Recurrent yeast infection in pregnancy
Yeast Infections and Pregnancy: Causes, Symptoms & More
What’s a yeast infection?
Vulvovaginal candidiasis, or moniliasis, is a yeast infection of the vulva and vagina. Yeast is a type of fungus. The yeast that most often causes these infections is Candida albicans, but other types of yeast — including Candida glabrata and Candida tropicalis — can also be responsible.
About three out of every four women will have at least one yeast infection in their lifetime, according to American Family Physician. Up to 45 percent will get two or more infections.
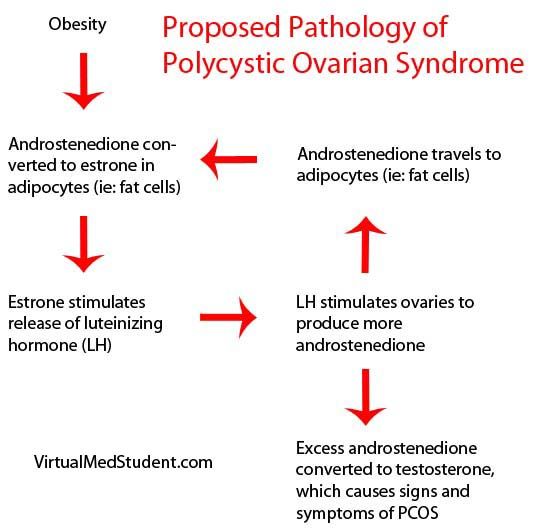
During pregnancy, Candida (and the infections it causes) is even more common. According to one study, about 20 percent of women have Candida yeast in their vagina normally. That number goes up to 30 percent during pregnancy. Yeast is more likely to cause infection during pregnancy due to hormone fluctuations.
Because you can pass the yeast to your baby during delivery, it’s important to get treated.
What causes candidiasis?
Candidiasis occurs when the normal number of fungi that reside in the vagina increases enough to cause symptoms. The most common factors that make a woman more likely to get yeast infections include:
- pregnancy
- diabetes
- use of birth control pills, antibiotics, or corticosteroids such as prednisone (Rayos)
- disorders that weaken the immune system, such as HIV
During pregnancy, shifting hormone levels change the pH balance in the vagina. This creates an environment that’s more favorable for yeast to grow.
What complications are associated with yeast infections?
In nonpregnant women who have a normal immune system, yeast infections rarely lead to serious complications.
Even in pregnancy, yeast infections don’t usually cause harmful effects in the mother. However, you can pass the yeast to your baby during delivery.
Most babies who develop a yeast infection have it just in their mouths or diaper area. However, though rare, a yeast infection in babies can become very serious, because their immune systems aren’t yet well-developed. It can spread through the infant’s body and affect breathing and heart rhythm, for example. This happens most often in babies who have other things affecting their immune systems, such as prematurity or an underlying infection.
However, though rare, a yeast infection in babies can become very serious, because their immune systems aren’t yet well-developed. It can spread through the infant’s body and affect breathing and heart rhythm, for example. This happens most often in babies who have other things affecting their immune systems, such as prematurity or an underlying infection.
Yeast infections can also cause body-wide infections and serious complications in women who have a weakened immune system because of conditions such as HIV.
What are the signs and symptoms of candidiasis?
With candidiasis, you’ll most likely have itching in your vagina and vulva. You may also notice a white vaginal discharge. This discharge may look similar to cottage cheese and shouldn’t have an odor.
Other symptoms include:
- soreness or pain in the vagina or vulva
- burning when you urinate
- a rash on the vulva and the skin around it, which sometimes appears on the groin and thighs as well
These symptoms may last for a few hours, days, or weeks.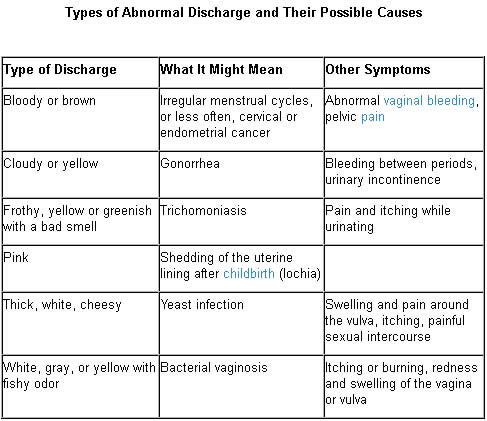
In newborn babies and in women who have a weakened immune system, candidiasis may occur in the mouth. This condition is known as thrush.
Other conditions can cause symptoms similar to a yeast infection, including:
- an allergic reaction to a product you’ve used in the vaginal area, such as soap or a condom
- sexually transmitted diseases (STDs) such as chlamydia and gonorrhea
- bacterial vaginosis, a type of infection
How can I prevent a yeast infection?
You can reduce your risk of future yeast infections by:
- keeping the vaginal area dry
- avoiding bubble baths, feminine hygiene sprays, and douches
- wearing cotton underwear
Although candidiasis isn’t an STD, oral sex may make your condition worse and affect your sexual partner.
How is candidiasis diagnosed?
Your doctor will ask about your symptoms and do a physical exam. To confirm the diagnosis, your doctor will use a cotton swab to take a sample of the vaginal discharge. The sample will be checked under a microscope for signs of the yeasts that cause infections.
The sample will be checked under a microscope for signs of the yeasts that cause infections.
In certain cases, your doctor may want to culture — or grow in a lab — a sample of your vaginal discharge. Cultures help them rule out other types of yeast, such as C. glabrata and C. tropicalis.
How is candidiasis treated?
Most of the time, vulvovaginal candidiasis is easy to treat with an antifungal cream or suppository. The medicine should relieve your symptoms within seven days. However, during pregnancy, you should see your doctor before starting treatment. They can confirm that you actually have a yeast infection and ensure you get a treatment that’s safe to use during pregnancy.
Both oral and topical antifungal drugs are used to treat yeast infections in nonpregnant women. However, oral drugs may not be safe to use during pregnancy. A 2016 study in JAMA found an association between higher risk of miscarriage and oral fluconazole (Diflucan) use during pregnancy. Oral antifungal drugs have also been linked to birth defects.
Oral antifungal drugs have also been linked to birth defects.
Topical antifungal drugs that are safe to use during pregnancy include:
How should repeat yeast infections be treated?
During pregnancy, you’re more likely to have repeated yeast infections. Four or more yeast infections in one year is called recurrent vulvovaginal candidiasis.
If you keep getting yeast infections, talk to your doctor. You may need to be evaluated for risk factors such as diabetes or an immune disorder. If pregnancy is the cause, the infections should stop after you deliver.
Research finds that taking an oral “azole” drug for six months reduces your chance of a repeat infection. However, oral antifungal medicines might not be safe to use during your pregnancy. You may have to wait until after you deliver to go on this treatment.
Yeast Infections During Pregnancy - American Pregnancy Association
Yeast infections during pregnancy are more common than any other time in a woman’s life, especially during the second trimester of pregnancy. You may be noticing an increase in the amount of thin, white, odd smelling discharge. This is common and a normal symptom in the second trimester.
You may be noticing an increase in the amount of thin, white, odd smelling discharge. This is common and a normal symptom in the second trimester.
If you think you may be experiencing a yeast infection, the following information will prepare you to discuss the possibility with your doctor. Though yeast infections have no major negative effect on pregnancy, they are often more difficult to control during pregnancy, causing significant discomfort for you. Don’t wait to seek treatment!
What is a yeast infection?
Yeast infection occurs when the normal levels of acid and yeast in the vagina are out of balance, which allows the yeast to overgrow causing an uncomfortable, but not serious, a condition called a yeast infection.
If you have never been diagnosed or treated by a physician for a yeast infection and have some of the symptoms, you should see your physician first for accurate diagnosis and treatment. Other infections have similar symptoms, so you want to make sure that you are treating the infection correctly. There are also treatments that are not appropriate during pregnancy.
There are also treatments that are not appropriate during pregnancy.
What causes yeast infections during pregnancy?
A yeast infection can be caused by one or more of the following:
- Hormonal changes that come with pregnancy or before your period
- Taking hormones or birth control pills
- Taking antibiotics or steroids
- High blood sugar, as in diabetes
- Vaginal intercourse
- Douching
- Blood or semen
Why are yeast infections more common during pregnancy?
Your body is going through so many changes right now, and it is difficult for your body to keep up with the chemical changes in the vagina. There is more sugar in vaginal secretions on which the yeast can feed, causing an imbalance which results in too much yeast.
What are the symptoms of yeast infections?
The symptoms of a yeast infection may include one or more of the following:
- Discharge that is usually white/tan in color, similar to cottage cheese and may smell like yeast/bread
- Other discharge may be greenish or yellowish, also similar to cottage cheese and may smell like yeast/bread
- An increase in discharge
- Redness, itching, or irritation of the lips of the vagina
- Burning sensation during urination or intercourse
What else could I be experiencing?
If you are experiencing symptoms similar to a yeast infection, but a physician has ruled this diagnosis out, you may have one of the following:
- Sexually Transmitted Diseases (STDs) like Chlamydia, Gonorrhea, & Trichomoniasis
- A vaginal infection called bacterial vaginosis
How do I know for sure if I have a yeast infection?
At your doctor’s office or medical clinic, a clinician will use a simple, painless swab to remove the discharge or vaginal secretions and examine it through a microscope. Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
How are yeast infections treated during pregnancy?
During pregnancy, physicians recommend vaginal creams and suppositories only. The oral medication, Diflucan (a single-dose medication), has not been proven safe during pregnancy and lactation. Not all vaginal creams and suppositories are okay to use during pregnancy, so it is best to consult your doctor or pharmacist to get the right one. If left untreated, yeast infections can pass to your baby’s mouth during delivery. This is called “thrush” and is effectively treated with Nystatin.
It may take 10-14 days to find relief or completely clear up the infection while you are pregnant. After the infection has cleared up and any sores have healed, it may be helpful to use a starch-free drying powder, or Nystatin powder to prevent a recurring infection.
How can I prevent a yeast infection or recurring yeast infections?
Most yeast infections can usually be avoided by doing the following:
- Wear loose, breathable cotton clothing and cotton underwear.

- After regular, thorough washing (using unscented, hypoallergenic or gentle soap), use your blow dryer on a low, cool setting to help dry the outside of your genital area.
- Always wipe from front to back after using the restroom.
- Shower immediately after you swim. Change out of your swimsuit, workout clothes, or other damp clothes as soon as possible.
- Do NOT:
- douche
- use feminine hygiene sprays
- use sanitary pads and tampons that contain deodorant
- take a bubble bath/use scented soaps
- use colored or perfumed toilet paper
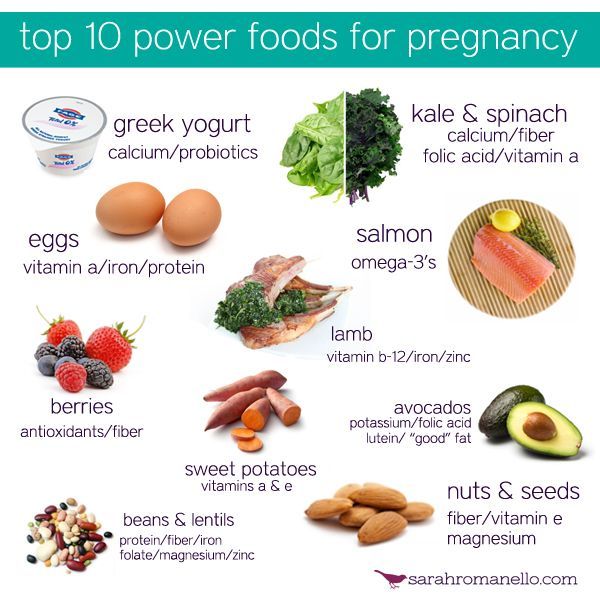
- Include yogurt with “lactobacillus acidophilus” in your diet.
- Limit sugar intake, as sugar promotes the growth of yeast.
- Get plenty of rest to make it easier for your body to fight infections.
When should I contact my doctor?
If you are experiencing the symptoms described in this article, call your doctor now. Yeast infections have similar symptoms of other infections, such as STDs. Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
If you see no improvement within three days, or if symptoms worsen or come back after treatment, you should contact your healthcare provider again.
Want to Know More?
- Pregnancy Nutrition
- Medication and Pregnancy
Compiled using information from the following sources:
1. American Academy of Family Physicians
https://familydoctor.org
1. Mayo Clinic Complete Book of Pregnancy & Babys First Year. Johnson, Robert V., M.D., et al, Ch. 11.
Ecofucin for the treatment of thrush during pregnancy.
Thrush is a disease of the vaginal and vulvar mucosa caused by yeast-like fungi of the genus Candida, which affects 35% of women during pregnancy 1 .
At risk for the occurrence of a recurrent form of thrush are those pregnant women who have already had episodes of thrush in their anamnesis the level of estrogens rises, in connection with which glycogen accumulates in the vaginal mucosa - a nutrient medium for yeast-like fungi of the genus Candida.
Lactobacilli are the predominant microorganisms in the vaginal microflora of a healthy woman. A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli also participate in the formation of local immunity
In addition, during thrush, the vaginal microflora is disturbed - the number of lactobacilli decreases sharply. These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush.
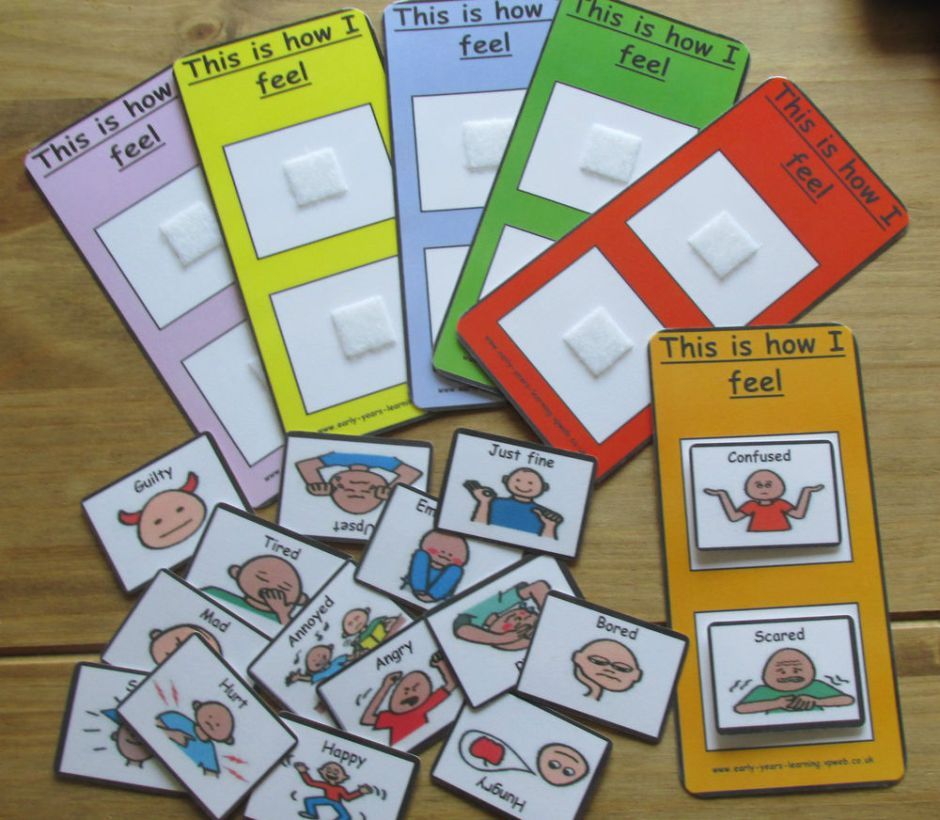
Symptoms of thrush in a pregnant woman:
- itching and burning in the vulva and/or vagina, swelling and irritation in the vulva
- vaginal discharge with a "curdled character" and occasional foul odor
- pain during and after intercourse
- urination disorder and pain
The appearance of at least one of the symptoms is a reason for an unscheduled visit to the doctor.
Why is it important to diagnose and treat thrush in a pregnant woman in time?
Some women are asymptomatic carriers of yeast-like fungi of the genus Candida and experience neither discomfort nor manifestations of the disease throughout the entire period of pregnancy 2
A pregnant woman with thrush (including an asymptomatic carrier) is a source of infection for her unborn child. Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with fungi of the genus Candida is especially dangerous 2 .
Timely and effective treatment of thrush in a pregnant woman is an important task
Treatment of thrush
Safety and efficacy are the main criteria for choosing a drug in the treatment of thrush in pregnant women
The earlier a pregnant woman is diagnosed and treated for thrush, the less the risk of negative consequences and complications for the course of pregnancy and for the health of the mother and her unborn child.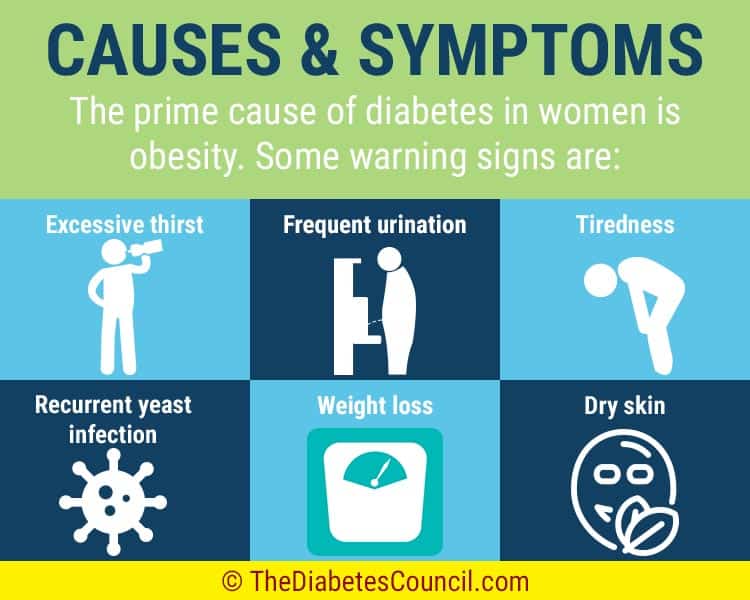 In the treatment of thrush, experts recommend an integrated approach to therapy.
In the treatment of thrush, experts recommend an integrated approach to therapy.
It is important to follow the recommendations of a specialist, following the prescribed dosage and regimen.
Comprehensive treatment should be aimed at solving two problems: eliminating the cause of thrush (fungi of the genus Candida) and restoring the vaginal microflora. It is important to know that not all drugs are approved for use during pregnancy. For example, most oral (systemic) drugs and some topical drugs for treating thrush are contraindicated during pregnancy.
Ecofucin
® in the treatment of thrush in pregnancyEcofucin
® is allowed at all stages of pregnancy and lactation 4
Natamycin
- practically not absorbed into the blood and has no systemic effect
- has a fungicidal effect - causes fungal cell death
- resistance to it does not develop
- does not inhibit the growth of natural microflora
+
Prebiotic 5
- actively fermented by the normal microflora of the vagina, stimulating the growth of lactobacilli 6
- causes restoration of the vaginal microflora, stimulates local immunity 6
The active substance 7 of Ecofucin ® eliminates the cause of thrush, and the prebiotic 5 in Ecofucin ® promotes the restoration of the vaginal microflora and strengthens local immunity 6 .
Efficacy and safety of the drug Ecofucin has been proven by clinical studies
Ecofucin promotes faster recovery of patients with thrush.
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Ecofucin helps to increase the number of own lactobacilli in the vagina and reduce the risk of recurrence of thrush.
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Dosage and Administration
The regimen for the use of Ecofucin ® in a pregnant woman is prescribed by the attending physician individually.
Additional conditions for effective treatment of thrush are: giving up bad habits, a carbohydrate-restricted diet, wearing underwear made from natural fabrics, etc.
It is important to consult a gynecologist in a timely manner and exclude self-medication.
1. Tikhomirov A.L., Sarsania S.I. Features of candidal vulvovaginitis in pregnant women at the present stage. // Farmateka No. 9, 2009, p. 64-70.
2. Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bairamova G.R. Federal clinical guidelines "Urogenital candidiasis". // 2013.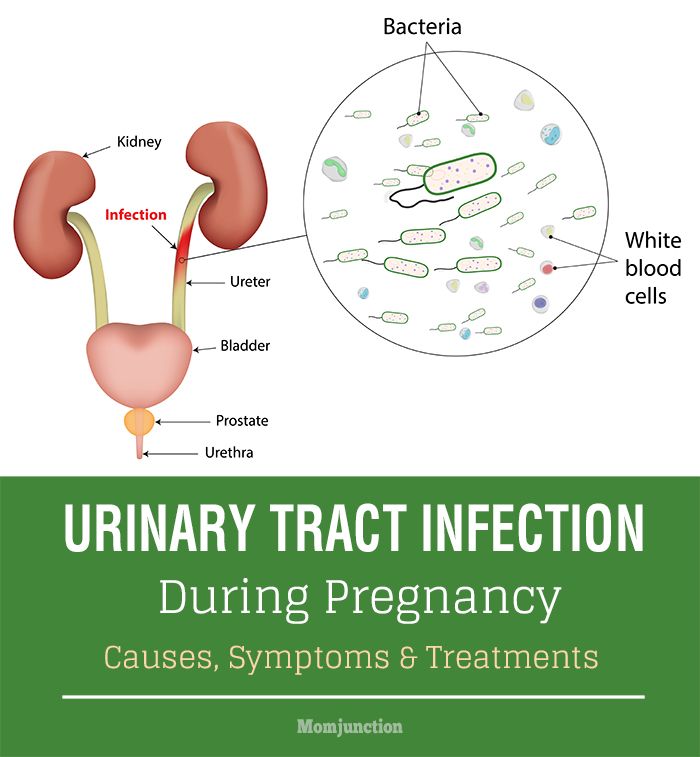
3. Kupert A.F., Akudovich N.V., Khoroshikh O.V., Vereshchagina S.A., Khmel T.V. Features of the clinic and treatment of vaginal candidiasis in pregnant women, depending on the type of fungi of the genus Candida. // Gynecology. v. 05, N 5b, 2003.
4. Instructions for use of the drug Ecofucin ® .
5. Excipient, lactulose.
6. Dikovskiy A.V., Dorozhko O.V., Rudoy B.A. Pharmaceutical composition of antimycotics and prebiotics and a method for the treatment of candidal vaginitis. // International publication WO 2010/039054 A1.
7. Active ingredient, natamycin.
treatment, symptoms, which suppositories and preparations can be used
A woman who is impatiently waiting for the birth of a baby, as a rule, is very attentive to her health. The slightest infection can have a fatal effect on the development of a child. However, there are ailments that pregnant women are particularly susceptible to. One of these diseases is thrush.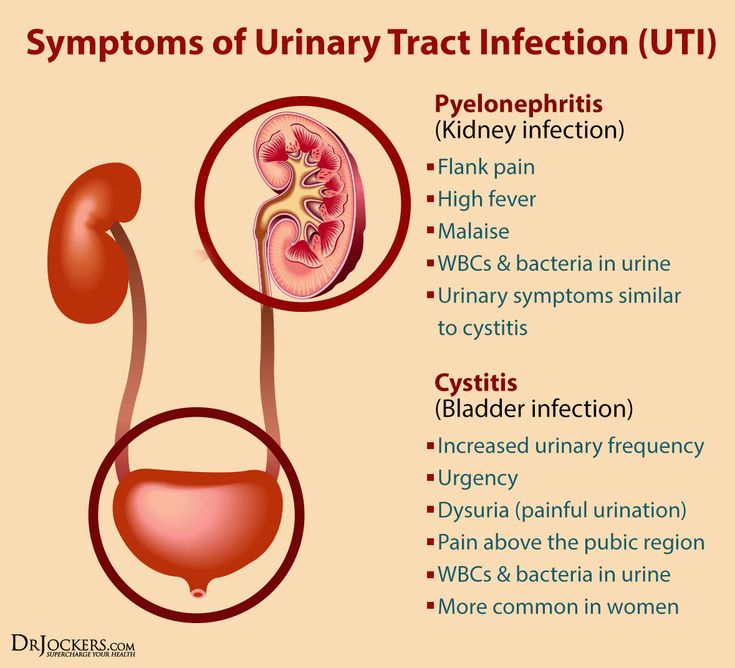
Causes of thrush in pregnancy
Vaginal candidiasis, or thrush, is three times more common in pregnant women than in non-pregnant women. The thing is that the body of the future mother is being rebuilt, the hormonal status is changing, her immunity is decreasing.
Physiological decrease in immunity is an important condition for the possibility of bearing a fetus and the course of pregnancy. Thus, more favorable conditions are created for the reproduction of the fungus of the genus Candida in the body, which cause inflammation. AT 95% of cases the cause lies in the action of Candida albicans.
Additional risk factors for the development of vaginal thrush are the wearing of synthetic underwear, violations of the rules of intimate hygiene.
The growth of own lactobacilli is promoted by lactulose, which is part of the vaginal suppositories of the drug Ecofucin® . Lactulose is a nutrient substrate only for its own lactobacilli, but not for fungi of the genus Candida. Therefore, the use of drug Ecofucin® is not only the treatment of thrush, but also the prevention of its recurrence. Normalization of the vaginal microflora contributes to the physiological course of pregnancy and childbirth, the birth of healthy children, in which the sterile organism is populated with physiological flora. And this creates a reliable and strong immunity in the baby from the first days of life!
Therefore, the use of drug Ecofucin® is not only the treatment of thrush, but also the prevention of its recurrence. Normalization of the vaginal microflora contributes to the physiological course of pregnancy and childbirth, the birth of healthy children, in which the sterile organism is populated with physiological flora. And this creates a reliable and strong immunity in the baby from the first days of life!
This is described in detail in a clinical study that was conducted on the basis of the city clinical hospital №315 named after. O.M. Filatov in Moscow.
More
CONTRAINDICATIONS. CONSULT A SPECIALIST
Symptoms of thrush in pregnancy
Symptoms of candidiasis in pregnancy are no different from symptoms of the same disease at any other time in life. Severe itching, discomfort, burning sensation in the vulva, which increases during intercourse and after urination, are the most common signs of thrush. If abundant curdled discharge is added to them, and sometimes with an unpleasant sour smell, this is a serious reason to consult a doctor.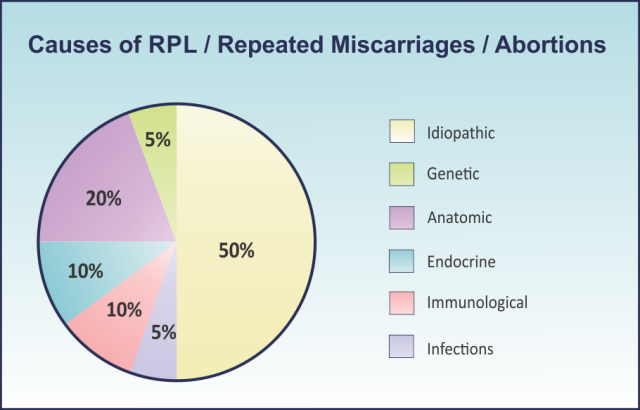
Sometimes thrush is manifested by swelling and redness of the mucous membranes of the external genital organs.
Forms of thrush in pregnant women
In clinical practice, there are several forms of candidiasis in pregnant women. Each of them has its own characteristics.
Carriage. In this case, there are no symptoms, but according to the data of a gynecological smear on the microflora, fungi are detected. If during pregnancy a large number of lactobacilli are found in the microbiome, then this is a reason for careful monitoring by a doctor.
Vulvovaginal candidiasis. It is characterized by a vivid clinical picture: itching, burning, a large amount of curdled discharge with a sour smell. In some cases, there may be swelling of the external genital organs, pain during urination and sexual intercourse.
In addition, thrush during pregnancy can be acute, when the inflammation occurs for the first time, the symptoms are pronounced. In the absence of treatment or the action of other predisposing factors, the acute form can turn into a chronic relapsing one. Outside of exacerbations, there are no symptoms, but with a relapse, the clinical picture is similar to the acute form.
In the absence of treatment or the action of other predisposing factors, the acute form can turn into a chronic relapsing one. Outside of exacerbations, there are no symptoms, but with a relapse, the clinical picture is similar to the acute form.
Persistent thrush. It is characterized by constant symptoms of pathology, although with active treatment there is an improvement in the condition.
Treatment of thrush in pregnancy
Treatment of thrush in pregnancy should be under medical supervision. The use of a number of drugs during the period of bearing a child is prohibited, as they affect the course of pregnancy and the development of the fetus. Many pills that can be used without problems by ordinary women are contraindicated for expectant mothers, but candles carry a much lower risk to the health of the baby.
IMPORTANT
Why women suffering from candidiasis during pregnancy and lactation should consider using Ecofucin® :
✓ allowed from the 1st trimester of pregnancy and during breastfeeding;
✓ natamycin — the active ingredient of the drug Ecofucin ® helps to eliminate the cause of thrush - fungi of the genus Candida;
✓ the preparation contains lactulose, which is a prebiotic that helps to increase the number of lactobacilli and restore the normal microflora of the vagina;
✓ Timely and effective treatment of thrush in pregnancy is especially important.
Read more
CONTRAINDICATIONS. CONSULT A SPECIALIST
Diagnosis
Symptoms of vulvovaginal candidiasis are similar to those of other diseases. Therefore, the diagnosis is aimed at identifying the cause of the symptoms. To do this, the doctor finds out when the symptoms appeared, what preceded them, how long they persist. After the interview, they proceed to the inspection. These data are sufficient to make a preliminary diagnosis, however, to confirm it, it is necessary to conduct laboratory examination methods:
- a gynecological smear for microflora allows to assess the qualitative and quantitative indicators of microflora, to identify possible inflammatory reactions and dysbacteriosis;
- PCR diagnostics allows you to detect fungal DNA in vaginal discharge and make a differential diagnosis, that is, to distinguish one disease from another.
Based on the results of the examination, a treatment plan is drawn up, taking into account the duration of pregnancy and the severity of the problem.
Modern methods of treatment of thrush in pregnant women
Treatment tactics should take into account the physiological characteristics of the body of a pregnant woman and a developing fetus. Systemic drugs, which are often the drugs of choice in the treatment of vulvovaginal candidiasis in women, are prohibited during pregnancy. Therefore, the tactics of treatment also depend on the trimester of pregnancy.
First trimester
The first trimester is very important for the development of a healthy baby. During this period, the choice of means for treatment is especially limited, but this does not mean that taking medications should be delayed.
If you wait to start therapy from the second trimester, there is a risk of getting complications. In the first trimester, natamycin and, accordingly, drugs that have it as the main active ingredient can be used to treat thrush. With the rest of the funds, it is better to wait until the second trimester.
These drugs include Primafungin, Pimafucin, etc.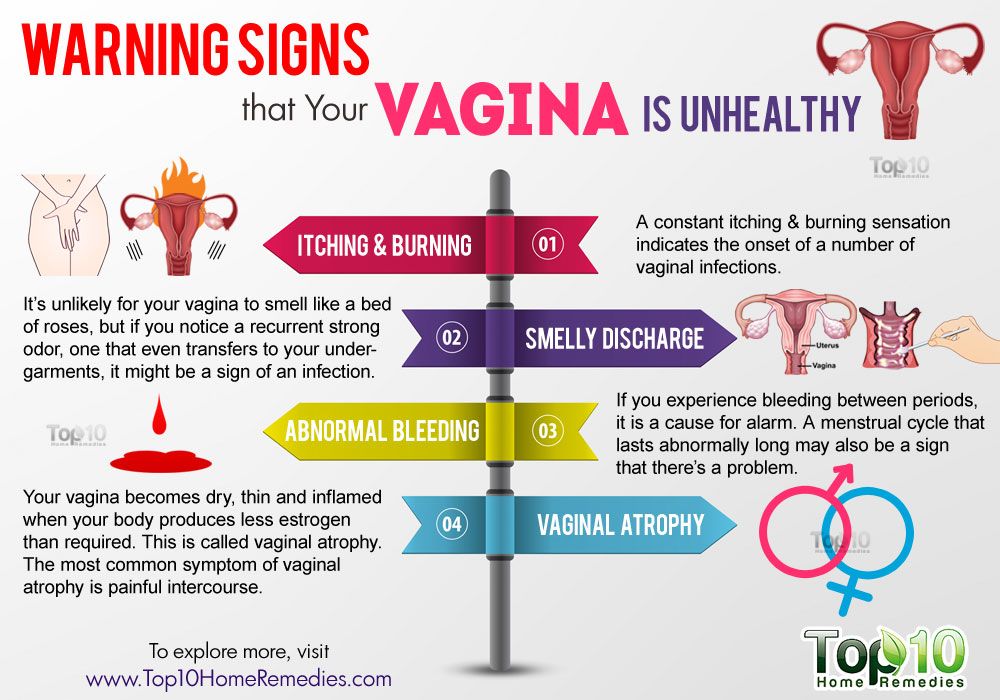
And you should also review your diet, exclude from it sugary foods containing a large amount of carbohydrates, which promote the growth and reproduction of Candida fungi.
IMPORTANT
Natamycin is the main active ingredient in Ecofucin® . Natamycin is practically not absorbed into the blood and does not have a systemic effect, contributing to the safety of use:
✓ has a fungicidal effect - causes the death of the fungus of the genus Candida;
✓ fungi practically do not develop resistance to natamycin.
Prebiotic lactulose, which is part of Ecofucin ® , is actively fermented by the normal microflora of the vagina, stimulating the growth of lactobacilli, and causes the restoration of the microflora of the vagina, stimulating local immunity.
Where to buy
CONTRAINDICATIONS. CONSULT A SPECIALIST
Second trimester
In the second trimester, the gynecologist has to choose drugs for treatment based on the benefit-risk ratio. At such periods, more effective means are allowed, which are based on substances such as clotrimazole, itraconazole and others. Sometimes drugs based on metronidazole are prescribed.
At such periods, more effective means are allowed, which are based on substances such as clotrimazole, itraconazole and others. Sometimes drugs based on metronidazole are prescribed.
In the second trimester, the choice of drugs is much wider, because the protective mechanisms of the fetus have already been formed. The doctor can prescribe Candide B6, Irunin, Primafungin, Pimafucin, etc.
Third trimester
If in the early stages doctors are limited in the choice of pharmacological drugs, then in the later stages the list of drugs is significantly expanded. During this period, it is especially important to get rid of the disease, because infection with Candida fungi from mother to child occurs in 75-80% of cases during childbirth.
After the examination, the doctor may prescribe Sertoconazole, Econazole, Clotrimazole, etc.
Can suppositories be used
then expectant mothers are allowed to use candles. But you should consult a doctor of choice, as some suppositories are allowed in certain trimesters.
It is important to remember that pregnant women should not use suppositories for thrush containing metronidazole or fluconazole as an active ingredient, as well as nystatin, without consulting a doctor.
Natamycin is considered one of the common drugs for the treatment of thrush in pregnant women. It underlies a number of drugs. Its target is the structural elements of fungi, not enzymes, so the formation of drug resistance to it rarely occurs.
Can I use
tabletsMost oral medications are contraindicated during pregnancy. Gynecologists recommend giving preference to local therapy: suppositories, creams and ointments.
Effective folk remedies
For obvious reasons, gynecologists do not advocate the treatment of thrush during pregnancy with folk remedies. Their effectiveness is sometimes questionable, and the risk is great, both for the mother and for the baby.
During pregnancy, thrush is sometimes treated with douching with a decoction of chamomile, calendula, oak bark, St.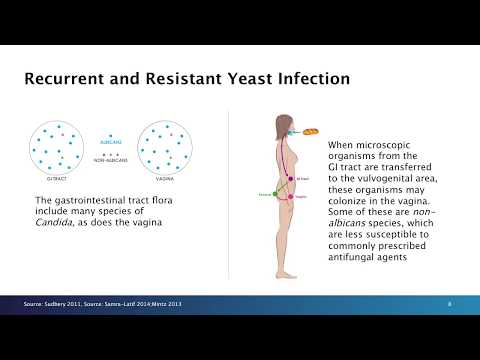 John's wort and sage. But it is worth remembering that they are not safe either. In addition, practice shows that such treatment does not eliminate the fungus that caused the disease and most often aggravates the violation of the vaginal microflora.
John's wort and sage. But it is worth remembering that they are not safe either. In addition, practice shows that such treatment does not eliminate the fungus that caused the disease and most often aggravates the violation of the vaginal microflora.
What is not recommended for use in the treatment
Most pharmacological agents that act on Candida fungi are either contraindicated for pregnant women or have restrictions in use at specific terms of pregnancy. Therefore, it is important to remember that what you used to treat thrush before pregnancy should not be taken out of habit during the period of expectation of the child.
Photo: MART PRODUCTION, pexels.comNutrition for thrush in pregnant women
It is necessary to review the diet. It is recommended to avoid spicy and fried foods, sweet, starchy foods. It is also necessary to exclude foods that contain hidden sugars, such as mayonnaise, ketchup, flavors for cooking first and second courses, etc.
Carbohydrates are an excellent breeding ground for Candida.
Fermented products or those that can cause these processes in the intestines, as well as those containing artificial dyes, are prohibited.
Why is thrush coming back? How to avoid it?
One of the reasons for the development of recurrence of thrush or exacerbation of candidiasis is the situation when the number of lactobacilli is reduced in the vagina, resulting in a state of dysbiosis and this creates excellent conditions for the development of fungi of the genus Candida. When the number of own lactobacilli is restored, the risk of developing a recurrence of thrush is significantly reduced. It is important to increase the number of own lactobacilli, whose genetic structure is not alien. Their growth should be gradual.
Prevention of thrush in pregnant women at home
In addition to the general rules for the prevention of thrush (hygiene, proper nutrition, avoidance of synthetic underwear), pregnant women should regularly visit an obstetrician-gynecologist. In the first trimester, it is recommended to make an appointment once a month, in the second - once every 2-3 weeks, and in the third - once every 7-10 days.
In the first trimester, it is recommended to make an appointment once a month, in the second - once every 2-3 weeks, and in the third - once every 7-10 days.
With constant monitoring in the antenatal clinic during pregnancy and timely correct treatment, if thrush is detected, the risk of passing it on to the unborn baby will be extremely small.
Frequently Asked Questions
Is it possible to use baking soda for thrush in pregnant women?
Baking soda is considered relatively safe and is often used in alternative and even evidence-based medicine. However, it is forbidden to use it during pregnancy. Symptoms of thrush are also characteristic of a number of other diseases that require a completely different treatment.
The use of soda can blur the clinical picture and give false hope of recovery. However, the underlying disease progresses and this leads to complications, sometimes fatal. Self-treatment of thrush during pregnancy is unacceptable.