Gestational sac at 8 weeks miscarriage
Blighted Ovum (Anembryonic Pregnancy): Causes & Symptoms
Overview
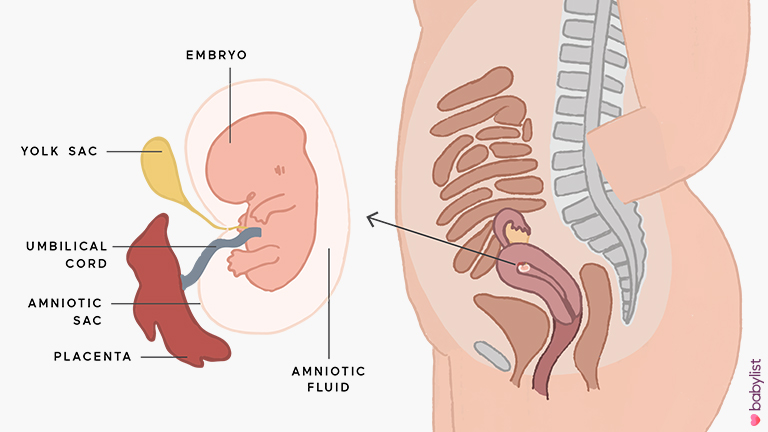
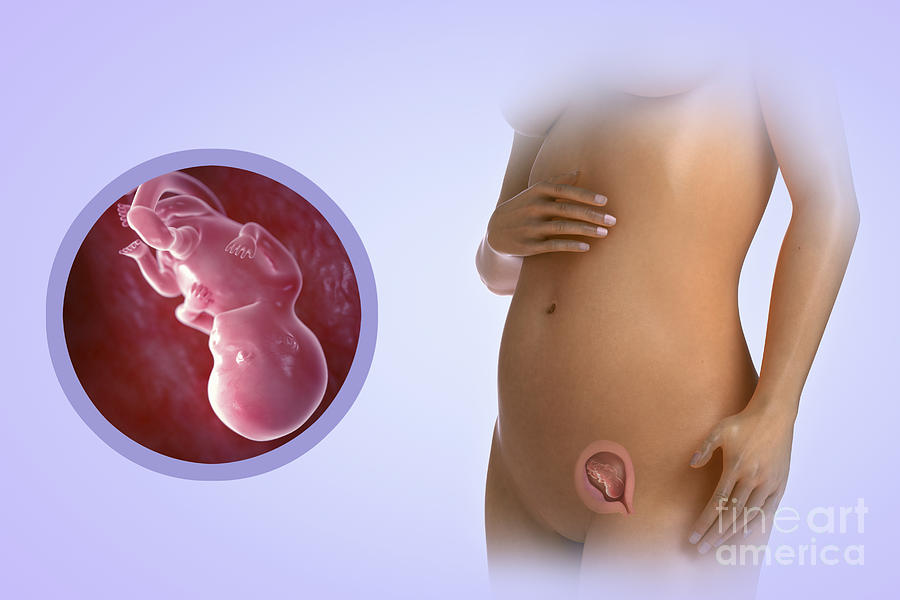
A blighted ovum is when the gestational sac containing the embryo is empty.What is a blighted ovum?
A blighted ovum (also called an anembryonic pregnancy) is a type of early miscarriage that occurs when a fertilized egg implants into the uterus but does not develop into an embryo. The embryo will stop growing, but the gestational sac (where the embryo would develop) continues to grow. The placenta and empty gestational sac will release pregnancy hormones — even without an embryo present. This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
When does a blighted ovum happen?
A blighted ovum causes an early miscarriage in the first trimester of pregnancy. During fetal development, a fertilized egg turns into a blastocyte. At around four weeks of pregnancy, this blastocyte implants in the wall of the uterus and develops into an embryo. When you have a blighted ovum, the gestational sac that would hold the embryo continues to grow, even without an embryo present. The following can occur:
- A blighted ovum happens so early in pregnancy, that you never realize you are pregnant.
- You have a positive pregnancy test and signs of pregnancy only to discover a blighted ovum at your first ultrasound.
- You have a positive pregnancy test and signs of pregnancy but then experience a miscarriage.
How common is a blighted ovum pregnancy?
A blighted ovum is the number one cause of first trimester miscarriages.
Symptoms and Causes
What are the symptoms of a blighted ovum?
A blighted ovum can occur so early in pregnancy that you never knew you were pregnant. In other cases, you may experience signs of pregnancy such as a missed menstrual period or a positive pregnancy test. You can have symptoms of early pregnancy, such as breast tenderness and morning sickness.
Other times your symptoms will resemble those of a miscarriage:
- Vaginal bleeding: Spotting (light bleeding), bleeding or passing light gray tissue or blood clots.
- Cramping: Mild to moderate cramping in your pelvic and abdominal region.
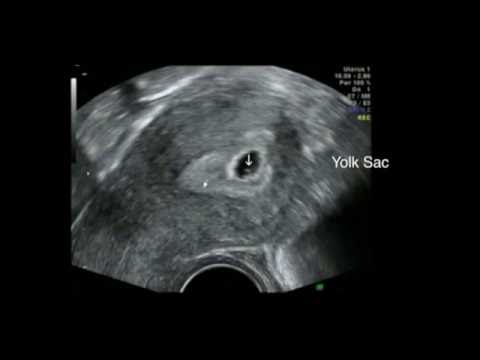
The only way to confirm a blighted ovum is through an ultrasound. It will show a gestational sac that is missing an embryo inside.
What causes a blighted ovum?
A blighted ovum is usually caused by chromosomal or genetic problems during cell division. During conception, the egg will begin to divide shortly after being fertilized by sperm. Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
How does a blighted ovum miscarriage start?
A blighted ovum miscarriage will cause vaginal bleeding and abdominal cramping. A miscarriage usually feels more intense than your regular menstrual period. You can take an over-the-counter medicine like acetaminophen to relieve cramping. Avoid lifting anything heavy or any strenuous exercise as it can increase your bleeding. You may experience spotting for several weeks after a miscarriage.
Diagnosis and Tests
How is a blighted ovum diagnosed?
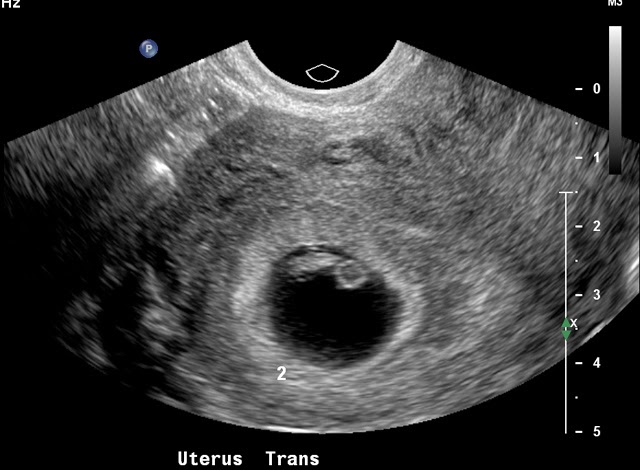
Your healthcare provider will diagnose a blighted ovum using transvaginal ultrasound. This happens in the first trimester, usually between seven and nine weeks of pregnancy. An embryo should be visible at this time in pregnancy. With a blighted ovum, the gestational sac will be empty.
- You will lie back on an exam table and place your feet in stirrups like you do for a pelvic exam. Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus.
- A blighted ovum will appear as an empty sac — almost like a bubble.
A blighted ovum is when the gestational sac containing the embryo is empty.
People are often unaware that they have a blighted ovum. This is because your placenta continues to give off hormones, making your body think you are pregnant. This is also why you can still have symptoms of pregnancy, including a positive pregnancy test.
If you’ve already experienced bleeding or signs of a miscarriage, your healthcare provider will use ultrasound to look at the contents of your uterus to diagnose a blighted ovum.
Some healthcare providers will collect a series of blood samples that check the levels of hCG (human chorionic gonadotropin) in your body. HCG is known as the pregnancy hormone because it's only produced if you are pregnant. The level of hCG in your blood increases rapidly in early pregnancy and reaches its peak around weeks eight to ten. If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
Management and Treatment
How is a blighted ovum treated?
For some people, there may be no treatment needed, because your body passes the embryo through your vagina (a miscarriage). If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
- Dilation & Curettage (D&C): This is a surgical procedure to remove the contents of your uterus. Your healthcare provider will dilate, or open, the cervix and use medical tools and suction to remove the pregnancy tissues from your uterus. This is done under sedation or general anesthesia.
- Natural miscarriage: If it's safe, you may be able to watch and wait to see if your body eventually releases the pregnancy tissues. It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins.
- Medication-induced miscarriage: You may be given a medication called misoprostol to trigger your body to miscarry.
 This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
A follow-up appointment is usually scheduled four to six weeks after a miscarriage or D&C. You may be given another ultrasound to confirm the uterus is empty. Your healthcare provider will check for signs of infection and make sure there were no complications.
What are the complications of a blighted ovum?
Complications of a blighted ovum are uncommon, but the possible complications could include:
- Excessive bleeding or hemorrhage.
- Infection.
- Scarring (from the D&C procedure).
- Tears in the uterus (from the D&C procedure).
How long does it take to recover from a blighted ovum?
Recovering from a blighted ovum miscarriage or D&C can last from one or two weeks to a month. Cramping generally lasts up to a week, but bleeding can last several weeks. Your bleeding should get lighter until it stops completely.
Your bleeding should get lighter until it stops completely.
You can resume normal activities when you feel comfortable. Bleeding can increase with strenuous activity or exercise. Hormones may remain in your body and delay your menstrual cycle. Most people will get their period within four to six weeks after a blighted ovum.
It may take longer to recover emotionally from a blighted ovum miscarriage. You may have feelings of sadness, anger or confusion. It’s OK to take time to grieve. Ask your friends and family for support.
Prevention
Can a blighted ovum be prevented?
A blighted ovum can’t be prevented. Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Outlook / Prognosis
How soon after a blighted ovum can I get pregnant again?
Most healthcare providers recommend having one or two regular menstrual cycles before trying to conceive again after any type of miscarriage.
What are my chances of having another blighted ovum?
Your chances of having another blighted ovum are low. Most people go on to have healthy, full-term pregnancies. If you experience more than one blighted ovum, your healthcare provider may suggest testing to determine if there is an underlying cause.
Living With
When should I see my healthcare provider?
Call your healthcare provider right away if you have any of these symptoms:
- Excessive bleeding from your vagina.
- Dizziness or fainting.
- Fever that does not go away.
- Symptoms that get worse over time.
- Severe pain that isn’t helped with pain medicine.
When should I go to the ER?
Go to the nearest ER If you experience heavy vaginal bleeding — more than two pads per hour for two consecutive hours — or have symptoms of anemia like dizziness, palpitations or paleness.
What questions should I ask my doctor?
Losing a pregnancy is upsetting and confusing. Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
- Can I let my body miscarry or should I take medication to induce a miscarriage?
- What are the risks of miscarriage?
- Do I have to have a D&C?
- What are the risks of a D&C?
- How long can I expect to bleed or have cramping?
- Is there any indication this will happen again?
- When can I start trying to conceive?
- Do I need to come back for another ultrasound?
Frequently Asked Questions
Is a blighted ovum considered a miscarriage?
Yes, a blighted ovum is a miscarriage. A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
How long can you carry a blighted ovum?
The amount of time you can carry a blighted ovum varies. Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Can a blighted ovum turn into a baby?
No, an empty gestational sac will not turn into an embryo. The formation of the embryo occurs within two weeks of conception. By the time the gestational sac is formed, the cells should have already formed the embryo. Your healthcare provider will be able to examine your gestational sac to confirm that no embryo has developed.
Do hCG levels rise with blighted ovum?
Yes, most of the time hCG levels will rise, giving you a positive pregnancy test and symptoms of pregnancy. This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
Is a blighted ovum more common with IVF?
A blighted ovum is not more common with IVF (In Vitro Fertilization). Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
A note from Cleveland Clinic
Losing a pregnancy is difficult. If you are struggling after a miscarriage, speak with your healthcare provider so they can recommend support groups or counselors. Finding support may help you get through this hard time. Most people who have had a blighted ovum will go on to have a healthy pregnancy.
Blighted Ovum (Anembryonic Pregnancy): Causes & Symptoms
Overview
A blighted ovum is when the gestational sac containing the embryo is empty.What is a blighted ovum?
A blighted ovum (also called an anembryonic pregnancy) is a type of early miscarriage that occurs when a fertilized egg implants into the uterus but does not develop into an embryo. The embryo will stop growing, but the gestational sac (where the embryo would develop) continues to grow. The placenta and empty gestational sac will release pregnancy hormones — even without an embryo present. This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
When does a blighted ovum happen?
A blighted ovum causes an early miscarriage in the first trimester of pregnancy. During fetal development, a fertilized egg turns into a blastocyte. At around four weeks of pregnancy, this blastocyte implants in the wall of the uterus and develops into an embryo. When you have a blighted ovum, the gestational sac that would hold the embryo continues to grow, even without an embryo present. The following can occur:
- A blighted ovum happens so early in pregnancy, that you never realize you are pregnant.
- You have a positive pregnancy test and signs of pregnancy only to discover a blighted ovum at your first ultrasound.
- You have a positive pregnancy test and signs of pregnancy but then experience a miscarriage.
How common is a blighted ovum pregnancy?
A blighted ovum is the number one cause of first trimester miscarriages.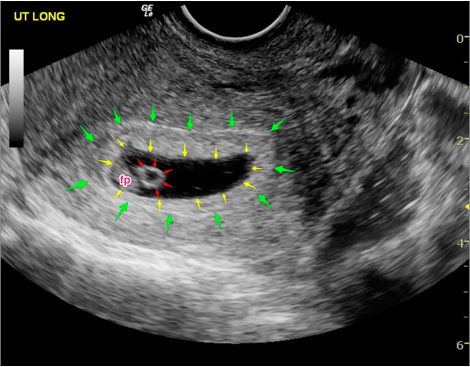
Symptoms and Causes
What are the symptoms of a blighted ovum?
A blighted ovum can occur so early in pregnancy that you never knew you were pregnant. In other cases, you may experience signs of pregnancy such as a missed menstrual period or a positive pregnancy test. You can have symptoms of early pregnancy, such as breast tenderness and morning sickness.
Other times your symptoms will resemble those of a miscarriage:
- Vaginal bleeding: Spotting (light bleeding), bleeding or passing light gray tissue or blood clots.
- Cramping: Mild to moderate cramping in your pelvic and abdominal region.
The only way to confirm a blighted ovum is through an ultrasound. It will show a gestational sac that is missing an embryo inside.
What causes a blighted ovum?
A blighted ovum is usually caused by chromosomal or genetic problems during cell division. During conception, the egg will begin to divide shortly after being fertilized by sperm. Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
How does a blighted ovum miscarriage start?
A blighted ovum miscarriage will cause vaginal bleeding and abdominal cramping. A miscarriage usually feels more intense than your regular menstrual period. You can take an over-the-counter medicine like acetaminophen to relieve cramping. Avoid lifting anything heavy or any strenuous exercise as it can increase your bleeding. You may experience spotting for several weeks after a miscarriage.
Diagnosis and Tests
How is a blighted ovum diagnosed?
Your healthcare provider will diagnose a blighted ovum using transvaginal ultrasound. This happens in the first trimester, usually between seven and nine weeks of pregnancy. An embryo should be visible at this time in pregnancy. With a blighted ovum, the gestational sac will be empty.
- You will lie back on an exam table and place your feet in stirrups like you do for a pelvic exam.
 Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus.
Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus. - A blighted ovum will appear as an empty sac — almost like a bubble.
A blighted ovum is when the gestational sac containing the embryo is empty.
People are often unaware that they have a blighted ovum. This is because your placenta continues to give off hormones, making your body think you are pregnant. This is also why you can still have symptoms of pregnancy, including a positive pregnancy test.
If you’ve already experienced bleeding or signs of a miscarriage, your healthcare provider will use ultrasound to look at the contents of your uterus to diagnose a blighted ovum.
Some healthcare providers will collect a series of blood samples that check the levels of hCG (human chorionic gonadotropin) in your body. HCG is known as the pregnancy hormone because it's only produced if you are pregnant. The level of hCG in your blood increases rapidly in early pregnancy and reaches its peak around weeks eight to ten. If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
Management and Treatment
How is a blighted ovum treated?
For some people, there may be no treatment needed, because your body passes the embryo through your vagina (a miscarriage). If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
- Dilation & Curettage (D&C): This is a surgical procedure to remove the contents of your uterus. Your healthcare provider will dilate, or open, the cervix and use medical tools and suction to remove the pregnancy tissues from your uterus. This is done under sedation or general anesthesia.
- Natural miscarriage: If it's safe, you may be able to watch and wait to see if your body eventually releases the pregnancy tissues.
 It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins.
It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins. - Medication-induced miscarriage: You may be given a medication called misoprostol to trigger your body to miscarry. This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
A follow-up appointment is usually scheduled four to six weeks after a miscarriage or D&C. You may be given another ultrasound to confirm the uterus is empty. Your healthcare provider will check for signs of infection and make sure there were no complications.
What are the complications of a blighted ovum?
Complications of a blighted ovum are uncommon, but the possible complications could include:
- Excessive bleeding or hemorrhage.
- Infection.
- Scarring (from the D&C procedure).
- Tears in the uterus (from the D&C procedure).
How long does it take to recover from a blighted ovum?
Recovering from a blighted ovum miscarriage or D&C can last from one or two weeks to a month. Cramping generally lasts up to a week, but bleeding can last several weeks. Your bleeding should get lighter until it stops completely.
You can resume normal activities when you feel comfortable. Bleeding can increase with strenuous activity or exercise. Hormones may remain in your body and delay your menstrual cycle. Most people will get their period within four to six weeks after a blighted ovum.
It may take longer to recover emotionally from a blighted ovum miscarriage. You may have feelings of sadness, anger or confusion. It’s OK to take time to grieve. Ask your friends and family for support.
Prevention
Can a blighted ovum be prevented?
A blighted ovum can’t be prevented.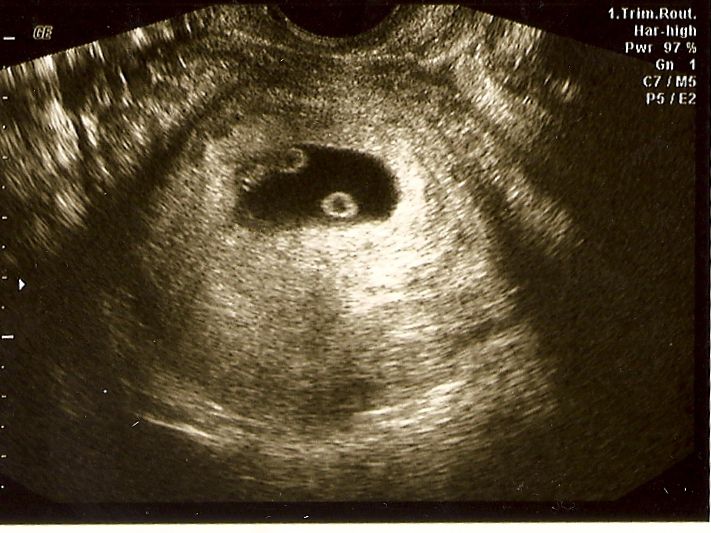 Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Outlook / Prognosis
How soon after a blighted ovum can I get pregnant again?
Most healthcare providers recommend having one or two regular menstrual cycles before trying to conceive again after any type of miscarriage.
What are my chances of having another blighted ovum?
Your chances of having another blighted ovum are low. Most people go on to have healthy, full-term pregnancies. If you experience more than one blighted ovum, your healthcare provider may suggest testing to determine if there is an underlying cause.
Living With
When should I see my healthcare provider?
Call your healthcare provider right away if you have any of these symptoms:
- Excessive bleeding from your vagina.
- Dizziness or fainting.
- Fever that does not go away.
- Symptoms that get worse over time.
- Severe pain that isn’t helped with pain medicine.
When should I go to the ER?
Go to the nearest ER If you experience heavy vaginal bleeding — more than two pads per hour for two consecutive hours — or have symptoms of anemia like dizziness, palpitations or paleness.
What questions should I ask my doctor?
Losing a pregnancy is upsetting and confusing. Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
- Can I let my body miscarry or should I take medication to induce a miscarriage?
- What are the risks of miscarriage?
- Do I have to have a D&C?
- What are the risks of a D&C?
- How long can I expect to bleed or have cramping?
- Is there any indication this will happen again?
- When can I start trying to conceive?
- Do I need to come back for another ultrasound?
Frequently Asked Questions
Is a blighted ovum considered a miscarriage?
Yes, a blighted ovum is a miscarriage. A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
How long can you carry a blighted ovum?
The amount of time you can carry a blighted ovum varies. Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Can a blighted ovum turn into a baby?
No, an empty gestational sac will not turn into an embryo. The formation of the embryo occurs within two weeks of conception. By the time the gestational sac is formed, the cells should have already formed the embryo. Your healthcare provider will be able to examine your gestational sac to confirm that no embryo has developed.
Do hCG levels rise with blighted ovum?
Yes, most of the time hCG levels will rise, giving you a positive pregnancy test and symptoms of pregnancy. This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
Is a blighted ovum more common with IVF?
A blighted ovum is not more common with IVF (In Vitro Fertilization). Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
A note from Cleveland Clinic
Losing a pregnancy is difficult. If you are struggling after a miscarriage, speak with your healthcare provider so they can recommend support groups or counselors. Finding support may help you get through this hard time. Most people who have had a blighted ovum will go on to have a healthy pregnancy.
Ultrasound at the 8th week of pregnancy
For ultrasound in the first trimester of , certain terms are set - 10-13 weeks. During the gestation period of this particular duration, the fetus will already begin laying the main internal organs, the skeleton, and the brain. With the help of ultrasound, all these parameters can be seen and evaluated.
With the help of ultrasound, all these parameters can be seen and evaluated.
However, it happens that the doctor prescribes an ultrasound at the 8th week of pregnancy, when it is too early to judge the presence or absence of pathologies in the fetus. Such early research has goals.
Why is ultrasound done at 8 weeks pregnant?
Ultrasound at the eighth week is done for:
- Confirmation of uterine pregnancy.
- Clarification of the position of the ovum (it is necessary to exclude a pathological ectopic pregnancy).
- Detection of the number of embryos in the fetal egg (at this time it will already be possible to detect a multiple pregnancy).
- Identification of pathologies of the female reproductive system (for example, a shortened cervix can cause miscarriage or premature birth).
- Clarification of the gestational age.
- Identification of threats of miscarriage or its fading.
Fetal development at 8 weeks of gestation
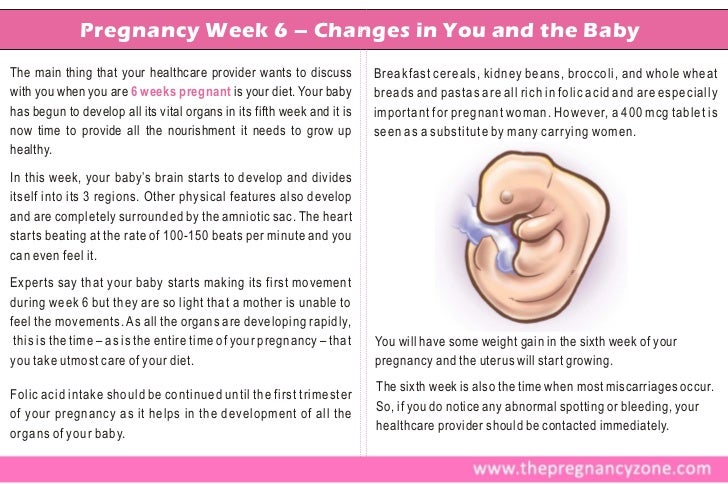
By the eighth week, the fetus reaches a length of two centimeters.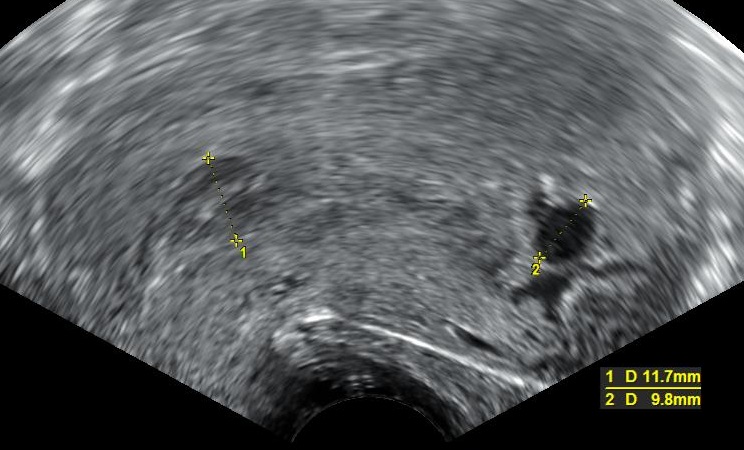 He has already formed the circulatory system, the first veins and the main internal organs, which will continue to develop throughout the entire period of pregnancy. The fetal heart is already beating, and this can be seen if an ultrasound is performed.
He has already formed the circulatory system, the first veins and the main internal organs, which will continue to develop throughout the entire period of pregnancy. The fetal heart is already beating, and this can be seen if an ultrasound is performed.
Fingers are already appearing on the hands and feet of the baby, and the upper limbs are increasing in length. Shoulders and knees appeared. The inner ear, that is, the center of balance, begins to form.
The eyes of the fetus are forming, they are already closed by thin eyelids.
Preparation for ultrasound at 8 weeks
Ultrasound at the 8th obstetric week of pregnancy does not require special preparation. Women are simply advised 2-3 days before the study to refrain from food that provokes excessive gas formation in the intestines, as well as from carbonated drinks. You need to come to the doctor's appointment calm and in a good mood.
How is an ultrasound done at the eighth week of pregnancy?
At the eighth week, ultrasound can be performed in two ways:
- Transvaginally using a special probe inserted into the vaginal cavity.

- Transabdominally , i.e. through the skin of the abdomen of a pregnant woman.
The first method will give more accurate results, but may cause some discomfort to the woman. In addition, transvaginal ultrasound is not recommended if a woman complains of abdominal pain or bloody discharge.
After the ultrasound, the doctor may take a photo showing the tiny embryo.
What will the ultrasound show?
Ultrasound at the eighth week of pregnancy, with its correct course, visualizes a fetal egg with a live embryo inside. Also, according to the results of the study, it will be possible to judge the place of attachment of the chorion, the position of the fetal egg in the uterine cavity.
Ultrasound at 8 weeks should show the fetal heartbeat and the frequency can be assessed.
At a period of 8 weeks, it is already possible to identify some pathologies in the development of the fetus, in particular in the work of his heart. At the same time, specialists have not yet made unambiguous conclusions about the presence of heart disease.
At the same time, specialists have not yet made unambiguous conclusions about the presence of heart disease.
Ultrasound will also show how the neural tube of the fetus develops, how limbs are formed.
Embryo examination
A large proportion of the total ultrasounds at the eighth week of is the study of the embryo. Its size, location, structure is important. It is also necessary to evaluate the motor activity of the embryo, which should be present even at such a short time. At the eighth week, the embryo should be clearly visible. If it is not there, most likely its development has froze or there is an anembryonic fact, that is, the initial absence of an embryo in a fetal egg (or its death immediately after conception).
Yolk sac examination
When conducting an ultrasound scan at 8-9 obstetric weeks of pregnancy, it is required to assess not only the state of the embryo itself, but also the organs outside its structure. These organs include the yolk sac.
Its presence in the ovum is temporary. The pouch appears approximately 15-16 days after fertilization and disappears by the end of the first trimester.
The yolk sac plays an important role in the development of the embryo - it produces germ cells, forms embryonic red blood cells for the first time, produces proteins necessary for development, helps to form immunity, and so on.
At the eighth week, the ultrasound should show the yolk sac. Its size should be approximately 4-5 mm. An increase in the size of the yolk sac can be the first sign of pathological development of the fetus.
Ultrasound norms at the 8th week of pregnancy
At the eighth week of gestation, an ultrasound is done and they look at how the parameters of the developing fetus correlate with the norm for a particular gestational age. The main indicators of fetal development include:
- The size of the embryo from the coccyx to the crown (KTP). At 8 weeks for KTP, the norm is 14-20 mm.

- Heart rate (HR). The norm for the 8th week is 110-150 beats / min.
- Bipaterial head size (BDP). The norm is 6 mm.
- Yolk sac. This extraembryonic organ should be visualized and reach 4-5 mm in diameter.
A deviation from the norm of one or several parameters at once can be a signal that the fetus is developing with pathology. Although doctors do not make unambiguous conclusions on such a short period of time and, as a rule, prescribe a second ultrasound in 1-2 weeks.
Book a diagnostic or consultation today!
You can make an appointment by phone: +7 (812) 901-03-03
Or leave a request
full name
Phone number
By clicking the "Make an appointment" button, I accept the terms of the Personal Data Processing and Security Policy and consent to the processing of my personal data.
Our medical centers
Making an appointment
Patient's last name *
Incorrect first name
Name *
Middle name
Contact phone *
E-mail *
By clicking the "Make an appointment" button, I accept the terms of the Personal Data Processing and Security Policy and consent to the processing of my personal data.
Registration and payment for repeated online appointment
Patient's last name *
Incorrect first name
Name *
Middle name *
Contact phone *
E-mail *
By clicking the "Submit request" button, I accept the terms of the Personal Data Processing and Security Policy and consent to the processing of my personal data.
About cookies on this website
We use cookies, IP addresses and device data for analytics to make your visit to the site convenient and personalized. You can disable cookies in your browser settings. By continuing to use our site, you consent to the processing of the listed data and accept the terms of the Privacy Policy.
Anembryonic - pregnancy or not?
Unfortunately, not all pregnancies end in childbearing. Reproductive losses in this case can be due to various reasons. And one of them is a non-developing or missed pregnancy. The proportion of this pathology accounts for up to 15-20% of reproductive losses. Currently, there are 2 variants of missed pregnancy: embryonic death and anembryony. It is important to understand that the differential diagnosis between them does not affect the subsequent treatment tactics, but is taken into account when assessing the prognosis. Anembryony is more often determined, and this condition in many cases is not accompanied by spontaneous abortion and therefore requires artificial termination of a missed pregnancy.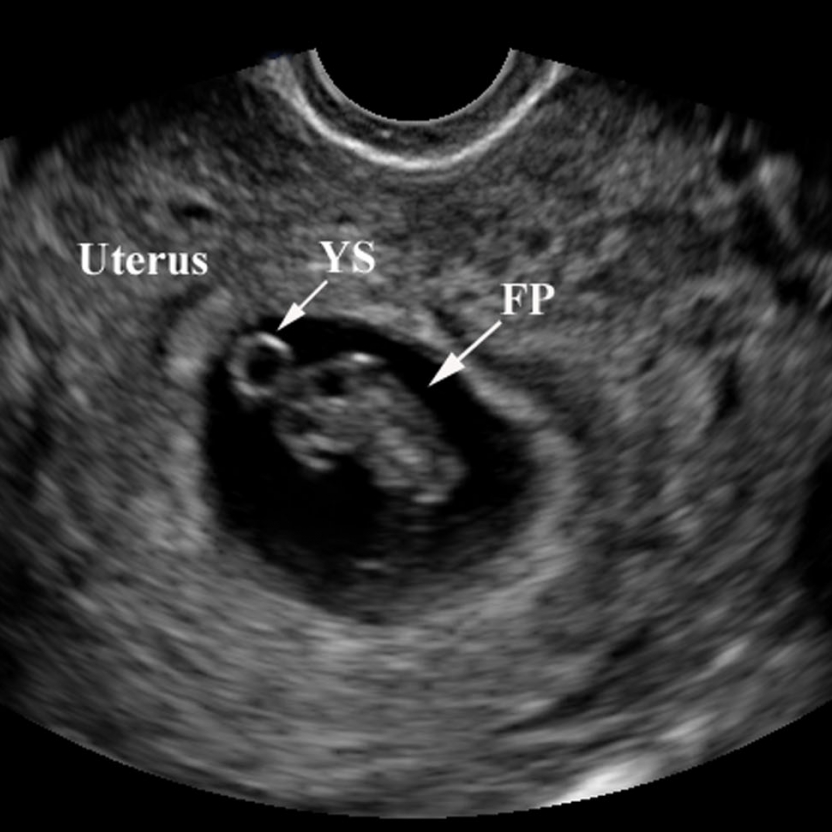
Anembryony – what is it?
Anembryony - is the absence of an embryo in a developing fetal egg. This condition is also called the empty gestational sac syndrome. This is by no means a rare pathology that can be diagnosed in primigravida and in women who already have healthy children.
At present, quite a lot of possible causes of anembryony have been identified. These include:
- Genetic anomalies , which are observed in almost 80% of the pathological condition. They are usually associated with gross and/or multiple chromosomal abnormalities. Moreover, with anembryony, such anomalies are of a qualitative nature, and with the death of the embryo and its abortion, they are predominantly quantitative. Unviable combinations of parental genes or mutations in key areas responsible for the early stages of embryogenesis and the synthesis of the main structural proteins of cell membranes are also possible.

- Some acute viral and bacterial diseases occurring in early pregnancy and leading to damage to embryonic tissues or trophoblast. The most dangerous in this regard are TORCH infections, although other pathogens can also be embryotropic.
- Persistent viral-bacterial infections of the organs of the reproductive system, leading to the development of chronic endometritis . And in most cases, such a pathology occurs without obvious clinical symptoms and is detected after a frozen pregnancy.
- Radiation exposure of to a developing embryo.
- Exogenous intoxications : taking drugs with embryotoxic action, drug addiction, exposure to certain industrial and agricultural poisons (toxins).
- Endocrine disorders in a pregnant woman. And the most critical is the deficiency of progesterone and disorders of its metabolism, which is the main cause of the pathology of endometrial decidualization and abnormal implantation of the fetal egg.

In general, the causes of pathology in most cases remain undiagnosed. Usually it is possible to determine only a presumptive etiology.
Genetic diagnosis of aborted tissues can reveal obvious anomalies in the hereditary material. But such a study, unfortunately, is carried out in a very small percentage of cases. Basically, it is indicated with a burdened obstetric history in a woman, when she already had frozen or spontaneously interrupted in the early stages of gestation in the past. But even such a diagnosis is not always informative enough, which is associated with the limited possibilities of modern genetics and the high probability of the impact of other etiological factors.
Pathogenesis
Anembryony is a consequence of the cessation of reproduction and differentiation of the embryoblast or inner cell mass - a group of cells that normally give rise to fetal tissues. And this happens at the earliest stages of pregnancy (usually at 2-4 weeks of gestation), and without disturbing the development of the fetal membranes from the trophoblast. As a result, a so-called empty fetal egg is formed, which continues to grow even in the absence of an embryo in it.
As a result, a so-called empty fetal egg is formed, which continues to grow even in the absence of an embryo in it.
Pathogenetically important factors in the development of the disease include:
- Inherited or acquired chromosome aberrations and other genetic abnormalities. They can lead to a gross desynchronization of the development of embryonic tissues, critical changes in the structure of collagen and other proteins, disruption of the induction of differentiation and migration of dividing cells. The most common autosomal trisomy, monosomy, triploidy, tetraploidy.
- Excessive formation of circulating immune complexes in a woman's body . Their deposition in the walls of small vessels leads to thromboembolism and other critical microcirculation disorders in the area of the implanting egg. Antiphospholipid antibodies are of the greatest clinical importance.
- Excessive activation of T-helpers with an increase in the concentration and aggression of the cytokines secreted by them.
 These substances are able to have a direct and indirect damaging effect on embryonic tissues with a violation of their proliferation and differentiation. In fact, the fetal egg in this case acts as a target for the cellular link of immunity. The reason for such an abnormal immune response of a woman's body may be a chronic infection of the endometrium, hormonal abnormalities, and some other endogenous factors.
These substances are able to have a direct and indirect damaging effect on embryonic tissues with a violation of their proliferation and differentiation. In fact, the fetal egg in this case acts as a target for the cellular link of immunity. The reason for such an abnormal immune response of a woman's body may be a chronic infection of the endometrium, hormonal abnormalities, and some other endogenous factors.
It is important to understand that during anembryony a woman's body produces substances that help prolong pregnancy. Therefore, in a significant proportion of cases, spontaneous abortion does not occur. The patient develops and maintains signs of pregnancy, there is an increase in hCG in the blood serum. Therefore, the basal temperature during anembryony usually does not have characteristic features. And on the first early ultrasound, the fact of successful implantation of the fetal egg in the uterine cavity is confirmed. After all, pregnancy does occur, but it develops without a key component - the embryo.
Subsequently, rejection of the abnormal fetal egg is possible. In this case, the threat of termination of pregnancy (including with the formation of exfoliating retrochorial hematomas) or spontaneous abortion (miscarriage) can be diagnosed. But often anembryony is diagnosed only during a routine examination, in which case the diagnosis is absolutely unexpected and shocking news. Such a pregnancy requires an artificial interruption.
How does this manifest itself?
Anembryony does not have its own clinical symptoms , all emerging disorders are usually associated with the threat of termination of such a pathological pregnancy. And the warning signs include the presence of clinical manifestations of relative progesterone deficiency, which creates the prerequisites for spontaneous abortion. Therefore, pain in the lower abdomen and bloody discharge can become a reason for contacting a doctor; with anembryony, they can appear at almost any time during the 1st trimester. But often a woman learns about the existing pathology only when conducting a screening ultrasound for a period of 10-14 weeks.
But often a woman learns about the existing pathology only when conducting a screening ultrasound for a period of 10-14 weeks.
Diagnosis
Like other forms of miscarriage, anembryony is detected in the first trimester of gestation. And the main diagnostic tool in this case is ultrasound , because it is this study that allows you to visualize the existing deviations.
At the same time, symptoms can be reliably detected only after the 8th week of gestation. At earlier dates, visualization is often insufficient due to the too small size of the ovum, so an erroneous diagnosis is not ruled out. Therefore If a missed pregnancy and anembryony are suspected, it is recommended to conduct an examination several times, repeating the procedure on expert-class equipment with an interval of 6-8 days. At the same time, the initial diagnosis of an empty fetal egg can be removed if subsequent ultrasound scans can visualize an embryo with signs of a heartbeat and sufficient developmental dynamics.
The main echographic features:
- absence of the yolk sac when the diameter of the fetal egg is 8-25 mm;
- absence of an embryo in a fetal egg with a diameter of more than 25 mm.
Additional signs of a missed pregnancy include an irregular shape of the fetal egg, an insufficient increase in its diameter in dynamics, a weak severity of the decidual reaction, and the absence of a heartbeat at a gestational age of 7 or more weeks. And signs of the threat of its interruption are a change in the tone of the uterus and the appearance of areas of chorion detachment with the appearance of subchorial hematomas.
Anembryony can also be suspected by a dynamic assessment of the level of hCG in the blood. An increase in the level of this hormone along the lower limit of the norm should be the basis for further examination of a woman with an ultrasound scan. It is important to understand that hCG is also produced in the syndrome of an empty ovum.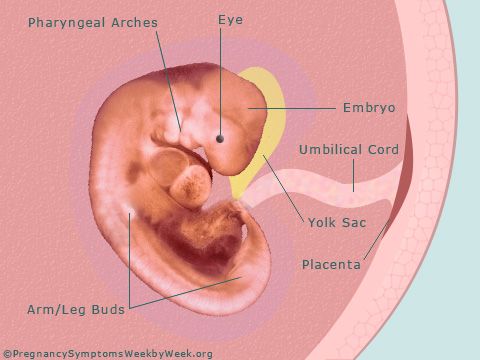 Moreover, its level in this pathology will be almost normal, in contrast to a frozen pregnancy with the death of a normally developing embryo. Therefore, monitoring of indirect signs of pregnancy and the growth of hCG during anembryony cannot be attributed to reliable diagnostic methods.
Moreover, its level in this pathology will be almost normal, in contrast to a frozen pregnancy with the death of a normally developing embryo. Therefore, monitoring of indirect signs of pregnancy and the growth of hCG during anembryony cannot be attributed to reliable diagnostic methods.
Varieties
Several variants of the empty ovum syndrome are possible:
- Type I anembryony. The embryo and its remains are not visualized, the size of the fetal egg and uterus does not correspond to the expected gestational age. The diameter of the egg is usually no more than 2.5 mm, and the uterus is enlarged only up to 5-7 weeks of gestation.
- Type II anembryony. There is no embryo, but the ovum and uterus correspond to the gestational age.
- Resorption of one or more embryos in multiple pregnancies. At the same time, normally developing and regressing fetal eggs are visualized.
 According to this type, anembryony often occurs after IVF, if several embryos were implanted in a woman.
According to this type, anembryony often occurs after IVF, if several embryos were implanted in a woman.
All these varieties are determined only by ultrasound, they do not have characteristic clinical features .
What to do?
Confirmed anembryos are an indication for abortion. This does not take into account the gestational age, the woman's well-being and the presence of signs of a possible spontaneous abortion. An exception is the situation when the anembryony of the second fetal egg is diagnosed in a multiple pregnancy. In this case, a wait-and-see strategy is taken, evaluating the dynamics of the development of the preserved embryo.
Termination of a missed pregnancy is carried out only in a hospital. After the procedure for the evacuation of the fetal egg, the woman should be under medical supervision. In many cases, after it, additional medication and sometimes physiotherapy are prescribed, aimed at normalizing the hormonal background, preventing inflammatory and hemorrhagic complications, and eliminating the detected infection.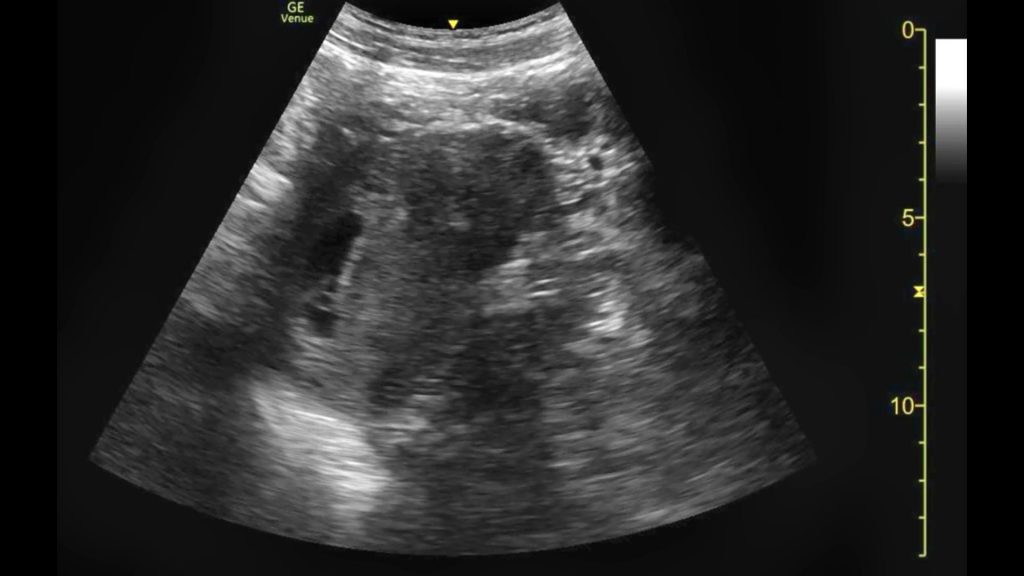
Several techniques can be used to perform a medical abortion in this pathology. Can be used:
- medical abortion - termination of pregnancy with the help of hormonal drugs that provoke rejection of the endometrium along with an implanted ovum;
- vacuum aspiration of the contents of the uterine cavity;
- curettage is an operation involving the mechanical removal of the ovum and endometrium with a special instrument (curette) after the forced expansion of the cervical canal with bougie.
Medical abortion for anembryos is possible only for a period of 6-8 weeks. In later periods of gestation, preference is given to mechanical methods, which requires the use of general anesthesia. The choice of the method of artificial abortion depends on whether the stomach hurts after an abortion, the length of the rehabilitation period, the likelihood of early and late complications.
Examination after induced abortion necessarily includes ultrasound control.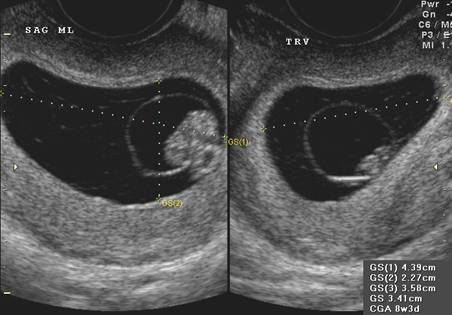 This allows you to confirm the complete evacuation of the membranes and endometrium, to exclude undesirable consequences of abortion in the form of hematomas, perforation and endometritis.
This allows you to confirm the complete evacuation of the membranes and endometrium, to exclude undesirable consequences of abortion in the form of hematomas, perforation and endometritis.
Prediction
Can anembryony recur? Can I still have children? These questions concern all patients who have undergone this pathology. Fortunately, in most cases, the condition does not recur, the woman subsequently manages to safely become pregnant and bear the child. But at the same time, she is classified as a risk group for the possible development of complications of pregnancy and childbirth. Therefore, in the first trimester, she is usually assigned dynamic ultrasound control of the development of the fetal egg, determination of the hormonal profile and assessment of the state of the hemostasis system.
Pregnancy after anembryos is theoretically possible already in the next ovarian-menstrual cycle. But it is desirable to let the body recover. Therefore, it is recommended to start planning for re-conception no earlier than 3 months after the induced abortion . If it proceeded with complications, the rehabilitation period, while maintaining reproductive rest, is extended for up to six months. If a woman has chronic endometritis and various infections, 2 months after the completion of treatment, a control examination is carried out and only then the possible timing of re-conception is determined.
Therefore, it is recommended to start planning for re-conception no earlier than 3 months after the induced abortion . If it proceeded with complications, the rehabilitation period, while maintaining reproductive rest, is extended for up to six months. If a woman has chronic endometritis and various infections, 2 months after the completion of treatment, a control examination is carried out and only then the possible timing of re-conception is determined.
Barrier method and hormonal contraception are preferred for preventing pregnancy. The selection of funds in this case is carried out individually. Intrauterine devices immediately after a frozen pregnancy are not used in order to avoid the development of endometritis.
Prevention
Primary anembryonic prevention includes careful planning of pregnancy with a comprehensive examination. If deviations are found, they are corrected. Of course, such preparation does not allow 100% to exclude the possibility of pathology, but reduces the risk of its development.