How does a child get hand foot and mouth
Causes & Transmission of Hand, Foot, and Mouth Disease
Español (Spanish) | Print
Hand, foot, and mouth disease spreads easily through
- Person-to-person contact
- Respiratory droplets containing virus particles when an infected person coughs or sneezes
- Contact with contaminated surfaces and objects
Hand, foot, and mouth disease is contagious
Hand, foot, and mouth disease is caused by viruses. A person infected with one of these viruses is contagious, which means that they can pass the virus to other people.
The virus can spread to others through an infected person’s
- Nose and throat secretions, such as saliva, drool, or nasal mucus
- Fluid from blisters or scabs
- Feces (poop)
People with hand, foot, and mouth disease are usually most contagious during the first week that they are sick. People can sometimes spread the virus to others for days or weeks after symptoms go away or if they have no symptoms at all.
How it spreads
You can get hand, foot, and mouth disease by
- Contact with respiratory droplets containing virus particles after a sick person coughs or sneezes
- Touching an infected person or making other close contact, like kissing, hugging, or sharing cups or eating utensils
- Touching an infected person’s feces, such as changing diapers, then touching your eyes, nose, or mouth
- Touching objects and surfaces that have the virus on them, like doorknobs or toys, then touching your eyes, nose, or mouth
Rarely, you can also get the viruses by swallowing recreational water, such as water in swimming pools. This can happen if the water is not properly treated with chlorine and becomes contaminated with feces from a person who has hand, foot, and mouth disease.
Hand, Foot, and Mouth Disease is Common
HFMD is common and in the U.S. occurs mostly in the summer and fall, but you can get it any time of year.
Because it is common and usually mild, children can continue to go to child care and schools as long as they:
- Have no fever.
- Have no uncontrolled drooling with mouth sores.
- Feel well enough to participate in classroom activities.
Talk with your child’s healthcare provider if you are still not sure when it is okay for them to return. In some cases, the local health department may require children with HFMD to stay home to control an outbreak.
Viruses that cause hand, foot, and mouth disease
Hand, foot, and mouth disease is caused by viruses that belong to the Enterovirus family.
Common causes of hand, foot, and mouth disease are:
- Coxsackievirus A16 is typically the most common cause of hand, foot, and mouth disease in the United States. Other coxsackieviruses can also cause the illness.
- Coxsackievirus A6 can also cause HFMD and the symptoms may be more severe.
- Enterovirus 71 (EV-A71) has been associated with cases and outbreaks in East and Southeast Asia. Although rare, EV-A71 has been associated with more severe diseases such as encephalitis (swelling of the brain).
Animals do not get hand, foot, and mouth disease
Animals such as cattle, pigs, sheep, and goats can get foot and mouth disease (or hoof-and-mouth disease), which is different than hand, foot, and mouth disease.
Visit the USDA website to learn more about foot and mouth disease.
Prevent HFMD from spreading
Learn more
Related Topics
Prevention
Symptoms
Treatment
Hand-foot-and-mouth disease - Symptoms and causes
Overview
Hand-foot-and-mouth disease is a mild, contagious viral infection common in young children. Symptoms include sores in the mouth and a rash on the hands and feet. Hand-foot-and-mouth disease is most commonly caused by a coxsackievirus.
There's no specific treatment for hand-foot-and-mouth disease. Frequent hand-washing and avoiding close contact with people who have hand-foot-and-mouth disease may help lower your child's risk of infection.
Products & Services
- Book: Mayo Clinic Guide to Raising a Healthy Child
- Book: Mayo Clinic Guide to Your Baby's First Years
Symptoms
Hand-foot-and-mouth disease on the hand
Hand-foot-and-mouth disease on the hand
Hand-foot-and-mouth disease often causes a rash of painful, blister-like lesions on the palms of the hands. Rashes appear differently depending on skin tone.
Hand-foot-and-mouth disease on the foot
Hand-foot-and-mouth disease on the foot
Hand-foot-and-mouth disease often causes a rash of painful, blister-like lesions on the soles of the feet. Rashes appear differently depending on skin tone.
Hand-foot-and-mouth disease may cause all of the following symptoms or only some of them.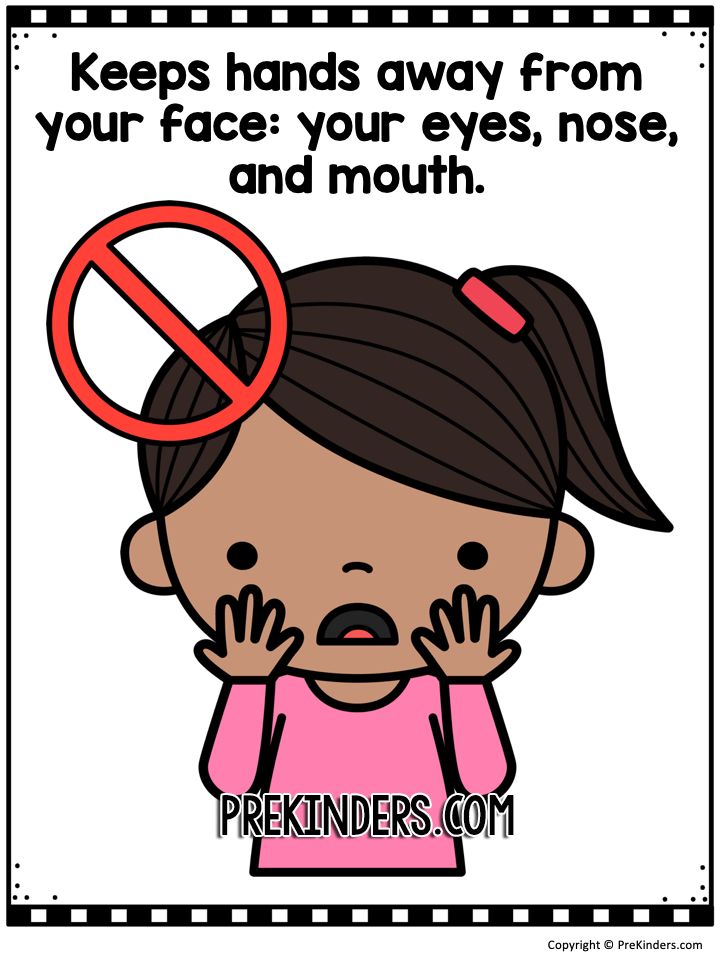 They include:
They include:
- Fever.
- Sore throat.
- Feeling sick.
- Painful, blister-like lesions on the tongue, gums and inside of the cheeks.
- A rash on the palms, soles and sometimes the buttocks. The rash is not itchy, but sometimes it has blisters. Depending on skin tone, the rash may appear red, white, gray, or only show as tiny bumps.
- Fussiness in infants and toddlers.
- Loss of appetite.
The usual period from initial infection to the time symptoms appear (incubation period) is 3 to 6 days. Children may get a fever and develop a sore throat. They sometimes lose their appetites and don't feel well.
One or two days after the fever begins, painful sores may develop in the front of the mouth or throat. A rash on the hands and feet and sometimes on the buttocks may also appear.
Sores that develop in the back of the mouth and throat may suggest a related viral illness called herpangina. Other features of herpangina include a sudden high fever and, in some instances, seizure.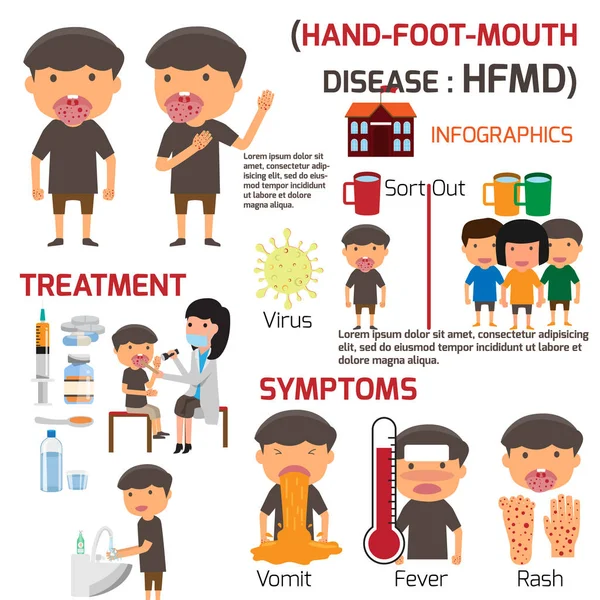 In rare cases, sores develop on the hands, feet or other parts of the body.
In rare cases, sores develop on the hands, feet or other parts of the body.
When to see a doctor
Hand-foot-and-mouth disease is usually a minor illness. It typically only causes fever and mild symptoms for a few days. Call your health care provider if your child is younger than six months, has a weakened immune system, or has mouth sores or a sore throat that makes it painful to drink fluids. Call your provider, too, if your child's symptoms don't improve after 10 days.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The most common cause of hand-foot-and-mouth disease is infection from coxsackievirus 16. This coxsackievirus belongs to a group of viruses called nonpolio enteroviruses. Other types of enteroviruses also may cause hand-foot-and-mouth disease.
Most people get the coxsackievirus infection — and hand-foot-and-mouth disease — through the mouth. The illness spreads by person-to-person contact with an infected person's:
- Nose secretions or throat discharge
- Saliva
- Fluid from blisters
- Stool
- Respiratory droplets sprayed into the air after a cough or sneeze
Common in child care setting
Hand-foot-and-mouth disease is most common in children in child care. That's because young children need frequent diaper changes and help using the toilet. They also tend to put their hands in their mouths.
That's because young children need frequent diaper changes and help using the toilet. They also tend to put their hands in their mouths.
Your child is most contagious during the first week of having hand-foot-and-mouth disease. But the virus can remain in the body for weeks after the symptoms go away. That means your child still can infect others.
Some people, especially adults, can pass the virus without showing any symptoms of the disease.
Outbreaks of the disease are more common in summer and early autumn in the United States. In tropical climates, outbreaks occur during the rainy season.
Different from foot-and-mouth disease
Hand-foot-and-mouth disease isn't related to foot-and-mouth disease (sometimes called hoof-and-mouth disease), which is an infectious viral disease found in farm animals. You can't get hand-foot-and-mouth disease from pets or other animals, and you can't spread it to them.
Risk factors
Age is the main risk factor for hand-foot-and-mouth disease. The disease mostly affects children younger than ages 5 to 7 years. Children in child care settings are especially vulnerable because the infection spreads by person-to-person contact.
The disease mostly affects children younger than ages 5 to 7 years. Children in child care settings are especially vulnerable because the infection spreads by person-to-person contact.
Hand-foot-mouth-disease typically affects young children, but anyone can get it.
Older children and adults are thought to have immunity against hand-foot-and-mouth disease. They often build antibodies after exposure to the viruses that cause the disease. But adolescents and adults sometimes still get hand-foot-and-mouth disease.
Complications
The most common complication of hand-foot-and-mouth disease is dehydration. The illness can cause sores in the mouth and throat, making it painful to swallow.
Encourage your child to drink fluids during the illness. If children become too dehydrated, they may need intravenous (IV) fluids in the hospital.
Hand-foot-and-mouth disease is usually a minor illness. It usually only causes fever and mild symptoms for a few days. Sometimes the enterovirus that causes hand-foot-and-mouth disease enters the brain and causes serious complications:
- Viral meningitis.
 This is a rare infection and inflammation of the membranes (meninges) and cerebrospinal fluid surrounding the brain and spinal cord.
This is a rare infection and inflammation of the membranes (meninges) and cerebrospinal fluid surrounding the brain and spinal cord. - Encephalitis. This severe and potentially life-threatening disease involves brain inflammation. Encephalitis is rare.
Prevention
You can lower your child's risk of hand-foot-and-mouth disease in many ways:
- Wash hands often. Wash your hands for at least 20 seconds. Be sure to wash your hands after using the toilet or changing a diaper. Also, wash your hands before preparing or eating food and after blowing your nose, sneezing or coughing. When soap and water aren't available, use hand sanitizer.
- Teach good hygiene. Show your children how to wash their hands and help them do it often. Show them how to practice overall good hygiene. Explain to them why it's best not to put their fingers, hands or any other objects in their mouths.
- Disinfect common areas.
 Clean high-traffic areas and surfaces first with soap and water. Next, clean with a diluted solution of chlorine bleach and water. If you're in a child care setting, follow a strict schedule of cleaning and disinfecting. The virus can live for days on surfaces in common areas, including on door knobs, and on shared items such as toys.
Clean high-traffic areas and surfaces first with soap and water. Next, clean with a diluted solution of chlorine bleach and water. If you're in a child care setting, follow a strict schedule of cleaning and disinfecting. The virus can live for days on surfaces in common areas, including on door knobs, and on shared items such as toys. - Avoid close contact. Because hand-foot-and-mouth disease is highly contagious, people with the illness should limit their exposure to others while they have symptoms. Keep children with hand-foot-and-mouth disease out of their child care setting or school until fever is gone and mouth sores have healed. If you have the illness, stay home from work.
By Mayo Clinic Staff
Related
News from Mayo Clinic
Products & Services
Motor development from 3 to 6 months
In the second half of the first half of the year, the body assumes more and more diverse postures, and the child has more and more opportunities to purposefully perform an increasing number of precisely coordinated movements.
In the supine position, the child can:
- By the beginning of the second trimester, grab an object located on the side of the grasping hand.
- Cross the center of the body to grab an object.
- Alternately use different sides of the body.
- Master your own feet by examining them, grabbing them with your hands and putting them in your mouth (hand-foot-mouth coordination).
- Perform various functions of the hands, for example, opening the palm with retraction with the spread of the metacarpal bones with the arm extended, the beginning of the opposition of the thumb. Both of these functions are important for the subsequent development of fine motor skills.
In the prone position, the child can:
- Perform one elbow support algorithm.
- Transfer the weight of the shoulder girdle to the supporting arm.
- Rest your knees on the bed in the first phase of the leg support function.

- Lean on a hand with an open, turned palm.
Development from the supine position
In the first half of the second trimester, the child begins to grasp objects with only one hand. which the object came into his field of vision. The child lacks objects that are interesting enough for him, provided that they are achievable for him. The preference of the right or left hand during this period does not play any role. If you calmly move the object to the center of the body, the child will follow the object with his eyes and reach for it with his hand. But when the object crosses the center and reaches the other side of the body, the child will change hands and grab the object with the other hand. Simultaneously with the grasping movement of the hand, the child imitates grasping movements with the feet. At the same time, grasping movements are performed by both feet, even if the child grabs with only one hand.
If a child at this age is offered an object in the center of the body, then the child, despite his desire to grab the object, will not be able to decide with which hand to do it. The reason for the difficulty of making this decision is, most likely, insufficient maturity for the coordinated work of both hemispheres of the brain. In the second half of the second trimester, the child's capabilities are noticeably expanded, which he had until now when grasping while lying on his back. If in the first half he had to change the grasping hand if the object crossed the center of the body, in the second half the child follows the object not only with his eyes, but also reaches for the object with the same hand, even if the object crossed the center of the body. When the child’s hand crosses the center body, the weight of the body is transferred to the second half of the body, resting on the shoulder.
This is how the child manages to use both sides of the body in different ways. The implementation of this new motor algorithm becomes achievable, since the child can coordinate the work of both hemispheres of the brain, which allows the distribution of work on both sides of the body: one half provides support, and the other makes movement. But the child uses this algorithm only on the condition that he considers the object of study interesting enough.
The implementation of this new motor algorithm becomes achievable, since the child can coordinate the work of both hemispheres of the brain, which allows the distribution of work on both sides of the body: one half provides support, and the other makes movement. But the child uses this algorithm only on the condition that he considers the object of study interesting enough.
At the end of the sixth month, the baby can usually roll over on his stomach to explore and explore everything that surrounds him. This rollover already begins with the ability to grab an object that has crossed the center of the body, and it means that the child is able to actively balance in an unstable position "lying on his side" . The side on which the child turns over first rests on the lateral surface of the body and the shoulder blade, while continuing to turn - on the shoulder blade, forearm and side of the pelvis, as well as on the hip joint. Purposeful use of the muscles of the body, especially the chains of the oblique rotatory muscles, becomes possible only at this age, i. e. at the sixth month of life. The child first uses the shoulder and hip joints as load-bearing and supporting joints in the "lying on its side" position.
e. at the sixth month of life. The child first uses the shoulder and hip joints as load-bearing and supporting joints in the "lying on its side" position.
Eyes and hand remain focused on the object to be grasped; in this situation, it is especially important to ensure a stable position of the body and spinal column. Such postural support requires an extraordinary expenditure of strength due to the instability of the “lying on one side” position. As a rule, the child does not linger in this position, since from it you can immediately go to the "lying on the stomach" position. The head in the "lying on its side" position is not on the plane of the body support, it is raised and directed towards the toy.
In the described sequence of movements, the transition from the thoracic to the lumbar spine is important, more precisely, from the 12th thoracic vertebra to the 3rd lumbar vertebra. In the first trimester, this area was already used to support the body in the supine position. In the second trimester it became a key turning point. From the involved musculature, it requires precisely coordinated work, since in the dynamics of the turn this place dictates the need for both postural stability and accuracy in the execution of the movement.
In the second trimester it became a key turning point. From the involved musculature, it requires precisely coordinated work, since in the dynamics of the turn this place dictates the need for both postural stability and accuracy in the execution of the movement.
During the rollover, the pelvis is slightly lifted up from the side of the grasping hand, while the other side of the pelvis acts as a support for the body.
In case of successful position adjustment, the body turn to the side is followed by legs half-bent at the hip, knee and ankle joints. In the lateral position until the final transition of the child to the position "lying on the stomach", the child extends the leg lying from below. The leg lying on top is still bent and is involved in the turn. But when the inner side of the knee touches the bed, the upper leg also straightens out. Upon reaching the position on the stomach, as a rule, the legs are half-bent at all joints and both inner sides of the knee are in contact with the bed. The feet at the beginning of the turn are raised at the ankle joints. But as the rotation increases, after passing through the side position, the lower foot turns inward (inversion), the toes flex, and the upper foot remains in its position.
The feet at the beginning of the turn are raised at the ankle joints. But as the rotation increases, after passing through the side position, the lower foot turns inward (inversion), the toes flex, and the upper foot remains in its position.
| At the first attempts to turn, the child, having reached the beginning of the position on the side, returns to the position on the back. But having become acquainted with the course of the movement, he continues to turn to find himself in the "lying on his stomach" position. |
Development from the prone position
In the prone position, the child discovers an abundance of new objects that he certainly wants to possess. In order to possess coveted objects, the child needs to get to them and grab them. The motor algorithm already known to us of the symmetrical elbow support expands into algorithm of the single elbow support . In this case, the weight of the whole body rests on one elbow, on the pelvis and thigh on one side, and also on the knee on the opposite side. The head and arm in this position are held and balanced outside the support surface).
In this case, the weight of the whole body rests on one elbow, on the pelvis and thigh on one side, and also on the knee on the opposite side. The head and arm in this position are held and balanced outside the support surface).
The flow of stimuli from the world surrounding the child has a stimulating effect, and the child uses all his abilities to grasp everything that attracts him. Its motto is "higher, further, stronger". The child then opens up the possibility of leaning on the arms and hips. This algorithm is called hand support . With this support, the child gains height, but he still cannot straighten up further, and therefore “falls” on his stomach again and again, raising his arms and legs up. This algorithm looks like the child is swimming, and is called swimmer algorithm . Approximately to by the end of the sixth month, the hands almost completely master their main functions grasping and support . The motor algorithm of the hands shows the following signs at this age: the hands can be aligned along the longitudinal axis of the forearms, the hands are raised at the wrist joint, the metacarpus is spread, the thumb is protruded This prepares the hands for what will be mastered in the next trimester, that is, by fine motor skills .
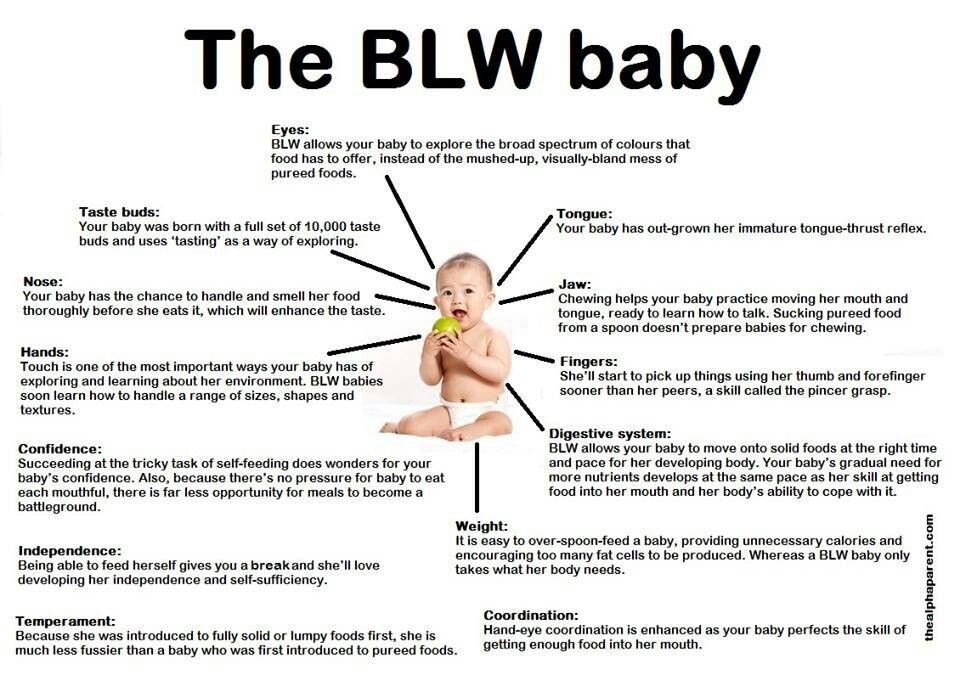
At the end of the sixth month of life, the child develops its grasping functions on its feet. When the feet come into his field of vision, the child grabs them and puts them in his mouth. This global motor algorithm is called hand-foot-mouth coordination . As the name implies, this is a very complex interaction of the most diverse functions of the whole body. Stabilization of the body position allows the child to bend the legs and raise the shins; at the same time, he can see his feet, grab them with his hands and put them in his mouth. Thus, he embraces them, tries to understand them (his feet) with all the senses, and the feet take their rightful place in the child's idea of his own body.
Speech development
On the fourth and before the fifth month of life, the tip of the child's tongue begins to rest against the incisive papilla (Papilla incisiva) of the palate. The chewing movements of the lower jaw become clearer. The teeth begin to cut. The child puts everything in his mouth, at this age the mouth becomes the most important sense organ. The child learns his world with his hands and mouth. The posture, as well as the straightening of the body and the spinal column, create the prerequisites for holding the head, as well as the prerequisites for the free development of fine motor functions of the muscles of the larynx, hyoid bone, and also the tongue itself. At this point, the child is able to purposefully use his speech motor skills. From the fourth to the fifth month of life, he discovers that his lips are able to form sounds. The child actively emits characteristic frictional consonants and vowels, begins to "walk".
The teeth begin to cut. The child puts everything in his mouth, at this age the mouth becomes the most important sense organ. The child learns his world with his hands and mouth. The posture, as well as the straightening of the body and the spinal column, create the prerequisites for holding the head, as well as the prerequisites for the free development of fine motor functions of the muscles of the larynx, hyoid bone, and also the tongue itself. At this point, the child is able to purposefully use his speech motor skills. From the fourth to the fifth month of life, he discovers that his lips are able to form sounds. The child actively emits characteristic frictional consonants and vowels, begins to "walk".
At this age, the child's speech consists of chains of sonorous syllables, modulated throat sounds, individual cries.
| The child in the first half of the second trimester should be offered unequivocally from one side. If you offer a child a midbody grasping toy, it must be done calmly so that the child can decide which hand to choose for grasping. |
Hand-foot-mouth disease - Appotek
Hand-foot-mouth disease or enteroviral vesicular stomatitis with exanthema is a common infection in children that causes sores in or around the mouth and rashes or blisters on the hands, feet, legs or buttocks.
This is a viral disease that is not serious and usually disappears on its own after a week, but is highly contagious. It most commonly occurs in late summer and autumn and predominantly affects children under 5 years of age, although adults can also be infected.

Causes
Viruses that commonly cause hand-foot-mouth disease are coxsackievirus a16 and enterovirus 71. Infection is most common in late summer and autumn. The infection is highly contagious and is spread through close contact, especially on the hands. Anyone can get sick, but children under 5 years of age are more likely to get sick. Those who have had the hand-foot-mouth disease will not get sick again.
Symptoms
Some children can carry the virus without getting any symptoms. But for most, the disease begins with the following symptoms, three to five days after infection:
- poor appetite
- fever
- feeling unwell
- sore throat
Eruptions usually appear on the arms, legs and around the mouth one to two days after these initial symptoms. At first, the rash looks like a red ring, and then develop into vesicular sores with blisters. They itch and hurt, and can also rupture, causing small sores.
The child is most contagious in the first 7 days of illness, even before blisters appear. But the virus can stay in their bodies for days or weeks and be spread through saliva or feces. Therefore, it is important to maintain proper hygiene to reduce the risk of infection.
Prevention and protection
Proper hygiene is the best defense against hand, foot and mouth disease. Washing your hands regularly can greatly reduce your risk of contracting this virus.
Teach your children how to wash their hands using hot water and soap. Hands should always be washed after using the toilet, before eating and after going outside. Children should also be taught not to put their hands or other objects in their mouths.
Treatment
There is no cure or vaccine for diseases of the hand, foot and mouth. Since the virus causes illness, antibiotics will not help. The disease usually goes away on its own in 7-10 days. In the meantime, you can help your child feel better:
- Pain relievers such as ibuprofen or paracetamol or mouth sprays.
 In no case should you move the object quickly from side to side, this puts the grasping process in conditions that do not correspond to the age of the child, confuses the child and makes him nervous. Until the end of the sixth month of life, the child can only grab his own feet, they are not yet sufficiently developed to walk. Therefore, a child at this age should not be planted or put on his feet. Passive sitting or standing can damage a child's spine and hip joints.
In no case should you move the object quickly from side to side, this puts the grasping process in conditions that do not correspond to the age of the child, confuses the child and makes him nervous. Until the end of the sixth month of life, the child can only grab his own feet, they are not yet sufficiently developed to walk. Therefore, a child at this age should not be planted or put on his feet. Passive sitting or standing can damage a child's spine and hip joints.