Painful let down opposite breast
Pain: General - La Leche League International
IT HURTS WHEN MY MILK “LETS DOWN.” WHAT COULD BE CAUSING THIS AND HOW CAN I REMEDY THIS SITUATION? WHAT IF MY PAIN IS DEEP IN MY BREAST?A painful let-down reflex can occasionally happen while your body adjusts to feeding your baby. You may find that using relaxation techniques that were helpful during labor might help you cope with this early discomfort.
Make sure you are using good positioning techniques and are not straining or leaning over your baby as you are breastfeeding your baby. Your back, arms, feet and elbows should be well-supported, and your shoulders and neck muscles relaxed.
Some deep breast twinges during let-down can occur as the milk ducts constrict to force the milk toward the nipple. As your body becomes more used to breastfeeding, these disappear.
There can be several other causes of painful let-downs that you may want to consider:
- Lots of milk. Some nursing parents find they make a great deal of milk and/or their milk-ejection reflex (let-down) is very strong.
If this is the case, you will notice your baby choking or sputtering on the volume and intensity of the milk as it is let-down. Breastfeeding only on one breast per feeding can be helpful. When your milk lets down, you may find that your baby is more comfortable if you gently break suction, allow the milk to spray into a towel, and then re-latch when the flow slows down. In time, your supply and let-down will become more manageable for the baby to handle and your discomfort should lessen.
- Yeast. Another cause of painful let-down may be yeast (a candida yeast infection) that has entered the milk ducts of the breasts. Please note that it has been suggested by some researchers that thrush cannot spread in milk ducts. Contact your local La Leche League Leader or your health care provider if you suspect you have yeast.
- Engorgement. Engorgement can cause breast discomfort.
- Muscle strain or injury during birth. Straining or injuring chest muscles which support the breasts may also cause what seems to be deep breast pain.

- Breast infection or plugged ducts. Sometimes pain can be an indication of a breast infection or clogged ducts. This may occur when milk is not sufficiently removed from the breast in a timely manner, or when an injury to the nipple allows bacteria to enter the breast. If you have a fever, red streaks on your breasts, or if you feel like you have the flu, contact your health care provider to rule out a case of mastitis, which is an infection of the breast, and can require an antibiotic for healing. Clogged ducts can feel like a pea or string embedded deep within the breast; it is milk that is trapped in the breast and can’t get out. In either case, you should continue to nurse a lot, rest a lot and drink a lot of fluids.
Several other causes of deep breast pain (not necessarily during let-down) are:
- Vasospasms and/or Raynaud’s Syndrome
- Improper breast pump usage
- An ill-fitting bra
- Injury or surgery to the breast tissue
- Premenstrual pain
- Fibrocystic breast pain
Also, some mothers with very large breasts have experienced deep breast pain.
One other cause of deep breast pain or painful let-down is that the baby might be clamping down instead of suckling. You will not hear the baby doing much swallowing if this is the case. Your local LLL Leader can help you review good latching and sucking signs.
Breastfeeding without pain is important not only for the comfort of the nursing parent, but also for your baby. Pain is typically a sign that something is not going well. Resolving your pain goes a long way toward your baby getting sufficient milk and your milk production remaining strong so you can meet your breastfeeding goals.
Is It Normal to Hurt Like This?
You’ve got your latch figured out, your baby isn’t biting, but still — hey, that hurts! It’s not something you’ve done wrong: A painful letdown reflex can sometimes be part of your breastfeeding journey.
But the good news is that as your amazing body adjusts to this new role, the letdown reflex should become painless. If not, something else may be wrong. Let’s look at what you should know.
Let’s look at what you should know.
Think of the letdown reflex as an intricate dance in which you and your baby are partners. Your body responds to input from your baby when they begin to feed or cry out in hunger. Sometimes even thinking about nursing them, touching your breasts, or using a pump can begin the process.
When your body gets the signal from your baby it triggers the nerves in your nipple and areola. These nerves send messages to the pituitary gland in your brain signaling it to release oxytocin and prolactin into your bloodstream.
So what do these hormones do? Prolactin signals the alveoli in your breast to remove the sugars and protein from your blood and produce more milk.
Oxytocin makes cells around the alveoli contract and push the milk into the milk duct. Oxytocin also widens the milk ducts so that the milk can flow more easily.
Your milk actually lets down several times during one feeding session, but you’ll probably only feel the first time. Some moms feel the letdown reflex seconds after their baby begins to suck. Some feel it only after a couple of minutes. And some don’t feel anything at all.
Some moms feel the letdown reflex seconds after their baby begins to suck. Some feel it only after a couple of minutes. And some don’t feel anything at all.
Like everything in our bodies, there isn’t an exact timetable or expectation to follow.
Here’s what you might notice:
- A tingling sensation sort of like pins-and-needles. And, yes, it can be disconcertingly intense and even painful. Some moms feel this only in the early days of breastfeeding and then the feeling fades. Others feel letdown during each feed throughout breastfeeding.
- A sudden fullness or warmth.
- Dripping from the other breast. Keep breast pads handy because letdown usually happens simultaneously in both breasts.
- An adjustment in your baby’s sucking rhythm as they change from short, quick sucks to longer paced-out sucks when the milk flows and they start to swallow.
- A sudden thirst. Researchers aren’t sure why this happens, but it may be due to the release of oxytocin.

There’s a lot going on in your body when letdown happens. Since we’re each unique in our experience of and response to pain, it’s not surprising that some people feel more discomfort than others.
Remember that it can take some time for your body to adjust to the new sensation. Over time, many breastfeeding parents notice less discomfort during letdown.
That said, there are several causes that can make letdown painful. Happily, there are also solutions.
Forceful letdown
If too much milk flows quickly out of your breast, it can cause pain during the release. Additionally, it can causes issues as your baby will struggle to swallow it all.
Try these tricks to slow down the flow:
- Use your hand or a breast pump to express some milk and capture the first letdown before you settle down to breastfeed.
- Work with gravity. Recline or lay on your back and put your baby on your chest to feed. Your milk flow will be slower with your baby sucking against gravity.
- Alternate breasts at each feeding.
Engorgement
Your body is hard at work learning to produce milk in the quantities your baby needs. Until it learns, you may find that supply exceeds demand. If your breasts are hard and swollen, the letdown reflex can be more painful.
If this is happening to you, consider:
- Expressing a small amount of milk to ease the tenderness. Using a warm compress or expressing milk in the shower can help soften the breasts.
- Applying cold cabbage leaves to your breasts between feeding sessions. Why? It may be that plant compounds in the cabbage have anti-inflammatory effects that can help reduce swelling. Favor green cabbage over purple so that you don’t stain your clothing.
- Feeding regularly. Skipping feeds can increase engorgement.
Clogged milk ducts
Milk that’s trapped in the breast and cannot get out will let you know that it’s there. You may feel pressure and a hard lump in your breast or underarm area where the milk is clogged or blocked.
If you suspect a blocked duct:
- Try to release the blockage with warm compresses, hot showers, and gentle massage.
- Increase your feedings and massage gently at the blockage while your baby is nursing. It works wonders.
- Experiment with different feeding positions to release the clog.
- Begin each feed on the affected breast.
Blebs
Sometimes, you’ll notice small white spots on your nipples at the end of a milk duct. These “milk blisters” or “blebs” are filled with hardened milk. Just as with clogged milk ducts, you can release the milk using with warm compresses and hot showers.
Mastitis
Noticed red streaks on your breast? Feel like you have flu and that you need some chicken soup? It may be mastitis, a breast infection. Sometimes a clogged duct or other issue can lead to an infection in the breast.
Don’t try to treat this on your own because a breast infection can require antibiotics. It’s important that you see your doctor or midwife for prompt treatment.
In the meantime, you can follow the suggestions above for a clogged duct to alleviate discomfort. Continue to breastfeed and rest as much as possible.
Sore nipples
Check that your baby is latching on correctly. If they aren’t your nipples will most likely become red, sore, and cracked. The discomfort from sore nipples can intensify during letdown.
If you’re struggling with sore nipples:
- Promote healing by dabbing some of your breast milk, lanolin, olive oil, or coconut oil onto your nipples after each feed.
- Experiment with different holds.
- Use cool compresses to reduce swelling.
- Seek assistance from a lactation consultant to improve your latch.
Thrush
This yeast infection is usually caused by a fungus called Candida albicans. It can make nipples appear red or shiny, or they may not look any different than normal. It can also make your nipples crack and hurt horribly.
If you feel burning, itching, or sharp shooting pains, you may have thrush. Since thrush spreads very easily, it’s most likely that your baby has thrush too. Peep into their mouth. A white, stubborn coating on the gums or the inside of your baby’s cheeks will confirm your suspicions. Keep in mind that it is normal to see a thin coating of milk on your baby’s tongue.
Since thrush spreads very easily, it’s most likely that your baby has thrush too. Peep into their mouth. A white, stubborn coating on the gums or the inside of your baby’s cheeks will confirm your suspicions. Keep in mind that it is normal to see a thin coating of milk on your baby’s tongue.
Turn to your medical practitioner for help as both you and your baby should be treated with antifungal medication.
Vasospasms
Vasospasms can happen in different parts of the body when the blood vessels tighten and go into spasm, preventing the blood from flowing normally. When this occurs in the nipple area, you’ll feel sharp pain or stinging in the nipple.
Vasospasms can happen from exposure to the cold or simply because your baby isn’t latching on correctly.
If you’re feeling vasospasms in the nipple:
- Try warming up your breasts using breast warmers or a gentle olive oil massage.
- Check to ensure you have a good latch. See a lactation consultant if needed.

- Talk to your medical practitioner about supplements or medications that may help.
Injury
Giving birth can strain all sorts of muscles, including the chest muscles that support your breasts. This injury can intensify pain felt during the letdown reflex.
Uterine contractions
We’re back to oxytocin. This multifunctional hormone also makes your uterus contract, especially in the first week or 10 days after birth. The good news is that this is a sign your uterus is returning to its normal size and place. The not-so-good news is that these contractions can get harder and last longer with each subsequent birth.
These contractions can become more painful during letdown. If you’re in pain due to uterine contractions:
- Use a heating pad to reduce discomfort.
- Consider taking acetaminophen (Tylenol) or ibuprofen (Advil).
The hours that you and your baby spend snuggling down to breastfeed are probably some of the most precious hours that you’ll spend together. Here’s what you can do to maximize your comfort.
Here’s what you can do to maximize your comfort.
Easing the letdown reflex
- If you take a warm shower or bath before you breastfeed, you’ll give your letdown reflex a head start. Don’t be surprised if your milk starts dripping before you get dry!
- Short on time? Press a warm, wet towel to your breasts or massage them gently.
- Relax. Sit or lie down and breathe out the stress. You deserve to enjoy this.
- Undress your baby and place them on your chest skin-to-skin with you.
- Cuddle your baby and breathe in that sweet baby smell.
- Condition yourself. Your body will learn to respond to cues that you associate with breastfeeding. Follow a set routine before you start: make a cup of tea, put on some soft music, and breathe deeply.
General tips
- It’s hard to time feedings, especially at first. But you can try to take acetaminophen or ibuprofen 30 minutes before feeding time to ease pains.
- Invest in comfortable nursing bras.
 They’re the tools of the trade and can help avoid pain and clogged ducts.
They’re the tools of the trade and can help avoid pain and clogged ducts. - Invest in a rocking chair or other comfortable spot to breastfeed.
- Work with a lactation consultant to solve persistent problems.
- Keep a bottle of water handy so you can stay well hydrated.
It’s not just you. At first, the letdown reflex can be a real pain in the breast. Hang in there because this pain should be temporary.
But don’t ignore symptoms or signs that the discomfort you’re feeling could be something more. And don’t forget to slip your breast pads into your bra or else you may find that the front of your shirt is suddenly wet.
90,000 how to get rid of back pain on your own. Back pain, as a possible manifestation of many, often dissimilar diseases, is today such a common complaint among our environment that it seems that almost everyone suffers from the same sore. This feeling is close enough to the truth - indeed, 85% of the world's population suffers from back pain, but the source of this pain is different.
Unquenchable pain will definitely appear at some stage of the oncological process in the spine itself, and will only manifest itself as fatigue after non-traumatic, but monotonous and long-term physical work in a healthy person. It can sharply worsen after an awkward lifting of heavy weight, so much so that for several days it will be impossible to get to the toilet on your own. In an absolutely amazing way, defying any reasonable explanation, the back can ache after a strong nervous shock, and how can one not think about someone's curse, evil eye or damage? It can lead to both rheumatism and some infectious and viral diseases. It may be “reflected” and indicate a disease of some internal organ, or it may, quite naturally, be simply the result of a direct back injury. Therefore, the complaint “My back hurts ...” sounds both in the office of a traumatologist and in the offices of a neuropathologist, gastroenterologist, orthopedist, surgeon and many other doctors more often than other, specific complaints with which patients turn only to a surgeon or only to a neuropathologist. To paraphrase the classic, we can say that all healthy people are equally healthy, but sick people get sick in different ways.
To paraphrase the classic, we can say that all healthy people are equally healthy, but sick people get sick in different ways.
Many-sided, understandable and incomprehensible, it can appear in a perfectly healthy person due to a long stay of one of the joints in the extreme position of flexion or extension.
It is quite possible that you had to whitewash the ceiling in your apartment, after which, the next day, you probably had at least a little neck pain. Why did this pain occur? Because of illness? Well no. Just by throwing your head back for a long time, you brought the joints of the cervical spine into a state of excessive extension. The joint capsules were unnecessarily stretched in an unusual direction for them, as a result of which pain arose in a healthy joint.
The true source is sometimes so carefully masked by a variety of symptoms that, imitating other diseases, causes serious diagnostic difficulties for doctors.
An incomprehensible patient, a young man of twenty-six years old, appeared in the traumatology department of one of the Moscow clinics. In the department, he treated his compound fracture of the lower leg, which he received while drunk. The bone fragments were compared and the fracture healed successfully. However, a week after admission, he began to complain of severe pain in his back and right side, turned pale, and began to moan. The nature of patients in trauma departments is quite typical - most often they are people who got their injuries "drunken", so the attending physician, accustomed to such a turn of affairs, suspected delirium tremens in his patient (a common thing) and called a psychiatrist-narcologist for a consultation.
In the department, he treated his compound fracture of the lower leg, which he received while drunk. The bone fragments were compared and the fracture healed successfully. However, a week after admission, he began to complain of severe pain in his back and right side, turned pale, and began to moan. The nature of patients in trauma departments is quite typical - most often they are people who got their injuries "drunken", so the attending physician, accustomed to such a turn of affairs, suspected delirium tremens in his patient (a common thing) and called a psychiatrist-narcologist for a consultation.
The overweight and short of breath narcologist rejected “his” disease “out of the blue” and, after talking with the sick guy for a couple of minutes, in an unreadable underline wrote a whole novel in the case history, from which it followed that the patient had no delirium tremens. Meanwhile, the next temperature measurement showed an increase to 37.3 ° C, and the area of the focus expanded somewhat.
Having smoked a couple of cigarettes in the staff's room, an impromptu consultation, consisting of two traumatologists and an anesthesiologist who accidentally ran into them "on the light" decided to call a urologist for a consultation. The professor of urology came accompanied by two assistants and ten students. The consultation was held in the ward with all the luxury of a theatrical lecture, as a result of which a positive diagnosis was made - renal colic. However, objective studies conducted an hour later disproved this diagnosis.
The situation was becoming alarming. The head of the traumatology department joined in solving the problem. With a broad gesture, he called for a consultation with his friends-managers - a therapist and a surgeon. Imbued with the seriousness of the problem, not wanting to get into an absurd position, like an overly self-confident urologist, they examined, questioned and probed the patient for a long time, studied the analyzes that had accumulated by that time and thoughtfully “clicked” with their tongues.
The therapist spread his hands, and the surgeon suggested developing inflammation of the pancreas ("After all, the drinking guy ..."). However, here, too, objective research methods did not confirm this assumption. The “drinking guy” was getting heavy before his eyes, his back pain intensified, his temperature remained at the same alarming and suspicious numbers. He groaned softly, and grimacing heavily, swearing tiredly.
The next day, a venerable group of all the leading specialists of the hospital gathered in the smoky trauma intern's room. They drank tea with cognac, played chess, smoked, remembered their youth, made thoughtful assumptions about a strange patient with a wild mixture of Latin and truly Russian expressions, prescribed tests, and after waiting for their results, made new assumptions. Tired of the hospital routine, elderly doctors took the incomprehensibility of the disease as a challenge to their professionalism.
A vascular surgeon invited from the central venerable clinic suggested the development of thrombosis (impaired patency) of the arteries supplying the intestines, and an orthopedist respected throughout the country suggested a prolapse of an intervertebral disc herniation that appeared simultaneously with a leg injury, but this, like many other things, was refuted by x-ray data, ultrasonography and ingenious blood tests.
After a couple of days of doctors' stay in complete bewilderment, the problem resolved itself - on the skin of the back, where the patient had pain, rashes of shingles appeared.
As you can see, the problem of a sore back can be so ambiguous that it can be difficult to understand it even for a whole council of highly qualified doctors. Therefore, in this book we will not talk about diseases, but about that banal back pain that can appear when doing routine household chores, sitting for a long time at a student desk or computer, and uncomfortable tilting of the body. In other words, let's talk about pain that is concentrated in the ligaments and muscles of the back.
A bit of history
Traditionally, since the Old Testament times, the banal pain in the back, which appeared after an unsuccessful turn or heavy lifting, was treated by a chiropractor. In the writings of ancient Rome there is a story about a famous free gladiator named Kazanasta, who suffered from pain in his shoulder after falling from a chariot. He was cured by the famous Claudius Galen, a doctor of gladiators, who, according to today's table of ranks, apparently could be attributed to traumatologists. Galen kneaded his patient's back, pulled his neck, massaged his shoulder, after which the pain disappeared, and Kazanasta returned to his sweet pastime. It follows from this and many other stories that the doctors of the ancient world were quite successful in dealing with the problem.
He was cured by the famous Claudius Galen, a doctor of gladiators, who, according to today's table of ranks, apparently could be attributed to traumatologists. Galen kneaded his patient's back, pulled his neck, massaged his shoulder, after which the pain disappeared, and Kazanasta returned to his sweet pastime. It follows from this and many other stories that the doctors of the ancient world were quite successful in dealing with the problem.
The active Christianization of Europe prevented the spread and improvement of this skill. In the Middle Ages, during the era of the Holy Inquisition, curiosity was considered heresy, and all inquisitive people, usually on Saturdays, with a general gathering of people, in the main square, were burned at the stake. Therefore, in those twilight times, many scientific directions stopped in their development. However, due to the constant traumatic epidemics - wars, the need to eliminate pain in the joints and muscles was exceptionally high. That is why certain techniques of chiropractors were still preserved in the hands of medieval doctors who knew how to set dislocations of the joints of the limbs, and who considered this exclusively their professional work.
That is why certain techniques of chiropractors were still preserved in the hands of medieval doctors who knew how to set dislocations of the joints of the limbs, and who considered this exclusively their professional work.
In a more visible era, when a cohort of orthopedists and traumatologists emerged from universal doctors, work on the joints and muscles of the limbs became an obligatory part of their narrow specialization. However, conservative, therapeutic treatment of the back remained the lot of the underground work of healers.
As recently as thirty years ago, a patient with a chronic back problem was the most disliked patient among neurologists. We, today, have only to be surprised at the amazing limitation and deformation of the then professional consciousness, which rejected real methods of eliminating back pain.
In the late 1970s, an elderly, nationally renowned professor of neuropathology received a patient in her office in the presence of several residents, novice doctors. The patient was a young man in his thirties who complained of constant pain radiating to his right buttock and thigh. His suffering had lasted for several years, during which he managed to be treated by many neuropathologists, but the disease, having stopped a little, continued to torment him, and each time with a new passion. "Cute!" - the professor's wife told him after the examination - "Darling! And don't try harder... It's not fatal, but It'll never go away. It will always hurt, so stop worrying and don’t think… It will get a little better, a little worse, but it won’t let go completely… So stop going to the doctors…”
The patient was a young man in his thirties who complained of constant pain radiating to his right buttock and thigh. His suffering had lasted for several years, during which he managed to be treated by many neuropathologists, but the disease, having stopped a little, continued to torment him, and each time with a new passion. "Cute!" - the professor's wife told him after the examination - "Darling! And don't try harder... It's not fatal, but It'll never go away. It will always hurt, so stop worrying and don’t think… It will get a little better, a little worse, but it won’t let go completely… So stop going to the doctors…”
Protected by regalia, position and age, the professor said aloud what any neurologist would like to say to such a patient, but did not dare. I would like to say this because it is a thankless task to fight chronic pain with drugs and massage alone, the main weapon of a neuropathologist. I did not dare to say it because to say it out loud means to sign your professional failure. It must be said that a neuropathologist who is not involved in manual therapy still has a dislike for this category of patients.
It must be said that a neuropathologist who is not involved in manual therapy still has a dislike for this category of patients.
The orthopedists of the seventies also did not like patients with chronic back pain. They, orthopedists, are surgeons by vocation, guys are serious and dashing. They were the first to feel one of the causes of the problem in the literal sense of the word - operating on the spine for intervertebral hernias. Operative access to a hernia of the spine in those years was carried out through the abdominal cavity. This means that in order to “crawl” to the hernial protrusion, it was necessary to open the abdominal cavity, move the intestines away, and then ... The operations were difficult, but interesting, with a large number of complications. However, if there was nothing to operate on, the orthopedist automatically lost all interest in the patient with a bad back and sent him to a neurologist.
Unsettled by the explanation that "It will never pass", offended by the negligence of neurologists and orthopedists, the patients went to the bone-cutting healer. Legends were passed from mouth to mouth about the supernatural ability to treat the back, some village grandmothers or healers, who always live in the Darkness-Cockroach, accept their patients in complete secrecy and raise sick people literally from their deathbed. At what level these folk healers worked is actually unknown. Probably, there were skillful ones among them, who intuitively did not do stupid things, but there were others ... Perhaps the number of positive results of their work was blocked by the same number of failures or complications. Nevertheless, the very fact of pain relief, after manipulations on the joints and ligaments of the spine, aroused interest among professional doctors, and the technique of these manipulations, preserved in the hands of healers, made it possible to overcome the zero cycle of medical ignorance in order to further improve and develop methods of conservative treatment of the patient. back. One of the ways to get rid of back pain on your own will be discussed in this book.
Legends were passed from mouth to mouth about the supernatural ability to treat the back, some village grandmothers or healers, who always live in the Darkness-Cockroach, accept their patients in complete secrecy and raise sick people literally from their deathbed. At what level these folk healers worked is actually unknown. Probably, there were skillful ones among them, who intuitively did not do stupid things, but there were others ... Perhaps the number of positive results of their work was blocked by the same number of failures or complications. Nevertheless, the very fact of pain relief, after manipulations on the joints and ligaments of the spine, aroused interest among professional doctors, and the technique of these manipulations, preserved in the hands of healers, made it possible to overcome the zero cycle of medical ignorance in order to further improve and develop methods of conservative treatment of the patient. back. One of the ways to get rid of back pain on your own will be discussed in this book.
New handy doctor - chiropractor
So, a specialist who treats back pain is today called a chiropractor. Manus is Latin for "hand". Hence the name - manual, that is, one that heals with hands.
The first graduation of certified chiropractors in Russia took place in 1982. For many years the status of these specialists, within the medical "coterie", was very uncertain and only in 19In 1998, the chiropractor was officially included in the register of medical specialties and became a full-fledged doctor, such as a neurologist, therapist and surgeon.
There are over 18,000 chiropractors in Russia today, and this army continues to grow as the demand for back pain relief increases every day. According to American chiropractors and osteopaths (as chiropractors without medical education are called in America), in the United States, over the past 10 years, the need for specialists who eliminate back pain has increased 163 times! There is no reason to think that this need is less in Russia.
In Russia, unlike many countries of the world, only a doctor can be a chiropractor. The spectrum of knowledge is very large and has an integrative (systemic) character. Due to the fact that manual medicine is located at the intersection of neurology, orthopedics, rheumatology and physiotherapy, the need to master the basics of these disparate disciplines is at the center of their education. The difficult task is made easier by the fact that doctors entering manual medicine usually already have a specialization and experience in one of these disciplines.
A good chiropractor is not just a healthy, muscular guy who knows how to “crunch” his vertebrae, but a clinician with a broad professional outlook and deep clinical thinking. This medical specialization provides the aspiring physician with the opportunity to realize the Art in his work. Unfortunately, many other narrow specialists were forced to forget about art in medicine, whose professional freedom is enslaved by a huge amount of diagnostic and medical equipment, in which they are just laboratory assistants. Unlike the elements of industrial, computerized medicine, nothing can replace the live, skillful, warm human hands of a chiropractor!
Unlike the elements of industrial, computerized medicine, nothing can replace the live, skillful, warm human hands of a chiropractor!
The technique to which this book is devoted, developed just by chiropractors, is used by them both as a separate type of treatment and as preparation for manipulations on the spine.
The problem of pain
One of the obligatory symptoms of back pain is muscle tension. At the moment of exacerbation, the patient himself says that he cannot relax, that is, relax entire muscle groups, tense by the will of some kind of evil fate. At this moment, his posture takes on a strange, bizarre configuration, which is held together by tense muscles. This protective reaction of the muscle sheath is similar to a splint that is applied to the fracture site in order to prevent the displacement of fragments.
It follows that the muscle is not a fool to strain just like that - it begins to work in such a debilitating mode when a certain, painful impulse comes to it - a sign of the vital need to limit the range of motion in a certain place in our body. In this case, after a few hours, the muscle itself becomes the main source of pain.
In this case, after a few hours, the muscle itself becomes the main source of pain.
Since ancient times, long before the ancient Hippocrates, it was found that by mechanical stretching of a tense muscle, a person can get rid of pain on his own. Most people know how to get rid of pain in the calf muscle, which often occurs during long swimming. To do this, the swimmer grabs the toes and pulls them in such a way as to bend the foot towards the front surface of the lower leg. With this movement, the soleus (calf) muscle is stretched along the length, as a result of which the pain that has arisen in it disappears.
This method is suitable for any muscle in our body, therefore, knowing the specific points of application of their efforts, you can significantly alleviate your back pain, at least until you go to the doctor.
Pain Relief Principle for a Tight Muscle
It's very simple. In any case, none of my patients have had problems mastering these simple techniques, but first you need to understand the very principle of manipulation.
A muscle always attaches itself to various bones with its ends in order to contract and bring them closer together. The bones are connected to each other by a joint, which is the center of this movement.
Painful, contracted muscle is always shortened, and stretching it is painful. But if you first cause a slight tension in this muscle, without shortening it in length, and then its relaxation and slow stretching, then the painful tension in it will disappear.
However, in the event of pathological, that is, disease-causing processes, not one muscle contracts, but a whole complex of the most diverse and often quite distant muscles. Therefore, for the most accessible description of pain relief techniques, we will not delve into the anatomy and physiology of muscles, we will focus on the presence of certain symptoms.
Perhaps such an approach is a simplification, but an ordinary person, not burdened with knowledge of medical terms, very quickly gets tired of a thorough description of anatomical and physiological parameters, laws and conditions that are not interesting for him. For an ordinary person, the main thing is to quickly achieve a result, in this case, an anesthetic, and I would redirect those who are especially interested to professional literature.
For an ordinary person, the main thing is to quickly achieve a result, in this case, an anesthetic, and I would redirect those who are especially interested to professional literature.
And now let's move on to the study of the subject.
Imagine that you have thrown a square scarf over your shoulders with the ends up, down and to the sides. The projection of the tissue that covered your shoulders and a triangular flap - part of the neck and back, corresponds to the so-called trapezius muscle. This muscle throws the head back, pulls it to the sides, raises the shoulders, raises and lowers the shoulder blades. It begins to hurt when articular problems arise, both the cervical spine and the thoracic. The pain is very characteristic and probably many are already familiar with it: it occurs and worsens when the head is tilted forward, it can stretch from the middle of the back to the back of the head, or it can “sip” part of the neck when tilted to the opposite shoulder, and even “give” to the upper part of the shoulder blade .
What to do
The procedure is best done in a sitting position.
As you exhale, put your clasped hands on the back of your head and with your own hands tilt your head slightly forward until an unpleasant sipping pain appears in the back of the neck or the symptoms that I have just described.
Begin to inhale slowly, at the same time slightly extending the neck, but preventing this extension with the hands. As a result of this confrontation, tension will arise in the trapezius muscle, but movement, that is, extension of the neck, at this stage, should not occur.
Holding your breath for 5-7 seconds, exhale slowly. Together with a slow exhalation, just as slowly relax, at the same time tilting your head down with your hands, to the level at which pulling pains again appear on the back of the neck or between the shoulder blades.
With the beginning of the next inhalation, repeat everything, but with an exhalation, try to lower your head a little lower than the last time. If done correctly, it should happen on its own. As the trapezius muscle relaxes, you will be able to move more, and as the pain begins to recede, you will be able to painlessly lower your head much lower than at the beginning of the session (but don’t get carried away - not below your own knees!).
If done correctly, it should happen on its own. As the trapezius muscle relaxes, you will be able to move more, and as the pain begins to recede, you will be able to painlessly lower your head much lower than at the beginning of the session (but don’t get carried away - not below your own knees!).
A few notes about
With what force do you press the back of your head on your hands, and with what effort do you resist your own head with your hands? With a similar question, but regarding professionally performed manipulations, my colleague once turned to the patriarch of manual medicine, a Czech professor, Karel Levit. In response, Levit rested his index finger on his relaxed shoulder and slightly pressed, while his finger, significantly immersed in the relaxed deltoid muscle of the shoulder, slightly bent at the joint of the nail phalanx.
However, this vague description of effort will be incomprehensible to many readers: what does it mean slightly? And where to look for this deltoid muscle, and who is this “phalanx”?
Try to bend the auricle with your index finger until it touches the skin of the temple - this is THAT effort. This effort can also be compared to a light morning sip on the first day of a long-awaited vacation. However, for those who are not satisfied with these comparisons, I propose to exert muscle tension of such strength, as if you were not paid money for it.
This effort can also be compared to a light morning sip on the first day of a long-awaited vacation. However, for those who are not satisfied with these comparisons, I propose to exert muscle tension of such strength, as if you were not paid money for it.
There is one more clarification that will significantly affect the effectiveness of your independent and irreconcilable struggle with pain. While inhaling, you need to raise your eyes up, as if you want to look at the ceiling, which your lovely neighbors from above flooded yesterday. This small addition will qualitatively improve the extension movement itself, and it will not strengthen it, but it will improve it - the movement will become more solid and organic.
You can feel the importance of this friendly eye movement with the help of a simple exercise. Turn your head to the side until it stops in such a way that further, with muscle effort, the head could no longer turn. But one has only to look in the same direction over the shoulder, as the head turns a few more degrees. In addition, with the help of a friendly movement of the eyes, the image of the characteristic movement is “imprinted” into the brain, which significantly increases the effectiveness of the procedure.
In addition, with the help of a friendly movement of the eyes, the image of the characteristic movement is “imprinted” into the brain, which significantly increases the effectiveness of the procedure.
The same applies to breathing during muscle tension and relaxation. In order to feel the importance of friendly breathing, try to do the above exercise without the help of hands and without muscle tension. Relax your neck so that it hangs limply on your chest. Take a slow deep breath and feel how, as the air is drawn into the chest, the muscles of the back of the neck will stretch slightly, and the head will rise slightly. With an exhalation, this tendency will be reversed - dragged by gravity, the head will sink even lower than before, stretching with its weight the already relaxed muscles of the neck.
And now, having convinced yourself of the effectiveness of the friendly movement of the eyes and breathing, feel how harmoniously all these movements are combined: inhalation, extension, “eyes to the ceiling” and the subsequent exhalation, flexion and “eyes to the floor”.
Last but very important update
The muscle relaxation phase in all muscle relaxation procedures should be very smooth and evenly slow. Rapid or uneven relaxation will drastically reduce the effectiveness of the procedure.
All of the above clarifications significantly affect the effectiveness of your fight against pain. Observe them. Otherwise, small retreats will negate all your big efforts.
A small addition to the main procedure that eliminates pain on the back of the neck can be two more exercises that are desirable to perform after the manipulations described above.
The first exercise is the mobilization of the joints between the occipital bone and the first cervical vertebra. Mobilization, in this case, means the improvement of mobility. To do this, while sitting, take the starting position: without bending your neck, turn your head to the side as far as it will go, and your eyes should look straight ahead. From this position, make a quick, short nod down, while exhaling and lowering the eyes “to the floor” and instantly returning to the starting position.
Similarly, from the same starting position, an upward nod is made, followed by an inhalation, eye movement "to the ceiling" and a quick return to the starting position. These two nods should be done alternately, 3-4 times each.
Following this, another short and very pleasant exercise should be done. Clasp your hands in a lock and put them on your neck so that the connected little fingers of both hands are under the back of your head. Relax your hands and feel their pleasant heaviness. From this position, turn your head VP
Breast prolapse: treatment of breast ptosis
Health Blog
POPULAR ARTICLES
Articles 04/13/2021 TOP 10 of your questions about botulinum therapy
For the first time you thought about injections of botulinum toxin, more often…
Read more
Articles 29.10.2020 Important questions about nutrition
How to understand the topic of nutrition and choose nutrition,…
Read more
Articles 10/13/2020 What is SMAS lifting with Liftera?
Every woman after 40 wants to look as young as…
Read more
10/30/2018
For most women, breast prolapse is a serious aesthetic problem that prevents them from loving their own body and causes complexes, so the issue of treating breast ptosis is especially relevant.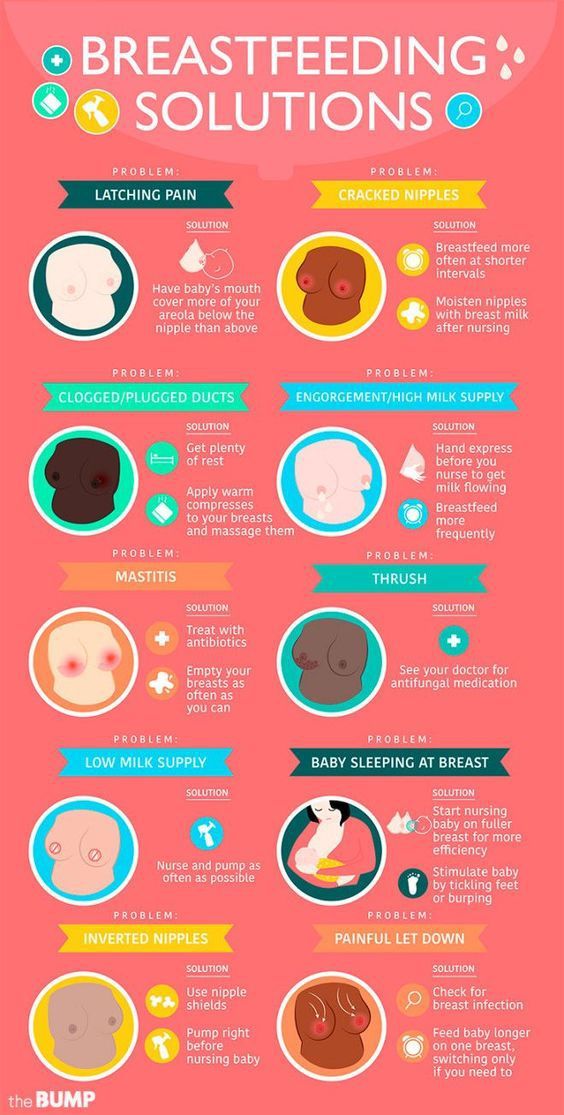 Involutionary aging processes, genetic predisposition and every minute impact of the Earth's gravitational forces contribute to the natural ptosis of the skin, body tissues and some internal organs. If we are talking about prolapse of the mammary glands, then in medicine it is called " mastoptosis ". With mastoptosis, a woman's breasts lose their elastic shape and look sagging. Special care for preventive purposes only helps to slow down the process of breast prolapse. It includes: a contrast shower, massages, body wraps, cosmetics, mesotherapy, biorevitalization of the breast skin, as well as some other salon procedures. However, with severe mastoptosis, conservative methods are no longer effective. In this article, we will talk about possible ways to treat ptosis of the mammary glands. The fastest and most effective of them is still mastopexy (mammopexy) - plastic surgery to lift the mammary glands with or without implants. But first, let's look at why the chest sags at all: what factors contribute to this?
Involutionary aging processes, genetic predisposition and every minute impact of the Earth's gravitational forces contribute to the natural ptosis of the skin, body tissues and some internal organs. If we are talking about prolapse of the mammary glands, then in medicine it is called " mastoptosis ". With mastoptosis, a woman's breasts lose their elastic shape and look sagging. Special care for preventive purposes only helps to slow down the process of breast prolapse. It includes: a contrast shower, massages, body wraps, cosmetics, mesotherapy, biorevitalization of the breast skin, as well as some other salon procedures. However, with severe mastoptosis, conservative methods are no longer effective. In this article, we will talk about possible ways to treat ptosis of the mammary glands. The fastest and most effective of them is still mastopexy (mammopexy) - plastic surgery to lift the mammary glands with or without implants. But first, let's look at why the chest sags at all: what factors contribute to this?
Causes of breast ptosis
The volume and appearance of the female bust is determined by: the state of the pectoralis major muscle and ligaments, the ratio of adipose and glandular tissue formed into lobules.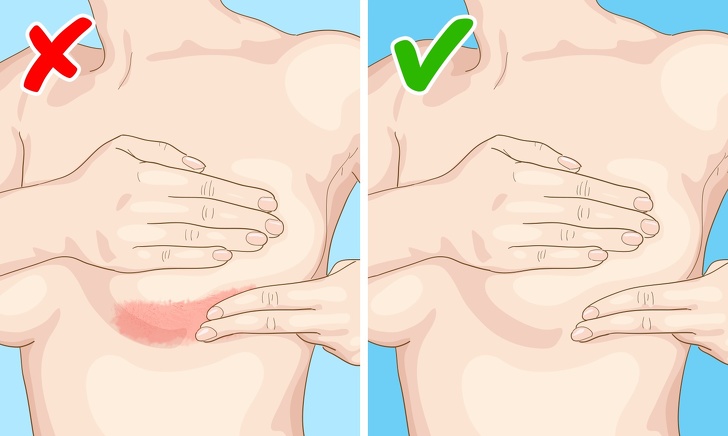
- Age-related changes - over time, after about 45 years, the process of fibro-fatty involution of the mammary glands starts in the woman's body. It consists in the degradation of glandular tissue and its gradual replacement with adipose tissue. This happens against the background of hormonal changes, which are especially actively carried out during menopause. These changes lead to a deficiency of the sex hormones estrogen and the gradual "extinction" of the body. The synthesis of collagen and elastane, which are the structural components of the connective tissue, dermis and ligaments, slows down. As a result of fibro-fat involution, a woman's breasts lose their aesthetically attractive appearance and, under the influence of the natural gravitational forces of the Earth, descend.
- Hereditary factor — innate features of collagen and elastin synthesis determine the rate of tissue aging and predisposition to gigantomastia and, consequently, to mastoptosis.

- Pregnancy and breastfeeding - during pregnancy, a woman's breasts increase in volume due to the filling of glandular lobules with milk. This increases the load on the ligaments, and the skin is stretched. After the end of lactation, the volume of the gland gradually decreases. Due to the stretching of the skin, the breast looks "empty" and saggy. In addition, the uneven distribution of milk, as well as feeding the baby with one breast, can lead to noticeable asymmetries.
- Rapid weight loss or weight gain - fatty tissue not only actually determines the shape of the mammary glands. In the case of rapid weight loss, part of the volume of the breast is lost, and the skin does not have time to recover. Hormones responsible for metabolism are stored and synthesized in adipocytes of adipose tissue. On the contrary, rapid weight gain leads to an increase in the volume of the mammary glands and stretching of the skin.

- Breast arthroplasty with implants that are too large - breast descent after mammoplasty occurs faster, the larger the prosthesis and the less elastic the skin.
- Smoking and alcohol abuse.
Stages of mastoptosis
According to the classification proposed by American plastic surgeons, there are 3 degrees of mastoptosis.
Breast ptosis of the 1st degree is the initial stage of breast prolapse, in which the nipple is at the level of the submammary (breast) fold or slightly lower.
Ptosis of the breast 2 degrees - the nipple falls less than 3 cm below the submammary fold.
Breast ptosis grade 3 - the nipple is located more than 3 cm below the level of the fold and looks down.
False ptosis (mastoptosis) is characterized by the normal position of the nipples and the sagging of the lower pole of the mammary glands - it is located under the submammary fold.
Breast ptosis treatment
With the help of exercise and diet, you can reduce the amount of fatty tissue, but this does not affect the state of the connective and glandular tissue, which also give the shape of the breast. In addition, with mastoptosis, the problem is also in stretching the skin.
In addition, with mastoptosis, the problem is also in stretching the skin.
On the contrary, breast lifting in the salon (mesotherapy, biorevitalization, massage and other cosmetic procedures) is aimed at improving the condition of the connective tissue. These non-surgical methods require regular repetition and will not correct severe breast ptosis. Injections of vitamin complexes, hyaluronic acid and other active substances will help to achieve a qualitative improvement in the condition of the skin, restore the synthesis of collagen and elastane fibers. Thanks to cosmetic procedures, it is possible to slow down the aging process and improve the appearance of the breast, but not to correct breast ptosis or its shape.
How to correct ptosis with a surgical lift (mastopexy)
With breast ptosis of the 1st degree, the beautiful shape of the bust can be restored with the help of arthroplasty - surgery to increase it with implants. The problem of more advanced ptosis of 2 or 3 degrees is solved by mastopexy (mammopexy), that is, a breast lift. The essence of this plastic surgery is the resection of excess skin, adipose and glandular tissue, as a result of which it is possible to lift the nipple-areolar complex. With insufficient volume of breast tissue, mastopexy can be combined with endoprosthetics and thus increase the size of the breast. If a woman has a noticeable asymmetry, then it can be eliminated by combining a facelift with reduction mammoplasty or arthroplasty. In general, mastopexy is performed under general anesthesia for 1-3 hours.
The essence of this plastic surgery is the resection of excess skin, adipose and glandular tissue, as a result of which it is possible to lift the nipple-areolar complex. With insufficient volume of breast tissue, mastopexy can be combined with endoprosthetics and thus increase the size of the breast. If a woman has a noticeable asymmetry, then it can be eliminated by combining a facelift with reduction mammoplasty or arthroplasty. In general, mastopexy is performed under general anesthesia for 1-3 hours.
There are three main breast lift methods:
Periareolar mastopexy
It is used to eliminate mild and uncomplicated ptosis of 1 or 2 degrees. The plastic surgeon makes an incision around the areola to resect excess skin.
Vertical mastopexy
The method is used for breast ptosis of 2 and 3 degrees. The plastic surgeon makes two incisions: one around the areola, and the other vertically down from the circumference by 7-8 cm.

Anchor (or 'T') mastopexy
The most effective way to eliminate advanced breast ptosis of the 3rd degree. The technique involves a composition of three neat incisions: vertical, around the areola and along the contour of the submammary fold.
Why breast lift should be done in the clinic. N.I. Pirogov?
Our plastic surgeons know how to correct breast ptosis, giving it a beautiful and toned shape again without noticeable postoperative scars. Look at the portfolio of our specialists, and you can be convinced of this. From 1999 years old doctors of the clinic. N.I. Pirogov in St. Petersburg successfully perform all types of breast surgery: from endoprosthesis replacement to reconstruction after mastectomy. If after some time you are faced with the problem of breast prolapse after primary mammoplasty, our plastic surgeons will not only solve this problem, but will take care of the quality and long-term preservation of the result.