Fetus with spina bifida
Myelomeningocele (Spina Bifida) Fetal Repair
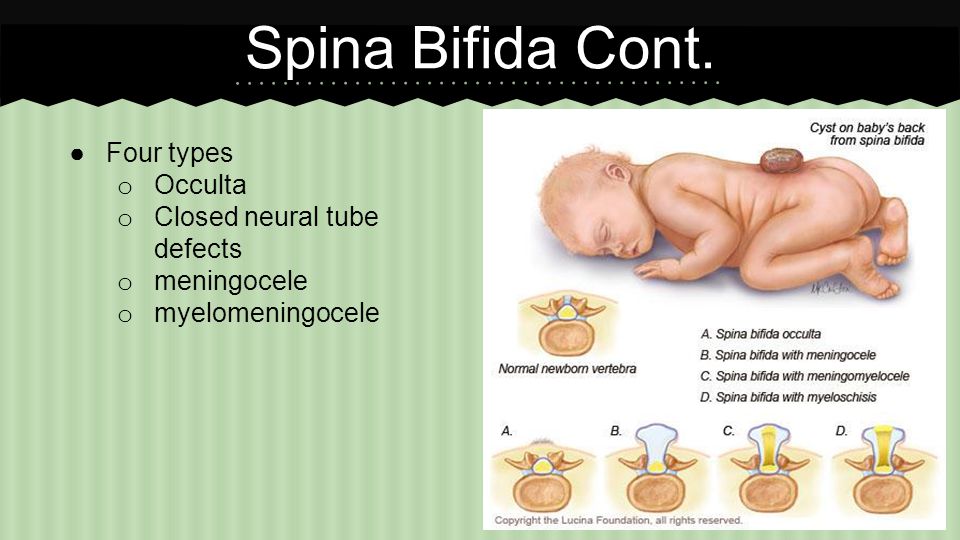
What is Spina Bifida?
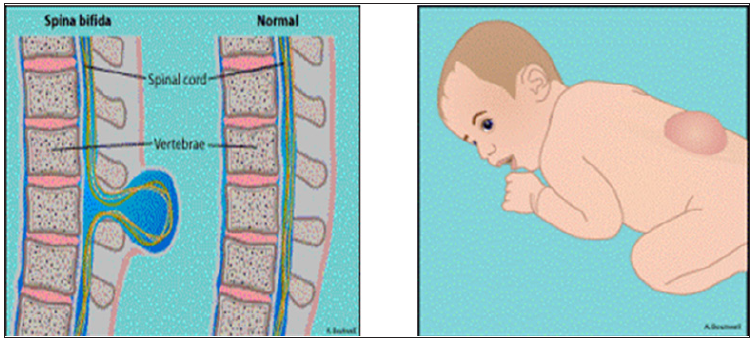
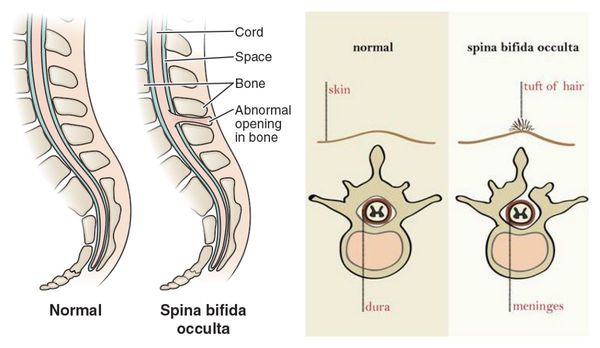
Spina bifida is a birth defect that occurs when the bones in a baby’s spine do not fully form during early pregnancy. This results in an opening on the back, usually in the mid- to lower back.
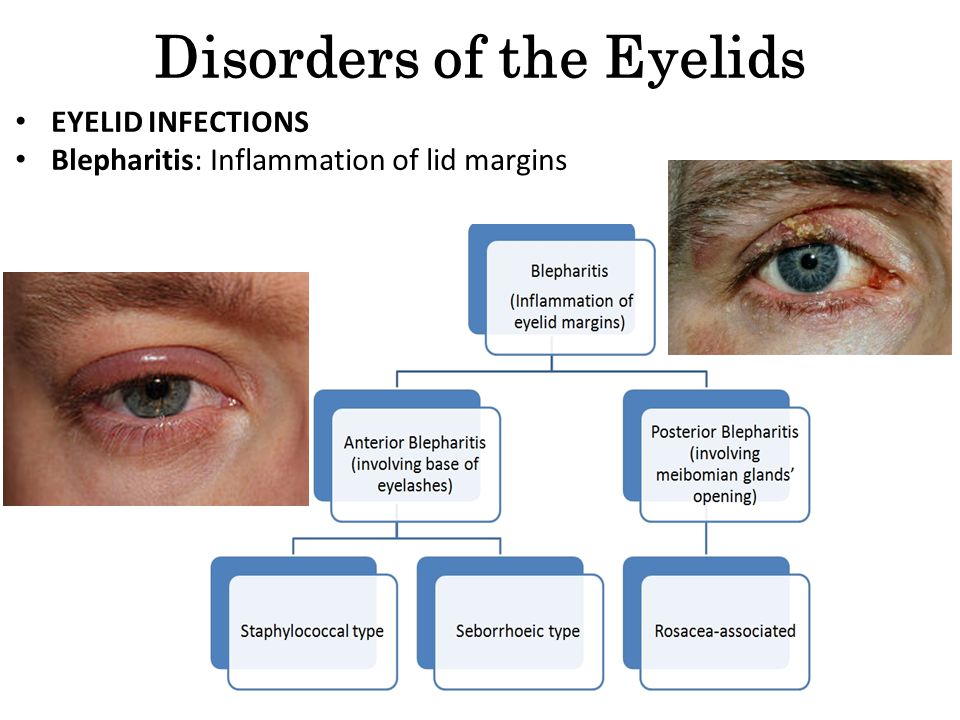
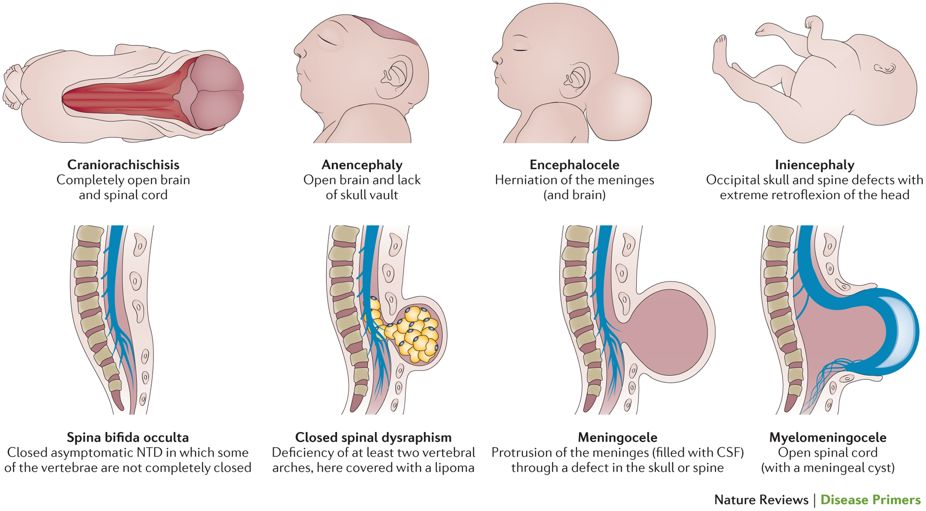
Types of Spina Bifida
Spina bifida can be mild to severe. The mildest form, called spina bifida occulta, usually does not cause health problems.
The more severe types of spina bifida include myelomeningoceles, meningoceles, lipomyelomeningoceles and other less common lesions.
- Myelomeningocele, a type of “open spina bifida,” is the most serious form of the disease. In myelomeningocele, a portion of the baby’s spinal cord and surrounding nerves protrude through an opening in the spine into an exposed, flat disc or sac that is visible on the back. This exposes the baby’s spinal cord to the amniotic fluid in the mother’s womb and can be harmful to the baby’s fetal development.
Myelomeningocele is the only type of spina bifida that exposes the baby’s spinal cord to amniotic fluid.
- Meningocele occurs when the spinal cord and nerve tissue do not protrude into the sac. In this case, the lesion is usually covered by skin.
- A lipomyelomeningocele is a type of spina bifida in which the spinal cord in the sac is covered by fat and skin.
Children who are born with myelomeningocele can experience serious health problems, such as hydrocephalus (an excessive accumulation of fluid in the brain) and paralysis. The severity of paralysis depends on where the opening occurs in the spine.
What Causes Myelomeningocele?
The cause of spina bifida is unknown, although some research suggests that genes, maternal diabetes, certain medications and nutrition may play a role. Spina bifida occurs in about three to four babies per 10,000 live births.
MOMS Myelomeningocele Study
Some babies who are diagnosed with myelomeningocele during pregnancy may undergo prenatal myelomeningocele surgery to repair the spinal defect.
In fact, results from a seven-year clinical research study called “Management of Myelomeningocele Study (MOMS)” showed that babies who received prenatal repair of myelomeningocele can significantly benefit. The study, published in 2011, compared the effects of fetal surgery vs. surgical repair after birth. It followed 183 women and found that if a baby is operated on while still in the womb, some serious complications of myelomeningocele can be lessened.
MOMS showed that babies who had fetal surgery for myelomeningocele are less likely to suffer from hydrocephalus, a fluid collection in the brain. Babies who are born with hydrocephalus usually need ventriculoperitoneal (VP) shunting, which involves surgically implanting a thin, hollow tube with a valve underneath the skin, behind the ear, that drains excess fluid from the brain into the belly or chest area.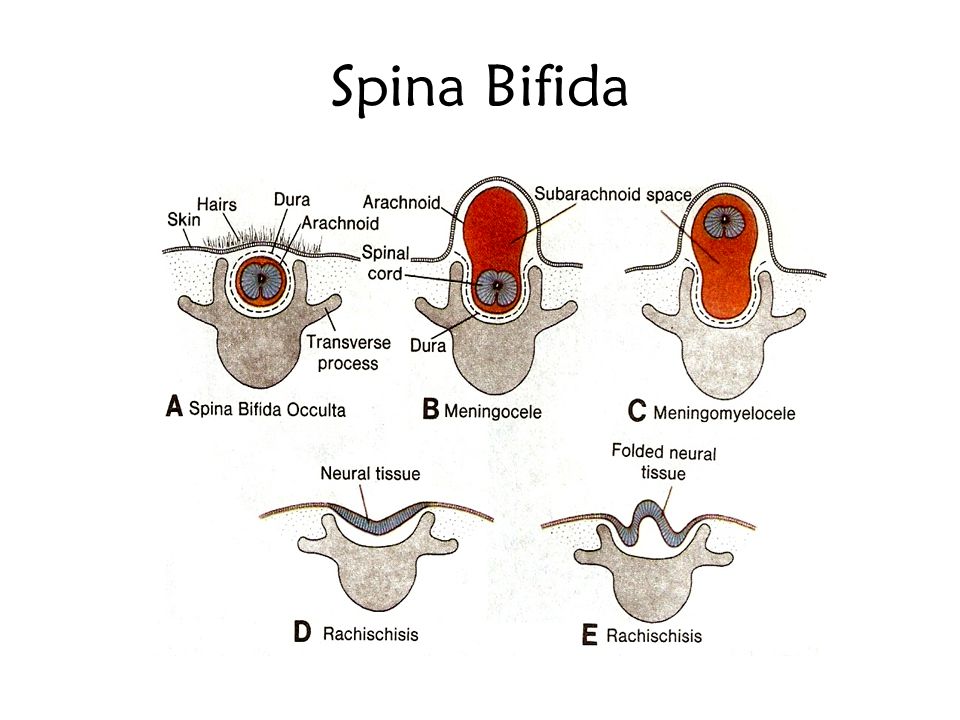 In MOMS, 40 percent of babies who had fetal surgery for myelomeningocele needed a VP shunt, while 82 percent of babies who had surgery after they were born needed a VP shunt.
In MOMS, 40 percent of babies who had fetal surgery for myelomeningocele needed a VP shunt, while 82 percent of babies who had surgery after they were born needed a VP shunt.
Another finding in the study is that 42 percent of the children who had fetal surgery were able to walk without crutches by age 2½. Only 21 percent of babies who had surgery after birth were able to walk unassisted at that age.
However, all this potential benefit comes at a cost that only the mothers can bear. She must go through extensive surgery, which requires Cesarean deliveries for future pregnancies and a risk for uterine rupture during the current pregnancy. This needs to be discussed with your doctors.
These and other results of MOMS are promising, and physicians are cautiously optimistic. Follow-up studies are under way to assess the long-term effect of prenatal myelomeningocele repair vs. surgery after birth.
Myelomeningocele Diagnosis & Treatment
Myelomeningocele typically is detected through routine ultrasound during the 18th to 22nd week of pregnancy. A preliminary diagnosis can be made as early as 16 weeks through a blood test that screens for maternal alpha-fetoprotein (AFP). Elevated AFP levels can suggest the presence of a neural tube defect. In this case, patients may undergo an amniocentesis or ultrasound to confirm the diagnosis.
A preliminary diagnosis can be made as early as 16 weeks through a blood test that screens for maternal alpha-fetoprotein (AFP). Elevated AFP levels can suggest the presence of a neural tube defect. In this case, patients may undergo an amniocentesis or ultrasound to confirm the diagnosis.
Patients referred to the Cincinnati Children's Fetal Care Center with a diagnosis of fetal myelomeningocele can be seen within a few days of their initial call to the center. We offer a two-day assessment that may include another ultrasound and MRI to confirm the diagnosis and provide additional anatomic detail about the myelomeningocele and the brain. At the end of the second day, patients meet with specialists at the center to discuss the diagnostic findings, treatment options and long-term prognosis. Whether patients can return home after the surgery or need to stay in Cincinnati is also discussed.
Our team includes maternal-fetal medicine specialists, fetal surgeons, pediatric neurosurgeons, neonatologists, genetic counselors, developmental pediatricians and social workers.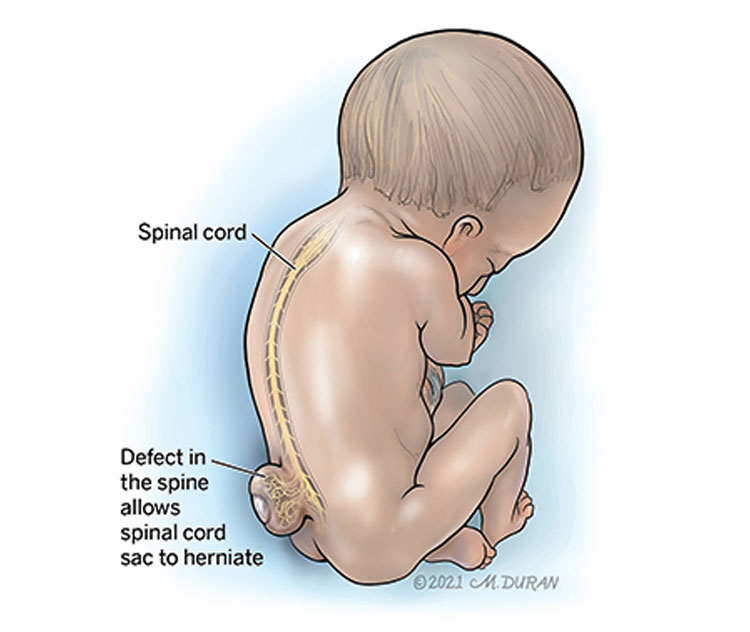 Referring physicians are welcome to participate in team meetings via video teleconferencing.
Referring physicians are welcome to participate in team meetings via video teleconferencing.
Our team works with each family to determine whether fetal surgery is a possible solution. Fetal surgery for myelomeningocele can offer significant benefits to the baby, but it also carries serious risks and potential complications. Our team provides extensive testing and counseling to ensure that patients meet the criteria for fetal myelomeningocele surgery and have all the information they need to make an informed decision about whether to undergo the procedure. Our surgeons have considerable experience in performing this delicate operation. Patients also benefit from exceptional follow-up care before and after the baby is born.
Who Is Eligible for Fetal Surgery?
MOMS provides specific guidelines about who is a good candidate for fetal surgery and who is not. The Fetal Care Center follows these guidelines closely.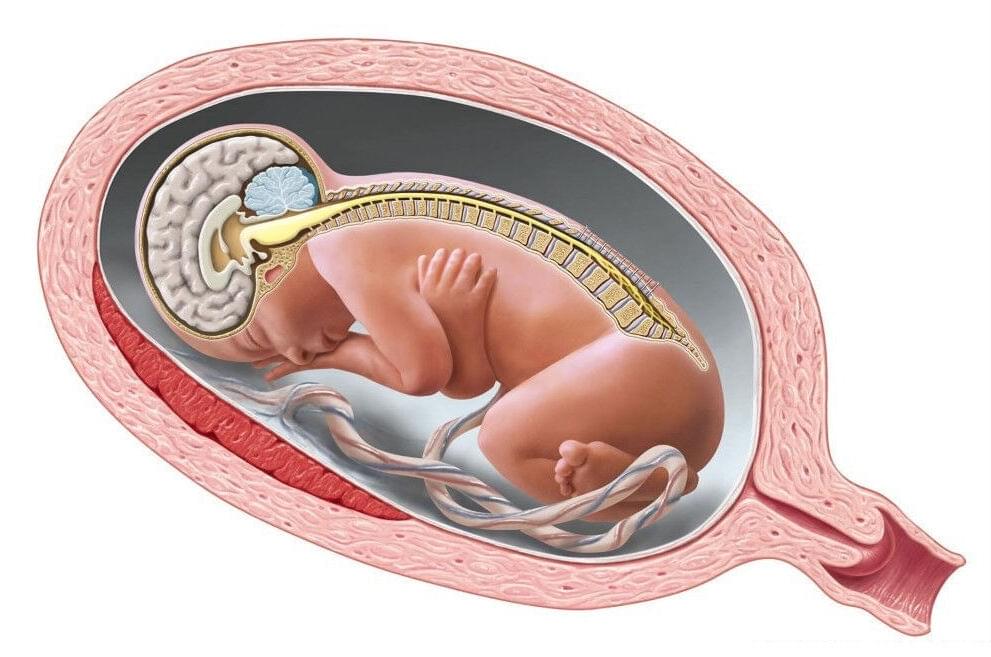 A full list of criteria can be found here.
A full list of criteria can be found here.
A partial list includes:
Patients may be eligible for surgery if they meet the following criteria:
- Maternal age of 18 years or older
- Gestational age of between 19 and 26 weeks at the time of surgery
- Normal fetal echocardiogram
- Singleton pregnancy (one baby)
Patients are not considered good candidates if the:
- Baby is experiencing significant medical problems not related to myelomeningocele
- Mother has medical issues that prevent abdominal surgery or general anesthesia
- Mother has HIV, active hepatitis B or hepatitis C (since surgery could lead to these conditions being passed along to her baby)
Prior to a patient’s first visit, we ask a number of questions by phone to ensure that she meets preliminary criteria for fetal surgery to repair myelomeningocele. An extensive screening takes place during the patient visit to the Fetal Care Center.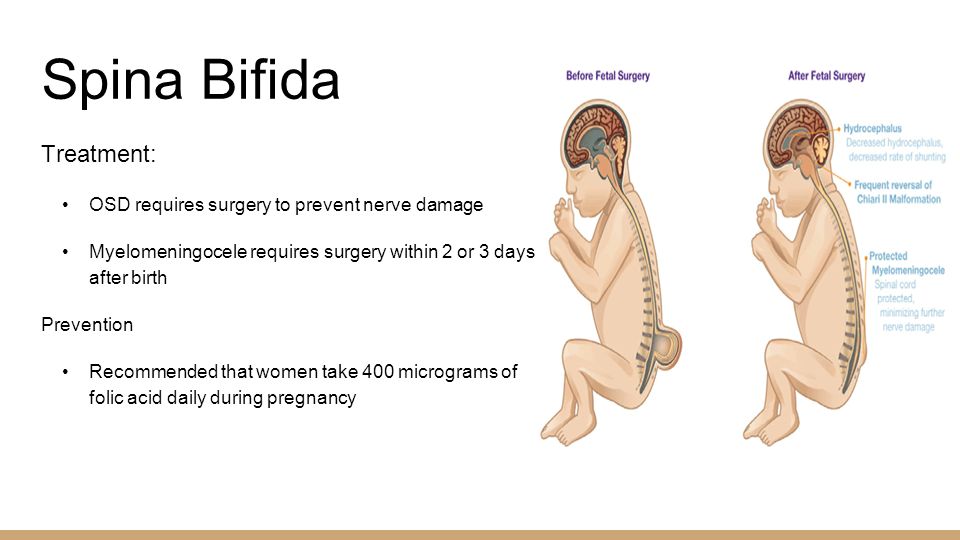
What Does Prenatal Repair Involve?
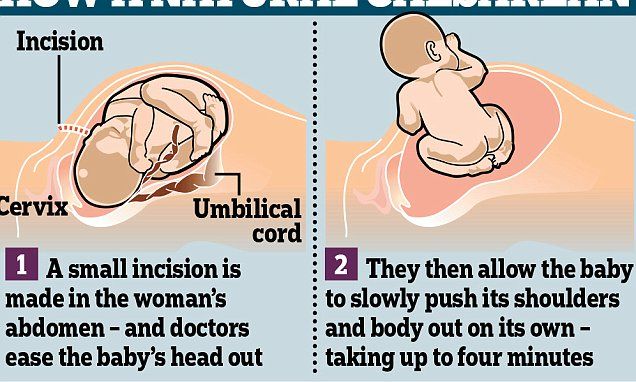
Open fetal surgery for myelomeningocele takes place after the 19th week of pregnancy and before the 27th week of pregnancy begins. During surgery, the doctor makes an incision across the mother’s abdomen and opens the uterus. The neurosurgeon removes the myelomeningocele sac, if one is present, and repairs the spinal defect in layers before closing the skin to protect the spinal cord from exposure to amniotic fluid. After the procedure, the uterus and abdomen are closed.
Patients recover in the hospital for four to five days. Weekly follow-up appointments and ultrasound tests take place to monitor the mother’s and baby’s condition.
Women who undergo fetal surgery deliver by a scheduled Cesarean section around 37 weeks gestation (earlier if labor begins before the scheduled date). This is done to prevent any stretching or tearing of the scar that was left on the uterus from the fetal surgery.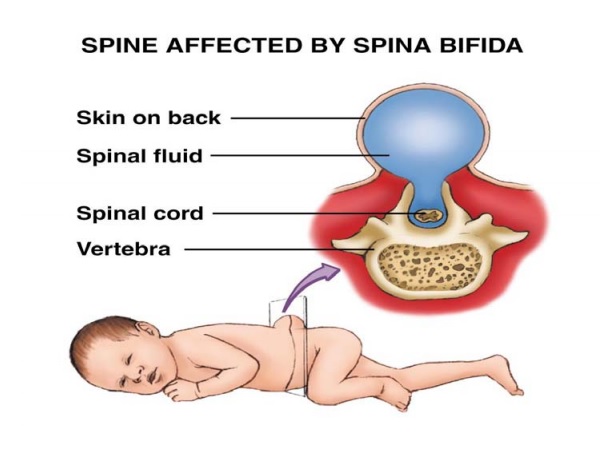
When patients are not eligible for fetal surgery or decide against it, surgical repair takes place after the baby is born. This involves operating on the baby within a few days after birth to close the opening in the spine to prevent infection and prevent further injury to the spinal cord and nerves.
However, it cannot correct the defects in the spinal cord and nerves. Babies who are born with hydrocephalus may need a shunt to help drain the excess fluid from the brain. Shunt placement surgery may take place within the first few weeks after the baby’s birth.
Associated Conditions
Other issues that occasionally can develop in children born with a myelomeningocele include trouble breathing or swallowing. This is called the Chiari II malformation, and it occurs when the myelomeningocele affects a part of the brain called the brainstem.
Learning disabilities, trouble with hand-eye coordination, scoliosis, sexual dysfunction and a number of other problems may develop or become noticeable as the child gets older.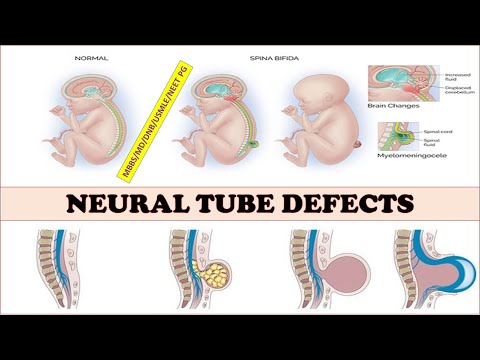
What Is the Outlook after Fetal Surgery?
How well a child with myelomeningocele does after fetal surgical repair depends on many factors. Some children will require minimal ongoing care, while others will require medical and educational support for many years.
The Center for Spina Bifida Care at Cincinnati Children’s Hospital Medical Center provides comprehensive, interdisciplinary and family-centered medical care to infants, children and adolescents living with repaired myelomeningoceles and other neural tube defects. In addition to excellence in medical service and care coordination, the center is committed to becoming a leader in spina bifida education and research.
Myelomeningocele Volume & Outcomes
- Total number of evaluations: 474
- Prenatal MMC repairs: 124
- Fetoscopic Prenatal MMC Repairs (2016+): 66
- Fetoscopic Prenatal MMC Repairs Delivering Vaginally (2016+): 41%
* Data based on patients cared for by the Cincinnati Children's Fetal Care Center from Feb.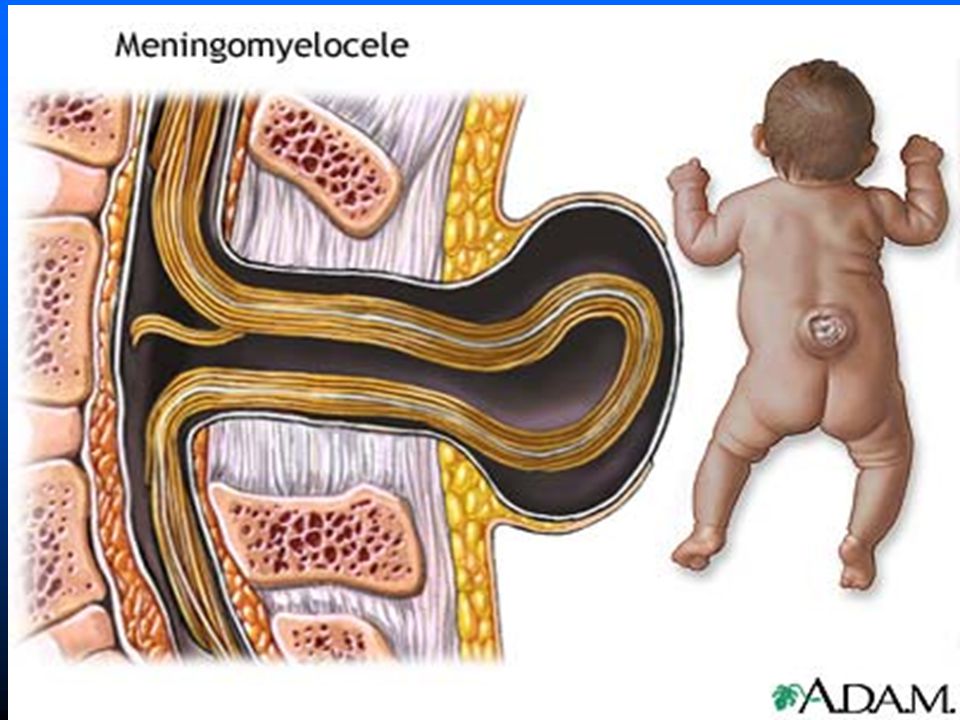 1, 2004, through June 30, 2022.
1, 2004, through June 30, 2022.
For More Information
For more information or to request an appointment, contact the Cincinnati Children's Fetal Care Center at 1-888-338-2559 or use our online form.
Fetoscopic Repair of Spina Bifida
Open Repair of Spina Bifida
View larger
Your baby has just been diagnosed with spina bifida. Here is some basic information about the condition. Read more on our blog
Spina Bifida (Myelomeningocele)
What is Spina Bifida (Myelomeningocele)?
Spina bifida is a congenital defect consisting of an opening in the spinal column.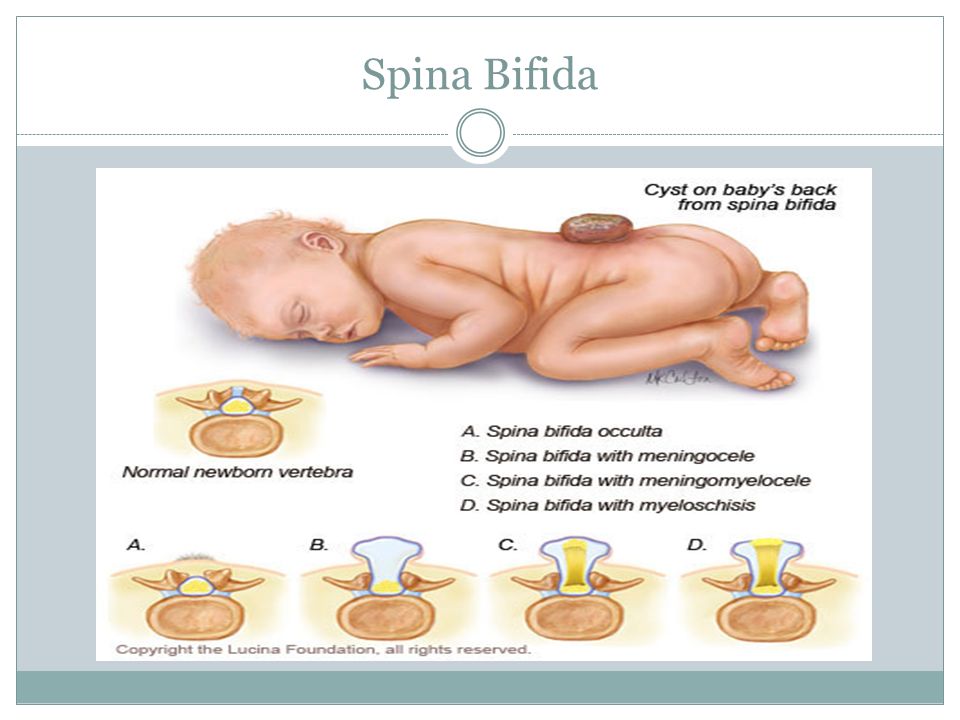 The most severe form is called myelomeningocele. Most children with this birth defect survive, but they can be left with many disabilities, including paralysis, difficulty with bowel and bladder control, a Chiari II malformation, hydrocephalus (excessive fluid in the brain), and developmental delay. In general, the higher the spinal opening occurs on the back, the greater the physical impairment.
The most severe form is called myelomeningocele. Most children with this birth defect survive, but they can be left with many disabilities, including paralysis, difficulty with bowel and bladder control, a Chiari II malformation, hydrocephalus (excessive fluid in the brain), and developmental delay. In general, the higher the spinal opening occurs on the back, the greater the physical impairment.
Treatment for Myelomeningocele
Infants with myelomeningocele have always had surgery shortly after birth to protect the spinal cord by closing the normal tissues of the back. Very often, a ventriculoperitoneal (VP) shunt was also placed to treat hydrocephalus. Due to the success of the MOMS Study, fetal surgery is now considered to be a treatment option for some cases of myelomeningocele.
Download our handout on Fetal Surgical Repair of Myelomeningocele PDF
Fetal Surgery for Myelomeningocele
Prenatal repair of myelomeningocele involves a fetal surgery handled by a multidisciplinary team of experts.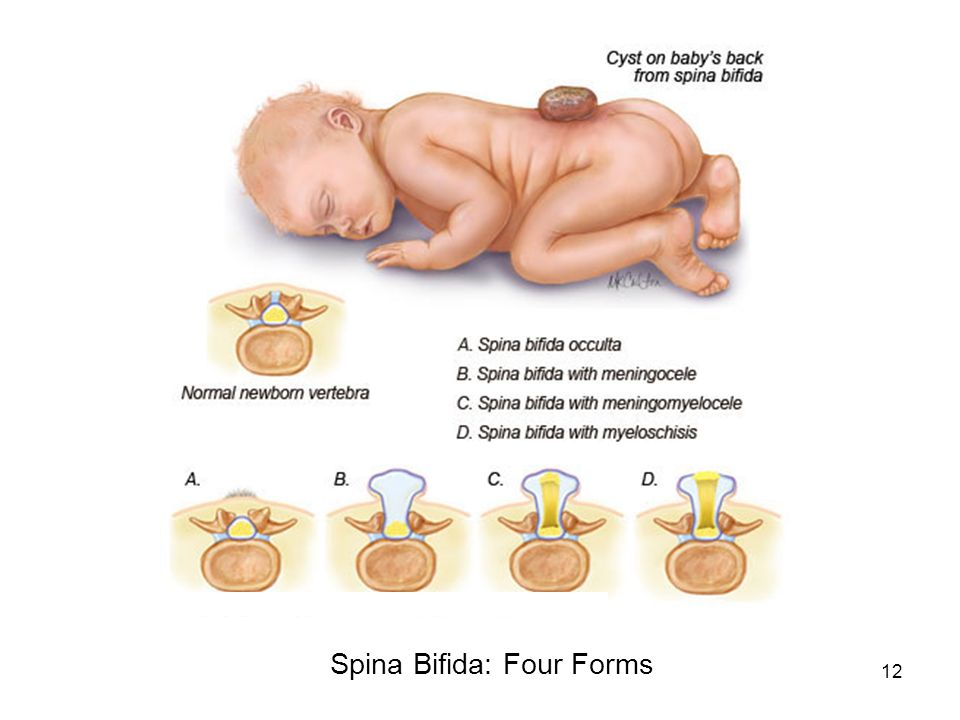 The procedure is much like a cesarean section however the fetus is not removed and the umbilical cord is not touched. An incision is made in the mother’s abdomen and uterus just large enough for the spinal defect to be operated upon. The neural tube and other layers of the back are surgically closed by the neurosurgeon. After the procedure, the incisions in the mother are closed.
The procedure is much like a cesarean section however the fetus is not removed and the umbilical cord is not touched. An incision is made in the mother’s abdomen and uterus just large enough for the spinal defect to be operated upon. The neural tube and other layers of the back are surgically closed by the neurosurgeon. After the procedure, the incisions in the mother are closed.
Recovery From Your Operation
After the procedure, patients will remain in the hospital for 4–5 days for recovery. They are cared for by skilled nurses with years of experience in fetal surgical care and the fetus will be monitored via ultrasound. Upon hospital discharge the mother is required to stay locally for at least 2-3 weeks. Travel home is determined by the mother's condition and the availability of medical services.
Evaluation and Counseling
Components of UCSF Evaluation
- Level II anatomic survey for fetal anomalies
- Fetal echocardiagraphy both for the structural integrity and functional pathology
- Fetal brain MRI and spine for presence and severity of the Chiari II Malformation
- Consultations with our multidisciplinary team including anesthesia, fetal surgery, neurosurgery, nursing, perinatology, and social work
Guidelines For Fetal Surgery
Fetal surgery can be a treatment option for spina bifida.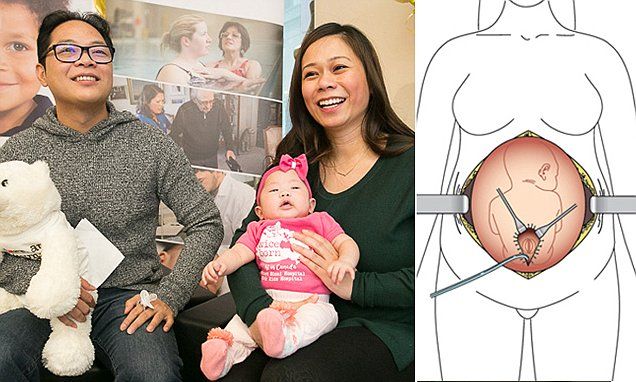 We have developed the following guidelines to determine fetal surgery candidates.
We have developed the following guidelines to determine fetal surgery candidates.
Inclusion Guidelines
- Myelomeningocele defect must start between T1-S1 (may extend below S1)
- Chiari II malformation diagnosed by MRI
- Normal fetal karyotype (amniocentesis)
- Gestational age at referral between 19 to 26 weeks
Exclusion Guidelines
- Multifetal pregnancy (twins, triplets, etc)
- Maternal contraindications to surgery or anesthesia
- Body Mass Index > 35
- Kyphosis (curve in the spine) in the fetus ≥ 30º
- Other fetal problem not related to the spina bifida
- Current or planned cerclage or documented history of incompetent cervix
- Short cervix (> 20 mm)
- Preterm labor in the current pregnancy
- Placenta previa or placental abruption
- Maternal-fetal isoimmuization
- Uterine abnormality
- Inability to comply with travel or follow-up requirements
How to Make an Appointment or Referral
Patients who wish to consider fetal surgery at UCSF for the treatment of spina bifida, and providers making a referral please use our online appointment form or call us at 1-800-RX-FETUS.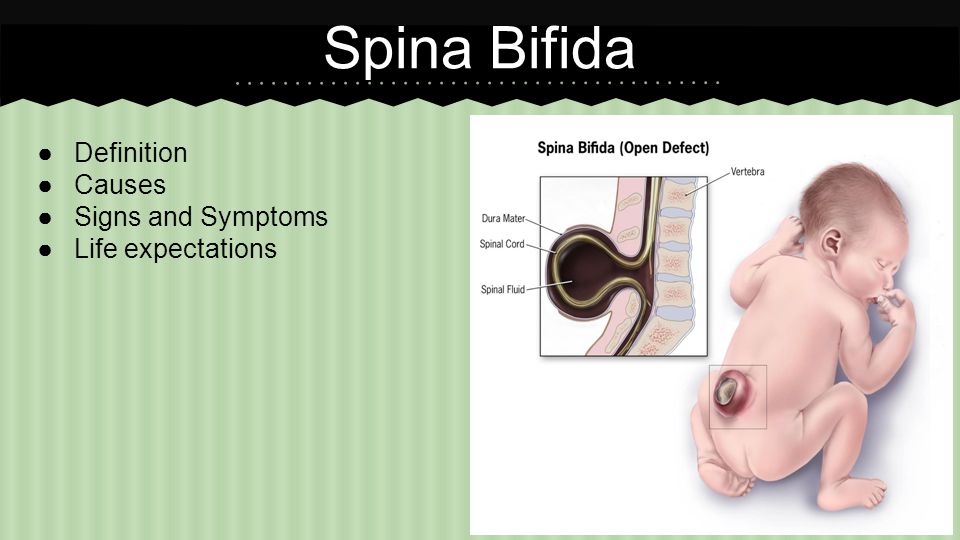 Also please have the following information faxed to 415-502-0660:
Also please have the following information faxed to 415-502-0660:
Name, home address, phone, email, date of birth
Copy of the front/back of their health insurance card
All OB/Perinatal medical records
If insurance authorization is required, please download the Spina Bifida Fetal Surgery FTC Codes.
Spina bifida | Hospital Sant Joan de Déu Barcelona
Diseases and treatments
Contact us
Call us +34 93 600 97 83
her treatment.
Description of pathology
What is spina bifida?
Spina bifida (myelomeningocele) is a congenital malformation in which the skin and bone in a certain area of the spine have not formed correctly, and part of the spinal cord that is normally protected by the spine is left exposed. Therefore Throughout pregnancy, the spinal cord is exposed to amniotic fluid, resulting in damage to the cord and deterioration of its function even before birth.
The spinal cord contains nerves that carry information from our brain to the rest of the body, so at birth symptoms such as reduced leg movement, loss of sensation and problems with urinary or stool retention appear.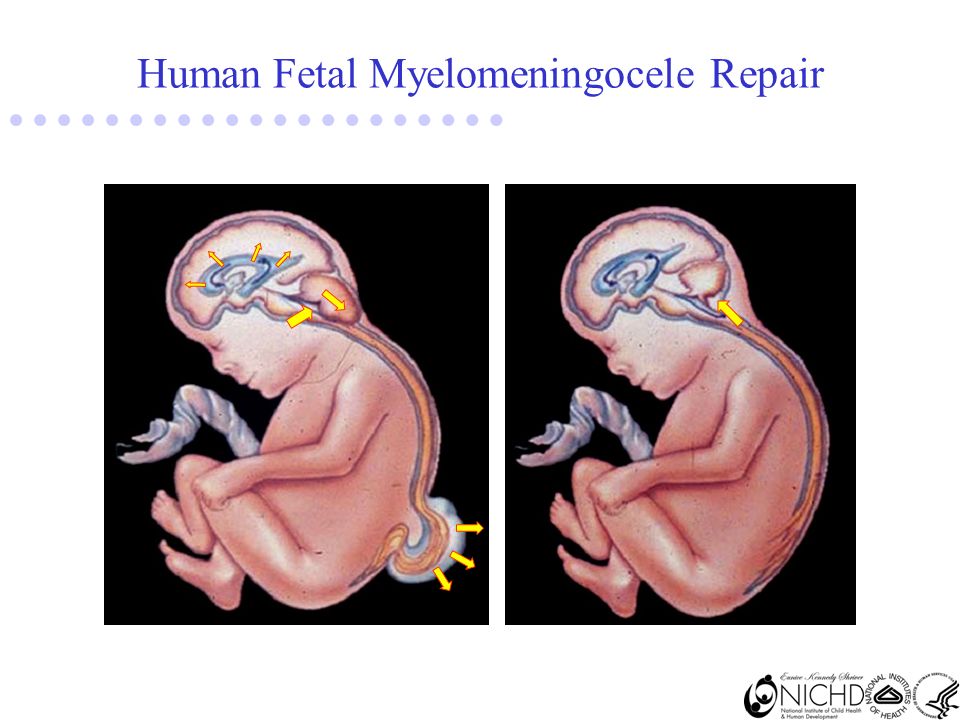 This complication occurs in 1 in 2,000 pregnancies.
This complication occurs in 1 in 2,000 pregnancies.
Why is this happening?
The main cause associated with spina bifida (spina bifida) is a lack of folic acid either due to the malnutrition of the pregnant woman or due to changes in her metabolism.
In some people with a genetic predisposition, this lack of folic acid causes a violation of the closure of the spine. In fact, the risk of recurrence after the birth of a child with spina bifida is 4-5%, so in this case it is recommended to take high doses of folic acid 3 or 4 months before pregnancy.
Some medications for epilepsy and obesity or diabetes in pregnancy are also considered risk factors for neural tube defects.
Although there is a genetic predisposition, it is not possible to find the abnormal gene or chromosome, so most boys and girls with spina bifida do not have genetic changes . Rarely spina bifida (spina bifida) may be accompanied by genetic problems, so investigation is recommended, usually by amniocentesis.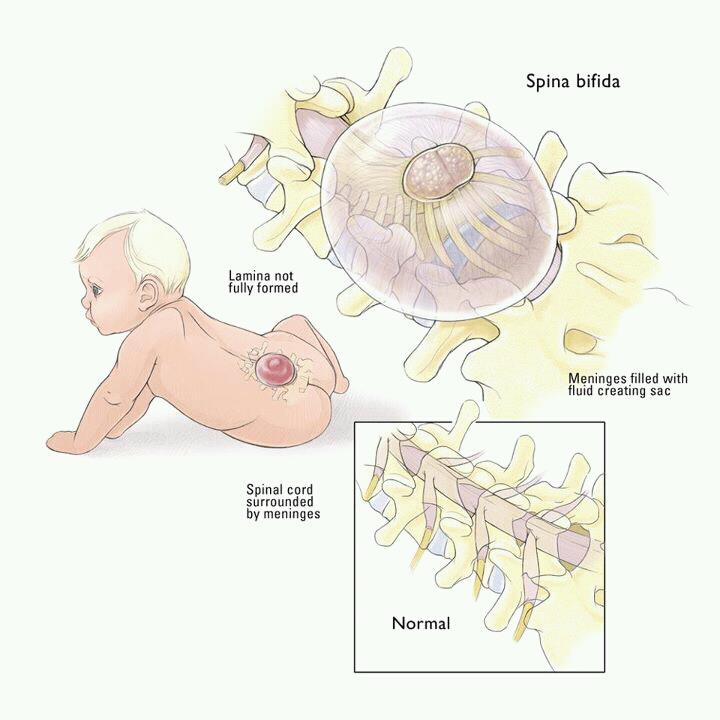
What complications can a child with spina bifida have?
Exposure of amniotic fluid to the spinal cord causes injury throughout pregnancy, causing neurological problems , both motor and sensory, below the level of injury. In the case of defects at the level of the chest or the upper lumbar region, paralysis of the legs and the inability to walk very often occur, often tying the child to a wheelchair.
However, most defects occur in the lower back, lumbosacral region, and in these cases walking is usually possible, but assisted (crutches, cane). Sensitivity below the lesion is reduced, and in many cases there are problems with the sphincters (incontinence and retention of urine and/or feces), as well as sexual function. There may also be problems with malpositions of the feet, such as clubfoot, or knees and hips. Thus, the higher the location of the defect on the spine, the more serious the complications .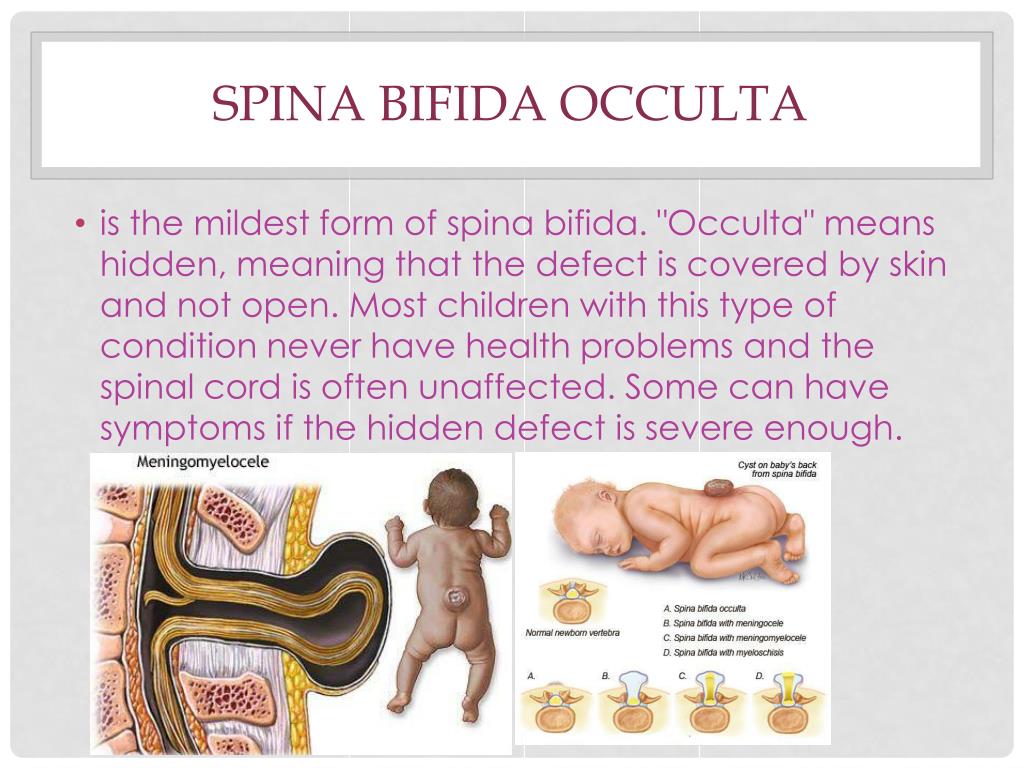
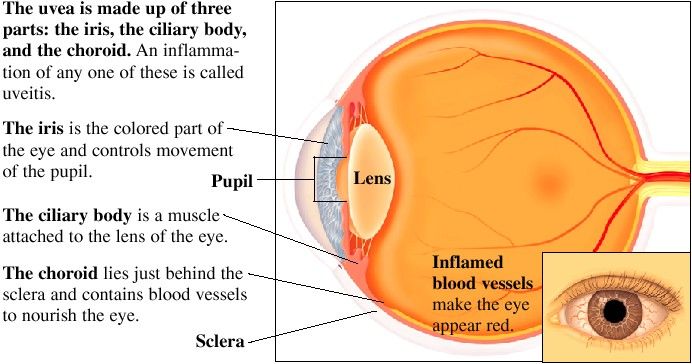
In addition, there is always a type II Arnold-Chiari malformation , which consists in the descent of the cerebellum towards the cervical spine in such a way that the normal flow of cerebrospinal fluid is obstructed. This causes an increase in fluid in the brain (hydrocephalus), which can lead to increased intracranial pressure and significant secondary damage.
Therefore, it is important to drain fluid after childbirth by placing a small tube or shunt , which improves brain pressure, but can have complications and worsen cognitive function in general.
Diagnosis
What tests are needed in my case to find out the prognosis?
The severity of the motor and sensory symptoms will depend mainly on the degree of damage to the spinal cord and the presence of fluid in the brain (hydrocephalus).
Diagnosis of requires a comprehensive examination by an experienced team of fetal medicine specialists , which will allow you to assess whether it is an isolated spina bifida (back bifida), that is, if there are any other malformations or associated genetic anomalies, as well as the level of damage to the spinal cord, that is, at the level of which vertebra the damage is located.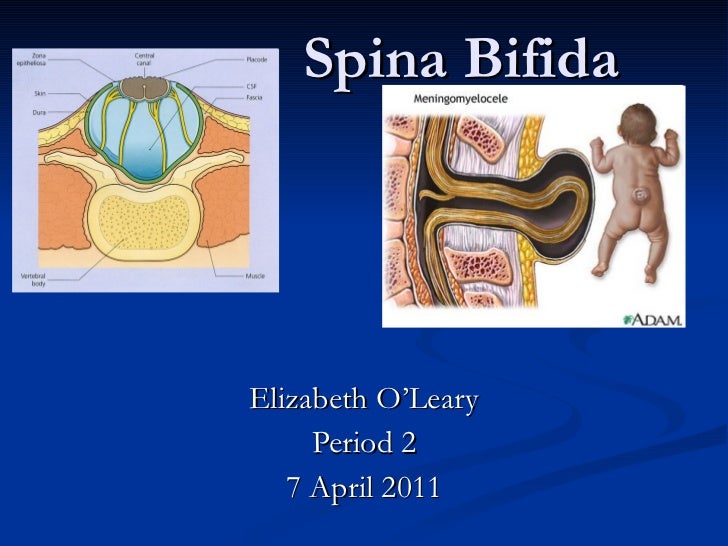
A number of examinations and assessments are carried out for this purpose:
- Specialized ultrasound examination for a detailed examination of the brain and spinal cord in order to assess the extent of the lesion and the presence of hydrocephalus.
- Magnetic resonance imaging
- Amniocentesis and genetic testing.
- Multidisciplinary assessment involving fetal medicine specialists, neonatologists and pediatric neurosurgeons.
Treatment
What are the treatment options?
After completion of the study, all details are discussed in detail with the parents, who always make the decision about treatment.
The traditional treatment for back bifida is to repair and close the injury within the first 24-48 hours after delivery. In addition, due to severe hydrocephalus, usually requires a shunt (see previous section for more information).
Because spinal cord injury is associated with contact with amniotic fluid, treatment during the prenatal period to prevent worsening prognosis after birth has become an option in some cases. In fact, there is evidence that in some cases (depending on the level of injury and the degree of hydrocephalus), surgical intervention on the fetus reduces the need for a shunt at birth and improves motor function.
In fact, there is evidence that in some cases (depending on the level of injury and the degree of hydrocephalus), surgical intervention on the fetus reduces the need for a shunt at birth and improves motor function.
Fetal surgery improves prognosis if performed between 19 and 26 weeks of gestation . It consists in access to the fetus and elimination of the back defect.
At the Hospital Sant Joan de Deu Barcelona , a pregnant woman is given an incision similar to a caesarean section. Another incision is made in the uterus, through which we gain access to the back of the fetus, and an experienced neurosurgeon closes the defect in layers to protect the spinal cord. In our center, we make a small incision (less than 5 centimeters) in the uterus, which significantly reduces the risk of complications. This is an operation that requires careful monitoring of the condition of the pregnant woman and is associated with risk of preterm birth .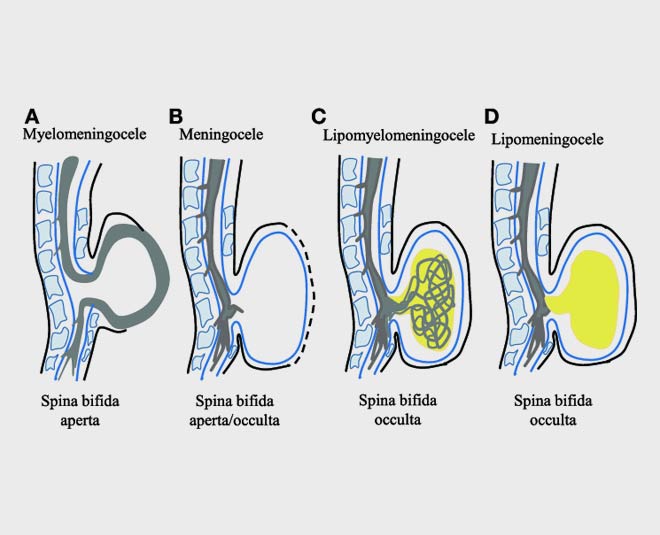
Some medical centers in the world also offer endoscopic treatment , that is, the incision is also made on the skin of the pregnant woman, but the entrance to the uterus is done through endoscopy. After two years of working on experimental models in BCNatal, we decided to continue with the uterine incision, as allows us to correct the defect in the back much more accurately and significantly reduce the operation time at the moment.
In any case, the type of operation can always be assessed, depending on the characteristics of the case, and what is considered a faster and less invasive operation for the pregnant woman and her uterus, and of course for the fetus.
Control in case of fetal surgery
What should I know in case of fetal surgery?
Before the operation, parents can discuss in detail with pediatric specialists all the details of postpartum care, what to expect and what is the quality of life of children with this problem.
Hospitalization of the pregnant woman will typically last 4 or 5 days, and then weekly check-ups with visits and ultrasounds will be required , and maintenance of relative rest at home for the rest of the pregnancy with little physical activity, especially in the first 3 or 4 weeks after the intervention . Usually, by 37 weeks, the pregnancy ends with a caesarean section.
During pregnancy you are supported by fetal nurses not only technically but also emotionally . Also, at the hospital, we can introduce you to other families who have gone through the same experience. This experience is very positive and helps to humanize and understand the problem much more intuitively and without the difficulties that can sometimes arise when receiving only technical information from medical personnel.
Why BCNatal?
Why BCNatal - Sant Joan de Deu?
For parents who want to continue their pregnancy and have a baby with us, we offer fetal surgery team with the best survival and quality of life rates available today .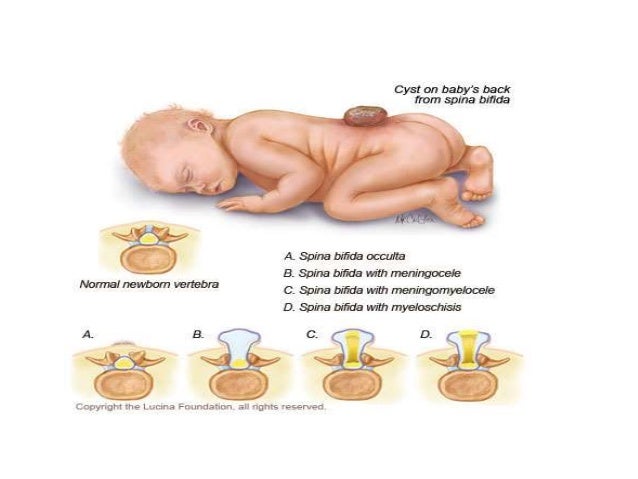
In the case of spina bifida , the operation on the fetus is carefully prepared and modeled using 3D models by a multidisciplinary team of fetal and neurosurgeons. The team from the Hospital's Department of Neurosurgery has extensive experience in repairing spina bifida and is able to perform highly accurate repairs with the best possible results.
Adding to the excellent quality of the antenatal team is the Level 3 Pediatric Center, which has medical teams made up of a large number of specialists trained in neonatal intensive care and equipped with the best and most modern technology.
In particular, children with spina bifida are very familiar and have often been examined prenatally by our specialists in neonatology, neurology, neuroradiology and of course neurosurgery. The hospital employs highly specialized and skilled medical and nursing professionals available 365 days a year, 24 hours a day, to care for these delicate patients and to meet their every need.
After discharge, the pediatric team will monitor the child during the first months and years later, in order to achieve the best possible development of the patient and solve problems in this fundamental part of his life.
What makes us special?
- We have extensive experience in fetal surgery : more than 2000 surgeries performed, the shortest duration of operations described in the medical literature and, as a result, a very low complication rate.
- Our fetal surgery team demonstrates the best survival rates and quality of life that can be achieved today.
- In addition to our surgical experience, being at the same time one of the largest research and development centers at the international level, we are constantly improving materials and methods, which allow us to further improve the accuracy and speed of operations.
- We have formed a multidisciplinary team in , which allows us to approach surgery in a complex way: from choosing the best strategy to individual postpartum care.
Spina bifida (spina bifida) - treatment, symptoms, causes, diagnosis
Spina bifida (spina bifida) is a complex congenital defect in the development of the spinal cord and spine. This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.
Spina bifida (back bifida) is an incurable, life-long condition that affects the neuromuscular and musculoskeletal systems.
This defect varies by type and ranges from moderate to severe.
Children with this defect may need corsets as the body grows, and in severe cases, a wheelchair.
Treatment is mainly aimed at slowing down the deformity and maintaining motor activity.
The defect may occur along the entire length of the spine and may present with part of the spinal cord and surrounding tissues protruding outward rather than inward. Approximately 85 percent of defects occur in the lower back and 15 percent in the neck and thoracic region. Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis).
Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis).
According to studies, this developmental anomaly occurs in 7 cases per 10,000 newborns. There are several types of spina bifida that have varying degrees of severity.
- Latent spina bifida (spina bifida occulta) - the most moderate form, in which there are no obvious signs of malformation and changes in the skin. In this form, at least one vertebra changes, but the nerves and spinal cord do not bulge. A child at birth may have a spot or depression in the area of the anomaly. And usually, the baby will not have symptoms. With this form of anomaly (as well as with others), there may be an anomaly in the development of the spinal cord, characterized by attachment of the spinal cord to the spine to the end of the lumbar region, when normally the spinal cord ends at the level of the first lumbar vertebrae and sags freely without attachment to the spine.

- Meningocele (meningocele) moderate anomaly (and the most common), in which the spinal canal is not properly closed and the meninges (membranes that cover the spinal cord) bulge outside the bony structures of the spinal canal, but the spinal cord itself remains intact. The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord.
- Lipomeningocele is an anomaly in which fatty tissue is attached to the spinal cord and puts pressure on it. Children with this form of anomaly may not have severe nerve damage, but bladder and bowel function may be impaired. In these cases, surgical treatment is also often used.
- Myelomeningocele: the most severe common form and associated with spina bifida.
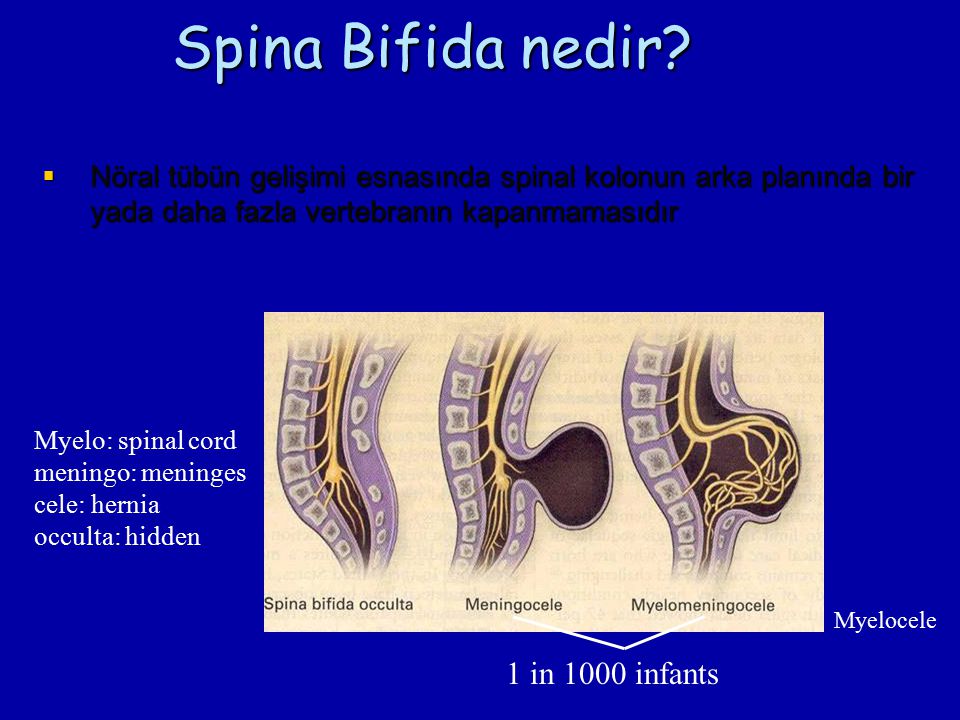 The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part. In addition, nerve damage and other pathologies are observed.
The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part. In addition, nerve damage and other pathologies are observed.
Symptoms
The symptoms of spina bifida vary greatly, depending on the form and severity of the individual child. For example, at birth:
- In latent splitting (spina bifida occulta) there may be no obvious signs or symptoms—only a small spot, depression, or birthmark.
- With a meningocele, there will be a sac-like protrusion that will be located on the back in the spinal region.
- With myelomeningocele (myelomeningocele) there will also be a protrusion, but with altered skin, there will be a release of nerves and spinal cord.
In severe spina bifida with localization in the lumbar spine, the following symptoms may occur: paralysis of the lower extremities, dysfunction of the bladder, intestines.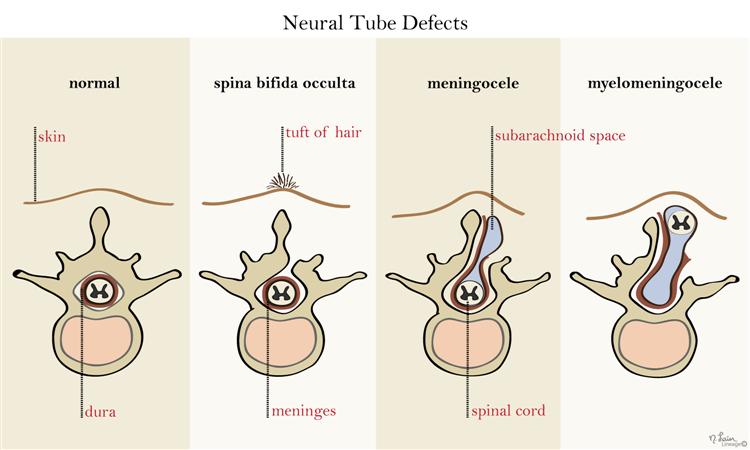
- Hydrocephalus occurs in 75 percent of myelomeningocele cases and this condition requires operative endoscopic treatment in order to restore normal CSF flow or a shunt to drain excess fluid from the brain.
- Chiari anomaly (displacement of the brain into the upper cervical vertebrae) can cause pressure on the brainstem, which can manifest as impaired speech, swallowing and motor disorders in the limbs.
- Underdevelopment of the spinal cord Orthopedic problems including scoliosis, kyphosis, hip dysplasia (congenital dislocation), combined deformities, clubfoot, etc.
- Precocious puberty (especially in girls with spina bifida and hydrocephalus).
- depression and other neurotic conditions
- obesity
- dermatological problems
- developmental anomalies of the urinary tract.
- heart disease
- vision problems
Diagnosis
Diagnosis may be performed during pregnancy to evaluate the fetus for spina bifida. These include:
These include:
- Amniocentesis: A procedure in which a long, thin needle is inserted through the mother's abdomen into the amniotic sac to remove a small amount of amniotic fluid for examination. The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects.
- Prenatal ultrasound: this technique, being absolutely harmless, allows you to non-invasively assess the condition and visualize the internal organs, vessels, tissues of the fetus. Sometimes it is possible to diagnose not only spina bifida, but also other anomalies.
- Blood tests: It is recommended that blood tests be performed between 15 and 20 weeks of gestation for all women who have not previously had a child with an open neural tube defect and who do not have a family history of the condition. A blood test for alpha-fetoprotein and other biochemical parameters can determine how high the risk of developing spinal anomalies is.
- At birth, severe cases of spina bifida are evident by the presence of a fluid-filled sac bulging on the back of the newborn. Visual indicators of mild forms (spina occulta) may be a hairy patch on the skin or a depression along the spine. Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography).
Causes
During pregnancy, the human brain and spinal column begin to form as a flat sheet of cells that folds into a tube called the neural tube. If all or part of the neural tube fails to close, then the open area is called an open neural tube defect. An open neural tube is open in 80 percent of cases, and is covered by bone or skin in 20 percent of cases. The cause of spina bifida (spina bifida and other defects) remains unknown, but is most likely the result of a combination of genetic, nutritional, and environmental factors, such as:
- maternal dietary folic acid (vitamin B) deficiency during pregnancy (sufficient folic acid intake during pregnancy may reduce the risk of this anomaly).
- maternal uncontrolled diabetes
- Certain medicines (antibiotics, anticonvulsants).
- The genetic factor, as a rule, matters only in 10 percent of cases.
- Mother's age
- What kind of births on the account (firstborns are more at risk).
- Socioeconomic status (children born in lower socioeconomic families are at higher risk).
- ethnicity
- obesity or excessive consumption of alcohol by a pregnant woman
- When exposed to pregnant hyperthermia in the early stages (sauna, jacuzzi).
Treatment
Spina bifida can be treated immediately after birth. If this defect is diagnosed prenatally, then a caesarean section is recommended in order to reduce possible damage to the spinal cord during the passage of the birth canal. Newborns with meningocele or myelomeningocele are recommended to have surgery within 24 hours of birth. With such an operation, the bone defect is closed and it is possible to preserve the function of the intact part of the spinal cord.