Second stage of labor begins when
Stages of labor | March of Dimes
Every woman’s labor is different. And it may be different each time you have a baby.
Learning about stages of labor before your due date can help you know what to expect so you can feel ready for your baby’s birth.
Use a birth plan so your health care provider and hospital staff know what your plans are for labor and after birth.
Having a professional support person, like a doula, during labor can help you have a better experience with labor and birth.
Try to stay comfortable and relaxed through labor. Move around and try different positions to find what works best for you.
What are stages of labor?
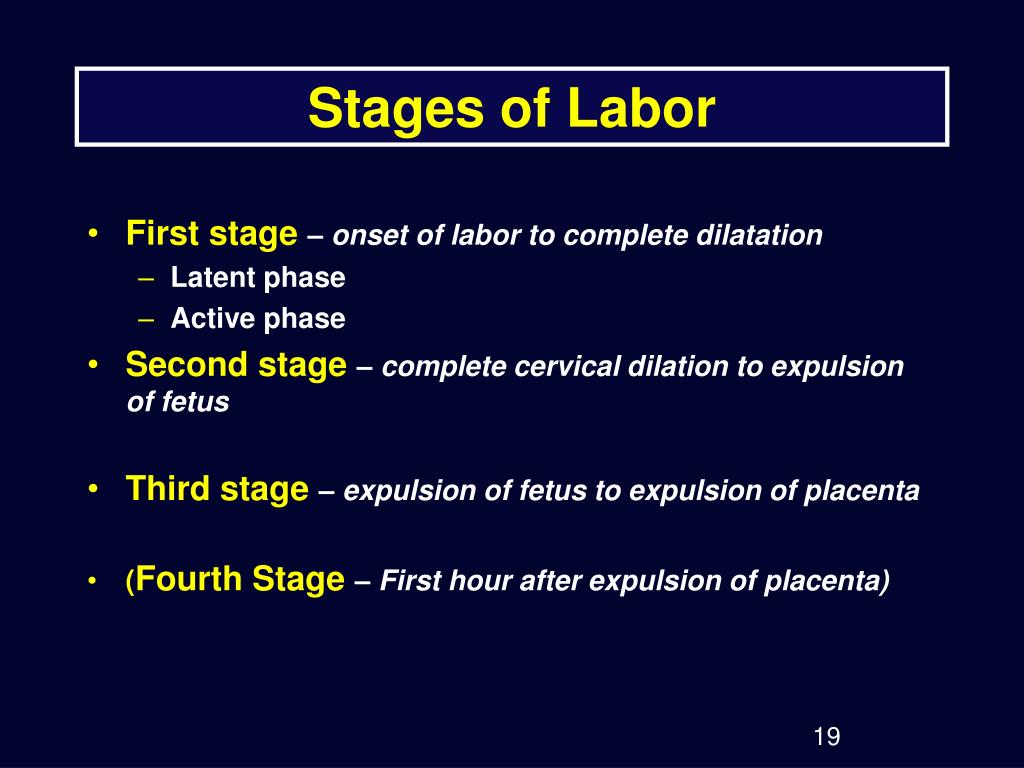
Labor (also called childbirth) is the process of your baby leaving the uterus (womb). Labor is divided into three stages:
- Labor
- Pushing and birth
- Delivery of the placenta
Every woman’s labor is different. And your labor may be different each time you have a baby. But there are patterns to labor that are true for most women. Learning about the stages of labor and what happens during each one can help you know what to expect once labor begins.
What is a birth plan?
A birth plan is a set of instructions you make about your baby’s birth. It includes things like:
- Where you want to have your baby
- Who you want to be with you during labor and birth
- If you want medicine to help with labor pain
- If there are cultural traditions you’d like to follow during labor and birth
- If you plan to breastfeed
Before your due date, use the March of Dimes birth plan to help you think about how you want your labor to be. Share the completed plan with your partner, your health care provider and the staff at the hospital where you plan to give birth.
What is a doula?
You may want to have a professional support person help you through labor and childbirth. A doula is a professional labor assistant.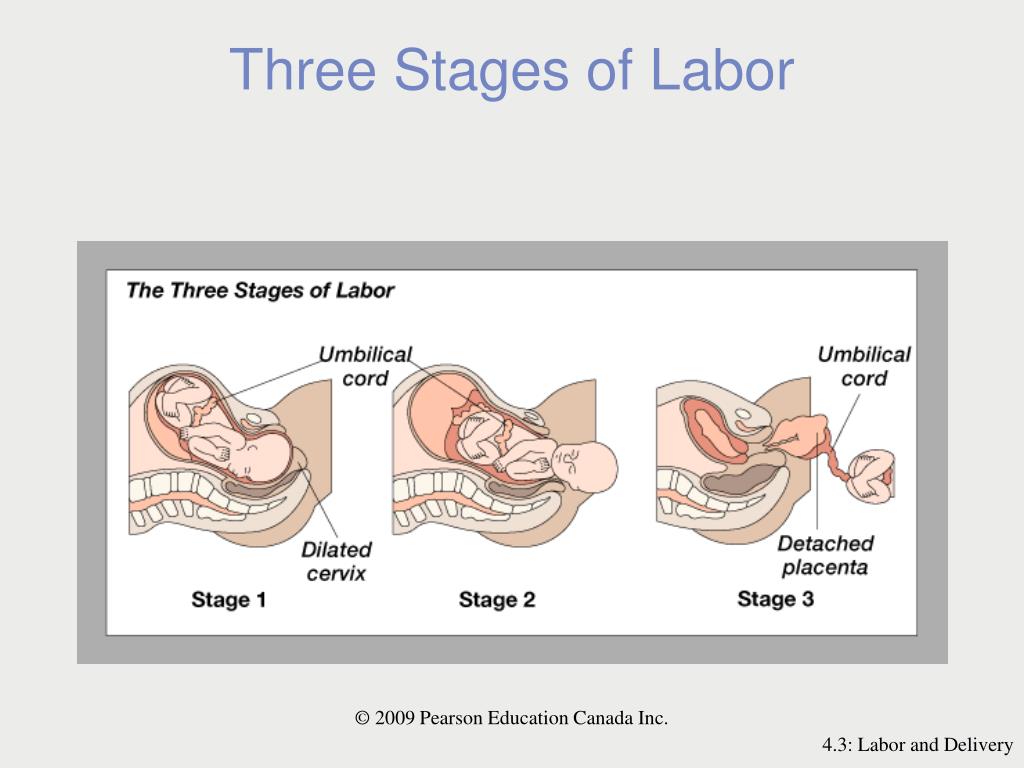 This is someone who is trained to give physical and emotional care and support to women and their families before, during and after childbirth. For example, a doula can:
This is someone who is trained to give physical and emotional care and support to women and their families before, during and after childbirth. For example, a doula can:
- Help you stay comfortable
- Explain what’s happening during labor and birth and any procedures you may have
- Encourage you and give you confidence
- Support your family and friends who are with you during labor
- Let hospital staff know what you need
- Help you get started breastfeeding
Having a support person like a doula can be good for you, your baby and your family. It can help you feel good about your birth experience. Having a doula can help:
- Shorten your labor
- Reduce your need for pain medicine during labor
- Reduce your risk of needing a cesarean birth or the need for your provider to use forceps or suction with a vaginal birth
- Your baby get a good Apgar score at birth. Your baby gets an Apgar test right after birth to check his overall health.
 The test checks his heart rate, breathing, muscle tone, reflexes and skin color.
The test checks his heart rate, breathing, muscle tone, reflexes and skin color.
To find a certified doula, ask your provider or go to DONA International.
You also may want to have your partner, a friend or a family member be a support person to help you through labor. They can go to childbirth education classes with you to learn ways to help, like timing your contractions, helping you relax and helping you move around to find a comfortable position. Ask your provider about childbirth education classes in your area.
If you decide to have a doula or another support person help you with labor and birth, put their names and contact information in your birth plan. Share your plan with your provider and with hospital staff.
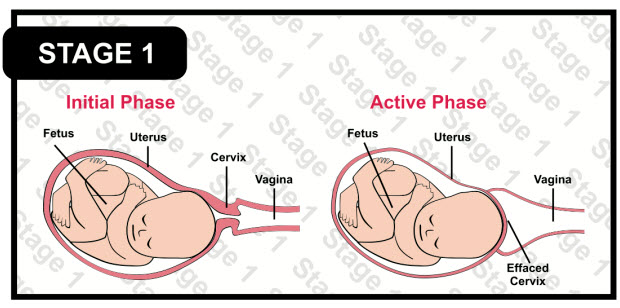
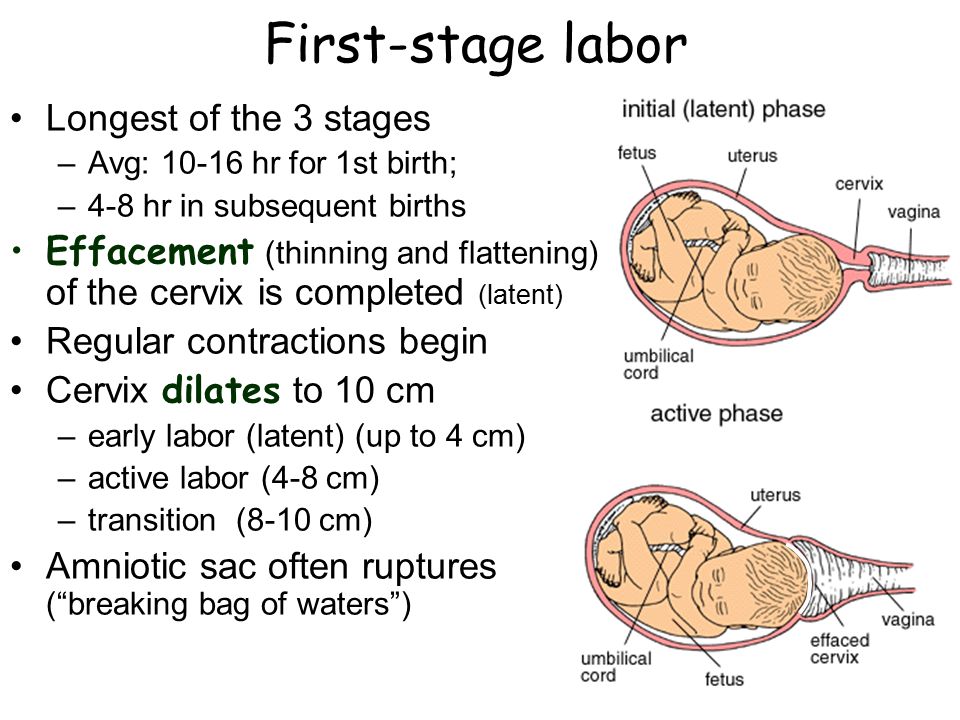
What happens in the first stage of labor?
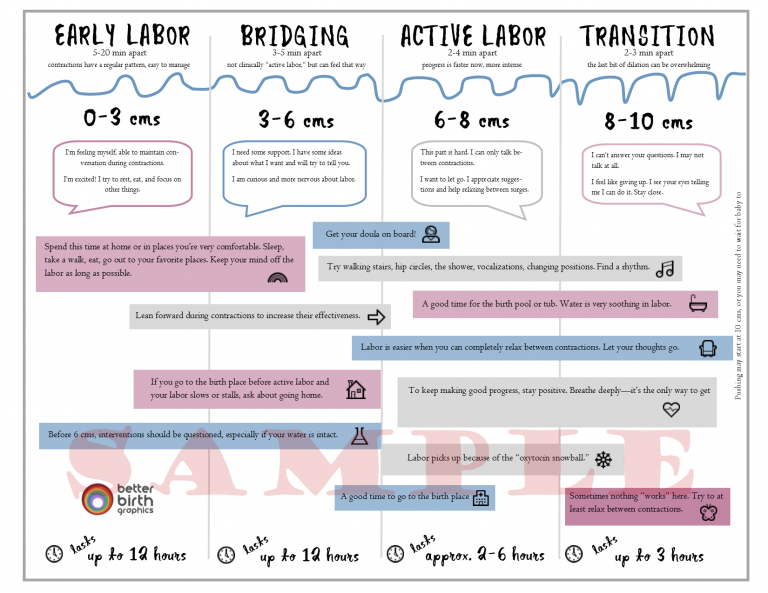
The first stage of labor is the longest stage. For first-time moms, it can last from 12 to 19 hours. It may be shorter (about 14 hours) for moms who’ve already had children. It’s when contractions become strong and regular enough to cause your cervix to dilate (open) and thin out (efface).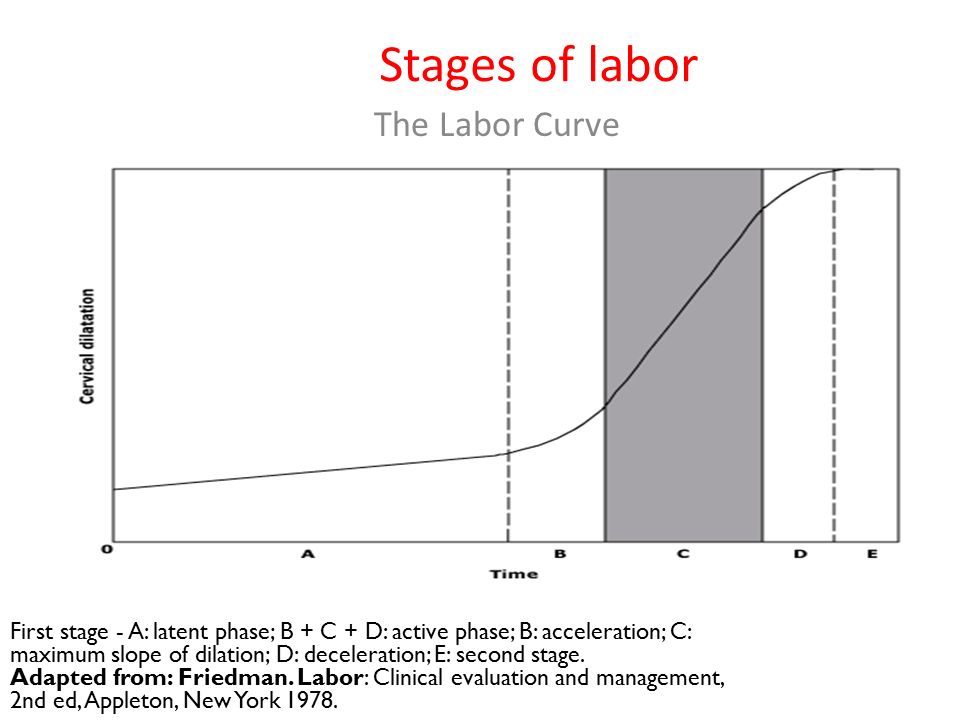 This lets your baby move lower into your pelvis and into your birth canal (vagina). This stage of labor ends when you are 10 centimeters dilated. The first stage is divided into three parts: early labor, active labor and transition to stage 2 of labor.
This lets your baby move lower into your pelvis and into your birth canal (vagina). This stage of labor ends when you are 10 centimeters dilated. The first stage is divided into three parts: early labor, active labor and transition to stage 2 of labor.
Early labor
For most first-time moms, early labor lasts about 6 to 12 hours. You can spend this time at home or wherever you’re most comfortable. During early labor:
- You may feel mild contractions that come every 5 to 15 minutes and last 60 to 90 seconds.
- You may have a bloody show. This is a pink, red or bloody vaginal discharge. If you have heavy bleeding or bleeding like your period, call your provider right away.
What you can do in early labor:
This is a great time for you to rely on your doula or labor support person. Try the methods you learned about in childbirth education classes about how to relax and cope with pain. During early labor:
- Rest and relax as much as you can.
- Take a shower or bath.
- Go for a walk.
- Change positions often.
- Make sure you’re ready to go to the hospital.
- Take slow, relaxing breaths during contractions.
Active labor
This is when you head to the hospital! Active labor usually lasts about 4 to 8 hours. It starts when your contractions are regular and your cervix has dilated to 6 centimeters. In active labor:
- Your contractions get stronger, longer and more painful. Each lasts about 45 seconds and they can be as close as 3 minutes apart.
- You may feel pressure in your lower back, and your legs may cramp.
- You may feel the urge to push.
- Your cervix will dilate up to 10 centimeters.
- If your water hasn’t broken, it may break now.
- You may feel sick to your stomach.
What you can do in active labor:
- Make sure the hospital staff has a copy of your birth plan.
- Try to stay relaxed and not think too hard about the next contraction.
- Move around or change positions. Walk the hallways in the hospital.
- Drink water or other liquids. But don’t eat solid foods.
- If you’re going to take medicine to help relieve labor pain, you can start taking it now. Your choice about pain relief is part of your birth plan.
- Go to the bathroom often to empty your bladder. An empty bladder gives more room for your baby’s head to move down.
- If you feel like you want to push, tell your provider. You don’t want to start pushing until your provider checks your cervix to see how dilated it is.
Transition to the second stage of labor
This can be the toughest and most painful part of labor. It can last 15 minutes to an hour. During the transition:
- Contractions come closer together and can last 60 to 90 seconds. You may feel like you want to bear down.
- You may feel a lot of pressure in your lower back and rectum. If you feel like you want to push, tell your provider.

What happens in the second stage of labor?
In the second stage of labor, your cervix is fully dilated and ready for childbirth. This stage is the most work for you because your provider wants you to start pushing your baby out. This stage can be as short as 20 minutes or as long as a few hours. It may be longer for first-time moms or if you’ve had an epidural. An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief used during labor. The second stage ends when your baby is born.
During the second stage of labor:
- Your contractions may slow down to come every 2 to 5 minutes apart. They last about 60 to 90 seconds.
- You may get an episiotomy. This is a small cut made at the opening of the vagina to help let the baby out. Most women don't need an episiotomy.
- Your baby’s head begins to show. This is called crowning.

- Your provider guides your baby out of the birth canal. She may use special tools, like forceps or suction, to help your baby out.
- Your baby is born, and the umbilical cord is cut. Instructions about who’s cutting the umbilical cord are in your birth plan.
What you can do:
- Find a position that is comfortable for you. You can squat, sit, kneel or lie back.
- Push during contractions and rest between them. Push when you feel the urge or when your provider tells you.
- If you’re uncomfortable or pushing has stopped, try a new position.
What happens in the third stage of labor?
In the third stage of labor, the placenta is delivered. The placenta grows in your uterus and supplies your baby with food and oxygen through the umbilical cord. This stage is the shortest and usually doesn’t take more than 20 minutes.
During the third stage of labor:
- You have contractions that are closer together and not as painful as earlier.
 These contractions help the placenta separate from the uterus and move into the birth canal. They begin 5 to 30 minutes after birth.
These contractions help the placenta separate from the uterus and move into the birth canal. They begin 5 to 30 minutes after birth. - You continue to have contractions even after the placenta is delivered. You may get medicine to help with contractions and to prevent heavy bleeding.
- Your provider squeezes and presses on your belly to make sure the uterus feels right.
- If you had an episiotomy, your provider repairs it now.
- If you’re storing your umbilical cord blood, your provider collects it now. Umbilical cord blood is blood left in the umbilical cord and placenta after your baby is born and the cord is cut. Some moms and families want to store or donate umbilical cord blood so it can be used later to treat certain diseases, like cancer. Your instructions about umbilical cord blood can be part of your birth plan.
- You may have chills or feel shaky. Tell your provider if these are making you uncomfortable.
What happens after your baby is born?
Congratulations! It’s time to hold your baby! Right after birth your provider places your baby skin-to-skin on your chest and covers him with a blanket. Holding your baby skin-to-skin helps your baby stay warm as he gets used to being outside the womb. It’s also a great way to get started breastfeeding. You can start breastfeeding even within an hour of your baby’s birth. Even if you don’t plan to breastfeed, hold your baby skin-to-skin so you get to know each other right away. Your baby will welcome your gentle touch, and this closeness can help you and your baby bond.
Holding your baby skin-to-skin helps your baby stay warm as he gets used to being outside the womb. It’s also a great way to get started breastfeeding. You can start breastfeeding even within an hour of your baby’s birth. Even if you don’t plan to breastfeed, hold your baby skin-to-skin so you get to know each other right away. Your baby will welcome your gentle touch, and this closeness can help you and your baby bond.
After birth, your body starts to change to help you heal. Your provider takes your temperature and checks your heart and blood pressure to make sure you’re doing well. If you had anesthesia during labor, your provider makes sure you’re recovering without any complications.
Last reviewed: March, 2019
Stages of Labor - StatPearls
Continuing Education Activity
Labor is a process that subdivides into three stages. The first stage starts when labor begins and ends with full cervical dilation and effacement. The second stage commences with complete cervical dilation and ends with the delivery of the fetus. The third stage initiates after the fetus is delivered and ends when the placenta is delivered. This activity outlines the stages of labor and its relevance to the interprofessional team in managing women in labor.
The third stage initiates after the fetus is delivered and ends when the placenta is delivered. This activity outlines the stages of labor and its relevance to the interprofessional team in managing women in labor.
Objectives:
Summarize the three stages of labor.
Describe potential complications that may arise during each stage of labor.
Identify what therapies may be targeted at the different stages of labor to result in better patient outcomes.
Review the importance of accurate communication between the interprofessional team members regarding the stages of labor, leading to improved patient outcomes.
Access free multiple choice questions on this topic.
Introduction
Labor is the process through which a fetus and placenta are delivered from the uterus through the vagina.[1] Human labor divides into three stages. The first stage is further divided into two phases. Successful labor involves three factors: maternal efforts and uterine contractions, fetal characteristics, and pelvic anatomy.[1] This triad is classically referred to as the passenger, power, and passage.[1] Clinicians typically use multiple modalities to monitor labor. Serial cervical examinations are used to determine cervical dilation, effacement, and fetal position, also known as the station. Fetal heart monitoring is employed nearly continuously to assess fetal well-being throughout labor. Cardiotocography is used to monitor the frequency and adequacy of contractions. Medical professionals use the information they obtain from monitoring and cervical exams to determine the patient's stage of labor and monitor labor progression.
Successful labor involves three factors: maternal efforts and uterine contractions, fetal characteristics, and pelvic anatomy.[1] This triad is classically referred to as the passenger, power, and passage.[1] Clinicians typically use multiple modalities to monitor labor. Serial cervical examinations are used to determine cervical dilation, effacement, and fetal position, also known as the station. Fetal heart monitoring is employed nearly continuously to assess fetal well-being throughout labor. Cardiotocography is used to monitor the frequency and adequacy of contractions. Medical professionals use the information they obtain from monitoring and cervical exams to determine the patient's stage of labor and monitor labor progression.
Initial Evaluation and Presentation of Labor
Women will often self-present to obstetrical triage with concern for the onset of labor. Common chief complaints include painful contractions, vaginal bleeding/bloody show, and fluid leakage from the vagina. It is up to the clinician to determine if the patient is in labor, defined as regular, clinically significant contractions with an objective change in cervical dilation and/or effacement.[1] When women first present to the labor and delivery unit, vital signs, including temperature, heart rate, oxygen saturation, respiratory rate, and blood pressure, should be obtained and reviewed for any abnormalities. The patient should be placed on continuous cardiotocographic monitoring to ensure fetal wellbeing. The patient's prenatal record, including obstetric history, surgical history, medical history, laboratory, and imaging data, should undergo review. Finally, a history of present illness, review of systems, and physical exam, including a sterile speculum exam, will need to take place.
It is up to the clinician to determine if the patient is in labor, defined as regular, clinically significant contractions with an objective change in cervical dilation and/or effacement.[1] When women first present to the labor and delivery unit, vital signs, including temperature, heart rate, oxygen saturation, respiratory rate, and blood pressure, should be obtained and reviewed for any abnormalities. The patient should be placed on continuous cardiotocographic monitoring to ensure fetal wellbeing. The patient's prenatal record, including obstetric history, surgical history, medical history, laboratory, and imaging data, should undergo review. Finally, a history of present illness, review of systems, and physical exam, including a sterile speculum exam, will need to take place.
During the sterile speculum exam, clinicians will look for signs of rupture of membranes such as amniotic fluid pooling in the posterior vaginal canal. If the clinician is unsure whether or not a rupture of membranes has occurred, additional testing such as pH testing, microscopic exam looking for ferning of the fluid, or laboratory testing of the fluid can be the next step.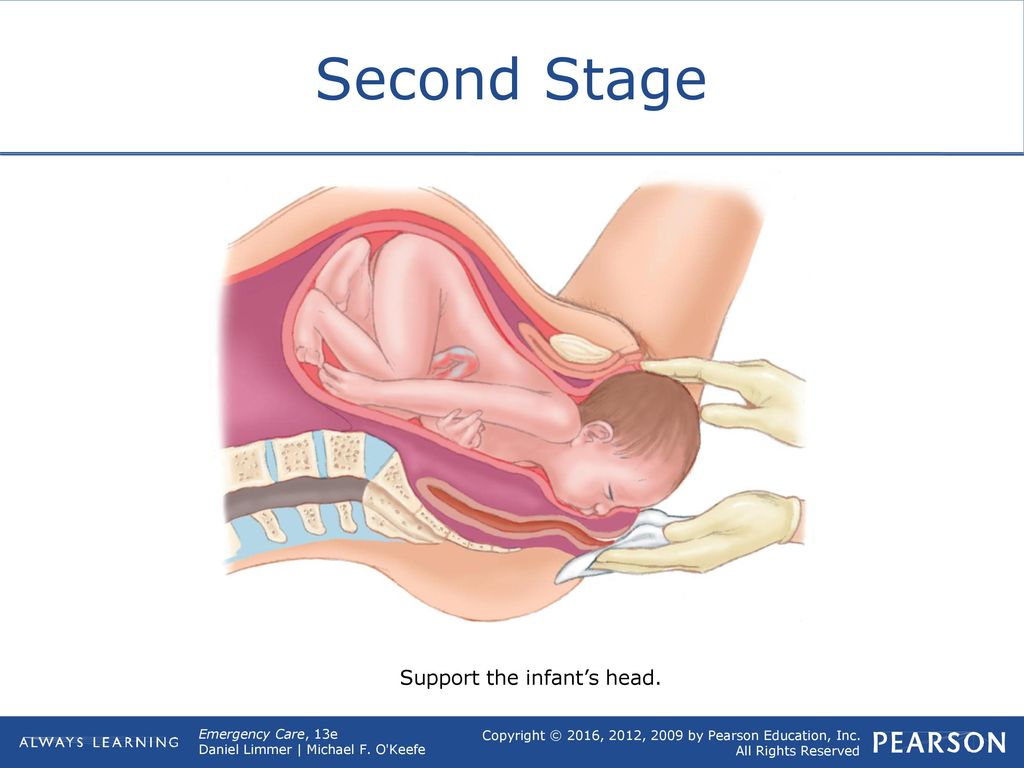 [2] Amniotic fluid has a pH of 7.0 to 7.5, which is more basic than normal vaginal pH. A sterile gloved exam should be done to determine the degree of cervical dilation and effacement. The measurement of cervical dilation is made by locating the external cervical os and spreading one's fingers in a ‘V’ shape, and estimating the distance in centimeters between the two fingers. Effacement is measured by estimating the percentage remaining of the length of the thinned cervix compared to the uneffaced cervix. During the cervical exam, confirmation of the presenting fetal part is also necessary. Bedside ultrasound can be employed to confirm the presentation and position of the fetal presenting part. Particular mention should be noted in the case of breech presentation due to its increased risks regarding fetal morbidity and mortality compared with the cephalic presenting fetus.
[2] Amniotic fluid has a pH of 7.0 to 7.5, which is more basic than normal vaginal pH. A sterile gloved exam should be done to determine the degree of cervical dilation and effacement. The measurement of cervical dilation is made by locating the external cervical os and spreading one's fingers in a ‘V’ shape, and estimating the distance in centimeters between the two fingers. Effacement is measured by estimating the percentage remaining of the length of the thinned cervix compared to the uneffaced cervix. During the cervical exam, confirmation of the presenting fetal part is also necessary. Bedside ultrasound can be employed to confirm the presentation and position of the fetal presenting part. Particular mention should be noted in the case of breech presentation due to its increased risks regarding fetal morbidity and mortality compared with the cephalic presenting fetus.
Management of Normal Labor
Labor is a natural process, but it can suffer interruption by complicating factors, which at times necessitate clinical intervention.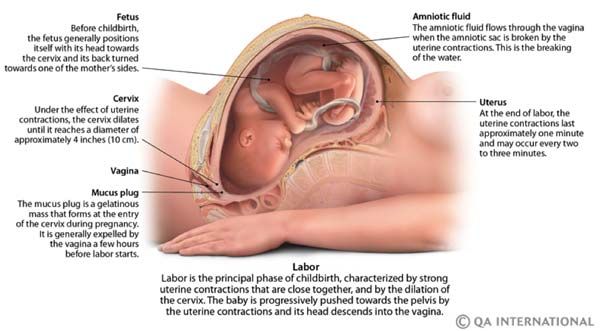 The management of low-risk labor is a delicate balance between allowing the natural process to proceed while limiting any potential complications.[3] During labor, cardiotocographic monitoring is often employed to monitor uterine contractions and fetal heart rate over time. Clinicians monitor fetal heart tracings to evaluate for any signs of fetal distress that would warrant intervention as well as the adequacy or inadequacy of contractions. Vital signs of the mother are taken at regular intervals and whenever concerns arise regarding a clinical status change. Laboratory testing often includes the hemoglobin, hematocrit, and platelet count and is sometimes repeated following delivery if significant blood loss occurs. Cervical exams are usually performed every 2 to 3 hours unless concerns arise and warrant more frequent exams. Frequent cervical exams are associated with a higher risk of infection, especially if a rupture of membranes has occurred. Women should be allowed to ambulated freely and change positions if desired.
The management of low-risk labor is a delicate balance between allowing the natural process to proceed while limiting any potential complications.[3] During labor, cardiotocographic monitoring is often employed to monitor uterine contractions and fetal heart rate over time. Clinicians monitor fetal heart tracings to evaluate for any signs of fetal distress that would warrant intervention as well as the adequacy or inadequacy of contractions. Vital signs of the mother are taken at regular intervals and whenever concerns arise regarding a clinical status change. Laboratory testing often includes the hemoglobin, hematocrit, and platelet count and is sometimes repeated following delivery if significant blood loss occurs. Cervical exams are usually performed every 2 to 3 hours unless concerns arise and warrant more frequent exams. Frequent cervical exams are associated with a higher risk of infection, especially if a rupture of membranes has occurred. Women should be allowed to ambulated freely and change positions if desired.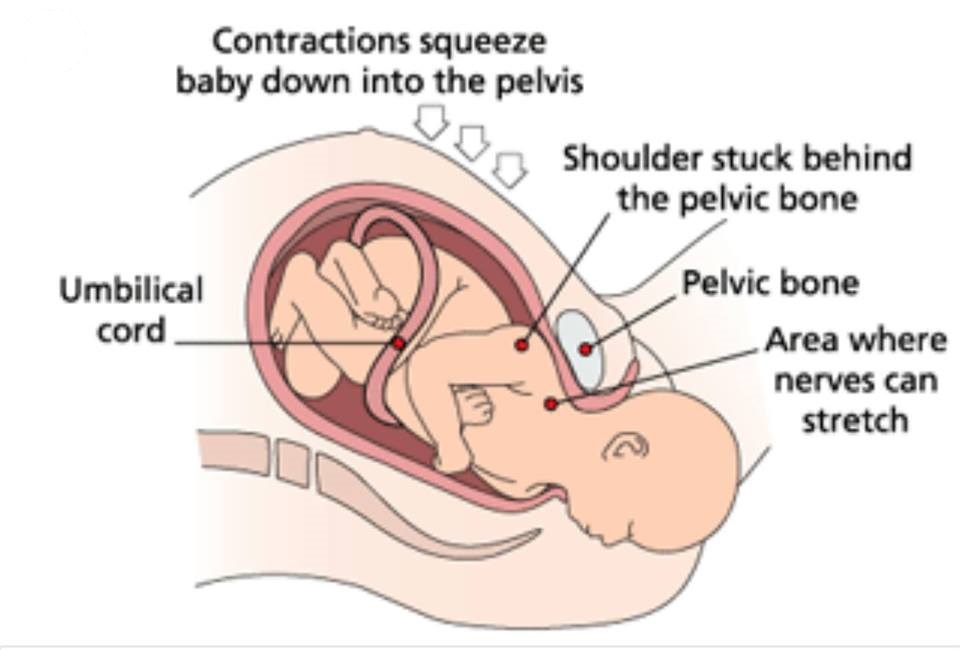 [3] An intravenous catheter is typically inserted in case it is necessary to administer medications or fluids. Oral intake should not be withheld. If the patient remains without food or drink for a prolonged period of time, intravenous fluids should be considered to help replace losses but do not need to be used continuously on all laboring patients.[3] Analgesia is offered in the form of intravenous opioids, inhaled nitrous oxide, and neuraxial analgesia in those who are appropriate candidates.[4] Amniotomy is considered on an as-needed basis for fetal scalp monitoring or labor augmentation, but its routine use should be discouraged.[3] Oxytocin may be initiated to augment contractions found to be inadequate.
[3] An intravenous catheter is typically inserted in case it is necessary to administer medications or fluids. Oral intake should not be withheld. If the patient remains without food or drink for a prolonged period of time, intravenous fluids should be considered to help replace losses but do not need to be used continuously on all laboring patients.[3] Analgesia is offered in the form of intravenous opioids, inhaled nitrous oxide, and neuraxial analgesia in those who are appropriate candidates.[4] Amniotomy is considered on an as-needed basis for fetal scalp monitoring or labor augmentation, but its routine use should be discouraged.[3] Oxytocin may be initiated to augment contractions found to be inadequate.
First Stage of Labor
The first stage of labor begins when labor starts and ends with full cervical dilation to 10 centimeters.[1] Labor often begins spontaneously or may be induced medically for a variety of maternal or fetal indications.[5] Methods of inducing labor include cervical ripening with prostaglandins, membrane stripping, amniotomy, and intravenous oxytocin. [5] Although precisely determining when labor starts may be inexact, labor is generally defined as beginning when contractions become strong and regularly spaced at approximately 3 to 5 minutes apart.[1] Women may experience painful contractions throughout pregnancy that do not lead to cervical dilation or effacement, referred to as false labor. Thus, defining the onset of labor often relies on retrospective or subjective data. Friedman et al. were some of the first to study labor progress and defined the beginning of labor as starting when women felt significant and regular contractions.[6] He graphed cervical dilation over time and determined that normal labor has a sigmoidal shape. Based on the analysis from his labor graphs, he proposed that labor has three divisions. First, a preparatory stage marked by slow cervical dilation, with large biochemical and structural changes. This is also known as the latent phase of the first stage of labor. Second, a much shorter and rapid dilational phase is also known as the active phase of the first stage of labor.
[5] Although precisely determining when labor starts may be inexact, labor is generally defined as beginning when contractions become strong and regularly spaced at approximately 3 to 5 minutes apart.[1] Women may experience painful contractions throughout pregnancy that do not lead to cervical dilation or effacement, referred to as false labor. Thus, defining the onset of labor often relies on retrospective or subjective data. Friedman et al. were some of the first to study labor progress and defined the beginning of labor as starting when women felt significant and regular contractions.[6] He graphed cervical dilation over time and determined that normal labor has a sigmoidal shape. Based on the analysis from his labor graphs, he proposed that labor has three divisions. First, a preparatory stage marked by slow cervical dilation, with large biochemical and structural changes. This is also known as the latent phase of the first stage of labor. Second, a much shorter and rapid dilational phase is also known as the active phase of the first stage of labor. Third, a pelvic division phase, which takes place during the second stage of labor.[1]
Third, a pelvic division phase, which takes place during the second stage of labor.[1]
The first stage of labor is further subdivides into two phases, defined by the degree of cervical dilation. The latent phase is commonly defined as the 0 to 6 cm, while the active phase commences from 6 cm to full cervical dilation. The presenting fetal part also begins the process of engagement into the pelvis during the first stage. Throughout the first stage of labor, serial cervical exams are done to determine the position of the fetus, cervical dilation, and cervical effacement. Cervical effacement refers to the cervical length in the anterior-posterior plane. When the cervix is completely thinned out, and no length is left, this is referred to as 100 percent effacement.[1] The station of the fetus is defined relative to its position in the maternal pelvis. When the bony fetal presenting part is aligned with the maternal ischial spine, the fetus is 0 station. Proximal to the ischial spines are stations -1 centimeter to -5 centimeters, and distal to the ischial spines is +1 to +5 station. [1] The first stage of labor contains a latent phase and an active phase. During the latent phase, the cervix dilates slowly to approximately 6 centimeters. The latent phase is generally considerably longer and less predictable with regard to the rate of cervical change than is observed in the active phase. A normal latent phase can last up to 20 hours and 14 hours in nulliparous and multiparous women, respectively, without being considered prolonged.[1] Sedation can increase the duration of the latent phase of labor.[7] The cervix changes more rapidly and predictably in the active phase until it reaches 10 centimeters and cervical dilation and effacement are complete. Active labor with more rapid cervical dilation generally starts around 6 centimeters of dilation. During the active phase, the cervix typically dilates at a rate of 1.2 to 1.5 centimeters per hour. Multiparas, or women with a history of prior vaginal delivery, tend to demonstrate more rapid cervical dilation.[1] The absence of cervical change for greater than 4 hours in the presence of adequate contractions or six hours with inadequate contractions is considered the arrest of labor and may warrant clinical intervention.
[1] The first stage of labor contains a latent phase and an active phase. During the latent phase, the cervix dilates slowly to approximately 6 centimeters. The latent phase is generally considerably longer and less predictable with regard to the rate of cervical change than is observed in the active phase. A normal latent phase can last up to 20 hours and 14 hours in nulliparous and multiparous women, respectively, without being considered prolonged.[1] Sedation can increase the duration of the latent phase of labor.[7] The cervix changes more rapidly and predictably in the active phase until it reaches 10 centimeters and cervical dilation and effacement are complete. Active labor with more rapid cervical dilation generally starts around 6 centimeters of dilation. During the active phase, the cervix typically dilates at a rate of 1.2 to 1.5 centimeters per hour. Multiparas, or women with a history of prior vaginal delivery, tend to demonstrate more rapid cervical dilation.[1] The absence of cervical change for greater than 4 hours in the presence of adequate contractions or six hours with inadequate contractions is considered the arrest of labor and may warrant clinical intervention.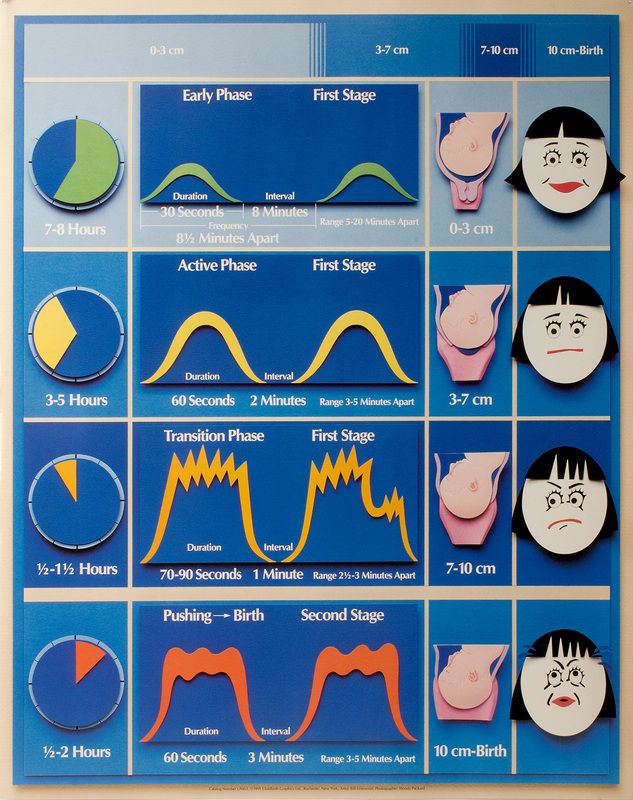 [7]
[7]
Second Stage of Labor
The second stage of labor commences with complete cervical dilation to 10 centimeters and ends with the delivery of the neonate. This was also defined as the pelvic division phase by Friedman. After cervical dilation is complete, the fetus descends into the vaginal canal with or without maternal pushing efforts. The fetus passes through the birth canal via 7 movements known as the cardinal movements. These include engagement, descent, flexion, internal rotation, extension, external rotation, and expulsion.[1] In women who have delivered vaginally previously, whose bodies have acclimated to delivering a fetus, the second stage may only require a brief trial, whereas a longer duration may be required for a nulliparous female. In parturients without neuraxial anesthesia, the second stage of labor typically lasts less than three hours in nulliparous women and less than two hours in multiparous women. In women who receive neuraxial anesthesia, the second stage of labor typically lasts less than four hours in nulliparous women and less than three hours in multiparous women.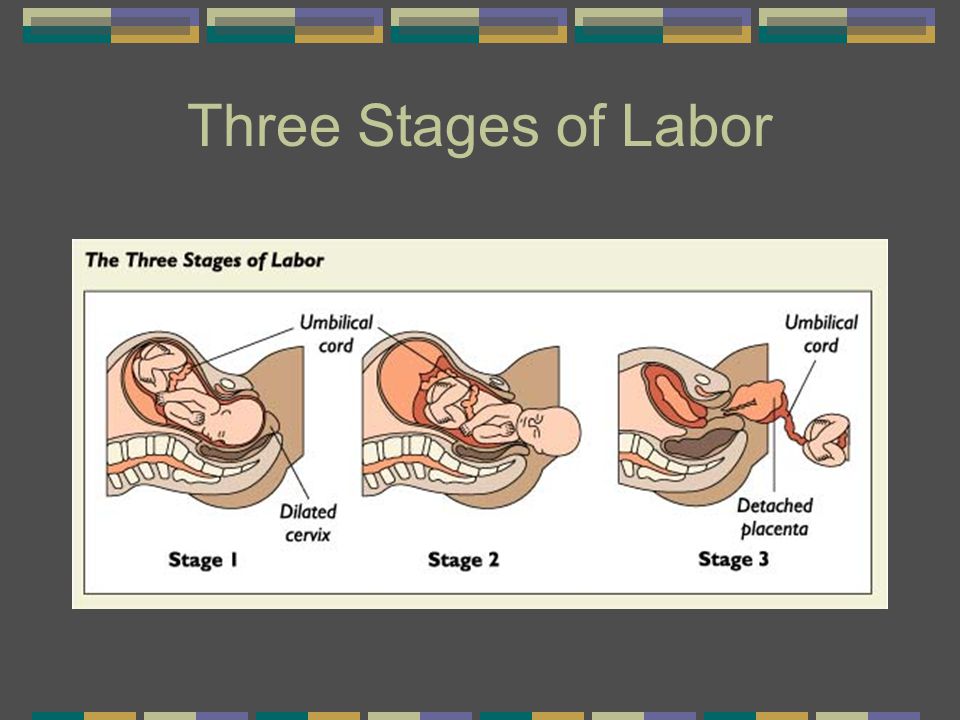 [1] If the second stage of labor lasts longer than these parameters, then the second stage is considered prolonged. Several elements may influence the duration of the second stage of labor, including fetal factors such as fetal size and position, or maternal factors such as pelvis shape, the magnitude of expulsive efforts, comorbidities such as hypertension or diabetes, age, and history of previous deliveries.[8]
[1] If the second stage of labor lasts longer than these parameters, then the second stage is considered prolonged. Several elements may influence the duration of the second stage of labor, including fetal factors such as fetal size and position, or maternal factors such as pelvis shape, the magnitude of expulsive efforts, comorbidities such as hypertension or diabetes, age, and history of previous deliveries.[8]
Third Stage of Labor
The third stage of labor commences when the fetus is delivered and concludes with the delivery of the placenta. Separation of the placenta from the uterine interface is hallmarked by three cardinal signs, including a gush of blood at the vagina, lengthening of the umbilical cord, and a globular shaped uterine fundus on palpation.[1] Spontaneous expulsion of the placenta typically takes between 5 to 30 minutes.[1] A delivery time of greater than 30 minutes is associated with a higher risk of postpartum hemorrhage and may be an indication for manual removal or other intervention. [1] Management of the third stage of labor involves placing traction on the umbilical cord with simultaneous fundal pressure to effect faster placental delivery.
[1] Management of the third stage of labor involves placing traction on the umbilical cord with simultaneous fundal pressure to effect faster placental delivery.
Function
The function of the stages of labor is to create a universal definition that medical professionals can use to communicate with each other about labor. The stages of labor can be used to help determine where the patient is on the labor spectrum. Clarifying the stages of labor has helped create guidelines, which define normal and abnormal trends in labor. Clinical management also gears toward the various stages of labor.
Issues of Concern
Complications may arise during any of the stages of labor to result in abnormal labor. During the first stage, women may experience the arrest of parturition, necessitating cesarian delivery, which may carry greater maternal or fetal risk. Second stage complications include a variety of complications related to the trauma of the delivery process to either the fetus or the mother. The fetus can suffer acidemia, shoulder dystocia, bony fractures, nerve palsies, scalp hematomas, and anoxic brain injuries. Similarly, the mother can develop a host of traumatic complications ranging from uterine rupture, vaginal laceration, cervical laceration, uterine hemorrhage, amniotic fluid embolism, and death. The third stage of labor may encounter complications from hemorrhage, cord avulsion, retained placenta, or incomplete removal of the placenta.[5]
The fetus can suffer acidemia, shoulder dystocia, bony fractures, nerve palsies, scalp hematomas, and anoxic brain injuries. Similarly, the mother can develop a host of traumatic complications ranging from uterine rupture, vaginal laceration, cervical laceration, uterine hemorrhage, amniotic fluid embolism, and death. The third stage of labor may encounter complications from hemorrhage, cord avulsion, retained placenta, or incomplete removal of the placenta.[5]
Clinical Significance
Defining the stages of labor with a specific beginning and end has allowed clinicians to study labor trends and to create labor curves. For example, in the 1950s, Dr. Friedman created a graphical representation of the rate of normal labor during latent and active labor using observed clinical data.[9] These, in turn, can be used to determine if a woman is progressing through labor as expected and helping to identify abnormal labor. Friedman observed that labor typically has a sigmoidal shape when measured by cervical dilation over time.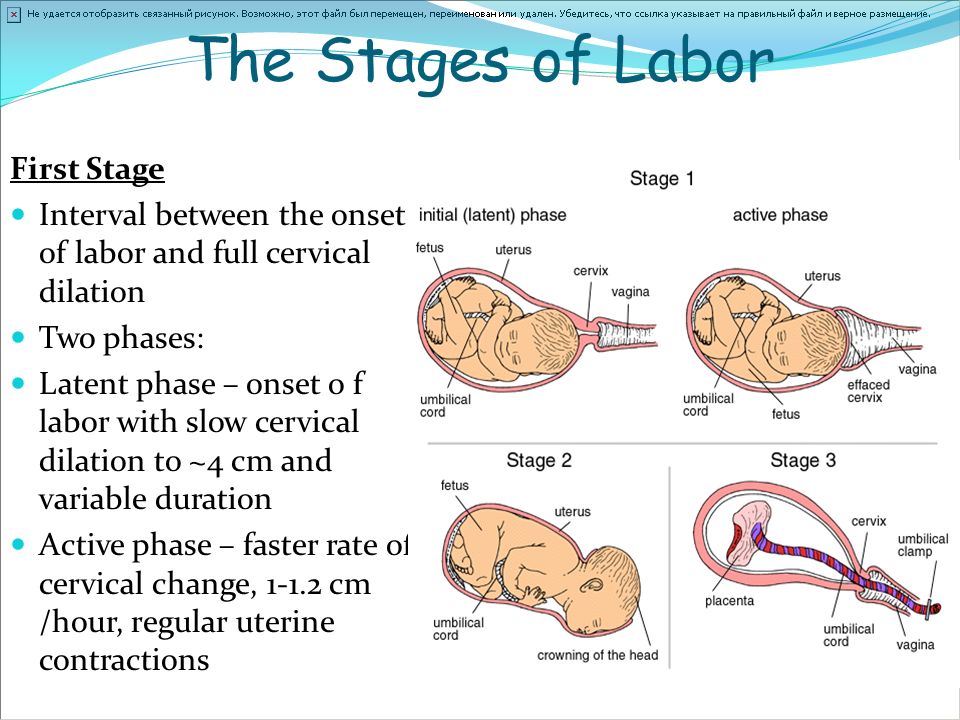 During the active phase of labor, cervical dilation occurs at a rate of 1 centimeter or more per hour. If dilation occurs much slower, the patient may be at risk for abnormal labor or arrest of labor.[10]
During the active phase of labor, cervical dilation occurs at a rate of 1 centimeter or more per hour. If dilation occurs much slower, the patient may be at risk for abnormal labor or arrest of labor.[10]
If a woman is found not progressing through the first stage of labor as expected, this could lead to the diagnosis of the arrest of dilation or descent, which could result in cesarean delivery. The findings of Dr. Friedman have recently been challenged, and the current consensus is the normal latent phase of labor lasts longer than was previously observed.[8] The criteria for the stages of labor create a universal language that allows healthcare professionals to communicate with one another about patient care accurately. Also, specific interventions are tailored to particular stages of labor to try to create better patient outcomes. For example, active management in the third stage of labor is carried out by placing immediate traction on the umbilical cord and administering intravenous oxytocin, which correlates with a lower risk of postpartum hemorrhage.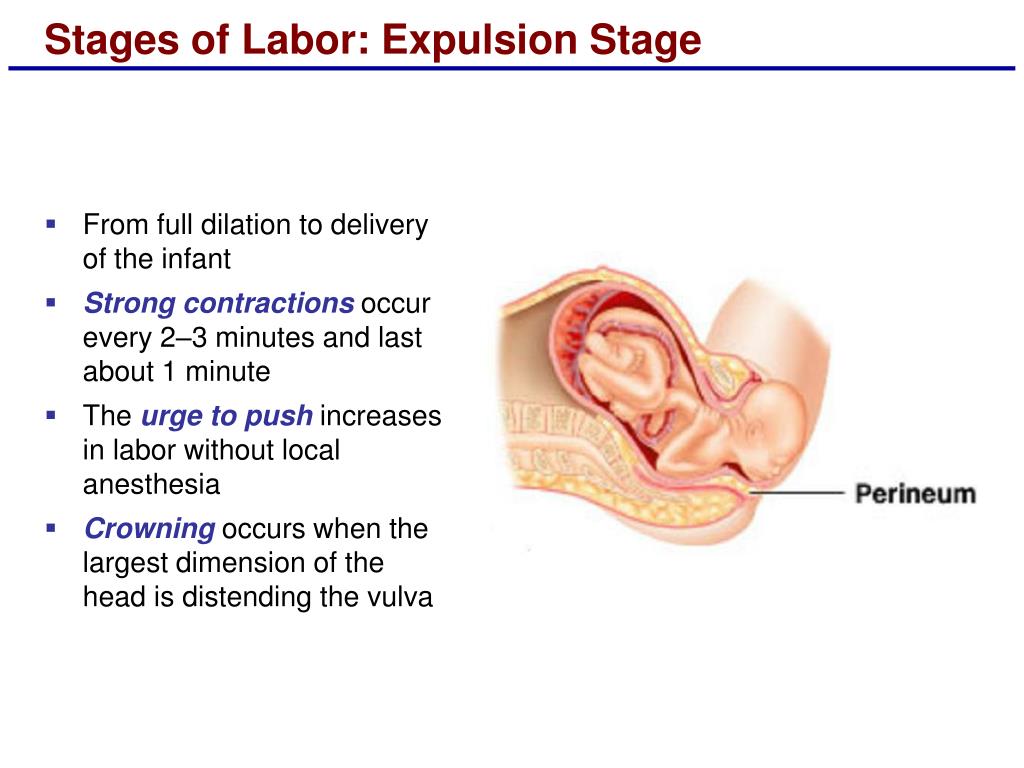 [11] Clinicians will continue to use the stages of labor to guide labor management and study labor patterns to improve patient care.
[11] Clinicians will continue to use the stages of labor to guide labor management and study labor patterns to improve patient care.
Enhancing Healthcare Team Outcomes
The stages of labor describe a complex physiologic process that starts when labor beings and ends with the delivery of the fetus and placenta. Labor is usually monitored clinically with multiple modalities by an interprofessional team. The process of labor can proceed as typically expected with certain cardinal events and time parameters or can encounter complications and delays, which may require identification and medical intervention.
The role of the interprofessional team in monitoring and caring for women during labor is critically important in keeping women safe and improving outcomes during the labor process.
A wide variety of medical professionals such as nurses, midwives, pharmacists, family physicians, anesthesiologists, and obstetrician/gynecologists may be involved in a woman’s labor process. Close communication is needed between these professionals to create an atmosphere of safety and patient-centered care. Midwives often manage labor and delivery and work closely with physicians when complications arise, requiring physician intervention, such as Caesarian section or operative delivery. Pharmacists ensure that patients receive the proper analgesics, tocolytics, and other medications that may be needed during or following labor. Anesthesiologists and nurse anesthetists administer epidurals for analgesia and are available for general endotracheal anesthesia when necessary. Nurses monitor the patient’s vital signs, contractions, cervical exams, pain scores, administer medications, recognize complications, and update the physician or midwife responsible for the patient. Each labor is unique, but an interprofessional approach prenatally and during labor can be used to improve patient outcomes and provide patient-centered care, as each provider class works collaboratively to ensure communication lines remain open between different disciplines on the health care team [Level 5]
Close communication is needed between these professionals to create an atmosphere of safety and patient-centered care. Midwives often manage labor and delivery and work closely with physicians when complications arise, requiring physician intervention, such as Caesarian section or operative delivery. Pharmacists ensure that patients receive the proper analgesics, tocolytics, and other medications that may be needed during or following labor. Anesthesiologists and nurse anesthetists administer epidurals for analgesia and are available for general endotracheal anesthesia when necessary. Nurses monitor the patient’s vital signs, contractions, cervical exams, pain scores, administer medications, recognize complications, and update the physician or midwife responsible for the patient. Each labor is unique, but an interprofessional approach prenatally and during labor can be used to improve patient outcomes and provide patient-centered care, as each provider class works collaboratively to ensure communication lines remain open between different disciplines on the health care team [Level 5]
A Canadian retrospective cohort study of 1238 women found that an interprofessional team approach to obstetrical care was shown to provide better patient outcomes by decreasing the rate of cesarian sections and length of hospital stays for women. [12] [Level 4]
[12] [Level 4]
Nursing, Allied Health, and Interprofessional Team Interventions
Nurses are intimately involved in monitoring and caring for laboring women. Nurses administer and titrate medications during labor, such as oxytocin. Nurses monitor the vital signs, pain scores, and labor progression of women and fetuses closely and are responsible for recognizing and then notifying physicians and midwives when abnormalities arise.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Liao JB, Buhimschi CS, Norwitz ER. Normal labor: mechanism and duration. Obstet Gynecol Clin North Am. 2005 Jun;32(2):145-64, vii. [PubMed: 15899352]
- 2.
van der Ham DP, van Melick MJ, Smits L, Nijhuis JG, Weiner CP, van Beek JH, Mol BW, Willekes C. Methods for the diagnosis of rupture of the fetal membranes in equivocal cases: a systematic review.
 Eur J Obstet Gynecol Reprod Biol. 2011 Aug;157(2):123-7. [PubMed: 21482018]
Eur J Obstet Gynecol Reprod Biol. 2011 Aug;157(2):123-7. [PubMed: 21482018]- 3.
ACOG Committee Opinion No. 766 Summary: Approaches to Limit Intervention During Labor and Birth. Obstet Gynecol. 2019 Feb;133(2):406-408. [PubMed: 30681540]
- 4.
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 209: Obstetric Analgesia and Anesthesia. Obstet Gynecol. 2019 Mar;133(3):e208-e225. [PubMed: 30801474]
- 5.
ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol. 2009 Aug;114(2 Pt 1):386-397. [PubMed: 19623003]
- 6.
Zhang J, Troendle J, Mikolajczyk R, Sundaram R, Beaver J, Fraser W. The natural history of the normal first stage of labor. Obstet Gynecol. 2010 Apr;115(4):705-710. [PubMed: 20308828]
- 7.
Zhang J, Landy HJ, Ware Branch D, Burkman R, Haberman S, Gregory KD, Hatjis CG, Ramirez MM, Bailit JL, Gonzalez-Quintero VH, Hibbard JU, Hoffman MK, Kominiarek M, Learman LA, Van Veldhuisen P, Troendle J, Reddy UM.
 , Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010 Dec;116(6):1281-1287. [PMC free article: PMC3660040] [PubMed: 21099592]
, Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010 Dec;116(6):1281-1287. [PMC free article: PMC3660040] [PubMed: 21099592]- 8.
Cheng YW, Caughey AB. Defining and Managing Normal and Abnormal Second Stage of Labor. Obstet Gynecol Clin North Am. 2017 Dec;44(4):547-566. [PubMed: 29078938]
- 9.
Pitkin RM. Friedman EA. Primigravid labor: a graphicostatistical analysis. Obstet Gynecol 1955;6:567-89. Obstet Gynecol. 2003 Feb;101(2):216. [PubMed: 12576240]
- 10.
Kilpatrick SJ, Laros RK. Characteristics of normal labor. Obstet Gynecol. 1989 Jul;74(1):85-7. [PubMed: 2733947]
- 11.
Güngördük K, Olgaç Y, Gülseren V, Kocaer M. Active management of the third stage of labor: A brief overview of key issues. Turk J Obstet Gynecol. 2018 Sep;15(3):188-192. [PMC free article: PMC6127474] [PubMed: 30202630]
- 12.
Harris SJ, Janssen PA, Saxell L, Carty EA, MacRae GS, Petersen KL.
 Effect of a collaborative interdisciplinary maternity care program on perinatal outcomes. CMAJ. 2012 Nov 20;184(17):1885-92. [PMC free article: PMC3503901] [PubMed: 22966055]
Effect of a collaborative interdisciplinary maternity care program on perinatal outcomes. CMAJ. 2012 Nov 20;184(17):1885-92. [PMC free article: PMC3503901] [PubMed: 22966055]
Second stage of labor
Second stage of childbirth – period of exile. It begins after the full disclosure of the cervix and ends with the birth of the baby. Duration of the period of exile in primiparous is 1-2 hours , in multiparous - 15-30 minutes . Here, in addition to strong contractions, contractions of the muscles of the abdominal wall, diaphragm and pelvic floor are added, and a feeling of pressure on the rectum - this condition is called pushing.
During the period of exile, the woman in labor is in the delivery room on a special bed, in a supine position with legs bent at the hip and knee joints. The head end of the bed is raised. In a semi-sitting position, the axis of the uterus and the axis of the small pelvis coincide, which improves the advancement of the head through the birth canal.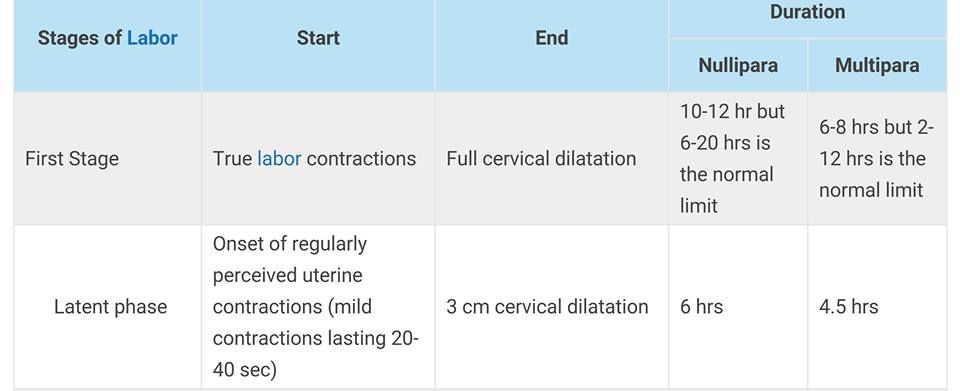 At the moment of an attempt, in order to strengthen it, the woman in labor holds on to the bed with her hands, and rests her feet on the stand. It is necessary to prepare a sterile package for the initial treatment of the newborn and a set of sterile linen - a blanket and 3 diapers heated to 40 * C. Treat the pubis, inner thighs, external genitalia, perineum. nine0019
At the moment of an attempt, in order to strengthen it, the woman in labor holds on to the bed with her hands, and rests her feet on the stand. It is necessary to prepare a sterile package for the initial treatment of the newborn and a set of sterile linen - a blanket and 3 diapers heated to 40 * C. Treat the pubis, inner thighs, external genitalia, perineum. nine0019
The average duration of each push is 10-15 seconds. Usually, during one contraction, a woman feels the need to push on average three times . And although at this point the contractions are the strongest, most women say that when attempts were added to the contractions, they became less painful. Attempts, unlike contractions, can be controlled - a woman can delay attempts or, conversely, intensify. If the doctor or midwife still forbids pushing, then the “dog-like” breathing technique will help to restrain the attempts. Usually the midwife says: “Don’t push, try to breathe!” Then you need to breathe superficially with short inhalations and exhalations. nine0019
nine0019
How to push correctly? With the onset of attempts, you should always listen to the doctor or midwife. If the midwife says: “Push!”, you need:
- At the moment when it is time to push, the woman in labor should take full lungs of air, taking a breath through her mouth and hold her breath, as before immersion in water, while the shoulders should be lowered down . You need to exhale very smoothly through a slightly open mouth. So you need to act until the end of the attempt. The most important thing is the movement of attempts and all the efforts of a woman should be directed to the perineum. nine0034
- During each contraction, you need to push three times.
3. You need to push smoothly, and between attempts - to rest and set yourself up for work.
Attempts are the main moment of childbirth the outcome of childbirth and the condition of the child depend on them. Therefore, even if the forces are no longer there, you need to gather your will into a fist and start pushing. Between contractions, it is very important to take deep, calm breaths. This will allow you to gain strength before the next fight and effectively carry out another attempt. In between attempts, the doctor will listen to the baby's heartbeat with a CTG sensor or an obstetric stethoscope. Pushing is hard and painful, but it is very important for the baby: at this moment it is also difficult for him, and only mother can help. nine0019
Between contractions, it is very important to take deep, calm breaths. This will allow you to gain strength before the next fight and effectively carry out another attempt. In between attempts, the doctor will listen to the baby's heartbeat with a CTG sensor or an obstetric stethoscope. Pushing is hard and painful, but it is very important for the baby: at this moment it is also difficult for him, and only mother can help. nine0019
If there is a possibility of perineal rupture during attempts, the doctor makes an incision in it - an episiotomy. As soon as the fetal head stops hiding in the pelvis, the midwife removes the newborn baby into the light.
Immediately after the head appears, it clears the child's airways and he screams for the first time. The baby is laid out on the mother's stomach, the baby takes its first breath and illuminates the delivery room with a long-awaited cry. At the same time, the midwife dries the baby's wet skin with a warm diaper, then the umbilical cord is cut, and the pediatrician assesses the baby's condition on the Apgar scale.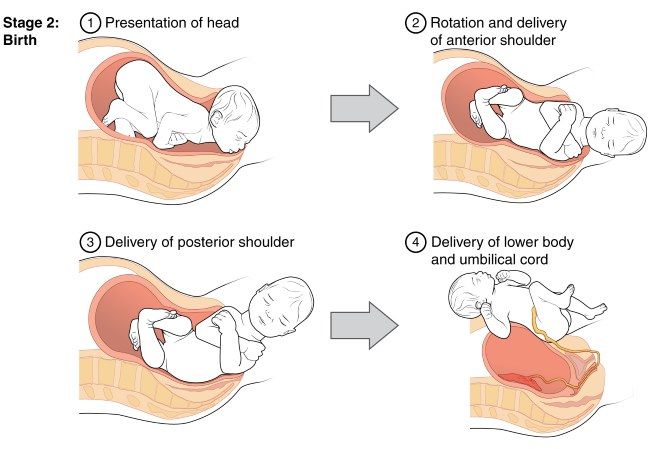 The baby is handed over to the mother and applied to the breast. So he warms up and adapts to the situation, and in the mother's body, the production of oxytocin begins, which starts the process of milk production and causes postpartum uterine contractions. It is in skin-to-skin contact with his mother that his acquaintance with the world begins. At this time, an invisible psycho-emotional connection arises between mother and child, which in the future will become the basis for the formation of attachment between them. The first 20 minutes after birth is a period of relaxation for the baby. During this period, he recuperates after hard work. After 20 minutes, the next phase begins - awakening. The baby begins to move, turns his head, opens his fists and makes attempts to crawl. With the beginning of motor activity, the first feeling of hunger comes to the baby. It is very important that the child finds and takes the breast at the moment of the search reflex. The baby begins to open his mouth, clenching and unclenching his palms, then he begins to crawl, raising his head and pushing off with his legs and elbows, towards his mother's chest.
The baby is handed over to the mother and applied to the breast. So he warms up and adapts to the situation, and in the mother's body, the production of oxytocin begins, which starts the process of milk production and causes postpartum uterine contractions. It is in skin-to-skin contact with his mother that his acquaintance with the world begins. At this time, an invisible psycho-emotional connection arises between mother and child, which in the future will become the basis for the formation of attachment between them. The first 20 minutes after birth is a period of relaxation for the baby. During this period, he recuperates after hard work. After 20 minutes, the next phase begins - awakening. The baby begins to move, turns his head, opens his fists and makes attempts to crawl. With the beginning of motor activity, the first feeling of hunger comes to the baby. It is very important that the child finds and takes the breast at the moment of the search reflex. The baby begins to open his mouth, clenching and unclenching his palms, then he begins to crawl, raising his head and pushing off with his legs and elbows, towards his mother's chest. nine0019
nine0019
In the second stage of labor - attempts and expulsion of the fetus, the partner's role is moral support : a woman in labor can simply be held by the hand, wipe sweat from her forehead and help to breathe correctly (at the doctor's command).
For the father of a child, partner delivery is an opportunity to help the beloved woman during childbirth, to see how the child is born and to take him in his arms. In this way, inextricable bonds are formed between all family members.
Important to know - St. Petersburg citizen's health
The total duration of labor and its course
The total duration of labor depends on many factors: age, physique and physical condition of the woman, her psychological attitude, the speed of cervical dilatation, first or second pregnancy, size of the child, type of presentation and row other moments.
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).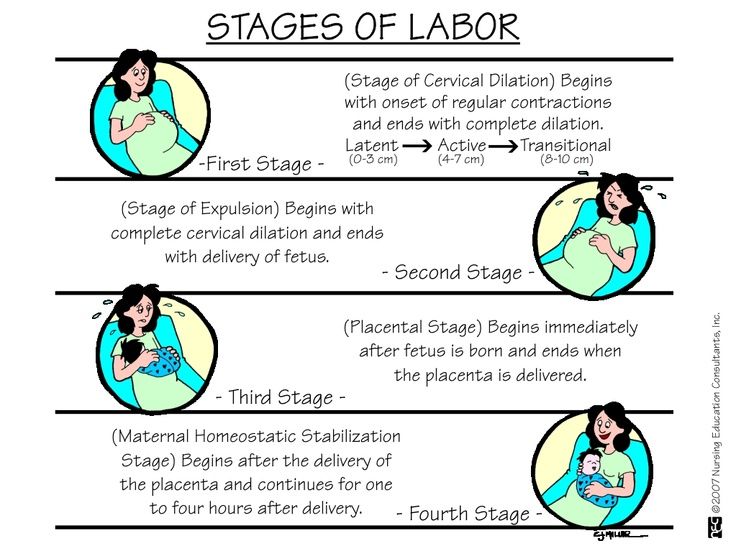 nine0019
nine0019
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent.
The dilation period is the time elapsed from the onset of regular contractions until the cervix is fully dilated. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations. nine0019
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm.
3. Transitional (transient) phase, or deceleration phase (lasts from 40 minutes to 2 hours, may be absent in multiparous women). This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process.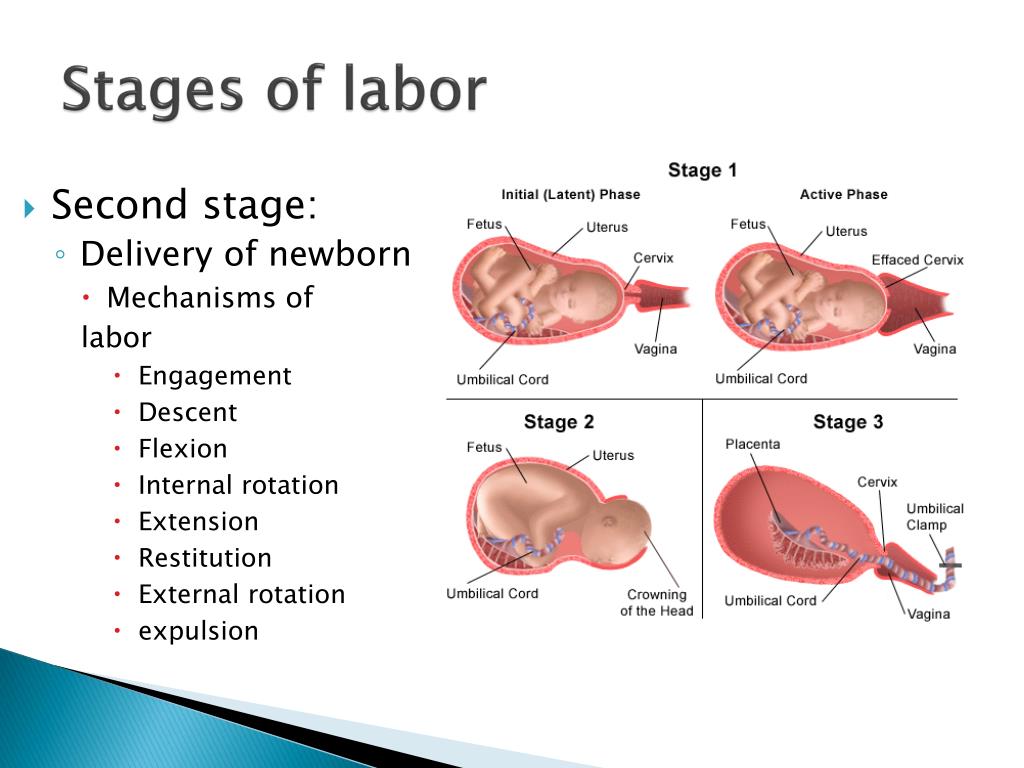 Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because in a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts. nine0019
The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts. nine0019
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
During one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant. nine0019
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta.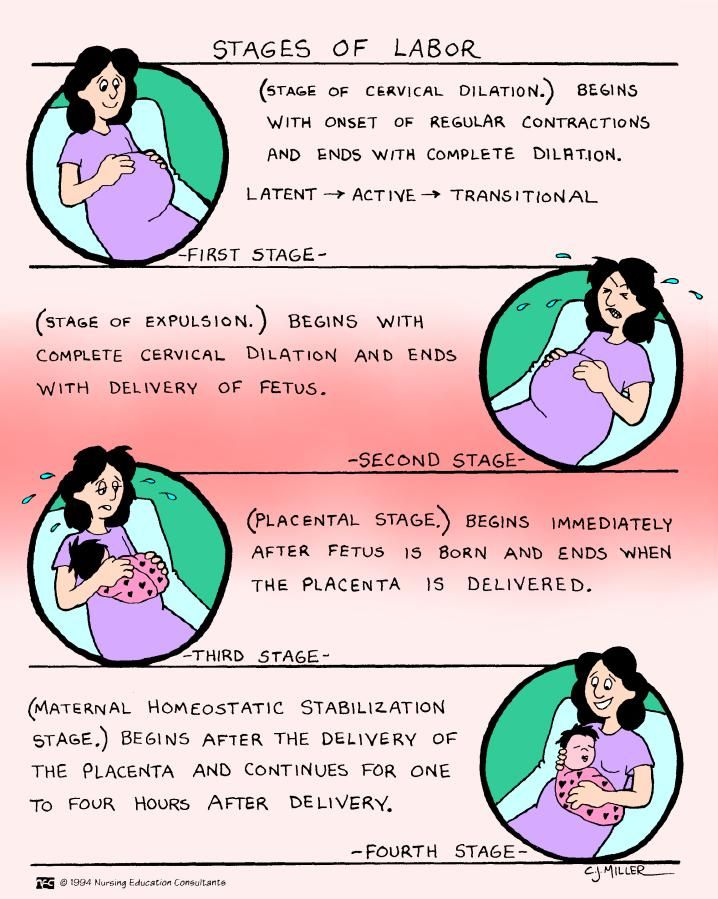 During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel. nine0019
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).