Pumping to relieve engorgement
Tips from Dr. Harvey Karp – Happiest Baby
By Dr. Harvey Karp, MD, FAAP
How to Relieve Engorged Breasts
Breastfeeding success most often depends on moms having the right information at their fingertips in those first crucial days, in addition to getting support. So, if you’re pregnant, set this article aside now but remind yourself (a calendar alert is a good idea!) to look at it 1-5 days after birth. That’s when engorgement peaks, and you’ll want these tips (and video) handy.
What to Expect as You Start Breastfeeding
From the get-go, your baby will suck colostrum from your breast, sometimes called "liquid gold" because it's rich with immune-boosting antibodies and protein. Then your milk “starts to come in” 3-5 days after birth and your breast will feel full, warm and heavy for 1-2 days (all totally normal). Both blood and milk are rushing to your breasts! Feeding your baby frequently is important during the early days of your child’s life.
What is breast engorgement?
You’ll know you are engorged when your breasts are swollen, very firm, hot and painful. The skin may feel tight or look shiny. Swelling may go all the way to your armpit. Ouch!
How to Relieve Engorged Breasts at Home
Below you’ll find tips for how to treat breast engorgement.
- Feed your little one often. It’s hands-down the best thing to do!
- Sometimes your breast is so hard your baby’s mouth just pops off! You’ll want to hand express some milk and massage toward the armpit before your baby latches. You can also do reverse pressure to soften around the nipple.
- To relieve pressure/pain, hand express for a few minutes until you feel better (but don’t drain the breast).
- Between feedings you can use cold compresses, bags of frozen veggies, ice packs etc. Some women swear by gel “soothies” that are cooled in the fridge.
- Apply moist heat BEFORE you breastfeed (warm shower, warm towel, warm compress).
 This will help your milk let down. A cool trick is to put a few tablespoons of water in a diaper and heat it in the microwave for 10 seconds to make a compress that holds its heat well. Just make sure it’s not so hot to burn or irritate your skin!
This will help your milk let down. A cool trick is to put a few tablespoons of water in a diaper and heat it in the microwave for 10 seconds to make a compress that holds its heat well. Just make sure it’s not so hot to burn or irritate your skin! - Ask your doctor if ibuprofen can be used for breast swelling or pain.
Will Engorged Breasts Go Away?
As you breastfeed and empty your breasts, engorgement should get better in a day or two. However, if you can’t or are unable to breastfeed, breast engorgement may last several days, which if untreated, may lead to plugged ducts or mastitis.
Will Pumping Make Engorgement Worse?
Pumping shouldn’t make engorgement worse—in fact, it might help alleviate engorgement. If your breast is engorged, it might become too firm for your baby to latch. Pumping a little bit before breastfeeding may help soften the areola and lengthen the nipple to make it easier for your infant to connect with your breast.
Watch & Learn the Techniques
When to Get More Breastfeeding Help
- Call your doctor right away if your breast is red and painful, you have flu-like symptoms or you have a temp of +101 degrees.
- Seek advice from a lactation consultant if your engorgement and related pain don't improve within 2 days.
Breast Engorgement: Final Thoughts
Engorgement is one of the reasons women abandon breastfeeding. Share this advice with a pregnant friend (or mom who just gave birth...but act fast!) and you'll have done a very good deed!
Advice is adapted from materials by Breastfeeding Medicine of Northeast Ohio.
About Dr. Harvey Karp
Dr. Harvey Karp, one of America’s most trusted pediatricians, is the founder of Happiest Baby and the inventor of the groundbreaking SNOO Smart Sleeper. After years of treating patients in Los Angeles, Dr. Karp vaulted to global prominence with the release of the bestselling Happiest Baby on the Block and Happiest Toddler on the Block. His celebrated books and videos have since become standard pediatric practice, translated into more than 20 languages and have helped millions of parents. Dr. Karp’s landmark methods, including the 5 S’s for soothing babies, guide parents to understand and nurture their children and relieve stressful issues, like new-parent exhaustion, infant crying, and toddler tantrums.
His celebrated books and videos have since become standard pediatric practice, translated into more than 20 languages and have helped millions of parents. Dr. Karp’s landmark methods, including the 5 S’s for soothing babies, guide parents to understand and nurture their children and relieve stressful issues, like new-parent exhaustion, infant crying, and toddler tantrums.
View more posts tagged, moms & dads
Have questions about a Happiest Baby product? Our consultants would be happy to help! Connect with us at [email protected].
Disclaimer: The information on our site is NOT medical advice for any specific person or condition. It is only meant as general information. If you have any medical questions and concerns about your child or yourself, please contact your health provider.
Engorged Breasts - avoiding and treating
You are here: Home / Breastfeeding information / Engorged Breasts – avoiding and treating
Engorged breasts are painful. They feel heavy, hard, warm and sensitive —as if they are ready to burst! As well as being painful, engorgement can lead to other breastfeeding problems if not treated. Being able to recognise engorgement will help you to treat it promptly, avoiding complications.
They feel heavy, hard, warm and sensitive —as if they are ready to burst! As well as being painful, engorgement can lead to other breastfeeding problems if not treated. Being able to recognise engorgement will help you to treat it promptly, avoiding complications.
Most mothers experience some engorgement in the first weeks after birth. With changing hormone levels, your breasts swell and enlarge as milk production increases. It may seem as though they are filling up with milk, but engorgement is more than milk storage. Your body directs extra blood and fluids to your breasts to boost milk production. This causes congestion and swelling which will decrease as your body adjusts.
Minimizing early engorgement
Treat engorgement to…
When to treat engorgement
After the first few weeks
Causes of engorgement
Treating engorgment
Be sure your baby is sucking effectively
Reverse pressure softening
Keep comfortable
Watch out for signs of mastitis
Minimizing early engorgement
New mothers vary in how engorged their breasts become in the weeks after birth; some experience little engorgement, others describe their breasts as feeling like watermelons!
Try these suggestions
- Breastfeed your baby frequently from birth: at least 8–12 times in 24 hours.
 Keeping your baby close makes it easier to nurse every hour or two.
Keeping your baby close makes it easier to nurse every hour or two. - If your baby is sleepy, perhaps from a medicated birth, you may need to wake him and encourage him to nurse.
- Aim to be comfortable while breastfeeding, and learn how to get your baby latched on well.
- If your newborn is unable to breastfeed, hand express frequently until your milk ‘comes in’, then combine with using a hospital-grade electric breastpump to help establish your milk production and relieve engorgement. Your milk can be given to your baby until he is able to nurse.
Treat engorgement to…
Make breastfeeding easier
Even if you feel as though you have lots of milk, engorgement can make it harder for your baby to latch on to your breast and feed well. A poor latch-on can give you sore nipples. Your baby may also have trouble coping with the flow of milk from engorged breasts.
Protect milk production
When milk isn’t removed from your breasts, you will produce less milk. Treating engorgement gives your baby more milk now and helps protect milk production for when your baby is older.
Treating engorgement gives your baby more milk now and helps protect milk production for when your baby is older.
Avoid blocked ducts or mastitis
Engorgement can result in blocked ducts leading to mastitis.
When to treat
Take action to relieve engorgement if your breasts feel firm, hard, shiny or lumpy. When milk is removed, blood circulation improves and swelling reduces. Use the suggestions below to reduce swelling and keep your milk flowing. Many mothers have a slight temperature when their breasts are engorged. Temperatures under 38.4ºC are not usually associated with infection. Keep your baby close and continue breastfeeding.
Engorgement after the first weeks
Treat as outlined below while working out the cause so you can prevent it happening again.
Common causes of engorgement are:
- A missed feed or expressing session.
This can easily happen during holidays and festivities or when visitors arrive. Encourage your baby to feed more often, or express more frequently if you’re apart from your baby.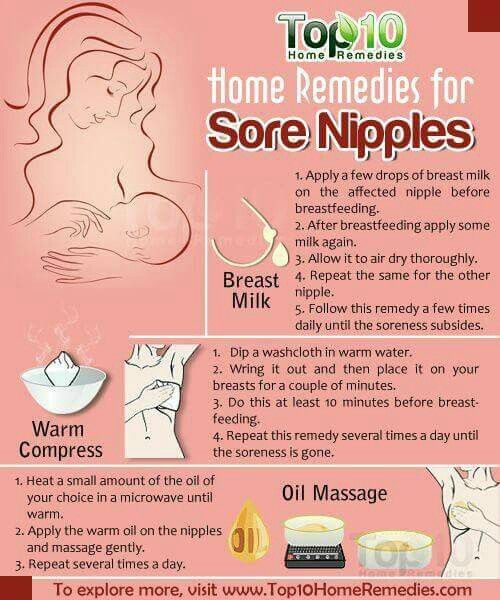
- Feeding a baby on a schedule
Recent research has revealed that mothers vary in how much milk their breasts can store without becoming uncomfortable. Mothers following routines often suffer from engorgement, mastitis and low milk production because their breasts are not drained often enough. - Expressing milk.
Some books advise expressing to keep milk production one step ahead of a baby’s needs. However, making more milk than your baby needs can increase your risk of engorgement and mastitis, especially if you go for several hours without feeding or expressing. - A baby who is unable or unwilling to nurse well for any reason
Expressing milk frequently until your baby can nurse well will help you maintain milk production and avoid blocked ducts or mastitis. - Weaning from the breast too quickly
If you experience engorgement during weaning, you may need to slow down the process. This will give your breasts time to adjust to the reduced demand for milk. If breastfeeding more often is not an option, try expressing just enough milk to relieve the fullness by hand or pump.
If breastfeeding more often is not an option, try expressing just enough milk to relieve the fullness by hand or pump.
Treating engorgement
Reduce swelling and keep milk flowing:
- Aim to breastfeed every 1½ to 2 hours during the day, and at night every 2–3 hours from the start of one feed to the start of the next. Let your baby finish on the first breast before switching to the second
- Avoid using bottles or dummies. If a supplement is needed try using a spoon, flexible feeding cup or syringe.
- Between feeds, apply ice for 15–20 minutes at a time between feeds to reduce swelling. Use an ice pack, crushed ice in plastic bags or bags of frozen vegetables (that can be refrozen several times before being thrown away). Wrap them in a lightweight towel to protect your skin.
- Just before feeding, apply moist warmth to your breasts for up to two minutes to help milk flow. Try a warm wet towel, warm shower or immersing breasts in a bowl of warm water.
 Then, express to comfort if your baby isn’t ready to feed.
Then, express to comfort if your baby isn’t ready to feed. - Use gentle massage from the chest wall toward thenipple area in a circular motion.
Be sure your baby is sucking effectively:
Position your baby with his chest and tummy in full contact with your body. With his cheek in close contact with your breast, your baby can easily tip back his head to latch on. This way he’ll take a large mouthful of breast. Listen for swallowing as he feeds.
If your baby is finding it hard to latch on – when your baby bobs his head and licks the nipple, he naturally makes it easier to latch on.
For more information on getting your baby positioned and attached comfortably see here.
Reverse pressure softening
works by moving fluid away from the nipple area.
- Press all five fingertips of one hand around the base of the nipple. Apply gentle steady pressure for about a minute to leave a ring of small dimples on the areola.
- You can also press with the sides of fingers.
 Place your thumb on one side of the nipple and two fingers on the other side where your baby’s lips will be.
Place your thumb on one side of the nipple and two fingers on the other side where your baby’s lips will be. - If this isn’t enough, gently hand express a little milk before feeding to soften the areola. If you choose to use a breastpump, set it to minimum suction.
Keep comfortable:
- Ask your midwife or GP to recommend an over-the-counter, anti-inflammatory medication suitable for breastfeeding mothers to relieve pain and swelling.
- A well-fitting, supportive bra may help. Avoid bras (and underwires) that are tight or put pressure on specific areas of the breast.
- Cold, raw cabbage leaves worn inside a bra can be soothing. Change when they become wilted or after about 2 hours. Use only until swelling goes down as long-term use may reduce milk supply. Stop use if a skin rash or other signs of allergy appear.
Watch out for symptoms of mastitis:
- Inflamed, hot, red or darkened localised areas of your breast, depending on your skin tone.
 Changes in breast appearance may be harder to spot in darker skin. You may still have engorged breasts without a noticeable red or darkened area.
Changes in breast appearance may be harder to spot in darker skin. You may still have engorged breasts without a noticeable red or darkened area. - Temperature over 38.4ºC or flu-like symptoms.
- Weaning can make a breast infection worse so continue to breastfeed frequently especially on the affected side and treat as for engorgement. Rest and drink fluids. If fever persists, continue breastfeeding and check with your GP as you may need antibiotics. More information on mastitis.
Engorgement should improve within a day or two. If not, contact an LLL Leader for further suggestions. You may need to improve your baby’s breastfeeding technique or find ways to reduce your milk supply. These are not difficult problems to solve, especially if treated promptly.
Written by Karen Butler, Sue Upstone & mothers of La Leche League Great Britain
Further Reading
The Womanly Art of Breastfeeding. LLLI. London: Pinter & Martin, 2010.
Beginning Breastfeeding
Comfortable Breastfeeding
Dummies and Breastfeeding
Hand Expression of Breastmilk
Mastitis
My Baby Won’t Breastfeed
Nipple Pain – why and what to do
Positioning and Attachment
Sleepy Baby – why and what to do
This information is available to buy in printed format from our shop
Copyright LLLGB 2016
Filed Under: Breastfeeding information, Common Concerns Tagged With: blocked ducts, engorgement, express, expressing, lumps, mastitis, milk, newborn / beginning breastfeeding, red, reverse pressure softening, swollen
Article "Pumping - when and how?"
There are times in the life of mother and baby when breastfeeding is either impossible or difficult for some reason. For example, a child has to be left without a mother for several hours - which means that a supply of milk is needed for him. Or in the case when the baby sucks badly at the breast, but eats well from the bottle, and pumping is the only way to feed him.
For example, a child has to be left without a mother for several hours - which means that a supply of milk is needed for him. Or in the case when the baby sucks badly at the breast, but eats well from the bottle, and pumping is the only way to feed him.
This can happen if the baby is born prematurely, and the very process of sucking the mother's breast turns out to be hard physical work for him - such an infant can also be offered expressed milk.
The same applies to the situation when the baby is ill and feeling unwell prevents him from fully sucking, as he is too weak to make the efforts necessary to "extract" breast milk. In this case, it should be expressed for 2 reasons: firstly, to provide the child with complete and optimal nutrition for him, and secondly, to maintain lactation.
Situations are different, so it is important to understand why pumping is necessary, how to do it correctly and what are the conditions for storing breast milk.
When and why to express?
Pumping is the process by which a nursing mother manually or with the help of a breast pump extracts milk from her breast.
This is not a mandatory procedure for everyone, and it does not need to be carried out after each feeding, since the milk in the female breast is formed exactly as much as is needed to saturate the baby at a certain age. Those. how much milk the baby ate in one feeding - so much will appear in the breast by the next.
But if, after applying, you also express the rest of the milk, then by the upcoming feeding it will be produced more than the child can eat - and this often leads to stagnation of milk (lactostasis).
Milk should be expressed when:
-
Having to bottle feed or supplement a baby for one reason or another. If at the same time the pediatrician did not forbid the baby to eat breast milk, then the mother needs to feed the baby expressed.
-
The baby is left without a mother for a long time. There are times when a woman needs to go away, and she cannot take the child with her. In this case, you can leave a supply of milk for several hours, after decanting it.

-
Mom is sick. It happens that during lactation a woman becomes seriously ill and is forced to take medications that penetrate into breast milk, which is strictly forbidden to give to a child. Medicines contained in milk, once in the child's body, can have an adverse effect on it. To prevent this from happening, the pediatrician will help you choose the milk formula that you need to feed the baby during the mother’s illness. Pumping in such a situation will help a woman maintain lactation until recovery.
-
Mom goes to work. A mother's return to work before the end of lactation can put her before a choice: transfer the baby to formula milk or feed it with expressed milk. Recently, more and more parents are choosing the latter option, since breast milk is much healthier than artificial nutrition.
-
Injured nipples. With improper care and attachment of the child to the breast, cracks may appear on the nipples. Feeding in this condition of the nipples becomes very painful for the mother, and then the baby should be briefly transferred to expressed milk from a bottle.
 This is useful because the nipples are less likely to get irritated when they are expressed than when they are sucked by an infant. In a few days, the nipples will heal, and it will be possible to resume feeding the crumbs directly from the breast.
This is useful because the nipples are less likely to get irritated when they are expressed than when they are sucked by an infant. In a few days, the nipples will heal, and it will be possible to resume feeding the crumbs directly from the breast. -
There is a risk of lactostasis. A child, especially in the first days after birth, is not always able to suck out all the milk. To avoid lactostasis, mom needs to express excess milk. If this is not done in a timely manner, stagnation of milk can lead to inflammation of the mammary gland - mastitis. However, you must follow all the rules of pumping and do not resort to it after each feeding: this will only increase the flow of milk.
-
Not enough milk is produced. Pumping will help normalize lactation, as it leads to an increase in the production of milk in the breast, which can be useful during a lactation crisis.
5 pumping inhibitions
In order not to harm herself and not leave the baby without breast milk, the mother must know and be sure to follow the basic rules of pumping:
-
Do not express more than 3 times a day if pumping is combined with breastfeeding because this will lead to excess milk production.
 If the mother is sick and the baby is not applied to the breast, it is necessary to express with a frequency approximately equal to the number of feedings (on average, once every 3 hours - 8 times a day).
If the mother is sick and the baby is not applied to the breast, it is necessary to express with a frequency approximately equal to the number of feedings (on average, once every 3 hours - 8 times a day). -
Do not express immediately after feeding, as this may lead to hyperlactation, ie. increased milk production.
-
Do not express "to the last drop". The main indicator by the end of pumping should be a feeling of relief in the chest. The female body regards the emptying of the breast without a trace as an increased need for milk by the child - and begins to produce more milk, which the baby cannot eat, therefore, there will be a threat of milk stagnation.
-
Do not express during the night, as this may also lead to the formation of excess milk. The main hormone responsible for milk production - prolactin - has a daily rhythm of formation, most of all it is produced at night, in response to the baby sucking or pumping.
-
Do not express on the first day after the arrival of milk.
 Usually, when lactation begins, more milk is produced than the newborn needs, and it is necessary to get rid of its excess. Therefore, just at the time of the arrival of milk, you can not express everything without a trace. If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
Usually, when lactation begins, more milk is produced than the newborn needs, and it is necessary to get rid of its excess. Therefore, just at the time of the arrival of milk, you can not express everything without a trace. If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
Substances that signal that milk is being produced in excess appear in the filled breast after about 1 day. If you express all the milk accumulated in the chest earlier than in a day, then it will be produced in the same amount.
Hand Expression Technique
There are two ways to express - manually and with a breast pump. Usually, each mother chooses the most convenient option for her. It is better to do it manually at home, when a woman has enough time, since the whole process will take some time. Breast pumps will help a working mother, which greatly facilitate the pumping process.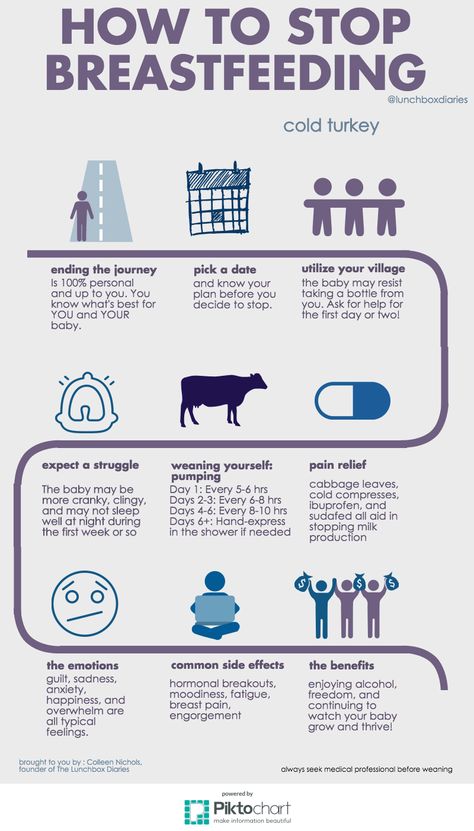
Rules for hand pumping
It is best to express milk 10-15 minutes after the end of feeding the baby. Wash your hands thoroughly beforehand. If you use any breast cream, wipe the skin and nipples with a cotton swab or pad soaked in breast milk. Prepare a wide-mouth milk container by first washing it under running water and then sterilizing it (by boiling, in a steam sterilizer or in a dishwasher).
Sit comfortably, keeping your back straight, because pumping can take some time, and an uncomfortable position can cause back pain.
Gently grasp the chest: the little finger is under the chest at the ribs, the remaining fingers are positioned so as to support the chest from below. The thumb lies on top, about 3-4 cm from the nipple. In this case, the thumb and forefinger are located opposite each other, forming the letter "C".
Use your thumb and forefinger to gently press down on your chest and hold this position for a few seconds. In no case do not bring your fingers together, they should remain in the same position, the letter "C".
In no case do not bring your fingers together, they should remain in the same position, the letter "C".
Repeat pressing, moving the palm in a circle - this way you will use all the ducts of the mammary gland.
Be patient, milk may not come out immediately, but only after a while. If you are pumping for the first time, check with your doctor or lactation consultant beforehand to show you how to proceed.
Manual pumping errors
Do not squeeze the nipple: this way you will only hurt yourself and injure the breast, and you will not express milk fully.
Do not press the palm too tightly against the skin, moving the hand across the chest so that there is no irritation and microtrauma.
Do not give up at the first unsuccessful attempts, be patient.
Breast pumps
Breast pumps make pumping much easier, as they are designed to fit all the anatomical features of the female breast.
Which one to choose? Breast pumps are divided into mechanical and electrical.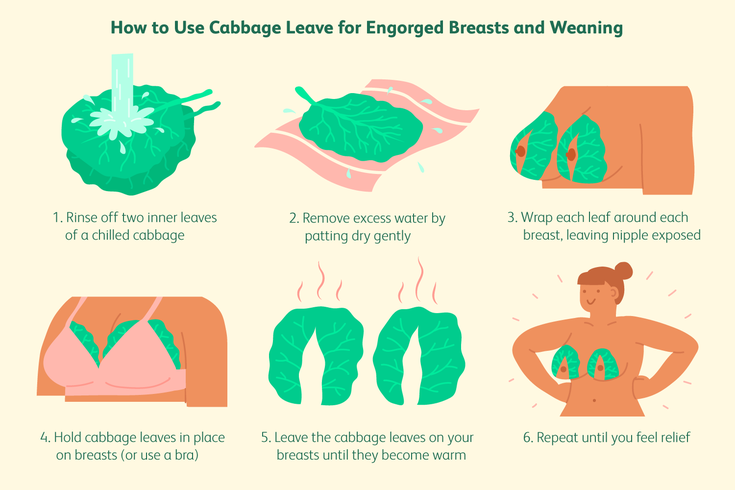 In the first case, the pumping process is carried out manually: by squeezing the “pear”, the woman starts the suction mechanism. Electric models are good because they work independently: from the mains or from batteries (batteries, accumulators) and do not require additional effort on the part of the woman.
In the first case, the pumping process is carried out manually: by squeezing the “pear”, the woman starts the suction mechanism. Electric models are good because they work independently: from the mains or from batteries (batteries, accumulators) and do not require additional effort on the part of the woman.
Mom usually chooses a breast pump model according to her taste and financial capabilities. It should be borne in mind that devices powered by batteries lose power faster than devices powered by the mains.
Many women are confused by the fact that electric breast pumps are loud enough. To date, there are a large number of silent devices, which is recommended to pay attention to when buying. The most effective are electric breast pumps that express both breasts at the same time and have the option of adjusting the thrust force and suction speed.
When choosing a breast pump, pay attention to the presence of the “boil and sterilize” marking. There must be the possibility of such heat treatment of parts of the apparatus. If the model cannot be boiled and sterilized, it is better to refuse to purchase it and look for another one.
If the model cannot be boiled and sterilized, it is better to refuse to purchase it and look for another one.
Rules for expressing with a breast pump
Before pumping for the first time, carefully read the instructions for the device. Check that it is properly assembled.
Sterilize the funnel and sump (boil or use a sterilizer).
Position the funnel so that the nipple is in the center of the funnel.
The draw should be the lowest, especially at first, until the breast is accustomed to expressing with a breast pump. Each breast must be pumped until a feeling of relief, add 2 minutes to this time. On average, the process will take about 15 minutes.
Pumping, like manual pumping, should be carried out some time after feeding.
Basic mistakes when expressing with a breast pump
Incorrect position of the funnel of the breast pump can cause pain to the woman. Remember: the nipple should be located strictly in the center of the funnel of the device.
Very long pumping. Do not exceed the time required to collect milk, this can lead to hyperlactation (production of excess milk).
Very strong traction. If your breast pump has a selectable thrust function, you should use the smallest one so as not to hurt your breasts.
Care of the breast pump. A breast pump, like any machine, needs proper care. It must not be clogged so as not to contaminate the milk.
Each model has a care instruction, which you should definitely read before using the device.
When washing, always disassemble the pump completely, removing even the smallest parts. This will prevent stagnation of milk residues in them.
Before each use, sterilize all parts of the machine that come into contact with milk. This can be done with a sterilizer.
Milk defrosting
Never thaw or heat breast milk in a microwave oven. When heated in the microwave, the milk warms up unevenly, while feeding the baby can burn. Also, due to the rapid heating of frozen milk when using a microwave, most of the useful properties of this invaluable product are lost.
Also, due to the rapid heating of frozen milk when using a microwave, most of the useful properties of this invaluable product are lost.
To defrost breast milk, place it on the refrigerator shelf, and when it becomes liquid, heat it up. To do this, lower the milk bottle into hot water or put it under hot water. Also, special heaters can be used to warm milk.
If you have questions or don't know how to express, it's worth talking to a specialist. The doctor will not only tell, but also show how to do it correctly, give recommendations on the pumping schedule and advise which method is better to choose.
Remember that milk is undoubtedly a valuable food for the baby, but feeding with expressed milk should be used in exceptional cases.
At the School of Moms, our doctors talk in detail not only about how and when to express milk correctly, but also about how to properly attach a baby to the breast, how to avoid common problems with breastfeeding, such as lactostasis, as well as the rules for self-examination mammary glands.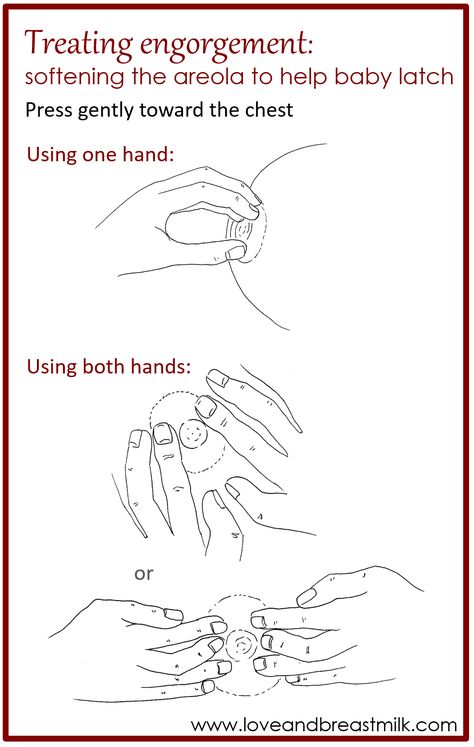
Breast engorgement symptoms and first aid
search support iconSearch keywords
One of the most common breastfeeding problems faced by mothers is breast engorgement. While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it.
Let's look at all the important issues, including prevention, symptoms, and help with engorgement.
What is breast engorgement?
Engorgement is an increase in the size of the mammary glands, in which the breast becomes painful and sensitive. This condition is associated with increased blood flow and increased milk production, so it very often occurs during the first few days after childbirth. In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs.
Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs.
How long does engorgement last?
All women are different, and, accordingly, the duration of this condition may vary. Some experience mild symptoms for only one day, while others may experience this condition for up to two weeks.
Breast engorgement occurs for various reasons. The most common:
- Missing a feeding or pumping session.
- Making more milk than the baby eats.
- Insufficient outflow of milk (improper latching on to the breast by the baby).
- Inflammation.
Breast engorgement symptoms
Breast engorgement symptoms vary, but the most common are:
- Breasts become hard or firm.
- Breasts become sore or warm to the touch.

- Breasts become heavy and swollen.
- Breasts become lumpy and swollen.
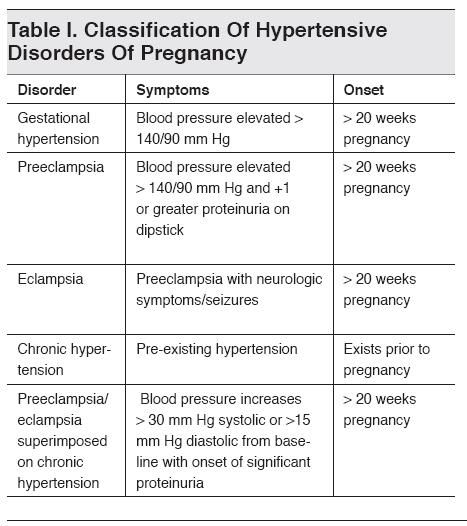
Although engorgement and mastitis may appear similar, they are actually completely different conditions. How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement.
Prevention of engorgement
There are several ways to prevent this condition. Prevention of breast engorgement in the first days after childbirth can be difficult as the mother's body adapts to the changes. But you can try to avoid it as follows:
- Check the mammary glands.
 Moms should schedule breast checks before the baby is born. The doctor will be able to recommend corrective measures, if needed, to make breastfeeding more comfortable, as well as explain how to distinguish engorgement from mastitis and how to relieve breast engorgement.
Moms should schedule breast checks before the baby is born. The doctor will be able to recommend corrective measures, if needed, to make breastfeeding more comfortable, as well as explain how to distinguish engorgement from mastitis and how to relieve breast engorgement. - After your baby is born, feed on demand or express milk regularly if you are separated from your baby. Breastfeeding mothers produce milk regularly, so it is important to breastfeed or express milk frequently. Moms should try to feed their baby at least eight times a day and make sure that their breasts are completely empty each time. If a mother is unable to breastfeed her baby, she should express milk with a breast pump.
The electronic breast pump will help you comfortably and efficiently express the right amount of milk between feedings, if necessary, or instead of feeding when the mother is away from the baby.
3. Make sure that the baby latch on correctly. To learn how to properly breastfeed a baby, a mother can seek advice from a breastfeeding specialist. Proper gripping of the breast during feeding is important for complete emptying of the breast. It also helps prevent other problems such as sore, irritated or cracked nipples.
Proper gripping of the breast during feeding is important for complete emptying of the breast. It also helps prevent other problems such as sore, irritated or cracked nipples.
4. Wean the baby gradually. When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement.
Treating breast engorgement
Breastfeeding during engorgement is not only safe, but essential to prevent worsening of symptoms and provide relief. While the body is learning how to produce the right amount of milk, moms can use the Philips Avent bra pads to absorb excess milk and prevent stains on clothes all day long.
Philips Avent
Philips Avent 2 in 1 thermal pads can both warm and cool your breasts to both stimulate and soothe your breasts after feeding. Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
Philips Avent
Multifunction thermal pads
SCF258/02Overall rating / 5
- review review reviews Reviews
-
-{discount-value}
- Pictures It is important to achieve optimal outflow of milk during feedings. To stimulate the outflow of milk, during feeding, you can gently massage the breast.
- Express milk. There are situations when a nursing mother cannot be with the baby during feeding. It is important to empty your breasts by expressing milk to prevent engorgement and other problems.
- When feeding, change positions and rotate the mammary glands. Changing your position while breastfeeding can be beneficial, as it improves the outflow of milk from different parts of the mammary glands. In addition, mothers can change their breasts during one feeding so that the baby can empty both of them.
Remember that minor pain and discomfort is completely natural during breastfeeding, but if these symptoms persist or worsen, the mother should consult a doctor.
Philips Avent Articles & Tips
Baby+ App
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ App
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website.