Pumping colostrum before birth
Pumping Colostrum Before Birth – Spectra Baby Australia
If you're an expecting mother, you might have noticed your breasts leaking. This is completely normal - your body has started producing colostrum, which means you're getting ready to feed your baby. Colostrum is what you're newborn baby will eat for the first few days of life while your breastmilk is coming in. You can express colostrum before birth and save it for baby. This can get you used to pumping or hand expressing before baby gets here, and give you a stash of colostrum just in case. Here's everything you need to know about pumping colostrum before birth.
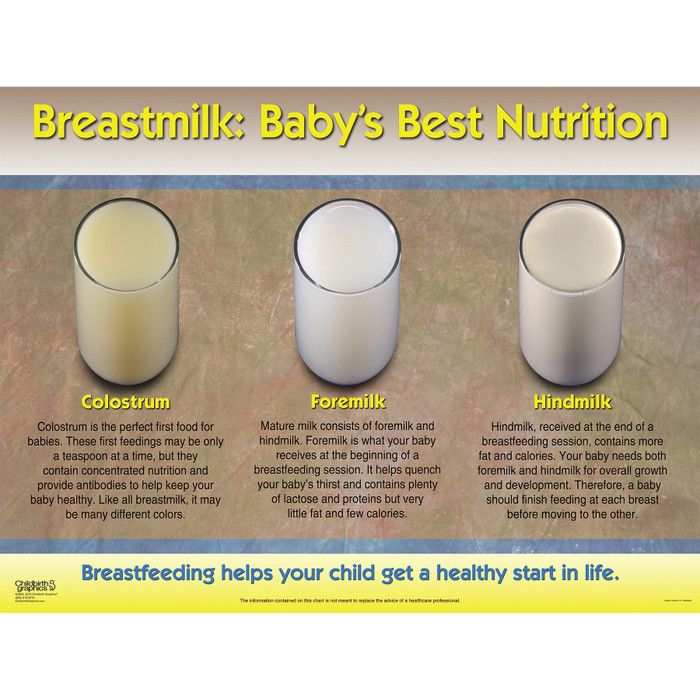
What is colostrum?
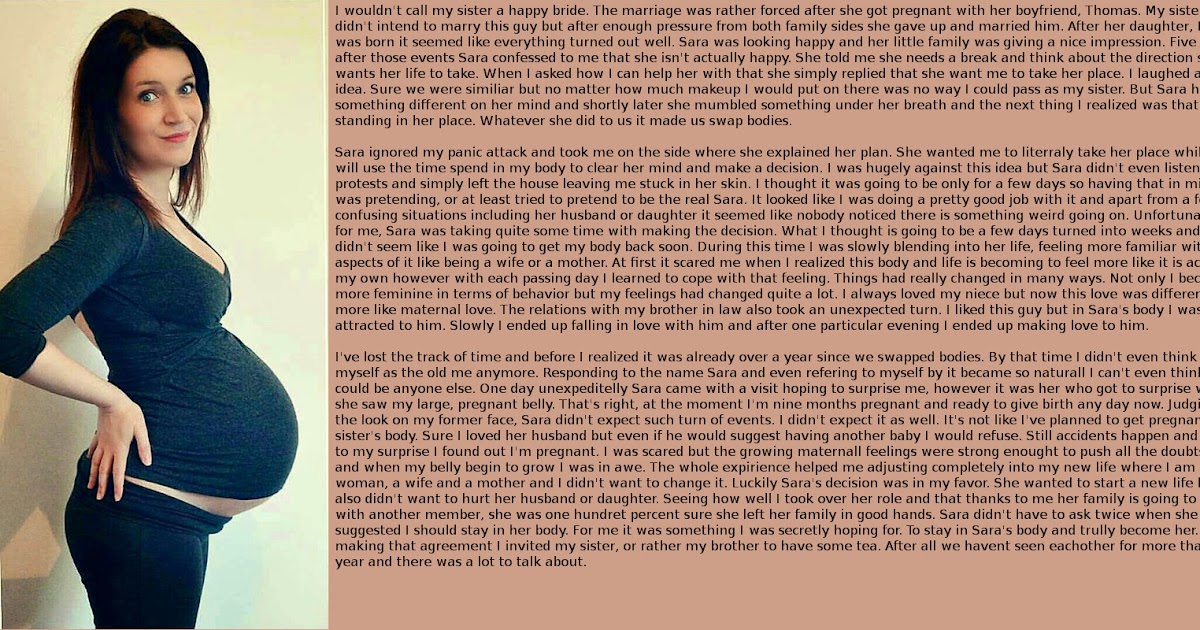
Colostrum is the first food your baby will eat. It's a clear to yellow colour fluid that your breasts produce before your breastmilk comes in. Colostrum is low in fat, but is high in protein, carbohydrates and antibodies. Colostrum is very important for your baby's digestive track. During the first week or so postpartum, your milk will gradually transition from colostrum to breastmilk.
Photo courtesy of Mama Natural
When does colostrum come in?
Your body will start producing colostrum during the second trimester of pregnancy, between 16 and 22 weeks. Many women don't notice colostrum right away because they aren't leaking. It's normal to start leaking colostrum during the third trimester, however, some women never leak.
Does colostrum mean labour is coming soon?
It's normal to start leaking colostrum a few weeks before labour. However, this doesn't necessarily mean that labour is imminent. Some women start producing colostrum as early as 16 weeks pregnant and their breasts may leak throughout pregnancy, while others may never leak. Although leaking colostrum is a good indication that your body is getting ready to give birth, there are some much better signs that labour is fast approaching, such as your baby dropping low into your pelvice.
Is pumping colostrum before birth safe?
Under normal circumstances pumping colostrum before birth is safe. There are no studies that show pumping or breastfeeding while pregnant is unsafe. Many women worry about pumping while pregnant because it causes mild contractions. These contractions, which may feel like menstrual cramps, are harmless to your unborn baby. They're caused by the hormone oxytocin that your body releases while breastfeeding, and the amount of oxytocin is so little there shouldn't be any concern about preterm labor. It's normal for women to continue breastfeeding through pregnancy and go on to tandem feeding, so there shouldn't be any concern about pumping colostrum before birth. In fact, your body will release more oxytocin during sex - which is considered safe during pregnancy - than from breastfeeding or pumping.
That said, there are some circumstances under which pumping during pregnancy may be risky. If you have one of the following conditions, you should talk to your care provider before pumping colostrum:
- You have a high-risk pregnancy, or are at risk for preterm labour (e.
 g. you have a thin cervix).
g. you have a thin cervix). - You are carrying multiples.
- If you have been advised not to have sex during pregnancy.
- You are experiencing bleeding or uterine pain.
Benefits of pumping colostrum before birth
Pumping colostrum before birth is not a requirement for a healthy baby. There are definitely some potential benefits should you choose to pump colostrum before birth - and, especially if you're leaking, it doesn't hurt to save it! Here's how pumping colostrum before birth can be advantageous:
- You'll learn how to use your breast pump or hand express ahead of time.
- If your baby is unable to latch due to a medical condition (e.g. cleft lip or tongue tie).
- You'll have colostrum available just in case while you're learning to breastfeed.
- If your baby is born prematurely and uses a feeding tube.
- You'll have colostrum that you can donate to infants in need - talk to your birthing centre for recommendations, or find local donor groups on Facebook.

How to pump colostrum before birth
Get started pumping colostrum by making sure you've cleaned and sterilised your milk collection kits and any storage containers you plan on using. Start by single pumping on one breast. When you begin pumping, you should start at a low vacuum setting and gradually increase to your comfort level. Massage your breast while you're pumping to encourage the colostrum out. If you need help getting started, Spectra has lot of resources on our website, so we encourage you to have a look. You can join the Spectra Mums Facebook group to talk to other mums about pumping, and our customer support team made up of expert pumping mamas is here to help too. When you pump colostrum, don't expect to get much. You may get a few drops, and you may not even see any land in the milk collection bottle! That's completely normal and fine. Your newborn baby will have a teeny tiny stomach, so just a few mililitres of colostrum will be enough at each feeding.
When you're done pumping, check in and around the breastshield for droplets of colostrum, and look in the valves, as these are places colostrum likes to get stuck. You can use a feeding syringe to suck the droplets up, and store the expressed colostrum.
Storing expressed colostrum
You should follow the same guidelines as you would for storing breastmilk. You can refrigerate expressed colostrum for up to 8 days, and you can store it in the freezer for several months.
Tip: You can use a finger to assist in inserting the syringe into baby's mouth, as shown here.
Also, since your newborn baby will eat just a very small amount of colostrum, you might consider storing it in a food syringe. One syringe can be more than enough for one meal for baby's tiny tummy. You can put several food syringes in a regular freezer safe snaplock bag, or into a milk storage bag. Remember to bring these (and your breast pump) with you when you go into labour, and let the staff know that you'll need a refrigerator for safe storage.
More From Spectra Blog
Should You Pump Colostrum During Pregnancy?
I am often asked if there are things people can do during pregnancy to boost their milk supply before the baby arrives.
My answer is annoying: maybe.
Listen, I get it. Pregnant people that are planning to breastfeed, chestfeed or pump are usually pretty hopeful that it will go smoothly. After all, we hear so many stories about how challenging it can be, especially when it comes to our milk supply. So it makes sense that we want to do everything we can to prepare. The bad news is that often, feeding challenges are out of our control—societal issues like the lack of support for new parents can make it difficult to meet our feeding goals. Plus, physical issues like latch problems, breast structural concerns and more can come into play, as well.
Plus, physical issues like latch problems, breast structural concerns and more can come into play, as well.
The good news is that there are things you can try to help boost your milk supply while you are still pregnant—and I’ll share them in a bit. But first, we need to delve into an idea that is resurfacing around the internet: pumping or expressing colostrum during pregnancy. There’s a lot to unpack here, and it’s actually a pretty important topic, with some misinformation circulating.
First, what is colostrum?
Colostrum is the first milk that babies receive after being born. It is nicknamed “liquid gold” because it is gold in color, and because it is amazingly nutritious and awesome for babies. It is calorie-dense, filling, full of antibodies and it helps babies poop; liquid gold, indeed.
When the baby is born (whether via vaginal birth or Cesarean birth) your body will start to express colostrum. But some people start to leak colostrum during their pregnancy.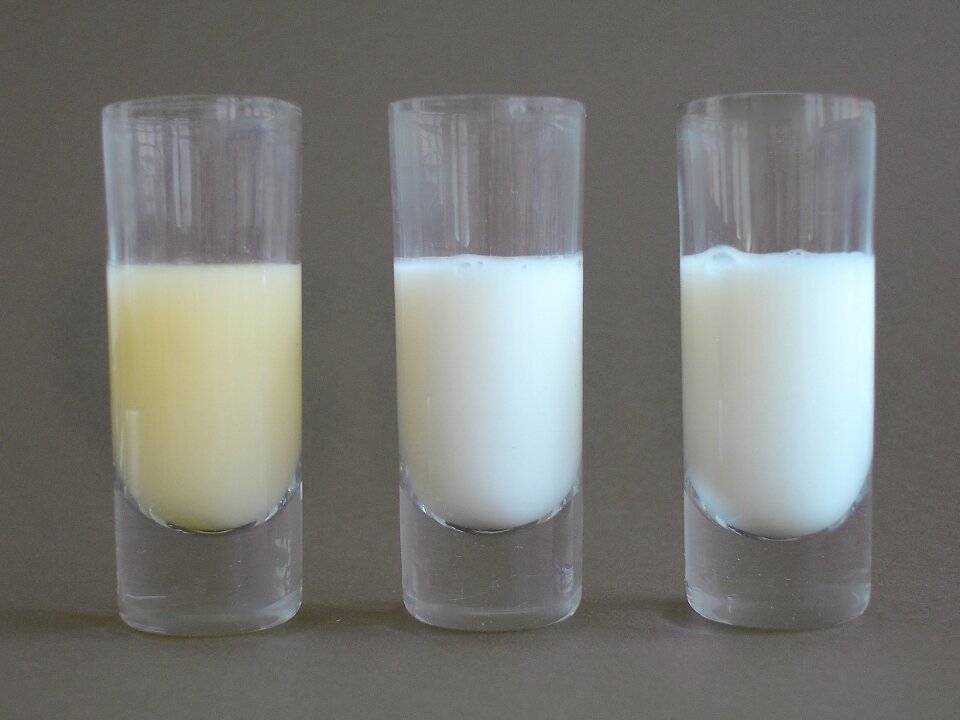
I am pregnant and not leaking colostrum—is that bad?
Nope! Whether or not you leak colostrum during pregnancy has no bearing on your future milk supply after the baby arrives.
How is a milk supply established?
(This seems off-topic, but it’s super related, promise.) In short, milk is made by a supply and demand system. The more your little boss (aka your baby) demands the more your body will supply. Every time your baby latches or you pump, hormones are released and your body gets the message that it needs to keep making milk.
Generally speaking, the more your breast/chest feed or pump, the more milk you will make.
This is why we often encourage new parents to breastfeed or chestfeed on demand—every time their baby is hungry. It is exhausting to be sure, but it helps your body to understand how much milk it needs to make to feed the baby.
Should I express colostrum during pregnancy?
Okay, so… There are a few reasons that people may want to pump colostrum during pregnancy.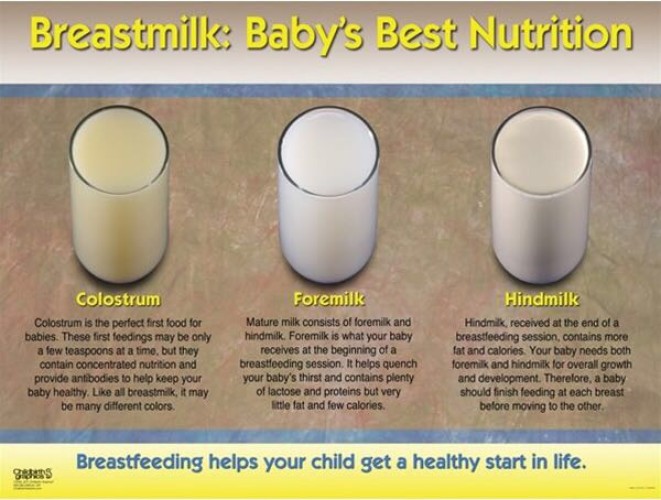 Some are doing so in hopes that it will boost their milk supply after the baby is born—they hope that if they start sending that message to the body early, their body might start to make more milk.
Some are doing so in hopes that it will boost their milk supply after the baby is born—they hope that if they start sending that message to the body early, their body might start to make more milk.
Other express colostrum during pregnancy to start building up a reserve. It is, after all, liquid gold so why not get as much of it as you can?
So in theory, expressing colostrum during pregnancy sounds like it could be a good idea. But is it? Probably not. Here’s why:
Expressing colostrum during pregnancy can be dangerous
When breasts are stimulated, they release oxytocin—this is wonderful once the baby is here since oxytocin in the “oh my gosh I love you so much” hormone.
But oxytocin is also the hormone that causes uterine contractions. The serious concern here is that if you pump or express colostrum during pregnancy, your uterus could start to contract, and you could start labor too soon—and we want to avoid this for sure.
In fact, people who are past their due date (or experiencing a slow labor) are often advised to perform nipple stimulation to get labor going (talk to your provider before attempting).
As a general rule, I do not recommend pumping or expressing colostrum during pregnancy, especially if you are experiencing a high-risk pregnancy, are at risk for pre-term labor, or are not yet full-term.
Are there situations when expressing colostrum during pregnancy is helpful?
Perhaps! This is absolutely a question you can ask your provider since they can guide you based on your situation.
For example, people with gestational diabetes may want to have some colostrum saved up to help stabilize their babies’ blood sugar right after birth. A study published in 2017 found that advising people with gestational diabetes (with otherwise low-risk pregnancies) to express colostrum starting at the 36 week-mark was not dangerous.
You also may be breast/chestfeeding an older child while you are pregnant. This is generally thought to be safe, though, of course, talk to your provider.
Are there other ways to increase your milk supply while I am pregnant?
I warned you that my answer to this question was annoyingly “maybe. ” Ultimately, milk supplies are established by using that supply and demand system—feeding your baby when they are hungry and thus letting your body know it needs to make a lot of milk.
” Ultimately, milk supplies are established by using that supply and demand system—feeding your baby when they are hungry and thus letting your body know it needs to make a lot of milk.
That said, there are steps you can take to optimize your health and situation. These are not guarantees; they fall into the “can’t hurt, might help” category—but hey, it could be worth a try?
Here’s what I would suggest:
1. Eat well and hydrate.
Nourish your body with healthy and delicious foods: avocados, salmon, fruits and veggies, nuts, chocolate… foods that you love, that will give you the energy that you need and maybe help your body do the important work of making milk.
And hydrate. Hydration is so important during pregnancy—it helps stave off pre-term contractions, it gives you more energy, it supports your growing baby, and maybe it will help your body to make more milk.
On a related note, keep taking your prenatal vitamin after pregnancy—your body will be working super hard to heal and make milk, and supporting it with minerals and nutrients is very helpful.
2. Set up a feeding station in your home.
Make feeding your baby as easy and comfortable as possible. Create a little nook for yourself or claim the most comfortable spot on your couch. You’ll need one-handed access to the remote, snacks (trail mix for the win) and a HUGE cup with a straw to be filled with ice water. Trust me on this one, you’ll see.
While this isn’t going to have a direct impact on your milk supply, it’s going to make the experience of feeding your baby more pleasant. And who doesn’t want that?
3. Establish your feeding team.
This is the team of people in your life who are going to support you and your baby-feeding goals. It might include your partner, family members, friends, co-workers and/or a lactation consultant or counselor.
As I said in the beginning, a huge barrier to meeting our feeding goals is our society—lack of paid parental leave, judgemental comments, unsupportive work environments and so much more. These issues need to be addressed; in the meantime, let the people closest to you know how they can help you.
These issues need to be addressed; in the meantime, let the people closest to you know how they can help you.
Do you need your best friend to help you if a stranger comments about you feeding your baby in public?
Do you want your partner to tell you that you are doing a great job every day, or to take at least one feeding a day off of your hands?
Do you need your company to set up a pumping room for you at work?
These are all completely fair requests to make, so do not hesitate to vocalize your needs.
Remember through all of this that every day you are going to do the best you can. And as far as your baby is concerned, you are already perfect—and that has nothing to do with your colostrum.
Some of our favorite items to support you in your feeding journey.
‘The Motherly Guide to Becoming Mama’
The guide will take you from trying to conceive through the fourth trimester and infant-feeding journey (and everything in between).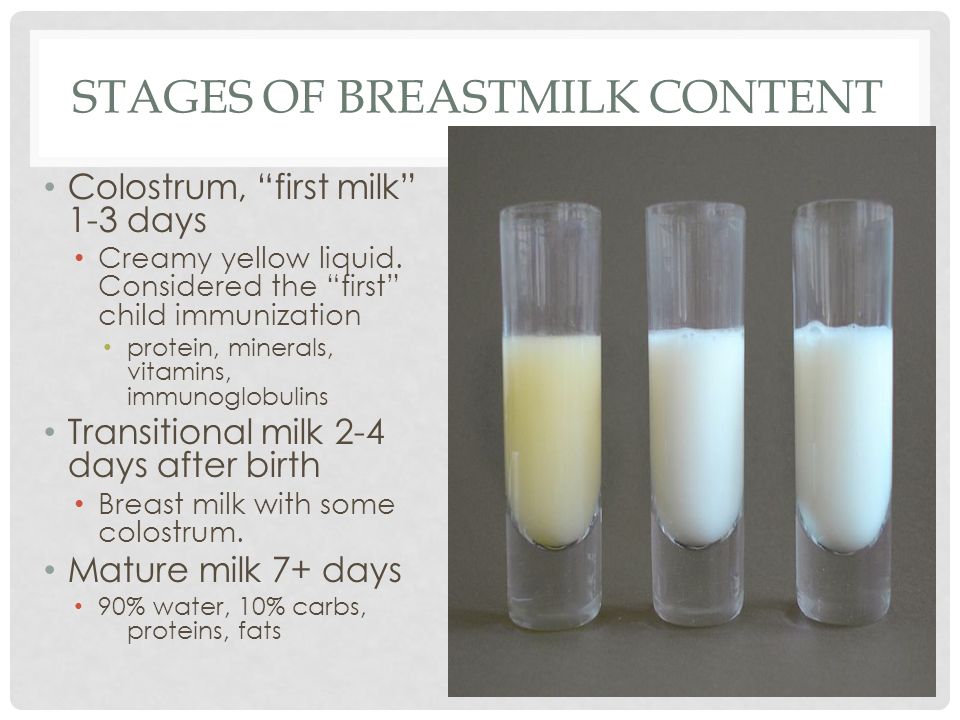
Willow breastpump
Meet the pump that everyone is obsessed with. This hands-free double electric pump allows you to get on with your day while providing nourishing milk for your baby, pumping efficiently and in comfort.
Nursing and pumping bralette
A good and supportive nursing bra makes more of a difference than we can describe. And when that bra also happens to be pretty? Sign us up for a drawer full, please. The Ruby bralette is stretchy and supporting and goes up to size 50G.
We independently select and share the products we love—and may receive a commission if you choose to buy.
Antenatal (prenatal) colostrum expression
Patient information leaflet * .
Colostrum is a fatty, nutrient-rich substance that is excellent for nourishing and protecting your baby from infections during the first days of life. It is especially rich in immunological factors that promote the growth and development of the infant's immune system and protect it from allergies and various diseases. Colostrum also helps the newborn eliminate meconium (original feces), which helps prevent jaundice. nine0005
Colostrum also helps the newborn eliminate meconium (original feces), which helps prevent jaundice. nine0005
This first milk begins to be produced at 16-20 weeks of gestation. Some women notice leakage of milk during pregnancy, while others may not. In both cases, this is normal and does not affect a woman's ability to breastfeed successfully.
The importance of exclusive breastfeeding for all newborns has been proven in many studies. Some babies may have difficulty breastfeeding as well as blood sugar regulation in the first few days after birth. By hand expressing and preserving colostrum during pregnancy, your baby will be able to get your milk despite the difficulties. Research data show that colostrum is able to stabilize blood sugar levels in newborns significantly better than formula. nine0005
You can start expressing colostrum from the 36th week of pregnancy, although if you notice milk leakage earlier, you can collect it in a sterile syringe. You can discuss this with your midwife or other healthcare provider. They can provide you with tools and guidance to start collecting colostrum.
They can provide you with tools and guidance to start collecting colostrum.
Benefits of collecting colostrum during pregnancy.
If women start harvesting colostrum during pregnancy, studies show that they:
- gain more confidence in how their breasts work even before the baby is born reach “full production” of milk faster
- increase their confidence that they will be able to breastfeed their baby manual pumping skills.
Most women can express during pregnancy, although there are several groups of mothers and children for whom antenatal colostrum expression may be particularly beneficial:
- Infants at risk for hypoglycaemia or possible difficulty sucking
- Children of mothers with diabetes mellitus
- Very small and low birth weight children
cleft lip or palate, or other congenital anomalies such as Down's Syndrome- when it is known during pregnancy that the baby will need special care in the neonatal unit
- Twins or triplets.
There are also women who, due to their common medical or gynecological history, will find it difficult to exclusively breastfeed their babies. Others suffer from certain diseases, such as multiple sclerosis, for which breastfeeding is very beneficial:
- any form of diabetes
- polycystic ovary syndrome
- breast hypoplasia
- previous breast surgery
planned caesarean section
In mothers with diabetes and allergies, as well as a family history of dairy intolerance, inflammatory bowel disease or diabetes, children may also have these diseases more often if they are fed artificial protein-based formulas from the first days of life cow's milk.
It is especially important for mothers with diabetes to completely avoid the use of artificial formulas, or at least not to use them until the baby is 6 months old. nine0005
Women with gestational diabetes are less likely to develop the disease after childbirth if they are breastfeeding.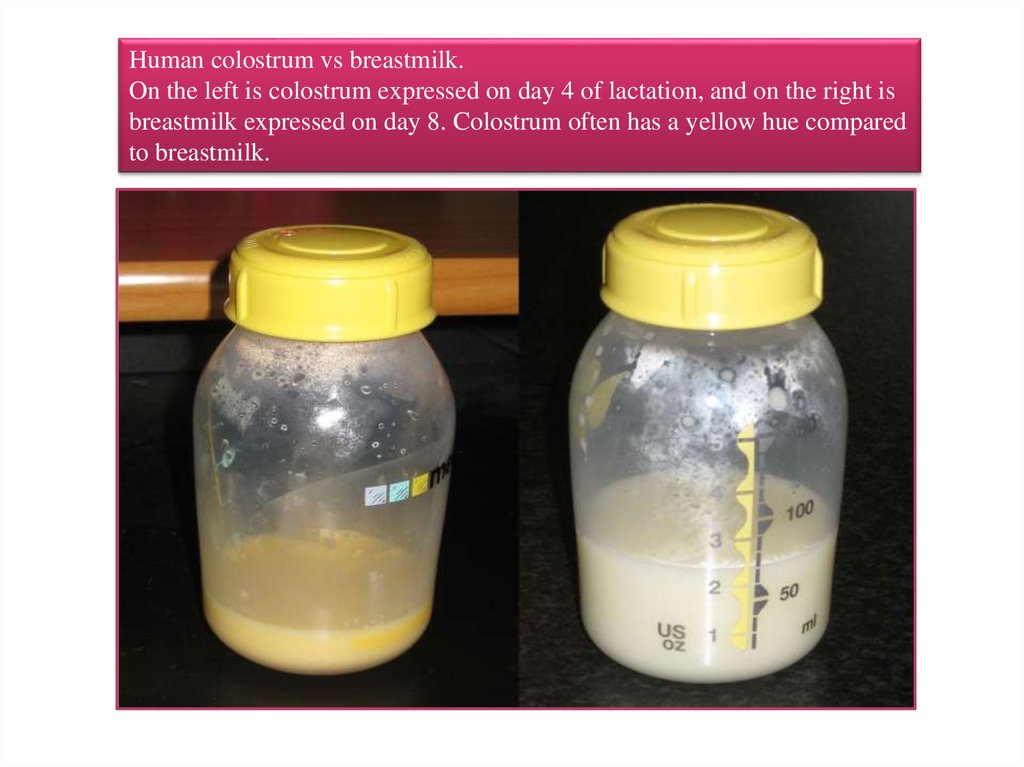
Women with diabetes should monitor their blood sugar levels especially if they express colostrum before giving birth. They may need to adjust their insulin doses and change their diet.
Are there women who should not express colostrum during pregnancy?
There is no scientific evidence that daily hand expression of colostrum activates labor in women who are not at risk for preterm birth. nine0005
However, we would advise some women not to actively express colostrum until a sufficient pregnancy is reached: multiple births before 36/40 weeks
- women with cervical sutures to prevent preterm labor
If you feel uterine contractions during pumping, you should stop the procedure. If contractions continue, contact your midwife. nine0005
How can I express colostrum during pregnancy?
Preparation.
To prevent cross-infection, please:
- wash your hands thoroughly before pumping
- wash your breasts no more than once a day (avoid using detergents that can irritate or dry out the skin on the nipples, causing soreness ).
Prepare a sterile milk collection container, such as a cup, bottle, wide-mouth container, or syringe (may be best for collecting small amounts of colostrum with minimal wastage). Activation of the release of OXYTOCIN (milk ejection reflex) can facilitate the outflow of milk. Find a quiet, secluded place where you can relax properly. You can gently massage your entire breast before pumping (you can see some of the massage techniques in the picture), be careful not to slide your fingers over the breast, as this can damage the skin. You can gently roll the nipple between your index and thumb. Some women find it helpful to put a warm diaper (soaked in warm water) over their breasts before pumping. nine0005
Make gentle circular motions with your fingertips.
Gently roll your clenched fist towards the nipple.
Locate the milk ducts.
Place your thumb on top of your chest with your index finger opposite it underneath. Both fingers are placed as far away from the base of the nipple as you can comfortably do. Gently “walk” your fingers along the chest until you find structures that feel different to the touch. nine0005
Gently “walk” your fingers along the chest until you find structures that feel different to the touch. nine0005
This means that you have felt the milk ducts (usually they are located 2-3 cm from the nipple).
Expression positions.
It can help if you lean forward slightly. Place your thumb and forefinger in the place where you found changes in the tissue of the gland. The thumb should be at 12 o'clock and the index finger at 6 o'clock, as shown in the picture (your hand is in a C-shape), covering the chest.
Pumping .
Without moving the thumb and forefinger, gently press the chest towards the chest (if the chest is large, it should be lifted first). Without releasing the pressure, roll your fingers towards each other to draw the milk out of the ducts. After that, you should reduce the pressure to allow the ducts to refill with milk. At first, you will be able to get only a few drops, but with practice, the amount of colostrum will increase. You can move your hand in a circle, changing the position of your thumb and forefinger, or change your hand, if necessary, to express milk from the entire breast. Collect drops of your colostrum in a sterile syringe or capped cup if more. You may find it easier to deal with this if your husband or other family members help you. Write your name, date of delivery, time and date of pumping on each syringe. Colostrum is usually produced in small amounts, so don't expect to be able to express a lot right away, although you might get lucky! You can make just 1 or 2 servings, but don't despair...every drop counts, and the more often you pump, the more likely you are to increase your milk production. Hand pumping is generally more effective than using a manual or electric breast pump. nine0005
You can move your hand in a circle, changing the position of your thumb and forefinger, or change your hand, if necessary, to express milk from the entire breast. Collect drops of your colostrum in a sterile syringe or capped cup if more. You may find it easier to deal with this if your husband or other family members help you. Write your name, date of delivery, time and date of pumping on each syringe. Colostrum is usually produced in small amounts, so don't expect to be able to express a lot right away, although you might get lucky! You can make just 1 or 2 servings, but don't despair...every drop counts, and the more often you pump, the more likely you are to increase your milk production. Hand pumping is generally more effective than using a manual or electric breast pump. nine0005
Colostrum can vary greatly in color from dark orange/brown, yellow/green to pale/clear. Don't worry if your colostrum changes color or consistency after a few pumps. This is fine. Rest assured, the colostrum has not "run out". You continue to produce colostrum until the milk "comes in" (about 3 days after your baby is born). You can pump as often as is comfortable for you.
You continue to produce colostrum until the milk "comes in" (about 3 days after your baby is born). You can pump as often as is comfortable for you.
What if colostrum is not produced? nine0004
Don't panic! For some mothers, pumping is not easy. Keep trying, it may take a few days for you to see the first drops of colostrum. If you're ready to continue, try to pump every day. Remember that it is not necessary to pump during pregnancy, however, if you do, it can be very beneficial. Be sure that when your baby is born, you will definitely be able to get colostrum.
Expression Assistance Manual:
- try pumping after a hot bath or shower
- put warm diapers on your chest to improve circulation
- relax!
- Gently massage your breasts before pumping
- Have your baby's ultrasound scan handy
What do you need?
You can ask your midwife for some sterile syringes for your first colostrum. Then you can buy them at a pharmacy or online. 1ml syringes work best. nine0005
Then you can buy them at a pharmacy or online. 1ml syringes work best. nine0005
How much colostrum should be collected?
As many as you want and can. Remember that a newborn's stomach is the size of a small balloon.
Colostrum storage.
In addition to preparing colostrum for your baby, there are other benefits to expressing your first milk. Many women feel more relaxed and secure knowing they have an "extra reserve" of colostrum in case their newborn needs it. nine0005
Put the syringe you used to collect the colostrum back into the package and place it in an airtight plastic container (such as a lunch box or freezer container). Freeze this serving of colostrum immediately.
Transportation of colostrum.
It is best to freeze the colostrum after you have collected it at home and take it to the hospital when needed. Use a cooler bag with ice when transporting colostrum to the hospital and ask medical staff to place it in a special refrigerator as soon as possible after delivery.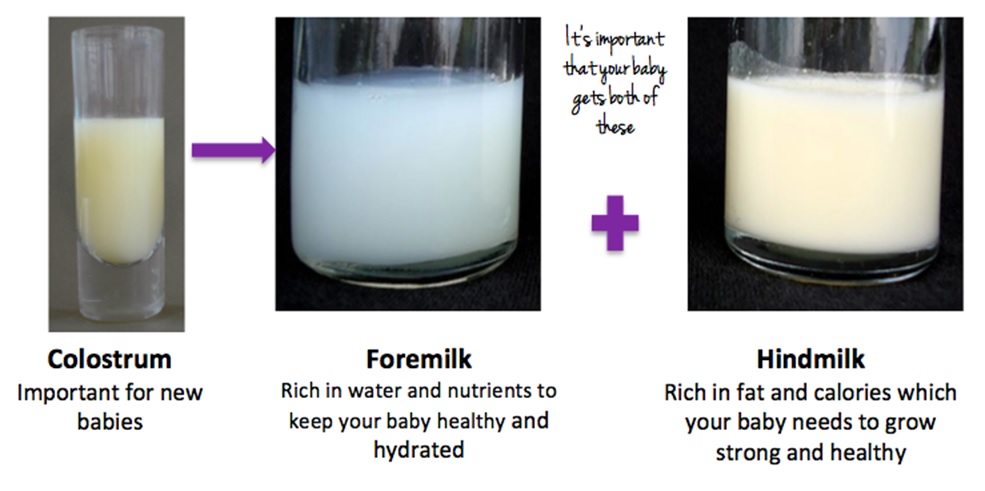 Once thawed, colostrum should be used within 12 hours, so to avoid wasting colostrum when it is thawed but not used, it is best to defrost a few syringes for each feed. nine0005
Once thawed, colostrum should be used within 12 hours, so to avoid wasting colostrum when it is thawed but not used, it is best to defrost a few syringes for each feed. nine0005
When the baby is born
Immediately after birth, continuous skin-to-skin contact between mother and baby should be established as early as possible to encourage initiation of breastfeeding (usually within the first 90 minutes after birth) . Ideally, your baby will suckle well at the breast soon after birth and will latch on frequently, so you won't need the expressed colostrum! However, some babies need regular supplements to keep their blood sugar levels stable, or the baby has some difficulty suckling. In this case, you will be provided with ongoing support to help resolve the difficulties, and in this situation, you can use pre-prepared colostrum. The medical staff will teach you how to feed your newborn with colostrum. You also need to take care to continue expressing colostrum regularly until your baby is able to breastfeed effectively in order to get the milk production back on track and provide the baby with it. We hope you enjoy expressing colostrum during pregnancy, as it will give you extra confidence and an invaluable reserve if you encounter difficulties in establishing breastfeeding. We hope you now know more about how your breasts work and how pumping during pregnancy will help you be more confident when you start breastfeeding your baby! nine0005
We hope you enjoy expressing colostrum during pregnancy, as it will give you extra confidence and an invaluable reserve if you encounter difficulties in establishing breastfeeding. We hope you now know more about how your breasts work and how pumping during pregnancy will help you be more confident when you start breastfeeding your baby! nine0005
Useful Contact Numbers Breastfeeding Midwife 01296 315799 Community Midwives Office (SMH) 01296 316120 Community Midwives Office (WH) 01494 425172
patients. If you have any comments or suggestions regarding this booklet, please contact us:
Head of Midwifery Women & Children’s Division Buckinghamshire Healthcare NHS Trust Stoke Mandeville Hospital Mandeville Road Aylesbury Buckinghamshire HP21 8AL
How can I help reduce hospital acquired infections?
Infection control is an important part of the well-being of our patients, which is why we have developed local infection control procedures. Frequent hand washing is an effective way to prevent the spread of infection. We ask you and your visitors to use hand sanitizer, which you can find before entering each room, before and after visiting the patient. In some cases, hands need to be washed in the sink with soap and water instead of just hand sanitizer. The hospital staff will let you know if additional hand sanitization is needed. nine0005
We ask you and your visitors to use hand sanitizer, which you can find before entering each room, before and after visiting the patient. In some cases, hands need to be washed in the sink with soap and water instead of just hand sanitizer. The hospital staff will let you know if additional hand sanitization is needed. nine0005
www.buckshealthcare.nhs.uk Follow us on Twitter @buckshealthcare
Author: L. Randell
Publication date: December 2016
Reissue date: December 2018
9 Leaflet code: n/a Version00 5002: 1
Translation: Tatyana Mamontova
*Attention! Antenatal (prenatal) expression of colostrum should be carried out only when indicated. If you think you need it, be sure to check with a breastfeeding support leader or lactation consultant beforehand
Colostrum during pregnancy | Medela
Colostrum is sometimes called liquid gold, and not only because of its color. We will tell you why this first food is so important for a newborn baby.
Share this information
Colostrum, the first milk produced at the start of breastfeeding, is the ideal nutrition for a newborn. It is very concentrated and rich in proteins and nutrients, so even in small quantities it saturates the tiny tummy of a newborn for a long time. Colostrum is low in fat and easy to digest, yet provides the baby with all the essential ingredients for an optimal developmental start. And perhaps most importantly, it plays a decisive role in the formation of the baby's immune system. nine0005
Colostrum looks thicker and yellower than mature milk. Its composition also differs in accordance with the special needs of the newborn.
Colostrum fights infections
Almost two-thirds of the cells in colostrum are white blood cells, which not only protect the baby's body from infections, but also teach them to fight them themselves. 1 “White blood cells are very important for the development of immunity. They provide protection and counteract pathogenic microbes,” says Professor Peter Hartmann of the University of Western Australia, a leading lactation expert. nine0005
They provide protection and counteract pathogenic microbes,” says Professor Peter Hartmann of the University of Western Australia, a leading lactation expert. nine0005
After giving birth, your body no longer protects the baby, and he must confront the new dangers of the world on his own. The white blood cells found in colostrum produce antibodies that can neutralize bacteria and viruses. These antibodies are especially good at dealing with indigestion and diarrhea, which is very important for very young children, whose intestines are not yet fully developed.
Colostrum supports the baby's immune system and intestinal function
Colostrum is especially rich in secretory immunoglobulin A -
is the most important antibody that protects the child from diseases, but not through the circulatory system, but as a protective coating of the mucous membrane of the gastrointestinal tract. 2 “The molecules that provide the mother's immune defenses enter the breast with her bloodstream, where they combine and form secretory immunoglobulin A, which is then transferred to the baby along with colostrum,” explains Professor Hartmann. “Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.” nine0005
“Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.” nine0005
Colostrum also contains many other immunological components and growth factors that stimulate the development of protective mucous membranes in the intestines of the child, and the prebiotics contained in it contribute to the formation of beneficial microflora. 3
Colostrum prevents jaundice
Colostrum not only protects against indigestion, but also has a laxative effect. This helps newborns to empty the intestines frequently, removing from it everything that was digested there in the prenatal state, in the form of meconium - dark and viscous feces. nine0005
Frequent stools in newborns also reduce the risk of jaundice. A baby is born with a high level of red blood cells that absorb oxygen from the air. As these cells break down, the liver helps to process them, producing a by-product called bilirubin. If the child's liver is not yet sufficiently formed to process it, bilirubin begins to be deposited in the body, causing jaundice. 4 The laxative properties of colostrum help the baby to remove bilirubin from the body along with the stool. nine0005
If the child's liver is not yet sufficiently formed to process it, bilirubin begins to be deposited in the body, causing jaundice. 4 The laxative properties of colostrum help the baby to remove bilirubin from the body along with the stool. nine0005
Colostrum contains vitamins and minerals
Carotenoids and vitamin A give colostrum its characteristic yellow color. . 7 Babies are usually born with a low supply of vitamin A, 8 and colostrum helps to replenish it.
"The first three days are especially important for establishing breastfeeding"
In addition, colostrum is rich in minerals such as magnesium, which is good for the baby's heart and bones, and copper and zinc, which are involved in the development of the immune system. 9.10 Zinc also contributes to the development of the brain, and there is almost four times more zinc in colostrum than in mature milk, 10 because the brain of a newborn must develop rapidly.
Colostrum helps your baby grow and develop
Colostrum contains many other ingredients that help your baby grow and develop. The role of some of them is still unknown to scientists. nine0005
“Colostrum retains its composition for about 30 hours after the baby is born,” says Professor Hartmann. - It contains quite a lot of proteins, because all the antibodies in its composition are essentially proteins. It is relatively low in lactose [milk sugar] and has a different fat composition than mature milk.”
In addition, colostrum is close in composition to the amniotic fluid that your baby swallowed and excreted while in the womb, making it ideal for adapting to the outside world. nine0225 11
Transition from colostrum to mature milk
Breast milk usually begins to arrive two to four days after birth. The breasts become firmer and fuller, and instead of colostrum, transitional milk is excreted, which is whiter in color and creamier in consistency.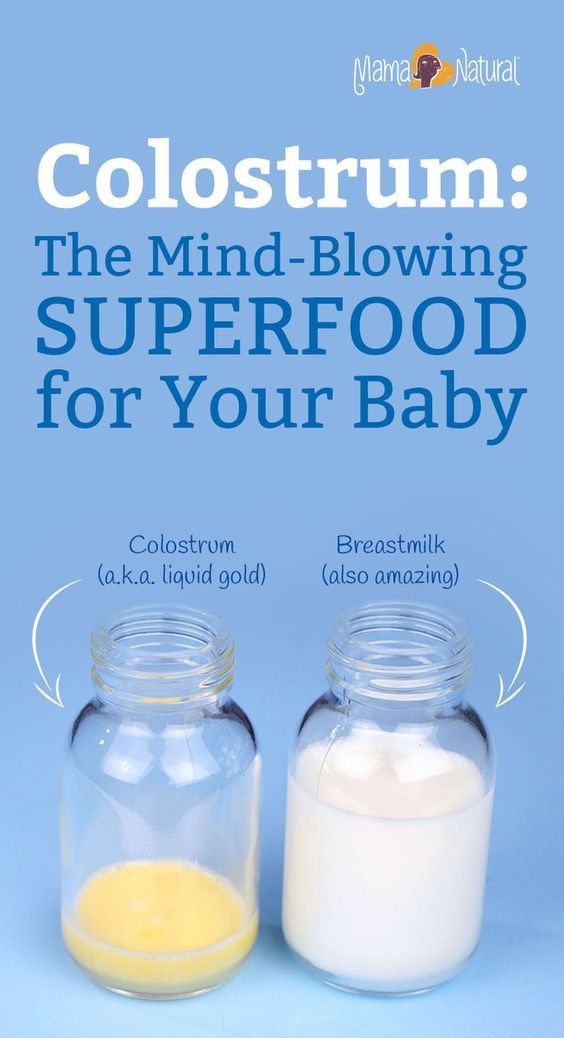
“The first three days are especially important for establishing breastfeeding,” says Prof. Hartmann. “If everything is done correctly during this period, lactation is likely to be good, and the baby will be able to grow normally.” nine0005
It seems unbelievable now, but in just one year your baby will be able to walk and maybe even talk. Colostrum is produced for only a few days, but makes an invaluable contribution to the development of the baby during the first 12 months, and the resulting benefits remain with him for life.
Want to know more? Read our free e-book Surprising Breast Milk Facts and article What is Transitional Milk?.
Literature
1 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk. 2 Pribylova J et al. Colostrum of healthy mothers contains broad spectrum of secretory IgA autoantibodies. nine0291 J Clin Immunol. 2012;32(6):1372-1380. - Pribylova J. et al., "Healthy mother's colostrum contains a broad spectrum of secretory autoimmune antibodies to immunoglobulin A". W Clean Immunol. 2012;32(6):1372-1380. 3 Bode L. Human milk oligosaccharides: every baby needs a sugar mama. Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." nine0291 Glycobiology (Glycobiology). 2012;22(9):1147-1162. 4 Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med (Lond). 20172;78(12):699-704. - Mitra S, Rennie J, Neonatal Jaundice: Etiology, Diagnosis, Treatment. 5 Patton S et al. Carotenoids of human colostrum. Lipids. nine0291 1990;25(3):159-165. - Patton S. et al., Carotenoids in Maternal Colostrum Lipidz. 1990;25(3):159-165.  " Clean Transl Immunology. 2013;2(4):e3.
" Clean Transl Immunology. 2013;2(4):e3. 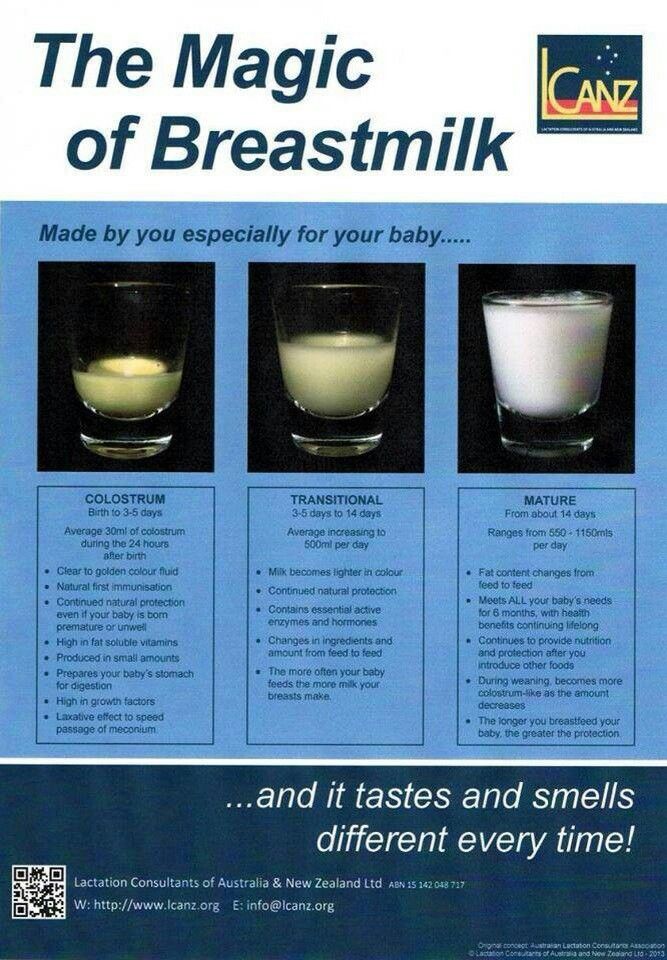 Br J Hosp Med (Lond). 20172;78(12):699-704.
Br J Hosp Med (Lond). 20172;78(12):699-704.
7 Bates CJ. Vitamin A. Lancet. 1995;345(8941):31-35. — Bates S.J., "Vitamin A". Lancet (Lancet) 1995;345(8941):31-35.
8 World Health Organization. e-Library of Evidence for Nutrition Actions (eLENA) [Internet]. Geneva , Switzerland : WHO ; 2018 [ Accessed : 05/14/2018].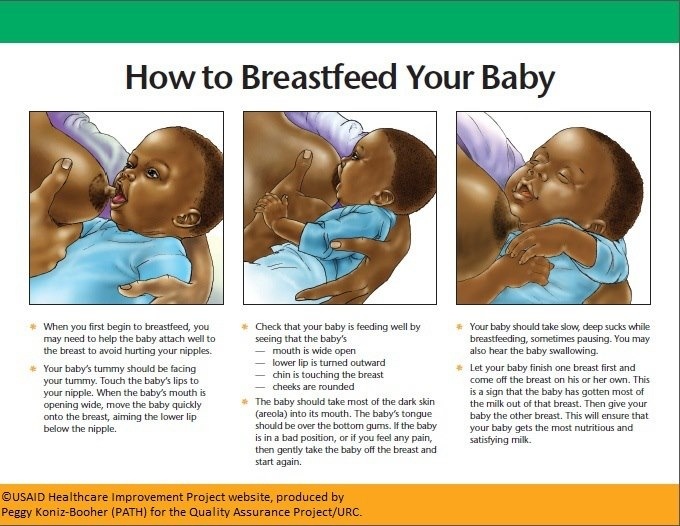 Available from Evidence-based electronic library on WHO nutrition activities ( eLENA ) [Internet]. Geneva, Switzerland: WHO; 2018 [visited 14 May 2018] Article at: [ www.who.int/elena/titles/vitamina_infants/en/ ]
Available from Evidence-based electronic library on WHO nutrition activities ( eLENA ) [Internet]. Geneva, Switzerland: WHO; 2018 [visited 14 May 2018] Article at: [ www.who.int/elena/titles/vitamina_infants/en/ ]
9 Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. AUST J EXP Biol MED SCI . 1981;59(1):101-114. - Kulsky JK, Hartmann PI, "Changes in the composition of breast milk at the onset of lactation". Aust Zh Exp Biol Med Sai. 1981;59(1):101-114. nine0291
10 Casey CE Studies in human lactation: zinc, copper, manganese and chromium in human milk in the first month of lactation. Am J Clin Nutr 1985;41(6):1193-1200.