Premature baby dies
What is a neonatal death?
What is a neonatal death? | Pregnancy Birth and Baby beginning of content4-minute read
Listen
A neonatal death is when a baby dies within the first 4 weeks after they are born. Dealing with a neonatal death can be very difficult for the whole family, but there is help and support available.
What is a neonatal death?
A neonatal death (also called a newborn death) is when a baby dies during the first 28 days of life. Most neonatal deaths happen in the first week after birth.
Neonatal death is different from stillbirth. A stillbirth is when the baby dies at any time between 20 weeks of pregnancy and the due date of birth.
Globally around 2.4 million children die in the first 28 days after birth. This is around half of all child deaths under the age of 5.
Neonatal death is rare in Australia, and rates are falling — there are about 700 neonatal deaths a year in Australia.
What are the causes of a neonatal death?
It’s not always known why a baby dies. However, the risk of neonatal death may be greater if a baby is born prematurely, is low birthweight, or has birth defects.
Prematurity and low birthweight cause about 1 in 4 neonatal deaths. Premature babies can develop life-threatening complications such as breathing problems, bleeding on the brain, infections and problems in their intestines (necrotising enterocolitis).
Low birthweight — if the baby weighs less than 2.5kg at birth — can also cause serious health problems such as difficulty breathing and feeding.
The most common birth defects that cause neonatal death include heart defects, lung defects, genetic conditions and brain conditions such as neural tube defect or anencephaly.
Sometimes a neonatal death may be caused by problems during the pregnancy, such as pre-eclampsia, problems with the placenta, or infections. It can also be caused by complications during the labour — for example, if the baby didn’t get enough oxygen.
It can also be caused by complications during the labour — for example, if the baby didn’t get enough oxygen.
What happens after a neonatal death?
If your baby dies, you might want to spend some time with them. You should take as long as you like. Some parents create memories of the baby by taking photos, handprints and footprints.
When you are ready to say goodbye, the hospital or a funeral director will take your baby to a funeral home. There will then be a burial or cremation.
By law, you must register both the birth and the death with Births, Deaths and Marriages in your state or territory.
In Australia, not all neonatal deaths are investigated by conducting an autopsy, also known as a post mortem examination. An autopsy is an examination to try to work out why the baby has died.
An autopsy cannot be done without the parents’ consent and it is up to you whether to agree to an autopsy after a neonatal death. The only time when an autopsy may be carried out without consent is if the case is referred to a coroner. This might happen if the death occurred in suspicious circumstances or if it was something to do with the health care the baby received.
This might happen if the death occurred in suspicious circumstances or if it was something to do with the health care the baby received.
An autopsy is done by a trained pathologist. If you agree to an autopsy, you can decide how detailed you would like it to be — whether it involves just examining the baby or removing organs to test why the death has happened.
Sometimes no cause of death can be found, even after an autopsy. It’s a good idea to discuss the benefits and downsides of an autopsy with a doctor, midwife or social worker. They will guide you through what needs to be done and will answer any questions you might have.
Learn more here about what happens after a neonatal death and what changes might occur to your body.
Where to find help
The death of a newborn baby can be devastating, both for the parents and for the whole family. So it’s important to get as much support as possible to help you through this difficult time.
Your doctor, midwife, maternal child health nurse or social worker will be able to guide you through what happens after the baby has died.
Sands Australia provides information and support for anyone who has experienced stillbirth or newborn death. You can speak to someone 24 hours a day on their helpline, 1300 072 637.
Red Nose Grief and Loss has information and resources. You can call their helpline 24 hours a day on 1300 308 307.
Lifeline supports anyone having a personal crisis — call 13 11 14 or chat online.
You can call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse.
Sources:
World Health Organization (Newborn deaths and illnesses), Raising Children Network (Neonatal death - a guide), March of Dimes (Neonatal death), The Royal Women’s Hospital Melbourne (Learning why a baby has died), Queensland Courts (Reportable deaths), Australian Institute of Health and Welfare (Stillbirth and neonatal deaths in Australia), Sands (Stillborn and newborn death), myDr (Low-birth-weight babies)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Your body after stillbirth or neonatal death
- Dealing with a neonatal death
- Birth trauma (emotional)
Need more information?
Baby and Infant Death
Baby and Infant Death A neonatal death is when a baby is born alive but dies within the first 28 days of life
Read more on Gidget Foundation Australia website
Death of a baby - Better Health Channel
Miscarriage, stillbirth or neonatal death is a shattering event for those expecting a baby, and for their families. Grief, relationship stresses and anxiety about subsequent pregnancies are common in these circumstances.
Read more on Better Health Channel website
When Your Baby is Stillborn or Dies Soon After Birth | Guiding Light - Red Nose Grief and Loss
Read more on Red Nose website
Breast care for breastfeeding mothers after the death of a child | Sydney Children's Hospitals Network
Time after the death of your infant can be physically and emotionally exhausting
Read more on Sydney Children's Hospitals Network website
Smoking | Red Nose Australia
Read more on Red Nose website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Neonatal death: a guide | Raising Children Network
What is neonatal death?
Neonatal death is when a baby dies within the first 28 days of life. Whether a baby dies soon after birth or after surviving a few weeks, it’s a very difficult experience for the whole family.
A baby might die for many reasons in the first 4 weeks after birth. For example, the baby might have been born prematurely, had congenital anomalies (birth defects) or become sick with an infection. Or there might have been complications in labour. And sometimes we just don’t know why.
Your baby’s death can bring intense feelings of grief, emptiness, anger, anxiety and depression. It’s OK to feel however you feel – there’s no one or right way to respond.
It’s OK to feel however you feel – there’s no one or right way to respond.
Spending time with your baby
Spending time with your baby creates memories and lets you acknowledge your baby as part of your family. Remembering and sharing these memories over time helps some people grieve. How you make memories of your baby is up to you and your family.
It’s OK to take as long as you need. Try not to feel pressured by other people’s expectations or experiences.
Spending time with your baby from birth
If you’ve been told your baby is unlikely to survive beyond 4 weeks, you can still spend time together from the moment your baby is born.
Nurses and midwives can help you hold and cuddle your baby as soon as possible.
You might name your baby and take photos together. And if you have other children, you might give them the chance to meet their sibling and have a photo taken together as a family.
Spending time with your baby when your baby has died
When your baby dies, you’ll have time with your baby. You might spend this time holding and cuddling your baby. You can name your baby, if you hadn’t done this already. Neonatal nurses and midwives can also help you to dress, bathe and take photos of your baby.
You might spend this time holding and cuddling your baby. You can name your baby, if you hadn’t done this already. Neonatal nurses and midwives can also help you to dress, bathe and take photos of your baby.
If you would like to spend a few days with your baby or take your baby home for a while, speak to your nurse or midwife, who can help to arrange this.
A neonatal death might affect other members of your family – children, grandparents and other relatives. You can decide whether you want to invite them to spend time with your baby.
Doctors, nurses, midwives, social workers, pastoral carers, bereavement midwives and funeral directors will help you with the things you need and want to do after your baby’s death. This includes organising a funeral.
Most hospitals will help you put some photos, footprints and a lock of your baby’s hair into a memory box. You can take this box home with you when you leave the hospital. Some hospitals might be able to look after this box for you until you feel ready to collect it. Or you can ask a trusted family member or friend to collect it for you.
Or you can ask a trusted family member or friend to collect it for you.
Moving your baby to the funeral home
Your hospital and chosen funeral directors will coordinate your baby’s move to a funeral home. Your baby will be cared for with dignity and respect.
While your baby is at the funeral home, you can still visit your baby up until the burial or cremation. Speak to your funeral director, who can arrange this for you.
For birthing mothers: your body after neonatal death
Bleeding
After birth, you might have some vaginal bleeding for 5-10 days. This can last up to 6 weeks. This is normal. It’s important to see a GP or obstetrician if you have:
- heavy bleeding that doesn’t stop
- severe abdominal cramps
- signs of a fever.
Milk production and breast soreness
Milk suppression – or stopping breastfeeding and expressing – can be physically and emotionally difficult after a neonatal death. It can be a few weeks before your breasts stop producing milk.
It can be a few weeks before your breasts stop producing milk.
To prevent engorged breasts, it helps to express breastmilk sometimes. Express just enough for comfort – expressing too much can stimulate an increase in supply. Or you could talk to your GP or obstetrician about medicines for managing breast discomfort or suppressing milk supply.
Neonatal nurses, midwives and lactation consultants can give you advice and support during this time.
If you have breast pain, swelling, warmth, fever and chills, it’s important to see a GP. This might be the beginnings of mastitis, which is an inflammation of the breast that can lead to an infection. Mastitis can happen when a milk duct becomes blocked. Massaging any lumps or expressing a small amount of milk can help with this.
It’s possible to donate frozen breastmilk to milk banks to feed premature babies. Speak to your nurse or midwife if this is something you’d like to do.
Understanding why your baby died
Your doctor might ask if you’d like to have an autopsy done on your baby to find out more about why your baby died. Knowing why a baby died helps some people grieve. The information might also help doctors give you advice about future pregnancies.
Knowing why a baby died helps some people grieve. The information might also help doctors give you advice about future pregnancies.
Sometimes an autopsy won’t be able to tell you why your baby died. Even if the autopsy can’t explain your baby’s death, knowing you tried to find out why your baby died can be reassuring.
It can be hard to decide about having an autopsy done on your baby. It’s your choice. Doctors, nurses, midwives, social workers and pastoral carers can explain your options and support you as you decide what’s best.
Getting help after stillbirth
It can help to talk to a trusted family member or friend about your loss. And if you feel you aren’t coping, you might need professional help too.
See your GP, a counsellor or a community spiritual leader, if you have one. A social worker at the hospital or your GP can help you find a local counselling service.
You can also get support by calling:
- Red Nose Grief and Loss on 1300 308 307
- Bears of Hope on 1300 114 673
- Sands on 1300 072 637
- MensLine on 1300 789 978
- Lifeline on 131 114.

Legal information about neonatal death
By law, all neonatal deaths in Australia must be registered with Births Deaths and Marriages in your state or territory. Visit your state or territory’s Births Deaths and Marriages website for more information.
In most states and territories in Australia, it’s also a legal requirement to arrange a burial or cremation for your baby.
In some cases, your baby’s death might require a coroner’s investigation to find out the cause of death. Hospital staff will guide you through this process if it needs to happen.
If your baby has died, you might be eligible for some financial support from Services Australia.
“The child was alive and was not going to die for the next few hours”
The Moscow Regional Court on Tuesday sentenced Kaliningrad doctors Elina Sushkevich and Elena Belaya to nine and nine and a half years in a penal colony in the case of the murder of a premature baby (part 2 of Art. 105 of the Criminal Code of the Russian Federation "Murder of a minor or other person who is obviously in a helpless state for the guilty person").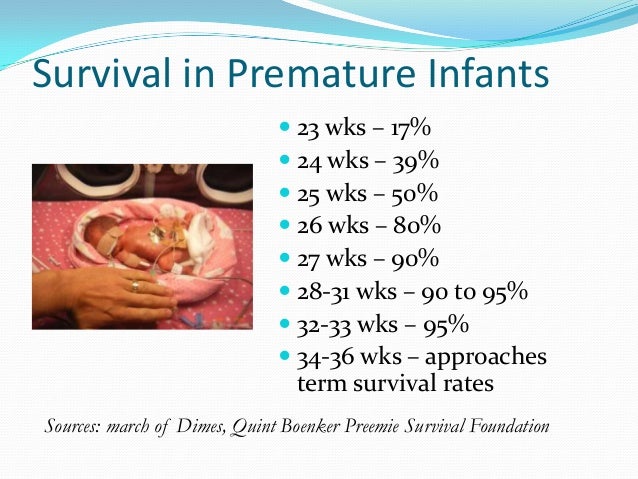 They were also banned from working in their profession for three years after their release.
They were also banned from working in their profession for three years after their release.
“To appoint Sushkevich a sentence of imprisonment for a term of nine years with serving a sentence in a general regime colony ... to appoint Belaya a sentence of imprisonment for a term of nine years and six months in a general regime colony,” the judge announced the decision.
In addition, they were banned from working in their profession for three years after their release. The prosecution asked for each defendant to be sentenced to 13 years in prison and a three-year ban on working in the profession after release.
Previously, the jury decided to find the doctors guilty and not deserving of leniency. The defense has already stated that it will appeal the verdict, believing that the judge actually took the position of the prosecution, thus influencing the decision of the jurors.
Question of guilt
In recent years, this is one of the most resonant "medical" criminal cases in Russia. The main question discussed in the medical community is whether the acting officers are guilty. the head physician of the maternity hospital and an anesthesiologist-resuscitator in the death of a premature newborn weighing 700 grams.
The main question discussed in the medical community is whether the acting officers are guilty. the head physician of the maternity hospital and an anesthesiologist-resuscitator in the death of a premature newborn weighing 700 grams.
The investigation proceeds from the fact that doctors intentionally killed baby , the defense insists that there was no malicious intent. According to the prosecution, in November 2018, a woman was admitted to the maternity hospital No. 4 in Kaliningrad, who at 23-24 weeks of pregnancy gave birth to a boy weighing about 700 grams.
The UK claims that acting The head physician of this maternity hospital, Belaya, decided to kill the newborn, for which she attracted the anesthesiologist-resuscitator of the regional perinatal center Sushkevich, who arrived at the scene as part of the resuscitation team and injected the baby with magnesium sulfate, from which he died.
After Roshal's letter. The Investigative Committee drew attention to the case of Kaliningrad doctors
Doctor Leonid Roshal stood up for Kaliningrad doctor Elina Sushkevich, who is accused of murder. ..
..
October 29 12:40
According to investigators, Belaya's decision to kill a child was connected with severe pathologies in a premature newborn, and she, fearing a deterioration in performance, instructed Sushkevich to administer drug . Further "deliberately false information was entered into the history of childbirth that there was a fact of death of the fetus" .
The defense insists that the fact of drug administration has not been proven. The same position was held by the jury, as a result of which, in December 2020, the doctors were acquitted. The defense also found that the mother of the child took a drug containing magnesium during pregnancy.
Progress
On December 10, 2020, the jury found the doctors not guilty. Representatives of the injured party and the Prosecutor General's Office filed an appeal, noting that the jury was pressured by the public and the media. The prosecutor's office appealed the verdict and at the end of May 2021, the First Court of Appeal of General Jurisdiction overturned it and sent it for review. At the request of the Prosecutor General's Office, the Supreme Court moved the hearings from Kaliningrad to the Moscow Regional Court.
At the request of the Prosecutor General's Office, the Supreme Court moved the hearings from Kaliningrad to the Moscow Regional Court.
The cancellation of the acquittal caused indignation in the professional community. Thus, the president of the National Medical Chamber Union of Doctors, Leonid Roshal, called for the release of doctors from custody and spoke of his readiness to sit in a pre-trial detention center instead of them.
During the investigation in Kaliningrad, the doctors were under house arrest. After the completion of the trials, Sushkevich returned to work at the regional perinatal center, and Belaya took the position of deputy head physician of maternity hospital No. 4. On November 5, 2021, at the very first meeting in the Moscow Regional Court, Sushkevich and Belaya were taken into custody, explaining the decision, among other things, by the fact that they do not have registration in the Moscow region. They were placed in SIZO No. 6 in Pechatniki.
“The child was not going to die at all”
One of the key witnesses in the case is Alena Sukhar (Kiyanenko), a nurse at maternity hospital No. 4, who was on duty on the night of November 6, 2018, when the child died. The defense needed the nurse's testimony during the hearing in order to record it in the case file (she had previously testified during the preliminary investigation). However, Sukhar failed to appear at the hearing three times, and the court refused to admit her testimony to the case.
4, who was on duty on the night of November 6, 2018, when the child died. The defense needed the nurse's testimony during the hearing in order to record it in the case file (she had previously testified during the preliminary investigation). However, Sukhar failed to appear at the hearing three times, and the court refused to admit her testimony to the case.
Doctors' lawyer Kamil Babasov in a conversation with the Kommersant newspaper told that the trial is proceeding, "to put it mildly, with an accusatory bias." According to him, the judge rejected all the motions of the defense, including a request to be heard by a panel of sworn neonatologists and a toxicologist. The court considered the motions unfounded.
“The court said that everyone understood everything. But we still have a lot of questions for the experts, primarily on the calculation of the concentration of magnesium sulfate in the baby's blood. We believe that the expert opinions in the case file are unreliable,” the lawyer complained.
Lawyer for the family of the victims Larisa Guseva, in her turn, is satisfied with the course of the trial and awaits a guilty verdict from the jury.
“I believe that the actions of Belaya and Sushkevich are qualified correctly, and it is unacceptable to talk about whether the child was in an agonal state. There is no such concept in the legislation. There are only the concepts of "liveborn" and "stillborn" . He was born alive, and the doctors had to save him in any case, ”said Guseva.
Guseva referred to the words of the head of the group of forensic experts: even at the beginning of the trial in Kaliningrad, he told the court that child
"was alive and would die for the next few hours, or maybe days, or maybe he was not going to die at all."
Doubts of professionals
The Russian Society of Neonatologists, the National Medical Chamber headed by Leonid Roshal, and a number of chief freelance specialists of the Ministry of Health of the Russian Federation stood up for the doctors. Initiative doctors launched the #YaElinaSushkevich campaign on social networks, and a petition in defense of the neonatologist gained more than 270,000 signatures. Sushkevich's colleagues reacted extremely negatively to the annulment of the acquittal and the return of the case to court, calling the process "demonstrative". According to doctors, the indictment and the trial are based, rather, on the ethical side of the death of a baby, and the objective medical indicators given by the defense and the expert community are not taken into account.
Initiative doctors launched the #YaElinaSushkevich campaign on social networks, and a petition in defense of the neonatologist gained more than 270,000 signatures. Sushkevich's colleagues reacted extremely negatively to the annulment of the acquittal and the return of the case to court, calling the process "demonstrative". According to doctors, the indictment and the trial are based, rather, on the ethical side of the death of a baby, and the objective medical indicators given by the defense and the expert community are not taken into account.
Doctors' case 2.0: how they kill the desire to treat
I quite consciously did not immediately give a detailed comment on the criminal case initiated against...
21 July 21:40
“We, as a community, support Elina (Sushkevich) and are absolutely sure of her innocence, as we have sorted out every letter of the case materials that were available. And we believe that the verdict can only be acquitted,” Diana Mustafina-Bredikhina, a lawyer with the Russian Society of Neonatologists, told Kommersant.
However, the editor-in-chief of the Medical Russia portal, Igor Artyukhov, in the course of his own analysis of the conclusions of forensic experts, the arguments of the defense and the prosecution, discovered "a number of contradictions." He noted the audio recording of a fragment of a conversation between Elena Belaya and her subordinates, on the morning of November 6, 2018, made by Tatyana Sokolova, head of the maternity ward of maternity hospital No. 4. On the recording, Belaya reprimands doctors for providing resuscitation care to a child in serious condition: “... You set everyone up, including the chief freelance obstetrician-gynecologist. Therefore, we sit down and rewrite history and do antenatal (antenatal death - the death of the fetus during pregnancy. - approx. "Gazety.Ru"). According to him, many doctors, including neonatologists, "understood what really happened to the child."
“It was after the publication of this recording that the defense suddenly began to publicly accuse the duty shift of negligence. It is only unclear where now the lawyers should put all the statements about the unexamined woman in labor and the negligible chances of the baby to survive, ”Artyukhov said.
It is only unclear where now the lawyers should put all the statements about the unexamined woman in labor and the negligible chances of the baby to survive, ”Artyukhov said.
According to Academician of the Russian Academy of Sciences, Honored Doctor of Russia Nikolai Volodin, the baby was not given proper assistance after birth, and the court, for some reason , does not insist on bringing important witnesses to the case.
“The prosecution does not take any measures to ensure the appearance in court for testimony of nurse Alena Sukhar, who previously indicated that while swaddling a newborn at 6 a.m. , she found him - 700-gram, lying in a pool of blood . And no one thought to do anything to still start saving his life! Upon arrival, Dr. Sushkevich immediately demanded to determine the child's blood type and Rh factor for an urgent order of donor blood, injected him with physiological saline and soda intravenously. But the time is irretrievably gone! Volodin said.
Neonatologist, Professor, Head of the Department of Neonatology, N.I. N.I. Pirogova Marina Degtyareva also insists on the inconsistency of the charges. In her opinion, the formula by which the concentration of a substance in the body of an infant was calculated is not used in medical circles . She also recalled that to determine the concentration of the drug in the blood, it is necessary to examine either the blood or the placenta, but not the blood in the organs.
“Calculations of the concentration of magnesium in the blood serum of a newborn infant, performed as part of a forensic medical examination, are based on sweeping statements and conjectures, unsubstantiated. The logical conclusions of experts do not take into account the laws of human physiology and, therefore, are UNACCEPTABLE PROOF of the cause of death of a very premature boy, ”Degtyareva said in an open letter.
Life in the palm of your hand. International Day of Premature Babies
How premature babies are saved in Russia
November 17 is International Prematurity Day to draw attention to this medical issue. In Russia, more than a hundred thousand babies are born prematurely every year. How doctors manage to save them - in a special TASS report.
In Russia, more than a hundred thousand babies are born prematurely every year. How doctors manage to save them - in a special TASS report.
"So, talkers, why are we standing?" - Olga Babak, head of the resuscitation department for premature babies, is rapidly entering the hospital box. She smiles fervently at the three mothers who are having a quiet conversation with their children near the incubators: "The children hardly saw them for a day, but they would only talk! Disgrace!"
When the doctor appears, the women perk up, take half a step away from the incubators and fix their glances on Olga, in which a dumb question is read. He is the same for everyone here - how does the child feel? Are there any improvements?
For parents who spend many months in intensive care unit No. 2 of the Moscow Perinatal Center of the 24th City Clinical Hospital, Olga Alekseevna is the person who supports them even in the darkest days, does not let them give up and despair.
Olga Babak has been working at in the intensive care unit for newborns and premature babies for 20 years
“When a new child comes to us and his parents come to me for the first time, I immediately explain to them: there’s no need to cry here,” says Olga Babak. , people who are clearly aware that we have a serious hard struggle ahead of us and that a child next to us needs not a sticky, but a loving and strong parent.
"That's what she's telling you! - immediately after the doctor leaves the ward, one of the mothers adds in a whisper, - but in fact she will cheer up and always say something kind, however, she really does not welcome tears in boxing" .
Olga Babak has been working in the intensive care unit for newborns and premature babies for 20 years. During this time, thousands of children born several months prematurely passed through her hands. She says that her patients are the most unpredictable, and every day is a battle for life, it is difficult to give predictions here, which parents are waiting for.
"Many people think that they have a very small child, such an inch, who just needs to grow up, gain weight in an incubator, and everything will be fine. And when such a child dies, they ask: "After all, he lived for three months, everything was fine Why did this happen?" The fact that the child lived on machines, on medicines, thanks to the incredible efforts of doctors, they sometimes do not realize.
Babies stay in the ICU for several months, and sometimes longer
Olga Babak admits that over the years of work she has never developed "professional cynicism" when you stop reacting sharply to the death or severe disability of a patient. Each such case for her is a defeat and pain that she has to pass through herself. But the strength to go on is given by those who managed to save. Fortunately, the doctors of the Perinatal Center of City Clinical Hospital No. 24 nurse 85% of their little wards per year.
"We communicate with many children and their parents later. I even have "favorites". For example, Pashka. That was more than ten years ago," recalls Olga Babak. the end of the shift was five minutes away when the doctor called me, because the condition of one child deteriorated sharply, resuscitation was needed. Then we literally “pulled” him out. Then I called my friends, apologized for not being able to come and did not warn. "
Pasha survived, now he is in the sixth grade. When meeting Olga Babak sometimes jokes: "Pashka, you owe me a ticket. When you grow up, take me to the theater!"
Doctors monitor the vital signs of premature babies around the clock
The prematurity resuscitation corridor is brightly lit day and night. To the right and to the left - boxes in which the blinds are almost always lowered and the lamps are turned off - for the eyes of premature babies, harsh light is fatal. In transparent incubators - special containers in which conditions are created as close as possible to those that were in the womb - children lie.
In transparent incubators - special containers in which conditions are created as close as possible to those that were in the womb - children lie.
When you see premature babies for the first time, you experience shock mixed with emotion and pity. The boy in the first box at admission weighed only 700 grams, and now - already 1300, but still resembles a baby doll from a toy store in size. A sensor with a red light is attached to the baby's heel, and the red light shines through the tiny leg. There are a lot of sensors and tubes - on the arm, on the stomach, in the nose.
A person who is far from medicine cannot understand how a catheter can be inserted into such veins, how one can even pick it up without damaging it, but then the nurse Zaira Magomedova comes and opens the incubator.
The conditions in the incubators are as close as possible to those in the mother's womb
"You're my good, let's change pants!" - Zaira says affectionately and removes a tiny, like a toy, diaper from the baby, which is still big for him. Then she deftly wipes the baby with wet wipes, smears it with cream, puts on a new diaper, knitted socks on the legs, covers it with a knitted blanket the size of a table napkin and closes the pitcher with a cotton blanket on top.
Then she deftly wipes the baby with wet wipes, smears it with cream, puts on a new diaper, knitted socks on the legs, covers it with a knitted blanket the size of a table napkin and closes the pitcher with a cotton blanket on top.
"Well, now sleep!" Zaira adds in a whisper and strokes the child's head. She has been working in the pediatric intensive care unit for a year, her mother brought her here, also an intensive care sister.
"At first I was afraid to even pick them up — they were so tiny. It was hard to get used to the fact that anything could happen to them at any moment. right in the heart. I remember how scared I was. The baby was saved. Now I'm already used to such situations. "
Zaira has been working in the intensive care unit for premature babies for a year now and admits that at first she was even wary of taking them in her arms, afraid of harming them
Zaira is a student, works day or night. It would seem that the schedule is convenient, but for a day here it is laid out in such a way that then it comes to its senses in two days. At lunchtime, she only has time to go to the staff room for a few minutes and have a quick bite to eat. Sleep at night, even if only for a couple of hours, is out of the question - you can't leave such patients a single step. But, despite the difficulties, Zaira is seriously thinking about working here after university.
It would seem that the schedule is convenient, but for a day here it is laid out in such a way that then it comes to its senses in two days. At lunchtime, she only has time to go to the staff room for a few minutes and have a quick bite to eat. Sleep at night, even if only for a couple of hours, is out of the question - you can't leave such patients a single step. But, despite the difficulties, Zaira is seriously thinking about working here after university.
“I really like talking to them,” says the girl, “Those who are already gaining a little, who are more than a kilogram, it’s generally interesting with them, their characters are already manifesting, you already know what someone loves. For example, some who he can already breathe on his own, they like to swim: I put a towel in a clean sink, pour warm water - and swim.
Most ICU patients weigh around a kilogram or less. There are even those who weigh only 600 grams. But the formula "the less weight, the more difficult the condition" does not always work here.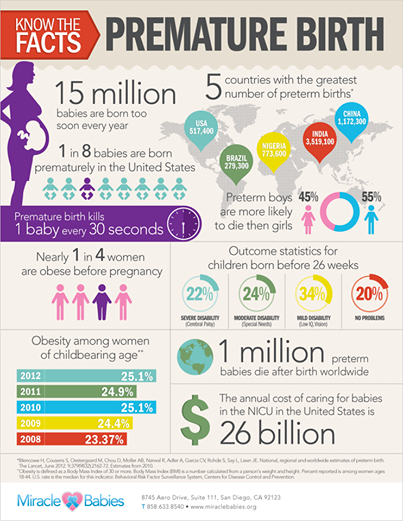
"If we take a child who was born weighing a kilogram at 26 and at 29 weeks, then it is likely that the later born one will have more chances of survival - simply because he already has better developed organs, a nervous system" , — explains resuscitator Maria Mumrikova.
Modern technology allows you to monitor whether the baby's body is developing correctly
One of the most common problems in premature babies is the lungs that have not yet formed. When exhaling, they seem to "stick together", and without special drugs that the doctor injects in the first hours of life, children die. Another danger is retinopathy, a serious eye disease that can develop due to the immaturity of the optic nerve. Toddlers are very susceptible to infectious diseases, which are much more severe than in adults, and can lead to severe disability. That is why antibiotics are almost always used in treatment.
Most premature babies spend several months in intensive care unit No. 2 of the Perinatal Center of City Clinical Hospital No. 24 before their condition, in medical terms, stabilizes.
2 of the Perinatal Center of City Clinical Hospital No. 24 before their condition, in medical terms, stabilizes.
"When a child can live without devices, without antibiotic treatment, when he starts breathing spontaneously, we transfer him to the children's department of the center, where he is already being prepared for life at home," says Maria Mumrikova.
At three o'clock in the afternoon, the parents of the kids come to the intensive care unit. They quietly go into the pits and cling to the couveuses - they are given two hours to communicate with the children.
“With those children who can be picked up, we practice the kangaroo method or “skin to skin”, when mom or dad presses the child to the naked body,” explains Olga Babak. This method provides physiological and psychological closeness with the child, helps him to regulate his own temperature.
But for almost all patients, breastfeeding has been replaced by tube feeding - it is still very difficult for premature babies to suckle, doctors save their energy, which is needed for growth and maintenance of the body.
Parents have two hours a day to communicate with their child
Ekaterina Guryanova cannot breastfeed her son - he is still very small, connected to the machines, but every day she brings him her milk in a bottle, and the nurses feed him through a tube.
“It is important for me that he eats his mother’s milk, the doctors looked at it very well,” says Ekaterina. “Many mothers lose milk because of nerves, but I still hold on, probably because I believe in its miraculous power.”
Kolya was born with a weight of 760 grams, recovered in a couple of months and now weighs 1300 grams. Ekaterina recalls that she did not have any visible health problems, although from the very beginning of pregnancy she felt unwell. She writes off premature birth by carrying her eldest three-year-old son in her arms.
Marina Zhoromskaya is leaning over her son Leonid in the next box. There is a smile on her face, her eyes are shining: in a few months of being here, she learned the rule, which Olga Babak, the head of the department, insists on, - to leave all sorrows and tears behind the doors of intensive care. Lenya, born on the 25th week of pregnancy, Marina considers a gift from above.
Lenya, born on the 25th week of pregnancy, Marina considers a gift from above.
Marina Zhoromskaya with her son
“I already have two almost adult sons - I didn’t even think about a third,” says Marina. “I got pregnant, despite contraception with a spiral. visiting my eldest son in China, where he studies, I even bought tickets, but on the eve of departure, I went into labor. It’s good that I wasn’t on the plane, they definitely wouldn’t have saved Kolya! And now I know for sure that everything will be fine. "
All causes of preterm birth are not yet fully understood by medical science. It is known that maternal infections can provoke early birth. At risk are pregnancies that occurred in adulthood, as a result of artificial insemination - IVF, after an abortion. Another reason that can cause premature birth is high blood pressure in the mother.
The pregnancy of 37-year-old Elena Polishchuk from Kemerovo was difficult. On the 28th week, she was hospitalized with high blood pressure, the doctors gathered a council, deciding that emergency intervention was needed due to the developed oxygen starvation in the child. The woman was transferred to the Kemerovo Regional Clinical Perinatal Center.
On the 28th week, she was hospitalized with high blood pressure, the doctors gathered a council, deciding that emergency intervention was needed due to the developed oxygen starvation in the child. The woman was transferred to the Kemerovo Regional Clinical Perinatal Center.
"I had an emergency caesarean section," Elena recalls. "My daughter Masha was born weighing 675 grams and 32 cm tall."
"At 28 weeks, the girl was smaller than expected by this period, when the weight should be about 900-1000 grams," says Olga Kireeva, deputy chief physician of the perinatal center for pediatrics.
A person who is far from medicine cannot understand how a catheter can be inserted into the veins of such a crumb
For the first time, Elena was able to take her daughter in her arms only 12 days after her birth. For more than a month the child could not breathe on his own, the doctors fought pneumonia, the girl did not digest food well. But resuscitators managed to save the baby: by the day she was discharged, she weighed 1300 grams, learned to breathe without an apparatus, and managed to avoid vision problems.
But resuscitators managed to save the baby: by the day she was discharged, she weighed 1300 grams, learned to breathe without an apparatus, and managed to avoid vision problems.
"Until the year we took courses in massage, gymnastics, physiotherapy, were observed by an ophthalmologist and a neurologist," says Elena Kireeva. "In the second year of life, we were faced with the fact that there were slight delays in speech development, but Masha coped with all this" .
Now five-year-old Maria Kireeva goes to an ordinary kindergarten and is no different from her peers, she even gets sick no more often than others.
Every year in Russia more than 110 thousand children are born with severe prematurity. According to the Russian Ministry of Health, 20 years ago, almost 80% of babies born weighing less than a kilogram died or received a profound disability.
In recent years, thanks to medical technologies and modern equipment that maternity hospitals and perinatal centers are equipped with, this figure has been reduced to 30%, and in some even to 10-15%.