Breast engorgement pregnancy
Exploring Breast Changes During Pregnancy: The Third Trimester and After Birth
If you are in the last trimester of pregnancy, your breasts will probably be feeling quite large and heavy now!
You will likely notice that everything has become more prominent; your nipples may have started to protrude more - unless you have inverted nipples, in which case you may not notice any difference - the skin of your areola is really quite dark, the veins just underneath your skin are clearly visible (if you have pale skin) and the stretchmarks may be much more noticeable too.
You may find the skin underneath and on top of your breasts become hot and sweaty and possibly even dry and itchy too, this is due to the skin stretching. Make sure you wear a comfortable, cotton and correct fitting bra...
Share this content
What to Expect After Birth
Once your baby and the placenta are born it sets off a hormonal reaction to start the milk-making cells producing mature milk in large quantities. In the first hour your baby will normally find and crawl to the breast themselves to breastfeed. If your baby is not yet able to breastfeed the midwives will help you to express your milk.
Small quantities of colostrum are perfect for your new baby right now. Their tummy is only tiny so they only require little amounts of colostrum at the beginning. Their tummies quickly grow over the next few days though, along with your increasing milk supply.
Over the next 2-5 days, you will notice that your breasts begin to feel much fuller and heavier as the milk ‘comes-in’. The milk inside your cells is changing from colostrum into mature milk and the volume available to your baby grows very quickly.
You may find you wake up one morning and your breasts feel like they have doubled in size! They will likely feel full, firm, and warm, and perhaps tender as milk production increases and colostrum begins to change to mature milk. The term for this change in breast fullness is physiological engorgement.
Some women find that their breasts feel uncomfortable. Other women barely notice any change. Mild to moderate discomfort is common and normal. Usually this situation lasts for about 18 to 24 hours. However, each woman is different, so physiological engorgement may last for longer or shorter periods of time.
Your milk will “come in” whether you breastfeed or not, but continued milk production only occurs if you empty your breasts of the milk regularly via breastfeeding or through expressing.
If you feel your breasts are rock hard and extremely full, a warm shower, some gentle breast massage and expressing a little milk to soften your areola before you feed baby can be helpful to ensure baby can attach and drink from the breast well. If baby is unable to attach on to the breast and feed well then it is a good idea to contact your midwife for support.
The Three Stages of milk: Colostrum, Transitional Milk and Mature Milk
Colostrum: Colostrum looks thick and sticky and varies in colour.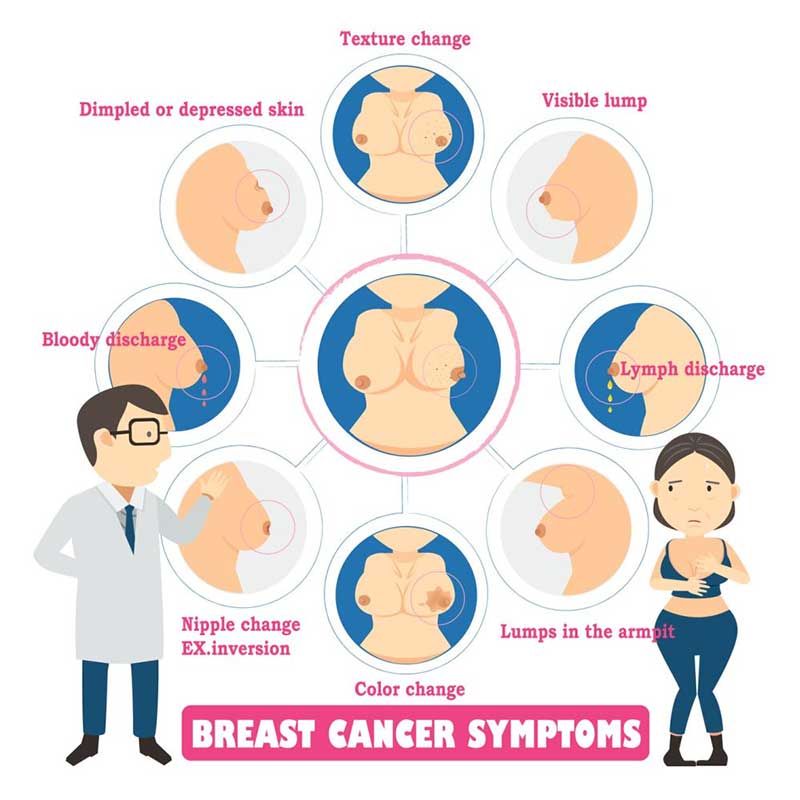 It is highly concentrated, easily digested and contains everything your newborn needs to build a strong immune system. It is available only in very small amounts, which is just right for your baby's tiny stomach.
It is highly concentrated, easily digested and contains everything your newborn needs to build a strong immune system. It is available only in very small amounts, which is just right for your baby's tiny stomach.
Colostrum has a laxative effect, which helps the baby to pass the meconium (the first poo) and helps prevent jaundice by clearing the bilirubin from the gut.
Transitional milk: During the next two weeks, the milk increases in quantity and changes in appearance as well as in composition. The immunoglobulin and protein content decreases, while the fat and sugar content increases.
Mature milk: Mature milk does not look as creamy as cow's milk, your breast milk is meant to look different- often thinner and watery looking, possibly with a cream layer on top. This does not mean it is poor quality milk at all. We are just different from cows! Mature milk contains all the nutrients needed for your baby’s healthy development.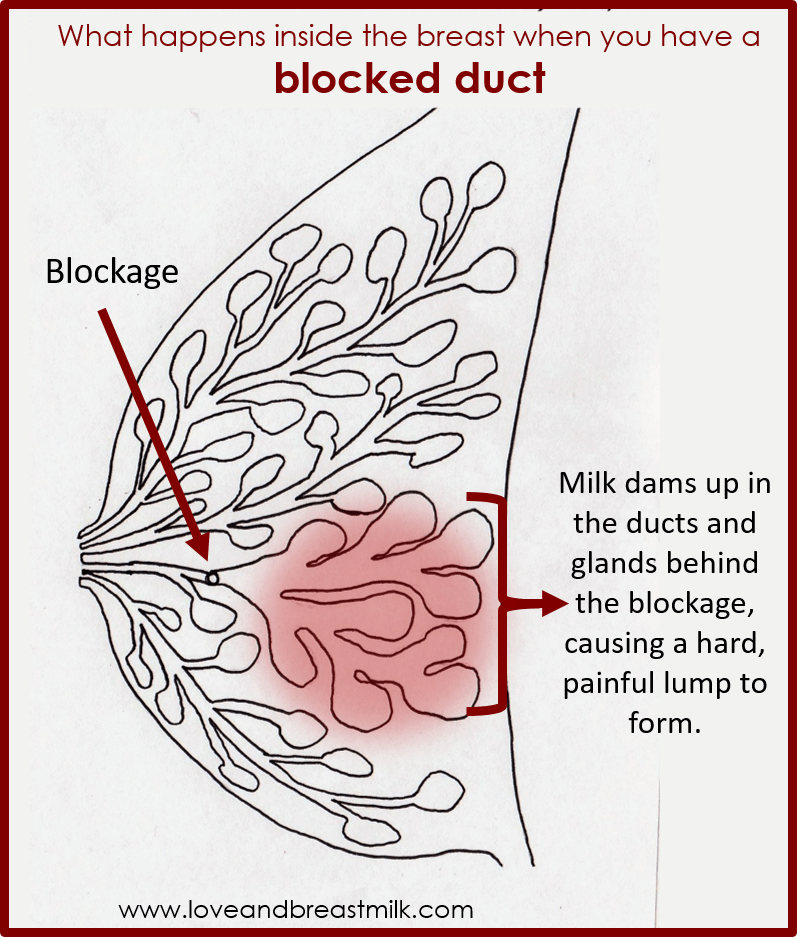 Breast milk is never “too thin.”
Breast milk is never “too thin.”
Mature milk changes over the length of a single feed, as well as over weeks and months, in order to meet your baby’s specific needs. The milk that flows at the beginning of a feed is low in fat and high in lactose, sugar, protein, vitamins, minerals and water. As the feed progresses, the milk changes and contains more fat and less sugar.
What questions do you have about the benefits of breastfeeding? Please join the conversation on the Medela Australia Facebook page.
Breast engorgement | Pregnancy Birth and Baby
Breast engorgement | Pregnancy Birth and Baby beginning of content3-minute read
Listen
What is breast engorgement?
Once your baby is born, your breasts are given a signal to start full milk production. Blood flows to your breasts, and your milk usually comes in 1 to 4 days after the birth. Breast engorgement is when the breast tissue overfills with milk, blood and other fluids and is a common problem in the early days and weeks of breastfeeding.
Blood flows to your breasts, and your milk usually comes in 1 to 4 days after the birth. Breast engorgement is when the breast tissue overfills with milk, blood and other fluids and is a common problem in the early days and weeks of breastfeeding.
What are the symptoms of breast engorgement?
Engorgement can make your breasts feel very full, hard, swollen and painful.
Your nipples can become flat and tight. This can make it difficult for your baby to attach to the breast.
What causes breast engorgement?
Breast engorgement can happen if:
- your baby is not feeding and attaching well and your breasts aren’t drained well during a feed
- you are making more milk than your baby needs
- your baby misses a feed or is feeding infrequently
Breast engorgement can occur at any time you are breastfeeding, especially when your baby’s feeding pattern changes and they feed less.
Engorgement is usually temporary — eventually you will produce just as much milk as your baby needs.
How to prevent breast engorgement
To reduce the chance of breast engorgement:
- Feed your baby often and on demand (not by the clock) from birth, with at least 8 to 12 feeds in the first 24 hours. It helps to sleep in the same room as your baby to keep up the feeds.
- Wake your baby for a feed if your breasts become full and uncomfortable (especially at night time).
- Don’t limit your baby’s time at the breast.
- Avoid giving your baby any fluids other than breastmilk unless needed for a specific medical reason.
- Ensure your baby is positioned and attached correctly, to maximise the amount of milk they are getting.
How to relieve breast engorgement
If your breasts become engorged, there are things you can do to relieve the discomfort.
The best way to is to empty the breast, either by feeding your baby at the breast, or by expressing your milk. It’s okay to wake your baby and offer a breastfeed day or night if your breasts become full and uncomfortable between feeds.
The following tips might also help:
- Apply a warm washer to the breast, or have a warm shower before a feed, for comfort and to help the milk flow.
- Remove your bra before breastfeeding (and leave it off).
- Hand-express a little milk before feeding your baby, or try ‘reverse pressure softening’ (applying pressure around the nipples to push fluid back into the breasts).
- Gently massage the breast in a downward motion from the chest wall toward the nipple while your baby is feeding.
- Use a cold compress, like a cool gel pack from the fridge, or a chilled washed cabbage leaf over the breast to relieve inflammation.
- Express milk after a feed, either by hand or with a breast pump, if your breasts still feel full.
Sometimes, if the engorgement does not improve, a complete ‘pump out’ with an electric pump may be necessary to relieve the milk pressure that is causing increased blood and fluid within the breast tissue (ask your lactation consultant or doctor for help).
If you are still uncomfortable, ask your doctor for appropriate pain relief.
For help with breast engorgement prevention and treatment, contact a health professional, including your doctor, lactation consultant or breastfeeding counsellor, child health nurse, or call Pregnancy Birth and Baby on 1800 882 436.
Sources:
Raising Children Network (Breast milk oversupply and engorgement), Australian Breastfeeding Association (Engorgement), HealthyWA (Engorgement), myDr (Engorgement and mastitis)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: December 2020
Back To Top
Related pages
- Expressing and storing breast milk
- Breastfeeding your baby
Need more information?
Engorgement and mastitis - MyDr.
 com.au
com.au If you experience difficulties with breastfeeding seek the advice of a midwife, lactation consultant, the Australian Breastfeeding Association or your doctor.
Read more on myDr website
Engorgement | Australian Breastfeeding Association
What is engorgement?You may find that your breasts become larger and feel heavy, warmer and uncomfortable when your milk ‘comes in’, usually about 2–6 days after your baby is born. This is normal. It does not affect milk flow or the ability of your baby to attach to your breast.
Read more on Australian Breastfeeding Association website
Breastmilk oversupply & breast engorgement | Raising Children Network
Breastfeeding mums can have breastmilk oversupply and breast engorgement. Check feeding patterns, techniques and positions. Hand-expressing can also help.
Check feeding patterns, techniques and positions. Hand-expressing can also help.
Read more on raisingchildren.net.au website
Breastfeeding
Breastfeeding is learnt over the first weeks and months of your child’s life. It is a unique and special experience for families as no two mothers or babies are the same.
Read more on Karitane website
Blocked ducts | Australian Breastfeeding Association
What are blocked ducts?Ducts carry the milk from deep in the breast to the nipple openings. Sometimes these ducts can become blocked. Milk builds up behind the blockage, a lump forms and your breast begins to feel sore. Your breast may become engorged in one area and might also look red.Occasionally, a mother with a blocked duct may notice a white spot on her nipple too.
Read more on Australian Breastfeeding Association website
Breastfeeding | Sydney Children's Hospitals Network
Breastfeeding is not always easy and you may have trouble breastfeeding your baby
Read more on Sydney Children's Hospitals Network website
Weaning: stopping breastfeeding | Raising Children Network
Whether weaning is led by you or baby, you can make the process of stopping breastfeeding easier if you take it slowly to start with. Get more tips.
Read more on raisingchildren.net.au website
Breastfeeding challenges - Ngala
Many new mothers experience breastfeeding challenges
Read more on Ngala website
Too much milk | Australian Breastfeeding Association
Some mothers make more milk than their babies can easily cope with. This is quite common in the first few weeks of breastfeeding, but for some mothers it can continue for longer.
This is quite common in the first few weeks of breastfeeding, but for some mothers it can continue for longer.
Read more on Australian Breastfeeding Association website
Breastfeeding your baby
Breastfeeding is the most natural way to feed your baby, providing all the nutrition your baby needs during the first six months of life and a loving bond with your baby.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.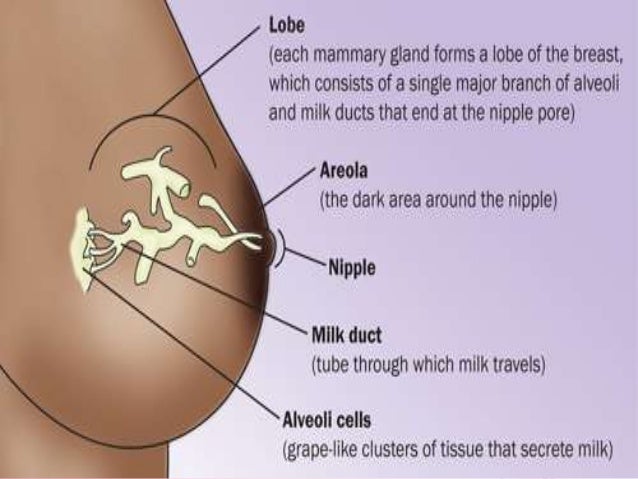
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Breast changes from the beginning of pregnancy to the end of breastfeeding
Medela's experts explain the changes that occur in the breast from the beginning of pregnancy to the end of breastfeeding, as well as tips for taking care of your breasts throughout this period.
Share this information
From the moment of conception, your body begins to prepare for the birth of your baby. This applies not only to the uterus - the anatomy of the breast also changes radically. This article will tell you what to expect in each trimester, during and after breastfeeding.
This applies not only to the uterus - the anatomy of the breast also changes radically. This article will tell you what to expect in each trimester, during and after breastfeeding.
First trimester breast changes
Early in pregnancy, many women notice changes in their breasts. Moreover, often they become the first signs of pregnancy. Fluctuations in hormone levels and changes in the structure of the mammary glands can cause increased sensitivity and soreness of the nipples and breasts as early as the third or fourth week. For some pregnant women, breast tenderness persists until childbirth, but for most it goes away after the first trimester.
“Sometimes during pregnancy, breasts grow very quickly in the first weeks, and sometimes their size increases gradually,” says Dr. Jacqueline Kent, a leading lactation specialist at the University of Western Australia. “All women are different. For some, breast size may not change much until childbirth or even after them. In general, we can say that by the time the milk arrives, the breast will most likely become one and a half times larger than before pregnancy! 1
In general, we can say that by the time the milk arrives, the breast will most likely become one and a half times larger than before pregnancy! 1
As soon as your regular bras start to feel tight (usually around 12 weeks), it's time to buy a maternity bra. The most comfortable, according to many women, are seamless models with wide straps made of soft, breathable fabric. It is best to avoid underwired bras as they can put pressure on the developing milk ducts.
It is important to take your measurements correctly in order to find the right bra with a good fit. Take measurements every couple of months, as you may need a different size bra as your baby grows and your breasts get bigger.
Breast changes in the second trimester
From about the 15th week of pregnancy, newly formed cells that produce milk are activated in the breast, and by about the 22nd week, production begins. 1 But don't worry - most of this milk will be absorbed by the body without going out, as pregnancy hormones prevent it from being overproduced or excreted.
“During the second trimester, you may notice that the nipples and areolas (the areas of skin around the nipples) become darker and larger,” says Dr. Daniel Prime, Medical Research Associate at Medela. tubercles - the so-called glands of Montgomery. They secrete oil that moisturizes the nipples and will protect them from inflammation and infection when you start to feed. Scientists believe that the smell of this fat is similar to the smell of amniotic fluid and helps the newborn baby find the nipple.” 2
Do not use harsh soap for breast hygiene and do not rub hard with a towel as this can damage this natural lubricant. Just wash your breasts with warm water and pat dry. And if someone tells you to pinch or rub your nipples to prepare them for breastfeeding, don't listen to them!
If you have flat or inverted nipples, your pregnancy is over 32 weeks, and your pregnancy is normal, you can try inserting special nipple formers* into your bra in consultation with your doctor. They help to gently pull out the nipples so that it is easier for the newborn to grasp them. Consult your healthcare professional or read our article on flat and inverted nipples to learn more.
They help to gently pull out the nipples so that it is easier for the newborn to grasp them. Consult your healthcare professional or read our article on flat and inverted nipples to learn more.
If breast size increases dramatically during pregnancy, breast skin may itch and stretch marks may appear on it. A good moisturizer can help soothe itching. The appearance of stretch marks usually depends on genetics and skin type. If you have a predisposition to stretch marks, it is unlikely that you will be able to prevent them, but, fortunately, over time they will become lighter and less noticeable.
Breast changes in the third trimester
In the last trimester, you may again experience soreness and heaviness in your chest. A sleep bra will keep you comfortable at night, while a supportive sports bra will help you avoid soreness and ligament damage during exercise.
Don't forget to buy a pair of nursing bras one month before your baby is born. If possible, consult a specialist in the store or study the online guide to select the appropriate model and size. Every woman is different, but usually cups of a nursing bra are chosen one or two sizes larger than before pregnancy. The underbust girth may also increase as the ribcage expands to provide enough room for the baby. The sales assistant should choose the size of your bra, taking into account the appearance of milk after childbirth. Models with fasteners that can be unfastened with one hand make it easier to attach the baby to the breast.
Every woman is different, but usually cups of a nursing bra are chosen one or two sizes larger than before pregnancy. The underbust girth may also increase as the ribcage expands to provide enough room for the baby. The sales assistant should choose the size of your bra, taking into account the appearance of milk after childbirth. Models with fasteners that can be unfastened with one hand make it easier to attach the baby to the breast.
Surprising but true: milk appears in the breast even before the baby is born. This is why your nipples may start to produce some colostrum (the first breast milk), which will be quite thick and sticky. Sometimes this happens as early as 14 weeks, but more often it still happens in late pregnancy. To avoid the appearance of stains and smudges on clothes, you can use special bra pads.
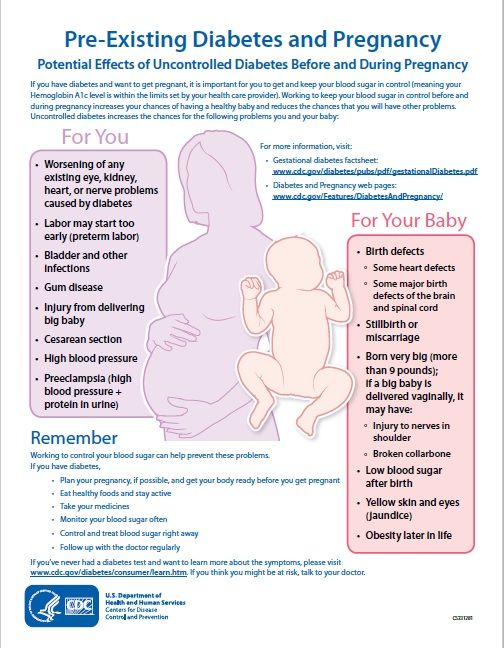
“If you have diabetes or have been diagnosed with gestational diabetes, your doctor may tell you to express some colostrum by hand and freeze it. A recent study showed that after the 36th week it is quite safe if the pregnancy does not have other complications, 3 , says Dr. Prime, “Storing colostrum can come in very handy because babies with diabetic mothers are at higher risk of hypoglycemia (low blood sugar) and frequent colostrum feeding is the best remedy. . However, be prepared for the fact that there will be very little colostrum. You may only be able to express a few drops at first, and that’s perfectly fine.”
Prime, “Storing colostrum can come in very handy because babies with diabetic mothers are at higher risk of hypoglycemia (low blood sugar) and frequent colostrum feeding is the best remedy. . However, be prepared for the fact that there will be very little colostrum. You may only be able to express a few drops at first, and that’s perfectly fine.”
What happens to the breast after childbirth
Approximately two to four days after the baby is born (sometimes later if there was a caesarean section or a traumatic delivery), you will feel your breasts becoming heavier and firmer - this means that the milk has come. 4
“This breast fullness is not only due to excessive milk production – there is also an increase in the amount of blood circulating around the breast and the volume of lymphatic fluid,” explains Dr. Prime, “All this is the result of a gradual decrease in pregnancy hormone levels that began after the birth of a child and which allows the hormones responsible for the production of milk to enter into work.
During this period, you may experience soreness and discomfort in your breasts, a condition called breast swelling. This is quite common and usually resolves after a few days, during which time breastfeeding must continue. Read on for our tips on how to relieve swelling and discomfort, and if the problem persists, see a lactation consultant or healthcare provider.
What happens to the breast during lactation
For about the first three months of breastfeeding, your breasts are likely to fill up a lot before feeding. Over time, you may notice that your breasts become less full, but this does not mean at all that your milk production has decreased. If you are breastfeeding your baby exclusively and on demand, and at the same time he is growing well, then everything is in order with the amount of milk.
“Be prepared for the fact that after six months of breastfeeding, your breast size will begin to decrease,” Dr. Kent explains, “This is not a sign that your body is producing less milk.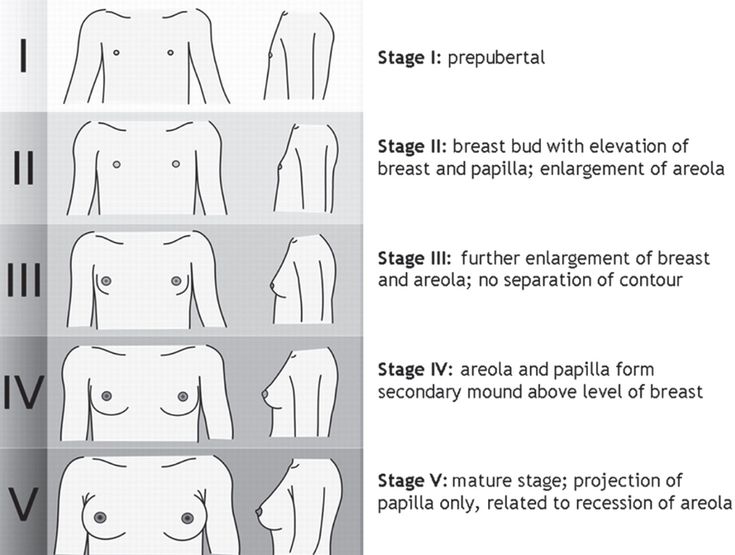 Most likely, the amount of adipose tissue in the breast simply decreased. By the time your baby is 15 months old, your breasts may be back to their pre-pregnancy size, but not smaller. However, whether you continue breastfeeding or not, you may still produce 100 to 300 ml of milk per day.”
Most likely, the amount of adipose tissue in the breast simply decreased. By the time your baby is 15 months old, your breasts may be back to their pre-pregnancy size, but not smaller. However, whether you continue breastfeeding or not, you may still produce 100 to 300 ml of milk per day.”
This may be due to the start of more efficient milk production after six months of breastfeeding, which, according to Dr. Kent's research, may be the result of redistribution of breast tissue. 5
How your breasts change after you stop breastfeeding
When you finally stop breastfeeding—be it after three weeks, three months, or three years—the breast changes associated with lactation disappear. “After the complete cessation of breastfeeding, the breasts, as a rule, return to the size that they were before pregnancy. This usually happens in about three months, and for someone else while breastfeeding,” Dr. Kent explains, “If you get pregnant again, the whole process starts all over again. ”
”
Literature
1 Cox DB et al. Breast growth and the urinary excretion of lactose during human pregnancy and early lactation: endocrine relationship. Exp Physiol . 1999;84(2):421-434. - Cox D.B. et al., "Breast growth and urinary lactose excretion during pregnancy and lactation: an endocrine relationship." Exp Physiol. 1999;84(2):421-434.
2 Doucet S et al. The secretion of areolar (Montgomery’s) glands from lactating women elicits selective, unconditional responses in neonates.PLoS One . 2009;4(10): e 7579. - Doucet S. et al., "Papillary gland secretion (Montgomery's glands) in lactating women induces a selective unconditioned response in the newborn." PLOS One. 2009;4(10):e7579.
3 Forster DA et al. Advising women with diabetes in pregnancy to express breastmilk in late pregnancy (Diabetes and Antenatal Milk Expressing [DAME]): a multicentre, unblinded, randomized controlled trial. Lancet. 2017;389(10085):2204-2213. - Forster D.A. et al., "Women with Gestational Diabetes are Recommended to Express Milk Late in Pregnancy (Diabetes and Antenatal Pumping [ DAME ]): A Multicenter, Open, Randomized, Controlled Trial. Lancet (Lancet). 2017;389(10085):2204- 2213.
Lancet. 2017;389(10085):2204-2213. - Forster D.A. et al., "Women with Gestational Diabetes are Recommended to Express Milk Late in Pregnancy (Diabetes and Antenatal Pumping [ DAME ]): A Multicenter, Open, Randomized, Controlled Trial. Lancet (Lancet). 2017;389(10085):2204- 2213.
4 Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals, Geneva : World Health Organization ; 2009. AVAILABLE FROM : https://www.ncbi.nlm.nih.gov/NBKS/NBK148965/ - "POSTICION" POSTICION "POSTRISS" POSTRIMENT "POST textbook for students of medical and related professions. Geneva: World Health Organization, 2009. Article cited: https://www.ncbi.nlm.nih.gov/books/NBK148965/
5 Kent JC et al. Breast volume and milk production during extended lactation in women. Exp Physiol. 1999;84(2):435-447. - Kent J.S. et al., "Amount and production of breast milk during long-term lactation in women". Ex Physiol. 1999;84(2):435-447.
Breast volume and milk production during extended lactation in women. Exp Physiol. 1999;84(2):435-447. - Kent J.S. et al., "Amount and production of breast milk during long-term lactation in women". Ex Physiol. 1999;84(2):435-447.
Read instructions before use. Consult a specialist about possible contraindications.
* RU № ФСЗ 2010/07352 of 07/19/2010
Breast changes during pregnancy
If you think that breasts grow only in youth, you are wrong! The complex internal structures needed to feed a baby only begin to form during pregnancy, and until recently we didn't even know how it happened.
Share this information
Did you think about your breasts during pregnancy? Surely only in the context of buying a special bra. Meanwhile, at this time, huge changes take place in the chest. Not only the uterus, but also the breast undergoes an amazing transformation to prepare for the birth of the baby. But to understand, let's go back a little...
But to understand, let's go back a little...
Breast development during adolescence
The breast changes continuously from adolescence until menopause. Unlike other organs, it does not grow until it is "activated" by hormones produced during puberty. However, even when the breast appears to be fully developed, it is not yet mature.
“After the completion of puberty, the female breast continues to develop. With each cycle, the amount of secretory [milk-producing] tissue increases slightly, and this continues until about 35 years old,” says Professor Peter Hartmann from the University of Western Australia, an expert in lactation, “After reaching this age, breast development stops, it becomes mature , but remains "sleeping" for the time being.
During the menstrual cycle, the cells of the breasts are renewed, which can make them more sensitive, painful or swollen. 1
You may have noticed that at the beginning of the cycle, the breasts are somewhat lumpy to the touch. During this period, preparation for a possible pregnancy takes place. If pregnancy does not occur, a new cycle of falling and rising hormone levels begins. 2
During this period, preparation for a possible pregnancy takes place. If pregnancy does not occur, a new cycle of falling and rising hormone levels begins. 2
Internal breast changes during pregnancy
When conception occurs, the cycle is interrupted. From the end of the first month of pregnancy, the breast begins to gradually turn into a milk-producing organ.
At this time, the number and branching of the milk ducts increase and an extremely complex feeding system is formed. At the same time, cells called lactocytes begin to develop in the breast, which produce milk. The amount of blood going to the breast doubles during pregnancy. That is why the veins sometimes shine through the skin. 3
"After the birth of the placenta, the level of progesterone begins to fall and the process of lactation starts"
“When pregnancy occurs, the breast literally turns on,” says Professor Hartmann. “After conception, the secretory tissue of the breast begins to grow. There are clusters of tubercle-like glands in the breasts, and when pregnancy occurs, these tubercles begin to grow and form ducts and tiny sacs, called alveoli, that will store the milk.”
There are clusters of tubercle-like glands in the breasts, and when pregnancy occurs, these tubercles begin to grow and form ducts and tiny sacs, called alveoli, that will store the milk.”
All of these processes in the breast can cause sensations of heaviness, soreness and swelling, which are early signs of pregnancy. Read more in the article about how breasts change during pregnancy.
Structure of the lactating breast
Believe it or not, scientists have only recently discovered how the complex system of ducts located in the breast works.
Until the beginning of this century, most medical knowledge about milk production was based on experiments conducted by the English surgeon, Sir Astley Cooper, in the 1840s. 4 He concluded that milk is stored in the ducts and exits through 15 to 20 orifices in the nipple. Professor Hartmann's colleague, Dr. Donna Geddes, along with a team of scientists backed by Medela, discovered that breasts function very differently.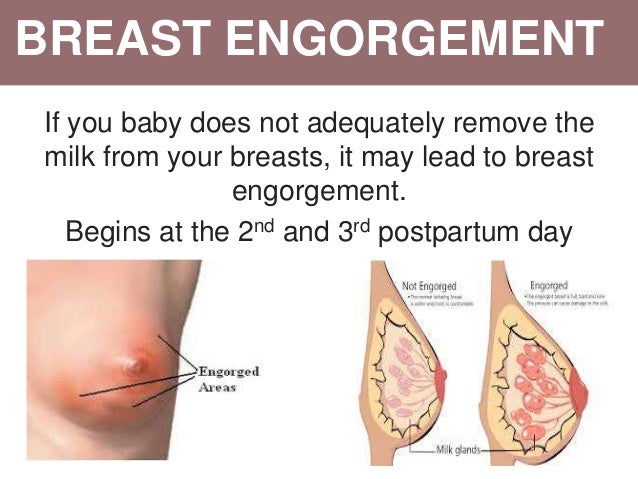 5 The ducts are indeed small tubes only a few millimeters in diameter, but they serve to transport the milk, not to store it. Milk is produced and stored in the alveoli. These sacs are connected to the ducts by even smaller tubes called tubules. 6
5 The ducts are indeed small tubes only a few millimeters in diameter, but they serve to transport the milk, not to store it. Milk is produced and stored in the alveoli. These sacs are connected to the ducts by even smaller tubes called tubules. 6
The milk stays in these sacs until the hormone oxytocin is produced in the body, which happens when the baby starts suckling. The alveoli are surrounded by muscle cells that contract under the influence of oxytocin, and these contractions move the milk through the ducts to the nipple. This process is called the milk flush reflex. Sometimes it can be felt as a tingling or slight movement that occurs in the breast when you start to feed the baby, but some women do not feel it at all. 7
Dr. Geddes and colleagues also found that there are fewer holes in the nipples than previously thought: usually around nine, sometimes as few as four. The ducts have to expand by almost 68% to accommodate the entire volume of milk flowing rapidly to these several outlets.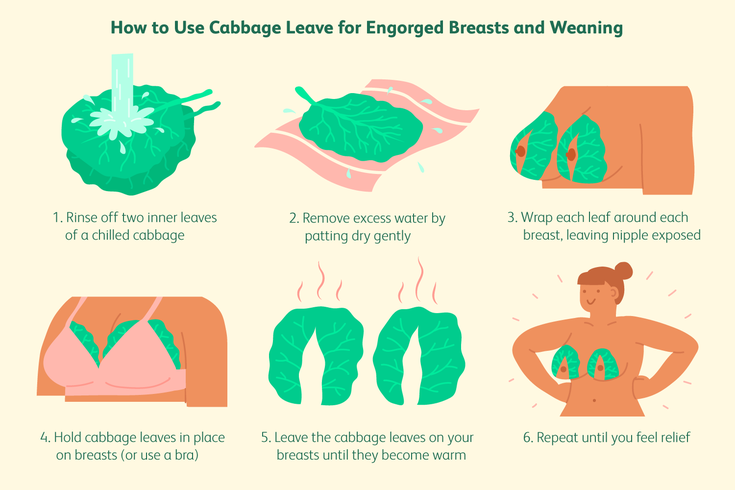 8
8
“Throughout breastfeeding, the structure and function of the breasts remain virtually unchanged until the baby begins to consume less milk,” explains Prof. Hartmann.
The breast begins to produce milk during pregnancy
From about the middle of pregnancy, the alveoli are already capable of producing milk. Fortunately, pregnancy hormones limit the production, 9 otherwise, by the time of delivery, the breast would simply burst.
“Producing 800 ml of milk a day during pregnancy is absolutely useless,” notes Professor Hartmann. “Therefore, the level of progesterone in the body rises, which prevents the activation of production. However, after the birth of the placenta, the level of progesterone begins to fall rapidly and the process of lactation starts.”
What happens to your breasts when you stop breastfeeding? She goes into a state of rest, but not immediately. “When a woman completely stops breastfeeding, it takes some more time – usually a month or two – for milk production to completely stop,” explains Professor Hartmann, “In humans, the process of stopping milk production takes a long time, although in other mammals this happens pretty fast. "
"
The breasts eventually return to their pre-pregnancy state. If you become pregnant again, the same cycle of growth and development will begin all over again. 1
Would you like to know more? Download the free e-book Surprising Breast Milk Facts or read our article Why Colostrum Is So Important?.
Literature
1 Hassiotou F, Geddes D. Anatomy of the human mammary gland: Current status of knowledge. Clin Anat . 2013;26(1):29-48. - Hassiot F., Geddes D., "The structure of the female breast: what we know today." Wedge Anat. (Clinical Anatomy) 2013;26(1):29-48. 2 Reed BG, Carr BR. The normal menstrual cycle and the control of ovulation. In: De Groot LJ et al., editors. Endotext [Internet]. South Dartmouth, MA, USA: MDText.com, Inc.; 2000. [ cited 2018 April 13] Available from : https://www. 3 Geddes DT. Ultrasound imaging of the lactating breast: methodology and application. Int Breastfeed J . 2009;4(1):4. - Geddes D.T., "Lactating Breast Ultrasound: Methodology and Application". Int Brestfeed J. 2009;4(1):4. 4 Cooper AP . On the anatomy of the breast. London: Harrison and Co; 1840. 193 p . - A.P. Cooper, "On the structure of the breast. 5 Ramsay DT et al. Anatomy of the lactating human breast redefined with ultrasound imaging. J Anat . 2005;206(6):525-534. - Ramsey D.T. and co-authors, "The structure of the lactating female breast: a new look through ultrasound." F Anat. 2005;206(6):525-534. 6 Geddes DT. Inside the lactating breast: the latest anatomy research. J Midwifery Womens Health. 2007;52(6):556-563. — Geddes D.T., "Lactating Breasts" by J Midwifery Women's Health. 2007;52(6):556-563. 7 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Hum Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Various Types of Electric Breast Pump Stimulation.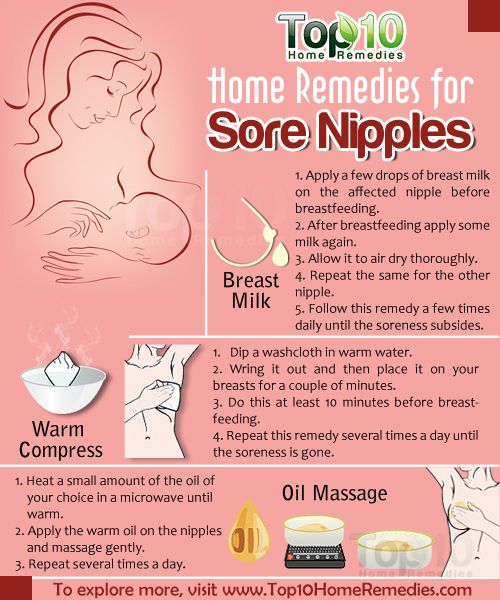 ncbi.nlm.nih.gov/books/NBK279054/. - Reid BJ, Carr BR, "Normal menstrual cycle and ovulation control". In De Groot L.J. et al. (ed.) Endotext [Internet]. South Dartmouth, Massachusetts, USA: MD Text . com , Inc ; 2000. [cited April 13, 2018] Article reference: https://www.ncbi.nlm.nih.gov/books/NBK279054/
ncbi.nlm.nih.gov/books/NBK279054/. - Reid BJ, Carr BR, "Normal menstrual cycle and ovulation control". In De Groot L.J. et al. (ed.) Endotext [Internet]. South Dartmouth, Massachusetts, USA: MD Text . com , Inc ; 2000. [cited April 13, 2018] Article reference: https://www.ncbi.nlm.nih.gov/books/NBK279054/  " London Publishing House Harrison and Co .; 1840. p. 193.
" London Publishing House Harrison and Co .; 1840. p. 193.