Red skin arms
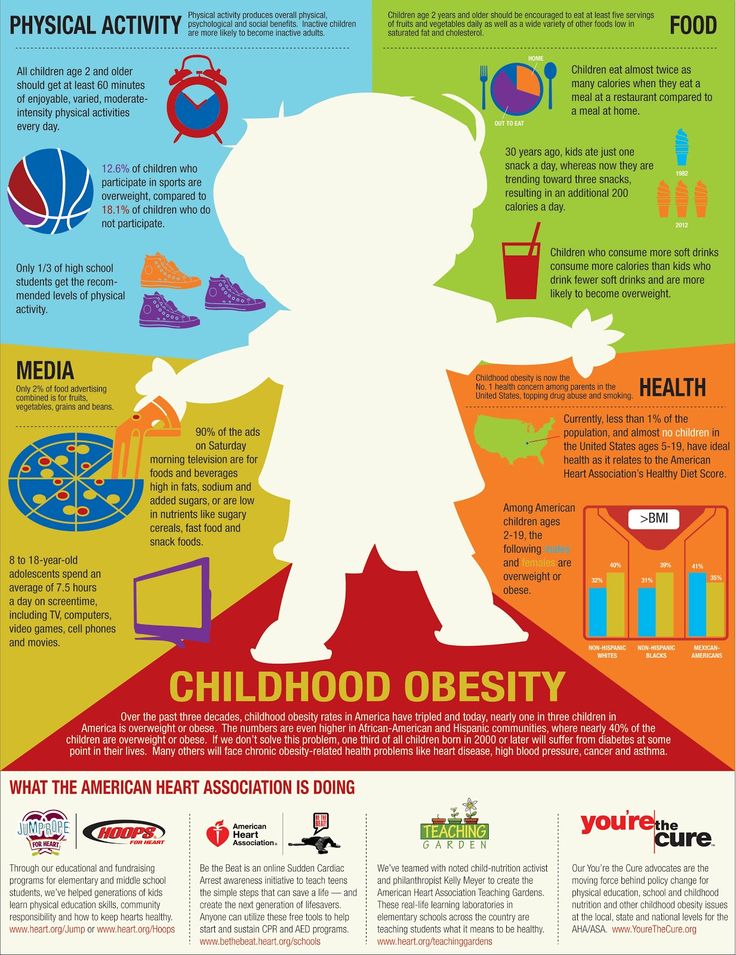
Skin Redness: Causes, Photos, and Treatments
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Why does my skin look red?
From a sunburn to an allergic reaction, there are many things that can cause your skin to become red or irritated. It may be because extra blood rushes to the skin’s surface to fight off irritants and encourage healing. Your skin can also become red from exertion, such as after a heart-pounding exercise session.
It’s not always a reason for concern, but skin redness can be irritating and uncomfortable. It might also be accompanied by other symptoms. Figuring out its underlying cause can help you treat your skin and keep it from happening again.
Many different conditions can skin redness. Here are 21 possible causes.
Warning: Graphic images ahead.
Diaper rash
- Rash located on areas that have contact with a diaper
- Skin looks red, wet, and irritated
- Warm to the touch
Read full article on diaper rash.
First-degree burn
- The mildest form of burn injury, it affects only the first layer of the skin.
- Painful, dry, red area turns white with pressure.
- Skin may peel, but ther is no blistering.

- Pain and redness will subside after a few days.
Read full article on first-degree burns.
Allergic eczema
- May resemble a burn
- Often found on hands and forearms
- Skin is itchy, red, scaly, or raw
- Blisters that weep, ooze, or become crusty
Read full article on allergic eczema.
Rosacea
- Chronic skin disease that goes through cycles of fading and relapse
- Relapses may be triggered by spicy foods, alcoholic beverages, sunlight, stress, and the intestinal bacteria Helicobacter pylori
- There are four subtypes of rosacea encompassing a wide variety of symptoms
- Common symptoms include facial flushing, raised, red bumps, facial redness, skin dryness, and skin sensitivity
Read full article on rosacea.
Burns
This condition is considered a medical emergency. Urgent care may be required.
- Burn severity is classified by both depth and size
- First-degree burns: minor swelling and dry, red, tender skin that turns white when pressure is applied
- Second-degree burns: very painful, clear, weeping blisters and skin that appears red or has variable, patchy coloration
- Third-degree burns: white or dark brown/tan in color, with leathery appearance and low or no sensitivity to touch
Read full article on burns.
Contact dermatitis
- Appears hours to days after contact with an allergen
- Rash has visible borders and appears where your skin touched the irritating substance
- Skin is itchy, red, scaly, or raw
- Blisters that weep, ooze, or become crusty
Read full article on contact dermatitis.
Chemical burn
This condition is considered a medical emergency. Urgent care may be required.
- This occurs when your skin, mucous membranes, or eyes come into contact with a chemical irritant, such as a strong acid or a base.
- The concentration of the chemical, duration of contact, and method of contact will determine severity of symptoms and urgency of treatment.
- First aid treatments for chemical burns include removing the chemical that caused the burn (including removing any clothing or jewelry that has touched the chemical) and rinsing the skin under lukewarm, slow, running water for 10 to 20 minutes (and at least 20 minutes for chemical eye injuries).

Read full article on chemical burns.
Drug allergy
This condition is considered a medical emergency. Urgent care may be required.
- Mild, itchy, red rash may occur days to weeks after taking a drug
- Severe drug allergies can be life-threatening and symptoms include hives, racing heart, swelling, itching, and difficulty breathing
- Other symptoms include fever, stomach upset, and tiny purple or red dots on the skin
Read full article on drug allergies.
Cellulitis
This condition is considered a medical emergency. Urgent care may be required.
- Caused by bacteria or fungi entering through a crack or cut in the skin
- Red, painful, swollen skin with or without oozing that spreads quickly
- Hot and tender to the touch
- Fever, chills, and red streaking from the rash might be a sign of serious infection requiring medical attention
Read full article on cellulitis.
Scarlet fever
- Occurs at the same time as or right after a strep throat infection
- Red skin rash all over the body (but not the hands and feet)
- Rash is made up of tiny bumps that make it feel like “sandpaper”
- Bright red tongue
Read full article on scarlet fever.
Angioedema
- This is a form of severe swelling beneath the skin’s surface.
- It may be accompanied by hives and itching.
- It’s caused by an allergic reaction to an allergen like food or medication.
- Additional symptoms may include stomach cramping and discolored patches or rash on the hands, arms, and feet.
Read full article on angioedema.
Thrombophlebitis
- This inflammation of a superficial vein is caused by a blood clot.
- It typically occurs in the legs.
- Symptoms include tenderness, warmth, redness, and visible engorgement along the vein.
Read full article on thrombophlebitis.
Bone infection
- A bone infection, also called osteomyelitis, occurs when bacteria or fungi invade a bone.
- Bones may get infected by migration of a bacteria or fungus infecting surrounding tissues or the blood stream, or by penetrating injury or surgery that exposes the bone.
- Symptoms include pain, redness, swelling, stiffness, and warmth in the infected body part.
- Fever and chills may also occur.
Read full article on bone infection.
Osteosarcoma
- This bone cancer typically develops in the shinbone (tibia) near the knee, the thighbone (femur) near the knee, or the upper arm bone (humerus) near the shoulder.
- It’s the most common type of bone cancer in children.
- Common signs include bone pain (in motion, at rest, or when lifting objects), bone fractures, swelling, redness, and limping.
Read full article on osteosarcoma.
Sunburn
- Superficial burn on the outermost layer of skin
- Redness, pain, and swelling
- Dry, peeling skin
- More severe, blistering burns may occur after extended periods of sun exposure
Read full article on sunburns.
Skin infection
- A skin infection is caused by a wide variety of infectious agents including bacteria, fungi, viruses. and parasites.
- Common symptoms include redness of the skin, tenderness, itching, and a rash.
- See a doctor if you have fever, chills, pus-filled blisters, skin breakdown, severe pain, or a skin infection that doesn’t improve or gets progressively worse.
Read full article on skin infections.
Bites and stings
This condition is considered a medical emergency. Urgent care may be required.
- Redness or swelling at the site of the bite or sting
- Itching and soreness at the site of the bite
- Pain in the affected area or in the muscles
- Heat around the bite or sting
Read full article on bites and stings.
Heat rash
- This irritating skin rash occurs due to a combination of heat, sweat, and friction.
- It’s caused by blockage of the sweat glands.

- Heat rash develops on body parts that rub together, such as between the inner thighs or under the arms.
- Small clear or white bumps filled with fluid appear on the surface of the skin.
- Itchy, hot or prickly red bumps on the skin are another symptom.
Read full article on heat rash.
Psoriasis
- Scaly, silvery, sharply defined skin patches
- Commonly located on the scalp, elbows, knees, and lower back
- May be itchy or asymptomatic
Read full article on psoriasis.
Ringworm
- Circular-shaped scaly rashes with raised border
- Skin in the middle of the ring appears clear and healthy, and the edges of the ring may spread outward
- Itchy
Read full article on ringworm.
Shingles
- Very painful rash that may burn, tingle, or itch, even if there are no blisters present
- Rash comprising clusters of fluid-filled blisters that break easily and weep fluid
- Rash emerges in a linear stripe pattern that appears most commonly on the torso, but may occur on other parts of the body, including the face
- Rash may be accompanied by low fever, chills, headache, or fatigue
Read full article on shingles.
The main symptom associated with skin redness is varying colors of redness on the skin. The redness can occur on different portions of the body. Here are some examples of symptoms that you may have along with red skin:
- blistering
- bumps
- burning
- flushing
- hives
- itching
- rash
- warmth in your skin
- sores
- swelling
Causes of skin redness vary drastically and can include irritants, the sun, and insect bites. Examples of skin conditions associated with skin redness include:
- bites
- cellulitis
- contact dermatitis
- diaper rash
- eczema
- allergic eczema
- heat rash
- medication allergy
- psoriasis
- ringworm
- rosacea
- scarlet fever
- shingles
- skin burns
- skin infections
- sunburns
- lymph node inflammation
- first-degree burns
- chemical burns
- angioedema
- thromboplebitis
- bone infection
- osteosarcoma
Skin redness can be a temporary, or acute, condition. It can also be a chronic condition that constantly reappears.
It can also be a chronic condition that constantly reappears.
You should get immediate medical attention if you experience any of the following symptoms associated with skin redness:
- a burn that’s twice the size of your palm
- difficulty breathing
- extreme pain
- loss of consciousness
- redness near or on your eyes that is affecting your vision
You should also get medical attention if you have an animal bite, even if you’ve had a tetanus shot.
See a healthcare provider or dermatologist for other symptoms that aren’t considered a medical emergency. If you don’t already have a dermatologist, you can browse doctors in your area through the Healthline FindCare tool.
Your healthcare provider will examine your skin redness. If your symptoms come and go, they’ll listen to your description of them. They’ll ask you a few questions. These could include:
- What activities were you engaging in before you noticed the skin redness?
- Are you taking any new medications or using any new skin care or cleaning products?
- Do you have a family history of any skin conditions?
- Have you experienced this skin redness before?
- Were you around others who may have a similar rash?
These and other questions can help your healthcare provider figure out what may have caused your skin redness.
Additional testing may include taking a skin sample or biopsy of the affected area, or allergy testing to determine if your skin reacts to certain irritants.
Ask your healthcare provider if your skin condition may be contagious and what steps you can take to prevent its spread. This can ensure that you don’t pass on the skin redness to someone else.
Treatments for skin redness depend on what’s causing it. Examples can include avoiding the irritant or allergen that caused your skin redness in the first place.
Other treatments for skin redness include:
- cleansing the affected area with soap and water
- taking medications like antihistamines to minimize irritation
- applying topical skin care treatments like calamine lotion to reduce skin redness
Keeping the affected area clean and dry can usually help reduce skin redness. If an infection is the cause of your skin redness, your healthcare provider may prescribe antibiotics to reduce the infection’s symptoms.
Skin Redness: Causes, Photos, and Treatments
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Why does my skin look red?
From a sunburn to an allergic reaction, there are many things that can cause your skin to become red or irritated. It may be because extra blood rushes to the skin’s surface to fight off irritants and encourage healing. Your skin can also become red from exertion, such as after a heart-pounding exercise session.
It may be because extra blood rushes to the skin’s surface to fight off irritants and encourage healing. Your skin can also become red from exertion, such as after a heart-pounding exercise session.
It’s not always a reason for concern, but skin redness can be irritating and uncomfortable. It might also be accompanied by other symptoms. Figuring out its underlying cause can help you treat your skin and keep it from happening again.
Many different conditions can skin redness. Here are 21 possible causes.
Warning: Graphic images ahead.
Diaper rash
- Rash located on areas that have contact with a diaper
- Skin looks red, wet, and irritated
- Warm to the touch
Read full article on diaper rash.
First-degree burn
- The mildest form of burn injury, it affects only the first layer of the skin.
- Painful, dry, red area turns white with pressure.
- Skin may peel, but ther is no blistering.

- Pain and redness will subside after a few days.
Read full article on first-degree burns.
Allergic eczema
- May resemble a burn
- Often found on hands and forearms
- Skin is itchy, red, scaly, or raw
- Blisters that weep, ooze, or become crusty
Read full article on allergic eczema.
Rosacea
- Chronic skin disease that goes through cycles of fading and relapse
- Relapses may be triggered by spicy foods, alcoholic beverages, sunlight, stress, and the intestinal bacteria Helicobacter pylori
- There are four subtypes of rosacea encompassing a wide variety of symptoms
- Common symptoms include facial flushing, raised, red bumps, facial redness, skin dryness, and skin sensitivity
Read full article on rosacea.
Burns
This condition is considered a medical emergency. Urgent care may be required.
- Burn severity is classified by both depth and size
- First-degree burns: minor swelling and dry, red, tender skin that turns white when pressure is applied
- Second-degree burns: very painful, clear, weeping blisters and skin that appears red or has variable, patchy coloration
- Third-degree burns: white or dark brown/tan in color, with leathery appearance and low or no sensitivity to touch
Read full article on burns.
Contact dermatitis
- Appears hours to days after contact with an allergen
- Rash has visible borders and appears where your skin touched the irritating substance
- Skin is itchy, red, scaly, or raw
- Blisters that weep, ooze, or become crusty
Read full article on contact dermatitis.
Chemical burn
This condition is considered a medical emergency. Urgent care may be required.
- This occurs when your skin, mucous membranes, or eyes come into contact with a chemical irritant, such as a strong acid or a base.
- The concentration of the chemical, duration of contact, and method of contact will determine severity of symptoms and urgency of treatment.
- First aid treatments for chemical burns include removing the chemical that caused the burn (including removing any clothing or jewelry that has touched the chemical) and rinsing the skin under lukewarm, slow, running water for 10 to 20 minutes (and at least 20 minutes for chemical eye injuries).

Read full article on chemical burns.
Drug allergy
This condition is considered a medical emergency. Urgent care may be required.
- Mild, itchy, red rash may occur days to weeks after taking a drug
- Severe drug allergies can be life-threatening and symptoms include hives, racing heart, swelling, itching, and difficulty breathing
- Other symptoms include fever, stomach upset, and tiny purple or red dots on the skin
Read full article on drug allergies.
Cellulitis
This condition is considered a medical emergency. Urgent care may be required.
- Caused by bacteria or fungi entering through a crack or cut in the skin
- Red, painful, swollen skin with or without oozing that spreads quickly
- Hot and tender to the touch
- Fever, chills, and red streaking from the rash might be a sign of serious infection requiring medical attention
Read full article on cellulitis.
Scarlet fever
- Occurs at the same time as or right after a strep throat infection
- Red skin rash all over the body (but not the hands and feet)
- Rash is made up of tiny bumps that make it feel like “sandpaper”
- Bright red tongue
Read full article on scarlet fever.
Angioedema
- This is a form of severe swelling beneath the skin’s surface.
- It may be accompanied by hives and itching.
- It’s caused by an allergic reaction to an allergen like food or medication.
- Additional symptoms may include stomach cramping and discolored patches or rash on the hands, arms, and feet.
Read full article on angioedema.
Thrombophlebitis
- This inflammation of a superficial vein is caused by a blood clot.
- It typically occurs in the legs.
- Symptoms include tenderness, warmth, redness, and visible engorgement along the vein.
Read full article on thrombophlebitis.
Bone infection
- A bone infection, also called osteomyelitis, occurs when bacteria or fungi invade a bone.
- Bones may get infected by migration of a bacteria or fungus infecting surrounding tissues or the blood stream, or by penetrating injury or surgery that exposes the bone.
- Symptoms include pain, redness, swelling, stiffness, and warmth in the infected body part.
- Fever and chills may also occur.
Read full article on bone infection.
Osteosarcoma
- This bone cancer typically develops in the shinbone (tibia) near the knee, the thighbone (femur) near the knee, or the upper arm bone (humerus) near the shoulder.
- It’s the most common type of bone cancer in children.
- Common signs include bone pain (in motion, at rest, or when lifting objects), bone fractures, swelling, redness, and limping.
Read full article on osteosarcoma.
Sunburn
- Superficial burn on the outermost layer of skin
- Redness, pain, and swelling
- Dry, peeling skin
- More severe, blistering burns may occur after extended periods of sun exposure
Read full article on sunburns.
Skin infection
- A skin infection is caused by a wide variety of infectious agents including bacteria, fungi, viruses. and parasites.
- Common symptoms include redness of the skin, tenderness, itching, and a rash.
- See a doctor if you have fever, chills, pus-filled blisters, skin breakdown, severe pain, or a skin infection that doesn’t improve or gets progressively worse.
Read full article on skin infections.
Bites and stings
This condition is considered a medical emergency. Urgent care may be required.
- Redness or swelling at the site of the bite or sting
- Itching and soreness at the site of the bite
- Pain in the affected area or in the muscles
- Heat around the bite or sting
Read full article on bites and stings.
Heat rash
- This irritating skin rash occurs due to a combination of heat, sweat, and friction.
- It’s caused by blockage of the sweat glands.

- Heat rash develops on body parts that rub together, such as between the inner thighs or under the arms.
- Small clear or white bumps filled with fluid appear on the surface of the skin.
- Itchy, hot or prickly red bumps on the skin are another symptom.
Read full article on heat rash.
Psoriasis
- Scaly, silvery, sharply defined skin patches
- Commonly located on the scalp, elbows, knees, and lower back
- May be itchy or asymptomatic
Read full article on psoriasis.
Ringworm
- Circular-shaped scaly rashes with raised border
- Skin in the middle of the ring appears clear and healthy, and the edges of the ring may spread outward
- Itchy
Read full article on ringworm.
Shingles
- Very painful rash that may burn, tingle, or itch, even if there are no blisters present
- Rash comprising clusters of fluid-filled blisters that break easily and weep fluid
- Rash emerges in a linear stripe pattern that appears most commonly on the torso, but may occur on other parts of the body, including the face
- Rash may be accompanied by low fever, chills, headache, or fatigue
Read full article on shingles.
The main symptom associated with skin redness is varying colors of redness on the skin. The redness can occur on different portions of the body. Here are some examples of symptoms that you may have along with red skin:
- blistering
- bumps
- burning
- flushing
- hives
- itching
- rash
- warmth in your skin
- sores
- swelling
Causes of skin redness vary drastically and can include irritants, the sun, and insect bites. Examples of skin conditions associated with skin redness include:
- bites
- cellulitis
- contact dermatitis
- diaper rash
- eczema
- allergic eczema
- heat rash
- medication allergy
- psoriasis
- ringworm
- rosacea
- scarlet fever
- shingles
- skin burns
- skin infections
- sunburns
- lymph node inflammation
- first-degree burns
- chemical burns
- angioedema
- thromboplebitis
- bone infection
- osteosarcoma
Skin redness can be a temporary, or acute, condition. It can also be a chronic condition that constantly reappears.
It can also be a chronic condition that constantly reappears.
You should get immediate medical attention if you experience any of the following symptoms associated with skin redness:
- a burn that’s twice the size of your palm
- difficulty breathing
- extreme pain
- loss of consciousness
- redness near or on your eyes that is affecting your vision
You should also get medical attention if you have an animal bite, even if you’ve had a tetanus shot.
See a healthcare provider or dermatologist for other symptoms that aren’t considered a medical emergency. If you don’t already have a dermatologist, you can browse doctors in your area through the Healthline FindCare tool.
Your healthcare provider will examine your skin redness. If your symptoms come and go, they’ll listen to your description of them. They’ll ask you a few questions. These could include:
- What activities were you engaging in before you noticed the skin redness?
- Are you taking any new medications or using any new skin care or cleaning products?
- Do you have a family history of any skin conditions?
- Have you experienced this skin redness before?
- Were you around others who may have a similar rash?
These and other questions can help your healthcare provider figure out what may have caused your skin redness.
Additional testing may include taking a skin sample or biopsy of the affected area, or allergy testing to determine if your skin reacts to certain irritants.
Ask your healthcare provider if your skin condition may be contagious and what steps you can take to prevent its spread. This can ensure that you don’t pass on the skin redness to someone else.
Treatments for skin redness depend on what’s causing it. Examples can include avoiding the irritant or allergen that caused your skin redness in the first place.
Other treatments for skin redness include:
- cleansing the affected area with soap and water
- taking medications like antihistamines to minimize irritation
- applying topical skin care treatments like calamine lotion to reduce skin redness
Keeping the affected area clean and dry can usually help reduce skin redness. If an infection is the cause of your skin redness, your healthcare provider may prescribe antibiotics to reduce the infection’s symptoms.
Scleroderma - treatment, symptoms, causes, diagnosis
Scleroderma is a term of Greek origin and means hard skin. The disease is both a rheumatological and connective tissue disorder. With scleroderma, the skin thickens and thickens, and it loses its elasticity. With scleroderma, damage to microvessels throughout the body is possible, which in turn can lead to damage to internal organs. And although the disease mainly affects the hands, face and legs, but the deterioration of blood supply can lead to problems in the digestive tract, in the respiratory system and in the cardiovascular system. nine0003
Scleroderma can present differently in different people. There are many subtypes of this disease. Doctors generally classify scleroderma as either localized or systemic, depending on the extent of skin damage. The widespread form of the disease is often referred to as systemic sclerosis and can be predictively life-threatening.
Approximately 300,000 Americans have been diagnosed with scleroderma.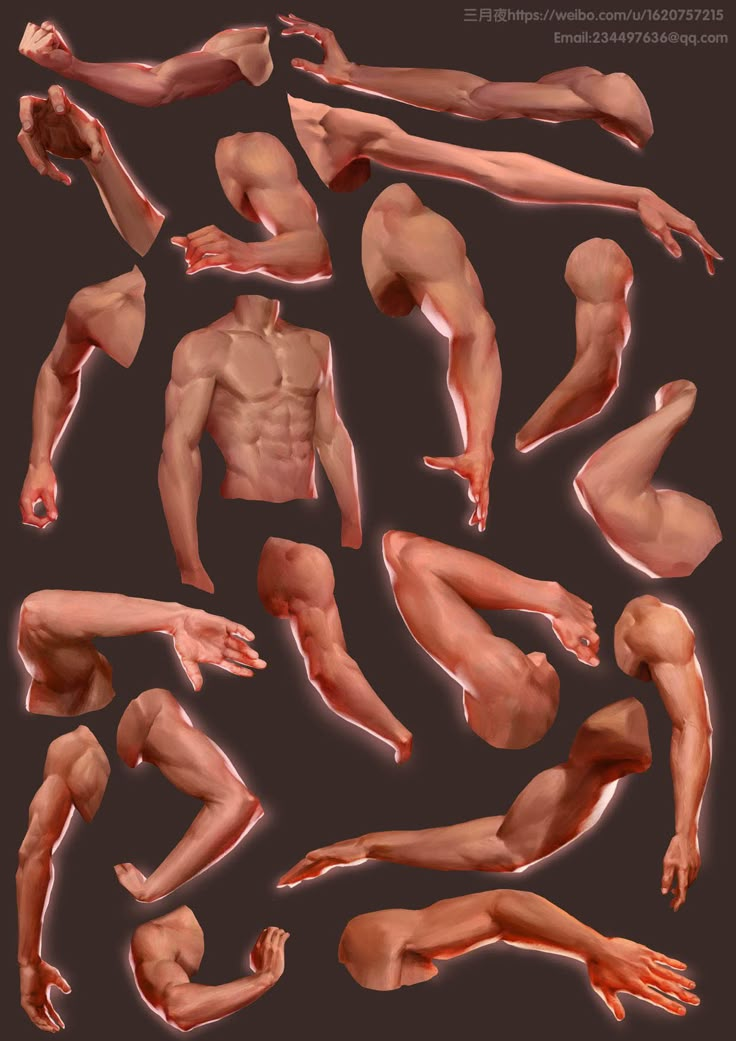 The disease is more common in the US than in Europe or Japan. But it was not possible to identify any dependence on racial or ethnic factors. The only thing that has been noted is that scleroderma is much more common in women than in men. nine0003
The disease is more common in the US than in Europe or Japan. But it was not possible to identify any dependence on racial or ethnic factors. The only thing that has been noted is that scleroderma is much more common in women than in men. nine0003
Women develop limited forms of the disease three times more often than men, and more than 80% of patients with systemic scleroderma are women aged 30 to 50. Rarely, children can also get scleroderma. Over the past 20 years, it has been possible to increase the life expectancy of patients with scleroderma through the use of more effective treatment. Thus, scleroderma is a chronic autoimmune disease, which is manifested by thickening and thickening of the skin and vasoconstriction (as a result, damage to internal organs). The disease develops mainly in adults aged 30-50 years, mainly in women. nine0003
There are two types of scleroderma: limited scleroderma and systemic (diffuse) scleroderma. Localized scleroderma mainly affects the skin, while systemic scleroderma is a systemic disease that can affect various organs and systems of the body.
There are two types of limited scleroderma:
- Plaque form: manifested by the appearance of spots on the skin, oval red or purple, dense to the touch (as the plaque develops, it may become whitish in the center)
- Linear: streaks of thickening appear on the skin of the arms, legs, or face.
Systemic scleroderma can begin gradually with involvement of the skin of the hands, face at first, or be progressive, involving not only the limbs, but also the trunk and internal organs (usually the lungs, esophagus, intestines):
Causes
The main feature of scleroderma is an overproduction of collagen. Collagen is one of the building materials that makes up the skin. With an excess of collagen, tissue thickening and loss of elasticity occur. nine0003
The underlying cause of scleroderma is still unclear. For some unknown reason, the immune system turns against body tissues and the result is an overproduction of collagen. Currently, studies are underway to identify the relationship between the immune system, the vascular system and the growth of connective tissue. Studies on twins have shown the absence of a genetic factor. And although the cause of scleroderma has not been established, the mechanism of the disease is associated with autoimmune processes, in which damage occurs to both the skin and other organs. The autoimmune process triggers an excess production of collagen, which leads to thickening and thickening of the skin. In addition, changes in the connective tissue lead to pressure on the vessels of both large and small arteries. nine0003
Studies on twins have shown the absence of a genetic factor. And although the cause of scleroderma has not been established, the mechanism of the disease is associated with autoimmune processes, in which damage occurs to both the skin and other organs. The autoimmune process triggers an excess production of collagen, which leads to thickening and thickening of the skin. In addition, changes in the connective tissue lead to pressure on the vessels of both large and small arteries. nine0003
Symptoms
The symptoms of scleroderma can vary from patient to patient. The most common manifestations are hardening and thickening of the skin on the toes and face. The skin may thicken during the first two to three years of the disease. After that, the thickening, as a rule, decreases. The main symptoms of scleroderma include:
- Swelling, stiffness, or pain in the toes or fingers, or face.
- Tingling, numbness, or swelling of the skin. nine0016
- Skin discoloration.
- Sensitivity to cold and intermittent and transient pallor of the fingers (Raynaud's syndrome), accompanied by pain in the fingers.
- Red spots on the fingers, palms, face, lips, or tongue, from persistently dilated capillaries (telangiectasia).
- Ulcers or sores on fingertips or elbows.
- Loss of the ability of the skin to stretch.
- Itching.
- Joint pain nine0015 Fatigue.
- Twisting fingers (sclerodactyly).
- Presence of calcifications under the skin
- Gastrointestinal disorders such as heartburn, difficulty swallowing, prolonged retention of food in the digestive tract due to decreased activity of intestinal smooth muscle.
- Loss of motor function of the hand due to tightening of the skin on the hand and fingers.
- Shortness of breath associated with damage to the lungs and heart. nine0019
- Never go without gloves in winter! Even once forgotten in a coat pocket or in a car, gloves can cause a lot of problems for the skin for a long time. This means that gloves should be worn even if there is a short walk from the parking lot to the nearest store. Remember that the skin on the hands must be protected with gloves not only when the temperature drops to minus or stays around zero, but already starting from +6 degrees. nine0016
- Never go outside with wet hands in cold weather – when moisture evaporates, it also takes part of the skin's natural moisture with it. If you recently washed your hands, gently dry them, apply cream on them, and wait until the cream is absorbed into the skin before leaving the house.
 Remember that it is best to wash your hands with moderately warm water.
Remember that it is best to wash your hands with moderately warm water. - Choose quality hand soap - this is especially important now that we wash our hands so often. Pronounced cleansing and antibacterial agents are very aggressive towards the skin of the hands. It is better to buy detergents in a pharmacy - they will treat your hands more carefully. You can also choose a quality hand soap based on oil or cream with Shea butter, which, in addition to the cleansing function, will nourish and moisturize the skin. nine0016
- Avoid moistening your hands too often - after each time you go to the tap to wash the cup, dry your hands. For this reason, if possible, homework should be planned: try to clean, clean, wash dishes consistently. When cleaning and washing dishes, it is always advisable to use gloves that will simultaneously protect your hands from the aggressive effects of household chemicals. It is advisable to choose gloves such that their outer surface is impenetrable, for example, rubber, and inside there is a small lining or protective layer - unlined rubber gloves may not be liked by damaged skin.
 nine0016
nine0016 - Use the cream several times during the day - hand washing and disinfection degreases the skin, depriving it of its natural protective layer. If it is not there, the skin quickly loses moisture, cracks form, which further accelerate the process of moisture loss. Therefore, after each time you have washed your hands or sanitized them, do not forget to apply the cream on your palms.
- Hands that already have dry skin are irritated by contact with the juice of food products rich in various acids. These are, for example, potatoes, carrots, oranges, tomatoes. For this reason, it is advisable to use protective gloves during cooking as well. nine0016
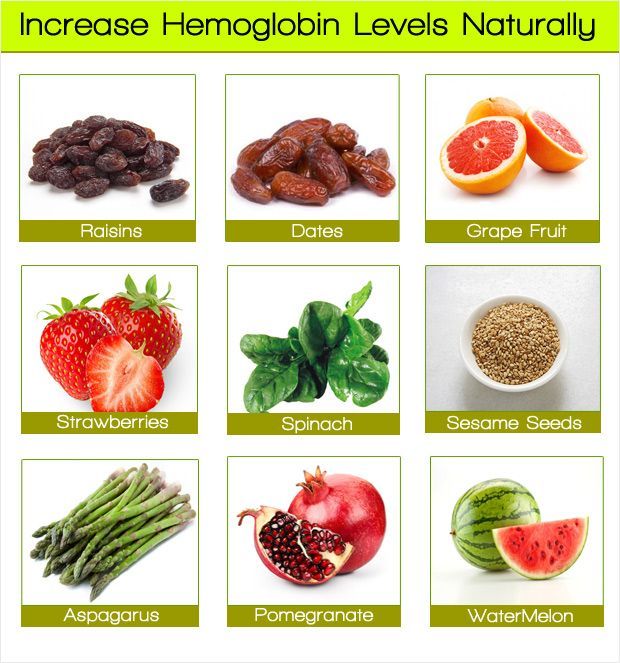
- Vitamins A and E: vitamin A improves skin texture and elasticity, while vitamin E protects against environmental aggressors and stimulates skin regeneration.
- Omega 3, 6 and 9 fatty acids are excellent skin moisturizers.

- Shea Butter is a natural miracle product that perfectly nourishes and moisturizes the skin, the same qualities have almond oil and argan oil. nine0016
- D-panthenol - if there are microdamages on the skin, this substance will help to heal them.
- Glycerin - helps create a thin protective layer on the skin that helps retain moisture in the skin.
- Uric acid - if the skin on the hands is rough, creams containing UREA at a concentration of 5-10% can come to the rescue. They will perfectly moisturize the skin and at the same time free the upper surface from roughness.
- NMF is a natural moisturizing factor that contains sodium lactate, lactic acid, urea and allantoin to deeply hydrate severely dehydrated skin.
- Bepanthen or Recreol (locally produced) is a healing, repairing and soothing ointment to repair skin damage.
- Creams with dexpenthenol, ceramides and zinc.
- Creams with names CICA, CICABIO, CICAPLAST B5 and CICAVIT . They include copper, zinc, panthenol and other active healing substances. nine0016
- Healing creams containing silver .

- Night mask - if the hands are very dry. Choose a rich, thick hand cream, such as one with 25% Shea butter. Spread a thick layer of cream on your hands and put on cotton gloves over it. The skin will appreciate if you keep such a mask all night or at least 20-30 minutes before going to bed.
- Scrub your skin twice a month. Sometimes, if the hands are too dry, the cream for rough skin does not cope and does not absorb at all. The solution is a scrub.

Diagnosis
Scleroderma is often difficult to diagnose because it can look like many other diseases. Changes in skin thickness, the presence of certain antibodies in the blood, or early changes in blood vessels can be helpful in diagnosing the disease. If necessary, it is possible to take a biopsy for tissue analysis, which also helps to make a diagnosis.
Changes in skin thickness, the presence of certain antibodies in the blood, or early changes in blood vessels can be helpful in diagnosing the disease. If necessary, it is possible to take a biopsy for tissue analysis, which also helps to make a diagnosis.
One useful test is the nail capillary analysis. It is based on the early manifestation of scleroderma and is manifested by the disappearance of capillaries in the skin of the hands and feet. For this analysis, a microscope or magnifying glass is used and the skin in the nail area is viewed. For an accurate diagnosis, it is necessary to compare both laboratory methods of research and clinical data, and the history of the disease. nine0003
Treatment
There is no pathogenic treatment for scleroderma yet. The goal of treatment is to reduce symptoms and reduce the risk of complications. Medicines used in scleroderma:
For limited manifestations, it is possible to use ointments of a moisturizing nature or containing corticosteroids. In addition, UVI procedures give a good result.
In addition, UVI procedures give a good result.
Vasodilator drugs that relax and widen the blood vessels may be given to reduce the symptoms of Raynaud's syndrome, when blood flow to the distal extremities is interrupted. ACE inhibitors are prescribed in the presence of hypertension and the presence of problems in the vessels of the kidneys. nine0003
Non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, naproxen, and ibuprofen can relieve joint pain. Corticosteroids such as prednisone may also be used to reduce inflammation.
Dyspepsia can occur when scleroderma affects the esophagus, stomach, or intestines. This can be treated with drugs that reduce the acidity of the stomach and normalize intestinal motility.
Immunosuppressants such as D-penicillamine reduce collagen production to some extent, but their therapeutic effect is accompanied by pronounced side effects and their use is rather limited. nine0003
Physical therapy and physiotherapy can be beneficial in the treatment of scleroderma by helping to maintain the elasticity of the ligaments and joints. Surgical methods of treatment are sometimes used for severe contractures, deformities, or scars.
Surgical methods of treatment are sometimes used for severe contractures, deformities, or scars.
Dry and cracked hands. What to do?
The cold season of the year is a real test for the skin of the hands. Gloves once again forgotten in the pocket, sudden changes in temperature and heating - all this has a negative effect on the hands. An even greater challenge to the health and well-being of the skin today is frequent washing and disinfection. Why hands become dry and crack in the winter season, how to properly care for them and restore them, said a dermatologist Dermatology clinics Veselības Centrs 4 Vita Come.
In winter, not only the hands become drier, but also the skin in general. One of the main culprits for this with the onset of the heating season is dry air, which literally dries our skin. We feel this better with our hands, because while the rest of the body is covered with clothes, the hands are more often exposed to air and temperature changes; Other aggressive factors also harm the skin of the hands - disinfectants that dry the skin, detergents and cleaning products, wind. nine0003
nine0003
Dermatologist V. Priedite emphasizes that the best advice for almost all cases is prevention: try not to let dry skin develop, because once dryness and cracks have already appeared, it will be much more difficult to deal with the problem.
What can I do to prevent dry hands?
In winter, it is very important not to forget about the regular use of the cream. When you feel that your hands are dry and as if they are asking for cream, it will be too late! It will be correct to apply the cream when such a sensation has not yet arisen.
If due to everyday worries you forget to use the cream during the day, make it easier for yourself: make sure that you always have a tube of cream at hand - in the bathroom where you wash your hands, in the kitchen, at work table, in an outdoor bag, next to the TV and on the nightstand. nine0003
nine0003
The main function of the cream is to help to stick the skin cells together, creating a protective layer on the hands, and thus slow down the loss of moisture from the deeper layers of the skin. Each person, based on their needs and skin characteristics, needs to choose one or more creams for themselves.
How to choose a hand cream?
If the hands are only dry, the cream can be chosen quite freely, according to one's taste and sensations. Each cream is uniquely formulated for its effectiveness and can be formulated to hydrate, nourish, or revitalize the skin. Although the choice of cream is very individual, a dermatologist recommends paying attention to its composition. nine0003
Useful ingredients to look for in hand cream:
How to choose a cream if the skin is already cracking?
If the skin is red, deeply cracked, itchy, or has small, fluid-filled blisters, this indicates a serious allergic reaction and inflammation. In such a situation, it makes sense to schedule a visit to a dermatologist, as you may have to take medication to fix the problem. However, you can try to cope on your own: for this you should choose a cream with healing qualities. In such cases, it is advisable to choose pharmacy products, because the composition of these creams is tested and has more pronounced healing properties than products that can be found in stores. Also in such creams there will be no harmful substances, irritating flavors and unnecessary preservatives. nine0003
In such a situation, it makes sense to schedule a visit to a dermatologist, as you may have to take medication to fix the problem. However, you can try to cope on your own: for this you should choose a cream with healing qualities. In such cases, it is advisable to choose pharmacy products, because the composition of these creams is tested and has more pronounced healing properties than products that can be found in stores. Also in such creams there will be no harmful substances, irritating flavors and unnecessary preservatives. nine0003
Try this:
Remember! First aid for chapped and severely damaged hand skin is to eliminate the irritating factor and protect hands: refrain from wetting, contact with aggressive chemicals, exposure to temperature changes. Even with the use of medicines prescribed by a doctor, nothing will help if we continue to irritate our hands! Taking care of your hands and protecting them from exposure to irritants is half the battle! nine0003