Rashes on infants stomach
Baby Rashes: Types, Symptoms & More
Baby’s have incredibly sensitive skin, which makes them more likely to develop rashes than adults and older kids. But with all the different types out there, it can be hard to identify what the baby rash is, what’s causing it and how to treat it. Plus, no parent wants to see their precious little one with a red or bumpy reaction on their soft skin. Many might wonder how rashes affect baby’s comfort level and whether they cause itchiness or pain. And how can parents tell if baby’s rash is a harmless diaper rash or something a little more serious?
Because there are so many types of baby rashes, it’s important to be aware of the symptoms to look out for and know when to call the pediatrician. To help you better identify a baby rash on the body, we’ve put together a handy guide on all things rashes. Keep reading to learn more about the common types of baby rash, tell-tale signs and symptoms and the best remedies to treat them.
In this article:
Baby rash causes
baby acne or baby rash?
Baby heat rash
Meningitis rash
Strep rash
Chicken pox
Baby drool rash
Baby eczema rash
Hives
Baby allergy rash
Baby fungal rash
Cradle cap
When to be concerned about baby rashes
Baby Rash Causes
When it comes to baby rashes, there are many types and many culprits. Some common causes include:
-
Irritants. Common irritants that can bother baby’s sensitive skin are saliva and drool, poop, baby wipes, detergents, soaps, sunscreen and nickel.
-
Allergies. Allergic reactions can cause a baby rash to appear in a bunch of different forms. Rashes can be itchy, welt-like hives or dry, itchy patches. Eczema is the most common version of a baby rash caused by allergies.
-
Infections. Infections can lead to different types of baby rash, the most common of which are fungal rashes. Sometimes, however, a viral baby rash can develop. “These rashes occur when babies have specific viral illnesses and may be associated with fever or other symptoms,” says Anna Bender, MD, a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian. A viral baby rash can appear as small dots on the torso and sometimes arms and legs, and can last for several days to a week.
 It may spread for a few days and then begin to clear up.
It may spread for a few days and then begin to clear up.
“Baby’s skin barrier is especially fragile because it’s thinner, immature and the skin is still developing, so that makes it a lot more vulnerable to damage and dryness. It’s also more reactive, especially to things that could be irritants,” explains Lauren R. Crosby, MD, FAAP, a pediatrician at LaPeer Pediatrics in Beverly Hills, California. Baby’s skin is typically ultra-sensitive from birth until around age 2, although diaper rash can continue to rear its head past that age until kids are potty trained.
In our guide below, we outline the different ways baby rashes look and behave. Keep reading for the most common types of baby rash to keep an eye out for, plus how to prevent and treat them. From heat rashes to chicken pox, we help make sense of any bumps or blotches you may find on baby.
Baby Acne or Baby Rash?
Breakouts aren’t just for teenagers—it’s actually totally normal for babies to get acne. “Also known as neonatal acne, it’s a common rash in babies during the first month of life,” Bender says. “It’s thought that maternal hormones—those that pass from mother to baby in utero—may cause baby acne to flare.”
“Also known as neonatal acne, it’s a common rash in babies during the first month of life,” Bender says. “It’s thought that maternal hormones—those that pass from mother to baby in utero—may cause baby acne to flare.”
But how can you tell if it’s baby acne or a baby rash? Baby acne typically looks like a bunch of small, red bumps, as opposed to the lacy red of a baby rash.
Image: iStock
Baby acne symptoms
- Pimples. Baby acne usually involves clusters of tiny red pimples and whiteheads.
- Irritated cheeks. Baby acne usually develops on the cheeks, but it can also appear on baby’s nose, forehead and sometimes behind the ears and on the scalp.
- Persistent symptoms. Baby acne can last up to three to four months.
Prevention and treatment
Usually, baby acne clears up on its own with gentle cleansing. Once in a while parents might need to see a dermatologist if it’s persisting beyond the normal three to four months, but that’s pretty rare.
Baby Heat Rash
Baby heat rash tends to happen when baby’s sweat glands become blocked and trap sweat under the skin, Crosby says. It’s usually seen in warm weather or when baby is overdressed. How do you know if the baby rash is caused by heat?
Image: Shutterstock
Heat rash symptoms
- Tiny red bumps. These typically appear on baby’s head, neck and shoulders, and sometimes on the chest.
- Itching. Sometimes heat rash can be itchy, so take note if baby is scratching at their irritated skin.
Prevention and treatment
To prevent baby heat rash, dress baby in lighter clothing to make sure they aren’t getting overheated or sweaty. In warm climates, it’s fine to let them sleep in just a onesie and diaper, and run a fan in the bedroom to keep the air cool and circulating. When baby heat rash does strike, “I recommend a daily bath with a non-fragrant sensitive skin cleanser to help clear out the sweat and keep the skin clear,” Crosby says.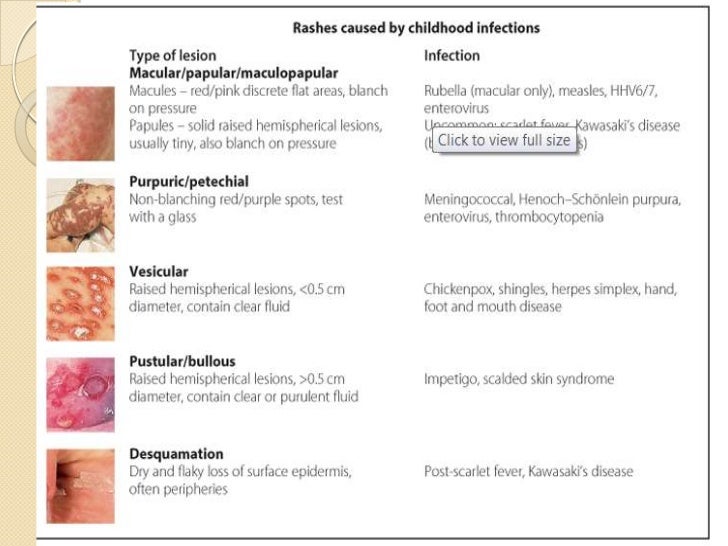 A baby rash from heat usually goes away on its own in three to four days, as long as baby isn’t overdressed and stays in a cool environment.
A baby rash from heat usually goes away on its own in three to four days, as long as baby isn’t overdressed and stays in a cool environment.
Baby Diaper Rash
It’s pretty self-explanatory where you can expect to see this baby rash. “Diaper rash can occur due to irritation from wet diapers and friction,” Bender says. Baby diaper rash is even more common in older babies who sleep through the night longer and may have wetter diapers in the morning.
Image: Shutterstock
Diaper rash symptoms
- Red patches. These typically appear on the rounded part of baby’s bottom.
- Puffy, warm skin. In some cases, baby’s skin may be slightly raised and feel warm to the touch.
Prevention and treatment
“Diaper rash can improve with frequent diaper changes and use of over-the-counter diaper paste containing zinc oxide, which helps in acting as a barrier to prevent friction and irritation in the diaper area,” Bender says. Ward off baby diaper rash by making sure the skin is completely dry before you put on a fresh diaper. In the past, baby powder was the go-to trick for absorbing moisture and protecting baby’s skin, but doctors no longer recommend using powder for diaper rash, since inhaled powder can irritate baby’s lungs.
Ward off baby diaper rash by making sure the skin is completely dry before you put on a fresh diaper. In the past, baby powder was the go-to trick for absorbing moisture and protecting baby’s skin, but doctors no longer recommend using powder for diaper rash, since inhaled powder can irritate baby’s lungs.
Sometimes a rash on baby’s butt can actually be a yeast rash caused by fungus that lives on our skin.
Image: iStock
Yeast rash symptoms
- Pink patches. These patches usually appear in baby’s skin folds, accompanied by small pink dots or pustules around the edge.
Prevention and treatment
To treat a baby yeast rash, apply a topical, over-the-counter antifungal cream a few times a day. Prevent yeast rash by keeping baby clean and dry.
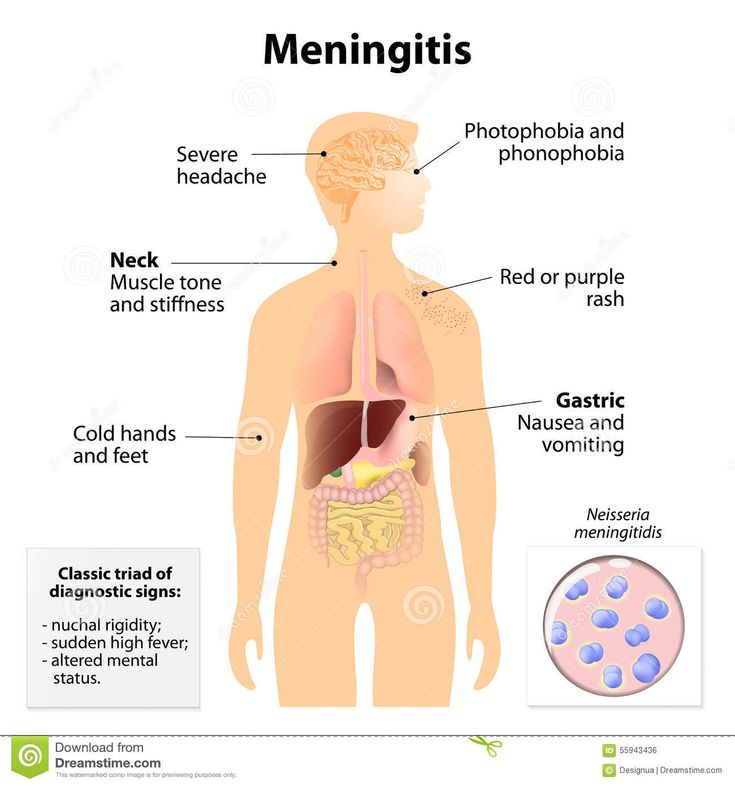
Meningitis Rash
Meningitis is when the lining around the brain and spinal cord (the meninges) is inflamed, and “is a serious infection because it can be present in the blood and brain and cause organ damage, permanent brain damage or death,” Bender says.
While the viral form of meningitis is serious, it’s almost never life-threatening, according to the Centers for Disease Control and Prevention (CDC). Bacterial meningitis, however, can be deadly and calls for immediate medical attention. There’s a vaccine for bacterial meningitis, but it typically isn’t given until later in childhood or before college. You can’t tell the difference between a baby rash caused by bacterial or viral meningitis, and in many cases a rash won’t appear at all.
Image: iStock
Meningitis symptoms
- High fever. Take baby’s temperature, since a high fever is a classic sign of meningitis.
- Lethargy. If baby is less active than usual, it could be another signal of meningitis.
- Vomiting. This symptom is more common in infants, along with a loss of appetite and irritability.
- Rashes. Meningitis rashes can vary in appearance, but the most common ones include pink or red dots all over, purple rashes that can look like tiny bruises or broken capillaries in the skin, and an itchy, red rash.
Prevention and treatment
Viral meningitis usually clears up on its own in seven to 10 days, but bacterial meningitis requires immediate medical attention so antibiotics can be given as soon as possible. Serious cases may call for hospitalization. If you think baby might have meningitis, call your doctor right away—they can determine if baby has the disease and the type of meningitis.
Strep rash
A strep rash on baby is another type of viral baby rash. Your child is more prone to strep rash if other family members have been exposed to strep throat.
Image: iStock
Strep rash symptoms
- Bright red skin. Strep rash on baby can be bright red and beefy-looking with wet, oozing patches in neck folds, or as a bright red circle patch in the area around baby’s anus, Bender says.
- Blisters and scabbing. Spotting scabs and blisters on baby’s skin is another common sign of strep.
Prevention and treatment
Since strep can spread from person to person through close contact, keep baby away from infected people.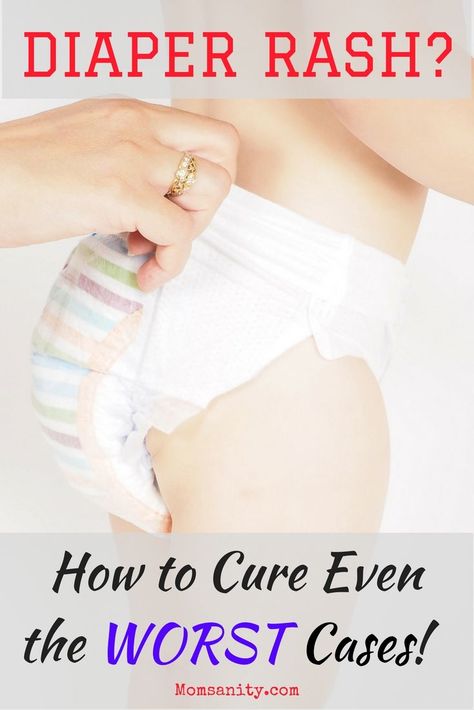 Unlike your run-of-the-mill neck rash, which can be treated with over-the-counter antifungal creams, strep requires a visit to the doctor. Once the diagnosis of strep rash is confirmed—typically with a skin swab test—your pediatrician may prescribe an oral antibiotic as treatment.
Unlike your run-of-the-mill neck rash, which can be treated with over-the-counter antifungal creams, strep requires a visit to the doctor. Once the diagnosis of strep rash is confirmed—typically with a skin swab test—your pediatrician may prescribe an oral antibiotic as treatment.
Chicken Pox
Chicken pox appears as a baby rash on the body. Before the chicken pox—or varicella—vaccine became available in 1995, practically every child came down with chicken pox before age 9, according to the American Academy of Pediatrics (AAP). Nowadays, it’s pretty rare for babies to get chicken pox, thanks to the vaccine. It’s a super-contagious viral infection caused by the varicella zoster virus, so avoid contact with infected people to keep baby safe.
Image: Shutterstock
Chicken pox symptoms
- Red bumps and blisters. Chicken pox causes a blister-like baby rash on the skin, starting on the back, tummy or face and spreading all over baby’s body.
 The blisters are often in different stages of healing, so some may look like pink bumps, some look like scabbed bumps and others may look like blisters.
The blisters are often in different stages of healing, so some may look like pink bumps, some look like scabbed bumps and others may look like blisters. - Itchiness. Chicken pox rashes are renowned for their intense itchiness.
- Fever. A temperature of 101 to 102 degrees Fahrenheit is common with chicken pox.
Prevention and treatment
Doctors recommend daily baths and keeping baby’s nails short so they can’t scratch and dig into their skin, which could cause a secondary infection. Typically, the course of treatment for chicken pox is to wait it out—it can last five to seven days—but in severe cases (which aren’t common), an antiviral medication may be prescribed. To prevent chicken pox, the APP recommends that healthy babies get the first dose of the vaccine between 12 and 15 months old, followed by a second dose at age 4 to 6.
Baby Drool Rash
Noticing a baby rash on your little one’s face? When babies’ saliva glands turn on, usually around 3 or 4 months of age, they start to drool. A lot. “If you think about it, saliva is part of your digestive tract,” Crosby says. “It’s not just water, so it’s irritating.”
A lot. “If you think about it, saliva is part of your digestive tract,” Crosby says. “It’s not just water, so it’s irritating.”
Image: Courtesy of Wissabo/Instagram
Baby drool rash symptoms
- A red, irritated baby rash on the face. Because the skin around baby’s mouth, chin and neck is constantly wet, these areas are especially prone to drool rash.
- Flaking skin. Baby rash from drool can also appear slightly flaky and dry-looking.
Prevention and treatment
One way to prevent and heal a baby rash caused by drool? Have a soft bib handy to keep the skin on baby’s face and chest dry. Apply a gentle over-the-counter ointment before and after meals as a barrier to prevent saliva from touching the skin, so baby’s drool rash can heal underneath it.
Baby Eczema Rash
Eczema, often-chronic red, dry patches of skin, is one of the most common skin disorders in babies—in fact, 60 percent of infants get eczema in the first year of life.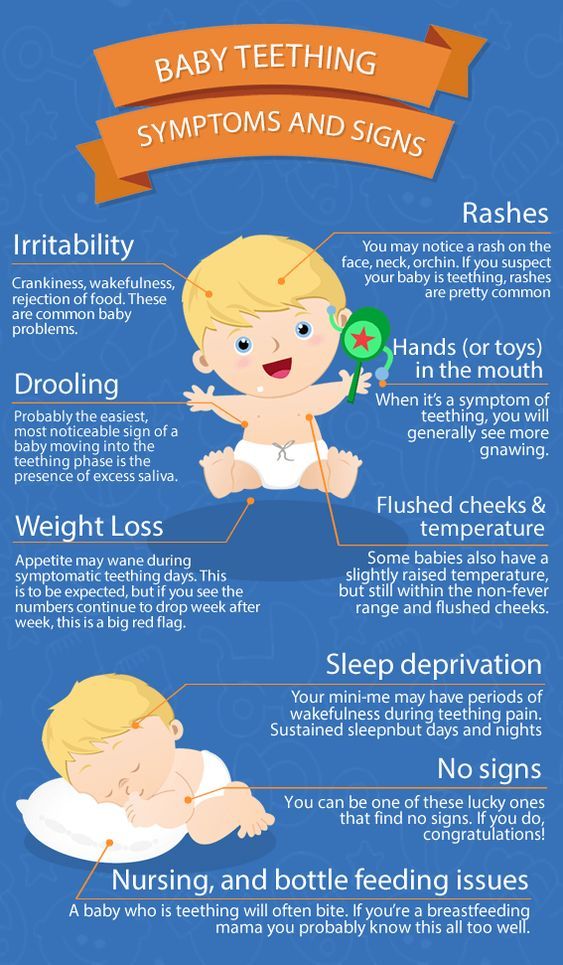 “Sometimes babies scratch so much, it can lead to bleeding and can interfere with sleep,” Bender says. “Babies with eczema often scratch more in the evening when they’re put to bed or at night when they aren’t distracted by other activities.” Eczema can get infected if not treated, leading to scabbing and oozing skin spots.
“Sometimes babies scratch so much, it can lead to bleeding and can interfere with sleep,” Bender says. “Babies with eczema often scratch more in the evening when they’re put to bed or at night when they aren’t distracted by other activities.” Eczema can get infected if not treated, leading to scabbing and oozing skin spots.
Image: iStock
Baby eczema symptoms
- Itchiness. The more severe baby’s eczema is, the more itchy the rash.
- Dry skin patches. This is a common sign of mild eczema.
- Pinker patches of dry, flaky skin. This signifies a moderate case of eczema.
- Red, flaky patches of skin. If baby’s skin is a darker red, it signifies severe eczema, which usually comes with worsened symptoms and intense itchiness across more of the body.
Prevention and treatment
Keeping baby’s skin well moisturized with a daily application of a thick cream can prevent the onset of eczema in infants who are at higher risk for the condition—aka those who have a strong family history of eczema or eczema-related diseases. A mild case of this baby rash can sometimes be treated with just moisturizer, while moderate eczema may need a cortisone cream or ointment to treat it. Severe eczema is treated with over-the-counter products.
A mild case of this baby rash can sometimes be treated with just moisturizer, while moderate eczema may need a cortisone cream or ointment to treat it. Severe eczema is treated with over-the-counter products.
“Hives can occur soon after baby eats something they’re allergic to or if baby is fighting a virus, in which case the hives may last for several days off and on,” Bender says. They can appear anywhere on the body, even if caused by food. If the baby rash is sparked by something your child touched, it usually appears on the part of baby’s body that came in contact with the allergen. If hives are accompanied by wheezing or if baby’s mouth or tongue starts to swell, see a doctor immediately.
Image: Shutterstock
Hive symptoms
- Pink, blotchy welts. These welts can come and go on baby’s skin.
- Itching. Hive welts are often very itchy.
Prevention and treatment
An oral antihistamine, such as Benadryl, can help treat hives. For a more natural remedy, try dabbing calamine lotion on the welts to soothe hives.
For a more natural remedy, try dabbing calamine lotion on the welts to soothe hives.
Baby Allergy Rash
As you expose baby to new products, foods and materials, there’s always a small chance they could be allergic to a certain ingredient or chemical. These rashes can be caused by food or medication that baby’s allergic to, or when baby’s skin comes into contact with an irritant, Crosby says.
So what does an allergy rash look like on a baby? A baby allergy rash can manifest in different ways, but the two most common signs are hives and eczema. As mentioned above, hives usually show up as pink blotchy welts, while eczema appears as red, dry, flaky patches. Both rashes are itchy.
Image: Shutterstock
Allergy symptoms
If you notice the following symptoms, take baby to the ER:
- Swelling of the lips or face. If baby’s lips or face become swollen, it’s a sign of a severe allergic reaction and should be treated by a doctor immediately.
- Wheezing. Any sign of difficulty breathing is a red flag.
Prevention and treatment
“Treatment depends on the age of the child and what is triggering it,” Crosby says. “You want to remove the allergen or trigger if you can, and use a topical or oral allergy medicine.” Sometimes a blood or skin test might be needed to figure out what baby is having an allergic reaction to, and then a baby rash treatment can be prescribed.
Baby Fungal Rash
A fungal baby rash is often caused by chronically wet or irritated skin. A yeast infection is the most common type of fungal rash. It can also appear in babies if another family member or family pet has ringworm.
Image: iStock
Fungal rash symptoms
- Pink, ring-like flaking patches of skin. These flaky patches can pop up anywhere on the skin, including the scalp and diaper area.
Prevention and treatment
“A fungal rash needs a special antifungal cream, or if it’s on the scalp and hair, it may need an oral antifungal medication,” Bender says. To prevent fungal baby rash, keep the skin clean and dry.
To prevent fungal baby rash, keep the skin clean and dry.
Cradle Cap
Essentially dandruff for babies, cradle cap is relatively common and typically caused by yeast. This type of baby rash usually shows up in the first month of life but can occur any time, Crosby says.
Image: iStock
Cradle cap symptoms
- Flaky skin. Rough, yellowish or pink crustry or oily scaly patches on the scalp are a classic sign of this type of baby rash.
- A slight oily scent. This results from the buildup of oil on baby’s scalp in moderate to severe cases.
Prevention and treatment
Most cases of cradle cap can be treated with regular shampooing and a soft scalp brush to loosen the flakes. If that doesn’t cut it, your pediatrician may recommend a medicated shampoo.
In general, the trick to preventing baby rash is keeping your child’s skin healthy. It’s best to keep baths to 10 minutes or less and use lukewarm water, since “during a bath, skin can really lose moisture, and babies are much more prone to getting dry skin,” Crosby says. Hydrating baby’s skin regularly is crucial. The best time to apply lotion? The first five minutes after a bath, to lock in moisture. “The skin is the largest organ in the body and it’s there to protect us from the elements and infections,” Crosby says. “The importance of really caring for it from infancy through adulthood can’t be stressed enough.”
Hydrating baby’s skin regularly is crucial. The best time to apply lotion? The first five minutes after a bath, to lock in moisture. “The skin is the largest organ in the body and it’s there to protect us from the elements and infections,” Crosby says. “The importance of really caring for it from infancy through adulthood can’t be stressed enough.”
Do baby’s lumps or bumps not line up with any of those listed in this guide? Baby can also develop a rash as a result of bug bites, sunburns, poison ivy and even dry skin. If you’re still not sure about baby’s rash, don’t hesitate to give your pediatrician a call or schedule an appointment.
When to Be Concerned About Baby Rashes
Now that you are familiar with some of the most common kinds of baby rashes, you’re probably wondering, “when should I be concerned about my baby’s rash?”
The truth is, many baby rashes are harmless, and some will come and go on their own without any medical treatment. The other good news is that there are vaccinations to prevent many serious rashes from developing in the first place.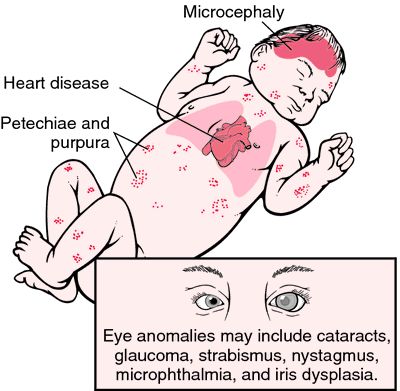
With that said, there are some signs you should keep an eye out for when you notice a baby rash on the body. Some baby rashes can indicate a potentially grave condition, particularly if the rash is persistent or if baby is experiencing swelling or wheezing.
Contact a doctor if baby experiences any of the following:
- If there is pain at the site of the rash
- If baby runs a fever
- If the rash develops bruise-like lesions
- If the rash oozes, bleeds or blisters
- If the rash continues to spread across baby’s body
- If baby develops any cold symptoms (coughing, wheezing, etc.)
- If baby has swollen neck glands or swollen lips
- If the baby rash doesn’t go away after two days
It’s true babies tend to get rashes left and right, but that doesn’t mean you should shrug them off as nothing. Whenever you notice a baby rash on their face or body, keep a watchful eye on it and look out for other symptoms. When it comes to baby’s health, it’s always best to be precautious and proactive.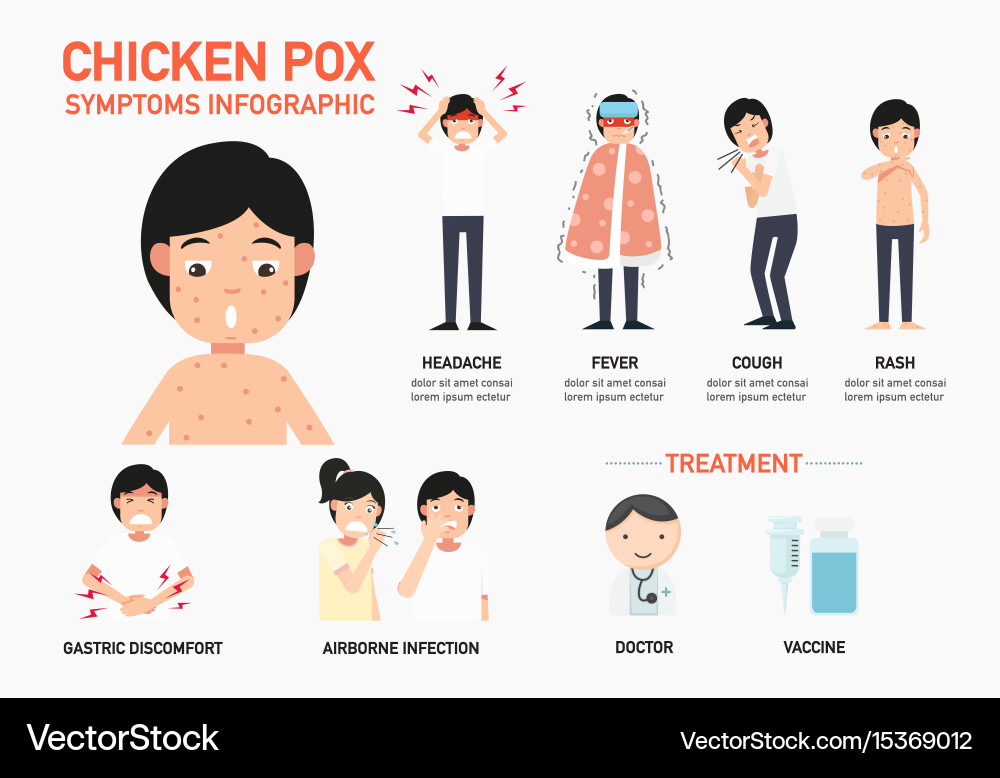
About the experts:
Anna Bender, MD, is a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian. She earned her medical degree from Columbia University College of Physicians and Surgeons in 2007. After completing her residency training in dermatology at New York Presbyterian Hospital - Weill Cornell Medical Center, Bender completed an additional year of specialized fellowship training in pediatric dermatology at the Johns Hopkins University School of Medicine.
Lauren R. Crosby, MD, FAAP, is a parenting expert and pediatrician at LaPeer Pediatrics in Beverly Hills, California. She earned her medical degree at UCLA School of Medicine and afterwards trained at Cedars-Sinai Medical Center, during which time she served as chief resident. She is a member and official spokesperson of the American Academy of Pediatrics.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Baby Skin Care 101
13 Diaper Rash Creams That Work Wonders
The Best Baby Eczema Creams, Shampoos and Washes
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.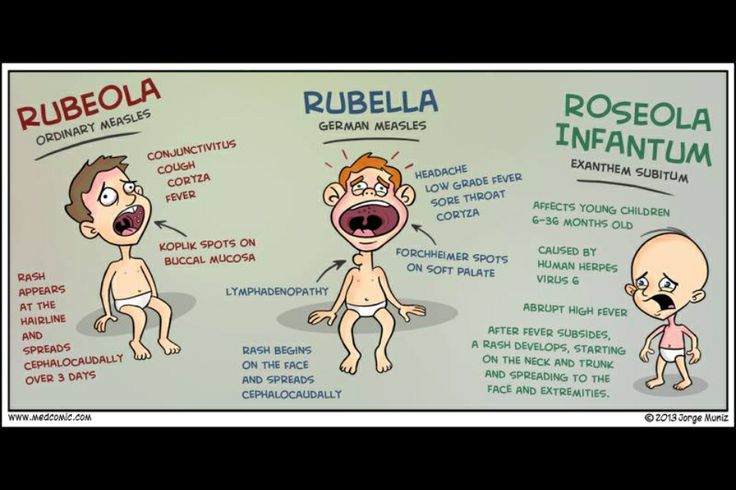
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics).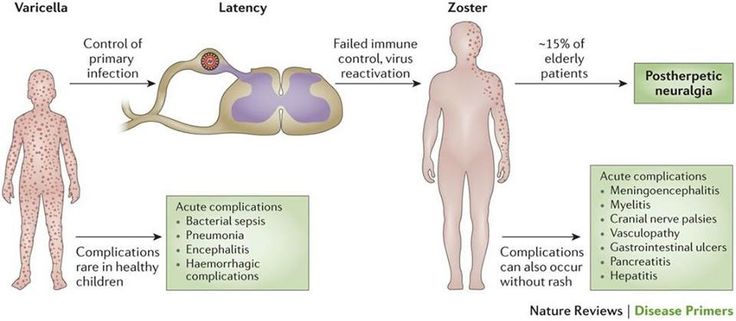 In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
Peak rash falls on the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).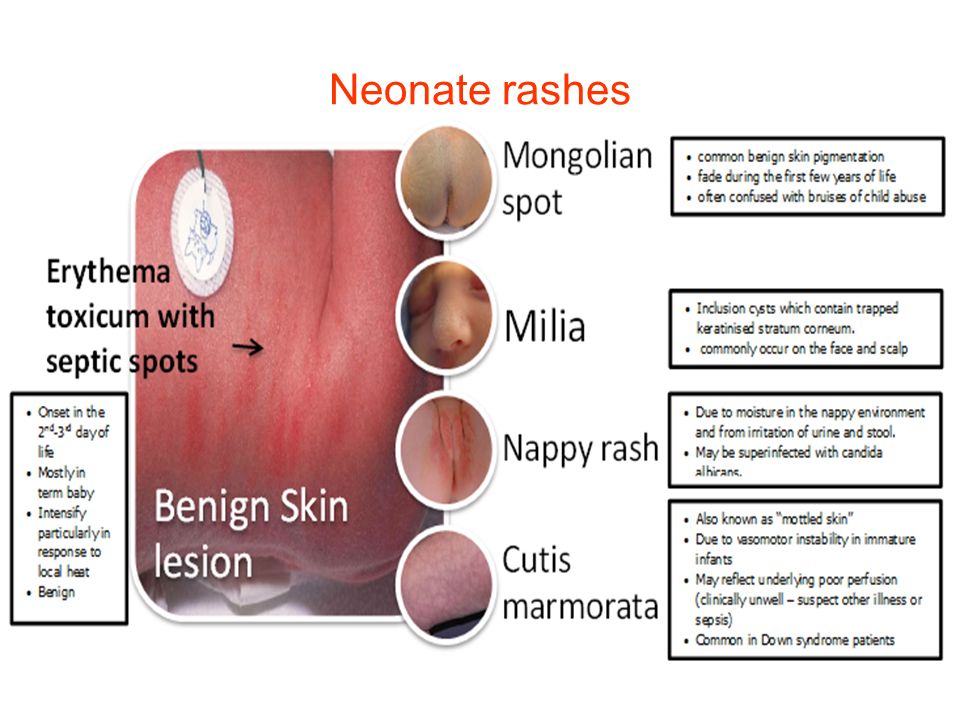
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“bonnet”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a variety of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
Usually, removal of the damaging agent and short-term use of anti-inflammatory creams will quickly lead to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (contact dermatitis prototype) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of life.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabrics, detergent residues on clothes, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc.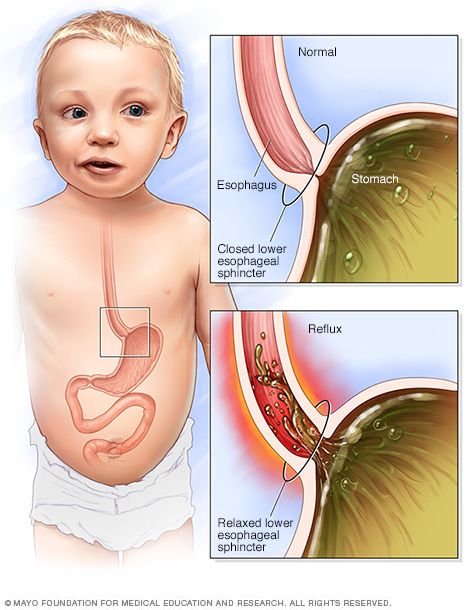 ). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.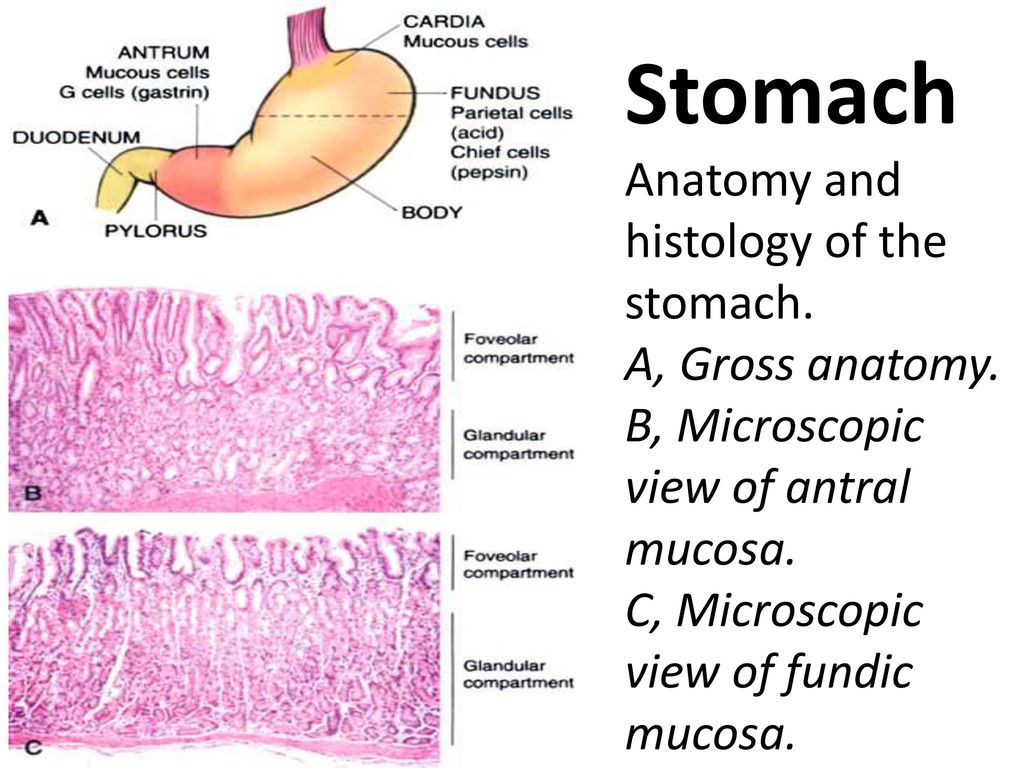
Author:
Eroshkina Maria Sergeevna
pediatrician
Skin rashes in babies - contraindications to vaccination
Dear Parents! Your baby needs to see a pediatrician on the day of vaccination . Of course, the child must be healthy , he needs to measure his body temperature the night before and in the morning before leaving the house and examine the skin. In the presence of skin rashes, vaccination is most often delayed, as this is a contraindication for the administration of most vaccines . Therefore, we recommend that parents be careful about skin rashes in their baby and always discuss the cause of their appearance with health workers.
Due to the frequent occurrence at appointments before vaccination of situations when parents of babies do not pay attention to skin manifestations in a child and come to an appointment on the day of vaccination, we suggest that you familiarize yourself with the causes of skin rashes in children.
Since the most intensive vaccination schedule is available for children in the first year of life, we will consider the causes of rash in young children (up to 3 years). But even at an older age, parents should not neglect the rule - we vaccinate children against the background of complete health, the absence of acute manifestations of the disease, if there are indications - against the background of the necessary medical preparation, in most cases - against the background of following a hypoallergenic diet.
So, the causes of skin rashes in young children:
- Allergic rash
- Intertrigo (diaper rash)
- Prickly heat
- Eruptions on the skin due to parasitic infestations
- Rash in infectious diseases
- Hemorrhagic eruptions in diseases of the blood and vessels
- Insect bites
Allergic rash
The most common cause of rashes in children of the first year of life is food allergy, the manifestations of which are diverse:
- rash of different shape and brightness on the body, more often on the cheeks,
- redness, peeling of the skin, accompanied by itching,
- persistent diaper rash,
- Gneiss on the scalp and eyebrows, persisting after the 3-4th month of a baby's life,
- copious prickly heat with slight overheating,
- appearance on the skin of blisters similar to nettle burn (urticaria),
- the appearance of swelling of the skin, subcutaneous fat and mucous membranes (angioedema).
In recent years, the number of children with skin manifestations of allergies has been growing. An increased risk of food allergies exists in children in whose families cases of allergies have already been recorded. In the presence of allergic diseases on the part of both parents, the risk of allergies in a child is approximately 70-80%, in the presence of an allergic pathology on the mother's side - 60%, on the father's side - 30%, in the absence of allergic problems on the part of the parents - from 10 to 18 %. In addition to hereditary factors, allergic reactions in an infant can be caused by fetal hypoxia (oxygen deficiency) during pregnancy and childbirth, a quick transition to artificial feeding, acute respiratory viral and intestinal infections suffered by the baby, followed by a violation of the composition of the intestinal microflora.
The occurrence of food allergies in children of the first year of life is associated with the functional features of their digestive tract: low enzyme activity, low production of IgA - protective antibodies located on the surface of the mucous membranes of the gastrointestinal tract. They provide local protection of the intestinal mucosa from foreign agents. With the introduction of complementary foods (individually for each child - from 4-6 months of life), further maturation of enzyme systems occurs. In case of violation of the terms and rules for the introduction of complementary foods, fermentopathy, imbalance of the microflora in the intestine, the appearance of rashes on the skin associated with an inflammatory reaction in the intestinal wall, requiring correction and treatment, may occur.
They provide local protection of the intestinal mucosa from foreign agents. With the introduction of complementary foods (individually for each child - from 4-6 months of life), further maturation of enzyme systems occurs. In case of violation of the terms and rules for the introduction of complementary foods, fermentopathy, imbalance of the microflora in the intestine, the appearance of rashes on the skin associated with an inflammatory reaction in the intestinal wall, requiring correction and treatment, may occur.
And of course, allergic reactions in breastfed children are associated with eating disorders of the nursing mother, with her excessive consumption of highly allergenic foods.
The so-called food diary helps to identify the causative allergen, in which the mother regularly (at least 14 days) notes all types of food and drink received by her or the baby during the day, indicates the composition of the dishes, the features of their culinary processing, feeding time and the appearance of unwanted reactions ( loose stools, regurgitation, skin rashes, etc. ). In children after a year, rashes are noted on the introduction of foods such as sweets, chocolate, cakes, muffins and other industrial culinary products containing a large amount of dyes and preservatives, which often cause allergic manifestations on the skin, even in adults. Given the immaturity of the enzymatic systems of the digestive tract in young children, the immaturity of the immune system, these products are not recommended to be introduced into the diet of children under 3 years of age.
). In children after a year, rashes are noted on the introduction of foods such as sweets, chocolate, cakes, muffins and other industrial culinary products containing a large amount of dyes and preservatives, which often cause allergic manifestations on the skin, even in adults. Given the immaturity of the enzymatic systems of the digestive tract in young children, the immaturity of the immune system, these products are not recommended to be introduced into the diet of children under 3 years of age.
If your baby periodically has manifestations of food allergies on the skin, vaccination is postponed until the rash fades and is carried out against the background of taking antihistamines prescribed by a pediatrician or an allergist-immunologist a few days before and after vaccination. It is necessary to follow a hypoallergenic diet for a nursing mother and child at least 7-10 days before and after the proposed vaccination. According to the doctor's prescription, probably, to stabilize the skin process, it will be necessary to use external agents to treat the skin so that vaccination does not serve as a factor that provoked an exacerbation.
Intertrigo (diaper rash)
Diaper rash usually appears in large folds of skin, especially where a child's skin comes into contact with urine, feces, and diapers. Most often, diaper rash appears on the buttocks, in the inguinal-femoral folds, but sometimes the skin can turn red in a similar way in the axillary and cervical folds and even behind the ears. In advanced cases, cracks, erosions and sores may appear on the surface.
Prevention of diaper rash is the timely change of diapers and diapers, air baths. In case of diaper rash, the pediatrician, in accordance with the type of skin, will prescribe baths with decoctions of certain herbs, as well as a remedy for application after bathing in skin folds.
Prickly heat
Prickly heat is associated with the peculiarities of the structure and functioning of the sweat glands. Usually occurs in hot weather, when the child overheats due to fever, high air temperature or excessive wrapping.
Prickly heat appears on the skin with multiple small (1–2 mm) bright red spots. Rashes in babies often appear on the neck, chest and abdomen. The prickly heat of the baby practically does not bother, and if the rules of skin care are followed, it quickly disappears. Small manifestations of miliaria are not a reason for a medical withdrawal from vaccination if there are no infected elements.
Rashes in babies often appear on the neck, chest and abdomen. The prickly heat of the baby practically does not bother, and if the rules of skin care are followed, it quickly disappears. Small manifestations of miliaria are not a reason for a medical withdrawal from vaccination if there are no infected elements.
Skin eruptions due to parasitic infestations
In infants, more often from the age of 6 months, infection with various parasites is very likely - pinworms, giardia, roundworms. Toxins, waste products of parasites, helminths are absorbed into the blood and are an allergenic factor, in most cases they can cause rashes on the skin of a child.
Only a pediatrician can identify this type of rash after an examination and necessary examinations, after which treatment is prescribed individually.
Rashes in infectious diseases
If the rash on the skin is accompanied by fever, chills, runny nose, general malaise, loss of appetite, if there has been contact with patients in the family or in a public place for 7–14 days, the child is likely to have manifestations of infection.
Rashes occur with such infectious diseases as: chicken pox, measles, rubella, scarlet fever, infectious mononucleosis, meningococcal infection, enterovirus infection and other viral diseases. To make a diagnosis, an examination of a child by a pediatrician must be carried out at home or in a special box in a children's clinic.
Hemorrhagic eruptions in diseases of the blood and vessels
In addition to infections, a rash occurs in diseases of the blood and blood vessels. Hemorrhagic rashes look like red or dark spots (bruises) that do not disappear when pressed. In the presence of a hemorrhagic rash, it is necessary to consult a pediatrician, a hematologist and conduct additional research methods.
Insect bites
Young children often suffer from mosquito and midge bites. Parents notice skin rashes in the morning, after the child wakes up or after walking in the forest park area. The appearance of pink or reddish spots is characteristic, mainly on open areas of the body, and the presence of elements on the face or on one half of it is obligatory (in the event that the child slept on his side).