Rash on 1 year old back
Nappy rash - NHS
Around 1 in 4 babies and toddlers in nappies have nappy rash at any one time. It doesn't usually develop in newborns, but all babies can get nappy rash.
Nappy rash can be caused by:
- your baby's skin being in contact with wee or poo for a long time
- the nappy rubbing against your baby's skin
- not cleaning the nappy area or changing the nappy often enough
- soap, detergent or bubble bath
- alcohol-based baby wipes
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
There may be red patches on your baby's bottom, or the whole area may be red. Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Most babies with mild nappy rash don't feel sore, but if the rash is severe your baby may feel uncomfortable and be distressed.
If your baby gets nappy rash, you can usually treat their skin yourself.
If the rash isn't upsetting your baby, at each nappy change apply a thin layer of a barrier cream to protect their skin. Ask your health visitor or pharmacist to recommend one.
Follow this advice to help look after your baby's skin.
- Change wet or dirty nappies as soon as possible.
- Clean the whole nappy area gently but thoroughly, wiping from front to back. Use water or fragrance-free and alcohol-free baby wipes. Read more about how to clean your baby and change your baby's nappy.
- Bath your baby daily – but avoid bathing them more than twice a day as that may dry out their skin.
- Dry your baby gently after washing them – avoid vigorous rubbing.
- Lie your baby on a towel and leave their nappy off for as long and as often as you can to let fresh air get to their skin.
- Do not use soap, bubble bath, or lotions.
- Do not use talcum powder as it contains ingredients that could irritate your baby's skin.
- Make sure your baby’s nappy fits properly. If it is too tight then it can irritate the skin and if it is too loose, then the nappy will not be able to soak up pee properly.
Nappy rash usually clears up after about 3 days if you follow this advice. You should keep following this advice as this will help prevent nappy rash from coming back.
If the rash is causing your baby discomfort, your health visitor or pharmacist can recommend a nappy rash cream to treat it.
You should apply the cream first and wait a few minutes before you apply the barrier cream.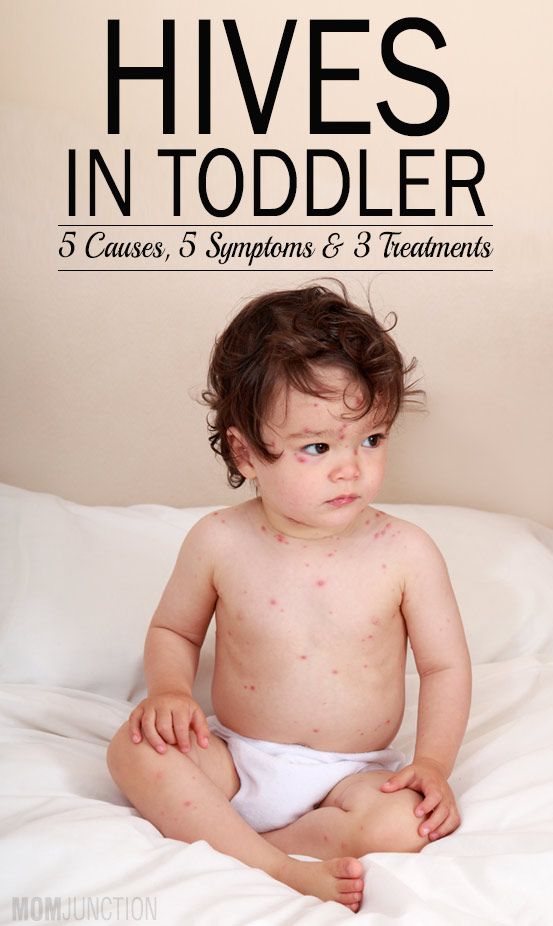
If the rash doesn't go away or your baby develops a persistent bright red, moist rash with white or red pimples that spreads into the folds of their skin, they may have an infection.
Ask a pharmacist or health visitor for advice. The pharmacist may recommend a cream for you to use.
If the rash is severe, take your baby to the GP who may prescribe cream or medicine. Follow a GP's instructions on whether and when to apply barrier cream as well as the prescribed cream.
It's normal for babies to develop skin rashes, but it's important to know the difference between a minor irritation and a condition that requires attention.
Read more about rashes in babies and children.
Page last reviewed: 17 September 2021
Next review due: 17 September 2024
Slapped cheek syndrome - NHS
Slapped cheek syndrome (also called fifth disease) is common in children and should get better on its own within 3 weeks. It's rarer in adults, but can be more serious.
It's rarer in adults, but can be more serious.
Check if it's slapped cheek syndrome
The first sign of slapped cheek syndrome is usually feeling unwell for a few days.
Symptoms may include:
- a high temperature
- a runny nose and sore throat
- a headache
Credit:
SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/550792/view
A few days later, a spotty rash may appear on the chest, arms and legs. The rash can be raised and itchy. It may be harder to see on brown and black skin.Credit:
John Kaprielian/SCIENCE PHOTO LIBRARY https://www. sciencephoto.com/media/618192/view
sciencephoto.com/media/618192/view
How long it lasts
The cheek rash usually fades within 2 weeks.
The body rash also fades within 2 weeks, but sometimes lasts for up to a month, especially if you're exercising, hot, anxious or stressed.
Adults might also have joint pain and stiffness. This can happen in children too, but it's rare. Joint pain can continue for many weeks, even after the other symptoms have gone.
If you're not sure your child has slapped cheek syndrome
Look at other rashes in babies and children.
Things you can do yourself
You do not usually need to see a GP for slapped cheek syndrome.
There are some things you can do to ease the symptoms.
Do
-
rest
-
drink plenty of fluids to avoid dehydration – babies should continue their normal feeds
-
take paracetamol or ibuprofen for a high temperature, headaches or joint pain
-
use moisturiser on itchy skin
-
speak to a pharmacist about itchy skin – they can recommend the best antihistamine for children
Important
Tell your midwife or a GP if you're pregnant or have a weakened immune system and have been near someone with slapped cheek syndrome.
Non-urgent advice: See a GP if:
you think you have slapped cheek syndrome and:
- you're pregnant – there's a very small risk of miscarriage or other complications
- you have a blood disorder, such as sickle cell disease or thalassaemia – there's a risk of severe anaemia
- you have a weakened immune system – for example, because of chemotherapy or diabetes
Ask for an urgent appointment if you have:
- very pale skin
- shortness of breath
- extreme tiredness
- fainting
These can be signs of severe anaemia and you might be sent to hospital for a blood transfusion.
How slapped cheek syndrome is spread
It's hard to avoid spreading slapped cheek syndrome because most people do not know they have it until they get the rash.
You can only spread it to other people before the rash appears.
Slapped cheek syndrome is caused by a virus (parvovirus B19). The virus spreads to other people, surfaces or objects by coughing or sneezing near them.
To reduce the risk of spreading the virus:
- wash your hands often with water and soap
- use tissues to trap germs when you cough or sneeze
- bin used tissues as quickly as possible
Information:
You do not have to stay off work or school after the rash appears.
Let the school or teacher know if your child has slapped cheek syndrome.
Page last reviewed: 18 February 2021
Next review due: 18 February 2024
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception.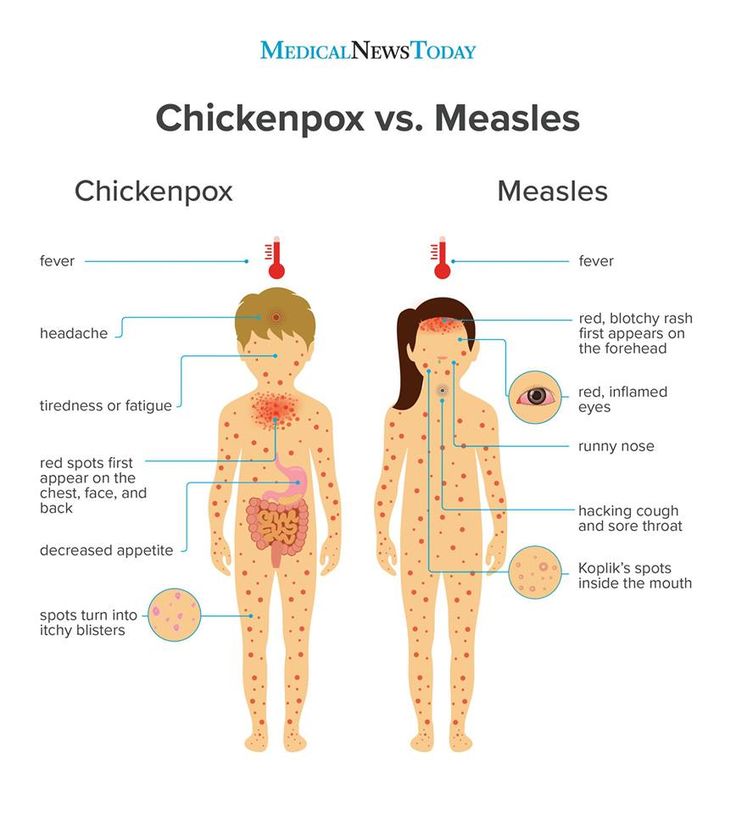 We try to make friends with the child and do everything to make the little patient feel comfortable with us.
We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the website
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child nine0034
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment nine0034
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
- nine0079
Causes of a rash in children
Naturally, only a pediatrician, dermatologist or allergist can correctly determine the cause of the rash , diagnose and prescribe treatment for a child. But provide initial assistance, relieve itching and the parents themselves can help the baby, knowing the main signs and causes of rash . At the first stage, it is important to determine the nature of the rash - infectious , allergic or none of the above.
But provide initial assistance, relieve itching and the parents themselves can help the baby, knowing the main signs and causes of rash . At the first stage, it is important to determine the nature of the rash - infectious , allergic or none of the above.
Causes of rashes in children:
1. Newborn acne . For the first time may occur in newborns at the age of 1 - 2 months. As a rule, such rashes are hormonal in nature, are not contagious and are not allergic . A rash in the form of pimples, sometimes with a white dot in the middle, appears on the head, body of the baby. If there are no purulent compartments, then the rash goes away on its own and does not require treatment. Acne can also occur in teenagers. They most often appear on the face in the form of black dots and are associated with hormonal changes in the body of a teenager and an increased work of the sebaceous glands. 2. Urticaria is an allergic reaction on the child's skin, accompanied by itching and the appearance of blisters on various parts of the body, in some cases the temperature may rise and the child's stool is disturbed. Blisters appear suddenly and can also disappear quickly, but sometimes they disappear only after a few days. The causes of urticaria can be various factors: hormonal disorders, malfunctions of the liver, kidneys, consumption of foods that caused an allergic reaction (fish, eggs, citrus fruits, etc.), insect bites, reaction to sunlight, temperature changes, emotional stress etc. Urticaria can be chronic does not go away for a long time, and acute disappears after a few hours. 3. Food allergy manifests as pinkish-red spots. It is slightly convex, edematous in places of scratching and is accompanied by itching. It is localized, as a rule, on the baby's cheeks, but can also appear on other parts of the body. It can occur in both infants and adolescents. If the baby is breastfed, then the allergy that has arisen is associated with the products consumed by the mother. If the newborn is artificially fed, then an allergic reaction may appear on the mixture. In older children, food allergies can be caused by fish, eggs, nuts, chocolate, strawberries, and other foods; nine0003 Allergy, as a rule, is accompanied by edema, which in turn, if not properly treated and provided with untimely assistance, cause suffocation . If an allergy of any nature occurs, a pediatrician's consultation is required to help in choosing the optimal mixture for the baby, or a pediatric dermatologist - allergist for referral to laboratory tests of older children ; 4. 5. Prickly heat . It occurs mainly in infants. It manifests itself in the form of red pimples all over the body, especially in the inguinal zone. The affected areas must be smeared with a special baby cream, air baths for the baby more often and a diaper change; nine0003 6. Roseola (erythema infectiosum) is an acute childhood viral disease affecting only children under 2 years of age. Very often, roseola is confused with SARS or rubella . 7. Windmill . This is a common childhood infectious disease that requires treatment. The incubation period of this disease can last from 11 to 21 days. Occurs at any age. It is accompanied by a rash on the skin and mucous membranes in the form of red spots, in the center of which blisters with a yellowish liquid are localized. Accompanied by itching. As the disease progresses, the blisters burst, crusts form, leaving scars if the child has scratched the blister and brought the infection. The disease can also cause fever and headache; nine0003 8. Measles is an acute infectious disease that is quite rare due to the use of vaccinations. 9. Scarlet fever is an acute infectious streptococcal disease. Begins with sore throat, high temperature, enlarged tonsils , in some cases with plaque. Then a small dotted rash appears on the back, chest, knees, armpits, groin and quickly spreads throughout the body and face. 10. Rubella is an acute infectious disease . The disease begins with a slight increase in temperature and enlargement of the lymph nodes in the parotid and cervical region. A small rash also appears on the face and behind the ears, and then all over the body. Rubella is very dangerous for pregnant women, and complications can occur in older children and adolescents. In children, the disease proceeds in a fairly mild form; 11. Meningitis is an inflammation of the membranes of the brain and spinal cord. Rash in meningitis is not the main symptom. However, with this disease, rashes appear on the back of the throat, as well as on the hips, back, buttocks in the form of a red rash of various shapes. Symptoms of meningitis include very high fever, severe headache, vomiting, photophobia, and neck muscle tension. 12. Streptoderma is a skin infection caused by Staphylococcus aureus. The disease affects, as a rule, the paranasal and perioral region. In the beginning, redness appears around the nose and mouth, then small bubbles with liquid. When they burst, yellow crusts remain. The disease may be accompanied by fever; 13. Herpes is an infectious disease accompanied by the appearance of blisters on the skin and mucous membranes, in children it is most often located on the lips. This disease is extremely rare in newborns, because. they are given maternal immunity. It affects children from 3 to 4 years of age. In addition to a rash, the disease may be accompanied by a sore throat, fever. nine0003 There are a lot of skin rashes and diseases in children, they can be very similar, but some are completely harmless to your child's health, while others pose a threat not only to the general condition, but also to the child's life! Do not take risks, and if you have any doubts, if any spots, rashes and other symptoms appear, contact your pediatrician, who, if necessary, will refer you and your child to a pediatric dermatologist, allergist, neurologist or other highly specialized specialist, depending on the nature of the rash and the severity of the skin disease. To prevent acne, there are cosmetic lotions, washing gels and other products. In case of inflammation, it is better to seek advice from a pediatric dermatologist or cosmetologist, because. antibiotic treatment may be needed; nine0003
To prevent acne, there are cosmetic lotions, washing gels and other products. In case of inflammation, it is better to seek advice from a pediatric dermatologist or cosmetologist, because. antibiotic treatment may be needed; nine0003  For the treatment of urticaria, it is important to identify the underlying cause that caused it;
For the treatment of urticaria, it is important to identify the underlying cause that caused it;  Household allergies . It can occur in both newborns and older children. It usually appears as pimples all over the body and is accompanied by lachrymation, sneezing. The causes of such a reaction of the body can be washing powder and other detergents, dust, plants, animal hair, etc. An allergic rash differs from an infectious rash in that the child does not have a temperature with it, he does not have general ailments, there is no loss of appetite, drowsiness;
Household allergies . It can occur in both newborns and older children. It usually appears as pimples all over the body and is accompanied by lachrymation, sneezing. The causes of such a reaction of the body can be washing powder and other detergents, dust, plants, animal hair, etc. An allergic rash differs from an infectious rash in that the child does not have a temperature with it, he does not have general ailments, there is no loss of appetite, drowsiness; 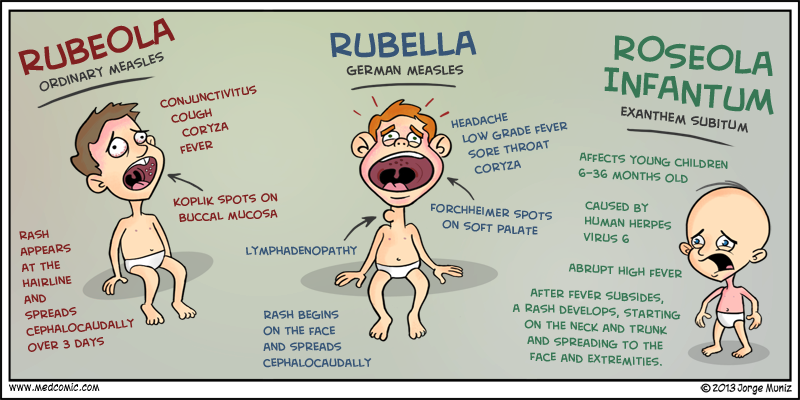 At the beginning of the illness, the baby's temperature rises sharply, which lasts 3-5 days, and after that the child becomes covered with a red-pink rash that disappears in 5-7 days. This is not a dangerous disease, it does not require treatment, and if it occurs, the child should be given only antipyretic drugs;
At the beginning of the illness, the baby's temperature rises sharply, which lasts 3-5 days, and after that the child becomes covered with a red-pink rash that disappears in 5-7 days. This is not a dangerous disease, it does not require treatment, and if it occurs, the child should be given only antipyretic drugs;  In addition, this virus is rarely activated in babies under 8 months old, because. they are protected by their mother's immunity. The disease begins with symptoms of a common cold - coughing, lacrimation, sneezing and fever up to 40 C. Then the child develops white spots on the mucous surface of the cheeks, nasal discharge, severe headache, photophobia. Then, within a few days, red spots of various shapes appear on the face, neck, near the head and further throughout the body. The disease is contagious within a week of the onset of the first symptoms. The virus is dangerous with complications such as: meningitis , pneumonia , development of deafness, brain damage and even death;
In addition, this virus is rarely activated in babies under 8 months old, because. they are protected by their mother's immunity. The disease begins with symptoms of a common cold - coughing, lacrimation, sneezing and fever up to 40 C. Then the child develops white spots on the mucous surface of the cheeks, nasal discharge, severe headache, photophobia. Then, within a few days, red spots of various shapes appear on the face, neck, near the head and further throughout the body. The disease is contagious within a week of the onset of the first symptoms. The virus is dangerous with complications such as: meningitis , pneumonia , development of deafness, brain damage and even death;  Only the area around the mouth remains white. Throat and tongue become very red. By the end of the disease, peeling of the skin on the toes and hands begins; nine0003
Only the area around the mouth remains white. Throat and tongue become very red. By the end of the disease, peeling of the skin on the toes and hands begins; nine0003 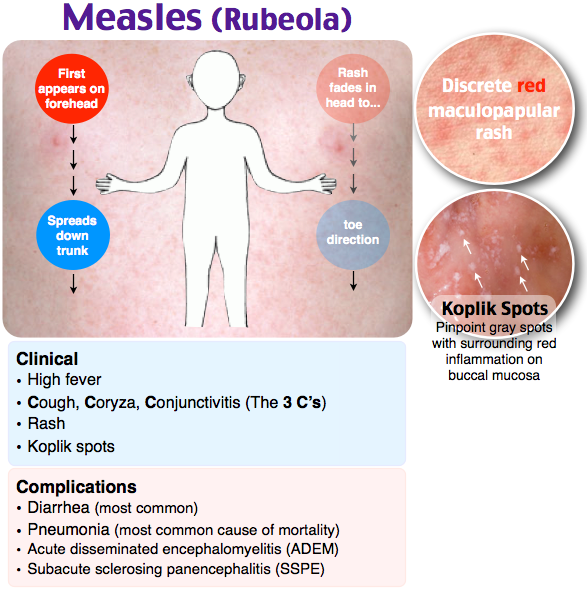 At the slightest suspicion of meningitis, parents should immediately consult a doctor. Timely help with this disease will save the child's life; nine0003
At the slightest suspicion of meningitis, parents should immediately consult a doctor. Timely help with this disease will save the child's life; nine0003