Round spot of dry skin
Discoid eczema | nidirect
Discoid eczema, also known as nummular or discoid dermatitis, is a long-term skin condition. It causes skin to become itchy, reddened, swollen and cracked in circular or oval patches. See your pharmacist or GP if you think you may have discoid eczema so they can recommend a suitable treatment.
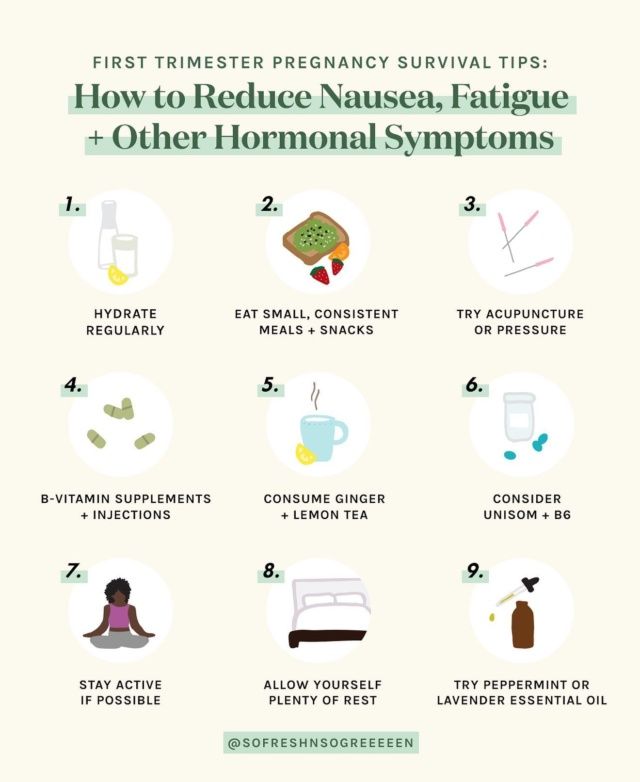
Symptoms of discoid eczema
Circular or oval patches of eczema
Circular or oval patches of eczema can affect any part of the body, although they don't usually affect the face or scalp.
They start as a group of small red spots or bumps on the skin which join up to form larger pink, red or brown patches that can range from a few millimetres to several centimetres in size.
Blistering
At first, these patches of eczema are often swollen, blistered (covered with small fluid-filled pockets) and ooze fluid.
Itchiness and pain
The patches also tend to be very itchy, particularly at night.
Dry, crusty, cracked and flaky skin patches
Over time, the patches may become dry, crusty, cracked and flaky. the centre of the patch also sometimes clears, leaving a ring of discoloured skin that can be mistaken for ringworm.
Discoid eczema causes circular or oval patches of eczema on the skinYou may just have one patch of discoid eczema, but most people get several patches. The skin between the patches is often dry.
Patches of discoid eczema can sometimes become infected.
Signs of an infection can include:
- the patches oozing a lot of fluid
- a yellow crust developing over the patches
- the skin around the patches becoming red, hot, swollen, and tender or painful
- feeling sick
- chills
- feeling unwell
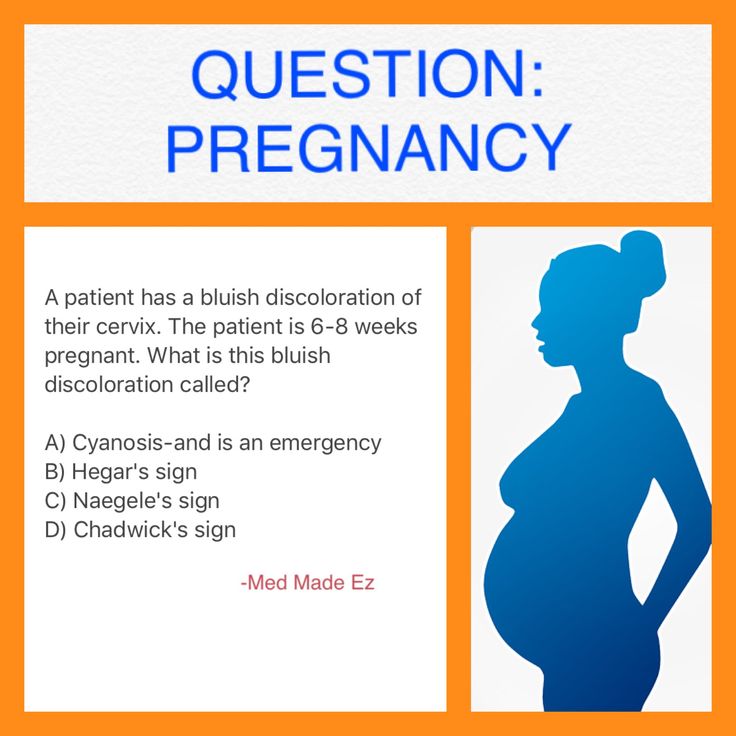
When to get medical advice
See your pharmacist or GP if you think you may have discoid eczema so they can recommend a suitable treatment.
You should also seek medical advice if you think your skin may be infected. You may need treatment.
You may need treatment.
Your GP should be able to make a diagnosis just by examining the affected areas of skin. In some cases they may also ask questions or arrange some tests to rule out other conditions.
Your GP may refer you to a dermatologist (a doctor who specialises in managing skin conditions) if they're unsure of the diagnosis or if you need patch testing.
Causes of discoid eczema
The cause of discoid eczema is unknown, although it may occur as a result of having particularly dry skin.
Dry skin means your skin can't provide an effective barrier against substances that come into contact with it. This could allow a previously harmless substance, such as soap, to irritate (damage) your skin.
It's important to look carefully at all the chemicals in cosmetics and toiletries that may have come into contact with your skin. Contact dermatitis, a type of eczema caused by coming into contact with a particular irritant, may have a role in discoid eczema.
Some people with discoid eczema also have a history of atopic eczema, which often occurs in people who are prone to asthma and hay fever. However, unlike atopic eczema, discoid eczema doesn't seem to run in families.
Other possible triggers
An outbreak of discoid eczema may sometimes be triggered by a minor skin injury, such as an insect bite or a burn.
Some medicines may also be associated with discoid eczema, as patches of eczema can appear in people taking:
- interferon and ribavirin – when they're used together to treat hepatitis C
- tumour necrosis factor-alpha (TNF-alpha) blockers – used to treat some types of arthritis
- statins (cholesterol-lowering medication) – which can cause dry skin and rashes
Dry environments and cold climates can make discoid eczema worse, and sunny or humid (damp) environments may make your symptoms better.
Treating discoid eczema
Discoid eczema is usually a long-term problem. But medications are available to help relieve the symptoms and keep the condition under control.
Without treatment, discoid eczema can last for weeks, months or even years. It may also keep recurring – often in the same area that was affected previously.
Treatments used include:
- emollients – moisturisers applied to the skin to stop it becoming dry
- topical corticosteroids – ointments and creams applied to the skin that can help relieve severe symptoms
- antihistamines – medications that can reduce itching and help you sleep better
There are also things you can do yourself to help, such as avoiding all the irritating chemicals in soaps, detergents, bubble baths and shower gels.
Additional medication can be prescribed if your eczema is infected or particularly severe.
Occasionally, areas of skin affected by discoid eczema can be left permanently discoloured after the condition has cleared up.
Other types of eczema
Eczema is the name for a group of skin conditions that cause dry, irritated skin. Other types of eczema include:
- atopic eczema (also called atopic dermatitis) – the most common type of eczema, it often runs in families and is linked to other conditions such as asthma and hay fever
- contact dermatitis – a type of eczema that occurs when the body comes into contact with a particular substance
- varicose eczema – a type of eczema that most often affects the lower legs and is caused by problems with the flow of blood through the leg veins
- Discoid eczema
Help improve this page - send your feedback
You must have JavaScript enabled to use this form.
report a problem
leave feedback
ask a question
Report a problemWhich problem did you find on this page? (Tick all that apply)
A link, button or video is not working
There is a spelling mistake
Information is missing, outdated or wrong
I can't find what I'm looking for
Another issue
Messages
Tell us more about the problem you're having with the nidirect website.
Enter your feedback
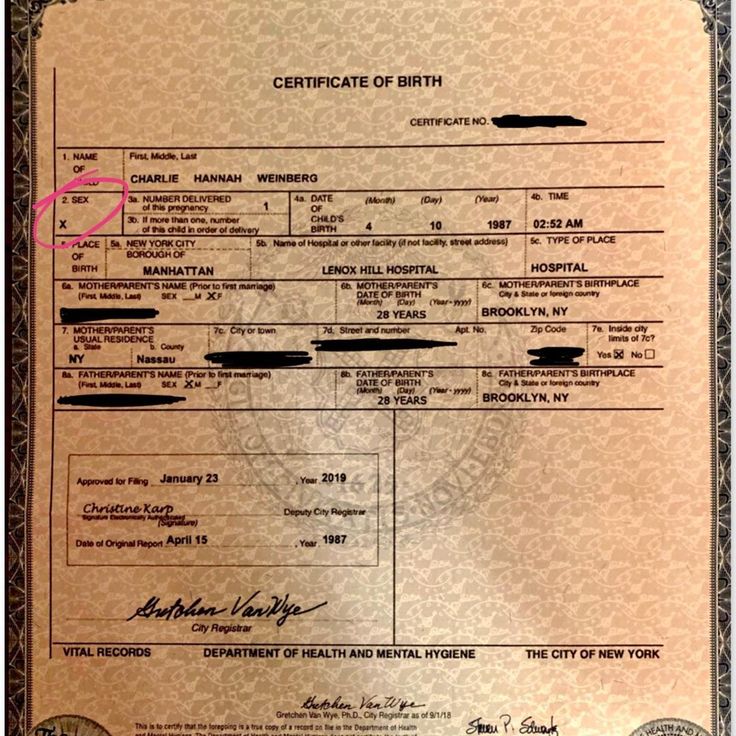
What is your question about?Choose a topic for your question: - Select -AnglingBenefitsBirth certificatesBlue BadgeCareersCompensation due to a road problemChild MaintenanceCivil partnership certificatesCoronavirus (COVID-19)COVID vaccination certificateCriminal record checks (AccessNI)Death certificatesEducational Maintenance AllowanceEmployment rightsHigh Street Spend Local SchemeMarriage certificatesMotoringnidirect accountPassportsPenalty Charge NoticesPensionsPRONI - historical recordsRates or property valuationProblems with roads and streetsSmartpassMy question is about something else
What to do next
Dry Skin Patches: Causes, Symptoms, and More
If you’ve noticed dry patches of skin on your body, you’re not alone. Many people experience these dry spots. They can have a number of causes, including contact dermatitis, psoriasis, and more.
Many people experience these dry spots. They can have a number of causes, including contact dermatitis, psoriasis, and more.
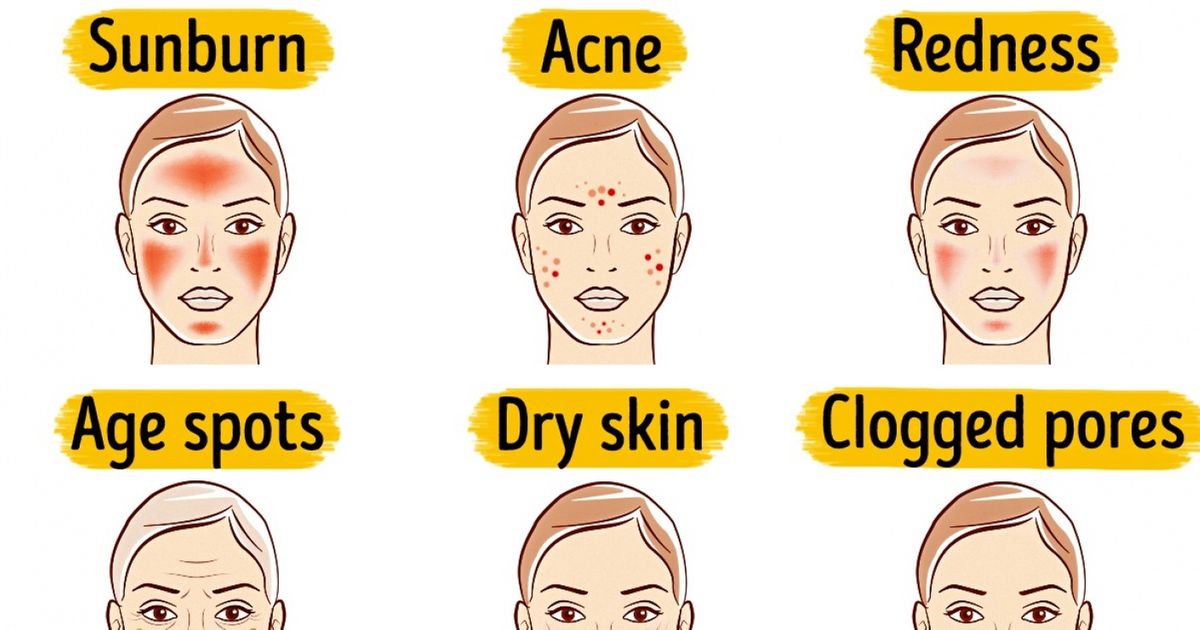
Dry skin patches can feel rough and scaly in only certain areas, which is different from just having overall dry skin.
While dry skin patches can crop up anywhere, they often appear on the:
- elbows
- lower arms
- hands or wrists
- feet or ankles
- chest
- knees or lower legs
- face
- eyelids
Read on to learn more about what could be causing your dry patches.
Dry patches can have several possible causes, many of which can be effectively treated.
Contact dermatitis
Contact dermatitis is a condition that occurs when you come into contact with a substance that causes a skin reaction. It often causes a discolored, itchy rash. If you have it on your hands, the American Academy of Dermatology says that you might develop scaling on your fingers.
Some triggers for contact dermatitis can include:
- perfumes
- chemicals in skincare or makeup products
- latex
- gold or nickel jewelry
- poison ivy or poison oak
Contact dermatitis can be treated, usually with steroid creams or oral medications. It’s not contagious, meaning you can’t give it to others or catch it from other people.
It’s not contagious, meaning you can’t give it to others or catch it from other people.
Psoriasis
Psoriasis is an autoimmune disorder that causes skin cells to multiply too quickly. People with psoriasis may develop scaly, itchy patches of skin on their bodies.
This chronic condition causes flare-ups. According to the National Psoriasis Foundation, flare-ups may be triggered by:
- stress
- smoking
- alcohol
- infections
- skin injuries
- certain medications
Many treatments are available to help manage symptoms of psoriasis, including:
- topical creams
- light therapy
- oral or injected medications
Your doctor will recommend one of these options based on how serious your condition is.
Eczema
Eczema, which is also known as atopic dermatitis, can occur at any age. But the National Eczema Association says that it’s most common in children.
The condition causes itchy patches that can range in color from reddish brown to grayish brown, depending on your skin color. These patches may crust over when you scratch them.
These patches may crust over when you scratch them.
Eczema tends to form on the:
- hands
- feet
- ankles
- wrists
- neck
- upper chest
- eyelids
- elbows
- knees
- face
- other areas
Eczema isn’t contagious. Several treatments can help you manage flare-ups, including creams, drugs, and light therapy.
Athlete’s foot
You don’t have to be an athlete to get athlete’s foot. A fungal infection causes this condition, which usually affects the area between your toes.
Symptoms include a scaly rash that causes itching, stinging, or burning.
The National Health Service says that athlete’s foot is contagious. It can be spread through sharing personal items or walking on floors where the fungus lives.
Doctors usually recommend antifungal ointments or creams to get rid of the infection.
Dry air
Sometimes, dry, cool air can strip your skin of moisture and cause you to develop dry skin patches.
In the summer, higher humidity levels can help stop your skin from drying out. But too much sun exposure can also leave you with dry skin.
Dehydration
If you don’t drink enough fluids throughout the day, you might develop patches of dry skin.
The Institute of Medicine looked at average water intake levels in a 2005 study. To avoid dehydration, they recommended drinking:
- 13 cups of fluid per day for men between the ages of 19 and 30
- 9 cups of fluid per day for women between the ages of 19 and 30
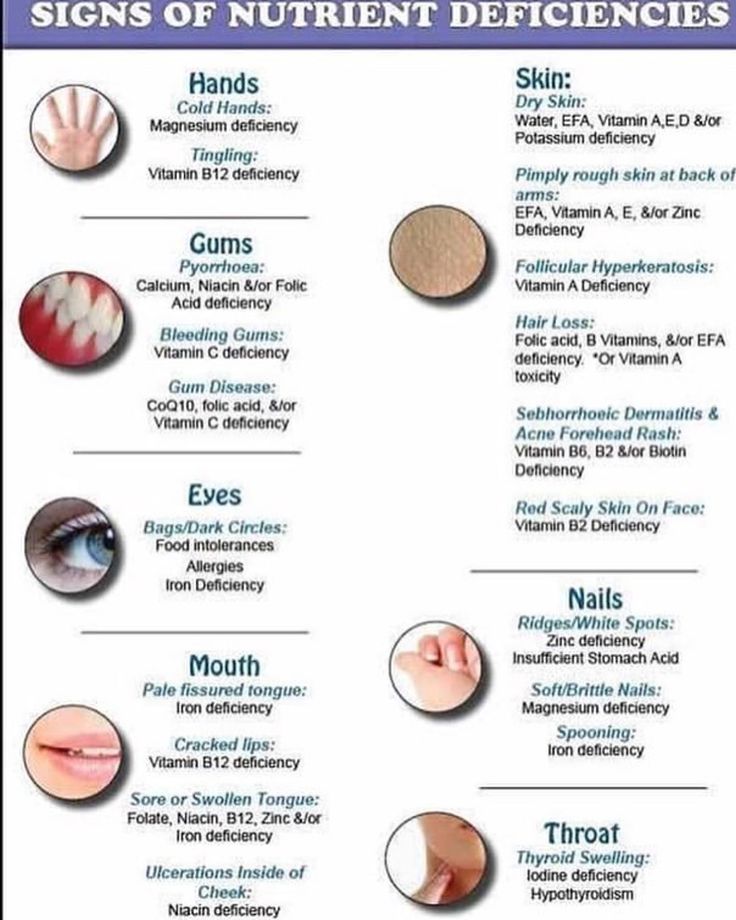
Nutritional deficiencies
Share on PinterestWeissman S, Aziz M, Saleem S, Hassan A, Sciarra M. Acrodermatitis Enteropathica Associated With Inflammatory Bowel Disease. ACG Case Rep J. 2019;6(9):e00209. Published 2019 Aug 29.Not consuming enough calcium, vitamin D, or vitamin E may cause dry, white or light-colored patches to form on your skin.
Dry patches caused by nutritional deficiencies are usually harmless. But a medical professional may suggest that you need to eat a more balanced diet or take supplements.
Smoking
Smoking can be a trigger for dry skin, according to the American Osteopathic College of Dermatology. It can also lead to wrinkles and a dull skin tone.
Older age
As you age, your pores naturally produce less oil, and you may notice that your skin becomes dryer.
Dry patches of skin in older adults often appear on the:
- lower legs
- elbows
- lower arms
Stress
Stress can affect your body in many ways. Some people develop dry skin.
If you have a condition like psoriasis or eczema, stress can make your symptoms worse or bring on a flare-up.
Soaps and overwashing
Using or overusing harsh soaps, perfumes, or antiperspirants may dry out your skin. Additionally, taking long, hot baths or showers can make the problem worse.
Cradle cap is a common condition in babies and toddlers. It causes itchy, discolored skin to form on the scalp, face, and chest.
In many cases, symptoms can be managed with special shampoos, creams, and other therapies.
The American Academy of Dermatology says that cradle cap usually goes away between 6 months and 1 year of age.
Treatment for your dry patches of skin will depend on what’s causing your symptoms.
Your doctor may recommend over-the-counter or prescription creams, ointments, or lotions. In some cases, pills or infusions of stronger medications are used to clear up the skin condition.
Talk with a healthcare professional about which treatment is best for what’s causing your symptoms.
You should contact a doctor if your dry skin becomes severe or doesn’t go away. It’s also a good idea to get checked out if you think your dry skin might be a sign of an underlying illness.
Seeking out early treatment for your skin condition may lead to a better outcome. The Healthline FindCare tool can provide options in your area if you don’t already have a dermatologist.
If you have dry patches of skin, your doctor will probably conduct an exam and ask about your medical and family history.
They’ll likely refer you to a dermatologist. A dermatologist is a doctor who specializes in skin issues.
Depending on the possible condition, you might need lab tests or skin biopsies.
You may be able to help prevent dry, itchy skin by doing the following:
- Use moisturizers every day to keep skin hydrated.
- Limit baths and showers to no more than one a day.
- Limit the time you spend bathing.
- Avoid hot baths or showers. Instead, take showers and baths in warm or lukewarm water
- Use a humidifier to add moisture to the air in your home.
- Use moisturizing body and hand soap.
- Cover up your skin, especially in cold or sunny weather.
- Avoid itching or rubbing your dry skin.
- Drink plenty of fluids throughout the day.
Dry patches of skin can have many possible causes. You may have a skin condition, or the dryness could be related to other habits or things you’re exposed to.
Most of the time, you can effectively manage symptoms with the right medications or home remedies. Talk with your doctor if the dry patches start to bother you or get worse.
Talk with your doctor if the dry patches start to bother you or get worse.
Dry spots on the skin: three common dermatological diseases
July 5, 2020
Dry spots on the skin are a common dermatological symptom that can indicate both a temporary failure and a violation of the barrier functions of the epidermis, and a skin disease. It all depends on the size of the spots, the clarity of their boundaries, as well as the duration of their presence on the skin.
The causes of dryness can be divided into two large groups:
- non-specific - allergic reactions to household chemicals, laundry soap, cosmetic products, dehydration due to cold and wind;
- specific - then the spots become a manifestation of dermatological diseases.
Sometimes a person may notice that dry spots appear on his skin after a certain event occurs, for example, after washing clothes with his hands. Then the reason is obvious and easy to eliminate. But if dry spots on the skin do not go away, itch, peel off, you should consult a doctor.
But if dry spots on the skin do not go away, itch, peel off, you should consult a doctor.
Dry spots with scales
Pink raised dry spots on the body and head may indicate psoriasis. With this dermatological pathology in humans, raised plaques appear on the skin - psoriatic papules. They protrude above the surface of the skin, cause intense itching and flake, tend to spread and merge.
Psoriasis is a chronic autoimmune disease in which rashes are most often localized on the elbows, head, knees and groin. Dry pink spots covered with white scales are foci of chronic inflammation. Under the influence of internal autoimmune processes, epidermal cells divide several times faster than necessary. As a result, small scales are constantly separated from dying skin cells.
Atopic dermatitis and its differences from psoriasis
Atopic dermatitis can also cause dry patches on the body. And as with psoriasis, they cause itching. Due to the increased sensitivity of the skin to environmental factors, the mechanisms of its self-regulation are violated, including the barrier function. That is, an allergy is a trigger for atopic dermatitis, but the tendency to such a skin reaction is genetically laid down.
That is, an allergy is a trigger for atopic dermatitis, but the tendency to such a skin reaction is genetically laid down.
Most often, atopic dermatitis occurs in children. The disease has a chronic course, when exacerbations are replaced by periods of remission. Here are the typical signs of atopic dermatitis:
- dry skin;
- peeling and redness of the eyelids;
- dry skin-colored plaques on the trunk and extensor areas of the body;
- cracks.
It is difficult for a person who does not have a medical education to distinguish psoriasis from atopic dermatitis, but a doctor can easily make a differential diagnosis. There are several differences that may speak in favor of a particular pathology. Atopic dermatitis often affects children, psoriasis can debut in adulthood. Psoriatic plaques are raised above the skin, and scales can be seen. Dry spots in atopic dermatitis are flat. It is also important to consider typical localization.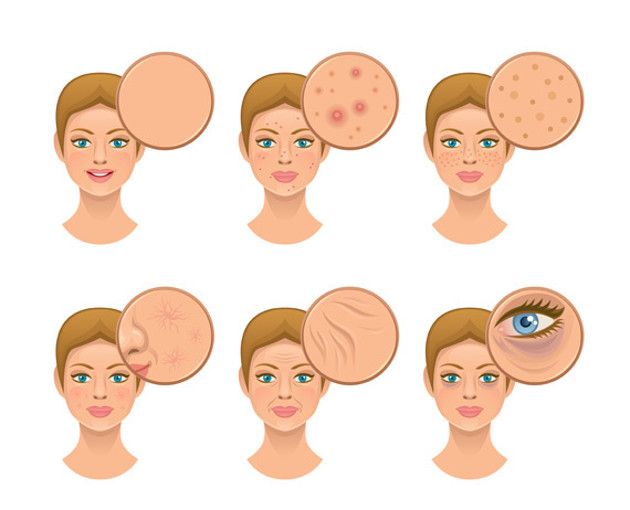
Useful links: State Center of Urology in Moscow - Clinic of Urology named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov
Dry eczema
Sometimes white, dry, scaly patches on the skin of the legs can indicate dry eczema. With this disease, dryness and tightness of the skin first occurs, then peeling and unbearable itching join, cracks may occur. In addition to the legs, the hands, the space between the fingers, and even the face are often affected.
Dry eczema can be caused by bacterial and fungal infections, allergens, synthetic clothing, poor hygiene, and other factors.
As you can see, the appearance of dry spots on the skin can be due to a variety of reasons. An important role is played by the features of the immune system and the tendency to allergic reactions. But in any case, when dry spots appear, it is important to contact a dermatologist and establish the cause of this skin condition.
July 5, 2020
Author of the article: dermatologist Mak Vladimir Fedorovich
ask a question make an appointment
Plaques on the skin - causes, what diseases it occurs in, diagnosis and treatment
- INVITRO
- Library
- Symptoms
Fungus
Allergy
Psoriasis
Keratoma
Mycosis
Nevus
Melanoma
25642 November 16
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment.
 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.Plaques on the skin: the causes of occurrence, in what diseases they occur, diagnosis and methods of treatment.
Definition
A plaque is a pathological element with clear edges that rises above the skin surface or merges with it, more than 5 mm in size.In dermatology, many types of plaques are distinguished - about 70 diseases occur with the formation of these elements, which makes the plaque one of the most common rashes.
Varieties of plaques
The shape of the plaques are round, oval and irregular in shape.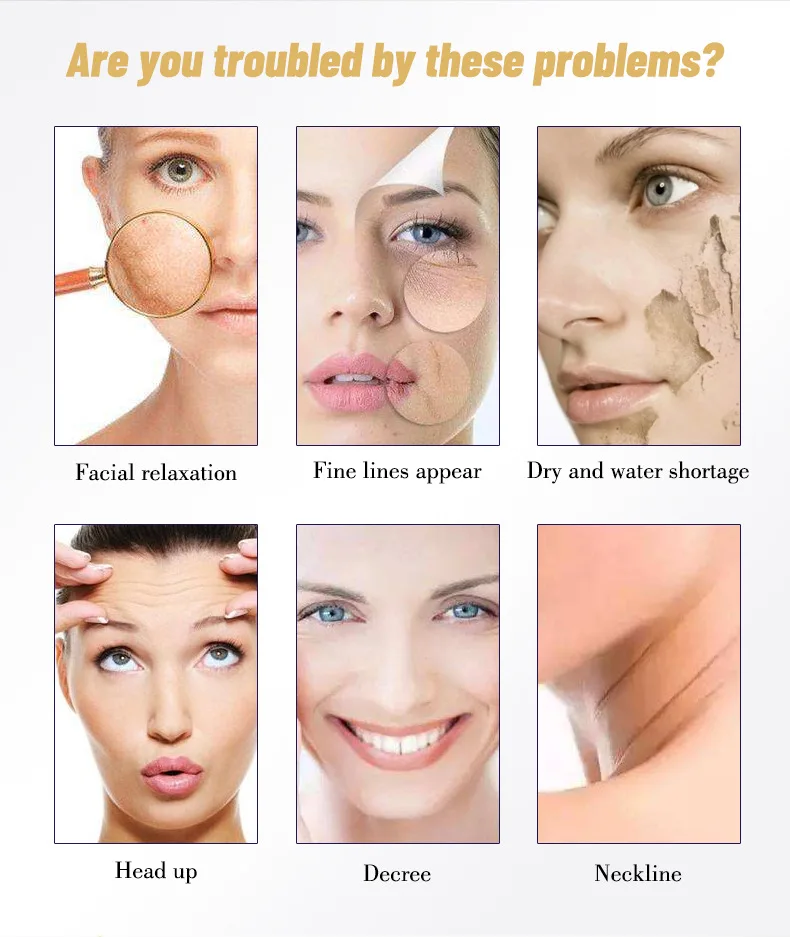 Over time, the shape, surface and appearance of this element may change.
Over time, the shape, surface and appearance of this element may change. Due to the occurrence of plaques, they can be both a manifestation of skin diseases and a symptom of diseases of internal organs and systems (autoimmune reactions, liver diseases, oncological processes, allergic reactions).
Plaques are dry, smooth, red, brown, gray-white, etc.
Possible causes of plaques
Dry plaques on the skin in adults can be a manifestation of the following diseases:
- Fungal infection of the skin, accompanied by plaques with severe itching.
- Allergic reactions are characterized by the appearance on the skin of smooth dry plaques, pink spots, blisters, which are very itchy and cause severe discomfort. They can develop both when the skin comes into contact with the allergen, and when it gets on the mucous membranes (for example, with urticaria, hay fever, food and contact allergies).

- Psoriasis is a chronic non-infectious skin disease in which scaly dry plaques form on the elbows, knees, scalp, prone to fusion and accompanied by mild itching.
- Dry plaques form on the skin if it is exposed to stress for a long time with the loss of its protective functions.
- Diseases of the digestive tract, accompanied by malabsorption syndrome (impaired absorption of vitamins and trace elements in the small intestine), chronic diseases of the liver and other organs, in which substances that are not normally present in the dermis accumulate, also lead to the appearance of dry plaques.
- Solar keratoma is a precancerous condition, which is characterized by the presence of many light grayish plaques on the skin.
The appearance of red plaques on the skin indicates their good blood supply. Possible causes of this condition may be the following nosologies:
- Drug toxidermia is an allergic reaction accompanied by the appearance of elements in the form of plaques on the skin.
 In severe cases, Lyell's syndrome or Stevens-Johnson syndrome, toxic epidermal necrolysis, may develop.
In severe cases, Lyell's syndrome or Stevens-Johnson syndrome, toxic epidermal necrolysis, may develop.
- Dühring's dermatitis (herpetiformis) is a chronic skin disease without established etiology, which is characterized by recurrent appearance of a rash of various morphologies on the skin, accompanied by severe skin itching and burning.
- Mycosis fungoides is a primary T-cell lymphoma of the skin, a malignant lymphoid lesion, primarily of the skin. Itchy red plaques appear on the skin, resembling eczema. In the initial stages, they respond well to treatment with hormonal ointments, but the disease itself requires more complex therapy.
- In children, the appearance of red spots and plaques on the skin is most often associated with an allergic reaction to food.
Brown plaques occur when melanin is deposited in the affected area of the dermis, which causes a brown (dark) color.
 Possible causes may be the following diseases:
Possible causes may be the following diseases: - Becker's nevus is an anomaly in the development of the dermis, when dark plaques with an uneven surface appear on the skin, on which hair can begin to grow over time.
- Pigmentary nevus - "birthmark", may rise above the skin, has a brown or dark color.
- Melanoma is the most malignant skin tumor characterized by rapid metastasis. It develops mainly from nevi and moles. If the nature of the surface, the boundaries of the mole change, its size increases, bleeding occurs, you should immediately contact a dermatologist or oncologist to exclude the development of melanoma.
- Basal cell skin cancer is more often localized on the head, face, neck, does not metastasize, is characterized by slow growth.
- Senile keratoma occurs in the elderly, most likely due to a lack of vitamins, an abundance of animal fats consumed, skin sensitivity to ultraviolet radiation due to a violation of its protective functions.
 Typical localization - face, neck, open areas of the body.
Typical localization - face, neck, open areas of the body. - Seborrheic keratoma is a yellowish plaque on the skin that, over time, transforms into a dark brown growth that tends to flake off, itch severely, crack, bleed, and can serve as an entrance gate for infection.
Which doctors to contact
With the formation of plaques on the skin, it is necessary to contact a dermatologist to determine the causes of the appearance of this element of the rash.
Diagnostics and examinations for plaques
For the diagnosis of fungal skin lesions, scraping from the affected area is used for subsequent microscopic examination.The development of an allergic reaction requires seeking medical help to identify the allergen, prescribing antihistamines, and sometimes hormonal drugs. In clinical cases of allergy, along with skin tests, analyzes are performed using various sets of common allergens and triggers: a panel for respiratory allergens, for food allergens, and for a combination of both.

Respiratory Panel
Synonyms: Comprehensive Respiratory Allergen Test Panel; Respiratory allergens panel, Allergen respiratory profile, Allergy testing. Brief description of the study "Panel respira...
Up to 5 business days
Available with home visit
5 515 RUB
Add to cart
Food Panel, IgE
Food Allergen Panel: hazelnut, peanut, Walnut, almond, cow's milk, egg white, egg ...
Up to 5 business days
Available with home visit
5 515 RUB
Add to cart
Food and Respiratory Panel
Panel different allergens: A mixture of grass allergens: fragrant spikelet; perennial rye; timothy; rye cultivated; Woolly buckthorn (GP3) IgE .
 ..
.. Up to 5 business days
Available with home visit
5 515 RUB
Add to cart
In psoriasis, a visit to a dermatologist and rheumatologist will help reduce the severity of the manifestations of the disease, if appropriate therapy is prescribed. For the diagnosis, it is usually sufficient to examine, determine, the skin manifestations of psoriasis are so characteristic, but if necessary, a differential diagnosis is carried out, including a clinical blood test, feces for the presence of worm eggs and protozoa, and a histological examination of the skin.
Clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, UAC.
 Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study CBC: general...
Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study CBC: general... Up to 1 business day
Available with house call
RUB 810
Add to cart
Fecal analysis for helminth eggs (helminth eggs)
Synonyms: Feces on worm eggs; Analysis of feces for eggs of worms. Ova and Parasite Exam; O&P; Stool O&P test. Brief description of the study "Analysis of feces for eggs of helminths&ra...
Up to 1 business day
Available with home visit
RUB 570
Add to cart
Fecal analysis for protozoa (PRO stool)
Synonyms: Analysis of faeces for protozoa.
 Parasite Exam, feces; Parasitic Examination, fecal. Brief description of the study "Analysis of feces for protozoa" Fecal analysis for ...
Parasite Exam, feces; Parasitic Examination, fecal. Brief description of the study "Analysis of feces for protozoa" Fecal analysis for ... Up to 1 business day
Available with home visit
RUB 570
Add to cart
Histological examination of biopsy material and material obtained during surgical interventions (endoscopic material; tissues of the female reproductive system; skin, soft tissues; hematopoietic and lymphoid tissue; bone and cartilage tissue)
Taking biomaterial is paid separately. According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia.
 ..
.. Up to 5 business days
Available with home visit
2 880 RUB
Add to cart
Diseases of the stomach and intestines can also lead to plaque formation on the skin. To identify the pathology of the gastrointestinal tract, it is enough to refer to therapist or gastroenterologist, conduct a number of endoscopic examinations (gastroscopy, and, if necessary, colonoscopy), ultrasound of the abdominal organs, perform some screening blood tests for diseases of the liver, intestines, stomach.
Gastroscopy
Examination of the mucosa of the upper gastrointestinal tract with the possibility of biopsy or endoscopic removal of small pathological ...
RUB 4,440 Sign up
Colonoscopy
Endoscopic examination of the large intestine to look for abnormalities, perform biopsies, and remove small polyps and tumors.
RUB 5,740 Sign up
Comprehensive ultrasound examination of the abdominal organs (liver, gallbladder, pancreas, spleen)
Scanning of the internal organs of the abdominal cavity to assess its functional state and the presence of pathology.
RUB 2,890 Sign up
Liver function tests: screening
Up to 1 business day
Available with home visit
RUB 1,935
Add to cart
Diagnosis of celiac disease: intolerance to cereal proteins (gluten)
Up to 8 working days
Available with home visit
7 520 RUB
Add to cart
Gastropanel
Up to 9 business days
Available with home visit
RUB 4,760
Add to cart
To clarify the diagnosis of keratoma, a skin biopsy is performed and an epithelium scraping is performed, followed by microscopic and histochemical examination.

Histological examination of biopsy material and material obtained during surgical interventions (endoscopic material; tissues of the female reproductive system; skin, soft tissues; hematopoietic and lymphoid tissue; bone and cartilage tissue)
Taking biomaterial is paid separately. According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia...
Up to 5 business days
Available with home visit
2 880 RUB
Add to cart
Examination of scrapings and impressions of tumors and tumor-like formations
Material for research.
 Imprints and scrapings are obtained from pathological lesions of the skin and mucous membranes (except for the cervix and cervical canal). Relative to test...
Imprints and scrapings are obtained from pathological lesions of the skin and mucous membranes (except for the cervix and cervical canal). Relative to test... Up to 2 working days
Available with home visit
RUB 1,030
Add to cart
If atypical cells are found in scrapings or biopsies, contact the oncologist.
If xanthomas appear on the skin, it is recommended to consult a cardiologist, take blood tests for lipid profile and blood glucose levels, and screen for diabetes.
Lipid profile screening
Up to 1 business day
Available with home visit
1 355 RUB
Add to cart
Glucose (in the blood) (Glucose)
Research material Serum or blood plasma.
 If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation...
If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation... Up to 1 business day
Available with home visit
335 RUB
Add to cart
Diabetes management: advanced
Up to 1 business day
Available with house call
RUB 5 820
Add to cart
What should I do if plaques appear on the skin?
Any newly appeared neoplasms should be shown to a dermatologist.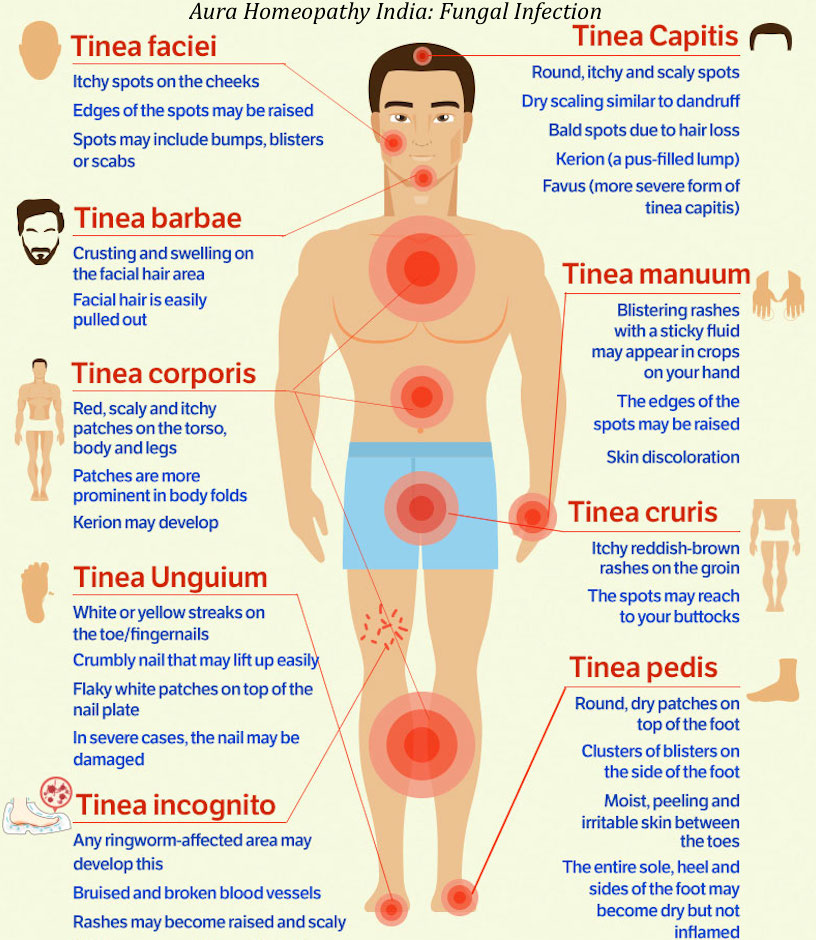 Their cosmetic removal without prior consultation with a specialist is fraught with serious consequences.
Their cosmetic removal without prior consultation with a specialist is fraught with serious consequences. In addition, there are symptoms that require immediate medical attention:
- change in the shape of the plaque - the edges have become uneven;
- change in the surface of the plaque - cracks, ulcerations appeared;
- change in the size of the plaque - it began to grow rapidly above the surface of the skin or actively spread over it;
- discoloration of the plaque - in cases of malignancy, an uneven color of the formation is usually observed with areas of darker and lighter shades;
- the appearance of bleeding - both contact and spontaneous;
- enlargement of regional (nearby) lymph nodes.
Plaque treatment
When plaques of an allergic nature appear on the skin, antihistamines are prescribed, in cases of a severe course of the disease, glucocorticosteroids. In addition, it is important to follow a hypoallergenic diet.
In addition, it is important to follow a hypoallergenic diet. Mycotic plaques require antifungal drugs, both local (ointments, creams) and systemic (tablets). Taking these drugs is associated with a high risk of side effects, and therefore it is possible only after consulting a doctor, accurate verification of the diagnosis and confirmation of the etiology of the disease.
Treatment of psoriasis is multi-stage and complex, it involves constant monitoring by a rheumatologist, taking cytostatics and other drugs, using ointments and shampoos to improve skin condition, using antihistamines to reduce itching, including physiotherapy and a hypoallergenic diet in the treatment regimen.
When confirming the presence of diseases of the gastrointestinal tract, properly selected therapy can stop the appearance of new plaques on the skin, as well as prevent the development of complications of the underlying disease.
Sources:
- Clinical guidelines.
 Dermatitis herpetiformis // Russian Society of Dermatovenerologists and Cosmetologists. 2016.
Dermatitis herpetiformis // Russian Society of Dermatovenerologists and Cosmetologists. 2016. - Clinical guidelines. Urticaria in children // Union of Pediatricians of Russia; Russian Association of Allergists and Clinical Immunologists. 2018.
- Clinical guidelines. Toxidermia // Russian Society of Dermatovenerologists and Cosmetologists. 2016.
- Clinical guidelines. Familial hypercholesterolemia // National Society for the Study of Atherosclerosis. 2018.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Cholesterol plaques
5413 November 18th
-
Hepatic colic
3109 09 November
-
Laryngeal edema
2258 07 November
Show more
Gastritis
Diarrhea
Flatulence
Dysbacteriosis
Allergy
Worms
Ascites
Bloating
In most cases, bloating is associated with flatulence - excessive accumulation of gases in the intestines.
 Bloating (enlargement) of the abdomen can be due to various reasons.
Bloating (enlargement) of the abdomen can be due to various reasons. More
Diarrhea
Pancreatitis
Allergy
Colitis
Rotavirus
Salmonellosis
Loose stools
Loose stools: causes, diseases in which it develops, methods of diagnosis and treatment.
More
Diphtheria
Diabetes mellitus
Laryngitis
Tonsillitis
Fungus
Gastroesophageal reflux
Caries
Bad breath
Halitosis is a medical term used to describe bad breath.
 Bad breath can cause social and psychological problems. People suffering from halitosis experience difficulties in starting a family, finding employment and daily communication with other people.
Bad breath can cause social and psychological problems. People suffering from halitosis experience difficulties in starting a family, finding employment and daily communication with other people. More
Acne
Acne
Fungus
Allergy
Menopause
PCOS
Hyperkeratosis
Intoxication
Demodicosis
Pimples on the face
Pimples on the face: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.

More
Allergy
COPD
Bronchial asthma
False croup
Laryngotracheitis
Lung cancer
Quincke's edema
Pulmonary edema
Epilepsy
Panic attack
Asphyxia
Asphyxiation attacks: causes of occurrence, in what diseases they occur, diagnosis and methods of treatment.