Help for engorged breasts
Engorgement | WIC Breastfeeding Support
It's normal for your breasts to feel different after your baby is born. They are making milk and have extra blood flow, so they may feel tender and full. But if your breasts are warm, hard, and painful, they may be too full of milk, or engorged. If you think your breasts are engorged, speak with your WIC breastfeeding staff.
Causes of Engorgement
Engorgement happens when milk isn't fully removed from your breast. It can happen any time, but it's most likely to happen:
- As your milk transitions from colostrum to mature milk.
- If there are sudden changes in how often you nurse, such as skipping a few feedings or pumping sessions.
Signs of Engorgement
If your breasts are engorged, they may be hard, full, warm, tender, and painful, and you may have a low-grade fever. It may also be hard for your baby to latch.
Preventing Engorgement
Engorgement is uncomfortable, and it can lead to other issues like plugged ducts or a breast infection. It also can slow or lower your milk supply, because your body is not getting the message to make more milk. Breastfeeding or expressing milk every 2-3 hours and taking good care of yourself can help prevent engorgement.
Breastfeed Often
- Breastfeed your baby often in the early weeks, 8-12 times in 24 hours.
- Make sure your baby latches well to ensure baby can remove milk effectively.
- Consider avoiding pacifiers and other artificial nipples until you and baby are comfortable and breastfeeding is going well. That will help regulate your milk supply.
- If you are going back to work or school, express milk frequently and at regular intervals while you and baby are apart.
Take Care of Yourself
- Eat well, drink plenty of fluids (especially water), and get enough sleep.
Relief for Engorgement
For most moms, engorgement usually goes away in a few days with these tips:
- Breastfeed first from the engorged breast.
- Before feedings, encourage your milk flow. Put a warm, moist washcloth on your breasts or take a warm shower for 10-20 minutes.
- Massage your breasts before and during feedings, moving from the chest wall to the nipple.
- If your breast is hard, hand express or pump a little milk before nursing. That will soften your breast and make it easier for your baby to latch. Be sure to only express enough milk to soften your breasts or provide comfort. If you express too much milk, you may encourage milk production and keep getting engorged.
- Between feedings, put cold compresses on your breasts to help reduce swelling and pain.
Oversupply of Milk
Some moms make more milk than their baby needs. This is called oversupply. It can cause frequent engorgement and fast milk flow. It can make it hard for your baby to nurse. If you think you might be making too much milk, talk to your doctor or your WIC breastfeeding expert.
If you think you might be making too much milk, talk to your doctor or your WIC breastfeeding expert.
Where to Find Help
Your local WIC breastfeeding staff can help you relieve engorgement. They can also give you tips to prevent it.
Complete Guide to Breast Engorgement Relief
Engorgement is common among breastfeeding mothers and can be very uncomfortable, but there are simple solutions that can help relieve the soreness. Learn what causes engorgement, symptoms, treatment, and how to prevent it from happening again.
Share this content
Engorged Breasts - Causes, Symptoms, Treatment, and Prevention
Engorgement is common among breastfeeding mothers, but there are simple solutions that can help relieve the soreness. If you recognize engorgement early and follow these steps for treating engorged breasts, your discomfort could subside in as little as 24 – 48 hours.
What Causes Engorged Breasts?
If you haven't experienced engorgement, it's a good idea to be prepared in case you eventually encounter this common breastfeeding challenge. Engorged breasts are the result of increased milk production, blood flow, and lymph fluids to the breasts after childbirth, all of which makes them feel full, hard, and even uncomfortable.
Engorged breasts are the result of increased milk production, blood flow, and lymph fluids to the breasts after childbirth, all of which makes them feel full, hard, and even uncomfortable.
It's not uncommon to experience engorgement within the first week after giving birth. You might also experience it when your baby's feeding pattern changes, such as when starting solid foods and demanding fewer feedings.
Breast engorgement can also be caused by any of the following situations:
- Skipping a breastfeeding session and not pumping
- Breast milk oversupply
- Waiting too long between nursing and/or pumping sessions
- Baby struggling to latch properly and not fully draining your breasts when feeding
- Baby not feeding well due to illness
Symptoms of Breast Engorgement
Breast engorgement is usually temporary and will go away when your body adjusts your breast milk production to suit your baby's needs.
Symptoms of breast engorgement include:
- Tender breasts
- Swelling and hardness
- Reddened areas
- Larger, flattened nipples (baby may struggle to latch)
- Sore nipples
Treatment for Engorgement Relief
If you're exhibiting symptoms of breast engorgement, there are several ways to find relief, including:
- Continue to breastfeed or pump frequently to relieve “fullness.
 ”
” - Apply warm, wet compresses and gently massage breasts 10 minutes before feeding to help with milk flow.
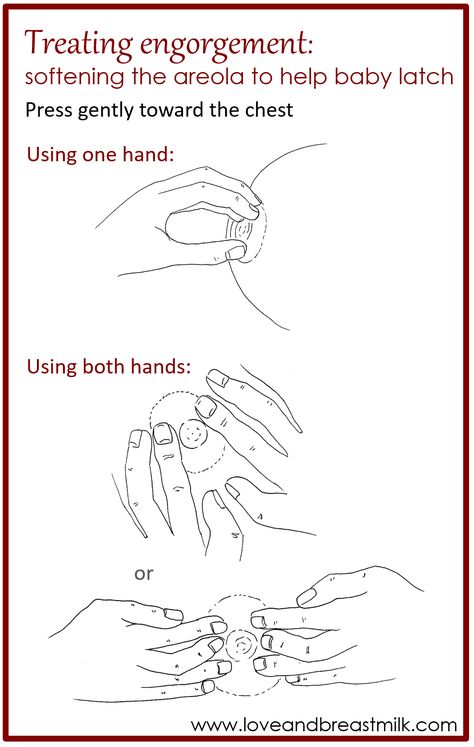
- If baby is having trouble latching, express a little milk by hand or by pumping on a low setting, until the areola has softened enough for him or her to latch easier.
- Cold compresses applied for 15 minutes every hour between feedings can help relieve pain and reduce swelling. Small bags of crushed ice or frozen vegetables wrapped in a thin dish towel work well for this. Some moms use cool cabbage leaf compresses 3-4 times per day for relief as well, but - while effective for treating engorgement - it's important to know that cabbage leaf compresses can also lower your milk supply.
- Rest, rest, rest!
- Call your medical provider if you have a fever higher than 101° F or severe pain. That may be a sign of a breast infection called mastitis.
Preventing Breast Engorgement
Of course, preventing breast engorgement is always preferable to treating it after it's already occurred. The best ways to avoid breast engorgement include:
The best ways to avoid breast engorgement include:
- Nurse or pump often. Lactation consultants recommend breastfeeding at least 8-10 times in a 24-hour period.
- Keep a compact, easily portable breast pump on hand - in your car, at your workplace, or at home - as a back-up, so you can pump if and when needed to prevent engorgement during times away from your baby. A single, manual breast pump like the Harmony® is designed for occasional use and short periods away from your little one. Best of all, it comes with our PersonalFit Flex™ breast shield, which is designed to optimize pumping comfort and milk flow, which gives you more milk faster. Just be sure to do your research and find the best back-up breast pump option for you and your unique needs!
- Establish a proper latch. If a baby latches deeply to the breast, that helps ensure your breasts are releasing milk efficiently.
- Nurse on or pump each breast until it is “empty” before switching.

- Express milk from breasts after each feeding if your baby has not completely relieved fullness.
As a breastfeeding mama, it's important that you practice meaningful self-care and always, always ask for help when you need it.
What is breast swelling? | Breast swelling
Some mothers experience breast swelling when milk begins to flow in the first days after childbirth. Usually this phenomenon is temporary and easily eliminated. Read our article to find out how to help yourself.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
Schoned, a mother of three, has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
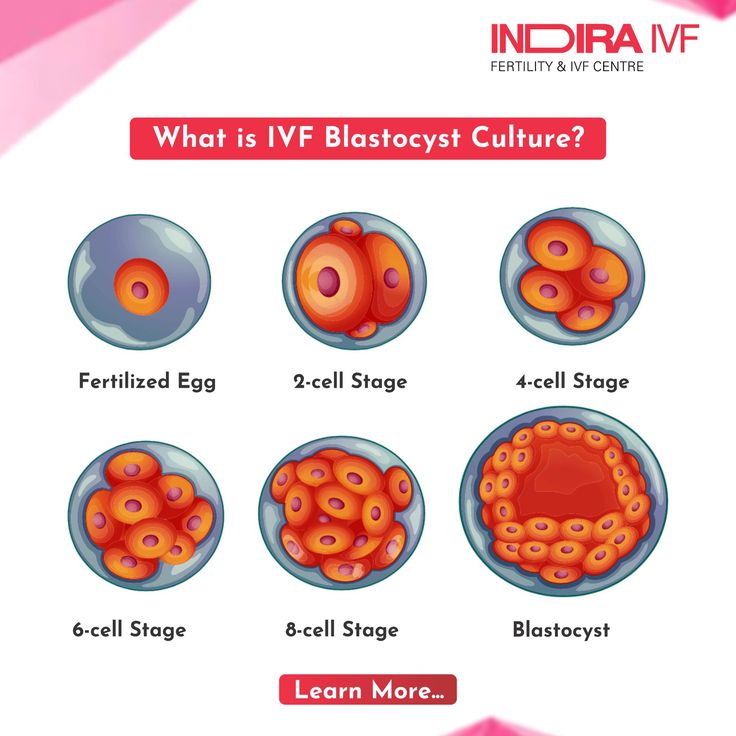
When you start breastfeeding, you first produce a small amount of colostrum, which gradually increases over the first few days. After about two to four days, production increases significantly. This phenomenon is called the "arrival" of milk. nine0012 1
After about two to four days, production increases significantly. This phenomenon is called the "arrival" of milk. nine0012 1
One of the signs that milk is starting to come in is a change in the breast - it fills up and becomes firmer. This is due not only to an increase in the amount of milk, but also to increased blood flow and additional lymphatic fluid to the breast tissues. 2
If the child eats well and often, then for most mothers this feeling of heaviness disappears over time without any complications. However, some women produce so much milk that their breasts fill up and become painful and very hard. This condition is called breast swelling. And although everything usually passes in a day or two, this period can be quite painful. nine0003
How does breast swelling manifest itself?
Swelling may affect one or both breasts. It can cause swelling, sometimes down to the armpits, and a throbbing sensation. The chest becomes quite hot, sometimes lumps are felt in it.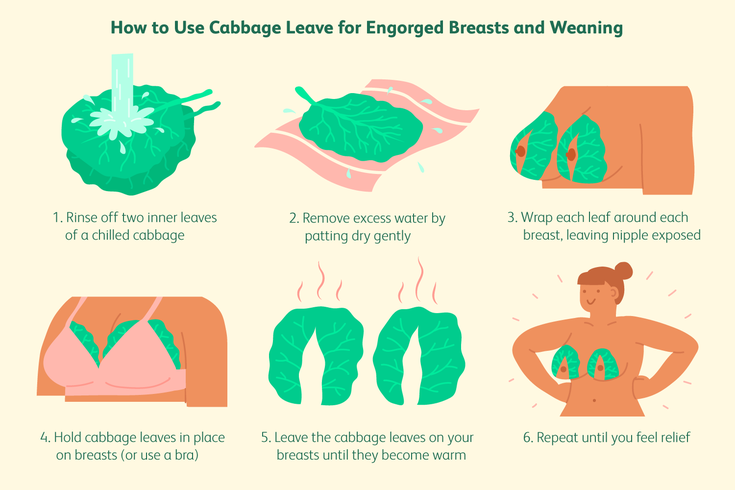 All this is due to the fact that a huge number of processes take place inside. You may also notice other symptoms, such as the skin on your breasts becoming shiny and tight, and your nipples becoming hard and flat. Swelling of the mammary glands can even cause a temperature to rise to 37.5–38.3°C (99–101°F). 3
All this is due to the fact that a huge number of processes take place inside. You may also notice other symptoms, such as the skin on your breasts becoming shiny and tight, and your nipples becoming hard and flat. Swelling of the mammary glands can even cause a temperature to rise to 37.5–38.3°C (99–101°F). 3
In addition to painful sensations, breast swelling is also dangerous because it can make breastfeeding difficult, and this, in turn, will worsen the situation even more. If the baby finds it difficult to latch on because the nipples have become flat and the breast tissue is firmer, nipples may become inflamed. In addition, in the event of a poor grip, he will not be able to completely empty the chest. Thus, if left untreated, swelling of the mammary glands can lead to blockage of the milk ducts, mastitis, and reduced milk production. nine0003
What causes breast swelling?
Usually breast swelling is due to the fact that the child does not feed often enough (less than eight times a day). In principle, this can happen to any mother, but women who have undergone various breast surgeries, including breast augmentation, are more prone to swelling of the mammary glands. 2 Wearing a bra that is the wrong size or that is too tight can increase discomfort and lead to clogged milk ducts and even mastitis. nine0003
In principle, this can happen to any mother, but women who have undergone various breast surgeries, including breast augmentation, are more prone to swelling of the mammary glands. 2 Wearing a bra that is the wrong size or that is too tight can increase discomfort and lead to clogged milk ducts and even mastitis. nine0003
Breast swelling can occur in both breastfeeding mothers and mothers who are not or cannot breastfeed. The hormonal changes that occur after the birth of a baby and the release of the placenta and increase milk production are independent of whether you are breastfeeding or not. Swelling can also occur if the number of feedings is drastically reduced, for example, if the child becomes ill, sleeps longer, starts eating solid foods, or goes to nursery.
How to treat breast swelling? nine0012 2
The best cure for swollen breasts is a hungry baby! Try to empty your breasts as much and as often as possible to facilitate the release of milk.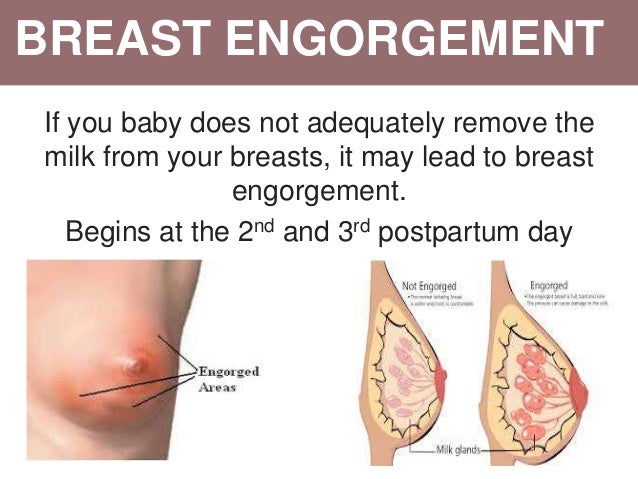 To do this, feed your baby on demand, preferably eight to twelve times a day.
To do this, feed your baby on demand, preferably eight to twelve times a day.
Maintain skin-to-skin contact with your baby, cuddling as often as possible during the day and at night when you are awake. This will allow him to smell the attractive smell of your milk and have easy access to the breast, and you will be able to better monitor signs that he is hungry and, accordingly, feed more often. Let the baby eat enough from one breast before offering the second. nine0003
It's a good idea to see a lactation consultant or specialist to check if your baby is properly grasped and positioned. It depends on how well he will eat and empty his chest. The tips below will also help you relieve the symptoms of breast swelling.
Tips for relief of breast swelling 2
- Breastfeed at least eight times a day.
- Make sure your baby is latching on well. nine0055
- Try other feeding positions.
- Gently massage your breasts during feeding to improve the flow of milk.

- Express some milk by hand or with a breast pump before feeding to soften the nipple and make it easier for your baby to latch on.
- If your breasts are still firm and full after a feed, pump more until you feel better.
- If your baby cannot breastfeed, express milk for him. Pumping must be continued until the breast becomes softer, and do this at least eight times a day. nine0055
- Try the areola pressure softening technique. This helps to remove excess fluid from the breast. A lactation consultant or specialist will show you how to do this.
- If milk leaks, try taking warm showers or applying warm flannel to your breasts just before feeding or pumping to soften your breasts and make it easier for your milk to flow. You should not, however, warm the chest for more than two minutes, as this can only increase swelling. nine0055
- If your milk isn't leaking, try applying cold compresses, chilled gel pads, or even frozen green peas wrapped in a towel for ten minutes after feeding to reduce swelling and relieve pain.

- Put clean cabbage leaves in your bra. Yes Yes! For many moms, it really helps reduce swelling and discomfort, and there are scientific explanations for this. 4
- Take an anti-inflammatory pain reliever. While breastfeeding, you can take some medications, in consultation with your doctor. Always consult your doctor, follow the drug manufacturer's instructions and the pharmacist's recommendations. To learn more about medications and breastfeeding, read our article on breastfeeding when sick. nine0055
- Wear an appropriately sized and comfortable nursing bra, avoid underwire or no bra at all.
- Do not skip feedings or stop breastfeeding abruptly as this may increase breast swelling.
Seek medical advice if your 5 temperature rises above 38 °C or if your baby is unable to suckle due to breast swelling.
And in any case, try to remain calm. Your body is just getting used to producing milk and feeding your baby. Breast swelling should go away on its own soon after you both get comfortable with breastfeeding. nine0003
Breast swelling should go away on its own soon after you both get comfortable with breastfeeding. nine0003
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Berens P, Brodribb W. ABM Clinical Protocol# 20: Engorgement, Revised 2016. Breastfeed Med . 2016;11(4):159-163. - Behrens P, Brodrhibb W, "AVM Clinical Protocol #20: Engorgement, 2016 edition". Brestfeed Med (Breastfeeding Medicine). 2016;11(4):159-163.
3 Affronti M Low-grade fever: how to distinguish organic from non-organic forms. Int J Clin Pract. 2010;64(3):316-321. - Affronti M. et al., "Subfebrile temperature: how to distinguish organic from non-organic cases." Int Zh Klin Prakt. 2010;64(3):316-321.
- Affronti M. et al., "Subfebrile temperature: how to distinguish organic from non-organic cases." Int Zh Klin Prakt. 2010;64(3):316-321.
4 Boi B et al. The effectiveness of cabbage leaf application (treatment) on pain and hardness in breast engorgement and its effect on the duration of breastfeeding. JBI Libr Syst Rev . 2012;10(20):1185-1213. - Boys B. et al., "Effectiveness of cabbage leaf (as a drug) for breast pain and engorgement, and its effect on the duration of breastfeeding." nine0095 JBAi Libr Sist Rev. 2012;10(20):1185-1213.
5 NHS Choices. How do I take someone's temperature? [Internet]. UK: NHS Choices; updated 2016 June 29. Available from : www.nhs.uk/chq/pages/1065.aspx?categoryid=72 - NHS Choice. "How to measure the temperature?" [Internet]. United Kingdom: NHS Choice, 29 June 2016 edition Article linked: www. nhs.uk/chq/pages/1065.aspx?categoryid=72
nhs.uk/chq/pages/1065.aspx?categoryid=72
Breast engorgement: symptoms and first aid
search support iconSearch keywords
Home ›› How to relieve the unpleasant symptoms of breast engorgement
Home ›› How to relieve the unpleasant symptoms of breast engorgement
↑ Top
One of the most common breastfeeding problems faced by mothers is breast engorgement. While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it. nine0003
Let's look at all the important issues, including prevention, symptoms, and help with engorgement.
What is breast engorgement?
Engorgement is an increase in the size of the mammary glands, in which the breast becomes painful and sensitive. This condition is associated with increased blood flow and increased milk production, so it very often occurs during the first few days after childbirth.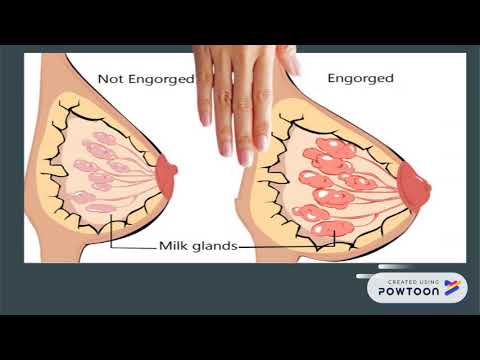 In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs. nine0003
In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs. nine0003
How long does engorgement last?
All women are different, and, accordingly, the duration of this condition may vary. Some experience mild symptoms for only one day, while others may experience this condition for up to two weeks.
Breast engorgement occurs for various reasons. The most common:
- Skipping a feeding or pumping session.
- Making more milk than the baby eats. nine0003
- Insufficient outflow of milk (improper latching on to the breast by the baby).
- Inflammation.
Breast engorgement symptoms
Breast engorgement symptoms vary, but the most common are:
- Breasts become hard or firm.
- Breasts become sore or warm to the touch.
- Breasts become heavy and swollen. nine0055
- Breasts become lumpy and swollen.
Although engorgement and mastitis may appear similar, they are actually completely different conditions. How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement. nine0003
Prevention of engorgement
There are several ways to prevent this condition. Prevention of breast engorgement in the first days after childbirth can be difficult as the mother's body adapts to the changes. But you can try to avoid it as follows:
But you can try to avoid it as follows:
- Check the mammary glands. Moms should schedule breast checks before the baby is born. The doctor will be able to recommend corrective measures, if needed, to make breastfeeding more comfortable, as well as explain how to distinguish engorgement from mastitis and how to relieve breast engorgement. nine0055
- After your baby is born, feed on demand or express milk regularly if you are separated from your baby. Breastfeeding mothers produce milk regularly, so it is important to breastfeed or express milk frequently. Moms should try to feed their baby at least eight times a day and make sure that their breasts are completely empty each time. If a mother is unable to breastfeed her baby, she should express milk with a breast pump.
The electronic breast pump will help you to comfortably and efficiently express the right amount of milk between feedings, if necessary, or instead of feeding when the mother is away from the baby..jpg) nine0055
nine0055
3. Make sure that the baby latch on correctly. To learn how to properly breastfeed a baby, a mother can seek advice from a breastfeeding specialist. Proper gripping of the breast during feeding is important for complete emptying of the breast. It also helps prevent other problems such as sore, irritated or cracked nipples.
4. Wean the baby gradually. When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement. nine0003
Helping with breast engorgement
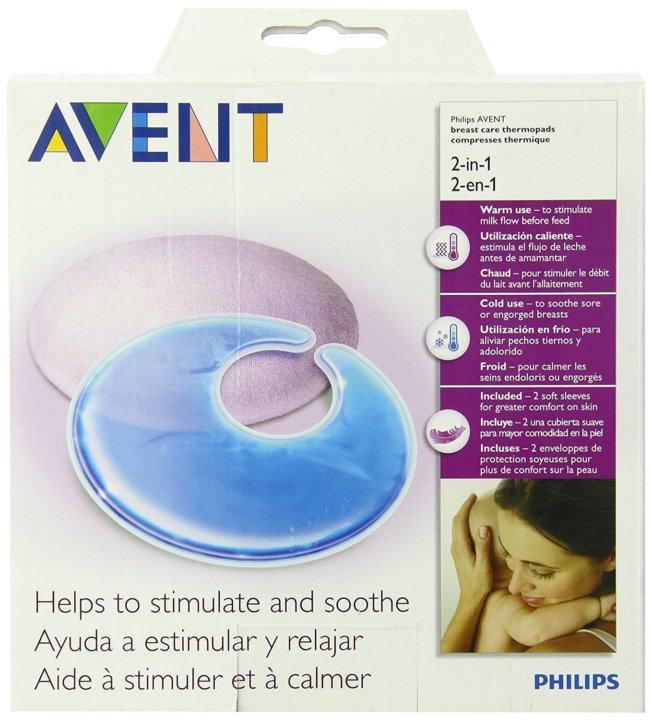
Breastfeeding with engorgement is not only safe, but essential to prevent worsening of symptoms and provide relief. While the body is learning how to produce the right amount of milk, moms can use the Philips Avent bra pads to absorb excess milk and prevent stains on clothes all day long.
Philips Avent
Philips Avent 2-in-1 thermal pads can both warm and cool your breasts to both stimulate and soothe your breasts after feeding. Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
Philips Avent
Multifunction thermal pads
SCF258/02Overall rating / 5
- review review reviews Reviews
-
-{discount-value}
- Pictures It is important to achieve optimal outflow of milk during feedings. To stimulate the outflow of milk, during feeding, you can gently massage the breast.
- Express milk. There are situations when a nursing mother cannot be with the baby during feeding. It is important to empty your breasts by expressing milk to prevent engorgement and other problems.
 nine0055
nine0055 - When feeding, change positions and rotate the mammary glands. Changing your position while breastfeeding can be beneficial, as it improves the outflow of milk from different parts of the mammary glands. In addition, mothers can change their breasts during one feeding so that the baby can empty both of them.
Remember that minor pain and discomfort is completely natural during breastfeeding, but if these symptoms persist or worsen, the mother should consult a doctor. nine0003
Philips Avent Articles & Tips
Baby+ App
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development. nine0003
Download app:
You are leaving the Philips Healthcare (“Philips”) official website.