Raynaud's syndrome breastfeeding
Raynaud's phenomenon of the nipple: a treatable cause of painful breastfeeding
Case Reports
. 2004 Apr;113(4):e360-4.
doi: 10.1542/peds.113.4.e360.
Jane E Anderson 1 , Nancy Held, Kara Wright
Affiliations
Affiliation
- 1 Department of Pediatrics, University of California, San Francisco, California 94115, USA. [email protected]
- PMID: 15060268
- DOI: 10.1542/peds.113.4.e360
Case Reports
Jane E Anderson et al. Pediatrics. 2004 Apr.
. 2004 Apr;113(4):e360-4.
doi: 10.1542/peds.113.4.e360.
Authors
Jane E Anderson 1 , Nancy Held, Kara Wright
Affiliation
- 1 Department of Pediatrics, University of California, San Francisco, California 94115, USA. [email protected]
- PMID: 15060268
- DOI: 10.1542/peds.113.4.e360
Abstract
Maurice Raynaud first described the vasospasm of arterioles in 1862, and Raynaud's phenomenon is now felt to be common, affecting up to 20% of women of childbearing age. Raynaud's phenomenon has been reported to affect the nipples of breastfeeding mothers and is recognized by many lactation experts as a treatable cause of painful breastfeeding. In 1997, Lawlor-Smith and Lawlor-Smith reported 5 women with Raynaud's phenomenon associated with breastfeeding, but there are few other case reports, and none report the possible relationship between Raynaud's phenomenon of the nipple and previous breast surgery. We report 12 women who breastfed 14 infants, all of whom were seen in 1 pediatric practice and 1 lactation consultation center in San Francisco, California, within the past 3 years. Of the 12 women, 11 were seen between June 2002 and May 2003. All women suffered from extremely painful breastfeeding, with symptoms precipitated by cold temperatures and associated with blanching of the nipple followed by cyanosis and/or erythema. Poor positioning and poor attachment or latch may cause blanching of the nipple and pain during breastfeeding, but 10 of the 12 mothers were evaluated by experienced lactation consultations, who were sure that inappropriate breastfeeding techniques were not contributing factors.
Raynaud's phenomenon has been reported to affect the nipples of breastfeeding mothers and is recognized by many lactation experts as a treatable cause of painful breastfeeding. In 1997, Lawlor-Smith and Lawlor-Smith reported 5 women with Raynaud's phenomenon associated with breastfeeding, but there are few other case reports, and none report the possible relationship between Raynaud's phenomenon of the nipple and previous breast surgery. We report 12 women who breastfed 14 infants, all of whom were seen in 1 pediatric practice and 1 lactation consultation center in San Francisco, California, within the past 3 years. Of the 12 women, 11 were seen between June 2002 and May 2003. All women suffered from extremely painful breastfeeding, with symptoms precipitated by cold temperatures and associated with blanching of the nipple followed by cyanosis and/or erythema. Poor positioning and poor attachment or latch may cause blanching of the nipple and pain during breastfeeding, but 10 of the 12 mothers were evaluated by experienced lactation consultations, who were sure that inappropriate breastfeeding techniques were not contributing factors. Because the breast pain associated with Raynaud's phenomenon is so severe and throbbing, it is often mistaken for Candida albicans infection. It is not unusual for mothers who have Raynaud's phenomenon of the nipple to be treated inappropriately and often repeatedly for C albicans infections with topical or systemic antifungal agents. Eight of our 12 mothers and their infants received multiple courses of antifungal therapy without relief before the diagnosis was made. To diagnose Raynaud's phenomenon accurately, additional symptoms such as precipitation by cold stimulus, occurrence of symptoms during pregnancy or when not breastfeeding, and biphasic or triphasic color changes must be present. All our mothers experienced precipitation of symptoms by cold stimuli and demonstrated biphasic or triphasic color changes, and 6 of the 12 experienced symptoms during pregnancy. Interestingly 3 of 12 mothers also reported a history of breast surgery, including 1 mother who had a fibroadenoma removed and 2 who had breast-reduction surgery.
Because the breast pain associated with Raynaud's phenomenon is so severe and throbbing, it is often mistaken for Candida albicans infection. It is not unusual for mothers who have Raynaud's phenomenon of the nipple to be treated inappropriately and often repeatedly for C albicans infections with topical or systemic antifungal agents. Eight of our 12 mothers and their infants received multiple courses of antifungal therapy without relief before the diagnosis was made. To diagnose Raynaud's phenomenon accurately, additional symptoms such as precipitation by cold stimulus, occurrence of symptoms during pregnancy or when not breastfeeding, and biphasic or triphasic color changes must be present. All our mothers experienced precipitation of symptoms by cold stimuli and demonstrated biphasic or triphasic color changes, and 6 of the 12 experienced symptoms during pregnancy. Interestingly 3 of 12 mothers also reported a history of breast surgery, including 1 mother who had a fibroadenoma removed and 2 who had breast-reduction surgery.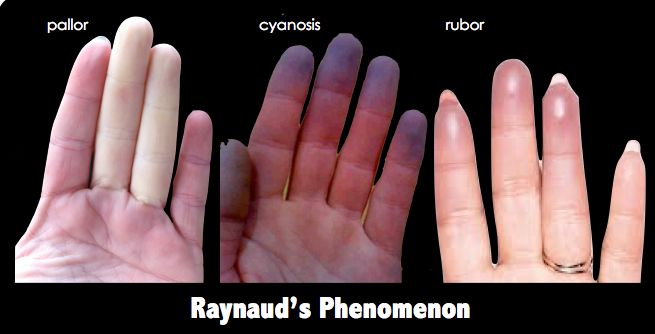 The association between breast surgery/implants and autoimmune disease, including Raynaud's phenomenon, has been discussed extensively, but the association of Raynaud's phenomenon of the nipple during breastfeeding has not been reported previously. Given the small numbers in the study, it is uncertain as to whether this may be a precipitating factor in developing Raynaud's phenomenon. Treatment options include methods to prevent or decrease cold exposure, avoidance of vasoconstrictive drugs/nicotine that could precipitate symptoms, and pharmacologic measures. There are reports in the lay press of the use of herbal medicines, aerobic exercise, and dietary supplements, but because most women with painful breastfeeding require immediate relief of the pain to continue breastfeeding successfully, it is important to offer a treatment plan that will alleviate the pain quickly. Nifedipine, a calcium channel blocker, has been used to treat Raynaud's phenomenon because of its vasodilatory effects.
The association between breast surgery/implants and autoimmune disease, including Raynaud's phenomenon, has been discussed extensively, but the association of Raynaud's phenomenon of the nipple during breastfeeding has not been reported previously. Given the small numbers in the study, it is uncertain as to whether this may be a precipitating factor in developing Raynaud's phenomenon. Treatment options include methods to prevent or decrease cold exposure, avoidance of vasoconstrictive drugs/nicotine that could precipitate symptoms, and pharmacologic measures. There are reports in the lay press of the use of herbal medicines, aerobic exercise, and dietary supplements, but because most women with painful breastfeeding require immediate relief of the pain to continue breastfeeding successfully, it is important to offer a treatment plan that will alleviate the pain quickly. Nifedipine, a calcium channel blocker, has been used to treat Raynaud's phenomenon because of its vasodilatory effects. Very little of the medication can be demonstrated in breast milk and thus is safe to use in breastfeeding mothers. Of the 12 mothers in our series, 6 chose to use nifedipine, and all had prompt relief of pain. Only 1 mother developed side effects from nifedipine. Pediatricians and lactation consultants should be aware of this treatable cause of painful breastfeeding and should specifically question their patients, because most mothers will not provide this information to the breastfeeding consultant. Prompt treatment will allow mothers to continue to breastfeed pain free while avoiding unnecessary antifungal therapy.
Very little of the medication can be demonstrated in breast milk and thus is safe to use in breastfeeding mothers. Of the 12 mothers in our series, 6 chose to use nifedipine, and all had prompt relief of pain. Only 1 mother developed side effects from nifedipine. Pediatricians and lactation consultants should be aware of this treatable cause of painful breastfeeding and should specifically question their patients, because most mothers will not provide this information to the breastfeeding consultant. Prompt treatment will allow mothers to continue to breastfeed pain free while avoiding unnecessary antifungal therapy.
Similar articles
-
Raynaud's phenomenon of the nipple.
Wu M, Chason R, Wong M. Wu M, et al. Obstet Gynecol. 2012 Feb;119(2 Pt 2):447-449. doi: 10.1097/AOG.0b013e31822c9a73. Obstet Gynecol. 2012. PMID: 22270434
-
[Raynaud's phenomenon of the papilla mammae caused by breastfeeding].

Laursen JB, Rørbye C. Laursen JB, et al. Ugeskr Laeger. 2015 Jan 26;177(2A):18-9. Ugeskr Laeger. 2015. PMID: 25612948 Danish.
-
Raynaud phenomenon of the nipple in breastfeeding mothers: an underdiagnosed cause of nipple pain.
Barrett ME, Heller MM, Stone HF, Murase JE. Barrett ME, et al. JAMA Dermatol. 2013 Mar;149(3):300-6. doi: 10.1001/jamadermatol.2013.1560. JAMA Dermatol. 2013. PMID: 23682366
-
Interventions for treating painful nipples among breastfeeding women.
Dennis CL, Jackson K, Watson J. Dennis CL, et al. Cochrane Database Syst Rev. 2014 Dec 15;(12):CD007366. doi: 10.1002/14651858.CD007366.pub2. Cochrane Database Syst Rev. 2014. PMID: 25506813 Review.
-
Drug Treatment of Raynaud's Phenomenon of the Nipple.
Anderson PO. Anderson PO. Breastfeed Med. 2020 Nov;15(11):686-688. doi: 10.1089/bfm.2020.0198. Epub 2020 Jul 17. Breastfeed Med. 2020. PMID: 32700966 Review. No abstract available.
See all similar articles
Cited by
-
Re-thinking lactation-related nipple pain and damage.
Douglas P. Douglas P. Womens Health (Lond). 2022 Jan-Dec;18:17455057221087865. doi: 10.1177/17455057221087865. Womens Health (Lond). 2022. PMID: 35343816 Free PMC article. Review.
-
Raynaud's Phenomenon: Reviewing the Pathophysiology and Management Strategies.

Nawaz I, Nawaz Y, Nawaz E, Manan MR, Mahmood A. Nawaz I, et al. Cureus. 2022 Jan 28;14(1):e21681. doi: 10.7759/cureus.21681. eCollection 2022 Jan. Cureus. 2022. PMID: 35242466 Free PMC article. Review.
-
Exosomes in Systemic Sclerosis: Messengers Between Immune, Vascular and Fibrotic Components?
Colletti M, Galardi A, De Santis M, Guidelli GM, Di Giannatale A, Di Luigi L, Antinozzi C. Colletti M, et al. Int J Mol Sci. 2019 Sep 4;20(18):4337. doi: 10.3390/ijms20184337. Int J Mol Sci. 2019. PMID: 31487964 Free PMC article. Review.
-
Raynaud's phenomenon of the nipple as a side-effect of labetalol: Case report and literature review.
Avila-Vega J, Urrea-Mendoza E, Lee C. Avila-Vega J, et al.
 Case Rep Womens Health. 2019 Jul 24;23:e00135. doi: 10.1016/j.crwh.2019.e00135. eCollection 2019 Jul. Case Rep Womens Health. 2019. PMID: 31388502 Free PMC article.
Case Rep Womens Health. 2019 Jul 24;23:e00135. doi: 10.1016/j.crwh.2019.e00135. eCollection 2019 Jul. Case Rep Womens Health. 2019. PMID: 31388502 Free PMC article. -
Raynaud's Phenomenon: A Brief Review of the Underlying Mechanisms.
Fardoun MM, Nassif J, Issa K, Baydoun E, Eid AH. Fardoun MM, et al. Front Pharmacol. 2016 Nov 16;7:438. doi: 10.3389/fphar.2016.00438. eCollection 2016. Front Pharmacol. 2016. PMID: 27899893 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Raynaud’s Phenomenon in Breastfeeding Mothers
This information can also be viewed as a PDF by clicking here.
The information provided is taken from various reference sources. It is provided as a guideline. No responsibility can be taken by the author or the Breastfeeding Network for the way in which the information is used. Clinical decisions remain the responsibility of medical and breastfeeding practitioners. The data presented here is intended to provide some immediate information but cannot replace input from professionals.
| Fig. 1 Raynaud’s Phenomenon |
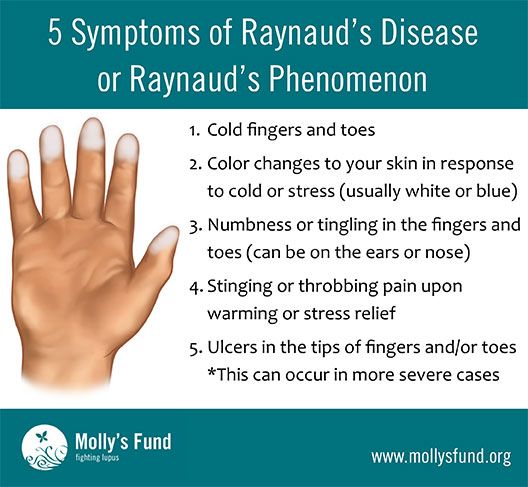
Raynaud’s phenomenon affects up to 10% of otherwise healthy women aged 21-50 years of age. It is 9 times more common in women than men. It was first described by Maurice Raynor 1862 who referred to “local asphyxia of the extremities” and “episodic digital ischaemia provoked by cold and emotion. Originally it was described as affecting mainly fingers and toes but it can affect ear lobes, nose and lips as well as parts of the body.
The first published study of the impact of Raynaud’s phenomenon on breastfeeding was published by Coates (1992)
[Printable version of this sheet includes images for descriptions at Fig.2 below – click to view]
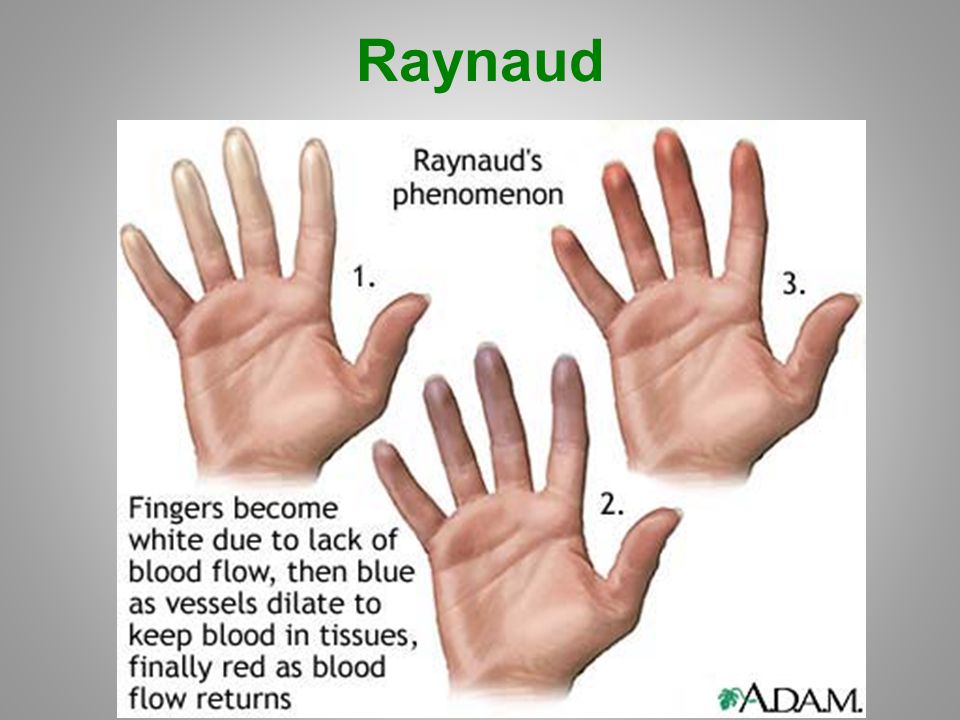
| White nipple Pallor (vasoconstriction) | Purple nipple Cyanosis (deoxygenation of blood) | Red nipple Rubor (vasodilatation) |
Fig. 2 Tri colour changes in the nipple affected by Reynaud’s disease (reproduced from Holmen 2009)
The mother took the photographs above on a camera phone. The mother was 25 years old and described pain in both breasts lasting 5-15 minutes after feeds. Symptoms began in the second week after her child’s birth. She had no medical history of poor circulation but suffered migraines. She did not smoke and had never undergone breast surgery. Nipple pain began in pregnancy but resolved immediately after delivery at 38 weeks gestation. The baby weighed 2.8kg. Breastfeeding technique was checked at 2 weeks post partum when the unbearable pain began. Prescription of Nifedipine produced resolution of the pain totally within a week but it re-occurred when the drug stopped. The mother took nifedipine 30milligrammes daily for 12 months and breastfed for a total of 18 months
The baby weighed 2.8kg. Breastfeeding technique was checked at 2 weeks post partum when the unbearable pain began. Prescription of Nifedipine produced resolution of the pain totally within a week but it re-occurred when the drug stopped. The mother took nifedipine 30milligrammes daily for 12 months and breastfed for a total of 18 months
Lawlor-Smith and Lawlor-Smith (1997) studied 5 patients with severe, debilitating nipple pain. Three had had symptoms during other lactations: one gave up breastfeeding at 6 weeks, another breastfed for 14 months, and the third breastfed for 7 months despite the pain. In all women the cold precipitated pain. All five exhibited blanching during, after, and between feeds. None of them smoked and 2 had history of Reynaud’s, 2 others had parents with Reynaud’s.
There are other case reports where women have been diagnosed with thrush and treated with oral or topical antifungal medication (Barrett). Among the 22 patients with Raynaud phenomenon of the nipple studied, 20 (91%) had previously been treated for Candida with oral or topical antifungals without effect. Of the 12 patients who tolerated a trial of nifedipine, 10 (83%) reported decreased or resolved nipple pain. All patients experienced marked improvement of symptoms with appropriate therapy involving treatment of Raynaud phenomenon. They reported that Nifedipine appeared to be an effective medication for the treatment of Raynaud phenomenon of the nipple and associated improvement of nipple pain.
Of the 12 patients who tolerated a trial of nifedipine, 10 (83%) reported decreased or resolved nipple pain. All patients experienced marked improvement of symptoms with appropriate therapy involving treatment of Raynaud phenomenon. They reported that Nifedipine appeared to be an effective medication for the treatment of Raynaud phenomenon of the nipple and associated improvement of nipple pain.
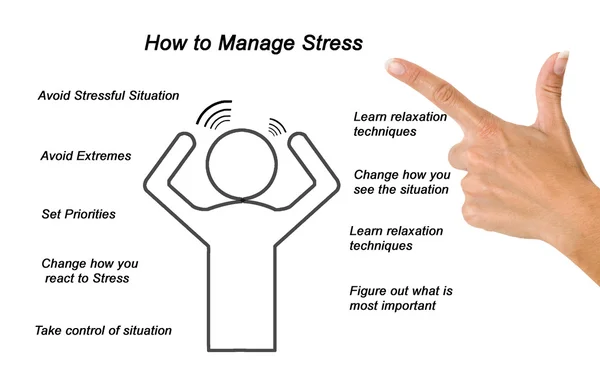
One study suggested that a mother’s stress increased the severity of symptoms.
- Pain which worsens in the cold e.g. passing fridges in the supermarket or even exposure of the nipple to feed
- Bi or tri-phasic colour changes immediately after feeds
- History of circulation problems or close family history of circulation problems
- History of migraines
- Early delivery of baby or small baby – due to vasoconstriction of placental blood vessels
- Optimisation of attachment should be undertaken before considering medical treatment.
- stop smoking Even 2 cigarettes a day are enough to increase constriction of blood vessels by 100% and reduce blood flow by 40%.

- limit caffeine intake (both nicotine and caffeine constrict blood vessels). Caffeine is not just in tea and coffee but also in soft and energy drinks as well as some painkillers
- avoid getting cold, and try moderate aerobic exercise (Cardelli 1989).
- rub the nipples gently with warm oil immediately after feeds or cover the breast immediately with a warm heat- retaining compress eg wheat bag.
- avoid decongestants (in cold remedies), the contraceptive pill and fluconazole which can make symptoms worse
- High doses of vitamin B6 (Newman 2012), magnesium (Smith 1960, Turlapaty Leppert1994), calcium (DiGiacomo 1989), fatty acids (Belch 1985) and fish oil supplementation (DiGiacomo 1989) have also been suggested but take a minimum of 6 weeks to be effective.
- Ginger 2000mg-4000mg daily. Capsules usually contain 500mg. It may also be beneficial to add ginger to your diet, to drink ginger tea, or to put a spoonful of ground ginger in your bathing water (Royal Free hospital http://www.
 royalfree.nhs.uk/pip_admin/docs/Raynaudsnatural_186.pdf
royalfree.nhs.uk/pip_admin/docs/Raynaudsnatural_186.pdf
Symptoms can be successfully managed by the use of nifedipine 30milligrammes daily (10milligrammes capsules three times a day or long acting tablet 30milligrammes daily) for two weeks. Some women need ongoing medication but many find symptoms resolve by this stage. However the drug produces flushing particularly of the face and headaches which some women find intolerable.
- Barrett ME, Heller MM, Fullerton Stone H, Murase JE. Raynaud Phenomenon of the Nipple in Breastfeeding Mothers: An Underdiagnosed Cause of Nipple Pain. Arch Dermatol. 2012 Dec 17:1-7.
- Belch JJ, Shaw B, O’Dowd A, Saniabadi A, Leiberman P, Sturrock RD, Forbes CD.Evening primrose oil (Efamol) in the treatment of Raynaud’s phenomenon: A double-blind study. Throm Haemost 1985; 54 (2):490–4.
- Cardelli MB Raynaud’s phenomenon and disease. Med Clin North Am. 1989; 73(5):1127-41
- Coates M. Nipple pain related to vasospasm J.
 Hum.Lact 1992; 8(3):153
Hum.Lact 1992; 8(3):153 - DiGiacomo RA. Fish oil supplementation in patients with Raynaud’s’s Phenomenon: a double blind, controlled, perspective study. Am J Med 1989; 86:158‐64
- Holmen L and Backe B. Underdiagnosed cause of nipple pain presented on a camera phone. BMJ 2009; 339:b2553
- Kernerman E and Newman J Vasospasm (www.drjacknewman.com/help/Vasospasm%20and%20Raynaud%E2%80%99s%20Phenomenon.asp)
- Lawlor-Smith L and Lawlor-Smith C Vasospasm of the nipple: a manifestation of Raynaud’s’s Phenomenon: case reports. BMJ 1997; 324:644
- Leppert J, Myrdal U, Hedner T, Edvinsson. The concentration of magnesium in erythrocytes in female patients with primary Raynaud’s phenomenon; fluctuation with the time of year. Angiology 1994; 45:283–8.
- Natural remedies in Raynauds Phenomenon Royal Free hospital http://www.royalfree.nhs.uk/pip_admin/docs/Raynaudsnatural_186.pdf
- Smith WO, Hammarsten JF, Eliel LP. The clinical expression of magnesium deficiency.
 JAMA 1960; 174:77–8.
JAMA 1960; 174:77–8. - Turlapaty P, Altura BM. Magnesium deficiency produces spasms of coronary arteries; relationship to etiology of sudden death ischemic heart disease. Science 1980; 208:198–200
©Dr Wendy Jones MBE, MRPharmS and the Breastfeeding Network Sept 2019
Breastfeeding Vasospasm - Milk Fairies
Some breastfeeding moms experience nipple discomfort during and after feeding their baby. Discomfort and pain can occur for various reasons, and one of them is vasospasm .
Vasospasm of the nipples is often correlated with Raynaud's syndrome - a disease characterized by a disorder of arterial circulation mainly in the vessels of the extremities (feet and hands) under the influence of cold or emotional excitement.
Vasospasm of the nipple occurs when the vessels in the upper part of the nipple spasm so much that all the blood drains from its tip, as a result of which the nipple turns white (as an option - successively turns white - blue - purple), and then, when the spasm passes , and the blood rushes back, turns pink again. Vasospasm can occur on one or both breasts at once and last from a few minutes to an hour or more. Soreness can be of a different nature.
Vasospasm can occur on one or both breasts at once and last from a few minutes to an hour or more. Soreness can be of a different nature.
The mother may feel burning, throbbing, stabbing or burning pain; moreover, pain and external manifestations of vasospasm can occur both immediately after feeding and between them [5]. Some moms feel Shooting pain that starts from the nipple and radiates deep into the chest, so vasospasm is often misdiagnosed as a yeast infection.
Vasospasm can occur on its own or as a result of infections or injuries to the nipple - this is how the nipple signals a problem. Often, a mother notices that it has become painful to feed, and after the feeding is completed, she finds that the nipple has become white. Usually injuries and damage to the nipples during lactation are associated with features breastfeeding the baby - in order to prevent or alleviate the symptoms of vasospasm, you must first make sure that the baby is properly attached to the breast and does not injure it when sucking.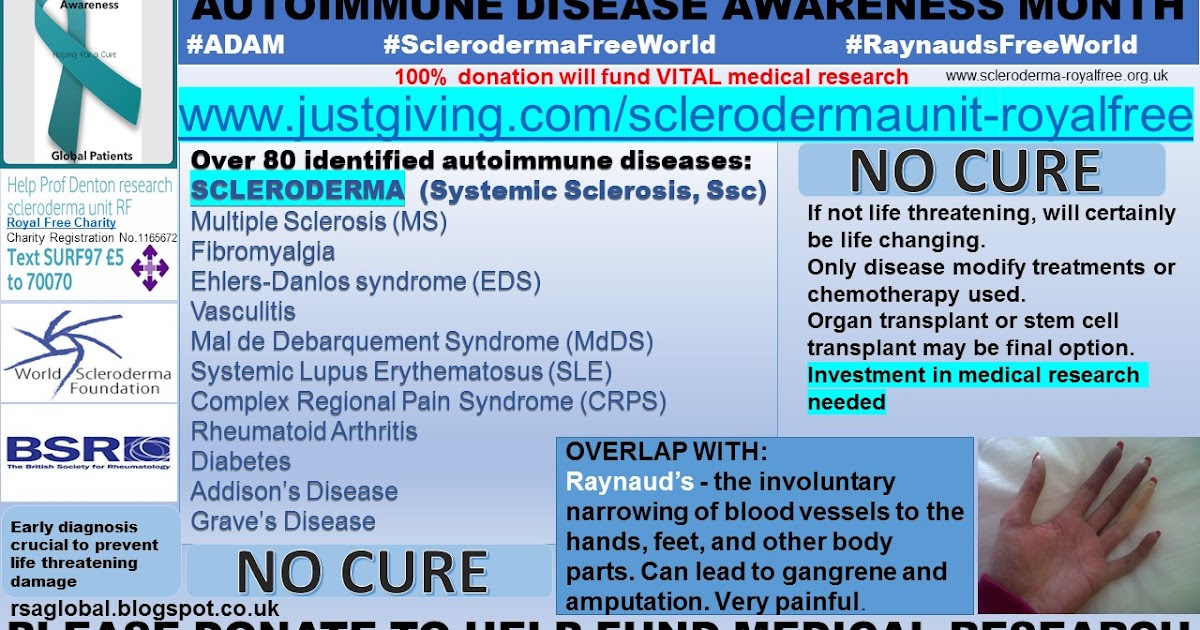
In addition, vasospasm may occur in women who have had breast or nipple surgery in the past, possibly due to tissue and nerve damage. Also, some drugs (eg, fluconazole and oral contraceptives [3]) and some substances, including nicotine and caffeine, can contribute to vasospasm [9].].
How to help yourself during vasospasm?
During the vasospasm itself, to stop the pain, you can try to restore blood flow to the tip of the nipple by gently squeezing the nipple at its base. [8] Gentle massage with light squeezing movements (you can lubricate your fingers with cosmetic or vegetable oil) will help to quickly restore blood supply to the nipple and reduce pain until it disappears completely.
In the case of prolonged and severe pain, you can take (on consultation with your doctor!) an anesthetic that is compatible with breastfeeding, such as Ibuprofen or Paracetamol. [1
How to prevent vasospasm?
To avoid or reduce the intensity of vasospasms, in the first place - do not overcool ! [2] Put on a warm vest or carry your baby in your arms for a while after feeding. Some mothers find it helpful to put a warm diaper on the nipple as soon as the baby releases the breast. Some people use a hair dryer on warm air, blowing it on their breasts. Similarly, any warm dry and wet compresses help or even your own warm hand covering the nipple immediately after breastfeeding.
Some mothers find it helpful to put a warm diaper on the nipple as soon as the baby releases the breast. Some people use a hair dryer on warm air, blowing it on their breasts. Similarly, any warm dry and wet compresses help or even your own warm hand covering the nipple immediately after breastfeeding.
If painful vasospasm continues despite non-traumatic breastfeeding and heat application after feedings, then medication prevention and treatment of vasospasm (only prescribed by your physician!) may be an option. For example, you can ask the doctor to prescribe vitamin B6, calcium and magnesium as a preventive measure and relieve vasospasm .
Some doctors recommend applying a moderate amount of nitroglycerin ointment or 2% spray to the nipples after each feed for the first 24 hours and then whenever symptoms of vasospasm begin [6]. However, its use can cause a side effect in the form of headaches, and only about half of the patients confirm the effectiveness of such an ointment for vasospasm.
One tablet Nifedipine long-acting tablets per day for two weeks may also help. Nifedipine is a calcium channel blocker commonly used to treat hypertension and is not excreted in breast milk. [7] Nifedipine therapy has been shown to be effective in vasospasm and has no side effects in the baby [4]. 9
 & Pitman, T. The Ultimate Breastfeeding Book of Answers. Roseville, California: Prima 2000
& Pitman, T. The Ultimate Breastfeeding Book of Answers. Roseville, California: Prima 2000 Alena Korotkova,
Clinical psychologist, breastfeeding consultant
Alena Lukyanchuk, Psychologist 9000 9000 9000 9000 9000 9000 9000 Mershondonate milk
Find milk
Being pregnant, I was sure that I would breastfeed. My mother breastfed me, my mother-in-law nursed my husband. I knew the benefits of breastfeeding and knew that breastfeeding is natural.
My mother breastfed me, my mother-in-law nursed my husband. I knew the benefits of breastfeeding and knew that breastfeeding is natural.
I am a supporter of natural parenting, so I planned for natural childbirth, the use of a sling, free swaddling, skin-to-skin contact, in general, to give my son all the best from birth. I didn’t buy bottles, because I planned to be at home with my child, the idea of \u200b\u200bpaying $ 200 for a breast pump seemed ridiculous to me.
It turned out that parenthood is not as easy as expected. Fate has thrown us problems. I gave birth to my son on September 15, 2011, helped me with a wonderful doula, and immediately began the struggle for breastfeeding. For 3 weeks I exclusively breastfed, through pain, cracked nipples and tears.
Every day I give my son 150-350 ml of breast milk from my supply, but it won't last long. The nearest milk bank is 4.5 hours away, milk is dispensed by prescription from a pediatrician, first of all, seriously ill and premature babies receive milk, and the cost of 30 ml is $ 3 (excluding delivery costs).
Doula advised her to seek help from breast milk donors. I found two donor mothers from my city on the relevant site who offered breast milk for free, very generous of them. Guilt choked me from the inside, I prayed that these women would not condemn me for not being able to feed my own child, the inability to express breast milk. In addition, the people around, having learned about donor milk, were wary of this idea - how do I know that donor milk is safe, that mothers do not get sick and do not take drugs?
Fortunately, the donor mothers did not judge me, they just helped, just like me, they were sure that breast milk is the natural, ideal food for a child. We became friends with one of the mothers, her daughter is a year older than my son, and is still breastfeeding, and she passes the expressed 170 ml of milk to my son! (I also told her about babywearing and now she's a babysling!)
At the end of October/beginning of November my son had 13 donors, by 24 weeks we were completely off formula supplementation.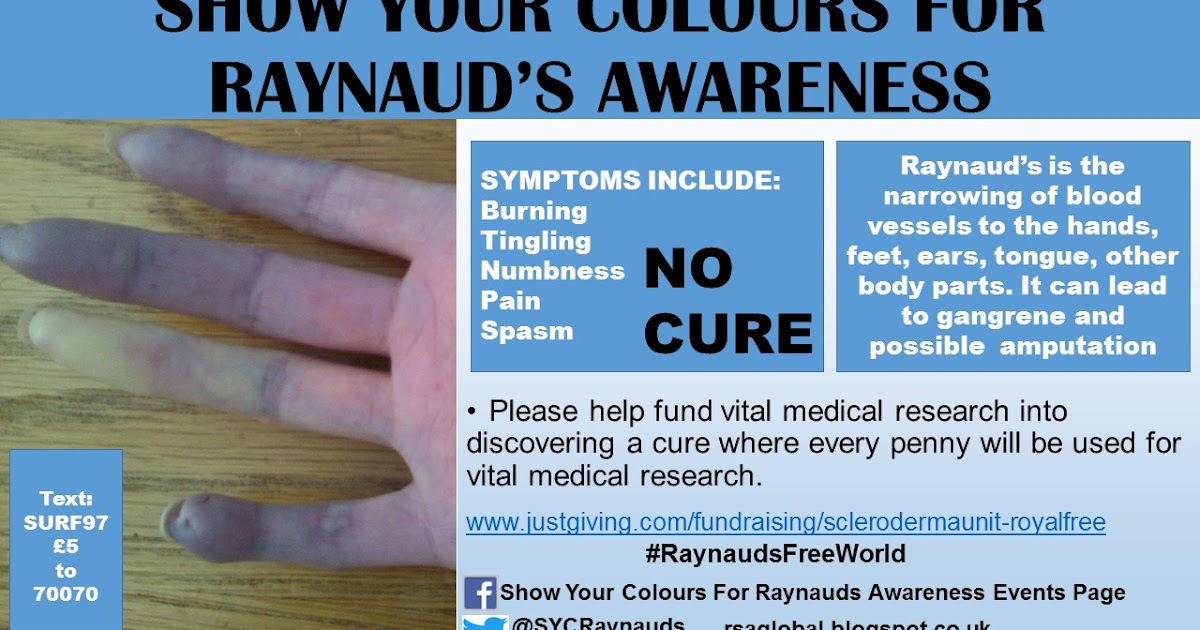 I met all the women, I saw how they pump or feed their children, many of them provided copies of the results of the blood test and medical history. One of the donors is my school friend, another is my husband's classmate, and the third is my classmate's half-sister. All of them shared breast milk selflessly, not for profit (which is prohibited by the rules of the GM sharing community). Through breast milk donation, I made friends in California, Oregon, Colorado.
I met all the women, I saw how they pump or feed their children, many of them provided copies of the results of the blood test and medical history. One of the donors is my school friend, another is my husband's classmate, and the third is my classmate's half-sister. All of them shared breast milk selflessly, not for profit (which is prohibited by the rules of the GM sharing community). Through breast milk donation, I made friends in California, Oregon, Colorado.
I realized that it is possible to combine natural parenting and bottle feeding. I hold my son in my arms and feed him myself (not allowing the child to hold the bottle himself), trying to organize the feeding process as close as possible to breastfeeding. When I go for a walk, I don’t use a stroller, I carry my son in a sling. I immediately respond to his crying, we do not have a feeding and sleeping regimen.
I would never have thought that I would not be able to breastfeed my son. I am so grateful to all the women I have met because of our situation.