Rash from milk allergy in infant
Dairy allergy rash in babies: Pictures, symptoms, and treatment
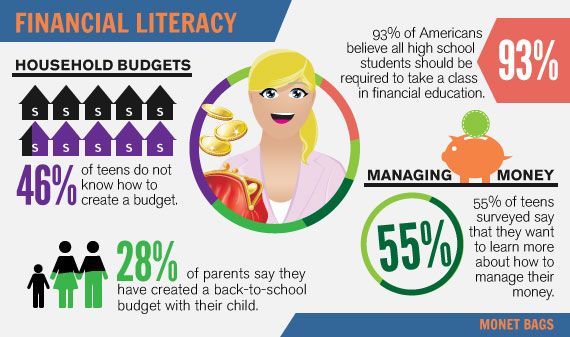
Babies often develop rashes, and finding a cause is often difficult. However, rashes on a baby’s face may result from a cow milk allergy.
A dairy allergy rash may be raised, discolored, and itchy. Rashes can appear suddenly or gradually. Additionally, they may worsen or improve over time.
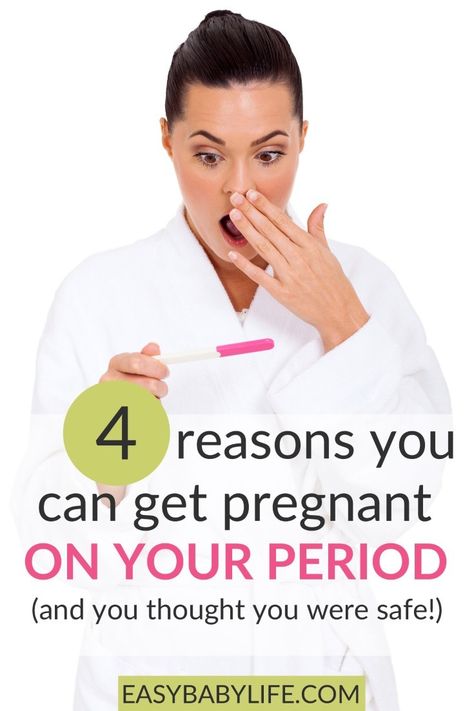
A cow milk allergy is one of the most common food allergies globally. In the United States, 1.9% of children have a milk allergy.
Some babies show symptoms of a dairy allergy or intolerance before they begin eating solid foods. This is because breast milk and formula often contain cow milk proteins.
Milk proteins in a breastfeeding person’s diet can pass into breast milk and cause a reaction in sensitized babies. Most formulas contain cow’s milk, but dairy-free options are available.
Allergic reactions can vary from mild to severe. Symptoms in babies include a rash, wheezing, and swelling around the mouth.
This article looks at the symptoms of a dairy allergy in infants and discusses what else may cause a rash. It will also explain when to contact a doctor about a rash.
Find more images of rashes here.
A dairy allergy is an overresponse by the body’s immune system to proteins in cow’s milk. There are many proteins in milk, but casein and whey are the most likely to be allergens.
There are two types of milk allergy:
- IgE-mediated: The immune system reacts to milk proteins by creating immunoglobulin (IgE) antibodies. The immune system then releases chemicals, such as histamines, which trigger an allergic reaction. Symptoms of an IgE-mediated allergic reaction can appear within minutes of consuming dairy. This type of allergy can lead to anaphylaxis, which can be life threatening.
- Non-IgE-mediated: Other parts of the immune system react to milk proteins and cause symptoms, often involving the digestive tract. Symptoms do not appear immediately.
 This type of reaction does not involve IgE antibodies.
This type of reaction does not involve IgE antibodies.
Learn more about milk allergy in babies here.
An IgE-mediated milk allergy can be life threatening, so it is vital to know the symptoms. Symptoms of an IgE-mediated milk allergy appear within 5–30 minutes of ingesting milk and include:
If a baby has an IgE-mediated milk allergy, a pediatrician may prescribe an epinephrine auto-injector (EpiPen). Caregivers will receive training on how to use it in an emergency. If a baby displays the severe symptoms above, a caregiver should administer epinephrine and then call 911.
Symptoms of a non-IgE-mediated milk allergy may take hours or days to appear and include:
Learn about baby poop and milk allergy here.
Could it be lactose intolerance?
A milk allergy is more common than lactose intolerance in children under 5 years old. Very few babies have lactose intolerance, which usually develops later in life.
Babies develop lactose intolerance when they are born without the enzyme necessary to digest lactose, a sugar in milk.
If a baby develops symptoms after consuming cow’s milk, they are more likely to have a milk allergy than lactose intolerance.
Learn more about lactose intolerance here.
Skin rashes are common in babies and can have many causes, including:
- diaper rash
- baby acne
- slapped cheek syndrome
- hand, foot, and mouth disease
- scarlet fever
- heat rash
- eczema
- ringworm
- chickenpox
- impetigo
- scabies
- erythema toxicum, which causes raised red, yellow, and white spots
- molluscum contagiosum, which causes small, firm, raised spots that may be skin-colored or darker, and pink
- milia, which are tiny white or yellow spots
The American Academy of Dermatology Association notes that some children with COVID-19 develop multisystem inflammatory syndrome in children (MIS-C). This condition can cause a rash. The symptoms include:
- fever
- abdominal pain
- vomiting
- diarrhea
- rash
- bloodshot eyes
If a child develops these symptoms, caregivers should contact a doctor immediately.
In many cases, a rash does not have a serious cause. If caregivers are concerned about a rash and other symptoms, they can talk with a doctor.
Most rashes will disappear on their own and do not require any special treatment. A baby’s skin is very delicate, so caregivers should avoid applying medication unless a doctor prescribes it for the baby.
Tips for looking after a baby’s skin include:
- Avoid rubbing and scrubbing the baby’s delicate skin.
- Use a soft washcloth to gently wipe away any milk, formula, or spit-up to avoid it sitting on the skin.
- Keep skin cleaning to a minimum to avoid stripping the skin of its natural oils.
- Use fragrance-free, hypoallergenic products.
- Avoid products containing perfumes or dyes.
- Use water that is lukewarm, not hot.
- Use physical barriers, such as clothing, hats, umbrellas, and shade, to protect a baby’s skin from the sun.
Find 27 natural and organic baby products here.
If a baby has symptoms of a dairy allergy, their caregiver should make a doctor’s appointment as soon as possible. The doctor may refer them to an allergist for testing and diagnosis.
If the child displays the following symptoms, call 911 for emergency medical help:
- shortness of breath
- a tight or swollen face
- a purple or discolored rash that looks like a bruise
The box below explains what to do in the event of anaphylaxis.
Anaphylaxis is a severe allergic reaction that can be life threatening. The symptoms develop suddenly and include:
- hives
- swelling of the face or mouth
- wheezing
- fast, shallow breathing
- a fast heart rate
- clammy skin
- anxiety or confusion
- dizziness
- vomiting
- blue or white lips
- fainting or loss of consciousness
If someone has these symptoms:
- Check whether they are carrying an epinephrine pen. If they are, follow the instructions on the side of the pen to use it.

- Dial 911 or the number of the nearest emergency department.
- Lay the person down from a standing position. If they have vomited, turn them onto their side.
- Stay with them until the emergency services arrive.
Some people may need more than one epinephrine injection. If the symptoms do not improve in 5–15 minutes, or they come back, use a second pen if the person has one.
According to the American College of Allergy, Asthma, and Immunology, 2–3% of children under 3 have a milk allergy. Around 20% of children outgrow their allergy by the age of 3.
About 80% of children outgrow their milk allergy before they are 16.
The only way to avoid allergic reactions in babies with a cow milk allergy is to avoid giving them cow’s milk or food containing it, including certain infant formulas. People who breastfeed should also avoid consuming milk products, as milk proteins can pass into breast milk.
Rashes are common in babies and young children, and they have many causes.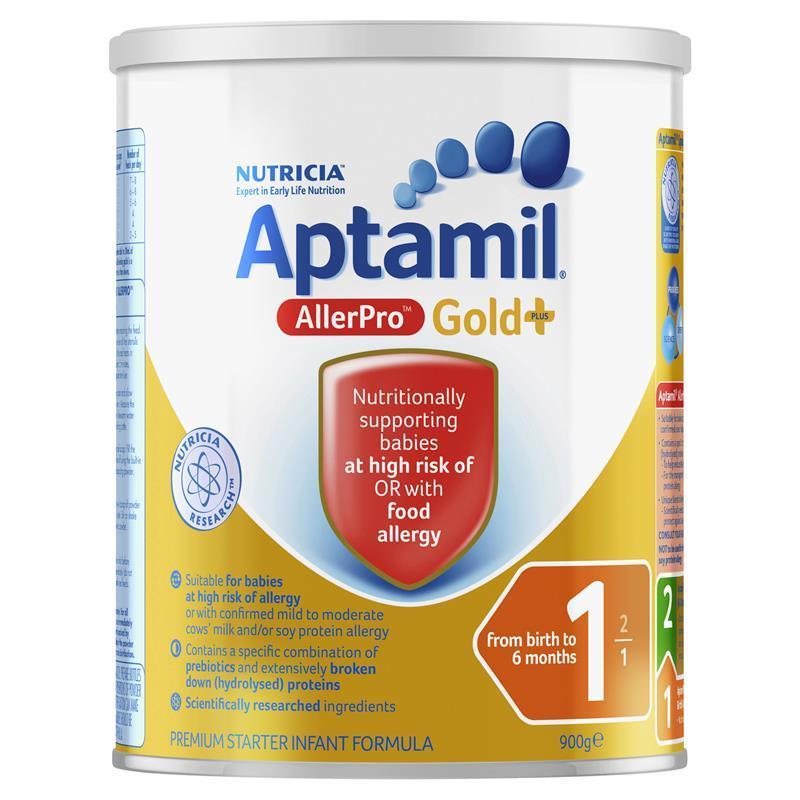 Milk allergies are also common and cause symptoms ranging from mild to severe.
Milk allergies are also common and cause symptoms ranging from mild to severe.
Rapid allergic reactions to milk may cause skin symptoms, such as itchy, raised, and red or discolored bumps.
A baby may also experience swelling around the mouth, difficulty breathing, and agitation. If a baby experiences these symptoms, caregivers should call 911 immediately.
Delayed allergic reactions may cause skin symptoms, such as eczema, rashes that come and go, and skin flushing. This type of reaction may also cause digestive symptoms, such as gas, diarrhea, or bloody stool. Caregivers should make a doctor’s appointment. The doctor may advise allergy testing.
Many other conditions can cause a skin rash. In many cases, a rash will clear without treatment.
Caregivers should care for a baby’s delicate skin by using mild, hypoallergenic products, lukewarm water, and avoiding rubbing.
Dairy allergy rash in babies: Pictures, symptoms, and treatment
Babies often develop rashes, and finding a cause is often difficult. However, rashes on a baby’s face may result from a cow milk allergy.
However, rashes on a baby’s face may result from a cow milk allergy.
A dairy allergy rash may be raised, discolored, and itchy. Rashes can appear suddenly or gradually. Additionally, they may worsen or improve over time.
A cow milk allergy is one of the most common food allergies globally. In the United States, 1.9% of children have a milk allergy.
Some babies show symptoms of a dairy allergy or intolerance before they begin eating solid foods. This is because breast milk and formula often contain cow milk proteins.
Milk proteins in a breastfeeding person’s diet can pass into breast milk and cause a reaction in sensitized babies. Most formulas contain cow’s milk, but dairy-free options are available.
Allergic reactions can vary from mild to severe. Symptoms in babies include a rash, wheezing, and swelling around the mouth.
This article looks at the symptoms of a dairy allergy in infants and discusses what else may cause a rash. It will also explain when to contact a doctor about a rash.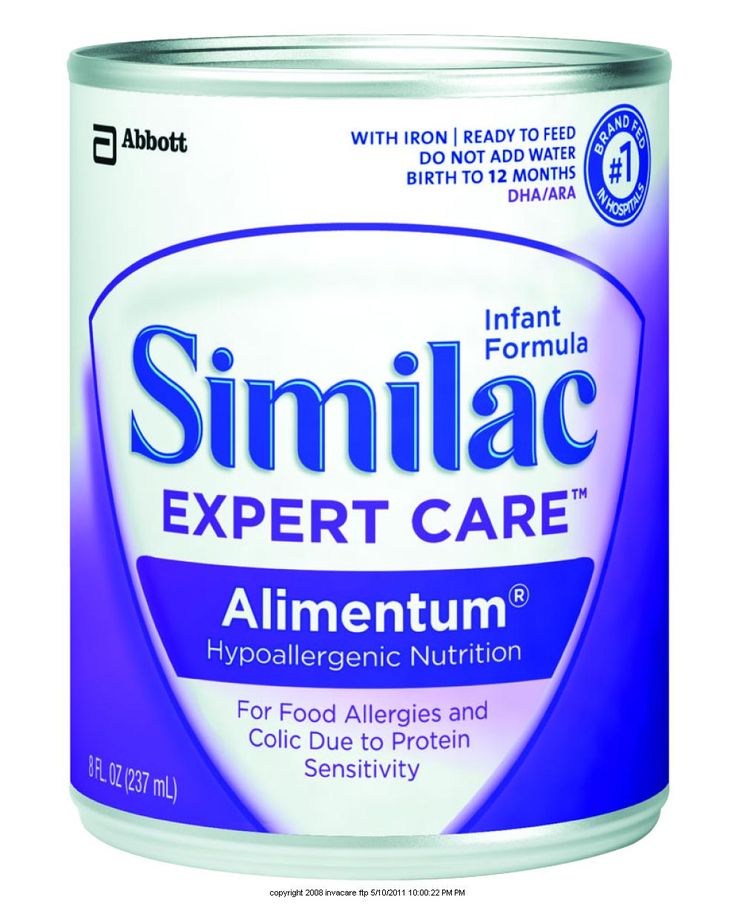
Find more images of rashes here.
A dairy allergy is an overresponse by the body’s immune system to proteins in cow’s milk. There are many proteins in milk, but casein and whey are the most likely to be allergens.
There are two types of milk allergy:
- IgE-mediated: The immune system reacts to milk proteins by creating immunoglobulin (IgE) antibodies. The immune system then releases chemicals, such as histamines, which trigger an allergic reaction. Symptoms of an IgE-mediated allergic reaction can appear within minutes of consuming dairy. This type of allergy can lead to anaphylaxis, which can be life threatening.
- Non-IgE-mediated: Other parts of the immune system react to milk proteins and cause symptoms, often involving the digestive tract. Symptoms do not appear immediately. This type of reaction does not involve IgE antibodies.
Learn more about milk allergy in babies here.
An IgE-mediated milk allergy can be life threatening, so it is vital to know the symptoms. Symptoms of an IgE-mediated milk allergy appear within 5–30 minutes of ingesting milk and include:
Symptoms of an IgE-mediated milk allergy appear within 5–30 minutes of ingesting milk and include:
If a baby has an IgE-mediated milk allergy, a pediatrician may prescribe an epinephrine auto-injector (EpiPen). Caregivers will receive training on how to use it in an emergency. If a baby displays the severe symptoms above, a caregiver should administer epinephrine and then call 911.
Symptoms of a non-IgE-mediated milk allergy may take hours or days to appear and include:
Learn about baby poop and milk allergy here.
Could it be lactose intolerance?
A milk allergy is more common than lactose intolerance in children under 5 years old. Very few babies have lactose intolerance, which usually develops later in life.
Babies develop lactose intolerance when they are born without the enzyme necessary to digest lactose, a sugar in milk.
If a baby develops symptoms after consuming cow’s milk, they are more likely to have a milk allergy than lactose intolerance.
Learn more about lactose intolerance here.
Skin rashes are common in babies and can have many causes, including:
- diaper rash
- baby acne
- slapped cheek syndrome
- hand, foot, and mouth disease
- scarlet fever
- heat rash
- eczema
- ringworm
- chickenpox
- impetigo
- scabies
- erythema toxicum, which causes raised red, yellow, and white spots
- molluscum contagiosum, which causes small, firm, raised spots that may be skin-colored or darker, and pink
- milia, which are tiny white or yellow spots
The American Academy of Dermatology Association notes that some children with COVID-19 develop multisystem inflammatory syndrome in children (MIS-C). This condition can cause a rash. The symptoms include:
- fever
- abdominal pain
- vomiting
- diarrhea
- rash
- bloodshot eyes
If a child develops these symptoms, caregivers should contact a doctor immediately.
In many cases, a rash does not have a serious cause. If caregivers are concerned about a rash and other symptoms, they can talk with a doctor.
Most rashes will disappear on their own and do not require any special treatment. A baby’s skin is very delicate, so caregivers should avoid applying medication unless a doctor prescribes it for the baby.
Tips for looking after a baby’s skin include:
- Avoid rubbing and scrubbing the baby’s delicate skin.
- Use a soft washcloth to gently wipe away any milk, formula, or spit-up to avoid it sitting on the skin.
- Keep skin cleaning to a minimum to avoid stripping the skin of its natural oils.
- Use fragrance-free, hypoallergenic products.
- Avoid products containing perfumes or dyes.
- Use water that is lukewarm, not hot.
- Use physical barriers, such as clothing, hats, umbrellas, and shade, to protect a baby’s skin from the sun.
Find 27 natural and organic baby products here.
If a baby has symptoms of a dairy allergy, their caregiver should make a doctor’s appointment as soon as possible. The doctor may refer them to an allergist for testing and diagnosis.
If the child displays the following symptoms, call 911 for emergency medical help:
- shortness of breath
- a tight or swollen face
- a purple or discolored rash that looks like a bruise
The box below explains what to do in the event of anaphylaxis.
Anaphylaxis is a severe allergic reaction that can be life threatening. The symptoms develop suddenly and include:
- hives
- swelling of the face or mouth
- wheezing
- fast, shallow breathing
- a fast heart rate
- clammy skin
- anxiety or confusion
- dizziness
- vomiting
- blue or white lips
- fainting or loss of consciousness
If someone has these symptoms:
- Check whether they are carrying an epinephrine pen. If they are, follow the instructions on the side of the pen to use it.

- Dial 911 or the number of the nearest emergency department.
- Lay the person down from a standing position. If they have vomited, turn them onto their side.
- Stay with them until the emergency services arrive.
Some people may need more than one epinephrine injection. If the symptoms do not improve in 5–15 minutes, or they come back, use a second pen if the person has one.
According to the American College of Allergy, Asthma, and Immunology, 2–3% of children under 3 have a milk allergy. Around 20% of children outgrow their allergy by the age of 3.
About 80% of children outgrow their milk allergy before they are 16.
The only way to avoid allergic reactions in babies with a cow milk allergy is to avoid giving them cow’s milk or food containing it, including certain infant formulas. People who breastfeed should also avoid consuming milk products, as milk proteins can pass into breast milk.
Rashes are common in babies and young children, and they have many causes.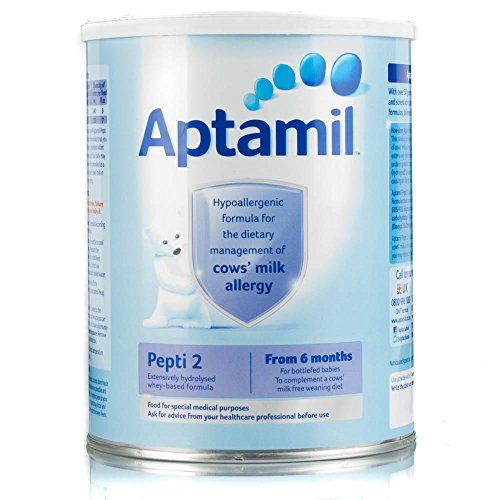 Milk allergies are also common and cause symptoms ranging from mild to severe.
Milk allergies are also common and cause symptoms ranging from mild to severe.
Rapid allergic reactions to milk may cause skin symptoms, such as itchy, raised, and red or discolored bumps.
A baby may also experience swelling around the mouth, difficulty breathing, and agitation. If a baby experiences these symptoms, caregivers should call 911 immediately.
Delayed allergic reactions may cause skin symptoms, such as eczema, rashes that come and go, and skin flushing. This type of reaction may also cause digestive symptoms, such as gas, diarrhea, or bloody stool. Caregivers should make a doctor’s appointment. The doctor may advise allergy testing.
Many other conditions can cause a skin rash. In many cases, a rash will clear without treatment.
Caregivers should care for a baby’s delicate skin by using mild, hypoallergenic products, lukewarm water, and avoiding rubbing.
Allergy to cow's milk protein in children
Food allergy is a food-induced adverse (pathological) reaction based on immune mechanisms. In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
A distinction is made between cow's milk protein allergy and cow's milk protein intolerance. In the first case immune mechanisms are involved, in the second - the baby simply does not have enough enzymes to digest cow's milk protein (for example, lactase deficiency).
There are only 36 cow's milk protein allergens, but 4 of them most often cause food allergies.
Casein is 80% BCM, it is heat stable (does not break down when boiled) and is not a species-specific protein. This means that if you are allergic to it, you may be allergic to the milk of other animal species.
β - lactoglobulin has the highest allergenic activity, species-specific, does not break down when boiled. This protein is not found in human milk.
α - lactalbumin is destroyed by boiling, species-specific.
Bovine serum albumin is not destroyed by boiling If an allergy to this cow's milk protein is detected, the child may also react to beef and veal meat.
It should be noted that mainly children who are bottle-fed with mixtures based on cow's milk protein suffer from cow's milk protein allergy.
This type of allergy can also develop in children who are breastfed - if the diet of a nursing mother contains products containing cow's milk protein (milk, cheese, cottage cheese, sour cream, butter, fermented milk products), especially in large quantities.
What symptoms suggest that the baby may be allergic to CMP:
- Skin manifestations (dry skin, dry nummular rashes, skin itching).
- Gastrointestinal manifestations (bloating, regurgitation, vomiting, loose stools, possibly stools with mucus and blood streaks).
- Respiratory manifestations (itchy eyes, cough, nasal congestion and even urticaria and Quincke's edema).
 These symptoms are rare in toddlers, but still possible.
These symptoms are rare in toddlers, but still possible.
Diagnosis
I must say that if the first manifestations of a food allergy in a baby appeared after switching to artificial feeding with a "regular" adapted formula based on cow's milk, then this is a reason to suspect cow's milk proteins as an allergen.
The next thing is correct history taking : the doctor will definitely find out if anyone in your family suffers from allergic diseases (bronchial asthma, allergic rhinitis, atopic dermatitis, hay fever). If the family has these diseases, the risk of developing allergies in the baby increases.
At the discretion of the doctor, it is possible to take blood from a child for the presence of immunoglobulin E (IgE) antibodies to cow's milk proteins, which were mentioned above. In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy.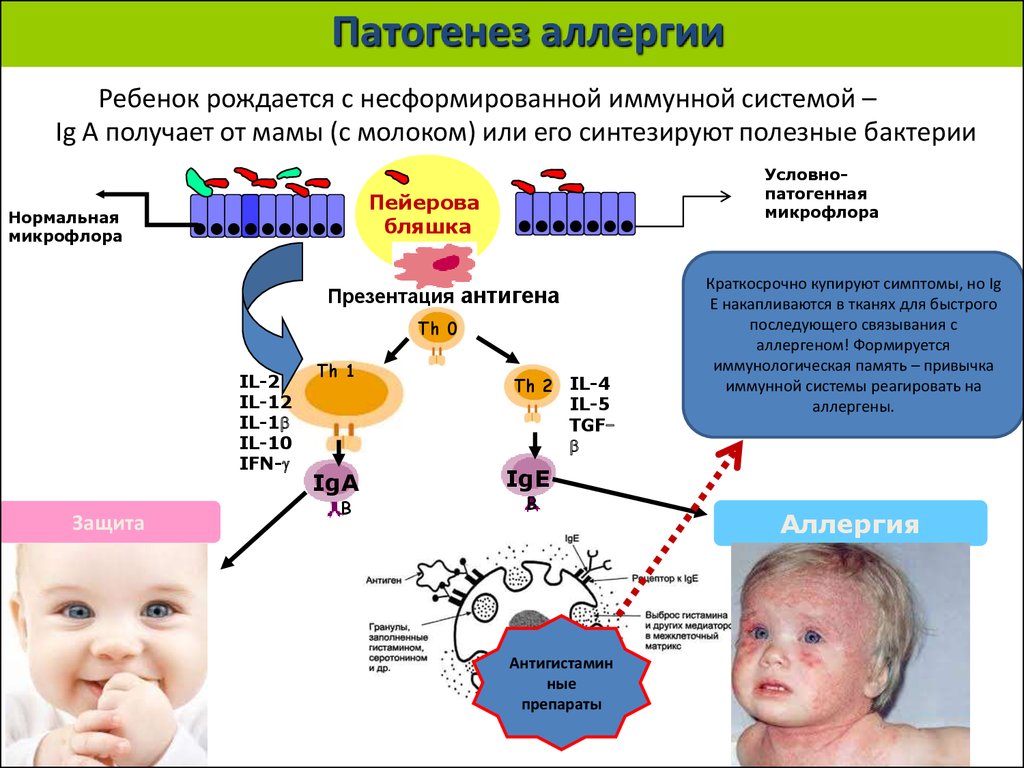 Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
And the simplest, most important and affordable method is the diagnostic diet with the exclusion of products from the child's diet (or from the mother's diet during breastfeeding) containing CMP. The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
If the child's condition improves, you may need challenge test . This means the introduction of dairy products into the child's diet again. And if the manifestations of allergies return, this will prove an allergy to BCM. This test is carried out under strict medical supervision.
In children who are fed exclusively with breast milk, it is necessary to exclude products containing CMP from the mother's diet .
There are 3 types of mixtures:
- based on the hydrolysis of whey proteins;
- based on the hydrolysis of the casein fraction;
- based on amino acids.
Allergy is possible for the first two options, the reaction is very unlikely for the third option.
If the baby is bottle-fed, then it must be transferred to amino acid blend or highly hydrolyzed blend. Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Usually, allergists first transfer children to mixtures based on complete hydrolysis of BCM or casein, if there is no proper effect within 2-3 weeks, it is recommended to transfer the baby to an amino acid mixture.
Perhaps, if the child has severe manifestations of food allergies, the doctor will advise you to immediately transfer the baby to an amino acid mixture. By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
Amino acid mixtures are more easily tolerated by children with various forms of food allergies, as they do not have the bitter taste characteristic of mixtures with a high degree of protein hydrolysis.
Amino acid mixtures can be used both for the short term diagnosis of CMP allergy and as a dietary base for long term use in children with food allergies.
Diet duration — at least 6 months . Then the issue of transferring the baby to a hypoallergenic mixture is decided. In case of recurrence of symptoms, the introduction of dairy products is postponed for another 6 months.
The prognosis for CMP allergy in infants and young children with the correct management of patients is favorable.
Approximately 50% of children by the age of 1 year can be introduced into the diet of foods that include CMP. More than 75% of children by age 3 or older 90% of children by the age of 6 do not show allergic reactions to CMP.
More than 75% of children by age 3 or older 90% of children by the age of 6 do not show allergic reactions to CMP.
Cow's milk protein allergy in children (CMP)
Cow's milk protein allergy (common abbreviation - CMP) ranks first among all allergies in children of the first year of life.
The article was written by leading allergist-immunologist, Euromed Kids pediatrician Artem Andreevich Batin
0012 intolerant to cow's milk.
Allergy to milk protein is due to the fact that the child's immune system perceives this protein as foreign and activates the body's defense reactions.
Milk intolerance is the result of insufficient work or an insufficient amount of enzymes necessary for its digestion. This condition is called lactase deficiency , and it is quite successfully corrected by the additional intake of enzymes.
Important: even if the baby is exclusively breastfed, allergies can occur if milk is present in the mother's diet.

One of the most common manifestations of cow's milk protein allergy is atopic dermatitis .
Favorite localizations - face, especially cheeks, elbows, popliteal fossae, but often elements appear on the body. At first, the skin becomes dry, and with an increase in symptoms, cracks, weeping, and crusts appear.
More about atopic dermatitis…
In addition to the so-called “skin symptoms”, there are other manifestations associated with the digestive system:
- regurgitation;
- vomiting;
- intestinal colic;
- flatulence, diarrhoea;
- the child worries, cries, does not sleep well.
IMPORTANT! Information from the article cannot be used for self-diagnosis and self-treatment! Only a doctor can prescribe the necessary examinations, establish a diagnosis and draw up a treatment plan for a consultation!
If you notice even some of these symptoms, bring them to the attention of a pediatrician who constantly monitors your child.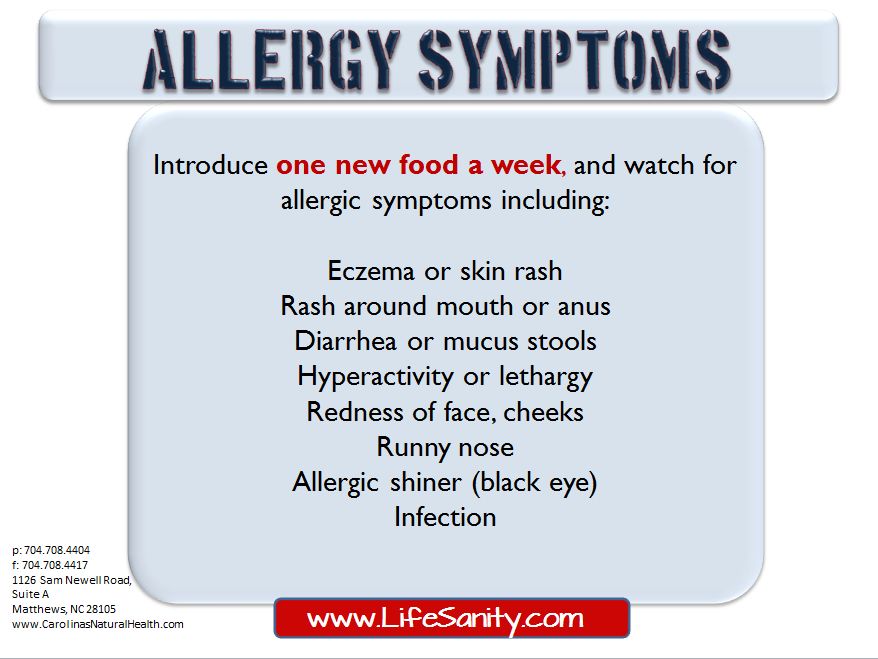 You will also need to consult a pediatric allergist-immunologist to clarify the diagnosis.
You will also need to consult a pediatric allergist-immunologist to clarify the diagnosis.
At the appointment, the doctor will conduct a thorough survey of the parents to clarify all the characteristics of the child, assess the symptoms of the disease, and, if necessary, recommend an allergological examination to confirm the diagnosis.
The treatment of cow's milk protein allergy is to follow a special diet , which completely eliminates the ingress of the allergen (protein) into the child's body.
To restore and care for the skin, the doctor will definitely recommend various products and emollients that will restore the integrity of the skin and sufficiently moisturize it.
If the child is breastfed , then a diet that completely excludes milk and products containing milk is intended for the mother. Especially carefully you need to monitor the content of milk in various semi-finished products, cookies, etc.
If the baby is formula-fed , the attending physician will certainly recommend several special therapeutic mixtures.