Retained placenta 3 months postpartum
Retained placenta | Pregnancy Birth and Baby
Retained placenta | Pregnancy Birth and Baby beginning of content6-minute read
Listen
It’s important to contact your doctor or medical team as soon as possible if you have any heavy bleeding from your vagina and/or pain in the days or weeks following birth.
If the bleeding and/or pain become significantly worse, call an ambulance on triple zero (000). Or go to your nearest hospital emergency department.
What is retained placenta?
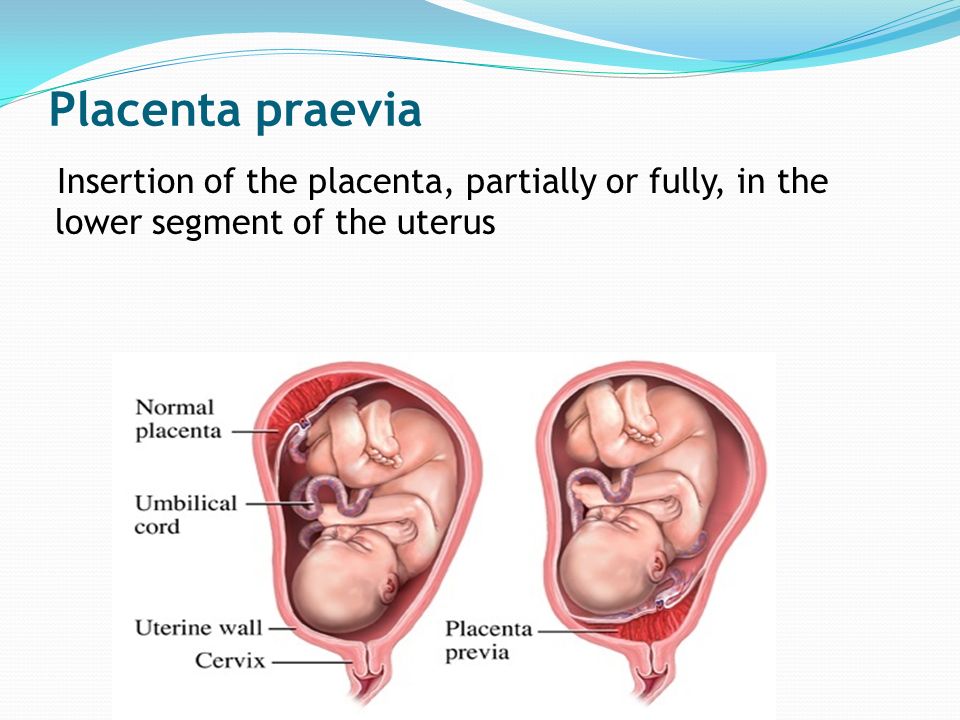
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes, a piece of the placenta is left behind in the uterus (womb). It’s not common, but it can be serious. It can cause problems days or weeks after the birth.
Retained placenta can lead to severe infection or life-threatening blood loss for the mother.
How is the placenta delivered after birth?
After your baby is born, the placenta also needs to be delivered. This is called the third stage of labour.
You may choose to ‘actively manage’ this stage of labour. Meaning that you will receive an injection of Syntocinon (a synthetic version of the hormone oxytocin) to help your uterus contact and birth the placenta. Actively managing your 3rd stage of labour can take up to 30 minutes. This also helps reduce the risk of heavy bleeding from the vagina (called postpartum haemorrhage).
Some women choose not to have the oxytocin injection. This is called ‘expectant management’ or ‘physiological management of the third stage’. It means waiting for the placenta to be born naturally, usually with gravity and some contractions. This may take up to one hour.
It’s important to make an informed decision by discussing the options with your midwife or doctor. You may choose to write your preferences in a birth plan.
You may choose to write your preferences in a birth plan.
What causes retained placenta?
Sometimes the placenta takes longer than expected to be delivered. The placenta can be retained after your baby is born if:
- your contractions aren’t strong enough to expel it
- the placenta is unusually strongly attached to the wall of the uterus
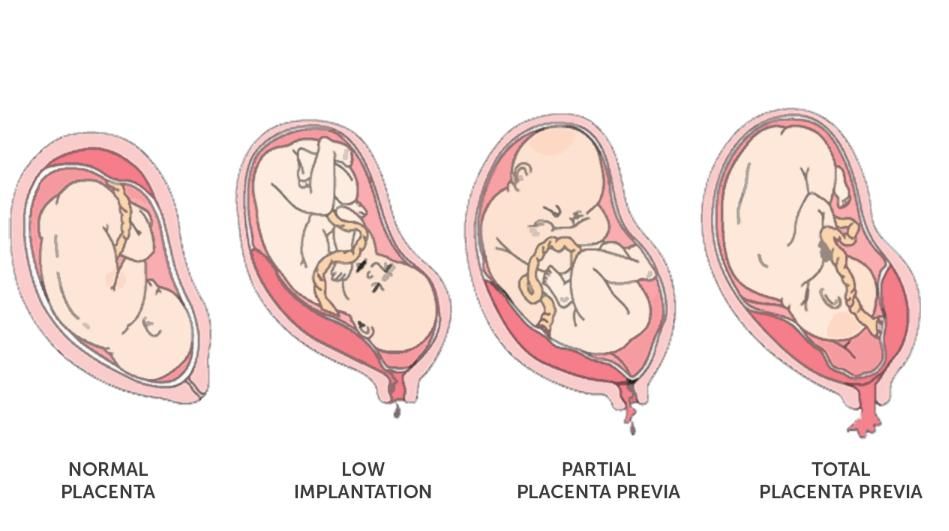
- you have placenta accreta (when the placenta implants too deeply into the wall of the uterus)
- the cervix closes and traps the placenta inside your uterus
What are the signs and symptoms of retained placenta?
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes a piece of placenta is left behind in the uterus. If this happens, you may develop symptoms days or weeks after the birth. These may include:
- fever
- a bad smelling discharge from the vagina
- heavy bleeding
- large pieces of tissue coming out of the vagina
- pain
It’s important to contact your doctor or medical team as soon as possible if you have any heavy bleeding from your vagina and/or pain in the days or weeks following birth.
If the bleeding and/or pain become significantly worse, call an ambulance on triple zero (000). Or go to your nearest hospital emergency department.
How is retained placenta diagnosed?
Your doctor or midwife will diagnose retained placenta if the placenta hasn’t completely come out of the uterus within 30 minutes - if you are actively manage or 1 hour - if you choose physiological management, after a vaginal birth.
At every birth, the midwife or doctor checks the placenta once it’s delivered. This is to check that none has been left in the uterus. But it is not always obvious if a small amount of tissue has been left behind.
If you have symptoms of retained placenta in the days or weeks after birth, your doctor may suspect that a piece of the placenta has been left behind. They may recommend an ultrasound scan. This is to check whether you have any retained placenta.
What is the treatment for retained placenta?
If you have just given birth, retained placenta might be treated by:
- emptying your bladder
- your doctor or midwife gently pulling on the umbilical cord.
If that doesn’t work, you will need a procedure to remove the placenta. You will be taken into surgery after the birth and given an epidural or anaesthetic so you don’t feel anything.
While you’re waiting for surgery, the medical team will keep a close eye on you to check you're not bleeding heavily (postpartum haemorrhage). The procedure itself is quick, but you will need to be monitored for several hours afterwards to make sure you are not bleeding.
It’s not always obvious after the placenta has been delivered that some placenta tissue may have been left behind. If you are bleeding heavily in the days or weeks after birth, you may need imaging tests or surgery to investigate the cause.
If you have an infection, you will need treatment with antibiotics.
What are the complications of a retained placenta?
Retained placenta can be serious. In rare cases, it can lead to life-threatening infection or blood loss (postpartum haemorrhage).
While there is usually some normal blood loss with birth, blood loss associated with retained placenta can be very severe. This is because the area in the uterus where the placenta is still attached can continue to bleed.
This is because the area in the uterus where the placenta is still attached can continue to bleed.
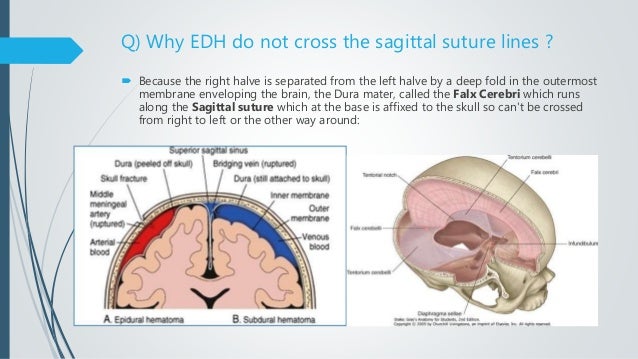
Postpartum haemorrhage can be divided into:
- primary postpartum haemorrhage – this happens within the first 24 hours after delivery
- secondary postpartum haemorrhage – this happens in the days and weeks following birth (between 24 hrs and 6 weeks after birth)
Diagnosing and managing retained placenta early helps prevent complications such as severe blood loss and infection.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Women’s Hospital (Postpartum Haemorrhage), Government of Western Australia NMHS Health (Labour: Third Stage), International Journal of Women's Health (Retained placenta after vaginal delivery: risk factors and management), Cochrane Database of Systematic Reviews (Active versus expectant management for women in the third stage of labour), RANZCOG (Management of Postpartum Haemorrhage PPH)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- About the placenta
Need more information?
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Asherman Syndrome
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Why do some mums stop breastfeeding before 6 months?
Most new parents know 'breast is best', but while more than 9 out of 10 babies are breastfed at birth, few mums are breastfeeding exclusively 5 months later.
Read more on Pregnancy, Birth & Baby website
What is freebirth?
Freebirth is when a woman chooses to birth her baby without medical or midwifery assistance, but this greater independence comes with some risks.
Read more on Pregnancy, Birth & Baby website
About the placenta
The placenta develops inside the uterus (womb) during pregnancy. It gives your baby nutrients and oxygen. Find out more about the placenta here.
Read more on Pregnancy, Birth & Baby website
Postpartum haemorrhage
Postpartum haemorrhage is when you bleed more than normal after giving birth. It can be very serious and requires medical attention right away.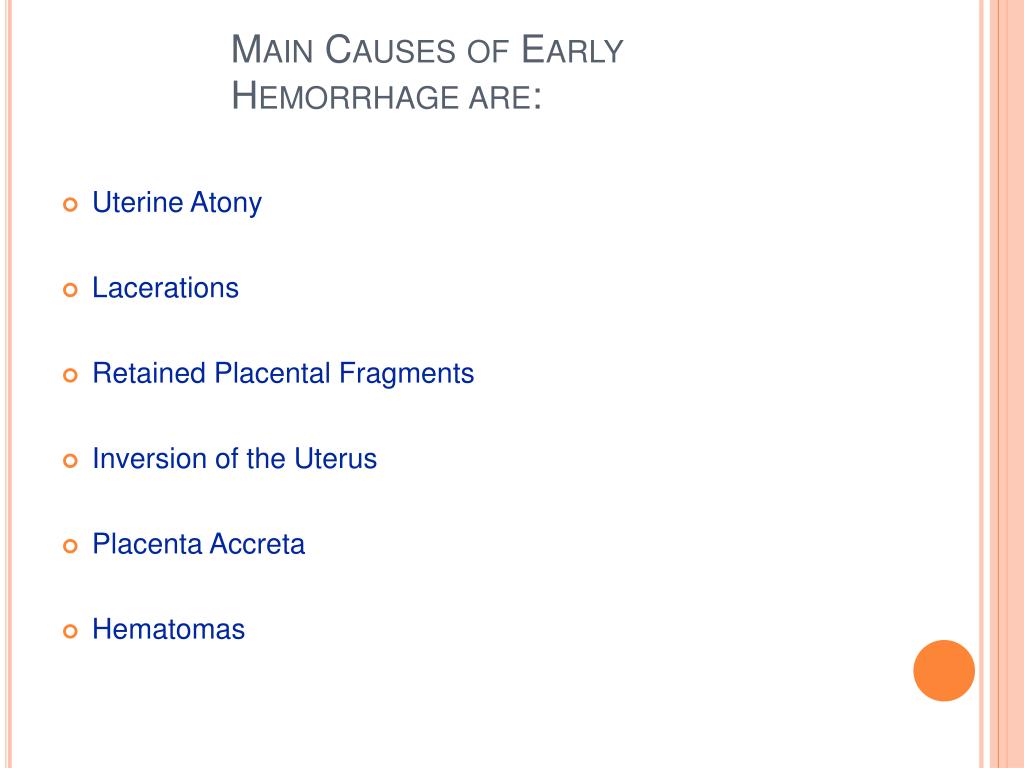
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Placenta after birth: Symptoms of retained placenta
Retained placenta happens when your placenta isn't delivered within 30 minutes of having your baby.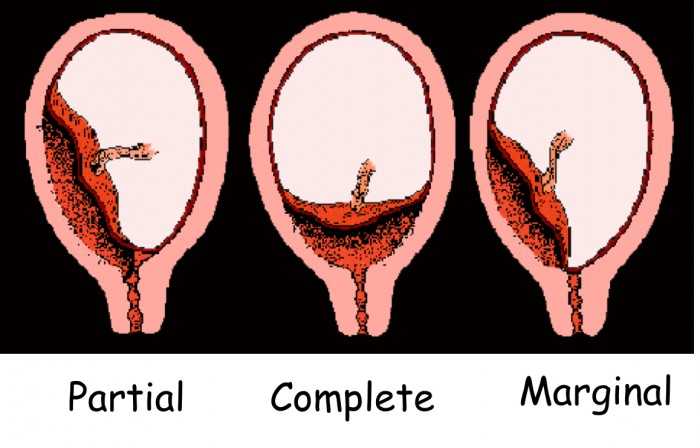 Though it's relatively uncommon and can be effectively treated, the condition does carry a serious risk of postpartum hemorrhage, or severe bleeding after childbirth. If you're diagnosed, your medical team will try several different ways to remove the placenta, with surgery as a last resort. Retained placenta can't be prevented, causes no symptoms when you're pregnant, and won't harm your baby.
Though it's relatively uncommon and can be effectively treated, the condition does carry a serious risk of postpartum hemorrhage, or severe bleeding after childbirth. If you're diagnosed, your medical team will try several different ways to remove the placenta, with surgery as a last resort. Retained placenta can't be prevented, causes no symptoms when you're pregnant, and won't harm your baby.
What is retained placenta?
Retained placenta occurs when your placenta isn't delivered within 30 minutes of vaginal childbirth. It affects up to three percent of vaginal deliveries and is a common cause of postpartum hemorrhage, or heavy bleeding. Left untreated, the condition can be life-threatening.
To understand retained placenta, it helps to know about the third stage of labor, which happens after you've had your baby. During this time, you'll feel a series of frequent, less-intense contractions. These are necessary to separate your placenta from your uterus so it can be delivered. When some or part of it is left behind, it can increase the risk of bleeding and infection later on.
When some or part of it is left behind, it can increase the risk of bleeding and infection later on.
What causes retained placenta after birth?
Retained placenta can be caused by a few issues. These include:
Trapped placenta. Also called an incarcerated placenta, a trapped placenta has disconnected fully from the uterine lining. It isn't delivered, however, because the cervix has closed or started to close too soon. Your provider may be able to see a bit of the trapped placenta through a small opening in the cervix.
Uterine atony. The word “atony” means your muscles lack tone, tension, or energy. With uterine atony, your uterus doesn't contract enough following childbirth, keeping the placenta from being pushed out.
Placenta accreta. In a small number of pregnancies, part or all of the placenta grows deeply into the uterus. As a result, the two organs don't separate in the third stage of labor – creating a major bleeding risk – and a procedure is needed to detach them.
Placenta accreta usually doesn't cause symptoms during pregnancy, though it's occasionally discovered in an ultrasound. In this case, you'll likely deliver via C-section and may need a hysterectomy afterwards. Often, the condition isn't discovered until after you've given birth.
What are the risk factors for retained placenta?
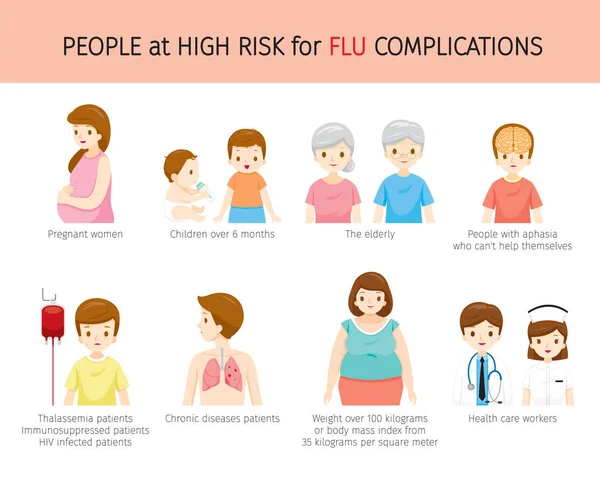
Preterm delivery, especially during the second trimester, is the strongest risk factor for retained placenta. And if you've had the condition once, the odds are higher you'll have it again in future pregnancies.
Other factors may also include:
Advertisement | page continues below
- Maternal age of 30 or older
- IVF pregnancy
- Giving birth more than five times previously
- Prior uterine surgery, including C-section and dilation & curettage
- Uterine abnormality, meaning a malformation of your uterus
- Velamentous cord insertion, or when the placenta and umbilical cord are abnormally attached
- Preeclampsia
- Prolonged labor
- Prolonged use of oxytocin during delivery
- Having a baby who is small for their gestational age
- Stillbirth
Currently, there is no known way for you to lower the odds specifically of retained placenta. However, if you are high-risk, your delivery team can prepare for the possibility. Once you are admitted to a hospital or birthing center, they can run tests and gather the right pain medication and needed equipment, just in case it happens.
However, if you are high-risk, your delivery team can prepare for the possibility. Once you are admitted to a hospital or birthing center, they can run tests and gather the right pain medication and needed equipment, just in case it happens.
What are the symptoms of retained placenta?
You very likely won't have any symptoms of retained placenta prior to delivery. From time to time, women experience bleeding in their third trimester.
The primary symptom is when all or part of the placenta isn't delivered following childbirth, or if you begin bleeding heavily without delivering the placenta.
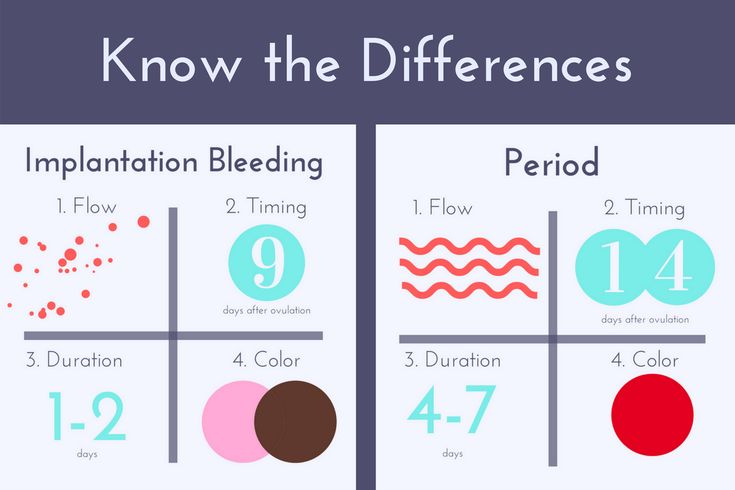
You may notice symptoms up to two weeks after you have your baby. These can include fever, foul-smelling discharge, heavy bleeding, and blood clots or large pieces of tissue coming out of your vagina. Make sure to report them to your provider right away.
Are there serious risks of retained placenta?
Yes. Retained placenta is a major cause of postpartum hemorrhage. The longer it takes you to deliver it, the higher your chances of this complication. If you're at risk, your medical team will prepare the delivery room to manage any serious issues that arise. Delayed postpartum hemorrhage, mentioned above, is another risk.
The longer it takes you to deliver it, the higher your chances of this complication. If you're at risk, your medical team will prepare the delivery room to manage any serious issues that arise. Delayed postpartum hemorrhage, mentioned above, is another risk.
Retained placenta can also lead to postpartum endometritis, which is inflammation or infection of your uterine lining after you give birth. The condition is different from endometriosis, a serious disease in which uterine tissue grows outside of your uterus. Endometritis is treated with antibiotics.
The good news: Retained placenta will have no effect on your baby.
What are the treatments for retained placenta?
First, your provider will try active management. When the placenta isn't delivered within a specific window of time, they'll attempt to move the process along by asking you to push or massaging your abdomen. They may also gently tug on your umbilical cord to loosen the placenta or administer oxytocin. Breastfeeding, peeing, or changing your position can help its delivery, as well.
Breastfeeding, peeing, or changing your position can help its delivery, as well.
Sometimes, active management doesn't work. When it fails, your provider will try to remove the retained placenta using their hands or via surgery. The timing of the procedure depends on your clinician's judgment.
Manual extraction is typically used first. During this procedure, a provider will try to detach the placenta from your uterine wall with their fingers. Then, they'll pull the separated tissue out through your cervix. You'll be given medication to manage pain and an antibiotic to prevent infection. There is a risk of hemorrhage during manual extraction, but your medical team will be prepared.
If manual extraction doesn't succeed – meaning part or all of the placenta remains in your uterus – the next step is surgery. Suction curettage, which involves using a small vacuum to remove tissue from your uterus, is the most common procedure.
If you have placenta accreta, there's a small risk that it's not possible to separate your placenta and uterus. Since trying it can cause a massive hemorrhage, hysterectomy may be necessary.
Since trying it can cause a massive hemorrhage, hysterectomy may be necessary.
This is uncommon, however, and the bottom line remains: Though retained placenta comes with serious potential health risks, it can be managed by your healthcare team – and won't harm your baby. If you have questions or concerns about your risk of retained placenta, or how it might affect your labor and delivery (and your postpartum recovery), talk with your healthcare provider.
Complications after childbirth - causes and consequences
- Increased discharge
- Retention of part of the placenta in the uterine cavity
- Changes in the blood coagulation system
- Disorder of uterine muscle contraction
- Inflammatory process in the vagina or uterus
- Vaginal candidiasis (thrush)
- Postpartum endometritis
- Laktostasis and mastitis
- Postpartum pyelonephritis
- Venous thrombosis
- Discomfort in the area of postoperative sutures
- Urinary incontinence, feces, uterine prolapse
- Hemorrhoids
After giving birth, a woman often thinks that all worries and anxieties are behind her.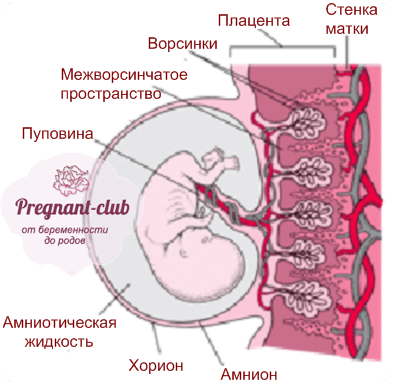 But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor?
But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor?
Labor ends after the third stage of labor, that is, after the birth of the placenta. Following this, the uterus immediately significantly decreases in size, becomes spherical, its cavity is filled with blood clots; the bottom of the uterus at this moment is located approximately in the middle between the womb and the navel. The early postpartum period lasts for 2 hours and during this time the woman is in the maternity ward. Then comes the late postpartum period. This period lasts 6-8 weeks. During this time, there is a reverse development (involution) of all organs and systems that have undergone changes due to pregnancy and childbirth. The exception is the mammary glands, whose function reaches its peak precisely in the postpartum period. The most pronounced involutional changes occur in the genital organs, especially in the uterus. The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml.
The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml.
What complications can occur after childbirth
You should consult a gynecologist in the following cases:
Increased amount of discharge
discharge does not stop for a long time, large blood clots appeared. When bleeding occurs, you need to contact an obstetrician-gynecologist, preferably at the maternity hospital where the birth took place.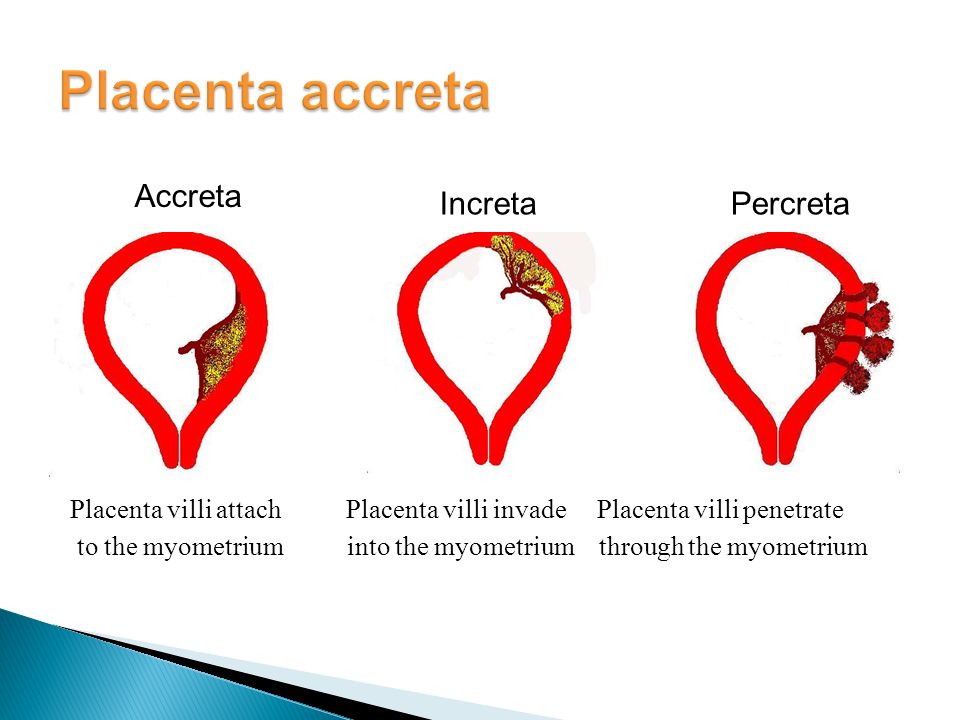 If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance.
If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance.
Retention of part of the placenta in the uterine cavity
The most common cause of late postpartum hemorrhage (that is, those that occur later than 2 hours after birth) is the retention of a part of the placenta in the uterine cavity. The diagnosis in this case is confirmed by ultrasound. To remove the remnants of the placenta, the walls of the uterus are scraped under general intravenous anesthesia with mandatory subsequent antibiotic therapy to prevent infectious complications.
Changes in the blood coagulation system
In rare cases, the causes of bleeding may be changes in the blood coagulation system of a hereditary or acquired nature, blood diseases. In these cases, complex drug therapy is required.
Violation of contraction of the muscles of the uterus
Development of bleeding associated with impaired contraction of the muscles of the uterus is possible.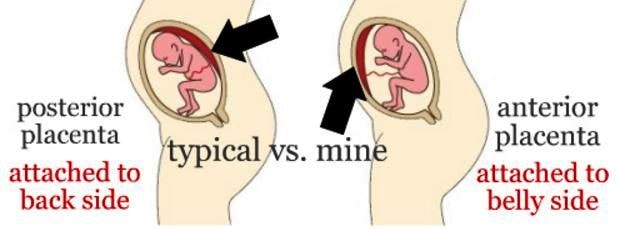 This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery.
This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery.
A sharp, unexpected cessation of spotting should also alert the woman and requires urgent medical attention. In this case, the outflow of blood from the uterus may be disturbed, that is, lochia accumulate in the cavity and the so-called lochiometer develops. Blood clots are a good breeding ground for bacteria, so if the lochiometer is not treated in time, bacteria enter the uterine cavity and endometritis develops - inflammation of the uterine mucosa. After a caesarean section, a lochiometer occurs more often than after a vaginal birth. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy.
After a caesarean section, a lochiometer occurs more often than after a vaginal birth. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy.
Learn more about the services:
- Ultrasound of the pelvic organs
Inflammatory process in the vagina or uterus
The discharge has acquired an unpleasant odor. This may indicate the development of an inflammatory process in the vagina or in the uterus. In the postpartum period, there was a significant increase in the composition of most groups of bacteria, including bacteroids, Escherichia coli, streptococci, staphylococci. Potentially, all of these species can be the cause of postpartum infectious diseases. A common problem for women after childbirth is the development of bacterial vaginosis.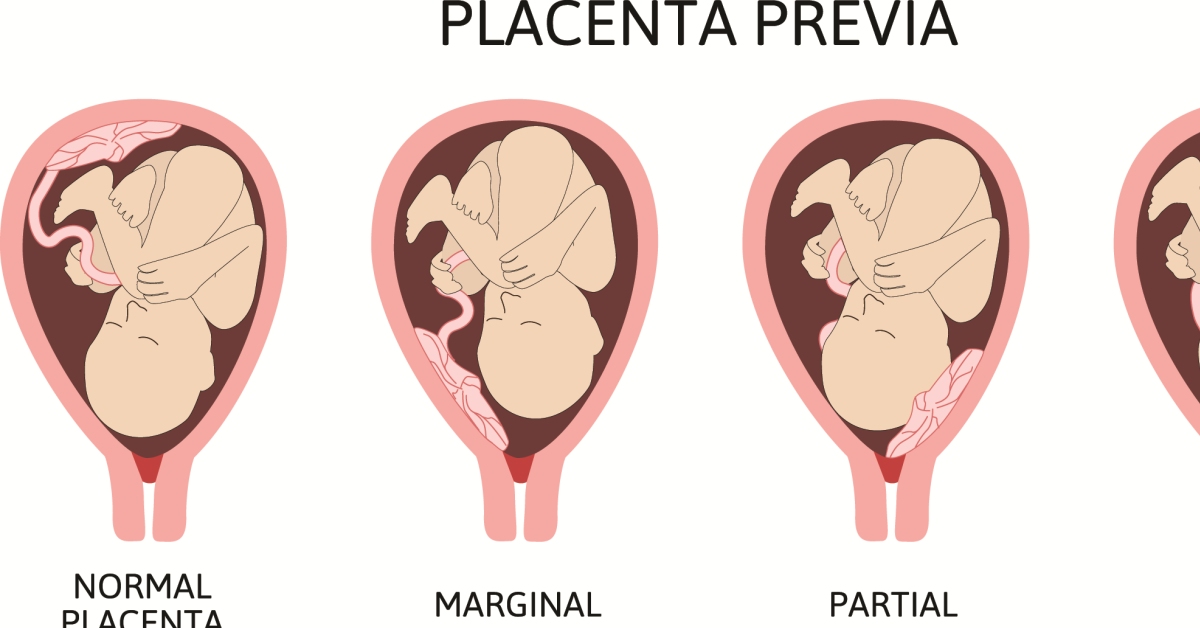 Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations.
Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations.
Vaginal candidiasis (thrush)
The appearance of curdled discharge, itching, burning in the genital area, redness indicates the development of vaginal candidiasis (thrush). The risk of this complication increases with antibiotics. Diagnosis is based on the detection of a large number of yeast-like fungi in a smear on the flora. For treatment, local preparations are used in the form of vaginal suppositories or tablets.
For treatment, local preparations are used in the form of vaginal suppositories or tablets.
Postpartum endometritis
Purulent discharge, lower abdominal pain, fever. These symptoms may indicate the development of a serious complication - postpartum endometritis (inflammation of the inner lining of the uterus). Most often, endometritis occurs in patients after cesarean section, manual examination of the postpartum uterus, manual separation of the placenta and removal of the placenta (if independent separation of the placenta is difficult due to a violation of the contractile function of the uterus), with a long anhydrous interval (more than 12 hours from the moment of amniotic fluid outflow to the birth of a baby), in women admitted to childbirth with inflammatory diseases of the genital tract (for example, against the background of sexually transmitted infections), in patients with a large number of abortions in the past. The classic form of endometritis occurs on days 1-5.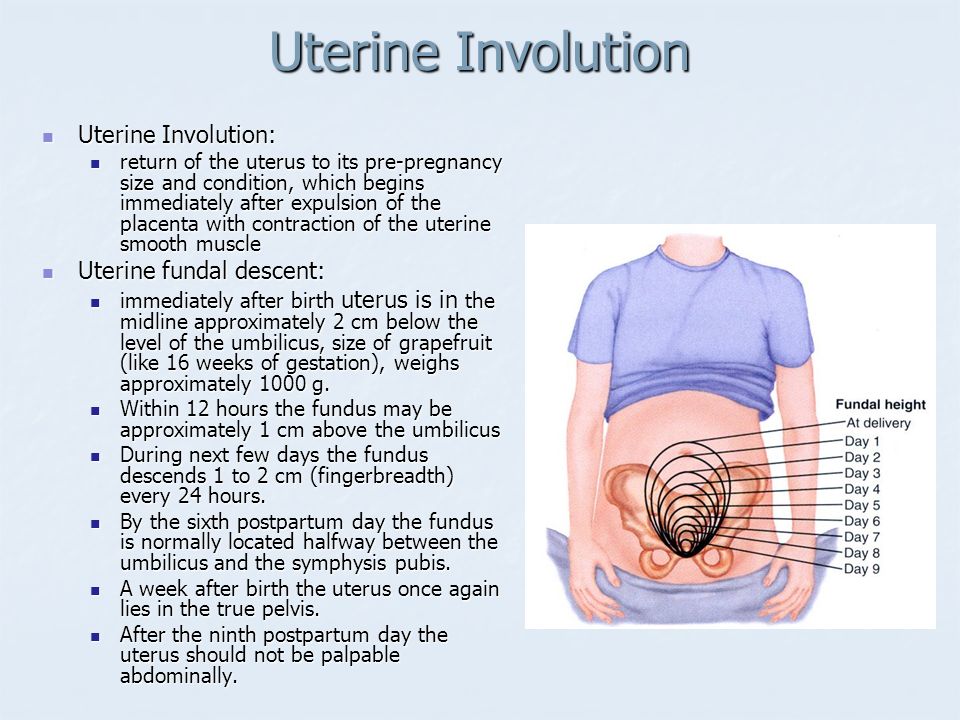 Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill. Endometritis after caesarean section always proceeds in a severe form.
Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill. Endometritis after caesarean section always proceeds in a severe form.
An ultrasound examination of the uterus and a complete blood count, which reveal signs of inflammation, help the doctor make a diagnosis. Treatment of endometritis should be started as early as possible. It is carried out in a hospital. Assign bed rest, with acute endometritis cold on the lower abdomen. Postpartum endomeritis is necessarily treated with antibiotics, along with them, agents that reduce the uterus are used. Currently, in many clinics and maternity hospitals, the uterine cavity is washed with cooled solutions of antiseptics. In severe cases, an intravenous infusion of saline solutions is required to improve blood circulation, relieve symptoms of intoxication.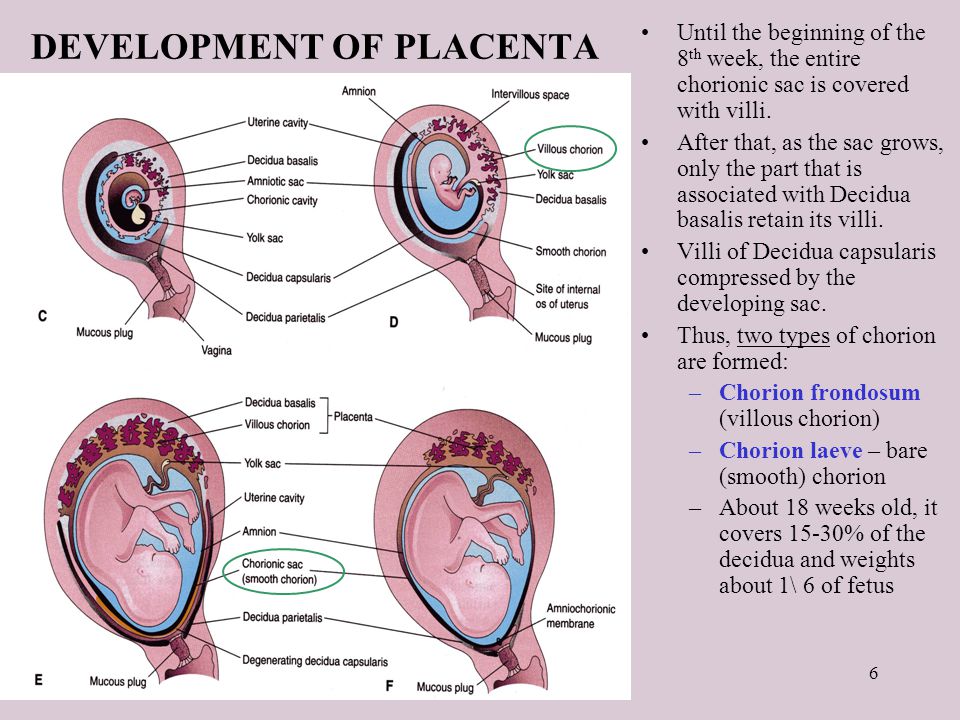
In case of untimely treatment, there is a very high risk of spreading the inflammatory process to the entire uterus, small pelvis, the development of sepsis (the appearance of infectious agents in the blood), up to the death of the patient.
Laktostasis and mastitis
In the postpartum period, there may be pain in the mammary glands, a feeling of fullness, an increase in body temperature. When these symptoms appear, you should definitely consult a doctor - an obstetrician-gynecologist in a antenatal clinic or a surgeon.
Possible causes of pain in the mammary glands and the accompanying fever are lactostasis and mastitis.
Laktostasis (stagnation of milk in the gland), due to blockage of the excretory ducts. Most often, this condition develops when the baby is not properly attached to the chest, violation of the feeding regimen. Laktostasis often affects primiparous women. With the stagnation of milk, the mammary gland increases in volume, its dense enlarged lobules are determined.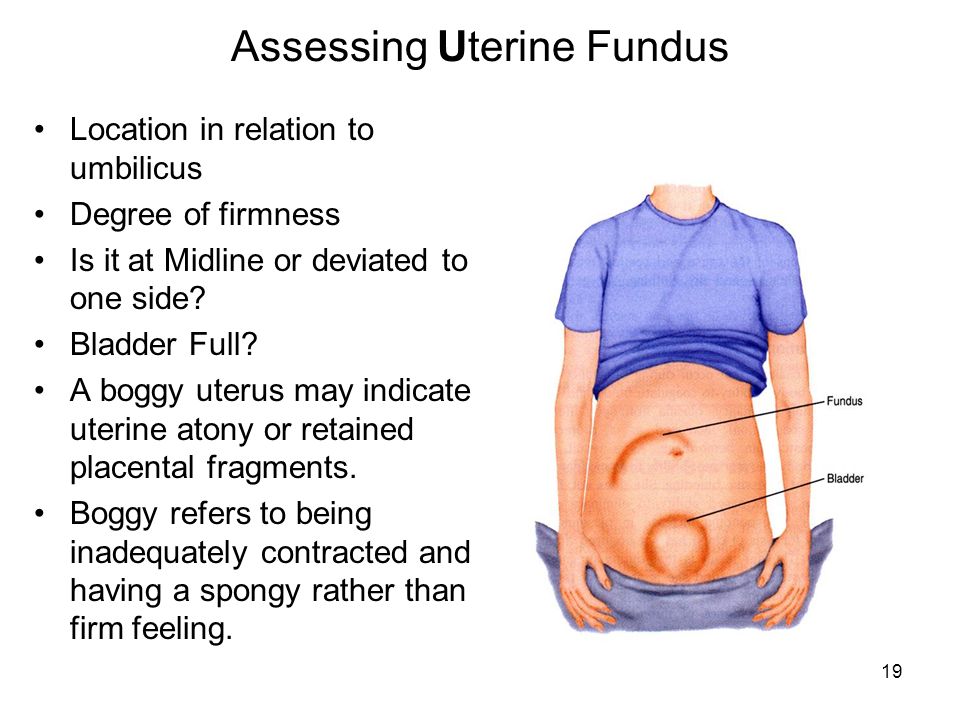 Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin.
Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin.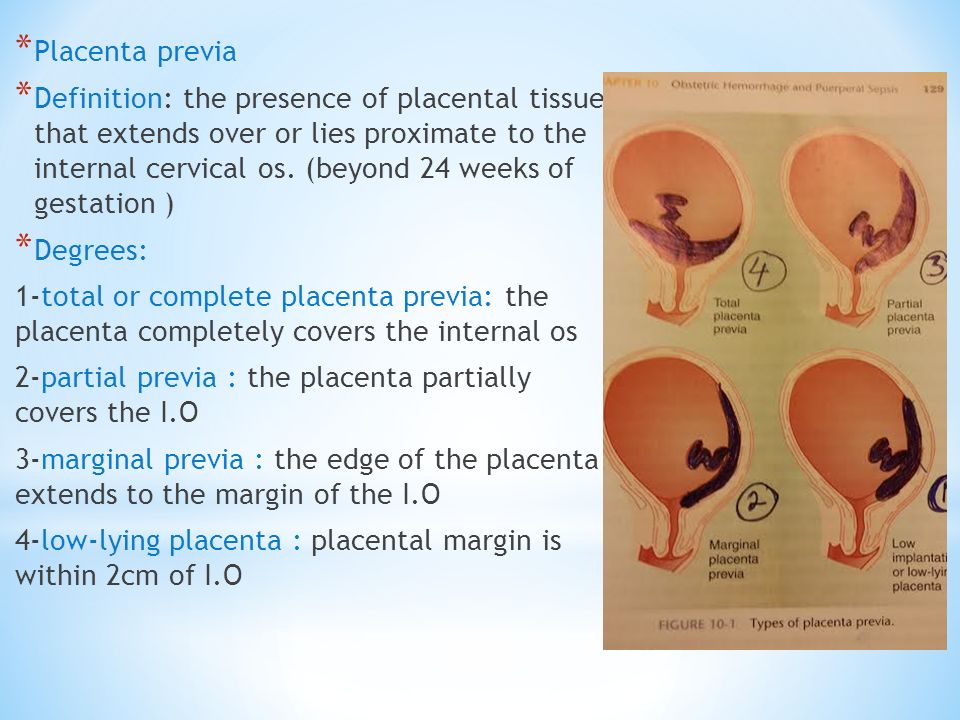 Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk.
Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk.
To eliminate lactostasis, pumping, local anti-inflammatory ointments, and physiotherapy are used. Mastitis is treated with antibiotics. In some cases, lactation suppression and surgical treatment are required.
Postpartum pyelonephritis
Fever, pain in the back or side, painful urination. These symptoms may indicate the development of postpartum pyelonephritis, that is, inflammation of the kidneys. Critical periods for the development of postpartum pyelonephritis, doctors consider 4-6 and 12-14 days of the postpartum period. The development of the disease is associated with infection in the urinary tract from the genital tract. Most often, the disease develops in puerperas, in the urine of which a small amount of bacteria was found during pregnancy. An ultrasound examination of the kidneys and bladder and a urine test help the doctor make the diagnosis.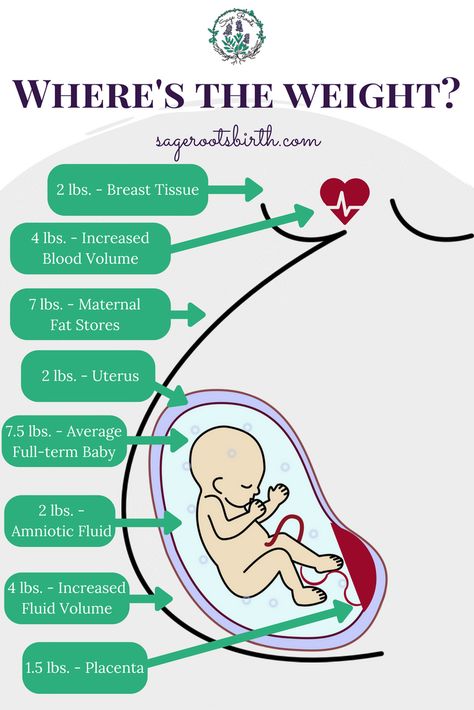
Treatment of pyelonephritis is mandatory with antibiotics.
Venous thrombosis
Pain in the legs, swelling, redness on the legs along the vein, increased pain when walking - these are symptoms of a serious pathology - venous thrombosis (formation of blood clots in the veins) and require an urgent visit to a surgeon or phlebologist. The most dangerous periods for the occurrence of thrombosis are considered 5-6 days after childbirth or cesarean section, less often thrombosis occurs 2-3 weeks after childbirth. The causes of thrombosis are changes in the blood coagulation system that occur during pregnancy and after childbirth. Physiologically, in the postpartum period, the activation of the coagulation system occurs. As the body tries to stop bleeding. At the same time, the tone of the vessels of the small pelvis and lower extremities is reduced, the veins have not yet had time to adapt to work in new conditions. These conditions trigger the mechanisms of thrombus formation. An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy.
An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy.
The risk of developing venous thrombosis is especially high in women with various pathologies of the blood coagulation system, which are detected even before pregnancy or during childbearing. There is a high probability of thromboembolic complications and in the presence of diseases of the cardiovascular system, overweight. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of varicose veins of the lower extremities. The risk of thrombus formation is increased in women who have undergone a caesarean section. An ultrasound examination of the veins, with Dopplerography, that is, an assessment of blood flow in the vessels, helps the doctor in making a diagnosis. For the treatment of venous thrombosis, medications are used, wearing compression stockings.
A severe complication of venous thrombosis is the detachment of part of the thrombus and its movement along the vascular bed.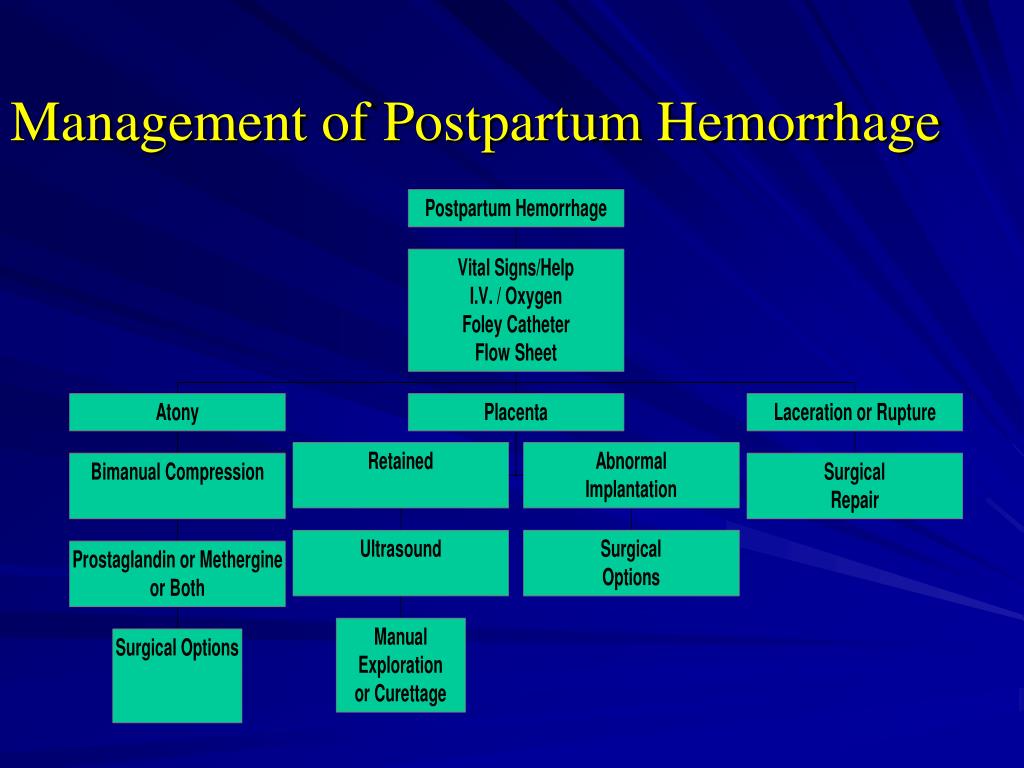 In this case, blood clots, entering the vessels of the lung or brain, cause strokes (impaired cerebral circulation) or pulmonary embolism (blockage of the pulmonary arteries by a thrombus). This serious complication appears as a sharp cough, shortness of breath, pain in the chest, hemoptysis may begin - the appearance of blood streaks in the sputum when coughing. In severe cases, the work of the heart is disrupted and death can occur.
In this case, blood clots, entering the vessels of the lung or brain, cause strokes (impaired cerebral circulation) or pulmonary embolism (blockage of the pulmonary arteries by a thrombus). This serious complication appears as a sharp cough, shortness of breath, pain in the chest, hemoptysis may begin - the appearance of blood streaks in the sputum when coughing. In severe cases, the work of the heart is disrupted and death can occur.
Unpleasant sensations in the area of postoperative sutures
Discomfort in the area of postoperative sutures after caesarean section or in the area of sutures on the perineum. Normally, after suturing vaginal tears, there may be slight pain for 1-2 days, but they quickly pass. Pain in the postoperative wound after cesarean section may be disturbing for 2 weeks, gradually decreasing. Feeling of heaviness, fullness, pain in the area of the postoperative wound may indicate the accumulation of hematoma (blood) in the area of the sutures.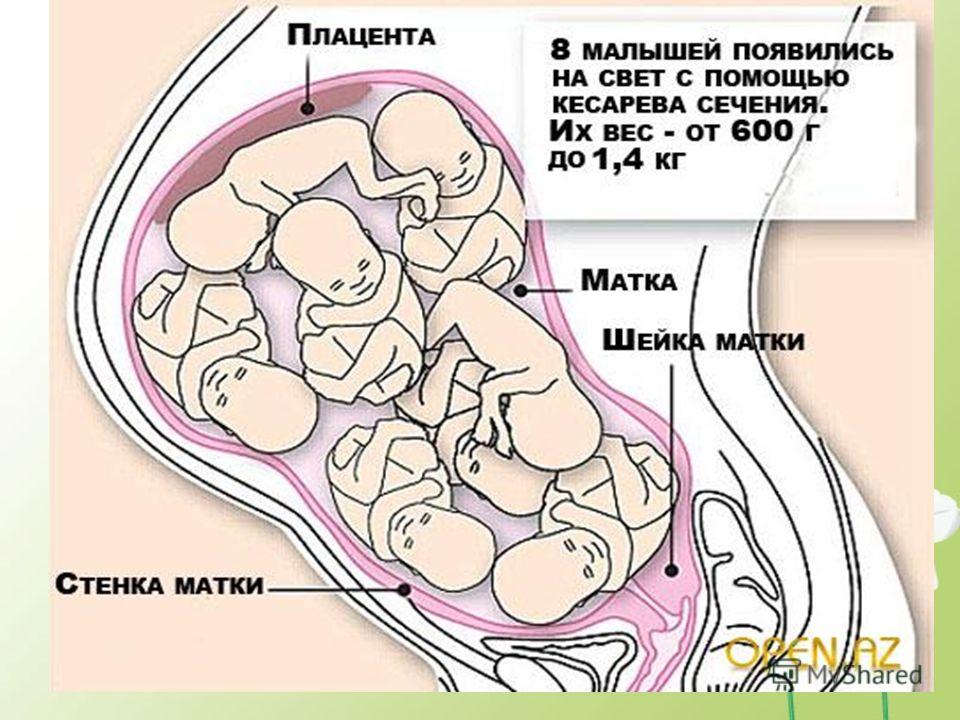 This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment.
This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment.
Urinary incontinence, feces, uterine prolapse
Violation of the physiological functions of the pelvic organs of varying degrees (bladder, rectum), which may appear as in the postpartum period - urinary incontinence, feces, uterine prolapse. The problem of genital prolapse occurs when the pelvic floor muscles have lost the ability to contract so much that individual organs or parts of them do not fall into the projection of the supporting apparatus. The most common cause of pelvic organ prolapse is trauma to the pelvic floor muscles during childbirth.
Hemorrhoids
Quite often, after childbirth, women are worried about the appearance of hemorrhoids - varicose veins of the rectum. The predisposing factor in this case is a significant increase in intra-abdominal pressure during pregnancy and during childbirth. In the case of hemorrhoids, formations appear in the anus, which can be painless, but most often - painful, bleeding and itchy. The appearance of intense pain in the anus, bloody discharge from the rectum are a reason to consult a doctor - a proctologist. Most often, uncomplicated forms of hemorrhoids are treated with local medications - creams and suppositories, in case of complications (nodule pinching, bleeding), surgical treatment is required.
In any case, if you experience any symptoms that cause concern, it is advisable to consult a doctor, because any complication is best prevented or treated at the very initial stage.
Postpartum hygiene
Congratulations! You have become a mother!
The postpartum period is no less important and responsible stage in the life of a family than pregnancy.
The postpartum period lasts 6-8 weeks (begins after the birth of the placenta and ends when the organs and systems that have changed during pregnancy return to their original state).
In the process of healing the inner surface of the uterus, postpartum discharge appears - lochia, which is a wound secret. Their character during the postpartum period changes: in the first days, lochia has a bloody character; from the 4th day, their color changes to reddish-brown; by the 10th day they become light, liquid, without blood, and after 3 weeks there is practically no discharge. There may be discomfort due to uterine contractions. To relieve discomfort, bend forward and gently massage your belly. If discomfort in the uterine area occurs during feeding, try choosing a different position. It is convenient to feed lying on your side. The stomach may ache for another reason. It hurts the abdominal muscles that were actively involved during childbirth, try to relax or do a light massage.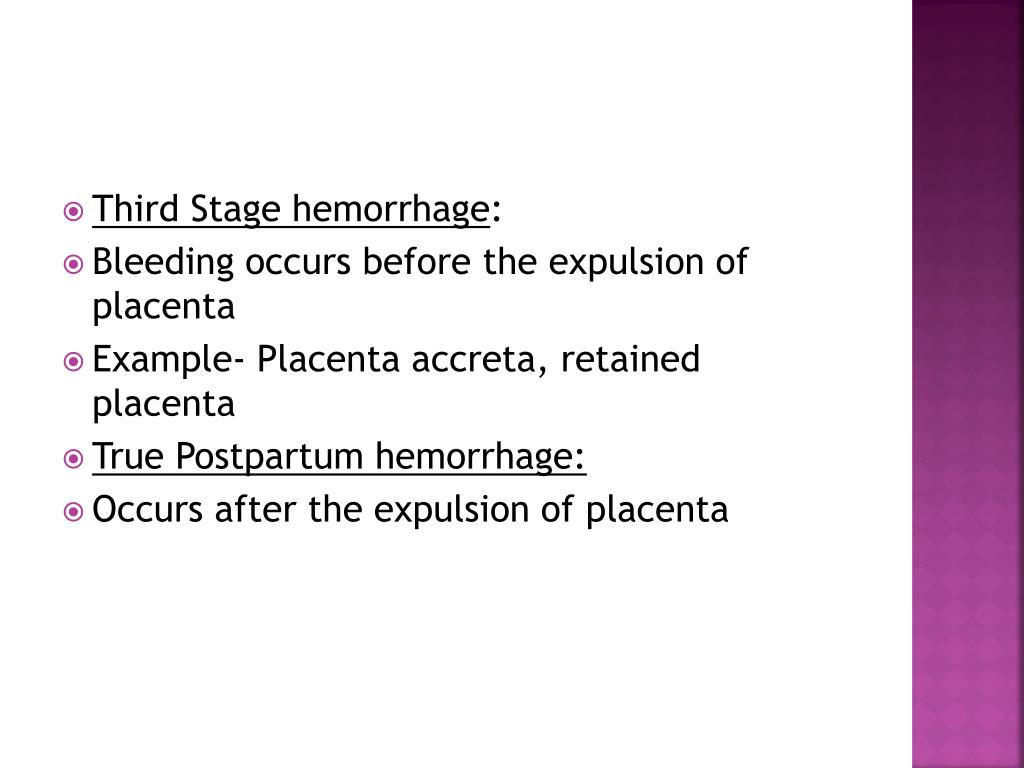
In most non-nursing women, menstruation occurs on the 6-8th week after childbirth, more often it comes without the release of an egg from the ovary. However, ovulation and pregnancy may occur during the first months after childbirth. In lactating women, the time of the onset of the first menstruation after childbirth can be delayed for many months.
The normal postpartum period is characterized by a good general condition of the woman, normal temperature, sufficient lactation. For the prevention of infectious complications, strict adherence to sanitary and epidemiological requirements and personal hygiene rules is important.
POSTPARTUM HYGIENE
The strictest cleanliness is essential.
- A woman in labor should take a shower twice a day (morning and evening), then wash her breasts with soap and brush her teeth.
- Particular attention should be paid to the cleanliness of hands. Nails should be cut short, hands should be washed more often with soap and be sure before each feeding of the child (if the hands are dirty, you can infect the child, infect the nipples).

- Among the hygienic measures of particular importance in the postpartum period is the maintenance of cleanliness of the external genitalia and the surrounding skin.
- Wash with warm water and soap (liquid with a dispenser, as microbes feel great on lumps) with a fluid stream, wash the genitals from front to back (from the pubis to the anus) after each visit to the toilet at least 4-5 times a day (you need to go to the toilet exactly at such a frequency that the filled bladder does not interfere with uterine contraction).
Wash hands cleanly before washing. - Keep the pads clean, change them every 3-4 hours, regardless of fullness. Remove pads from front to back to prevent microorganisms from entering the vagina from the anus. If there are seams on the perineum, they should be washed thoroughly enough - you can simply direct a jet of water at it. After washing, you need to dry the perineum and the seam area by blotting the towel from front to back.

- Do not take a bath for the first 6 weeks after giving birth. This is due to the fact that the entrance to the vagina is not yet closed enough and pathogenic microbes can penetrate into it along with water. It is clear that at this time you can not swim in the pool, river, lake, sea.
- The use of tight underwear is strictly excluded, as it puts significant pressure on the perineum, which disrupts blood circulation, preventing healing.
- If there are stitches on the perineum, a woman should not sit down for 7-14 days (depending on the degree of damage). At the same time, you can sit on the toilet already on the first day after childbirth. By the way, about the toilet. Many women are afraid of severe pain and try to skip bowel movements, as a result, the load on the muscles of the perineum increases and the pain intensifies.
To avoid constipation after childbirth, do not eat foods that have a fixative effect. If the problem of constipation is not new to you, drink a tablespoon of vegetable oil before each meal.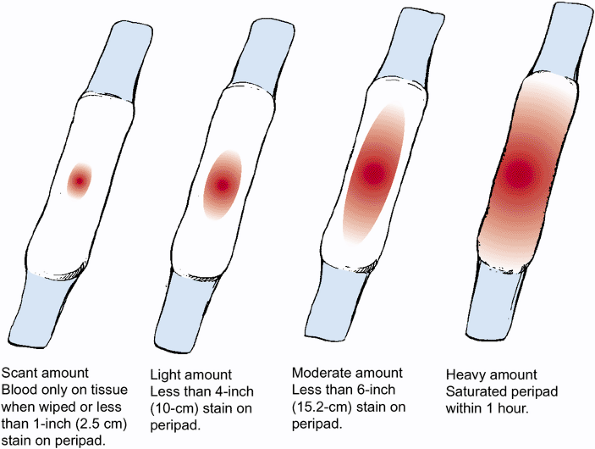 The stool will be soft and will not affect the healing process of the stitches.
The stool will be soft and will not affect the healing process of the stitches.
- Underwear and bed linen must be cotton. We change underwear daily, bedding - at least once every three to five days.
- Stitches after caesarean section do not require special care. After the stitches and bandage are removed, you can take a shower. Do not scrub the seam area with a washcloth. With painful sensations in the anterior abdominal wall, a postpartum or postoperative bandage, which must be worn for 4 months, will help to cope. Young mothers are often interested in: will the seams come apart if you carry a baby in your arms? For the first 2-3 months after surgery, it is recommended to lift no more than your child's weight.
It happens that redness, irritation, bloody or purulent discharge occurs at the suture site. This indicates suppuration or divergence of the seams. Then you should immediately consult a doctor in a antenatal clinic.
Sexual life after childbirth can be resumed after 6-8 weeks. By this time, the woman's body is already completely back to normal. Your doctor will advise you on contraceptives.
By this time, the woman's body is already completely back to normal. Your doctor will advise you on contraceptives.
To fully recover from childbirth, at least two years must pass before the next pregnancy.
BREASTFEEDING
Breastfeeding should not be done by the clock, but on demand, incl. at night time. At one feeding, put the baby on one breast so that he suckles for a long time and receives later milk, which contains brain and intelligence development factors, growth factors and immunoglobulins. Later, the milk comes in droplets like colostrum, the child sucks it intermittently. Sometimes the mother at this moment thinks that the child is indulging and tearing him off the breast. You don't need to do this. Let him let her go.
Breast milk is the best food for a baby!
- After the baby has had enough, the mother should carefully feel the mammary gland. If the breast is soft and there is no soreness and seals anywhere, then pumping is not necessary.
 If necessary, you can wash the mammary glands with warm water after feeding, starting from the nipple and ending with the armpit, and dry with a clean towel.
If necessary, you can wash the mammary glands with warm water after feeding, starting from the nipple and ending with the armpit, and dry with a clean towel.
Very useful for breasts after childbirth and air baths, which are best taken after feeding, to give the breast a chance to rest, "breathe". The duration of such an air bath may not exceed 15-20 minutes, but the benefits of it are enormous.
- The nipple should be carefully inspected daily, the surface of which should not be cracked, and as a preventive measure, leave a drop of milk on the nipple and let it dry in the open air.
Only breast milk should be used as the main and only product for feeding a newborn. The use of nipples, horns and "pacifiers" is unacceptable, as this leads to a weakening of sucking in newborns and, accordingly, to incomplete emptying of the mammary gland, a decrease in prolactin production.
Are you worried about the question - do I have enough milk?
To resolve this issue, you need to observe the child, if he urinates more than 6 times a day, then he receives a sufficient amount of milk.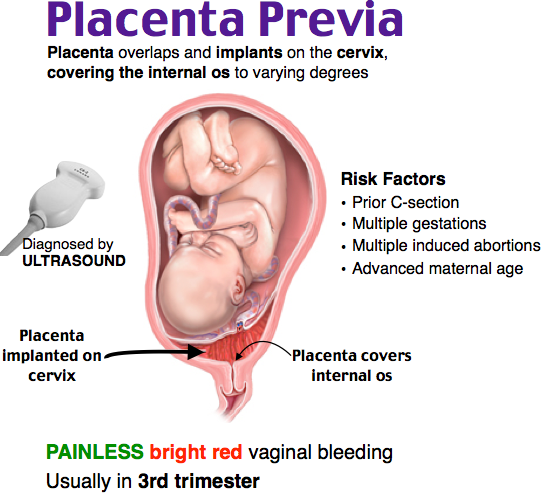 The reason for the decrease in the amount of milk can be:
The reason for the decrease in the amount of milk can be:
- rare feeding break (3 or more hours)
- if you do not feed at night
- short feedings or by the hour
To increase the amount of milk, you need to reorganize the feeding regimen, feed often and for as long as you want child. Try to feed with one breast so that the baby sucks out milk later, you can strain the empty breast for 10 minutes, thereby increasing the flow of milk. It is necessary to improve the mother's nutrition or use herbal teas to increase lactation.
NUTRITION
Nursing mother's nutrition should be rich in calories (3200 kcal), balanced with the proper amount of proteins, fats, carbohydrates, vitamins and microelements. This diet will be dominated by lactic acid, protein foods, fresh fruits and vegetables. Food should be rich in vitamins and minerals. Spicy, fatty, fried, smoked foods, canned food, sausages, alcohol and potential allergens for the child (chocolate, citrus fruits, coffee) should be excluded from the diet.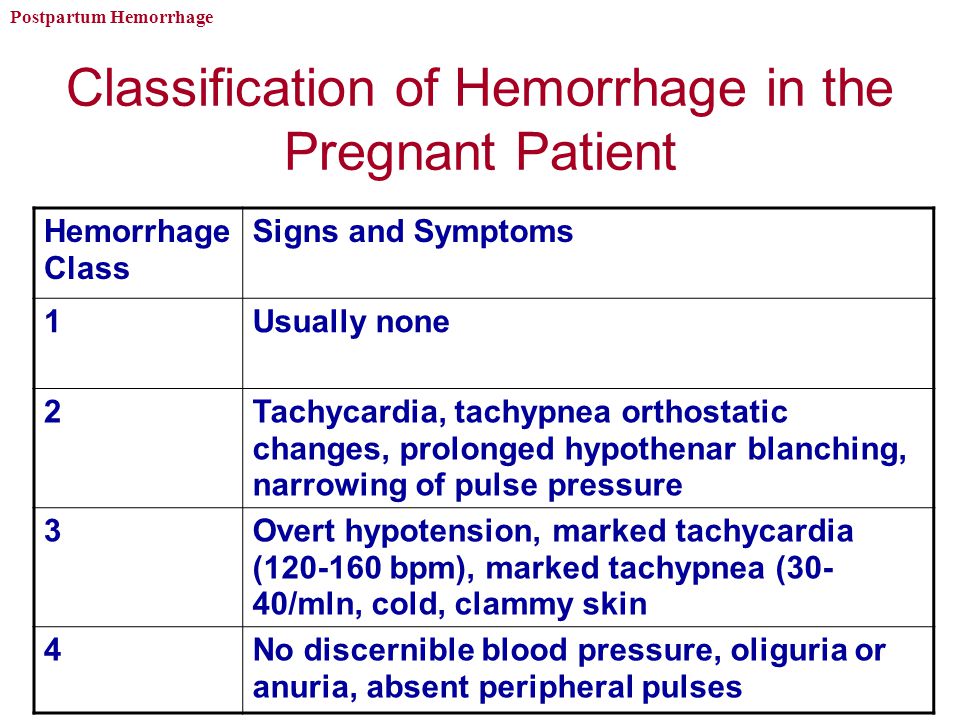
The food of the puerperal should be 5-6 times a day. It is necessary to distribute products in the daily menu in such a way that those that are rich in protein and are much more difficult to digest in the gastrointestinal tract (meat, fish, cereals) would be used during the first half of the day, and in the second half it is advisable to give preference to milk. - vegetable food.
Conditions requiring special attention
Unfortunately, the first month after childbirth does not always go smoothly. Situations may arise, when medical attention is needed . Monitor your well-being, regularly measure your body temperature, as fever is most often the first sign of complications in the postpartum period.
All complications of the postpartum period can be divided into several groups:
1. Complications of the uterus.
Subinvolution of the uterus - a decrease in the rate of contraction of the uterus, due to a delay in the uterus of postpartum discharge. The disease often occurs 5-7 days after childbirth, due to the closure of the cervical canal with a blood clot or a piece of membranes, as well as the inflection of the uterus due to relaxation of the ligamentous apparatus.
The disease often occurs 5-7 days after childbirth, due to the closure of the cervical canal with a blood clot or a piece of membranes, as well as the inflection of the uterus due to relaxation of the ligamentous apparatus.
Infection of the contents of the uterus can lead to inflammation of the uterine mucosa - endometritis. Predisposing factors for the occurrence of endometritis are difficult childbirth, violations of the separation of the placenta during childbirth, infections of the genital tract during pregnancy, impaired immunity, abortion. Symptoms of the disease are: fever, unpleasant odor in lochia, aching pain in the lower abdomen. If these symptoms appear, you should consult an obstetrician-gynecologist at the place of residence. To clarify the diagnosis, an ultrasound examination is performed and, if necessary, surgery, during which the contents are removed from the uterine cavity (washing or curettage of the uterus). After surgery, antibiotics must be prescribed.
2. Breast complications.
Breast complications.
Laktostasis - stagnation of milk in the mammary gland. At the same time, the chest swells and becomes painful, foci of seals appear, a short-term rise in body temperature is possible. In itself, lactostasis is not a disease, requiring only gentle pumping of the breast, restriction of fluid intake, and frequent feeding of painful breasts. However, when an infection joins, it turns into lactational mastitis, requiring immediate medical attention , antibiotic therapy, and sometimes surgery. The question of the possibility of breastfeeding with mastitis is decided individually, depending on the stage of the disease.
Another complication of the chest is the appearance of cracks in the nipples. The main reason for their appearance is improper attachment of the baby to the breast, when the baby captures only the nipple, and not the entire areola. Such a seizure is very painful for the mother - and this is the main danger signal. Breastfeeding doesn't have to be painful. Good advisory and practical help for lactostasis and cracked nipples is provided by breastfeeding consultants. Treatment of cracks consists in treating the nipple with wound healing drugs.
Breastfeeding doesn't have to be painful. Good advisory and practical help for lactostasis and cracked nipples is provided by breastfeeding consultants. Treatment of cracks consists in treating the nipple with wound healing drugs.
Hypogalactia - insufficient milk production. In order to increase the amount of milk, a mother needs to increase the frequency of feedings, not skip night feedings, offer her baby both breasts in one feeding, drink more, eat well and sleep a lot.
3. Complications from the tissues of the cervix, vagina and skin.
Inflamed wounds of these tissues are called postpartum ulcers. When an infection is attached, these wounds swell, become covered with a purulent coating, and their edges are painful. For the purpose of treatment, they are treated with various antiseptics, sometimes they require surgical treatment.
4. Complications of the venous system.
Hemorrhoids (varicose veins of the rectum) also cause pain. When infringed, they increase, become swollen, tense and painful. Thorough hygiene helps to reduce pain (shower after each visit to the toilet), applying ice to the perineum. Certain medications can be used as prescribed by a doctor.
When infringed, they increase, become swollen, tense and painful. Thorough hygiene helps to reduce pain (shower after each visit to the toilet), applying ice to the perineum. Certain medications can be used as prescribed by a doctor.
Thrombophlebitis is a disease of the veins characterized by inflammation of the venous wall and thrombosis of the vein. After childbirth, thrombophlebitis of the pelvic veins most often occurs. Usually this disease occurs in the third week after childbirth. In terms of symptoms, it is very similar to endometritis, but requires a different treatment. Surgeons are involved in the treatment of complications from the venous system.
Complications after childbirth require immediate treatment, as they can lead to a generalization of the process - postpartum peritonitis or sepsis. Therefore, if something bothers you in your condition, be sure to consult a doctor.
You must come to the antenatal clinic for the first time 10 days after discharge from the maternity hospital.