Salt in food for babies
How Much Should They Eat?
If you’re a new parent, you may be wondering how much salt is OK to include in your baby’s diet.
While salt is a compound that all humans need in their diets, babies shouldn’t get too much of it because their developing kidneys aren’t yet able to process large amounts of it.
Giving your baby too much salt over time may cause health problems, such as high blood pressure. In extreme and rare cases, a baby that’s had a large amount of salt may even end up in the emergency room.
Too much salt during infancy and childhood may also promote a lifelong preference for salty foods.
This article explains what you need to know about salt and babies, including how much salt is safe, and how to tell whether your baby has had too much salt.
You may add salt to your baby’s food in hopes that it’ll improve the taste and encourage your baby to eat.
If you use a baby-led weaning approach to feeding your baby, you may end up serving your baby foods containing more salt simply because you’re serving them the saltier foods you eat as an adult (1, 2).
However, babies who get too much salt through their diets can run into a few issues.
A baby’s kidneys are still immature, and they aren’t able to filter out excess salt as efficiently as adult kidneys. As a result, a diet that’s too rich in salt may damage a baby’s kidneys. A salt-rich diet may also affect a baby’s long-term health and taste preferences (3, 4).
Babies are born with a natural preference for sweet, salty, and umami-tasting foods (1, 4, 5).
Repeatedly being offered salty foods may reinforce this natural taste preference, possibly causing your child to prefer salty foods over those that are naturally less salty.
Processed foods, which tend to be salty but not typically rich in nutrients, may be preferred over whole foods with naturally lower salt contents, such as vegetables (4, 6, 7, 8, 9).
Finally, salt-rich diets may cause your baby’s blood pressure to rise. Research suggests that the blood-pressure-raising effect of salt may be stronger in babies than it is in adults (3).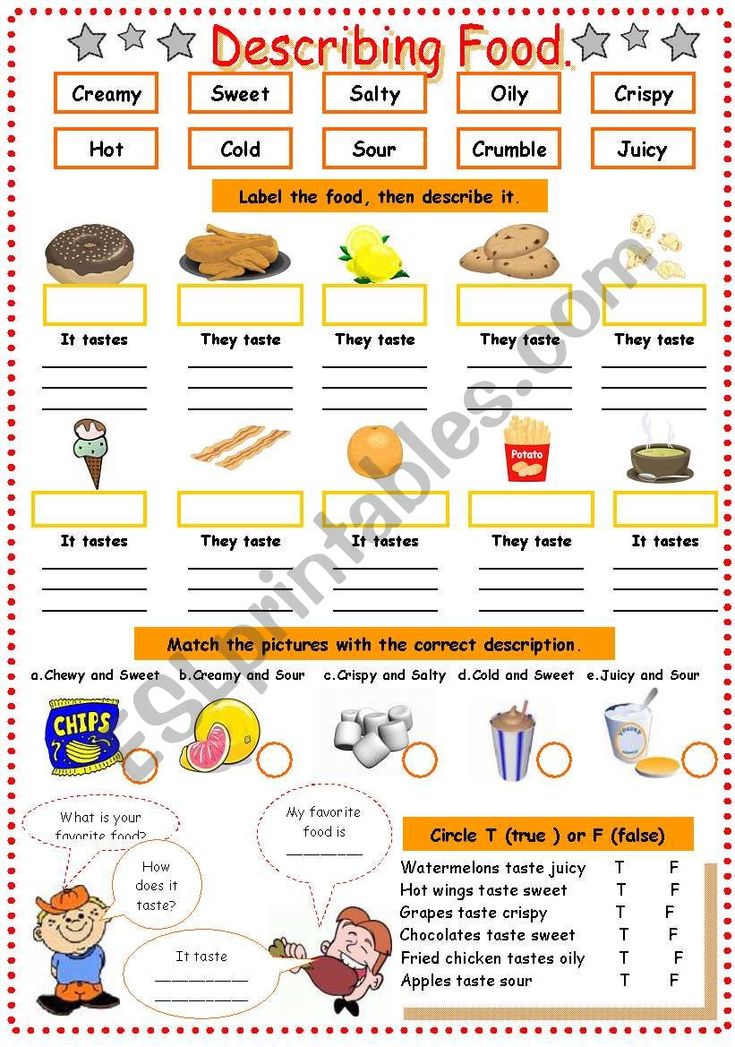
As a result, babies fed a salt-rich diet tend to have higher blood pressure levels during childhood and adolescence, which may increase their risk of heart disease later in life (10, 11).
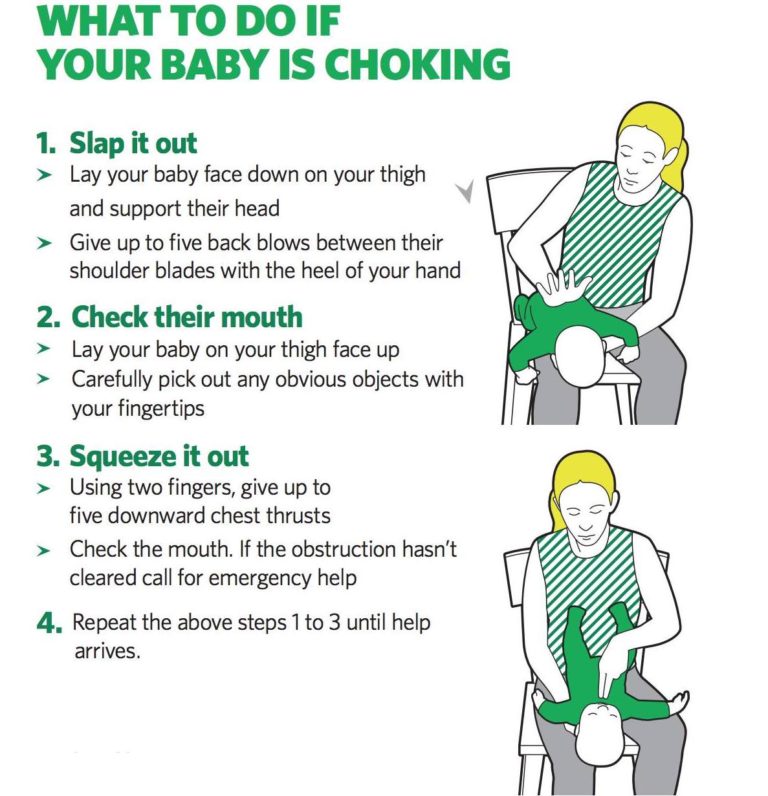
In extreme cases, very high intakes of salt can require emergency medical care, and in some cases, even lead to death. However, this is rare and usually results from a baby accidentally eating a quantity of salt much larger than parents would normally add to foods (12).
SummaryToo much salt can damage a baby’s kidneys, increase their blood pressure, and possibly raise their risk of heart disease later in life. A salt-rich diet may also cause your child to develop a lasting preference for salty foods.
Sodium, the main component in table salt, is an essential nutrient. Everyone, including babies, need small amounts of it to function properly.
Young babies under 6 months of age meet their daily sodium requirements from breast milk and formula alone.
Those 7–12-months-old are able to meet their needs from breastmilk or formula and the small amounts of sodium naturally present in unprocessed complementary foods.
As such, experts recommend that you don’t add salt to your baby’s food during their first 12 months (2, 4, 5).
Having an occasional meal with salt added is OK. You may sometimes feed your baby some packaged or processed foods with salt added or let them try a meal from your plate. That said, overall, try not to add salt to the foods you prepare for your baby.
After 1 year of age, recommendations vary slightly. For instance, the European Food Safety Authority (EFSA) considers 1,100 mg of sodium per day — about half a teaspoon (2.8 grams) of table salt — safe and adequate for children of 1–3 years (13).
In the United States, recommendations for the same age group average 800 mg of sodium per day. That’s about 0.4 teaspoons (2 grams) of table salt per day (14).
SummaryBabies under 12 months should not get any additional salt through their diet.
Intakes between 0.4–0.5 teaspoons of salt appear safe in children up to 4 years old.
If your baby eats a meal that’s too salty, they may seem thirstier than usual. Typically, you won’t notice the effects of a high salt diet immediately, but rather over time.
In extremely rare cases, a baby that’s eaten too much salt can develop hypernatremia — a condition in which there’s too much sodium circulating in the blood.
If left untreated, hypernatremia can cause babies to progress from feeling irritable and agitated to drowsy, lethargic, and eventually unresponsive after some time. In severe cases, hypernatremia can result in coma and even death (15).
Milder forms of hypernatremia can be more difficult to spot in babies. Signs that your baby may have a mild form of hypernatremia include extreme thirst and a doughy or velvety texture to the skin.
Very young babies may start crying in a high pitched fashion if they’ve accidentally eaten too much salt.
If you think that your baby may have gotten into too much salt or is beginning to show signs of hypernatremia, call your pediatrician.
SummaryIf a baby has a salty meal occasionally, you may notice they are thirsty. In extremely rare cases, babies who have ingested large amounts of salt may develop hypernatremia and require medical attention.
As a parent, you can limit the amount of salt your baby eats in several ways.
Most baby food purées may contain small amounts of naturally occurring sodium from the foods they are made with but very little, if any, added salt. If your baby is currently eating them exclusively, they’re unlikely to ingest too much salt.
If you make your own baby food, skip adding salt, choose fresh foods, and check labels on frozen or canned vegetables and fruits to find lower sodium options.
Also, remember to rinse canned foods, such as beans, lentils, peas, and vegetables, before adding them to purées or meals. Doing so helps reduce their sodium content (16).
Doing so helps reduce their sodium content (16).
If you’re doing baby-led weaning, you can set aside a portion of meals for baby before adding salt or make family meals with spices and herbs instead of salt.
Check the sodium content of foods you frequently buy, such as bread, cereal, and sauces. Lower sodium versions are available for most packaged foods, and comparing labels can help you find a brand with less salt added.
Frozen meals, as well as takeout or restaurant foods, are generally higher in salt. Occasionally, it’s fine for baby to have these meals, but when dining out, a lower salt alternative would be to bring a few foods from home for your baby.
SummaryYou can minimize the amount of sodium your baby eats by offering them foods without added salt. Replacing pantry foods like bread and sauces with low sodium alternatives can also help.
Babies need small amounts of salt in their diet. However, their bodies can’t handle large amounts. Babies fed too much salt may be at risk of kidney damage, high blood pressure, and possibly even an increased risk of heart disease.
Babies fed too much salt may be at risk of kidney damage, high blood pressure, and possibly even an increased risk of heart disease.
Moreover, a salt-rich diet may cause babies to develop a lifelong preference for salty foods, in turn, possibly lowering the overall quality of their diet.
Try not to add salt to your baby’s foods when they are under 12 months. After 1 year, you can include a small amount of salt in your child’s diet.
Just one thing
When cooking a family-style meal, get into the habit of adding salt near the end of cooking. This way, you can reserve a no-salt-added portion for your baby.
How Much Should They Eat?
If you’re a new parent, you may be wondering how much salt is OK to include in your baby’s diet.
While salt is a compound that all humans need in their diets, babies shouldn’t get too much of it because their developing kidneys aren’t yet able to process large amounts of it.
Giving your baby too much salt over time may cause health problems, such as high blood pressure.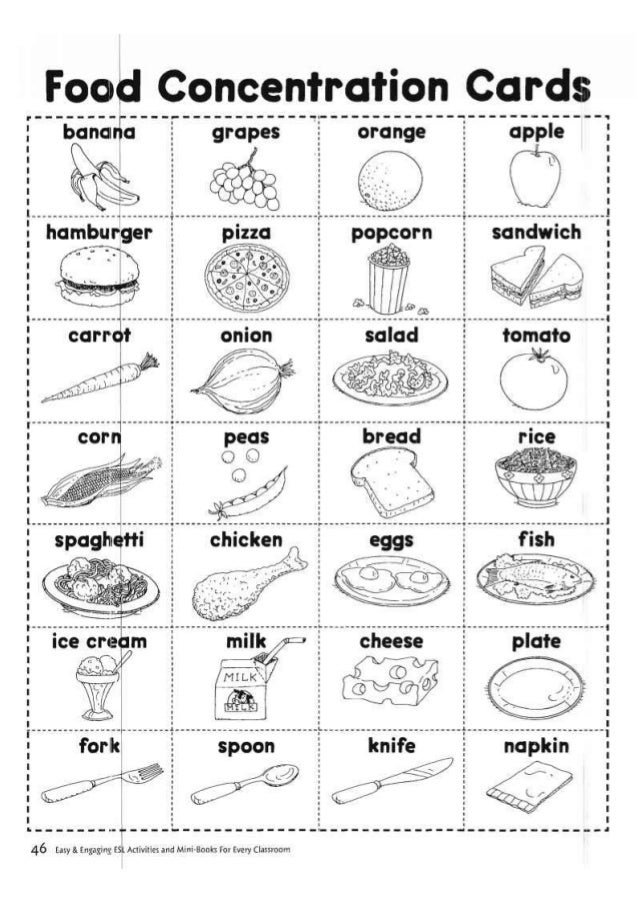 In extreme and rare cases, a baby that’s had a large amount of salt may even end up in the emergency room.
In extreme and rare cases, a baby that’s had a large amount of salt may even end up in the emergency room.
Too much salt during infancy and childhood may also promote a lifelong preference for salty foods.
This article explains what you need to know about salt and babies, including how much salt is safe, and how to tell whether your baby has had too much salt.
You may add salt to your baby’s food in hopes that it’ll improve the taste and encourage your baby to eat.
If you use a baby-led weaning approach to feeding your baby, you may end up serving your baby foods containing more salt simply because you’re serving them the saltier foods you eat as an adult (1, 2).
However, babies who get too much salt through their diets can run into a few issues.
A baby’s kidneys are still immature, and they aren’t able to filter out excess salt as efficiently as adult kidneys. As a result, a diet that’s too rich in salt may damage a baby’s kidneys. A salt-rich diet may also affect a baby’s long-term health and taste preferences (3, 4).
Babies are born with a natural preference for sweet, salty, and umami-tasting foods (1, 4, 5).
Repeatedly being offered salty foods may reinforce this natural taste preference, possibly causing your child to prefer salty foods over those that are naturally less salty.
Processed foods, which tend to be salty but not typically rich in nutrients, may be preferred over whole foods with naturally lower salt contents, such as vegetables (4, 6, 7, 8, 9).
Finally, salt-rich diets may cause your baby’s blood pressure to rise. Research suggests that the blood-pressure-raising effect of salt may be stronger in babies than it is in adults (3).
As a result, babies fed a salt-rich diet tend to have higher blood pressure levels during childhood and adolescence, which may increase their risk of heart disease later in life (10, 11).
In extreme cases, very high intakes of salt can require emergency medical care, and in some cases, even lead to death. However, this is rare and usually results from a baby accidentally eating a quantity of salt much larger than parents would normally add to foods (12).
SummaryToo much salt can damage a baby’s kidneys, increase their blood pressure, and possibly raise their risk of heart disease later in life. A salt-rich diet may also cause your child to develop a lasting preference for salty foods.
Sodium, the main component in table salt, is an essential nutrient. Everyone, including babies, need small amounts of it to function properly.
Young babies under 6 months of age meet their daily sodium requirements from breast milk and formula alone.
Those 7–12-months-old are able to meet their needs from breastmilk or formula and the small amounts of sodium naturally present in unprocessed complementary foods.
As such, experts recommend that you don’t add salt to your baby’s food during their first 12 months (2, 4, 5).
Having an occasional meal with salt added is OK. You may sometimes feed your baby some packaged or processed foods with salt added or let them try a meal from your plate.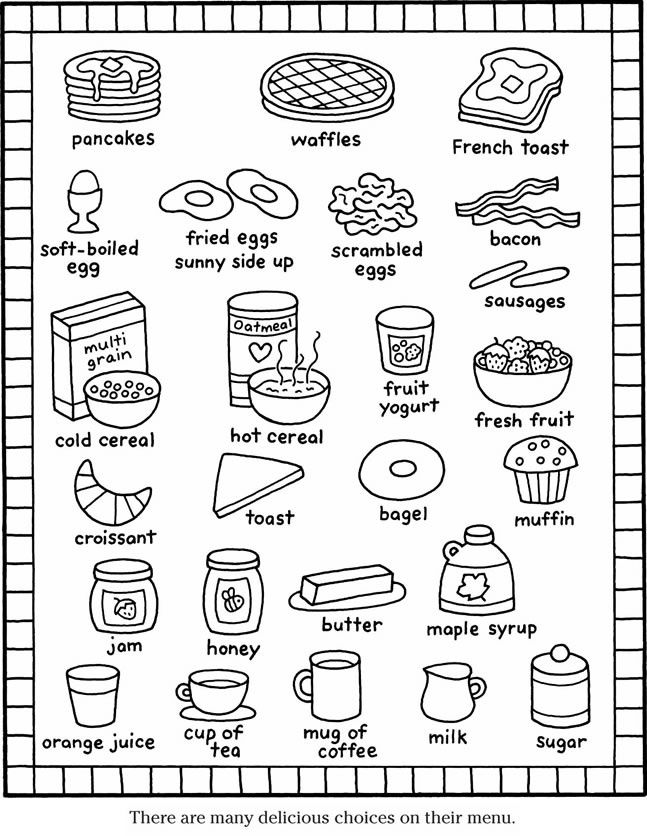 That said, overall, try not to add salt to the foods you prepare for your baby.
That said, overall, try not to add salt to the foods you prepare for your baby.
After 1 year of age, recommendations vary slightly. For instance, the European Food Safety Authority (EFSA) considers 1,100 mg of sodium per day — about half a teaspoon (2.8 grams) of table salt — safe and adequate for children of 1–3 years (13).
In the United States, recommendations for the same age group average 800 mg of sodium per day. That’s about 0.4 teaspoons (2 grams) of table salt per day (14).
SummaryBabies under 12 months should not get any additional salt through their diet. Intakes between 0.4–0.5 teaspoons of salt appear safe in children up to 4 years old.
If your baby eats a meal that’s too salty, they may seem thirstier than usual. Typically, you won’t notice the effects of a high salt diet immediately, but rather over time.
In extremely rare cases, a baby that’s eaten too much salt can develop hypernatremia — a condition in which there’s too much sodium circulating in the blood.
If left untreated, hypernatremia can cause babies to progress from feeling irritable and agitated to drowsy, lethargic, and eventually unresponsive after some time. In severe cases, hypernatremia can result in coma and even death (15).
Milder forms of hypernatremia can be more difficult to spot in babies. Signs that your baby may have a mild form of hypernatremia include extreme thirst and a doughy or velvety texture to the skin.
Very young babies may start crying in a high pitched fashion if they’ve accidentally eaten too much salt.
If you think that your baby may have gotten into too much salt or is beginning to show signs of hypernatremia, call your pediatrician.
SummaryIf a baby has a salty meal occasionally, you may notice they are thirsty. In extremely rare cases, babies who have ingested large amounts of salt may develop hypernatremia and require medical attention.
As a parent, you can limit the amount of salt your baby eats in several ways.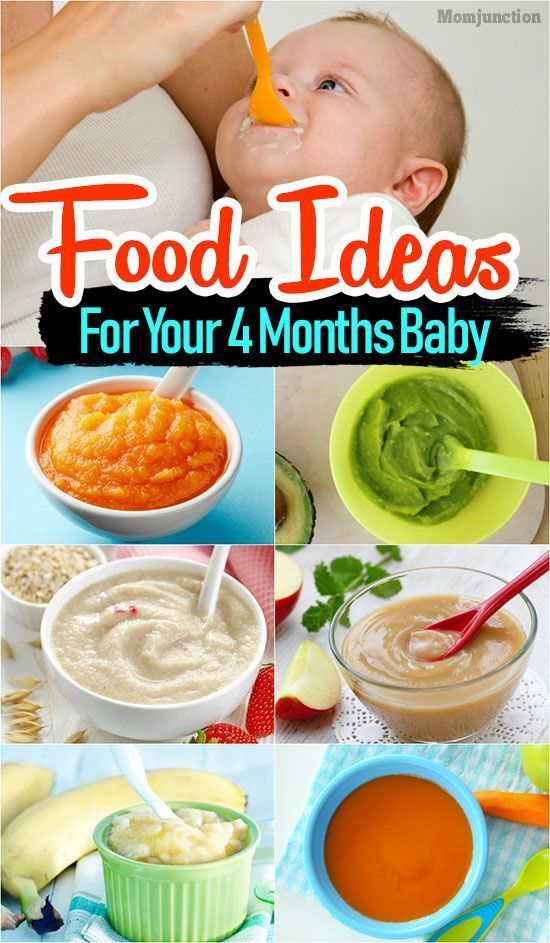
Most baby food purées may contain small amounts of naturally occurring sodium from the foods they are made with but very little, if any, added salt. If your baby is currently eating them exclusively, they’re unlikely to ingest too much salt.
If you make your own baby food, skip adding salt, choose fresh foods, and check labels on frozen or canned vegetables and fruits to find lower sodium options.
Also, remember to rinse canned foods, such as beans, lentils, peas, and vegetables, before adding them to purées or meals. Doing so helps reduce their sodium content (16).
If you’re doing baby-led weaning, you can set aside a portion of meals for baby before adding salt or make family meals with spices and herbs instead of salt.
Check the sodium content of foods you frequently buy, such as bread, cereal, and sauces. Lower sodium versions are available for most packaged foods, and comparing labels can help you find a brand with less salt added.
Frozen meals, as well as takeout or restaurant foods, are generally higher in salt. Occasionally, it’s fine for baby to have these meals, but when dining out, a lower salt alternative would be to bring a few foods from home for your baby.
Occasionally, it’s fine for baby to have these meals, but when dining out, a lower salt alternative would be to bring a few foods from home for your baby.
SummaryYou can minimize the amount of sodium your baby eats by offering them foods without added salt. Replacing pantry foods like bread and sauces with low sodium alternatives can also help.
Babies need small amounts of salt in their diet. However, their bodies can’t handle large amounts. Babies fed too much salt may be at risk of kidney damage, high blood pressure, and possibly even an increased risk of heart disease.
Moreover, a salt-rich diet may cause babies to develop a lifelong preference for salty foods, in turn, possibly lowering the overall quality of their diet.
Try not to add salt to your baby’s foods when they are under 12 months. After 1 year, you can include a small amount of salt in your child’s diet.
Just one thing
When cooking a family-style meal, get into the habit of adding salt near the end of cooking. This way, you can reserve a no-salt-added portion for your baby.
This way, you can reserve a no-salt-added portion for your baby.
Salt for children: benefits and harms
Salt is one of the most ancient and popular food additives to this day. About whether it is necessary to introduce it into the child's diet, what are the benefits and possible harm of salt for the child's body, read this article.
Salt is an irreplaceable source of useful trace elements
Sodium chloride, which is the main element in the composition of table salt, plays an important role in ensuring the correct functioning of various body systems, including the body of a child. For example, salt components (sodium, chlorine) contribute to the elimination of toxins, the absorption of a number of micronutrients, the normal metabolic process, water-salt metabolism, the proper functioning of the heart muscle, and neuromuscular endings. The use of salt by ninety percent covers the deficiency of chlorine in the body. nine0003
With insufficient salt intake, the child may complain of a constant desire to sleep, lethargy, loss of strength, deterioration in general well-being. Perhaps the occurrence of apathy, the disappearance of appetite. Toddlers may suffer from cramps and muscle pain. Thus, salt is a necessary element in the diet of a child, but it must be consumed based on age norms, since an excess of sodium chloride also threatens with negative health consequences.
Perhaps the occurrence of apathy, the disappearance of appetite. Toddlers may suffer from cramps and muscle pain. Thus, salt is a necessary element in the diet of a child, but it must be consumed based on age norms, since an excess of sodium chloride also threatens with negative health consequences.
Salt guidelines for children
Most pediatricians and nutritionists tend to believe that babies under the age of one and a half years do not feel the need to use salt as a dietary supplement, that is, they do not need to add salt to food. Children receive all the necessary amount of useful elements (for example, sodium) from their mother's breast milk and milk formula if the child is formula-fed, as well as from cereals, vegetables and fruits, meat, dairy products during the introduction of complementary foods. For adults, such food may seem insipid and tasteless, but the “unspoiled” receptors of the child perceive it quite normally, so parents should not reach for the salt shaker to enhance the taste of children's dishes. nine0003
nine0003
You can start adding salt to babies after they reach one and a half years of age, while monitoring the daily amount of salt that the child consumes. Children aged one to three years should not eat more than 0.5 grams of salt per day, three to six years old - more than one gram, six to eleven years old - more than three grams, over eleven years old - no more than five grams of salt should be consumed. It must be borne in mind that the norms are indicated taking into account the amount of salt contained in breast milk, formula and foods that the child eats during the day. nine0003
What threatens the excess of salt intake
With excessive intake of salt in the child's body, there is a violation of the normal functioning of the kidneys and pancreas (which are especially sensitive at an early age), the nervous and endocrine systems, and the thermoregulation system. The formation of salt deposits in the joints begins, the load on the heart increases, the risk of developing hypertension increases, and disturbances in water-salt metabolism occur.
Symptoms of an excessive amount of salt in the body of a child are the presence of swelling of the face, eyelids in the morning, complaints of headaches, whims for no apparent reason and irritability, a decrease in the number of urination, and an increase in blood pressure.
Which salt to choose
Now on the shelves of shops there are many types of salt. For use in baby food, rock (table, table salt) is recommended, which can be of various grinding. Refined and black Himalayan salt are not suitable for a children's menu. Iodized (with the addition of iodine-containing components) can be included in the child's diet after consultation with a pediatrician. The use of sea salt is acceptable in baby food after the child reaches the age of five years. Pink Himalayan salt, according to manufacturers, is distinguished by its natural purity and healing effect, however, experts differ on the possibility of using it for food by children. nine0003
Is it necessary to salt baby food
Reviewer Kovtun Tatyana Anatolievna
12200 views nine0003
The salt we use every day in cooking is called sodium chloride.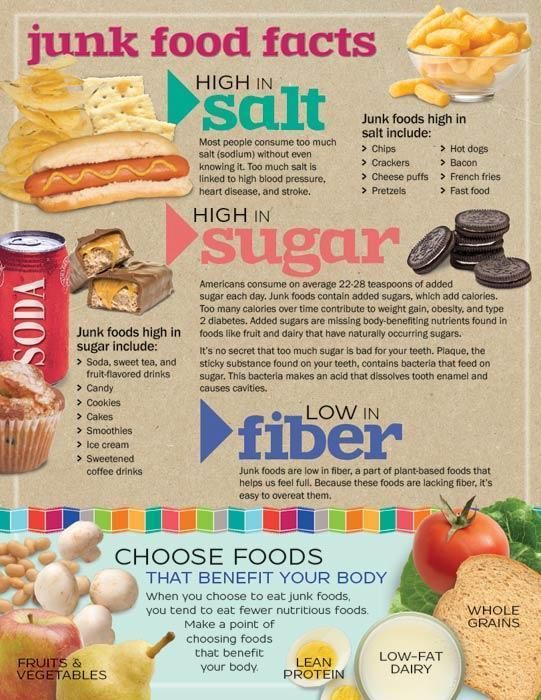 But if we talk about salt from the point of view of the human diet, then it makes sense to consider two elements, chlorine and sodium
But if we talk about salt from the point of view of the human diet, then it makes sense to consider two elements, chlorine and sodium
Sodium and chlorine ions play an enormous role in the human body - they maintain homeostasis (the constancy of the internal environment of the body), the level of fluid concentration inside and outside the cells necessary for normal life, ensure the normal permeability of the membrane of each cell in the body, participate in the conduction of electrical impulses in cells and perform a number of other physiological functions. nine0003
But do not immediately reach for the salt shaker.
Firstly, salt in its natural form can be obtained from many products, and secondly, there are strict restrictions on salt intake, and if they are not observed, then you can harm the body.
After all, a number of important mechanisms (renal, adrenal, vascular, etc.) are responsible for maintaining the balance of sodium and chlorine ions in the body, which, with excessive intake of salt from food, can experience excessive stress, and some systems can even fail.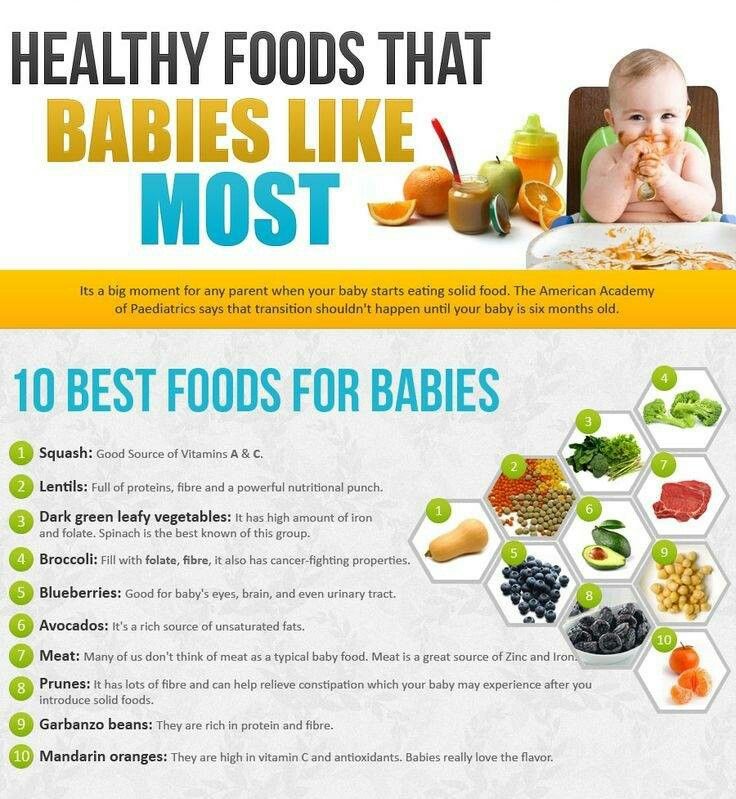 nine0003
nine0003
Today we will talk about the “salt” subtleties.
To salt or not to salt - that is the question
As for children, experts are unanimous in their opinion: infants do not need salt "from the outside" at all. Nature made sure that there was enough of it in mother's milk. By the way, it is equally important that mommy does not lean heavily on salty food.
And if the baby is bottle-fed, then the principle is the same - the balance of all the necessary elements has already been observed in the mixtures. nine0003
Salt can only be administered after breastfeeding or artificial feeding is completed, usually this happens at 1 or 1.5 years old. The baby will receive a third of the daily intake of sodium and chlorine "naturally" - from vegetables, fruits, cereals, meat and fish.
- Here are some foods from the high sodium diet for children:
- egg
- sardine
- cottage cheese
- kefir nine0065 tomatoes
- oats
- apples
- carrots
- And foods that are rich in chlorine :
- beef
- rice
- buckwheat
- egg white
But the remaining two-thirds of the norm for the baby can be obtained with the help of table salt. The rules of "pinch" or "tip of a knife" do not work very well here - these are not perfect measures of measurement. The only thing that parents should be guided by is that children's food should a priori seem unsalted and fresh for an "adult" taste. nine0003
The rules of "pinch" or "tip of a knife" do not work very well here - these are not perfect measures of measurement. The only thing that parents should be guided by is that children's food should a priori seem unsalted and fresh for an "adult" taste. nine0003
Additional salting of industrial products for children 1–3 years old is prohibited. Children's "salt norm" per day is about 0.5 g per 10 kg of body weight.
What happens if you add too much salt to baby food
The urinary system of the baby will hardly get rid of the excess of this mineral. The load on fragile kidneys, pancreas, blood vessels will increase, and disturbances in water-salt metabolism are also possible.
Alarming signals for parents can be the presence of edema in the child, unreasonable anxiety of the crumbs and a decrease in the number of urination.
What kind of salt to choose for the baby
In baby food, it is recommended to use regular table salt. Black, Himalayan pink or sea salt is not suitable for crumbs.