Can you get pregnant with herpes
What you should know about sex and pregnancy
Diseases & conditions
- Coronavirus Resource Center
- Acne
- Eczema
- Hair loss
- Psoriasis
- Rosacea
- Skin cancer
- A to Z diseases
- A to Z videos
- DIY acne treatment
- How dermatologists treat
- Skin care: Acne-prone skin
- Causes
- Is it really acne?
- Types & treatments
- Childhood eczema
- Adult eczema
- Insider secrets
- Types of hair loss
- Treatment for hair loss
- Causes of hair loss
- Hair care matters
- Insider secrets
- What is psoriasis
- Diagnosis & treatment
- Skin, hair & nail care
- Triggers
- Insider secrets
- What is rosacea
- Treatment
- Skin care & triggers
- Insider secrets
- Types and treatment
- Find skin cancer
- Prevent skin cancer
- Raise awareness
- Español
Featured
Monkeypox: What you need to knowMonkeypox is a contagious disease that causes a rash. A board-certified dermatologist explains what the rash looks like and when to seek medical care.
This contagious skin disease will usually clear on its own, but sometimes dermatologists recommend treating it. Find out when.
Everyday care
- Skin care basics
- Skin care secrets
- Injured skin
- Itchy skin
- Sun protection
- Hair & scalp care
- Nail care secrets
- Basic skin care
- Dry, oily skin
- Hair removal
- Tattoos and piercings
- Anti-aging skin care
- For your face
- For your skin routine
- Preventing skin problems
- Bites & stings
- Burns, cuts, & other wounds
- Itch relief
- Poison ivy, oak & sumac
- Rashes
- Shade, clothing, and sunscreen
- Sun damage and your skin
- Aprenda a proteger su piel del sol
- Your hair
- Your scalp
- Nail care basics
- Manicures & pedicures
Featured
Practice Safe SunEveryone's at risk for skin cancer. These dermatologists' tips tell you how to protect your skin.
These dermatologists' tips tell you how to protect your skin.
Find out what may be causing the itch and what can bring relief.
Darker Skin Tones
- Skin care secrets
- Hair care
- Hair loss
- Diseases & Conditions
- Acne
- Dark spots
- Dry skin
- Light spots
- Razor bumps
- Caring for Black hair
- Scalp psoriasis
- Weaves & extensions
- Central centrifugal cicatricial alopecia
- Frontal fibrosing alopecia
- Hairstyles that pull can cause hair loss
- Acanthosis nigricans
- Acne keloidalis nuchae
- Hidradenitis suppurativa
- Keloid scars
- Lupus and your skin
- Sarcoidosis and your skin
- Skin cancer
- Vitiligo
- More diseases & conditions
Featured
Fade dark spotsFind out why dark spots appear and what can fade them.
If you have what feels like razor bumps or acne on the back of your neck or scalp, you may have acne keloidalis nuchae. Find out what can help.
Cosmetic treatments
- Your safety
- Age spots & dark marks
- Cellulite & fat removal
- Hair removal
- Scars & stretch marks
- Wrinkles
- Younger-looking skin
Featured
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
Do you know which one?
If you want to diminish a noticeable scar, know these 10 things before having laser treatment.
BotoxIt can smooth out deep wrinkles and lines, but the results aren’t permanent. Here’s how long botox tends to last.
Public health programs
- Skin cancer awareness
- Free skin cancer screenings
- Kids' camp
- Good Skin Knowledge
- Shade Structure grants
- Skin Cancer, Take a Hike!™
- Awareness campaigns
- Flyers & posters
- Get involved
- Lesson plans and activities
- Community grants
Featured
Free materials to help raise skin cancer awarenessUse these professionally produced online infographics, posters, and videos to help others find and prevent skin cancer.
Free to everyone, these materials teach young people about common skin conditions, which can prevent misunderstanding and bullying.
Find a dermatologist
- Find a dermatologist
- What is a dermatologist?
- FAAD: What it means
- How to select a dermatologist
- Telemedicine appointments
- Prior authorization
- Dermatologists team up to improve patient care
Featured
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist that’s right for you.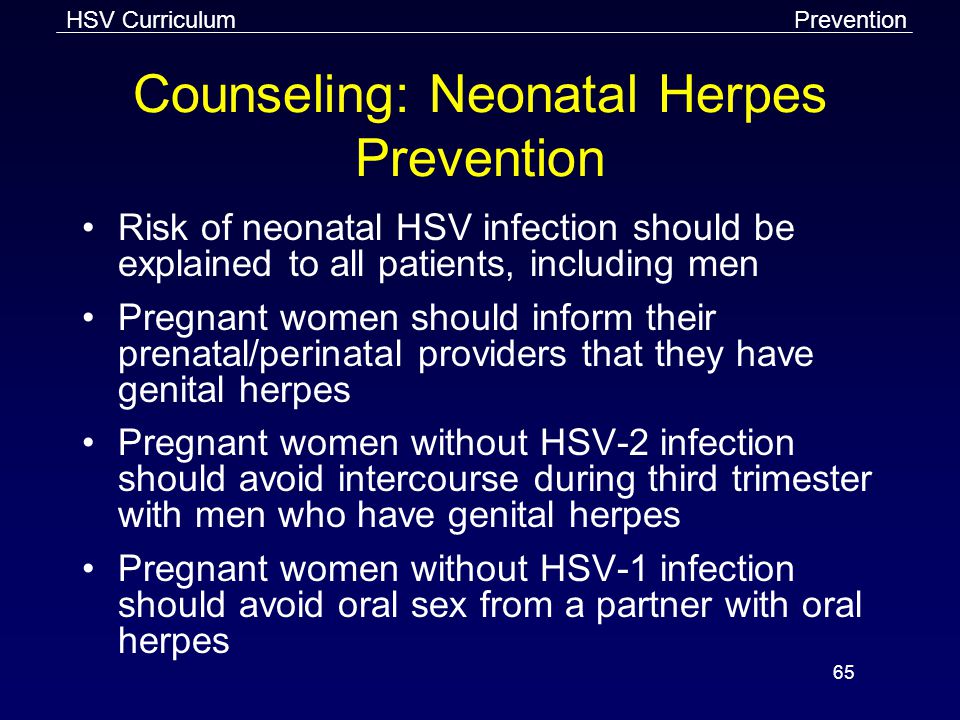
A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Does Herpes Impact Fertility? – Advanced Fertility Center of Texas
Herpes poses few serious risks when it comes to reproductive health.
Herpes is an infection caused by herpes simplex virus (HSV). It’s possible to contract the virus through skin-to-skin contact with a person who has HSV. It is most commonly spread through the moist skin that lines the mouth, genitals, or anus, though it can spread by way of other areas of skin or the eyes. Herpes may affect the mouth, external genitalia, anal area, or other regions of skin.
Since there is no cure for herpes, the condition is chronic. Luckily, many who contract the condition never experience symptoms. Those who do may experience blisters, ulcers, cold sores, vaginal discharge, or pain during urination. Luckily, there are a number of medications and home remedies that are able to treat symptoms.
Luckily, there are a number of medications and home remedies that are able to treat symptoms.
Around 17% of people aged 19-49 have genital herpes while around 50-80% of all Americans have oral herpes (the data is imprecise because people often assume that they simply have a cold sore instead of oral herpes and, as a result, don’t treat the infection).
Though the disease is extremely common, it still carries a stigma that discourages many patients from speaking about it candidly with their healthcare practitioners. A common concern expressed by patients is how the infection may affect their fertility. Here’s what you need to know:
Herpes and Female Fertility
While it’s true that other sexually transmitted infections (STIs) including gonorrhea and chlamydia can negatively impact female fertility if left untreated, herpes, whether treated or not, does not pose any similar threat. While symptoms of herpes may include sores or blisters around the genitals, these symptoms do not affect the reproductive organs.
Herpes cannot impact biological fertility levels — however, in the case of an outbreak, it is recommended that those experiencing herpes abstain from sexual intercourse. If you have herpes, you may need to delay efforts at conception, but once the outbreak passes, you can engage in normal sexual activity.
Herpes and Male Fertility
While herpes has no impact on female fertility, herpes can reduce a man’s sperm count. A 2013 study found that herpes was associated with low sperm count among men who were tested. This is the only known effect of herpes on fertility.
Herpes and Pregnancy
Many women worry about how having herpes might impact their pregnancy and childbirth.
Unless the first outbreak occurs while pregnant, there is practically no risk associated with herpes and pregnancy. In fact, according to the American Sexual Health Association, while 25-30% of pregnant women have genital herpes, less than 0.1% of babies both in the United States each year get neonatal herpes.
The only real danger that herpes poses to pregnancy is in the form of an extremely rare strain of the virus, HHV-6A, which can lead to miscarriage. However, the vast majority of pregnant women with herpes carry a healthy baby to term.
If you are pregnant and have herpes, it’s important that your doctor know about your diagnosis in order to effectively monitor you for outbreaks before childbirth. If you have an outbreak while giving birth, it is best to have a C-section to prevent the baby from coming into contact with the sores. If you don’t have any open sores, however, it is completely safe to have a vaginal birth while having herpes.
Protecting Your Sexual and Reproductive Health
A large body of research suggests that herpes poses no real risks to female fertility. Though herpes may potentially affect sperm counts in men, for the most part, those with herpes are able to conceive with no problem (barring the presence of any other fertility-affecting conditions).
Critically, it’s important to remember that you can get pregnant and give birth to a completely healthy baby if you have herpes. The best way to protect yourself and your future child is to undergo a full STI screening and asking your practitioner about any other potential risks to your fertility, pregnancy, or ability to give birth.
If you do have concerns about how herpes or other STIs can impact your sexual or reproductive health, don’t hesitate to schedule an appointment to address these concerns with a fertility specialist at AFCT. We’re here to ease the family planning process by guiding you through a fertility treatment or process that works for you.
Preparing and planning pregnancy for herpes infection | Tyutyunnik V.L., Zaidieva Z.S., Alieva S.A.
Preparation and planning of pregnancy in case of herpes infection
January 14, 2005
Share material print Add to favorites- Tyutyunnik V.
 L. 1 ,
L. 1 , - Zaidieva Z.S. ,
- Alieva S.A.
one
FSBI NMITs AGP im. IN AND. Kulakov» of the Ministry of Health of Russia, Moscow, Russia
For citation: Preparation and planning of pregnancy in case of herpes infection. breast cancer. 2005;1:28.
Currently, in many countries of the world, including Russia, there has been an increase in sexually transmitted infections, which firmly occupy a leading place in the structure of obstetric and gynecological morbidity. Most often, sexual infection is caused by several pathogenic factors - viruses, microbes, fungi, protozoa, which cause diseases similar in clinical course, but different in pathogenesis and methods of treatment.
Most often, sexual infection is caused by several pathogenic factors - viruses, microbes, fungi, protozoa, which cause diseases similar in clinical course, but different in pathogenesis and methods of treatment.
Among the viral lesions of the urogenital tract of women, herpetic, cytomegalo- and papillomavirus infections are the most common, and therefore they are included in the group of diseases that determine the future of infectious pathology by the WHO Regional Office for Europe.
In the occurrence of herpetic diseases of the genital organs, the main role belongs to the herpes simplex virus, the only reservoir of which is people infected with it, who spread it among the population. Once in the human body, the herpes simplex virus remains in it throughout life, periodically causing diseases of varying severity.
Given that genital herpes is a lifelong persistent infection, there are several types of clinical manifestations. Relapses of the disease occur as a result of intermittent immunodeficiency in apparently healthy people under the influence of provoking factors.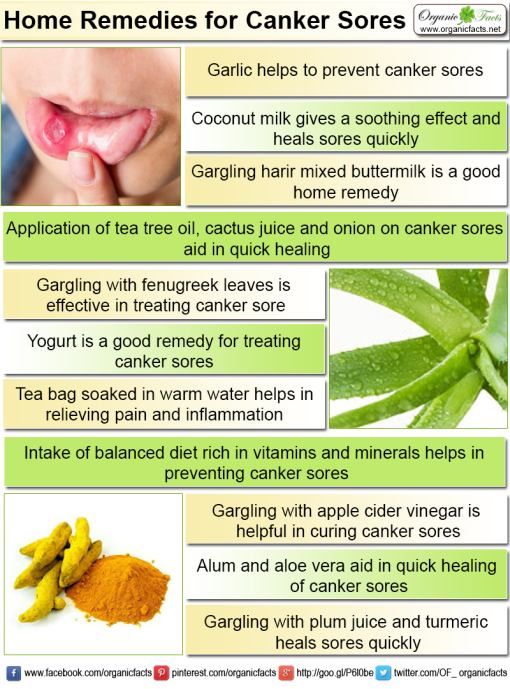 Recurrent nature of genital herpes acquires a third of infected people. Infection with the herpes simplex virus is possible not only in the acute stage of the disease, but also in the stage of deep remission.
Recurrent nature of genital herpes acquires a third of infected people. Infection with the herpes simplex virus is possible not only in the acute stage of the disease, but also in the stage of deep remission.
Genital herpes is a sexually transmitted disease (in 99.9% of cases). Autoinoculation can occur when the patient himself transfers the virus from the focus of infection to uninfected parts of the body. The vertical route of transmission is possible in the case of transplacental infection of the fetus. The causative agent of this infection is assigned a certain role in the etiology of spontaneous abortions and premature births, as well as in violation of embryogenesis and congenital pathology of newborns, etc., which is considered the result of intrauterine viral infection.
Knowledge of the principles of selection of patients who need in-depth examination in order to verify the diagnosis of genital herpes, can significantly increase the effectiveness of preventive measures aimed at preventing a complicated course of pregnancy, as well as intrauterine infection.
Works devoted to the preparation for pregnancy of women with chronic recurrent herpetic infection are extremely few and, as a rule, are aimed at correcting individual links of the pathological condition.
Proceeding from the foregoing, the most important and integral stage is the correct pre-gravid preparation of these women. Therefore, infection control measures must be started before pregnancy.
It is well known that the treatment of herpetic infection should be timely, etiotropic and complex. When a genital herpes infection is detected, regardless of the level of damage to the reproductive system, both basic types of therapy (a complex of antiviral treatment) and treatment of diseases associated with herpes are indicated.
The main objectives of antiherpetic therapy are:
• reduction of clinical manifestations of infection;
• relapse prevention;
• prevention of transmission of infection to a sexual partner or newborn.
The treatment strategy for patients with recurrent herpes is determined by a number of factors: the frequency of relapses and the severity of clinical symptoms (based on the subjective assessment of the patient), the state of the immune system, psychosocial characteristics, the risk of transmission of infection to a sexual partner or newborn, as well as economic aspects of therapy. Currently, there are two options for the treatment of genital herpes using nucleazide analogues: episodic and preventive (suppressive) therapy.
Currently, there are two options for the treatment of genital herpes using nucleazide analogues: episodic and preventive (suppressive) therapy.
Our experience in preparing women with genital herpes for pregnancy shows that one of the modern and most effective antiviral drugs is Alpizarin, an antiviral agent obtained from the herb kopek. The drug is active against DNA-containing viruses (Herpes simplex type I and II, Varicella zoster, to a lesser extent - cytomegalovirus and human immunodeficiency virus). Alpizarin inhibits the reproduction of the herpes simplex virus in the early stages of its development, inhibits bacterial nuclease without a pronounced inhibitory effect on viral neuraminidase, has a moderate bacteriostatic effect against gram-positive and gram-negative bacteria, protozoa and Mycobacterium tuberculosis. The drug has an immunostimulatory effect on cellular and humoral immunity, induces the production of g-interferon in blood cells.
Absorption of Alpizarin is high, the onset of Cmax is 1-3 hours, the drug penetrates well into the organs and tissues of the liver, kidneys, heart, spleen; after 12 hours it is found in a small amount in the brain tissues, excreted by the kidneys and through the gastrointestinal tract.
Indications for the use of the drug are: infections of the skin and mucous membranes caused by Herpes simplex and Varicella zoster viruses.
Alpizarin is administered orally (regardless of food intake) at a dose of 0.1-0.2 g 3-4 times a day for 5-10 days. At the same time, local applications of 5% ointment to the skin and 2% ointment to the mucous membranes are prescribed. The ointment is applied to the affected areas of the skin without a bandage 2-6 times a day. The therapeutic effect is more pronounced when it is used in the early stages of the disease. The duration of treatment is 10–30 days. In case of relapse, the course is repeated. In acute and recurrent forms of herpes simplex of extragenital localization with single rashes, the ointment is applied to the lesion 2-3 times a day for 3-5 days. In the case of widespread rashes, as well as in the presence of fever, lymphadenopathy is prescribed both orally and as an ointment for 5-14 days. With genital herpes, 2% ointment is applied to the affected areas 4-6 times a day for 7-10 days, with a recurrent course of the disease - additionally inside for 5-14 days. For the prevention of relapses of herpes simplex, an oral course is prescribed 1 month after the end of treatment and then in interrecurrent periods in courses of 10–14 days.
For the prevention of relapses of herpes simplex, an oral course is prescribed 1 month after the end of treatment and then in interrecurrent periods in courses of 10–14 days.
Episodic therapy involves oral administration of drugs at the time of an exacerbation of the infection. This method of therapy is indicated for patients with rare, clinically unexpressed exacerbations and in the presence of a clearly defined prodromal syndrome, during which the drug should be started. The use of Alpizarin during the recurrence of genital herpes 0.2 g 4 times a day for 5 days significantly reduces pain and discomfort in the affected area, reduces the healing time of herpetic eruptions by 1-2 days and the period of virus shedding.
Suppressive therapy is indicated in patients with rare but severe recurrences, in discordant genital herpes couples to prevent transmission of infection, in the presence of pronounced psychosocial and psychosexual reactions to relapses, and also with a significant effect of infection on the quality of life of the patient. The drugs are used daily continuously for a long time. When conducting preventive (suppressive) therapy, Alpizarin is prescribed 0.2 g 4 times a day.
The drugs are used daily continuously for a long time. When conducting preventive (suppressive) therapy, Alpizarin is prescribed 0.2 g 4 times a day.
An important condition for proper preparation for pregnancy is the normalization of the patient's immune and interferon status. Therefore, against the background of the blockade of virus replication, a promising direction for the prevention and treatment of herpes infection is the stimulation of nonspecific resistance of the organism, depending on the indicators of the immune and interferon status of patients (immunoglobulin preparations, interferon inducers, enzyme therapy, etc.).
Since the presence of foci of chronic infection is accompanied by a violation of energy and metabolism processes at the cellular, tissue and organ levels, pregravid preparation must necessarily include metabolic therapy. For this purpose, a complex of drugs is prescribed that stimulates bioenergetic processes in cells and tissues - metabolic therapy, consisting of 2 treatment complexes:
I complex (from 8–9 days to 13–14 days of the menstrual cycle):
1 Cocarboxylase 0. 1 g 1 time intramuscularly or benfotiamine 0.01 g 3 times a day.
1 g 1 time intramuscularly or benfotiamine 0.01 g 3 times a day.
2. Riboflavin mononucleotide 1–2 (0.005–0.01 g) tab. 3 times a day or 1 ml intramuscularly 1 time per day.
3. Calcium pantetonate 1 tab. 3 times a day or 20% solution 2 ml intramuscularly 1 time per day.
4. Lipoic acid 1 (0.025 g) tab. 3 times a day or 0.5% solution 4 ml intramuscularly 1 time per day.
5. a-tocopherol acetate 1-2 (0.05-0.1 g) capsules 3 times a day. or 1 ml intramuscularly.
Complex II (from the 15th day to the 22nd day of the menstrual cycle):
1. Riboxin 0.2 g 3 times a day.
2. Pyridoxine 1 (0.02 g) tab. 3 times a day
3. Folic acid 1 (0.001 g) tab. 3 times a day
4. Potassium orotate 1 (0.5 g) tab. 3 times a day
5. a-tocopherol acetate 1-2 (0.05-0.1 g) capsules 3 times a day. or 1 ml intramuscularly.
Metabolic therapy is prescribed for 3 consecutive months before pregnancy.
Immuno- and interferon-correcting and antibacterial therapy should be carried out while taking enzyme preparations. The basis for the use of systemic enzyme therapy is its immunomodulatory and anti-inflammatory effect, the ability to limit the manifestations of autoimmune processes, and the normalization of microcirculation. In addition, the use of the enzymatic complex contributes to a deeper penetration of antibiotics into the focus of inflammation.
The basis for the use of systemic enzyme therapy is its immunomodulatory and anti-inflammatory effect, the ability to limit the manifestations of autoimmune processes, and the normalization of microcirculation. In addition, the use of the enzymatic complex contributes to a deeper penetration of antibiotics into the focus of inflammation.
When carrying out the above therapy, simultaneous or sequential use of passive immunization with specific antiherpetic immunoglobulins in a titer of 1:320 or 1:640 is possible. Patients with acute manifestations of genital herpes specific antiherpetic immunoglobulin were prescribed 2 doses with an interval of 3-4 days for a course of 5 intramuscular injections.
Vaccine therapy may also be used to prevent recurrence of herpes infection. Currently, all existing vaccines are divided into live, inactivated (whole virus and subunit) and recombinant. The theoretical prerequisite for the use of vaccine therapy for genital herpes was the assumption of the possibility of strengthening specific antiherpetic immunity against the background of repeated administration of the viral antigen. The vaccine represents the herpes simplex virus of the 1st and 2nd antigenic type which is grown up on culture of cells of a chicken embryo and formalin inactivated. An important methodological feature of the use of the vaccine is its use to prevent recurrence of the disease only in the period of attenuation of its acute effects, which makes it possible to obtain a stable anti-relapse effect. Therefore, the vaccine should be administered immediately after a course of chemotherapy and immunoglobulins.
The vaccine represents the herpes simplex virus of the 1st and 2nd antigenic type which is grown up on culture of cells of a chicken embryo and formalin inactivated. An important methodological feature of the use of the vaccine is its use to prevent recurrence of the disease only in the period of attenuation of its acute effects, which makes it possible to obtain a stable anti-relapse effect. Therefore, the vaccine should be administered immediately after a course of chemotherapy and immunoglobulins.
In addition to the treatment of herpes infection, additional therapy is indicated. Treatment of a latent chronic inflammatory process in the endometrium (viral and bacterial etiology) should be carried out against the background of basic therapy and be etiotropic and pathogenetically justified. Given the prevalence of anaerobic-aerobic associations, as well as myco-ureaplasma and chlamydial infections, the use of broad-spectrum antibiotics is shown.
Thus, planning and preparation for pregnancy is possible only with persistent and long-term (more than 6 months) remission of herpes infection, as well as after the elimination of violations in the reproductive system, taking into account the main factors of abortion. Early diagnosis, prevention and treatment of infectious pathology of the reproductive system of women before pregnancy, preconception preparation and pregnancy planning can reduce the frequency of complications of the gestational period, the severity of the course (frequency and duration of relapses) of the infectious process during pregnancy, severe forms of neonatal infection, perinatal morbidity and mortality .
Early diagnosis, prevention and treatment of infectious pathology of the reproductive system of women before pregnancy, preconception preparation and pregnancy planning can reduce the frequency of complications of the gestational period, the severity of the course (frequency and duration of relapses) of the infectious process during pregnancy, severe forms of neonatal infection, perinatal morbidity and mortality .
Content is licensed under a Creative Commons Attribution 4.0 International License.
Get the pdf version of article
Download article All articles of the issueReproductive Health Training CenterReproductive Health Training Center
Having genital herpes does not mean you cannot have children. According to the American Public Health Association (ASHA), only 0. 1% of cases of herpes are transmitted during pregnancy from mother to unborn child. Most women with genital herpes successfully carry out pregnancy and give birth to healthy children .
1% of cases of herpes are transmitted during pregnancy from mother to unborn child. Most women with genital herpes successfully carry out pregnancy and give birth to healthy children .
Breast-feeding during herpes recurrence is possible. Except when herpetic eruptions are located on the nipples or mammary gland. If your doctor prescribes oral antiviral drugs during breastfeeding, the question of the advisability of continuing breastfeeding during the course of suppressive therapy should be discussed with your doctor.
The initial episode of genital herpes is usually a tragedy during pregnancy. It is characterized by pronounced manifestations, tk. there are no antibodies in the mother's body that protect against herpes. For the fetus, the risk is especially high when infected with genital herpes in the first and third trimesters. As a rule, fetal death and miscarriage occur in the first trimester. Damage to the developing organs of the fetus, the occurrence of congenital deformities are possible. Infection in the III trimester, especially after 36 weeks of pregnancy, is fraught with damage to the nervous system of the fetus, skin, liver, spleen. Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
Infection in the III trimester, especially after 36 weeks of pregnancy, is fraught with damage to the nervous system of the fetus, skin, liver, spleen. Despite postpartum treatment, up to 80% of newborns with a primary episode of genital herpes in the mother die or become severely disabled. Even intravenous administration of acyclovir to a newborn does not help. Fortunately, such situations are extremely rare and it takes several decades to work in obstetrics to see fetal lesions caused by a primary episode of herpes during pregnancy.
HOW TO DETECT THAT I HAVE A PRIMARY EPISODE OF GENITAL HERPES?
What does primary episode mean? It means that in your life there has never been a recurrence of genital herpes and the body has not yet developed protective antibodies to HSV.
In some cases it is difficult to determine: what is it? Whether the first episode of genital herpes in life or the first recurrence with visible symptoms of genital herpes that was previously asymptomatic or with atypical symptoms. The fact is that in most people infected with HSV, the disease is almost asymptomatic. It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo.
The fact is that in most people infected with HSV, the disease is almost asymptomatic. It is especially difficult to identify the disease in women if relapses occur inside her genitals, for example, on the cervix or in response to a relapse, a slight redness with cracks appears on the labia, which the woman takes for irritation. She lives and does not suspect that she has RGH. But here, during pregnancy, so that a miscarriage does not occur, hormonal changes occur in the woman's body, aimed at a physiological decrease in immunity - immunosuppression. Against this background, recurrences of herpes can become visible and rashes can come out, for example, on the labia, clitoris, perineum with manifestation in the form of itching, burning, vesicles and crusts, etc. In order to distinguish the primary episode of genital herpes from the first recurrence with visible symptoms, the patient needs to donate blood from a vein for antibodies to HSV-1,2. If there is Ig G (G class immunoglobulin) in the blood, then herpes is recurrent and there is practically no threat to the fetus or embryo. If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
If there is no Ig in the blood, but there is Ig M or Ig M is also absent, then this is the very first episode of genital herpes in life. In this case, you need to consult a doctor and be examined.
There are no specific methods for preventing the transmission of genital herpes during pregnancy. From non-specific, monogamous relationships, constant use of a condom can be recommended. If it is known that the father of the child is infected with genital herpes, and the mother is not, then you should either completely refrain from sexual activity during pregnancy (until the moment of delivery). Or a man should constantly use a condom + valaciclovir 1 tablet daily throughout the pregnancy. This measure will help to reduce the risk of transmission of genital herpes by 75%.
Should refrain from oral sex. Because if you have never had herpes of the lips in your life, and the husband or father of the child had it, then during cunniling he can bring the herpes simplex virus type I to your genitals.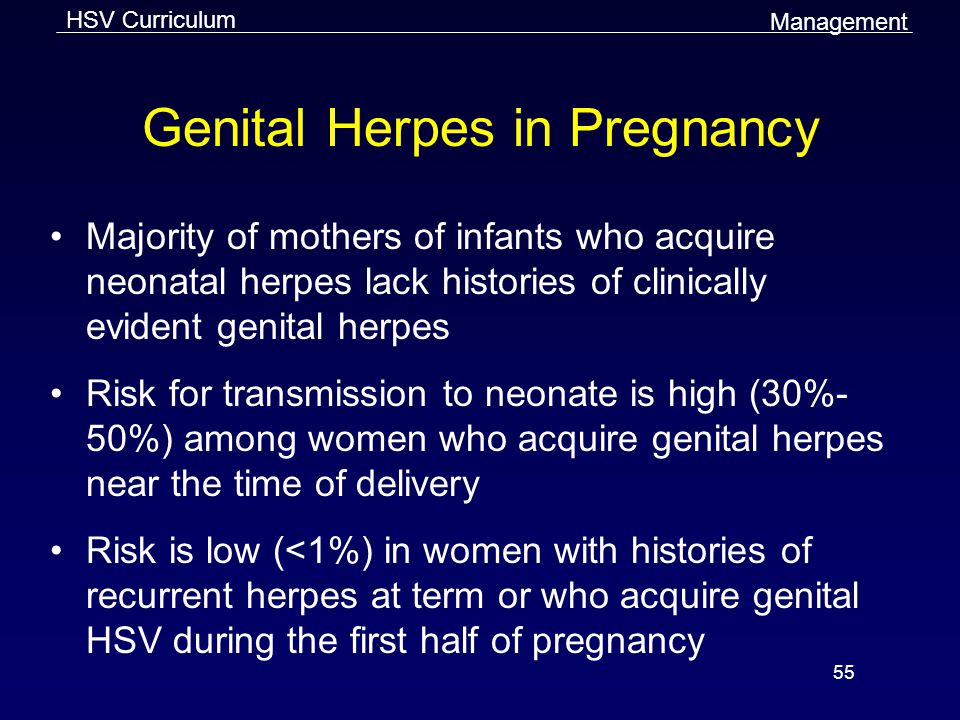 And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
And since If you have never had HSV-1, then there are no protective antibodies in your body, the fetus may suffer (this situation is called a non-primary episode of genital herpes during pregnancy). We also recommend to refrain from blowjob.
Treatment with acyclovir and valtrex. However, these drugs do not always allow to achieve good success in treatment.
According to the Centers for Disease Control (USA), the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect the development of the fetus. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Against the background of a primary episode of genital herpes, the loss of a desired pregnancy is a severe psychological trauma for both potential parents. But in any case, there is hope. The next pregnancy will proceed already against the background of recurrent genital herpes. After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
After the first outbreak, antibodies will circulate in the mother's blood until her death (in very advanced years), which will preserve the unborn child.
Recurrent genital herpes during pregnancy
As blasphemous as it may sound, but recurrent genital herpes is the most favorable option during pregnancy. If a woman before the onset of this pregnancy already had relapses of genital herpes, then the fetus is protected from infection by maternal antibodies that block the action of the herpes simplex virus. There is a 99% chance that your child will not get herpes.
STATISTICS:
During pregnancy, infection of a newborn with herpes simplex virus from a mother with recurrent genital herpes occurs quite rarely: in approximately 0.02% of cases.
The risk of infection of a child in childbirth from a mother suffering from recurrent genital herpes is less than 1% (According to the study: Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. Effect of serological status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant JAMA 2003;289: 203-9).
BEFORE PREGNANCY: Plan the onset of pregnancy , eliminate bad habits from your life, heal chronic diseases, take a course of restorative treatment, cure foci of chronic infection before pregnancy (sick teeth, sinusitis, gastritis).
In some cases, a woman cannot know whether she had recurrences of genital herpes before or not. This happens with herpes that occurs without symptoms or with an atypical course. In addition, it should be borne in mind that, unlike the stronger sex, the female genital organs are “not visible”. In order to find out if you have ever had a relapse, you should do a serological analysis. Donate blood for antibodies (immunoglobulins Ig G & Ig M) to HSV-1,2. If Ig G is present in the blood, then herpes is recurrent - herpes practically does not threaten pregnancy. The Ig G index is qualitative (higher than diagnostic titers). Regardless of the titer (the amount of Ig G & M), you can become pregnant.
DURING PREGNANCY:
- When having sex always use a condom ;
- Avoid oral sex
If you get cold sores during pregnancy, you can transfer it to the penis of the father of your unborn child during oral sex. And he will transfer the infection to your genital tract with this member. This can lead to bad consequences for the child. On the other hand, if you allow your husband to cunniling and he has cold sores on his lips, he may bring a different type of herpes to your genitals. That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
And he will transfer the infection to your genital tract with this member. This can lead to bad consequences for the child. On the other hand, if you allow your husband to cunniling and he has cold sores on his lips, he may bring a different type of herpes to your genitals. That's why it's better not to joke with oral sex during pregnancy - 9You can grind months in the name of a new life.
PROPHYLAXIS DURING PREGNANCY:
To prevent recurrence during pregnancy after 36 weeks, your doctor may prescribe a course of preventive treatment with acyclovir or valaciclovir. During pregnancy, it is better to use acyclovir, manufactured by GlaxoSmithKline under the name Zovirax or Valtrex. Unlike Russian and Indian analogues, the safety of Zovirax has been proven by clinical trials and experience in using this drug for more than 25 years. Take a multivitamin for pregnant and lactating women.
According to the Centers for Disease Control (USA), the use of antiviral drugs Zovirax and Valtrex by women during pregnancy was highly effective in preventing infection in newborns and did not adversely affect the development of the fetus. (Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
(Source: Centers for Disease Control, USA, Valaciclovir (VALTREX) and Acyclovir (ZOVIRAX) Pregnancy Registry, December, 1997).
Dynamic monitoring : Examination of pregnant women includes a mandatory three-time ultrasound examination: at 10-14 weeks of gestation, when the thickness of the nuchal space of the fetus is mainly assessed; at 20-24 weeks, ultrasound is performed to detect malformations and echographic markers of chromosomal diseases; an ultrasound examination at 32-34 weeks is performed in order to detect malformations with their late manifestation, as well as for the purpose of a functional assessment of the fetal condition. In the period of 16-20 weeks, blood samples are taken from all pregnant women to study their levels of at least two serum markers: alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG).
Treatment: Only under the supervision and prescription of a doctor! Outwardly, you can use an ointment based on acyclovir. Ointments and creams are over-the-counter products. The ointment does not affect the fetus, because. it is not absorbed into the blood. To prevent rashes 2 weeks before delivery, the doctor may prescribe valacyclovir or acyclovir orally.
Ointments and creams are over-the-counter products. The ointment does not affect the fetus, because. it is not absorbed into the blood. To prevent rashes 2 weeks before delivery, the doctor may prescribe valacyclovir or acyclovir orally.
PROPHYLAXIS DURING DELIVERY:
Treatment of the soft birth canal with polyvidone iodine (Betadine, Vocadine) or other antiseptics during childbirth can reduce the risk of contracting neonatal herpes to Genital herpes - abortion or childbirth?
Many women with recurrent genital herpes wonder how their illness might affect their unborn child.
The editorial office of the server received a letter describing a typical example of the illiterate approach of Soviet doctors to the management of pregnant women with genital herpes:
Professor D ***, from the Chelyabinsk Medical Academy, believes that it is highly undesirable to keep the pregnancy during an exacerbation of genital herpes in the early stages of pregnancy. He believes that it is necessary to achieve remission within 6 months before the onset of pregnancy. What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
What other schools in Russia consider it possible to maintain pregnancy in the event of an exacerbation (manifestation, relapse) of genital herpes in the early stages of pregnancy. They say that this threatens the deformity of the child and other problems. How to proceed. Get another course of treatment. do not want to risk. There are no good specialists in the city, No one can really answer my question. Being pregnant (4-5 weeks) passed tests for herpes. I suspected that I had herpes, because. and before pregnancy there were rashes and tests confirmed my worst assumptions. After that, I had an abortion. How do you think, what threatens the child with the manifestation of herpes in the first months of pregnancy.
In developed countries, the optimal tactics for managing pregnant women with genital herpes has long been developed, based not on the private opinion of some “Professor D *** from the Chelyabinsk Medical Academy”, but on the data of long-term clinical studies and observations.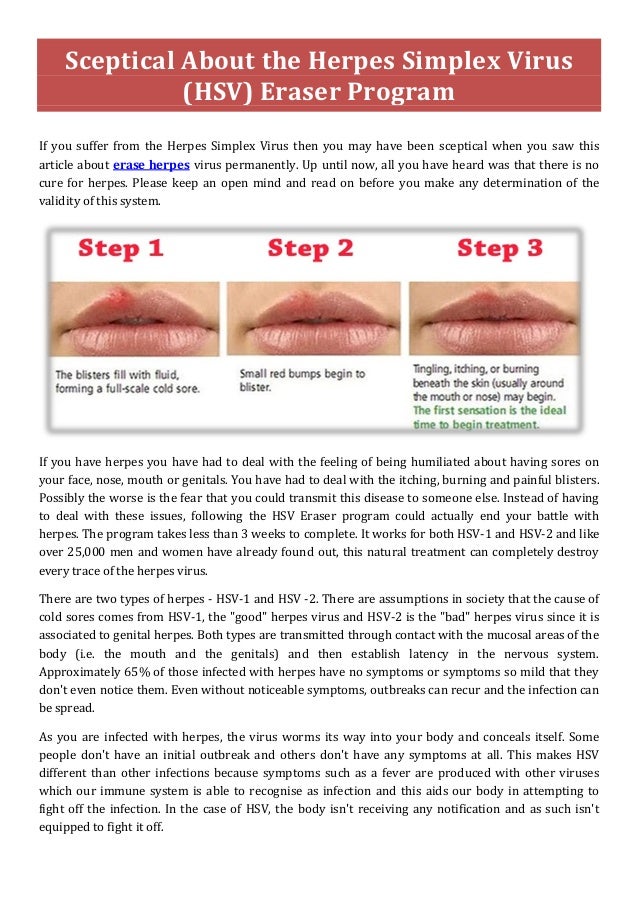
So that someone's subjective opinion does not lead you to an unnecessary abortion, we will tell you once again about what to do if you have herpes and pregnancy.
If a woman has the first time in her life Genital herpes recurs during pregnancy (primary genital herpes) or if the mother-to-be becomes infected with genital herpes during pregnancy, the fetus may be affected. The fact is that in this case, the mother's blood does not contain antibodies to the Herpes Simplex Virus - immunoglobulins G and Em (Ig G and Ig M), which block the pathological effect of the herpes simplex virus on fetal cells.
In the case of the first recurrence of genital herpes in a woman's life, the virus can penetrate the placenta and multiply in the tissues of the embryo or fetus, which leads to fetal death, miscarriage, congenital deformities, damage to the brain, liver, and other organs of the fetus, non-developing pregnancy. The risk of fetal damage in primary genital herpes is 75%.
If the first recurrence of genital herpes occurs 30 days before delivery, delivery by caesarean section is recommended.
From 36 weeks of pregnancy, a doctor may prescribe Zovirax tablets to prevent the recurrence of herpes.
To prevent infection with genital herpes during pregnancy, it is imperative to use a condom and avoid oral sex, i.e. a man should not caress the sexual organs of a pregnant woman with his mouth. The reverse situation is allowed.
If a woman had recurrences of genital herpes before pregnancy, then antiherpetic antibodies float in the pregnant woman's blood, which limit the infection and neutralize the virus. These antibodies pass through the placenta to the fetus, protecting it. Therefore, recurrent genital herpes is not so dangerous during pregnancy. In this case, due to herpes, there are no deformities and lesions of internal organs.
In recurrent genital herpes , the baby can become infected during childbirth, passing through the birth canal, where the herpes virus is present. The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
The risk of infection is 2 to 5%. Treatment of the birth canal and skin of a child with antiseptics containing polyvidone-iodine reduces the risk of developing neonatal herpes to 1-2%. To prevent the development of neonatal herpes from the 36th week of pregnancy, your doctor may prescribe you Zovirax.
Recurrent genital herpes is not an indication for abortion.
And despite all our clarifications about the relative safety of recurrent genital herpes during pregnancy, sometimes you have to receive such letters: A woman with recurrent genital herpes writes: “And most importantly, herpes is just natural selection. Nature removes lepers, because their offspring are doomed to death, so I don’t even dream of children ... ”It is ignorant to consider yourself a leper and refuse the happiness of motherhood just because you have recurrent genital herpes (the most favorable form for bearing and childbirth). Although, it cannot be ruled out that this is our medical defect.
There is also such a diagnosis as non-primary genital herpes . What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
What does this mean? Before pregnancy or during pregnancy, the woman was sick with recurrent genital herpes, which was caused by the herpes simplex virus type II. During pregnancy, the husband practiced cunniling (caressing the female genital organs with the mouth). As a result, the Herpes Simplex Virus type I (HSV-I) can enter the female genitalia. Another option is also possible: Before pregnancy, a woman suffered from genital herpes caused by HSV-I, became infected during oral sex. During pregnancy, her sexual partner rewards her with HSV-II. To I or II type of virus, respectively, there are no antibodies. As a result, the clinical picture may be the same as with primary genital herpes. Therefore, it is important to use condoms during pregnancy and not to practice cunnilingus.
The use of immunomodulators during pregnancy
The server editor received a letter describing a typical clinical situation:
« I have a problem that requires urgent consultation. My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
My obstetrician - gynecologist says that everything is fine, but I'm restless. For the second time during pregnancy (now the 31st week) I have a herpes rash on my lip, the gynecologist insisted on a course of Ridostin, and I have already made 1 injection, but the contraindications to the medicine say PREGNANCY. My doctor says that they have been treated with Ridostin for a very long time during pregnancy and nothing has happened. I have a question. How serious are the reasons for such contraindications (maybe this is reinsurance?) and should I do the next injection on Sunday?
In my opinion, the use of immunomodulators during pregnancy is IMPOSSIBLE:
* In this case, herpes on the lips of a woman cannot bring any harm to either the woman or the child.
*Long-term effect of immunomodulatory drugs on the fetus is unknown. As you know, some of these drugs, easily penetrating the placenta into the body of the fetus, can cause congenital deformities in the latter, disorders of the immune system, and increase the risk of developing cancer.