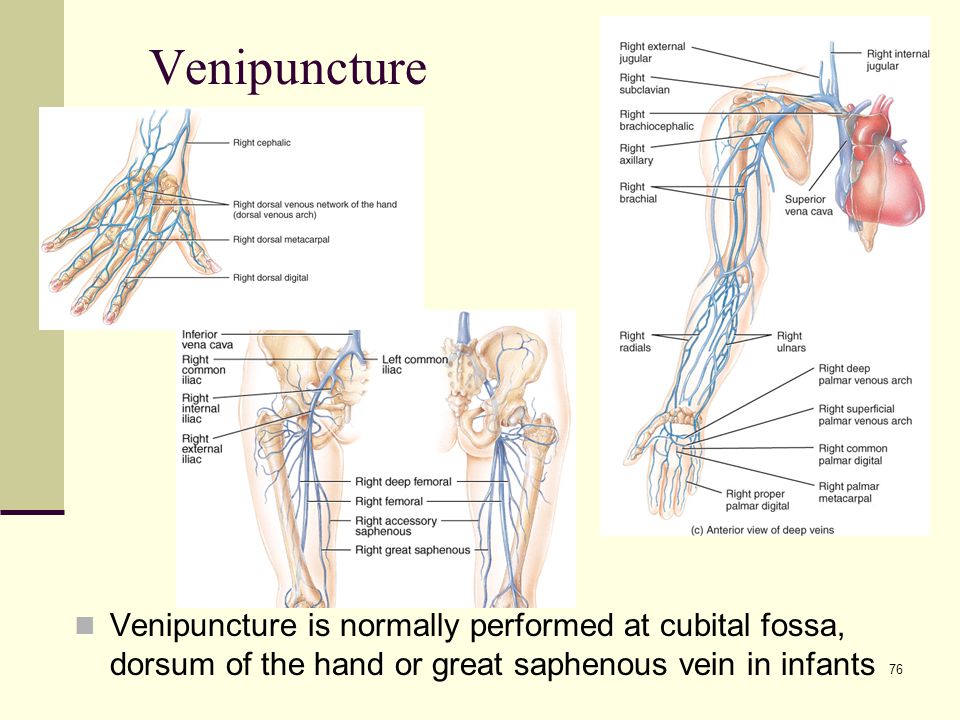
Risk of external cephalic version
What Is It, Procedure, Risks, Labor, & More
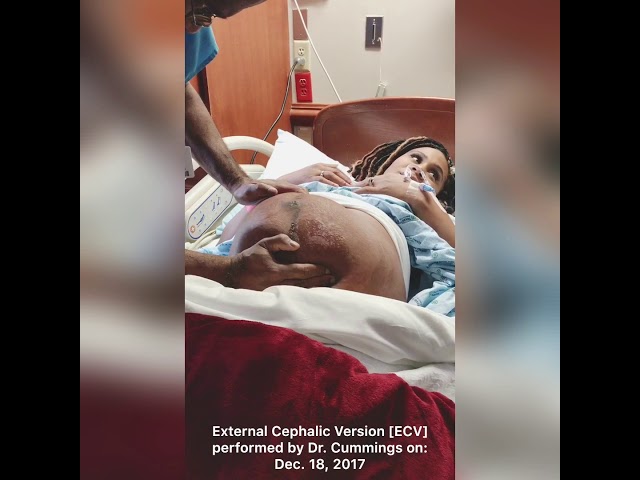
External Cephalic Version: What Is It, Procedure, Risks, Labor, & MoreMedically reviewed by Holly Ernst, PA-C — By Becky Young on April 12, 2018
What is external cephalic version?
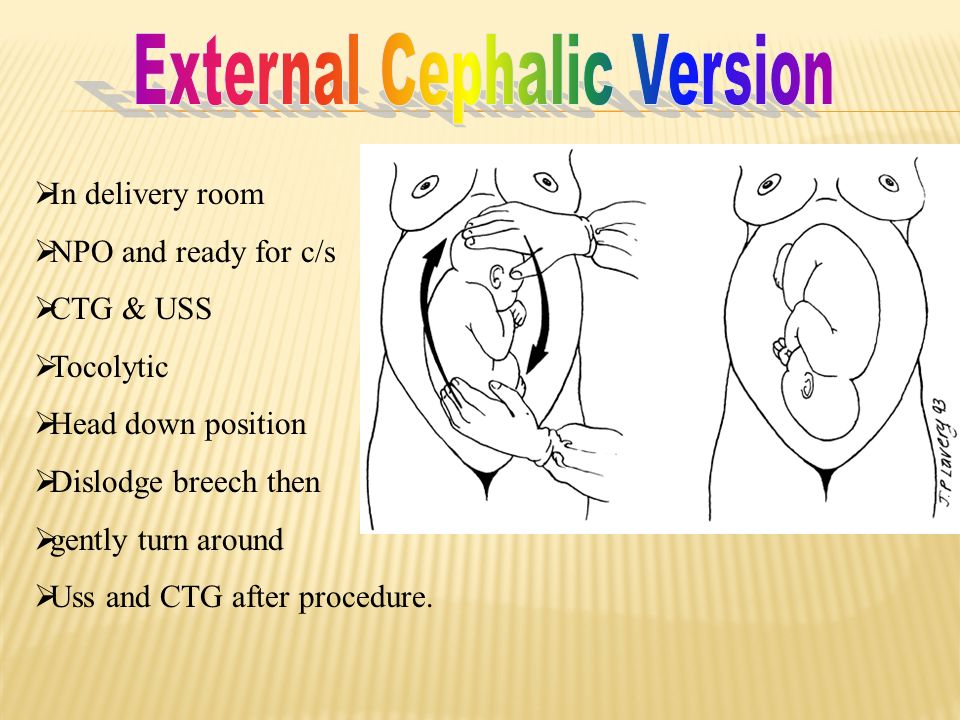
An external cephalic version is a procedure used to help turn a baby in the womb before delivery. During the procedure, your healthcare provider places their hands on the outside of your belly and attempts to manually turn the baby.
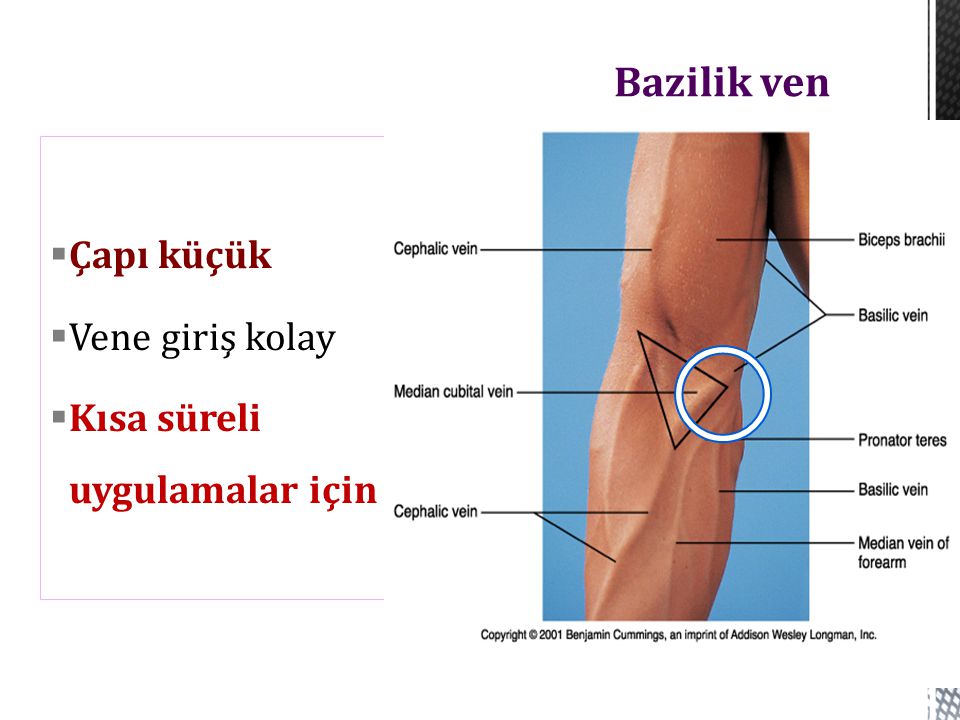
This procedure may be recommended if your baby is in a breech position. This means that their bottom or feet are pointing down toward the vagina, and their head is at the top of your uterus, near your rib cage. A vaginal breech birth is more complicated than a birth where the baby is head down, so it’s preferable that baby is head down before labor starts.
Some women opt to birth their babies via cesarean delivery (C-section) rather than attempt a vaginal breech birth if they’re near or past their estimated due date and the baby still hasn’t turned.
Is it safe?
Most women who are 37 weeks pregnant with a baby in the breech position are candidates for an external cephalic version. The procedure has been found to be successful in turning these babies into a head-down position in around 50 percent of cases. Since breech babies often result in C-sections, a successful external cephalic version may reduce your need for this type of delivery, which is considered an abdominal surgery.
There are some situations in which your healthcare providers may suggest an external cephalic version isn’t right for you. This procedure may not be right for you if:
- you’re already in labor or experiencing any vaginal bleeding
- you’ve had any issues with your placenta during the pregnancy
- there are signs of or concerns for fetal distress
- you are pregnant with more than one baby, such as twins or triplets
- you have any structural abnormalities in your uterus, like large fibroids
Your healthcare provider may also advise against the procedure if you’ve had a previous C-section, your baby is suspected to be larger than average, or you have low or high levels of amniotic fluid.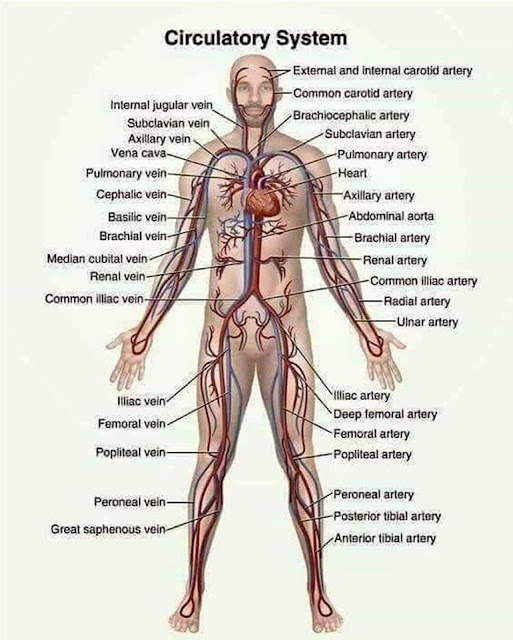 These risk factors are based upon clinical opinion, so you should talk with your healthcare provider to see what they recommend based on your individual pregnancy.
These risk factors are based upon clinical opinion, so you should talk with your healthcare provider to see what they recommend based on your individual pregnancy.
You discuss external cephalic version between 34 and 37 weeks of pregnancy with your doctor if your baby is noted to be breech. Babies often turn on their own before 34 weeks, so there is no need to attempt the procedure earlier in the pregnancy.
The procedure does increase your risk for premature labor and fetal distress. For that reason, most healthcare providers recommend waiting until you’re at term, or 37 weeks pregnant, to attempt this procedure. That reduces risk for complications in your baby if you do need to deliver shortly following the procedure.
You can also talk with your doctor about waiting past 37 weeks, as the baby may spontaneously turn to a head-down position.
The most common risk with an external cephalic version is a temporary change in your baby’s heart rate, which occurs in about 5 percent of cases.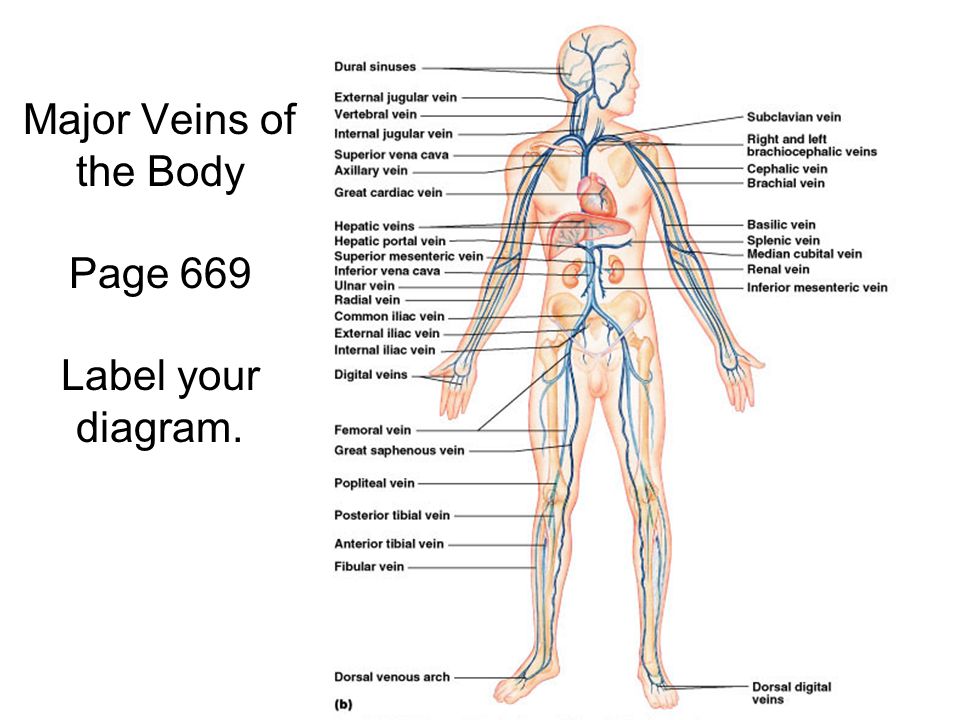 Serious complications are extremely rare but can include the need for emergency C-section, vaginal bleeding, loss of amniotic fluid, and umbilical cord prolapse.
Serious complications are extremely rare but can include the need for emergency C-section, vaginal bleeding, loss of amniotic fluid, and umbilical cord prolapse.
What to expect during the procedure
The procedure will normally be performed by an obstetrician. During an external cephalic version, your doctor will place their hand on your belly to physically push the baby into the optimal position. The procedure usually takes around 5 minutes and your baby’s heart rate will be monitored before, during, and after the procedure. If your doctor suspects your baby isn’t responding well to the procedure, it will be stopped.
Many women report that the procedure is uncomfortable, but medications can be used to reduce the amount of pain felt. Using certain medications during the procedure may also increase the chances of successfully turning the baby. This may be because the medication helps your muscles and uterus relax, allowing the healthcare provider to successfully turn the baby more easily.
How will this procedure affect labor and delivery?
If an external cephalic version is successful, then most of the time labor progresses in a regular way following the procedure. The procedure doesn’t generally affect the length of your labor.
There is a small risk that the procedure will rupture membranes e. This can mean that you will begin labor earlier than you might otherwise have done, and your contractions may be more intense from the beginning of labor instead of building in intensity as the labor progresses.
If the procedure is unsuccessful and your baby remains in the breech position, you could opt for a C-section or choose to attempt a vaginal breech delivery.
One of the main risks involved with a vaginal breech delivery is that your baby’s head could become trapped in the birth canal. The other serious concern is umbilical cord prolapse. With umbilical cord prolapse, the umbilical cord leaves your body before your baby. That increases the risk of the cord becoming compressed during delivery, which cuts off the baby’s supply of oxygen and nutrients.
Both of these complications are a medical emergency. Evidence does show an increased risk of perinatal mortality in planned vaginal breech birth as opposed to a C-section with breech presentation.
Are there other ways to turn the baby?
There are a number of different exercises you can try to attempt to turn your baby from the breech position, though these haven’t been proven in studies to be effective in spontaneously turning the breech baby. Always talk to your healthcare provider before trying these exercises to make sure that they are safe for your pregnancy.
Hip tilt
- Lie on the floor in front of a sofa or chair, with your feet on the sofa or chair. Place cushions under your hips to offer additional support. Your hips should be elevated about 1.5 feet above your head, and your body should be at a 45-degree angle.
- Hold this position for 10 to 15 minutes, three times a day. It’s best to do this when your baby is active.
Pelvic rotations
- Stand or sit on an exercise or birthing ball.
- Once you are in position, gently rotate your hips clockwise in a circular movement. Repeat 10 rotations.
- Switch directions, rotating your hips counterclockwise for 10 rotations.
- Repeated three times a day
Rocking back and forth
- Place your hands and knees on the floor.
- Keeping your hands and knees in place, gently rock your body back and forth.
- Do this for 15 minutes. Repeat up to three times a day.
Walk or swim
- Walk, swim, or engage in another low-impact exercise.
- Do this for 30 minutes a day. Staying active may help your baby move out of the breech position.
The takeaway
It’s recommended that an external cephalic version be offered to all women who have a baby in breech position at or close to term, where there are no other complications. The procedure has been shown to be successful in around half of all cases and may lower the likelihood that a C-section will be needed. There are some possible risks, so be sure to discuss the risks and benefits with your healthcare provider before moving forward with this procedure.
There are some possible risks, so be sure to discuss the risks and benefits with your healthcare provider before moving forward with this procedure.
Last medically reviewed on April 12, 2018
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Berhan Y, et al. (2015). The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: A meta-analysis including observational studies. DOI:
10.1111/1471-0528.13524 - Grootscholten K, et al. (2008). External cephalic version-related risks: A meta-analysis [Abstract]. DOI:
10. 1097/AOG.0b013e31818b4ade
1097/AOG.0b013e31818b4ade - Kathpalia BSK, et al. (2012). Outcome of external cephalic version in breech presentation. DOI:
10.1016/S0377-1237(12)60036-7 - Kuppens SM, et al. (2017). Fetal heart rate abnormalities during and after external cephalic version: Which fetuses are at risk and how are they delivered? DOI:
10.1186/s12884-017-1547-6 - Lim PS, et al. (2014). Successful external cephalic version: Factors predicting vaginal birth. DOI:
10.1155/2014/860107 - Wang Z-H, et al. (2017). Remifentanil analgesia during external cephalic version for breech presentation in nulliparous women at term: A randomized controlled trial. DOI:
10.1097/MD.0000000000006256 - What happens if your baby is breech? (2017).
nhs.uk/conditions/pregnancy-and-baby/breech-birth/
Share this article
Medically reviewed by Holly Ernst, PA-C — By Becky Young on April 12, 2018
related stories
What Is Back Labor and What Causes It?
Can You Turn a Transverse Baby?
What You Need to Know If Your Baby Is in an Oblique Lie
Is It Safe to Use Exercise to Induce Labor?
How Early Can You Safely Give Birth?
Read this next
What Is Back Labor and What Causes It?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Back labor can happen when your baby's head is against your cervix.
 We'll tell you what it's like and how to manage it.
We'll tell you what it's like and how to manage it.READ MORE
Can You Turn a Transverse Baby?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
As you near the end of your pregnancy, you may worry that your baby's transverse position will cause issues during delivery. Learn more about possible…
READ MORE
What You Need to Know If Your Baby Is in an Oblique Lie
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
An oblique lie is a fetal position in which baby's head is just to the side of the pelvic inlet. It presents some challenges, but there are ways to…
READ MORE
Is It Safe to Use Exercise to Induce Labor?
Medically reviewed by Michael Weber, MD
If you’re pregnant and past your due date, you might wonder if exercising will help induce labor.
 Here’s the truth.
Here’s the truth. READ MORE
How Early Can You Safely Give Birth?
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
Not all babies arrive on their due dates — in fact, most don't. So how many weeks early is safe to give birth? Learn more about why certain weeks are…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Does Swaddling Increase the Risk of SIDS?
Medically reviewed by Mia Armstrong, MD
Is swaddling safe, or is it a risk factor for SIDS? Here's what the most recent research says.
READ MORE
External Cephalic Version - StatPearls
Meaghan M. Shanahan; Caron J. Gray.
Author Information
Last Update: July 4, 2022.
Continuing Education Activity
About 25 percent of fetuses will be in breech presentation at 28 weeks, though this decreases to roughly 3 to 4 percent at term.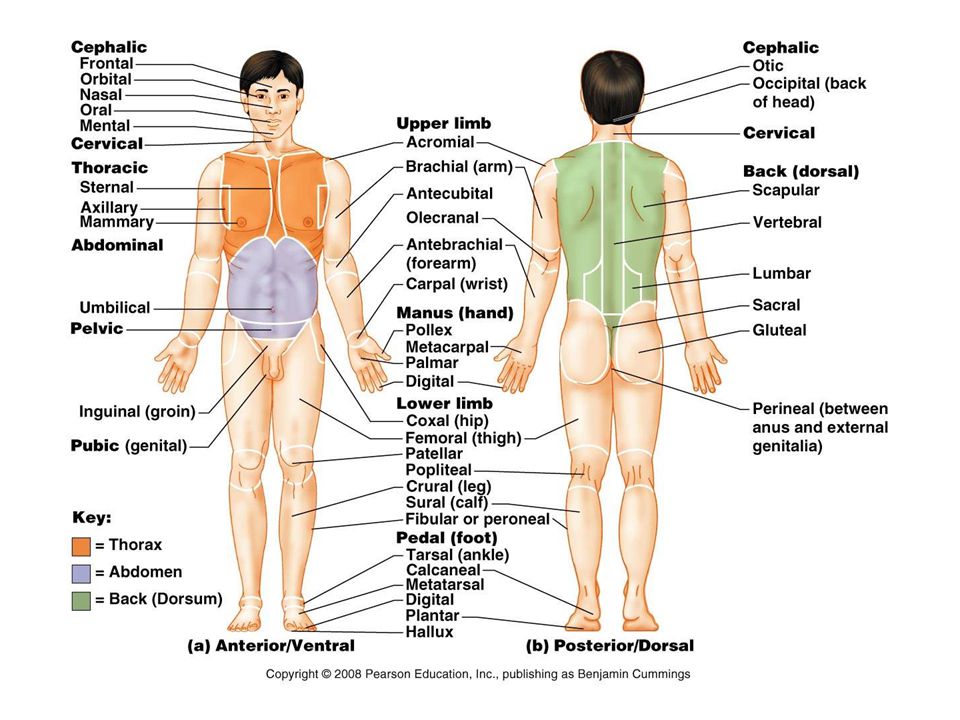 Most infants who are in breech presentation at the time of delivery will require a cesarean delivery. However, an alternative to immediately proceeding with cesarean section is a trial of external cephalic version. This procedure successfully brings the fetus into the vertex position, the ideal position for a vaginal birth, about 58 percent of the time. External cephalic version is performed strategically placing the hands on the gravid abdomen and applying pressure to encourage the fetus to move into the vertex position. This can be attempted for fetuses in the breech, transverse, or oblique positions and has the potential to decrease cesarean delivery rates. This activity reviews the indications, contraindications, and technique involved in performing external cephalic version and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
Most infants who are in breech presentation at the time of delivery will require a cesarean delivery. However, an alternative to immediately proceeding with cesarean section is a trial of external cephalic version. This procedure successfully brings the fetus into the vertex position, the ideal position for a vaginal birth, about 58 percent of the time. External cephalic version is performed strategically placing the hands on the gravid abdomen and applying pressure to encourage the fetus to move into the vertex position. This can be attempted for fetuses in the breech, transverse, or oblique positions and has the potential to decrease cesarean delivery rates. This activity reviews the indications, contraindications, and technique involved in performing external cephalic version and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
Objectives:
Describe the types of breech presentation.
Outline the indications for external cephalic version.
Review the contraindications to external cephalic version.
Summarize a structured interprofessional team approach to provide effective care and appropriate surveillance of patients undergoing external cephalic version.
Access free multiple choice questions on this topic.
Introduction
About 25% of fetuses will be in breech presentation at 28 weeks, and this decreases to about 3% to 4% of term pregnancies. Most of these patients will be delivered by cesarean delivery. It is held that the overall cesarean delivery rate is higher than it should be, and efforts to prevent the first cesarean section often present obstetricians with the task of decreasing the number of cesarean deliveries they perform. One alternative to cesarean delivery is an external cephalic version (ECV). Simply, it is a procedure to change the presentation of the fetus from breech, tranverse, or oblique to vertex by applying pressure externally to the fetus through the gravid abdomen. [1]The overall success rate for the procedure is about 58% and can lead to decreased cesarean delivery rates.[2]
[1]The overall success rate for the procedure is about 58% and can lead to decreased cesarean delivery rates.[2]
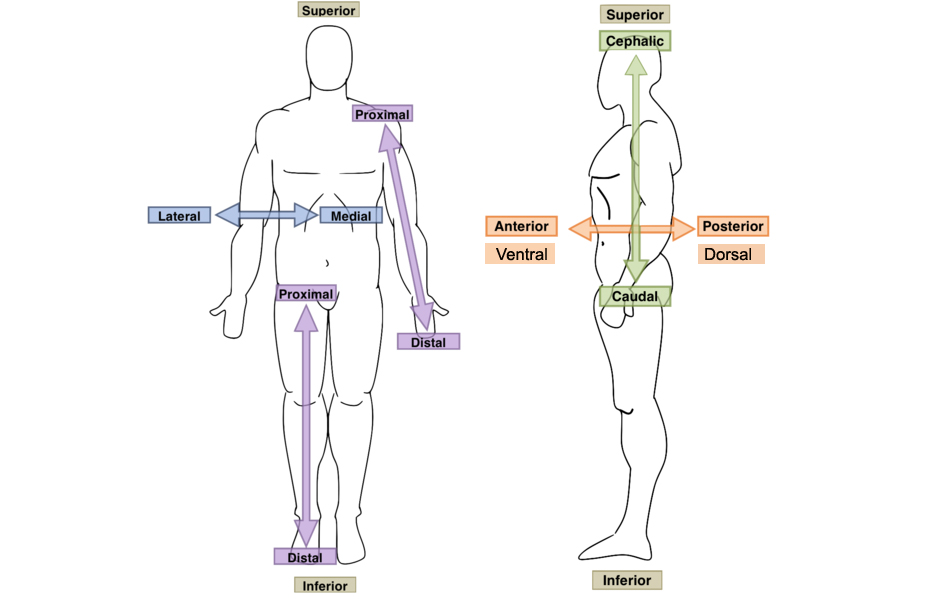
Anatomy and Physiology
ECV can be attempted with malpresentation of the fetus such as breech, transverse and oblique presentations. Complete breech occurs when the fetus has the buttocks as the presenting part and the knees are flexed with the feet near the buttocks. Frank breech occurs when the buttocks are the presenting part, and the legs are extending with the feet near the fetal head. Incomplete breech involves one bent leg and one extended leg. Transverse presentations occur when the long axis of the fetus is at a right angle to the mother with the fetal head to one side of the maternal abdomen and the back noted to be either be up or down in relation to the rest of the fetal body. Oblique presentation is when the long axis of the fetus is at a 45-degree angle to the mother, with the fetal head usually in the right or left lower quadrants.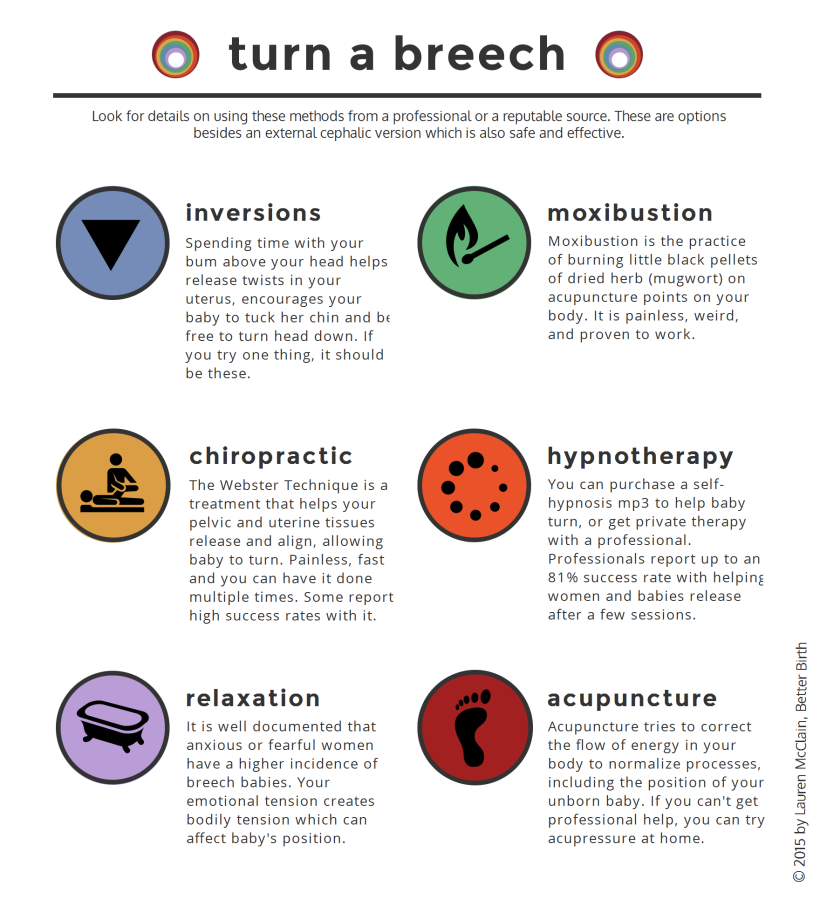
Indications
Indications for ECV include a fetus with greater than 36 weeks of gestation with malpresentation, reassuring fetal status, and no contraindications to vaginal delivery. Most practitioners will proceed with ECV at 37 weeks to decrease the risk of preterm delivery. Factors that may increase success include multiparity, transverse or oblique presentation, complete breech, adequate amniotic fluid, and unengaged presenting part. Factors that are associated with decreased success include nulliparity, advanced dilation, estimated fetal weight of less than 2,500 grams, anterior, lateral or cornual placenta, decreased amniotic fluid or ruptured membranes, maternal obesity, frank breech, fetal spine in the posterior position, and low station with an engaged presenting part.[3]
One alternative to ECV is expectant management with possible spontaneous version, although most fetuses that will spontaneously change presentations to vertex will do so before 36 weeks gestation and are noted more often in multiparous than nulliparous women. Other alternatives are expectant management with a vaginal or cesarean delivery of the breech fetus.
Other alternatives are expectant management with a vaginal or cesarean delivery of the breech fetus.
Contraindications
Any contraindication to vaginal delivery would also be a contraindication to ECV. These include but are not limited to placenta previa, vasa previa, active genital herpes outbreak, and prior classical cesarean delivery. Prior low transverse cesarean delivery is not a contraindication to external cephalic version, although not much data is available on uterine rupture rates.[4]
Antepartum ECV is contraindicated in multiple gestations, although it can be utilized for delivery of the second twin.[5]
Consideration should be used in patients with severe oligohydramnios, nonreassuring fetal monitoring, hyperextended fetal head, significant fetal or uterine anomaly, fetal growth restriction, and maternal hypertension due to these situations being associated with a low likelihood of success of ECV and possible increased risk to the fetus from the procedure.
If a woman presents in labor with malpresentation, ECV could be a reasonable option if she is in early labor, the presenting part is unengaged, there is a normal amniotic fluid index, and no contraindications to vaginal delivery or ECV.
Equipment
Not much equipment is necessary for this procedure as it is performed with the physician's own hands. Fetal monitoring and ultrasonography are necessary components for safety and reassurance.
Personnel
An obstetrician experienced in external cephalic version is needed to perform an ECV. The procedure can be performed by one or two people. Not necessary in the room, but those that should be aware of the ECV procedure would be those needed in case of emergency cesarean delivery, such as nursing, operating room, and anesthesia staff.
Preparation
In preparation for ECV, the fetal presentation must be determined by ultrasound and fetal well-being must be assessed, usually by a nonstress test. Contraindications are reviewed with the patient to confirm that they have none.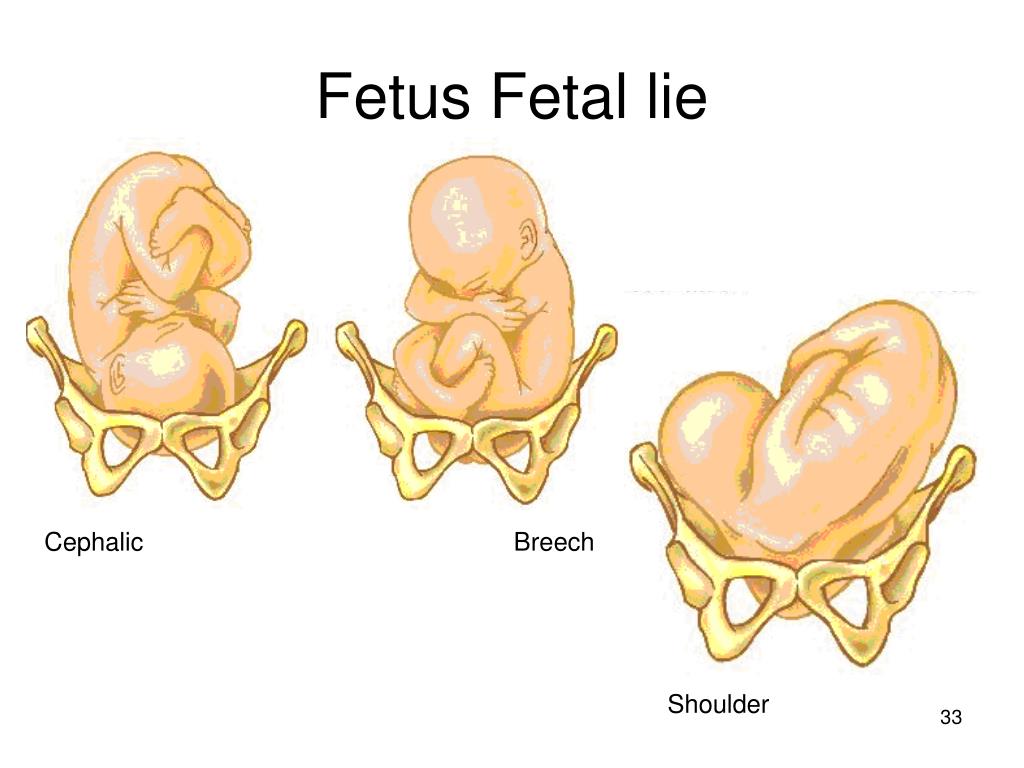 Risks, benefits, and alternatives are reviewed with the patient, and informed consent is obtained. Rh status should be known before the procedure and anti-D immune globulin administered after the procedure if indicated.
Risks, benefits, and alternatives are reviewed with the patient, and informed consent is obtained. Rh status should be known before the procedure and anti-D immune globulin administered after the procedure if indicated.
Technique
Some practitioners choose to administer a tocolytic, usually terbutaline 0.25 mg subcutaneously, 15 to 30 minutes before the procedure, if are no contraindications. Data does not support either calcium channel blockers or nitroglycerin for tocolysis in this situation.[6] Some practitioners choose to use regional anesthesia in the form of either a spinal or epidural, but data is insufficient to recommend this for all external cephalic version attempts, although it may add to success if tocolysis alone is not successful.[7]
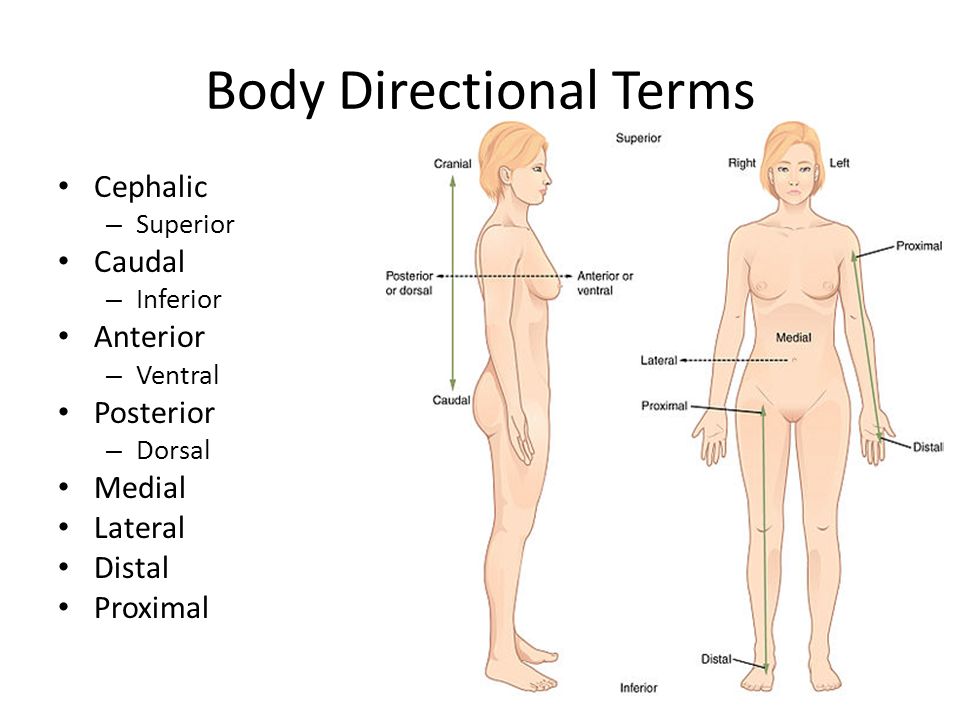
The patient is lying supine, with a sideways tilt with a wedge to keep pressure off the aorta and vena cava. If the fetal presentation is breech, then the breech is lifted out of the pelvis with one hand, and the other hand is used to apply pressure to the back of the fetal head to attempt a forward roll.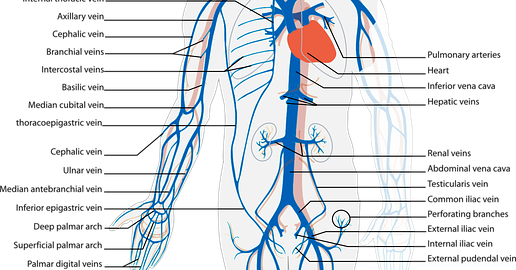 If a forward roll is unsuccessful, then a backward roll can be attempted. If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to attempt to move the fetal head to the pelvis, noting a shorter distance to move than if the fetus is in a breech presentation.[8]
If a forward roll is unsuccessful, then a backward roll can be attempted. If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to attempt to move the fetal head to the pelvis, noting a shorter distance to move than if the fetus is in a breech presentation.[8]
Intermittent use of ultrasonography during the procedure can be used to document fetal heartbeat and current presentation. The procedure should be abandoned if there is significant fetal bradycardia, discomfort to the patient, or if the procedure is not completed easily. Afterward, the patient should be monitored for at least 30 minutes, with fetal heart rate tracing and anti-D immune globulin given if indicated. Immediate induction is not recommended to minimize reversion, although this could be considered after 39 weeks of gestation. If ECV is unsuccessful, additional attempts can be made at the same admission or in one or more days following the initial procedure.
Complications
The most common complications associated with ECV are fetal heart rate abnormalities, occurring at a rate of 4.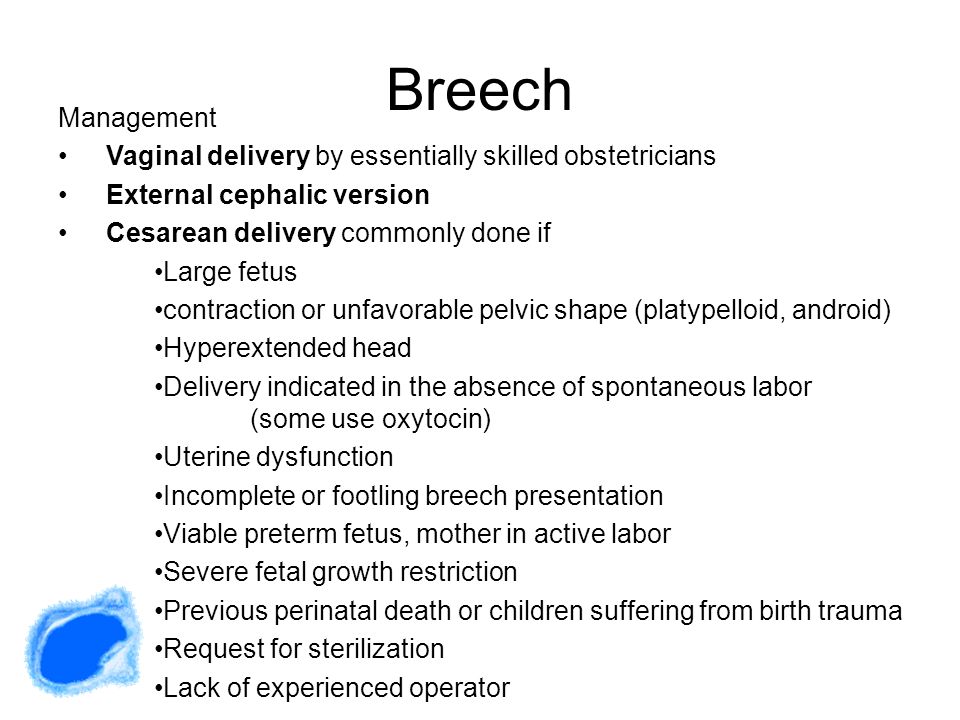 7%, but these usually are transient and improve upon completion or abandonment of the procedure. More severe complications of ECV occur at a rate of less than 1% and include emergency cesarean section, premature rupture of membranes, cord prolapse, vaginal bleeding, placental abruption, fetomaternal hemorrhage, and stillbirth. Although complications are rare, ECV should be attempted in locations where an emergency cesarean section can be performed. For this reason, some practitioners chose to perform ECV in the operating room, although this is not necessary.[9]
7%, but these usually are transient and improve upon completion or abandonment of the procedure. More severe complications of ECV occur at a rate of less than 1% and include emergency cesarean section, premature rupture of membranes, cord prolapse, vaginal bleeding, placental abruption, fetomaternal hemorrhage, and stillbirth. Although complications are rare, ECV should be attempted in locations where an emergency cesarean section can be performed. For this reason, some practitioners chose to perform ECV in the operating room, although this is not necessary.[9]
Clinical Significance
Patients should be counseled on and offered ECV when appropriate. Some data show that only 20% to 30% of eligible candidates are offered ECV.[10]
Women who have a successful ECV have a lower cesarean delivery rate than women who do not, although they are still at a higher risk of cesarean delivery than women with cephalic presenting fetuses and no ECV. ECV is cost effective if the probability of a successful ECV is greater than 32%.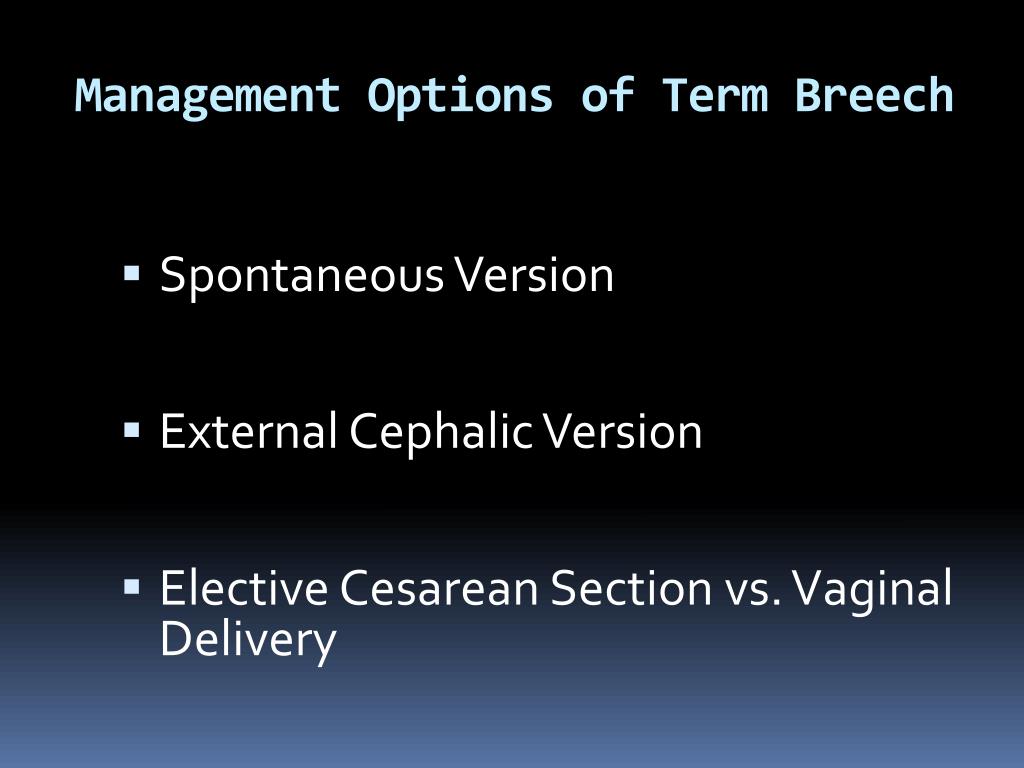
Enhancing Healthcare Team Outcomes
ECV is best performed by an interprofessional team. The actual procedure is performed by an experienced obstetrician aided by a labor and delivery nurse. This is not a benign procedure and it is recommended that the operating room be informed of the ECV procedure, in case of emergency cesarean delivery, such as nursing, operating room, and anesthesia staff. Fetal monitoring is necessary and steps to ensure safety must be paramount.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Levin G, Rottenstreich A. Re: External cephalic version at term: a cohort study of 18 years' experience: External cephalic version at term: a need for modifiable predictor. BJOG. 2019 Apr;126(5):675. [PubMed: 30575279]
- 2.
Nalam RL, Chinnachamy P, Emmanuel P. External Cephalic Version: A Dying Art Worth Reviving.
 J Obstet Gynaecol India. 2018 Dec;68(6):493-497. [PMC free article: PMC6207544] [PubMed: 30416278]
J Obstet Gynaecol India. 2018 Dec;68(6):493-497. [PMC free article: PMC6207544] [PubMed: 30416278]- 3.
What factors determine the success of an external cephalic version? BJOG. 2019 Mar;126(4):501. [PubMed: 30729658]
- 4.
Rosman AN, Guijt A, Vlemmix F, Rijnders M, Mol BW, Kok M. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [PubMed: 22994660]
- 5.
Bogner G, Wallner V, Fazelnia C, Strobl M, Volgger B, Fischer T, Jacobs VR. Delivery of the second twin: influence of presentation on neonatal outcome, a case controlled study. BMC Pregnancy Childbirth. 2018 May 18;18(1):176. [PMC free article: PMC5960113] [PubMed: 29776396]
- 6.
Mohamed Ismail NA, Ibrahim M, Mohd Naim N, Mahdy ZA, Jamil MA, Mohd Razi ZR. Nifedipine versus terbutaline for tocolysis in external cephalic version. Int J Gynaecol Obstet. 2008 Sep;102(3):263-6.
 [PubMed: 18554601]
[PubMed: 18554601]- 7.
Carlan SJ, Dent JM, Huckaby T, Whittington EC, Shaefer D. The effect of epidural anesthesia on safety and success of external cephalic version at term. Anesth Analg. 1994 Sep;79(3):525-8. [PubMed: 8067558]
- 8.
Nagy J, Huvar I. [External cephalic version in breech presentation of fetus]. Ceska Gynekol. 2004 Nov;69(6):444-51. [PubMed: 15633412]
- 9.
Rodgers R. External cephalic version is associated with a low complication rate. BJOG. 2019 Mar;126(4):500. [PubMed: 30461156]
- 10.
Rauf B, Nisa M, Hassan L. External cephalic version for breech presentation at term. J Coll Physicians Surg Pak. 2007 Sep;17(9):550-3. [PubMed: 17903404]
Surgical treatment of patients with intracranial aneurysms of the brain
Science
The Scientific Center of Neurology invites surgical treatment of patients with stenosis of the carotid and vertebral arteries and intracranial aneurysms of the brain
For consultations and hospitalization, please call tel.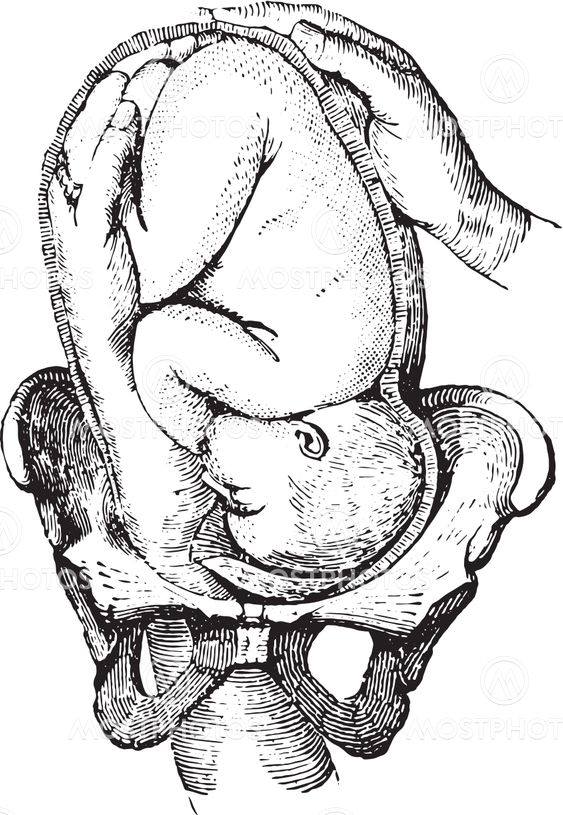 8-495-374-77-76 .
8-495-374-77-76 .
APPOINTMENT FORM...
WHAT IS ANEURYSM AND WHY DOES IT OCCUR?
Aneurysm is a local enlargement of a cerebral vessel of different shape and length.
The main causes of cerebral aneurysms are considered to be:
- High BP
- Atherosclerosis
- Genetic factor
- Infectious diseases
The presence of bad habits, smoking and alcohol abuse increases the risk of developing an aneurysm several times.
Intracranial aneurysms are most often located at the base of the brain. But the defeat of smaller arteries on the surface of the cerebral hemispheres or in the thickness of the brain tissue is not excluded. Allocate aneurysms of the internal carotid artery, middle cerebral, anterior cerebral and communicating arteries, vessels of the vertebrobasilar basin (circle of Willis). In some cases, the presence of symmetrical defects is noted.
CLINICAL MANIFESTATIONS OF CEREBRAL ANEURYSM
Almost all vascular diseases of the brain have common symptoms - cerebral aneurysm is no exception.
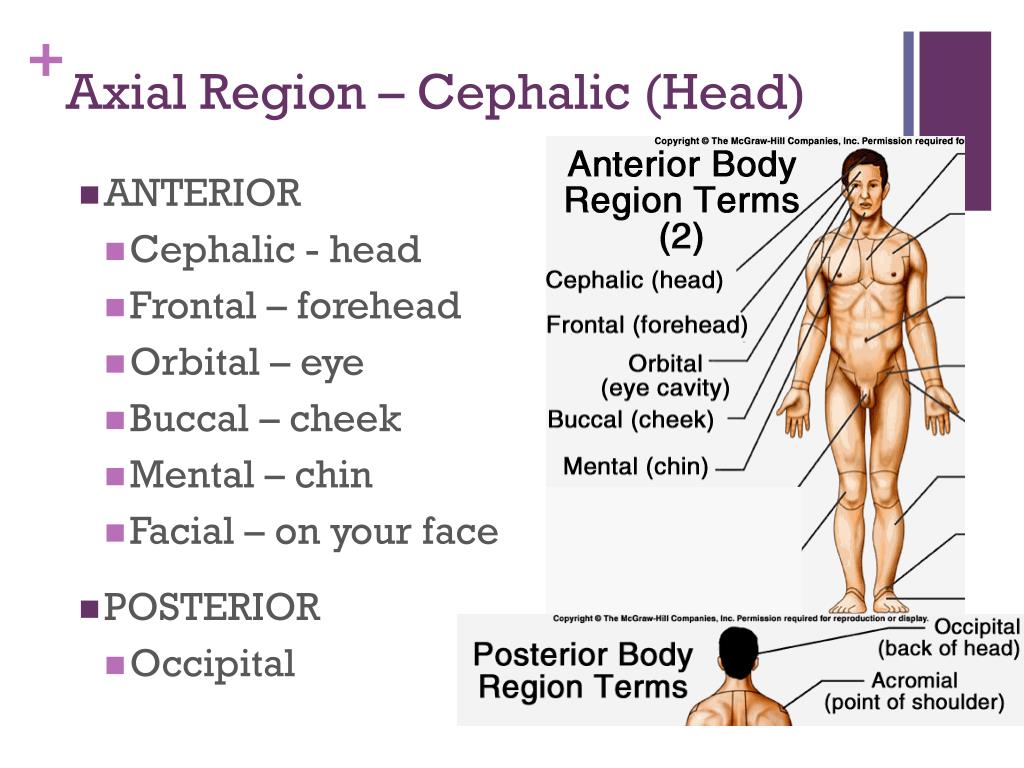
The appearance of neurological symptoms is associated with compression of various nerve formations by the aneurysm: cranial nerves, parts of the brain, nearby vessels. The most common complaint of people with intracranial vascular anomalies is headache (cephalgia). It can have a different character, localization and intensity. Migraine-like pains are possible with the capture of half of the head, pain in the back of the head, neck or eyeball. Localization of discomfort depends on the location of the aneurysm. If the liquor flow is disturbed, a hydrocephalic syndrome may develop due to an increase in intracranial pressure, accompanied by a diffuse headache with a feeling of pressure on the eyeballs and nausea.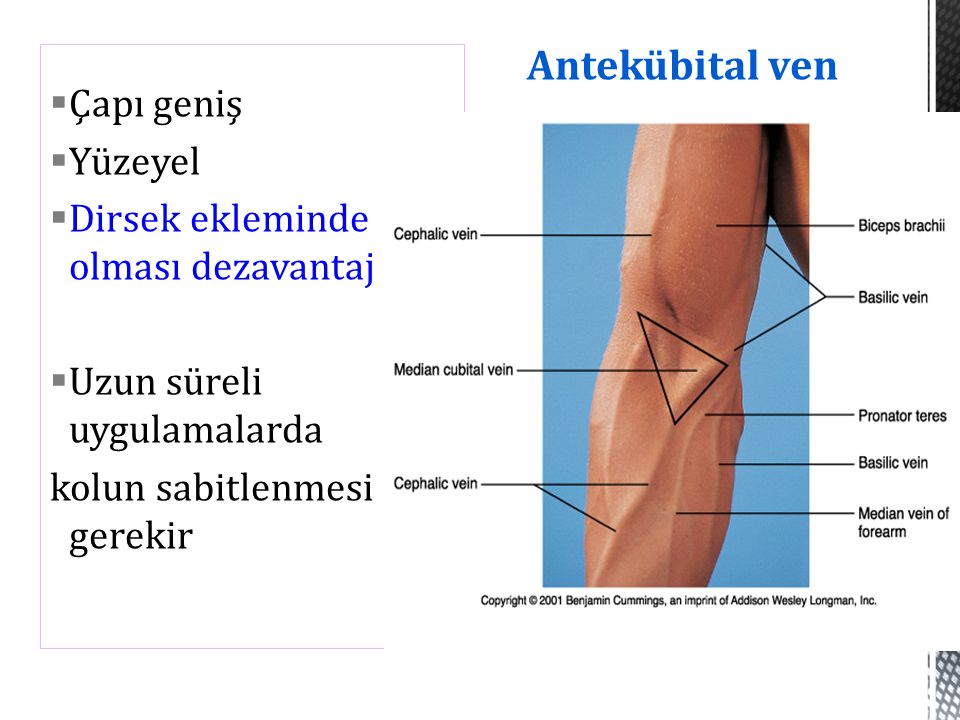
Cephalgia can be combined with signs of compression (compression) of certain cranial nerves or areas of the brain:
- double vision (diplopia) in the horizontal plane with impaired abduction of the eyeball outward in case of damage to the abducens nerve by an aneurysm in the cavernous sinus;
- oculomotor disorders, combined with ptosis, unilateral constriction of the pupil and a decrease in its reaction to light, occur when the oculomotor nerve is damaged by a large aneurysm in the junction of the internal carotid and anterior communicating arteries, or an aneurysm of the superior choroidal artery;
- loss of visual fields due to compression of the optic nerve or the outer part of the chiasm by a supra-sphenoid aneurysm of the internal carotid artery or an aneurysm in the bifurcation of this vessel;
- peripheral paresis of the facial nerve (with drooping of the lower eyelid, impaired tear production and severe facial asymmetry) due to pressure from an aneurysm of the basilar artery;
- unilateral facial pain with loss of sensation when the trigeminal nerve is compressed by an aneurysm located within the cavernous sinus;
- hemiparesis or hemiplegia with unilateral pyramidal symptoms, impaired sensitivity and decreased ability to voluntarily move with intracerebral hematoma or steal syndrome of the motor cortex;
- bulbar syndrome with an aneurysm located in the posterior cranial fossa;
- various forms of aphasia (speech disorders) and other disorders of cortical functions;
- emotional lability, emotional and volitional disorders with decreased drive control or apathy, mnestic decline, pseudobulbar syndrome in case of damage to the frontal lobes and hypothalamus by aneurysms of the anterior cerebral or anterior communicating artery, including intracerebral localization.

DIAGNOSTICS OF ANEURYSMS OF BRAIN VESSELS
To identify an aneurysm and choose the right treatment tactics, it is necessary to conduct a complete diagnosis of the patient, including spiral computed tomography (CT), magnetic resonance imaging (MRI), and radiopaque angiography of cerebral vessels. Accurate research results allow the neurologist and neuroangiosurgeon to choose the most appropriate treatment method.
- CT and MRI - tomography allows you to quickly determine the rupture of the aneurysm. Results can be obtained a few minutes after the tomography, which can play an important role in saving the patient.
- A referral for CT can also be issued if other pathologies are suspected during differential diagnosis. MRI shows what exactly led to the development of changes in the structure of blood vessels. This procedure is also performed after surgery. The picture clearly shows the consequences after the operation to remove cerebral aneurysms.
- Angiography - allows you to accurately determine the location and degree of vascular damage. With the help of angiography, it is possible to determine whether surgical repair of the aneurysm is necessary or whether conservative treatment can be dispensed with. The disadvantage of this type of research is the high complexity of manipulations. With the introduction of contrast into the blood, allergic reactions are possible. The revealed aneurysm is a “time bomb”, which sooner or later, but will certainly lead to rupture of the vessel and subarachnoid or intracerebral hemorrhage (hemorrhagic stroke). If surgical treatment is not carried out in a timely manner, the consequences of an aneurysm can be catastrophic.
- Coma after aneurysm rupture - occurs due to blood entering the subarachnoid space and mixing with cerebrospinal fluid
- Fatal outcome. About 75% of patients die at the preoperative stage. The probability of death after the operation is reduced to 15%.
 Sudden angiospasm of blood vessels is the cause of stroke, death, or with a favorable outcome of the patient's disability.
Sudden angiospasm of blood vessels is the cause of stroke, death, or with a favorable outcome of the patient's disability.
HOW TO TREAT ILLNESS
Surgery is the only effective treatment for cerebral aneurysm therapy. After receiving the results of the examination of the patient, the surgeon decides on the appropriateness of the surgical operation. Since the consequences of a ruptured cerebral aneurysm are fatal, surgical intervention can save the patient's life.
Beforehand, the surgeon discusses the possible risks and outcomes of the disease together with the patient, and determines the appropriate method of treatment. According to the indications, the following types of operations are prescribed:
- Aneurysm clipping - the procedure is carried out as follows: a hole is cut out in the skull, through which a special metal clip is inserted and the wall of the damaged vessel is clamped. Life after clipping has many restrictions, the patient is assigned a disability group.
In addition, this type of surgery does not prevent the formation of a recurrent aneurysm
- Aneurysm embolization is one of the most common methods of disease control.
Conducting intravascular spiral embolization is possible with saccular aneurysm and a small lumen of the anastomosis. With a wide lumen, simultaneous placement of a stent (closure of the lumen) with subsequent spiral embolization of the aneurysm is possible. In any case, the neuroradiosurgeon chooses tactics after angiography.
Embolization of the aneurysm leads to the cessation of blood flow in the aneurysm (protrusion), while maintaining normal blood flow through the cerebral artery. In the process of embolization, a catheter is inserted under radiological control through a convenient vascular access (usually inguinal) and carried to the aneurysm. Then, a thinner micro-catheter with a wire microcoil laid inside it is inserted into the catheter and inserted into the aneurysm cavity.
As soon as the tip of the microcatheter is in the cavity of the aneurysm, the microcoil is released from the microcatheter, which changes its shape and occupies the cavity of the aneurysm in the form of a random coil of wire. Larger aneurysms may require multiple coils. An aneurysm filled with a wire spiral is switched off from the bloodstream and gradually overgrown with connective tissue, that is, the possibility of its rupture is excluded.
In most cases, endovascular embolization is currently the least invasive treatment for cerebral aneurysms. If it is not possible to perform intravascular embolization or stenting, the usual neurosurgical operation of vessel stenting or aneurysm clamping can be performed.
06/22/2017
MRI for hydrocephalus of the brain in adults, the effectiveness of MRI for hydrocephalus
With the help of magnetic resonance imaging, changes in the pathological nature of the brain tissue are detected at the initial stages. The technique makes it possible to timely determine the type and extent of pathologies, prescribe adequate treatment. MRI for hydrocephalus is informative at any stage, even if the disease has not yet manifested itself.
The technique makes it possible to timely determine the type and extent of pathologies, prescribe adequate treatment. MRI for hydrocephalus is informative at any stage, even if the disease has not yet manifested itself.
Features and mechanism of development of the disease
Hydrocephalus or dropsy of the brain is a disease that is accompanied by the accumulation of excess cerebrospinal fluid inside the ventricles, in the intrathecal cerebral spaces and leads to their expansion, and also causes an increase in intracranial pressure.
Cerebrospinal fluid is produced in the ventricles of the brain. It serves as a kind of pillow, protects the brain, spinal cord, delivers nutrients, and is responsible for removing waste. Normally, fluid moves before being absorbed into the bloodstream. With hydrocephalus, its movement is blocked, and absorption is limited. In the absence of adequate treatment, complications develop, up to a fatal outcome.
Types of disease
There are several types of cerebral hydrocephalus.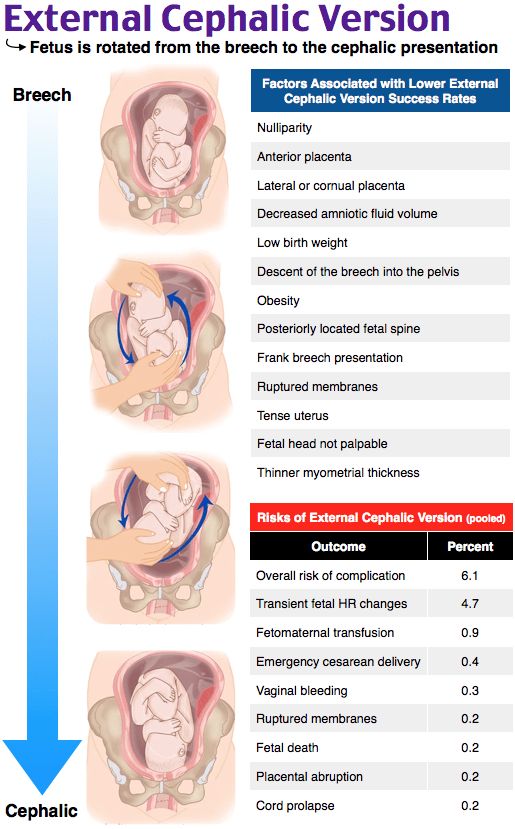 Pathology is congenital and acquired. The first progresses under the influence of unfavorable factors during fetal development. The second is formed under the influence of various pathologies and external factors.
Pathology is congenital and acquired. The first progresses under the influence of unfavorable factors during fetal development. The second is formed under the influence of various pathologies and external factors.
According to the place of localization the disease can be:
- External – with fluid accumulation under the meninges;
- Internal - with impaired outflow of CSF from the ventricles;
- General - combines the features of both previous forms.
According to the mechanism of development, hydrocephalus can be open, with the preservation of the connection between the ventricular system and the subarachnoid space, or closed, with a violation of this connection.
Forms of pathology
The form of hydrocephalus determines the nature of the course of the disease, its severity. For classification, the following criteria are most often used:
- The intensity of the manifestation of pathology - in case of severe, a lot of fluid accumulates, which disrupts the activity of the nervous system.
 In this case, the disease is accompanied by severe neurological symptoms. A moderate degree is characterized by the accumulation of a small volume of cerebrospinal fluid and the absence of symptoms;
In this case, the disease is accompanied by severe neurological symptoms. A moderate degree is characterized by the accumulation of a small volume of cerebrospinal fluid and the absence of symptoms; - The degree of impact on brain structures - in the compensated form, the fluid does not affect the brain; in the decompensated form, it impairs its functioning;
- The nature of the course - hydrocephalus of the brain in a chronic form is accompanied by a gradual increase in symptoms, in an acute form it leads to a sharp deterioration in a person's condition.
Determining the type of disease, its form and features of development allows modern diagnostic measures.
Stages of development
External hydrocephalus has 3 stages of development, each of them has its own signs:
- Mild – dropsy is small, the body tries to cope with CSF flow disturbances. A person usually feels a not too intense headache, he periodically feels dizzy, his state of health worsens slightly, sometimes it gets dark in his eyes;
- Moderate - manifestations become more noticeable, the intensity of headaches increases, especially during physical exertion.
 Violations of visual function, rapid onset of fatigue, pressure drops, depression and severe irritability are possible;
Violations of visual function, rapid onset of fatigue, pressure drops, depression and severe irritability are possible; - Severe - at this stage, hydrocephalus of the brain can cause convulsive seizures, apathy, fainting, apathy, and also lead to the development of conditions in which a person is no longer capable of self-care.
At the initial stages of the development of the pathology, neurological symptoms may be absent. They appear due to organic processes that occur in the cerebral substance, as well as against the background of circulatory disorders and atrophy of some areas.
Hydrocephalus in children
The signs of hydrocephalus are determined by the age of the person and the stage of the disease. In children, including newborns, the development of pathology can be indicated by capricious behavior and poor appetite, marbled skin and slow reactions, retraction of the eyelid and a look almost always directed downwards, as well as swelling of the fontanel and excessively enlarged head sizes.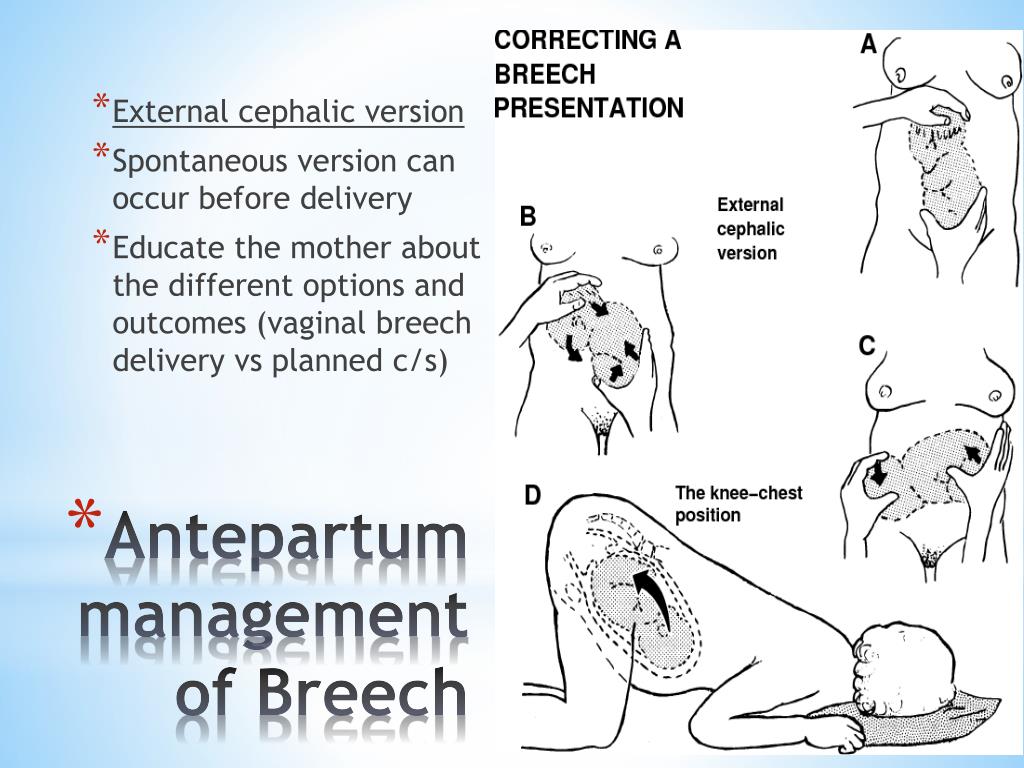
It is the size and shape of the child's head that often indicate pathological processes. By the age of six months, in babies with hydrocephalus, the head circumference is greater than the chest, the skull becomes oblong, pear-shaped, and this is noticeable to the naked eye.
With hydrocephalus in children, the normal functioning of the brain is blocked, which leads to a lag in mental, physical, mental development. The risk of pathology increases in newborns who were born prematurely with low body weight. The cause can also serve as birth intracranial trauma, infectious diseases suffered by the mother during pregnancy.
A child with this disease later than his peers begins to roll over, hold his head, sit down. In a severe form of pathology, these skills are not formed, muscle strength in the limbs decreases up to paralysis, and muscle tone increases. After the fusion of the fontanelles, the head begins to hurt a lot, more often in the morning, frequent vomiting, nosebleeds.
Symptoms of the disease in adults
Hydrocephalus in adults is manifested by:
- Headaches in which neither sleep nor drugs with analgesic effect save;
- Nausea, feeling like vomiting;
- Feeling constantly tired;
- An abrupt change of mood, a tendency to irritability;
- Changes in behavior;
- Clouding of consciousness, difficulty with memory, thought process;
- Disequilibrium;
- Inability to control urination;
- Seizures and convulsions;
- Sleep disorders;
- Appetite problems;
- Blurred vision, feeling of double vision, downward movement of the eyeballs.
Headache in hydrocephalus is aggravated by changing from horizontal to vertical position. Fluctuations in blood pressure are possible. With normotensive hydrocephalus, signs of dementia, urinary incontinence, and walking disorders appear in combination with a pronounced expansion of the ventricles of the brain, but without an increase in CSF pressure.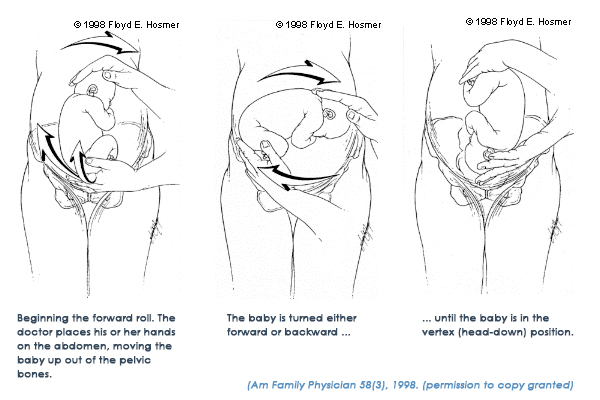
Causes of pathology
The main causes of hydrocephalus in adulthood are:
- Pathologies of the vascular system;
- Diseases of an infectious nature;
- Neurosurgical operations;
- Head injuries;
- Tumor processes;
- Previous stroke;
- Anomalies in the development of the central nervous system.
Hydrocephalus can be a complication of meningoencephalitis, meningitis, aneurysm rupture or intraventricular hemorrhage, cyst or tumor formation in the brain.
Hydrocephalus in adults may be caused by regular intoxication, such as frequent drinking. Alcohol has a damaging effect on neurons, because of this, tissue sections die off. An increased risk is created by chronic diseases in the form of multiple sclerosis, diabetes, metabolic disorders, and encephalopathy. Often, the disease develops against the background of age-related changes in the body associated with the aging of brain tissues and blood vessels.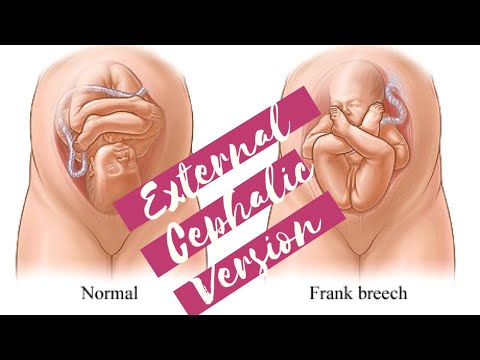
Effectiveness of MRI in hydrocephalus
Magnetic resonance imaging is used to diagnose hydrocephalus. This is the most informative imaging method that allows you to establish an accurate diagnosis, regardless of the stage of pathology.
The essence of MRI is to obtain layered images of the area used by scanning. The principle of operation of tomography is associated with the influence of a magnetic field and the fixation of radio frequencies emanating from the human body.
Unlike x-rays, MRI does not harm the body. This is a non-invasive and absolutely safe method that allows you to obtain high quality images, including three-dimensional ones. They clearly show brain tissues of different density and the boundaries between them, neoplasms and blood vessels. Thanks to the study in several projections at a given depth, it becomes possible to assess the state of any part of the brain.
How is the procedure carried out?
Brain MRI with or without contrast enhancement.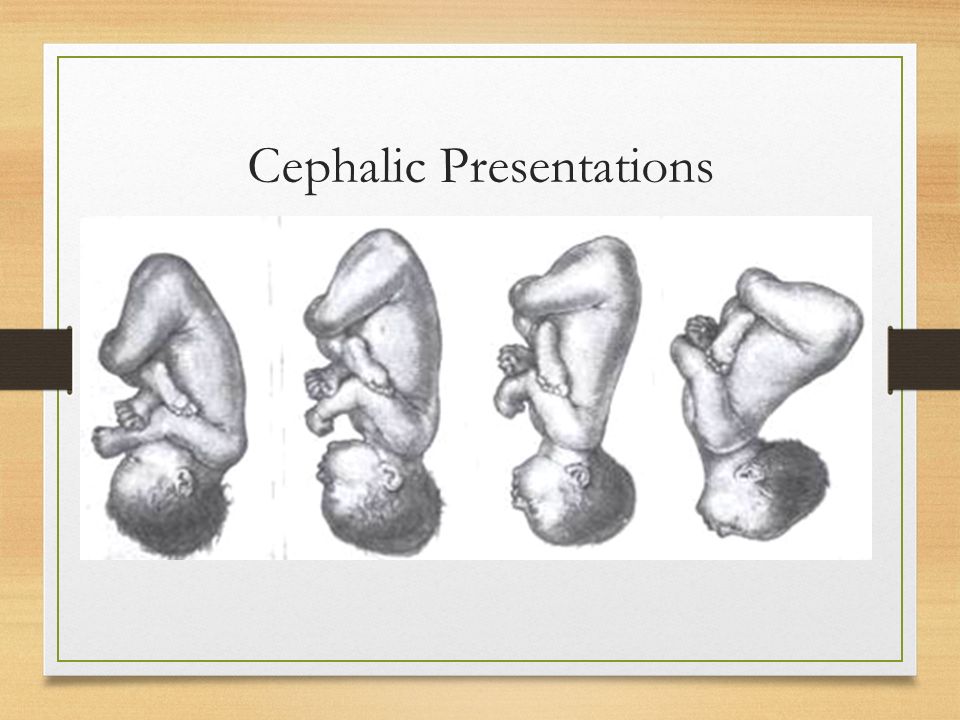 In the first case, special preparations are administered intravenously to the patient, which create a clear image of the affected areas and improve the quality of visualization. For example, with this approach, not only the tumor itself is clearly visible, but also its exact boundaries.
In the first case, special preparations are administered intravenously to the patient, which create a clear image of the affected areas and improve the quality of visualization. For example, with this approach, not only the tumor itself is clearly visible, but also its exact boundaries.
No special preparation is required for the procedure, but all metal jewelry must be removed before starting the procedure. The tomography machine itself looks like a large cylinder, inside of which there is a movable platform. The patient lies on it lying on his back. Ear plugs are used to protect against the noise emitted by the device.
The table slides into the scanner, the doctor performs the procedure from a neighboring office, controlling the device using a computer. Throughout the examination, voice communication with the doctor is maintained, so the patient can report unpleasant or uncomfortable sensations at any time.
The tomograph takes a series of images sequentially, which eventually form the finished image.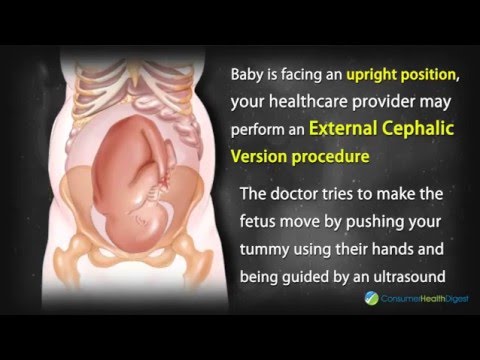 In order for the images to be of high quality, the patient must remain completely still. On average, the procedure takes about 30-45 minutes.
In order for the images to be of high quality, the patient must remain completely still. On average, the procedure takes about 30-45 minutes.
Evaluation of results
This technique makes it possible to detect not only hydrocephalus of the brain, but also concomitant diseases, to accurately determine the type of pathology. The picture shows both direct and indirect signs of the disease. The direct ones include an increase in the ventricles of the brain, subarachnoid space.
Indirect signs are:
- The value of the interventricular index is from 0.5 or more;
- Downward displacement of the hypothalamus;
- Edema with tension dropsy;
- Partial protrusion of the upper part of the lateral ventricles.
Based on the test results, a diagnosis is made and treatment is prescribed. An MRI may show replacement hydrocephalus. This means that a certain amount of fluid is present in the subarachnoid space, but its presence is not a sign of dropsy, but a manifestation of a compensatory mechanism associated with age-related or organic tissue changes.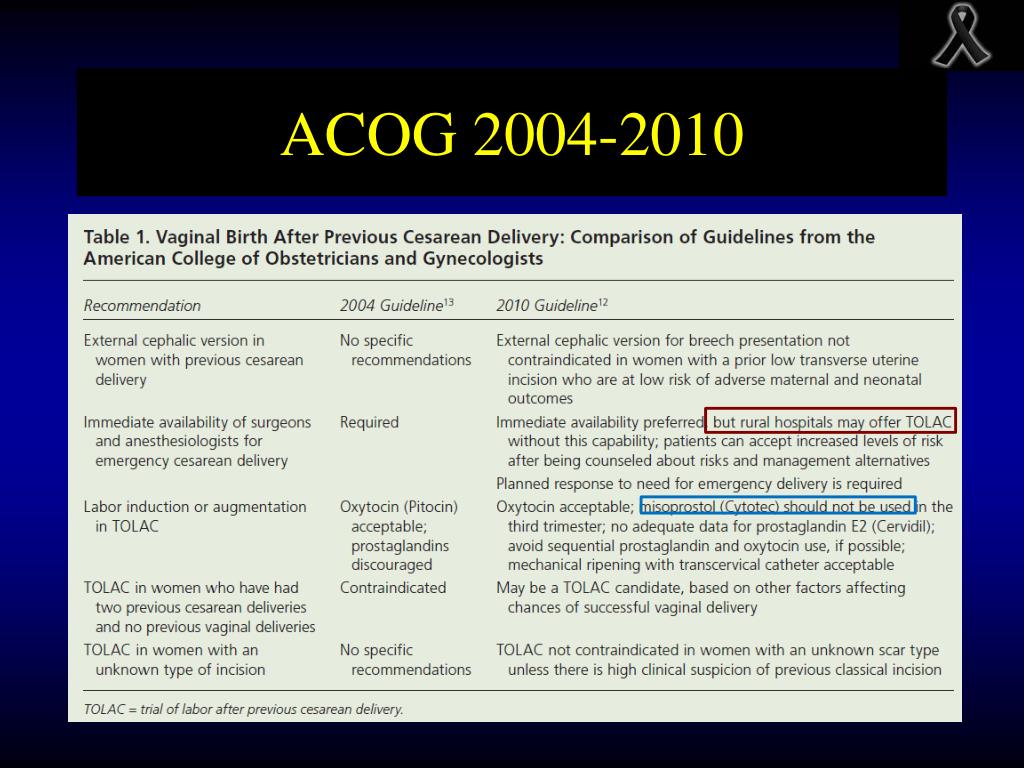
Methods and principles of treatment
The main task is to eliminate the accumulated excess of cerebrospinal fluid in order to restore its normal flow.
In some cases, medication is used. Improvement from conservative treatment of hydrocephalus usually occurs when the disease is a complication of an infectious or inflammatory disease, traumatic impact. When drugs do not give the desired effect, an operation is performed to install special shunts. This element ensures the removal of fluid to the abdominal cavity, where it is absorbed by the body. As a result, pressure decreases, the size of edema in the brain decreases.
Another option for surgical treatment is to create a hole in the 3rd cerebral ventricle for the flow of CSF between brain regions. Both methods allow you to relieve symptoms and block the development of dangerous complications. If the disease is due to the appearance of a tumor, it is removed.
The earlier hydrocephalus is detected, the better the treatment prognosis.