Red bumps on infant
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Nappy rash - NHS
Around 1 in 4 babies and toddlers in nappies have nappy rash at any one time. It doesn't usually develop in newborns, but all babies can get nappy rash.
Nappy rash can be caused by:
- your baby's skin being in contact with wee or poo for a long time
- the nappy rubbing against your baby's skin
- not cleaning the nappy area or changing the nappy often enough
- soap, detergent or bubble bath
- alcohol-based baby wipes
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
There may be red patches on your baby's bottom, or the whole area may be red. Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Most babies with mild nappy rash don't feel sore, but if the rash is severe your baby may feel uncomfortable and be distressed.
Treating nappy rashIf your baby gets nappy rash, you can usually treat their skin yourself.
If the rash isn't upsetting your baby, at each nappy change apply a thin layer of a barrier cream to protect their skin. Ask your health visitor or pharmacist to recommend one.
Follow this advice to help look after your baby's skin.
- Change wet or dirty nappies as soon as possible.
- Clean the whole nappy area gently but thoroughly, wiping from front to back. Use water or fragrance-free and alcohol-free baby wipes. Read more about how to clean your baby and change your baby's nappy.

- Bath your baby daily – but avoid bathing them more than twice a day as that may dry out their skin.
- Dry your baby gently after washing them – avoid vigorous rubbing.
- Lie your baby on a towel and leave their nappy off for as long and as often as you can to let fresh air get to their skin.
- Do not use soap, bubble bath, or lotions.
- Do not use talcum powder as it contains ingredients that could irritate your baby's skin.
- Make sure your baby’s nappy fits properly. If it is too tight then it can irritate the skin and if it is too loose, then the nappy will not be able to soak up pee properly.
Nappy rash usually clears up after about 3 days if you follow this advice. You should keep following this advice as this will help prevent nappy rash from coming back.
If the rash is causing your baby discomfort, your health visitor or pharmacist can recommend a nappy rash cream to treat it.
You should apply the cream first and wait a few minutes before you apply the barrier cream.
Other rashes in the nappy areaIf the rash doesn't go away or your baby develops a persistent bright red, moist rash with white or red pimples that spreads into the folds of their skin, they may have an infection.
Ask a pharmacist or health visitor for advice. The pharmacist may recommend a cream for you to use.
If the rash is severe, take your baby to the GP who may prescribe cream or medicine. Follow a GP's instructions on whether and when to apply barrier cream as well as the prescribed cream.
It's normal for babies to develop skin rashes, but it's important to know the difference between a minor irritation and a condition that requires attention.
Read more about rashes in babies and children.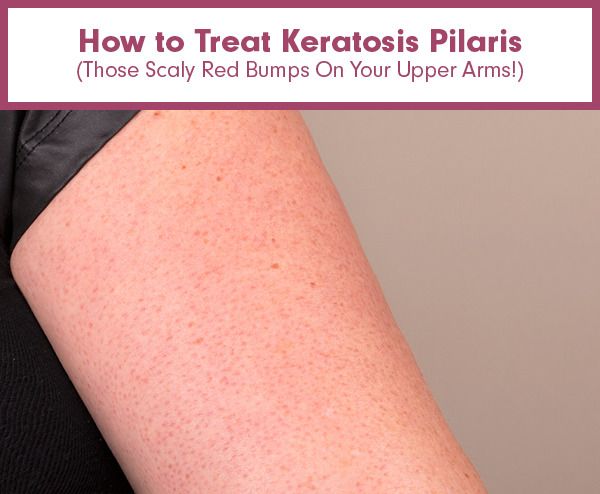
Page last reviewed: 17 September 2021
Next review due: 17 September 2024
How to care for the skin of a newborn.
After discharge from the hospital, mother and baby gradually get used to the daily routine. The child should eat well and be warm - this is the first on the list. No less important is the care of the skin of the baby, which is very delicate and sensitive to external stimuli. To adapt to the new environment, the baby needs time and care of parents. Chemicals, fragrances, dyes in clothes, and detergents cause redness, diaper rash, or a rash. How to properly care for the skin of a newborn to protect the child from contact dermatitis, allergies, and other rashes?
Bathing
The baby is born with a protective coating. During this period, there is no need to bathe the baby or use baby lotions and creams.
A full bath is normal from the first days of a baby's life, the main thing is to follow the rules:
- bathe your baby in a warm room.
- water should be at body temperature: 36-37 degrees to the touch.
- make sure the necessary items for the procedure are within reach. - remove jewelry that can scratch the child.
- hold the newborn firmly by lifting his head above the water.
- do not use cotton swabs to clean the nose and ears.
- To wash your baby's face, use water without soap.
- never leave a child unattended while bathing, even for a moment.
- For the first 2-3 months after birth, give up shampoo and soap, which can cause an allergic reaction in the baby.
- if you do use baby bath products, make sure they are soft, suitable for babies and odorless.
- then carefully wrap the baby in a cotton towel or a special corner robe for newborns.
- the room in which the baby will be after the bath should be warm, and air conditioners and fans should be turned off to prevent colds.
Umbilical cord care
By the time of discharge from the hospital, this organ, which connected mother and baby during all 9 months of pregnancy, will begin to dry out. Gradually, the umbilical cord atrophies and falls off within 1-2 weeks. Until then, the place of its attachment to the belly of the newborn must be kept clean and dry. All you need is plain water. You can not pull the keratinized part, even if it begins to fall off. The process will end by itself. To protect your baby's delicate skin, buy diapers for newborns that have a notch in the waistband for the unhealed navel. If you are using regular diapers, fold the edge so that the fabric does not rub against the tummy. In some cases, the child may need a doctor. Contact your pediatrician if your child has a fever of 38°C or more along with changes in the navel: the area is red and swollen; oozing yellow pus; there is an unpleasant smell. Many mothers are worried about the appearance of small specks of blood on the baby's undershirt or diaper, the child's bed. A little bleeding is normal.
Many mothers are worried about the appearance of small specks of blood on the baby's undershirt or diaper, the child's bed. A little bleeding is normal.
Diapers and diapers
Change diapers more often as soon as you notice that they are wet or dirty. If left for too long, it can cause infections. For newborn hygiene, thoroughly clean the genital area after every diaper change. Wash your baby under warm, running water to prevent irritation. Allow a few minutes for the skin to air dry, or gently pat dry with a soft towel. Use baby wipes less often to care for your newborn's skin. Perfume and alcohol in them can cause irritation, cause a rash. Make sure you buy diapers in a size that fits your baby. If the baby's skin in the diaper area is irritated, choose a different brand or stop using them for a while. . Wash reusable diapers and diapers with a mild, unscented detergent or clean, hot water. Most diaper rashes on a newborn's skin are not dangerous, but some can be a sign of an infection and need to be looked after. If the baby's skin is very reddened, itchy, or causes pain, contact your pediatrician immediately.
What to do in case of skin problems
In the first months after birth, the baby may develop a rash, irritation, diaper rash, which seem unusual to parents.
Most of the newborn skin problems do not need treatment:
- baby pimples - a small red rash on the face. As a rule, it disappears over time without intervention.
- milia are tiny whiteheads on a child's face.
- erythema is a common patchy rash that can affect newborns. Some appear as yellow or white bumps surrounded by a red halo. The rash tends to migrate to different parts of the body. It is most common on the second day of life, but may appear at birth or within the first two weeks. There is no cure - erythema gradually disappears on its own.
Eczema
This rash appears as red bumps that may fester. It usually appears on the forehead, cheeks, or scalp, and sometimes spreads to other parts of the body. The risk group includes infants who suffer from allergies from birth or have a genetic predisposition to the disease. In case of pathology, it is recommended to use special moisturizers: ointments, creams, oils. Do not bathe the baby for a long time with this disease. When an allergic rash appears, a consultation with a pediatrician is required.
Diaper rash
Causes:
- untimely diaper change. Urine or stool in a diaper irritates a newborn's skin, causing red weeping spots.
- bacterial or yeast infection. Taking antibiotics can cause the growth of fungi of the genus Candida. It usually appears around the genitals and buttocks of an infant. It looks like red spots with a whitish coating.
How to properly care for your skin to prevent diaper rash:
- do not use reusable diapers often.
- give up talcum powder: it dries out the skin of a newborn.
- air baths for half an hour. Heat rash is caused by overheating of the body. It is usually visible in the folds of the baby's skin. Hot, humid weather is a favorable time for prickly heat. To avoid rashes, keep your newborn cool by dressing him in loose cotton clothing.
Contact dermatitis
This disease develops when an infant's skin comes into contact with an irritant. The rash appears at the points of contact with the allergen: metal latches on T-shirts; dyes in clothes; washing powder; inappropriate soap, shampoo; allergic to the oil used. Parents need to trace, after which rashes appear, and eliminate the irritant. To bathe the baby, you need to use shampoo and soap that do not cause allergies in the newborn; iron baby clothes before putting them on. For washing, special powders or gels are used that do not contain fragrances and dyes, the child's clothes, bed linen and blankets are washed separately from the family's wardrobe items.
Newborn acne and all you need to know about it - Allergika Ukraine
Newborn acne occurs in almost every second child and usually appears within the first month after birth, but may appear earlier. Some babies are already born with mild acne.
The good news is that neonatal acne is a transient condition and almost always resolves quickly and without treatment. Most cases of acne in a newborn disappear completely by six months of age.
How can you tell if a child's rash is really acne?
Neonatal acne looks like small red bumps that form on the face, less often on the back or chest. In some children, newborn acne looks like a rough bumpy red rash. Newborn acne clears up on its own within a few weeks and may get worse when the baby cries or rubs their face with their hands.
Many other skin conditions common in children, such as eczema, erythema, miliaria, may resemble acne.
Eczema
Eczema usually appears as red, scaly patches on the face and body. They may also appear under the knees or in the crooks of the elbows. Often eczema occurs at an older age.
The most common type of eczema is known as atopic dermatitis.
Seborrheic dermatitis is a condition most often mistaken for neonatal acne. Seborrheic dermatitis is also known as gneiss or milk crusts.
Erythema toxic
Erythema toxic is another common skin condition that can present as a rash, tiny bumps, or red spots. They can be seen on your baby's face, chest, or limbs in the first few days after birth. Usually disappears less than a week after birth.
Milia are tiny white dots on the skin that look like pustules but are not inflamed and are common in newborns. Milia appear within the first few weeks of life, and many babies are born with them. Milia are completely harmless and, like acne in a newborn baby, the vast majority of cases will go away without treatment.
Causes of acne in newborns
Acne develops during the first weeks after birth under the influence of hormones.