hirsutism)
-
Weight gain, especially around the belly (abdomen)
-
Acne or oily skin
-
Male-pattern baldness or thinning hair
-
Infertility
-
Small pieces of excess skin on the neck or armpits (skin tags)
-
Dark or thick skin patches on the back of the neck, in the armpits, and under the breasts
How is PCOS diagnosed?
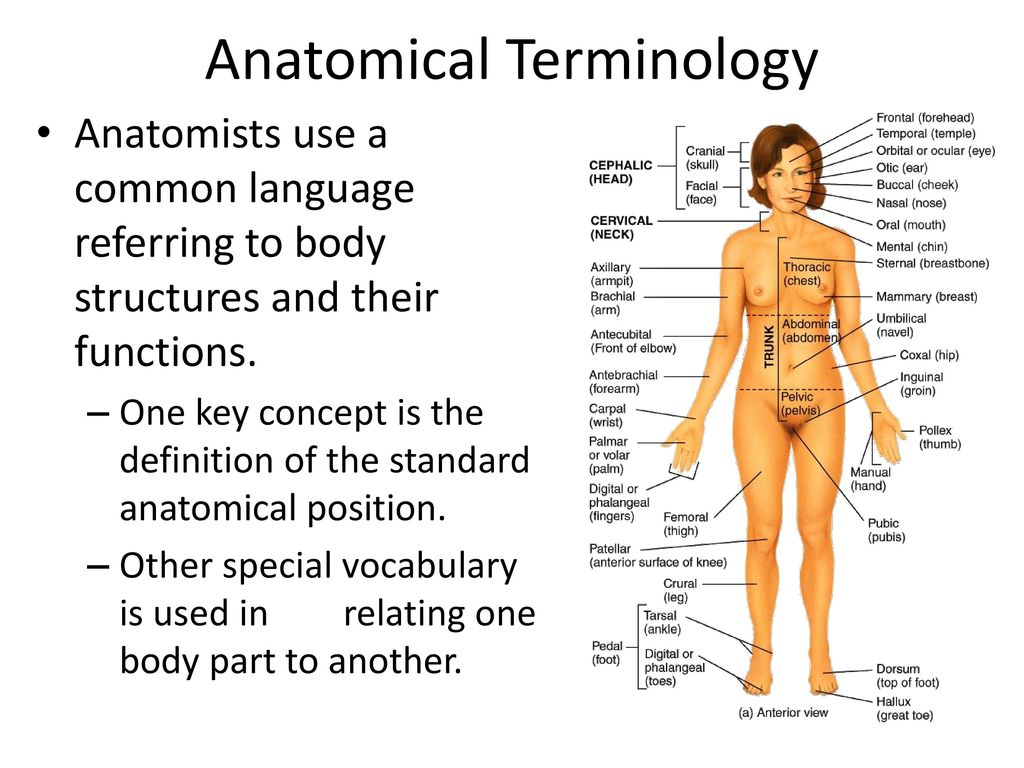
Your health care provider will ask about your medical history and your symptoms. You will also have a physical exam. This will likely include a pelvic exam. This exam checks the health of your reproductive organs, both inside and outside your body.
You will also have a physical exam. This will likely include a pelvic exam. This exam checks the health of your reproductive organs, both inside and outside your body.
Some of the symptoms of PCOS are like those caused by other health problems. Because of this, you may also have tests such as:
-
Ultrasound. This test uses sound waves and a computer to create images of blood vessels, tissues, and organs. This test is used to look at the size of the ovaries and see if they have cysts. The test can also look at the thickness of the lining of the uterus (endometrium).
-
Blood tests. These look for high levels of androgens and other hormones. Your health care provider may also check your blood glucose levels. And you may have your cholesterol and triglyceride levels checked.
How is PCOS treated?
Treatment for PCOS depends on a number of factors. These may include your age, how severe your symptoms are, and your overall health. The type of treatment may also depend on whether you want to become pregnant in the future.
The type of treatment may also depend on whether you want to become pregnant in the future.
If you do plan to become pregnant, your treatment may include:
-
A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
-
Medications to cause ovulation. Medications can help the ovaries to release eggs normally. These medications also have certain risks. They can increase the chance for a multiple birth (twins or more). And they can cause ovarian hyperstimulation. This is when the ovaries release too many hormones. It can cause symptoms such as abdominal bloating and pelvic pain.
If you do not plan to become pregnant, your treatment may include:
-
Birth control pills. These help to control menstrual cycles, lower androgen levels, and reduce acne.
-
Diabetes medication. This is often used to lower insulin resistance in PCOS. It may also help reduce androgen levels, slow hair growth, and help you ovulate more regularly.
-
A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
-
Medications to treat other symptoms. Some medications can help reduce hair growth or acne.
What are the complications of PCOS?
Women with PCOS are more likely to develop certain serious health problems. These include type 2 diabetes, high blood pressure, problems with the heart and blood vessels, and uterine cancer. Women with PCOS often have problems with their ability to get pregnant (fertility).
Living with PCOS
Some women struggle with the physical symptoms of PCOS, such as weight gain, hair growth, and acne.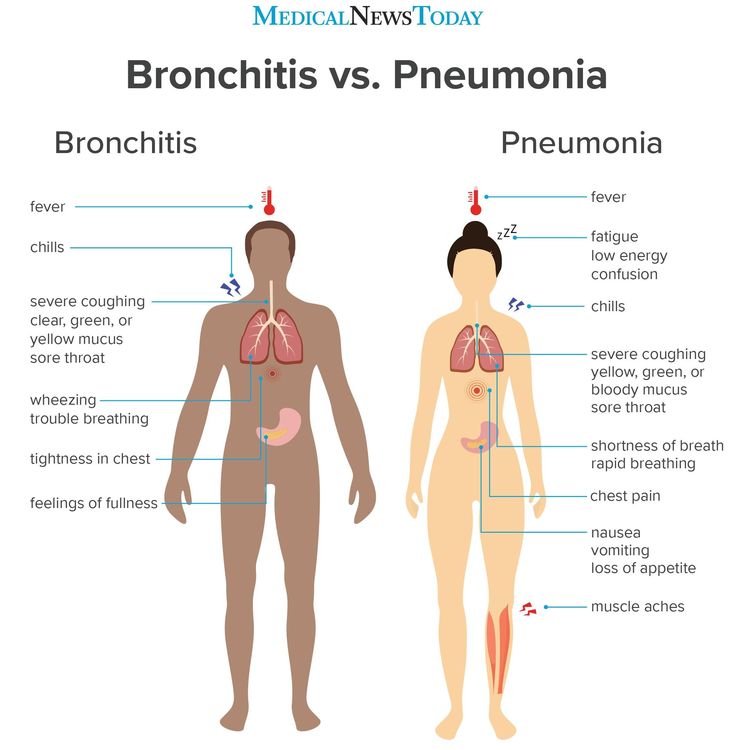 Cosmetic treatments, such as electrolysis and laser hair removal, may help you feel better about your appearance. Talk with your health care provider about the best ways to treat the symptoms that bother you.
Cosmetic treatments, such as electrolysis and laser hair removal, may help you feel better about your appearance. Talk with your health care provider about the best ways to treat the symptoms that bother you.
When should I seek medical care?
If you have missed or irregular periods, excess hair growth, acne, and weight gain, call your doctor for an evaluation.
Key points
-
PCOS is a very common hormone problem for women of childbearing age.
-
Women with PCOS may not ovulate, have high levels of androgens, and have many small cysts on the ovaries.
-
PCOS can cause missed or irregular menstrual periods, excess hair growth, acne, infertility, and weight gain.
-
Women with PCOS may be at higher risk for type 2 diabetes, high blood pressure, heart problems, and endometrial cancer.
-
The types of treatment for PCOS may depend on whether or not a woman plans to become pregnant.
 Women who plan to become pregnant in the future may take different kinds of medications.
Women who plan to become pregnant in the future may take different kinds of medications.
Next steps
Tips to help you get the most from a visit to your health care provider:
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.
Polycystic ovary syndrome
Kuznetsova Ekaterina Viktorovna
Reproductologist, Gynecologist
Novosibirsk Center for Reproductive Medicine
The criteria for the diagnosis of PCOS are:
- absence of ovulation (anovulation),
- hyperandrogenism,
- the presence of polycystic disease (multifollicular ovaries) with an increase in the volume of the ovaries according to ultrasound.
The diagnosis can be made if two of these three manifestations are present.
As a rule, the examination of a woman begins with an ultrasound examination of the pelvic organs. Often, if the conclusion indicates the presence of "multifollicular ovaries" (MFO), on this basis, the diagnosis of PCOS is erroneously established. The term "multifollicular ovaries" is simply a description of the ultrasound picture, which reflects the presence of a large number of antral follicles in the ovaries.
Such a conclusion, of course, is one of the criteria for PCOS, but, I remind you that not one symptom, but two, is required for a diagnosis. The presence of MFN by ultrasound performed at the beginning of the menstrual cycle does not make it possible to judge from the presence or absence of ovulation in a woman's menstrual cycles. The detection of a large number of follicles in the ovaries and by ultrasound is the norm for young women! With preserved ovulation, the absence of menstrual irregularities, this treatment does not require and does not prevent pregnancy!
To diagnose anovulation, it is necessary to perform ultrasonic folliculometry (FM), preferably within 2-3 menstrual cycles. Moreover, when performing FM, you need to decide on the period until which it makes sense to wait for the appearance of the dominant follicle. This is where mistakes often happen. The fact is that most women have a menstrual cycle of 28-30 days, while ovulation occurs on days 14-16 of the cycle.
Moreover, when performing FM, you need to decide on the period until which it makes sense to wait for the appearance of the dominant follicle. This is where mistakes often happen. The fact is that most women have a menstrual cycle of 28-30 days, while ovulation occurs on days 14-16 of the cycle.
But, if this is the case for the majority, should it be so for everyone? No. The normal length of a menstrual cycle is 21 to 42 days. This means that with a 21 day cycle, ovulation occurs on days 7–8 of the cycle, but with a 42 day cycle? On the 20th day? No. With a cycle duration of 42 days, ovulation should occur on days 26-30 of the cycle. Thus, when folliculometry is stopped on the 14th-16th day of the cycle due to the absence of a dominant follicle, an erroneous conclusion is made about anovulation. Although, with a regular, but long (32–42 days) menstrual cycle, ovulatory function can be preserved. Such a delusion is very dangerous, because it entails the start of stimulation therapy in women who are planning a pregnancy, although, in fact, they do not need it. Conversely, women who are not currently planning a pregnancy get the wrong impression that there is no need for contraception, which leads to unwanted pregnancies and, as a result, to abortion.
Conversely, women who are not currently planning a pregnancy get the wrong impression that there is no need for contraception, which leads to unwanted pregnancies and, as a result, to abortion.
The next symptom of PCOS is hyperandrogenism, which is an increase in the content of male hormones (androgens). This is a sufficient general statement. Characteristic of PCOS is an increase in testosterone, which is produced in excess in the ovaries. This can lead to appearances such as excessive hair growth on the skin of the abdomen, thighs and even the face (this is called hirsutism), as well as increased activity of the skin sebaceous glands, which is manifested by oily skin and a tendency to acne. But testosterone is not the only androgen in the body.
In addition, other male hormones are present in the body: androstenedione, DEHA, 17-OH progesterone, etc., which are produced mainly by the adrenal glands. Their determination is necessary during the examination in case of suspicion of PCOS, the presence of manifestations of hyperandrogenism, anovulation, but is not a sign of PCOS, since they are produced not in the ovary, but in the adrenal glands. So the determination of DHEA is necessary to exclude formations of the adrenal glands that produce hormones (hormone-producing tumors), the determination of 17-OH progesterone is performed to diagnose such a congenital disease as VDKN (formerly called adrenogenital syndrome - AGS), which can also lead to cycle disorders and anovulation, but, however, is not synonymous with PCOS and requires different treatment. With HCHD, there is at least a three-fold increase in the level of 17-OH progesterone, while a slight increase of 1-2 ng / ml or nmol / ml is neither a sign of HCHD nor PCOS, and, as a rule, is asymptomatic and does not require treatment.
So the determination of DHEA is necessary to exclude formations of the adrenal glands that produce hormones (hormone-producing tumors), the determination of 17-OH progesterone is performed to diagnose such a congenital disease as VDKN (formerly called adrenogenital syndrome - AGS), which can also lead to cycle disorders and anovulation, but, however, is not synonymous with PCOS and requires different treatment. With HCHD, there is at least a three-fold increase in the level of 17-OH progesterone, while a slight increase of 1-2 ng / ml or nmol / ml is neither a sign of HCHD nor PCOS, and, as a rule, is asymptomatic and does not require treatment.
Often, hormonal disorders in PCOS are accompanied by impaired insulin function (insulin resistance) and/or its excessive production (hyperinsulinemia). This leads to the fact that PCOS is accompanied by a complex of symptoms called metabolic syndrome (MS) and is manifested by obesity, arterial hypertension, high cholesterol and impaired glucose absorption.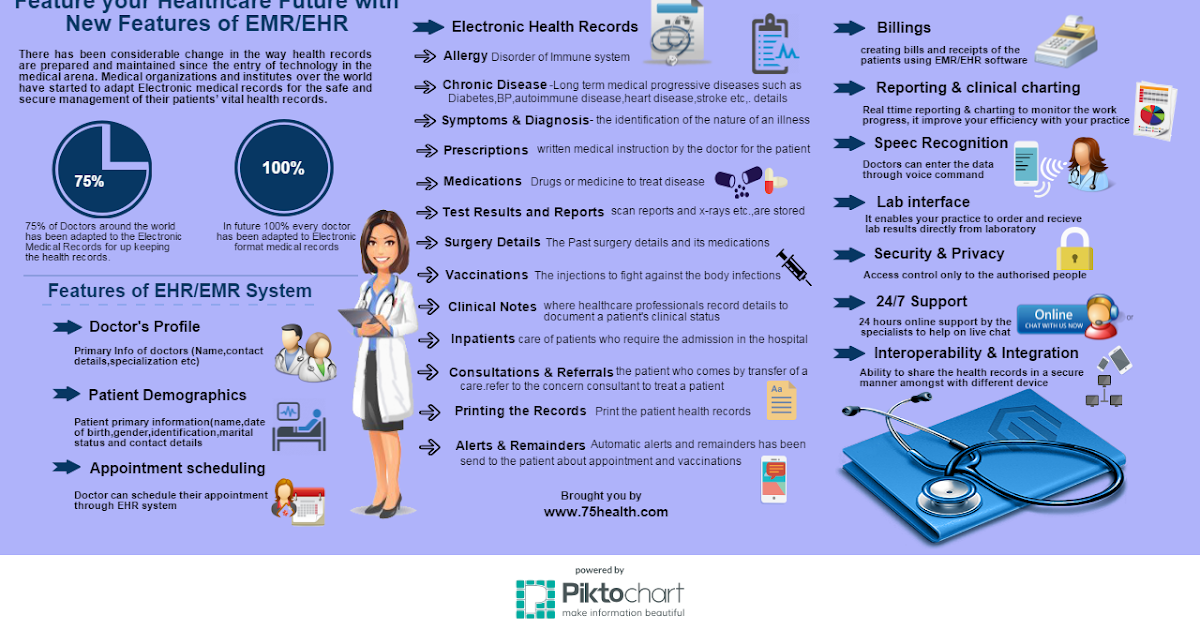 This manifestation of PCOS is dangerous with very serious consequences: if left untreated, type 2 diabetes mellitus, coronary heart disease, etc. develop over time, which is the main cause of death along with cancer. Insulin resistance, of course, requires medical correction with special drugs, but a woman herself can help the drugs work more efficiently. How? Weight loss, proper nutrition and regular physical activity. Agree, it is available to everyone.
This manifestation of PCOS is dangerous with very serious consequences: if left untreated, type 2 diabetes mellitus, coronary heart disease, etc. develop over time, which is the main cause of death along with cancer. Insulin resistance, of course, requires medical correction with special drugs, but a woman herself can help the drugs work more efficiently. How? Weight loss, proper nutrition and regular physical activity. Agree, it is available to everyone.
It's time to move on to treating PCOS.
Speaking about the treatment of this disease, it is important to answer the question: is a woman planning a pregnancy at the moment or not? So, if pregnancy is not planned in the near future, then combined oral contraceptives (COCs) are the best suited to normalize the cycle, prevent and treat endometrial hyperplasia, dysfunctional bleeding, and cosmetic problems. These drugs are quite effective, inexpensive and easy to take, which allows you to solve these problems.
On the topic "COC - to drink or not to drink?" many copies have been broken, but there is still no tool more effective, safer and easier to use. Like any other drug, COCs have both contraindications and side effects, so these drugs should be prescribed by a doctor who has experience working with them, after identifying possible contraindications to taking, for example, a tendency to thrombosis. There are a lot of drugs from this group on the market now, and their tolerance can be quite different. But I am convinced that among the existing variety it is possible to choose the right drug, it just does not always happen the first time, even if the appointment is made by a very experienced doctor. Unfortunately, in the medical literature, there is no unequivocal answer to the question of how long it is safe to take COCs. Based on my own experience, I can say that on average this is up to 5 years. I emphasize that this is an average value - in each individual case, this issue should be resolved individually.
Like any other drug, COCs have both contraindications and side effects, so these drugs should be prescribed by a doctor who has experience working with them, after identifying possible contraindications to taking, for example, a tendency to thrombosis. There are a lot of drugs from this group on the market now, and their tolerance can be quite different. But I am convinced that among the existing variety it is possible to choose the right drug, it just does not always happen the first time, even if the appointment is made by a very experienced doctor. Unfortunately, in the medical literature, there is no unequivocal answer to the question of how long it is safe to take COCs. Based on my own experience, I can say that on average this is up to 5 years. I emphasize that this is an average value - in each individual case, this issue should be resolved individually.
If a woman diagnosed with PCOS is planning a pregnancy, she needs to contact a reproductive specialist in a specialized clinic. Since for the onset of pregnancy it is necessary not only to make the menstrual cycle regular, but to establish the ovulatory function of the ovary, since without the release of the egg from the ovary, that is, ovulation, pregnancy is impossible. In such cases, ovulation induction is performed (stimulation of ovulation, stimulation of ovarian function) with the use of special preparations.
It is good if ovulation is stimulated by a reproductive specialist who knows ultrasound and can independently monitor the growth of follicles and prescribe appropriate drugs. Before using ovulation induction, it is necessary to perform a study of the patency of the fallopian tubes and a diagnosis of the state of the sperm in the husband/partner (spermogram, MAP test, strict morphology according to the Kruger criteria) and other examinations that are mandatory when planning a pregnancy. Since, unfortunately, the lack of ovulation may not be the only reason for the lack of a desired pregnancy.
Often, a replacement for ovulation stimulation is the appointment of progesterone preparations from days 16 to 25 of the cycle. However, this is not at all the case. The appointment of these drugs will help to even out the cycle, make it 28 days, may be an alternative to COCs for the prevention and treatment of endometrial hyperplasia, but will not help the onset of pregnancy. On the contrary, it's more likely to get in the way. The fact is that under the influence of these drugs, changes occur in the endometrium that are characteristic of the second phase of the cycle, that is, after ovulation has occurred, which allows you to get a menstrual-like reaction, but their effect does not extend to the ovary, does not allow you to establish ovulation. But, in the event that ovulation suddenly decides to occur (this happens, including with PCOS once a year or once every several years), then taking these drugs can desynchronize the development of the embryo and the preparation of the endometrium, and this is one of the necessary conditions for pregnancy .
Previously, to normalize the cycle and restore ovulation, the method of ovarian cauterization (“notches”, resection of the ovaries) was used, which was performed during laparoscopy. For a long time, this was almost the only means of restoring the functioning of the ovaries in the absence of special drugs, the wide availability of ultrasound and qualified reproductologists. But now this method is not the method of choice, since among its consequences there is often premature ovarian exhaustion, that is, the irreversible disappearance of the follicular apparatus.
These are very difficult situations when young women begin menopausal manifestations, and there are no own eggs left, and pregnancy planning becomes possible only with the use of donor oocytes. In addition, I want to note that ovarian biopsy during laparoscopy is also not a modern criterion for the diagnosis of PCOS and you will not find indications of its need in any modern manual on operative gynecology. Since, unfortunately, even a slight damage to the ovarian tissue can lead to irreversible consequences.
In conclusion, I want to say that although PCOS is a common pathology that leads to serious consequences, in the modern world there are many means to cope with it and realize the reproductive function. Take care of your health, contact qualified specialists and be happy!
Make an appointment
to the doctor - Kuznetsova Ekaterina Viktorovna
Novosibirsk Center for Reproductive Medicine
Posted at 2021-06-21 10:00 h
First, it should be clarified that the terms "polycystic ovary" and "polycystic ovary syndrome" (PCOS) are two different conditions.
What's the difference?
Polycystic ovaries can be seen on ultrasound. The ovaries are filled with a large number of partially matured follicles. This is the normal state of the female ovary.
Polycystic ovary syndrome is diagnosed in women with disorders in the metabolism of androgens and estrogen, and its cause is still not clear.
The synthesis of estrogen in the female body begins with the onset of puberty with the maturation of the first follicle. When ovulation occurs, the level of estrogen in the blood rises sharply, and this stimulates sexual activity. The female body also synthesizes male sex hormones - testosterone, DHEA, androstenedione. The disturbed balance between them leads to changes in the menstrual cycle, women may have too long or too short periods. In the ovaries, multiple small follicles are formed, from which the egg is not released and / or there is no ovulation. This, in turn, leads to fertility and reproductive health problems.
What are the symptoms?
Symptoms can range from reproductive to metabolic to psychological health. Few women have the same set of symptoms, and these can change at different stages of life and at different ages.
The most common and frequent symptoms indicating the need for a diagnosis are:
- irregular menstruation
- increased amount of hair on typical areas of the body - on the face, between the breasts, on the midline of the abdomen, back, thighs and fingers
- elevated levels of male hormone detected after blood test
- acne, hair loss, oily skin
- periods may be less frequent or more frequent due to less frequent or no ovulation
- 20 or more follicles present in 1 ovary on ultrasound
- mood swings - including anxiety and depression
- obesity
- sleep apnea
A woman may have irregular menstrual cycles and elevated androgens, indicating polycystic ovary syndrome, but her ovaries may not be polycystic. The differential diagnosis should also be made in cases where there are dysfunctions of the thyroid gland or pituitary gland, as well as in violations of the hypothalamic-pituitary axis.
How is PCOS diagnosed?
In order to diagnose polycystic ovary syndrome, a longer follow-up is needed, during which a woman's ovulation, cycle duration, and hormone changes in different phases are monitored.
- Gynecological examination with transvaginal ultrasonography - the doctor palpates the reproductive organs for the presence of neoplasms or abnormalities. The thickness of the mucous membrane of the uterus is established, as well as the structure of the ovaries.
- Blood tests are carried out - Androgens, which we have listed above, as well as female sex hormones and their ratio in different phases of the monthly cycle, are being studied.
A glucose tolerance test is also done, as insulin resistance is common in CJD.When diagnosing PCOS, the attending physician may recommend regular monitoring of blood glucose, cholesterol and triglycerides.
How is polycystic ovary syndrome treated?
Lifestyle changes:
Insulin resistance often leads to obesity and sometimes overweight. It has been shown that a weight loss of as little as 5% can lead to a significant reduction in insulin resistance and improved ovarian function.
The diet should be balanced and include enough fruits and vegetables, whole grains, brown rice, clean meats and fish.
Caffeine intake should be limited because caffeine reduces levels of the substance myoinositol (a form of vitamin B8), which is essential for good ovarian function.
Smoking is strictly prohibited in patients with PCOS. We all know that women are especially fond of chocolate and confectionery, but with proven polycystic ovary syndrome, it is useful to keep sugar intake to a minimum in order to maintain normal insulin levels. Type 2 diabetes medications are sometimes recommended, such as Metformin, which lowers insulin and blood sugar levels in women with PCOS, thereby delaying ovarian function.
Treatment
Polycystic ovary syndrome (JRCN):In some cases inclusion HORMONAL THERAPY - especially in cases of infertility and reproductive problems. Therapy is also necessary for pronounced external signs of PCOS - hair loss, increased hair growth, through the use of drugs that block the action of testosterone or suppress the production of other androgens.
Most women can successfully complete a short course of treatment over several monthly cycles. Progesterone preparations are recommended to induce regular periods, which reduces the long-term risk of endometrial cancer associated with the absence of periods.
Other hormonal methods of contraception and treatment are intrauterine systems (IUDs), or so-called coils. They maintain normal mucosal thickness but cannot induce menstruation.