Child birth and labor
Labor and birth | Office on Women's Health
Cesarean delivery, also called c-section, is surgery to deliver a baby. The baby is taken out through the mother's abdomen. Most cesarean births result in healthy babies and mothers. But c-section is major surgery and carries risks. Healing also takes longer than with vaginal birth.
Most healthy pregnant women with no risk factors for problems during labor or delivery have their babies vaginally. Still, the cesarean birth rate in the United States has risen greatly in recent decades. Today, nearly 1 in 3 women have babies by c-section in this country. The rate was 1 in 5 in 1995.
Public heath experts think that many c-sections are unnecessary. So it is important for pregnant women to get the facts about c-sections before they deliver. Women should find out what c-sections are, why they are performed, and the pros and cons of this surgery.
Reasons for c-sections
Your doctor might recommend a c-section if she or he thinks it is safer for you or your baby than vaginal birth. Some c-sections are planned. But most c-sections are done when unexpected problems happen during delivery. Even so, there are risks of delivering by c-section. Limited studies show that the benefits of having a c-section may outweigh the risks when:
- The mother is carrying more than one baby (twins, triplets, etc.)
- The mother has health problems including HIV infection, herpes infection, and heart disease
- The mother has dangerously high blood pressure
- The mother has problems with the shape of her pelvis
- There are problems with the placenta
- There are problems with the umbilical cord
- There are problems with the position of the baby, such as breech
- The baby shows signs of distress, such as a slowed heart rate
- The mother has had a previous c-section
Patient-requested c-section: Can a woman choose?
A growing number of women are asking their doctors for c-sections when there is no medical reason.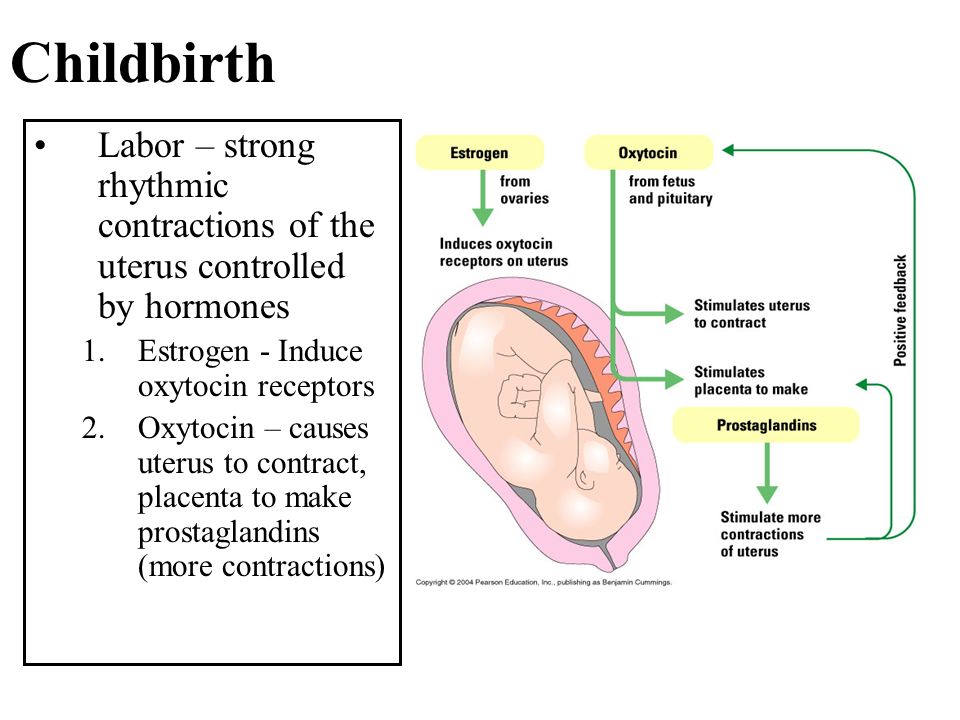 Some women want a c-section because they fear the pain of childbirth. Others like the convenience of being able to decide when and how to deliver their baby. Still others fear the risks of vaginal delivery including tearing and sexual problems.
Some women want a c-section because they fear the pain of childbirth. Others like the convenience of being able to decide when and how to deliver their baby. Still others fear the risks of vaginal delivery including tearing and sexual problems.
But is it safe and ethical for doctors to allow women to choose c-section? The answer is unclear. Only more research on both types of deliveries will provide the answer. In the meantime, many obstetricians feel it is their ethical obligation to talk women out of elective c-sections. Others believe that women should be able to choose a c-section if they understand the risks and benefits.
Experts who believe c-sections should only be performed for medical reasons point to the risks. These include infection, dangerous bleeding, blood transfusions, and blood clots. Babies born by c-section have more breathing problems right after birth. Women who have c-sections stay at the hospital for longer than women who have vaginal births. Plus, recovery from this surgery takes longer and is often more painful than that after a vaginal birth. C-sections also increase the risk of problems in future pregnancies. Women who have had c-sections have a higher risk of uterine rupture. If the uterus ruptures, the life of the baby and mother is in danger.
C-sections also increase the risk of problems in future pregnancies. Women who have had c-sections have a higher risk of uterine rupture. If the uterus ruptures, the life of the baby and mother is in danger.
Supporters of elective c-sections say that this surgery may protect a woman's pelvic organs, reduces the risk of bowel and bladder problems, and is as safe for the baby as vaginal delivery.
The National Institutes of Health (NIH) and American College of Obstetricians (ACOG) agree that a doctor's decision to perform a c-section at the request of a patient should be made on a case-by-case basis and be consistent with ethical principles. ACOG states that "if the physician believes that (cesarean) delivery promotes the overall health and welfare of the woman and her fetus more than vaginal birth, he or she is ethically justified in performing" a c-section. Both organizations also say that c-section should never be scheduled before a pregnancy is 39 weeks, or the lungs are mature, unless there is medical need.
The c-section experience
Most c-sections are unplanned. So, learning about c-sections is important for all women who are pregnant. Whether a c-section is planned or comes up during labor, it can be a positive birth experience for many women. The overview that follows will help you to know what to expect during a nonemergency c-section and what questions to ask.
Before surgery
Cesarean delivery takes about 45 to 60 minutes. It takes place in an operating room. So if you were in a labor and delivery room, you will be moved to an operating room. Often, the mood of the operating room is unhurried and relaxed. A doctor will give you medicine through an epidural or spinal block, which will block the feeling of pain in part of your body but allow you to stay awake and alert. The spinal block works right away and completely numbs your body from the chest down. The epidural takes away pain, but you might be aware of some tugging or pushing. See Medical methods of pain relief for more information. Medicine that makes you fall asleep and lose all awareness is usually only used in emergency situations. Your abdomen will be cleaned and prepped. You will have an IV for fluids and medicines. A nurse will insert a catheter to drain urine from your bladder. This is to protect the bladder from harm during surgery. Your heart rate, blood pressure, and breathing also will be monitored. Questions to ask:
Medicine that makes you fall asleep and lose all awareness is usually only used in emergency situations. Your abdomen will be cleaned and prepped. You will have an IV for fluids and medicines. A nurse will insert a catheter to drain urine from your bladder. This is to protect the bladder from harm during surgery. Your heart rate, blood pressure, and breathing also will be monitored. Questions to ask:
- Can I have a support person with me during the operation?
- What are my options for blocking pain?
- Can I have music played during the surgery?
- Will I be able to watch the surgery if I want?
During surgery
The doctor will make two incisions. The first is about 6 inches long and goes through the skin, fat, and muscle. Most incisions are made side to side and low on the abdomen, called a bikini incision. Next, the doctor will make an incision to open the uterus. The opening is made just wide enough for the baby to fit through. One doctor will use a hand to support the baby while another doctor pushes the uterus to help push that baby out. Fluid will be suctioned out of your baby's mouth and nose. The doctor will hold up your baby for you to see. Once your baby is delivered, the umbilical cord is cut, and the placenta is removed. Then, the doctor cleans and stitches up the uterus and abdomen. The repair takes up most of the surgery time. Questions to ask:
One doctor will use a hand to support the baby while another doctor pushes the uterus to help push that baby out. Fluid will be suctioned out of your baby's mouth and nose. The doctor will hold up your baby for you to see. Once your baby is delivered, the umbilical cord is cut, and the placenta is removed. Then, the doctor cleans and stitches up the uterus and abdomen. The repair takes up most of the surgery time. Questions to ask:
- Can my partner cut the umbilical cord?
- What happens to my baby right after delivery?
- Can I hold and touch my baby during the surgery repair?
- When is it okay for me to try to breastfeed?
- When can my partner take pictures or video?
After surgery
You will be moved to a recovery room and monitored for a few hours. You might feel shaky, nauseated, and very sleepy. Later, you will be brought to a hospital room. When you and your baby are ready, you can hold, snuggle, and nurse your baby. Many people will be excited to see you. But don't accept too many visitors. Use your time in the hospital, usually about four days, to rest and bond with your baby. C-section is major surgery, and recovery takes about six weeks (not counting the fatigue of new motherhood). In the weeks ahead, you will need to focus on healing, getting as much rest as possible, and bonding with your baby — nothing else. Be careful about taking on too much and accept help as needed. Questions to ask:
Many people will be excited to see you. But don't accept too many visitors. Use your time in the hospital, usually about four days, to rest and bond with your baby. C-section is major surgery, and recovery takes about six weeks (not counting the fatigue of new motherhood). In the weeks ahead, you will need to focus on healing, getting as much rest as possible, and bonding with your baby — nothing else. Be careful about taking on too much and accept help as needed. Questions to ask:
- Can my baby be brought to me in the recovery room?
- What are the best positions for me to breastfeed?
Vaginal birth after c-section (VBAC)?
Some women who have delivered previous babies by c-section would like to have their next baby vaginally. This is called vaginal delivery after c-section or VBAC. Women give many reasons for wanting a VBAC. Some want to avoid the risks and long recovery of surgery. Others want to experience vaginal delivery.
Today, VBAC is a reasonable and safe choice for most women with prior cesarean delivery, including some women who have had more than one cesarean delivery. Moreover, emerging evidence suggests that multiple c-sections can cause serious harm. If you are interested in trying VBAC, ask your doctor if you are a good candidate. A key factor in this decision is the type of incision made to your uterus with previous c-sections.
Moreover, emerging evidence suggests that multiple c-sections can cause serious harm. If you are interested in trying VBAC, ask your doctor if you are a good candidate. A key factor in this decision is the type of incision made to your uterus with previous c-sections.
Your doctor can explain the risks of both repeat cesarean delivery and VBAC. With VBAC, the most serious danger is the chance that the c-section scar on the uterus will open up during labor and delivery. This is called uterine rupture. Although very rare, uterine rupture is very dangerous for the mother and baby. Less than 1 percent of VBACs lead to uterine rupture. But doctors cannot predict if uterine rupture is likely to occur in a woman. This risk, albeit very small, is unacceptable to some women.
The percent of VBACs is dropping in the United States for many reasons. Some doctors, hospitals, and patients have concerns about the safety of VBAC. Some hospitals and doctors are unwilling to do VBACs because of fear of lawsuits and insurance or staffing expenses.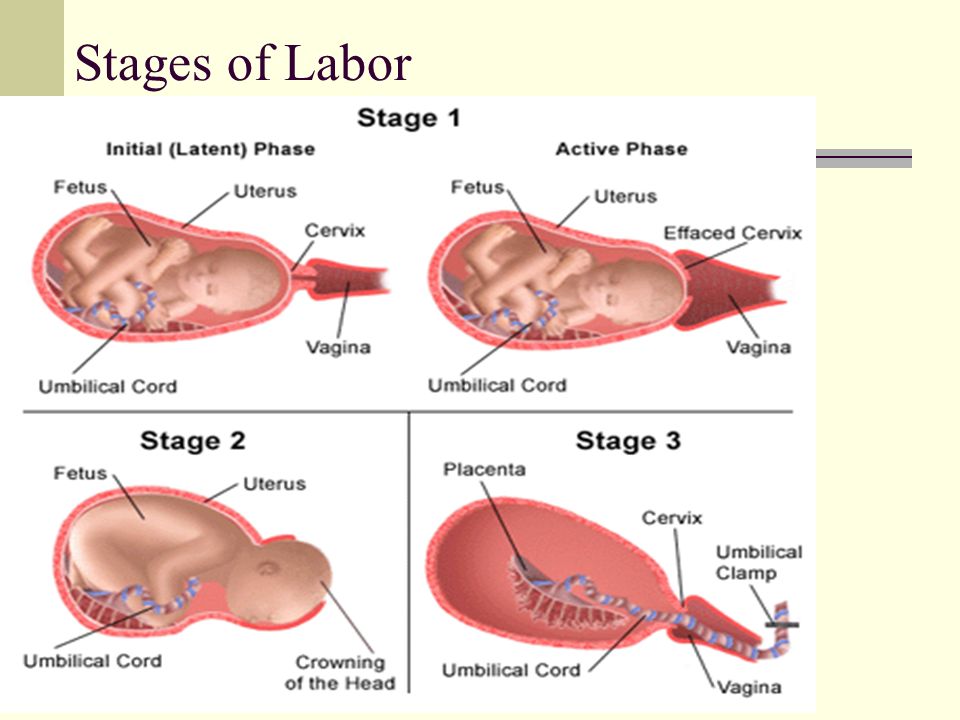 Many doctors, however, question if this trend is in the best interest of women's health.
Many doctors, however, question if this trend is in the best interest of women's health.
Choosing to try a VBAC is complex. If you are interested in a VBAC, talk to your doctor and read up on the subject. Only you and your doctor can decide what is best for you. VBACs and planned c-sections both have their benefits and risks. Learn the pros and cons and be aware of possible problems before you make your choice.
Childbirth | Stages of Labor | Effacement
On this page
Basics
- Summary
- Start Here
- Diagnosis and Tests
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
See, Play and Learn
- Images
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
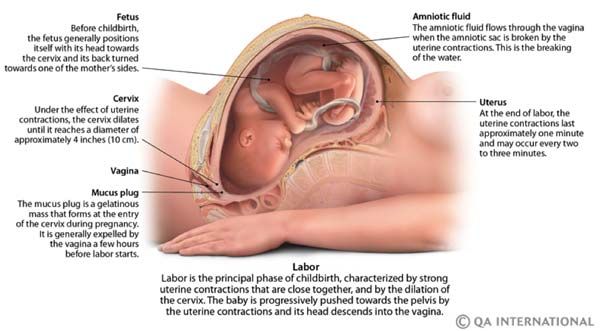
When you are ready to have your baby, you'll go through labor. Labor is the process of giving birth. Signs that you might be going into labor include:
Labor is the process of giving birth. Signs that you might be going into labor include:
- Contractions that are regular then start to come closer together
- Leaking fluid or bleeding from the vagina
- Low, dull backache
- Abdominal cramps
Call your health care provider if you have any of these signs, even if it is before your due date. Preterm labor can start before 37 completed weeks of pregnancy.
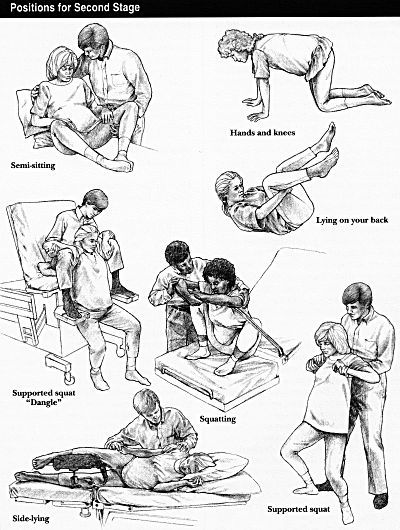
Labor happens in three stages. The first stage begins with contractions. It continues until your cervix has become thinner and dilated (stretched) to about 4 inches wide. The second stage is the active stage, in which you begin to push downward. Crowning is when your baby's scalp comes into view. Shortly afterward, your baby is born. In the third stage, you deliver the placenta. The placenta is the organ that supplied food and oxygen to your baby during pregnancy.
Mothers and babies are monitored closely during labor. Most women are able to have a baby through normal vaginal delivery. If there are complications, the baby may need to be delivered surgically by a Cesarean section.
If there are complications, the baby may need to be delivered surgically by a Cesarean section.
NIH: National Institute of Child Health and Human Development
- Labor and Birth (Department of Health and Human Services, Office on Women's Health) Also in Spanish
- Stages of Labor (March of Dimes Birth Defects Foundation) Also in Spanish
- What Is Labor? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Contractions and Signs of Labor (March of Dimes Birth Defects Foundation)
- Cord Blood Testing and Banking (National Library of Medicine) Also in Spanish
- Monitoring Baby's Heart Rate during Labor (American Academy of Family Physicians) Also in Spanish
- Water Breaking: Understand This Sign of Labor (Mayo Foundation for Medical Education and Research) Also in Spanish
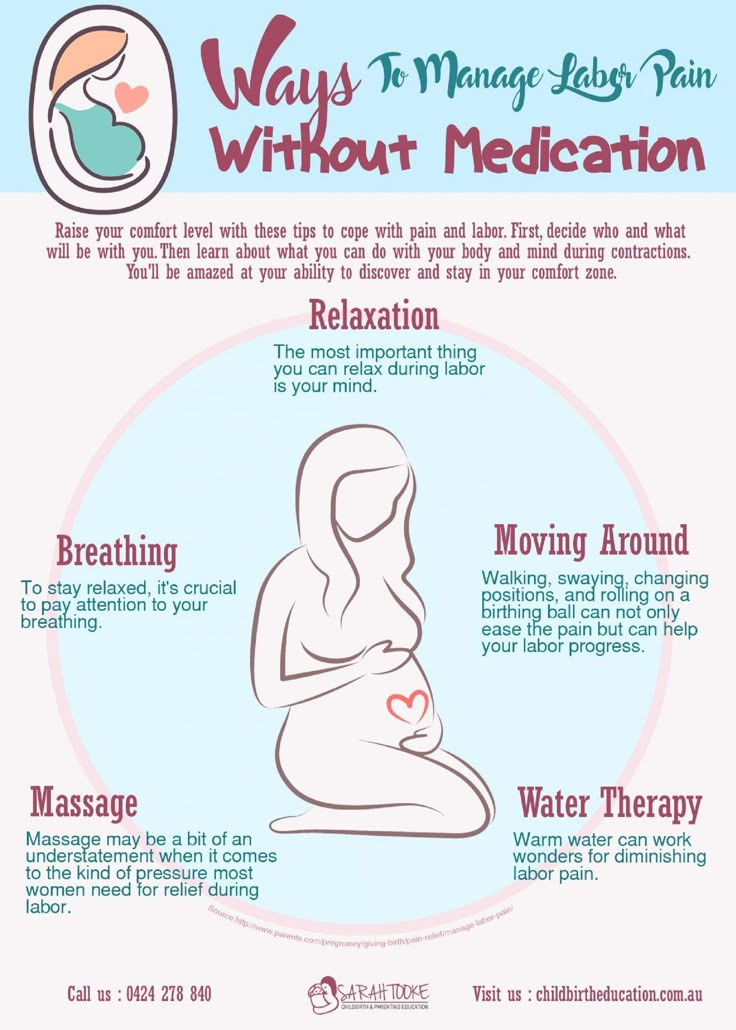
- Dealing with Pain during Childbirth (Nemours Foundation) Also in Spanish
- Apgar Scores (American Academy of Pediatrics) Also in Spanish
- Birthing Centers and Hospital Maternity Services (Nemours Foundation) Also in Spanish
- Birthing Classes (American Academy of Family Physicians) Also in Spanish
- Elective Deliveries Before 39 Weeks: Is It Worth It? (American Academy of Pediatrics)
- Why at Least 39 Weeks Is Best for Your Baby (March of Dimes Birth Defects Foundation)
- Assisted Vaginal Delivery (American College of Obstetricians and Gynecologists)
- Cesarean Section: MedlinePlus Health Topic (National Library of Medicine) Also in Spanish
- Episiotomy: When It's Needed, When It's Not (Mayo Foundation for Medical Education and Research) Also in Spanish
- Induction of Labor at 39 Weeks (American College of Obstetricians and Gynecologists)
- Labor Pain (American Society of Anesthesiologists)
- Natural Childbirth (Nemours Foundation) Also in Spanish
- FastStats: Births -- Method of Delivery (National Center for Health Statistics)
- PeriStats: Perinatal Statistics (March of Dimes Birth Defects Foundation)
- ClinicalTrials.
 gov: Delivery, Obstetric (National Institutes of Health)
gov: Delivery, Obstetric (National Institutes of Health) - ClinicalTrials.gov: Labor, Obstetric (National Institutes of Health)
- Article: A comparison of the effect of Swedish massage with and without.
 ..
.. - Article: Effect of implementing a birth plan on maternal and neonatal outcomes:...
- Article: Micturition in the toilet compared with bedpan in laboring Nulliparas: a.
 ..
.. - Childbirth -- see more articles
- Department of Health and Human Services, Office on Women's Health Also in Spanish
- Find an Ob-Gyn (American College of Obstetricians and Gynecologists)
Childbirth after 30 - articles from the specialists of the clinic "Mother and Child"
Broitman Evgeniya Viktorovna
Reproductologist
Clinical Hospital "AVICENNA" GC "Mother and Child"
According to psychologists, the birth of a child at a more mature age is more favorable than in youth.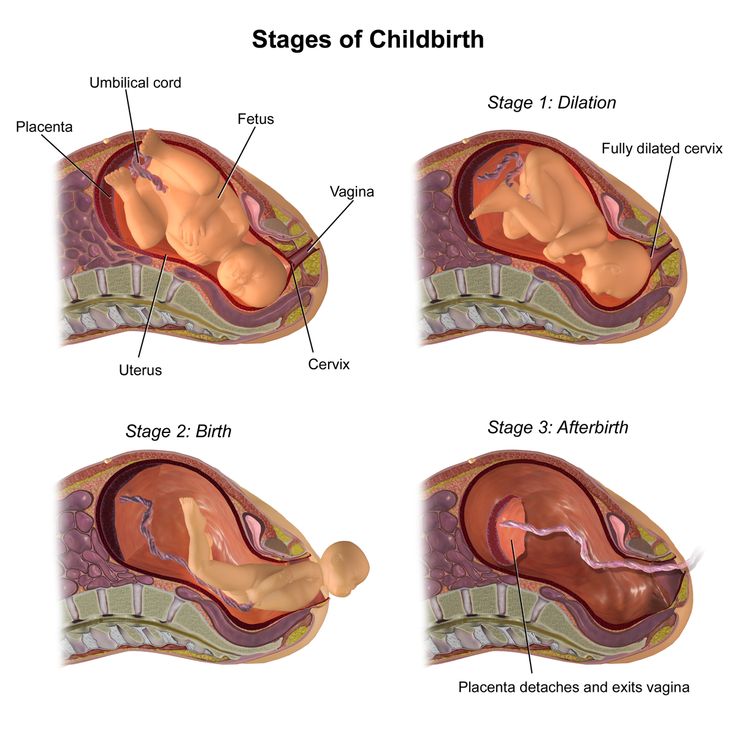 As a rule, in a couple where parents are over 30, they prepare in advance for the appearance of the first child, and the child is born desired.
As a rule, in a couple where parents are over 30, they prepare in advance for the appearance of the first child, and the child is born desired.
In addition, it is by the age of 30 that life experience, wisdom, and psychological maturity appear. All these qualities allow you to calmly relate to your condition, make informed decisions. Psychological comfort for the baby in such a family is provided.
The medical aspects of late pregnancy and childbirth have also improved in recent years.
Previously, there was an opinion that with increasing age, the number of possible complications of both pregnancy and childbirth increases in direct proportion.
However, in recent years this point of view has been refuted by most of the studies. The frequency of occurrence of such pathology of pregnancy as fetoplacental insufficiency (and as a result, intrauterine hypoxia and fetal growth retardation), as well as nephropathy of pregnant women occurs among women over 30 years of age with the same frequency as among younger pregnant women. Moreover, patients after 30 years of age, as a rule, are more disciplined and responsible, better follow the doctor's recommendations. This contributes to the prevention and timely treatment of emerging complications of pregnancy.
Moreover, patients after 30 years of age, as a rule, are more disciplined and responsible, better follow the doctor's recommendations. This contributes to the prevention and timely treatment of emerging complications of pregnancy.
It is widely known that the incidence of diseases of internal organs, such as arterial hypertension, diabetes mellitus, obesity, metabolic syndrome, unfortunately increases after 30 years. However, the level of development of modern medicine allows timely diagnosis and treatment of such conditions at the stage of preparation for pregnancy and during it.
A necessary condition in such a situation is careful monitoring of the course of pregnancy, the state of internal organs. If necessary, the doctor prescribes treatment (both drug and non-drug), which does not adversely affect the baby's condition, and at the same time contributes to the normalization of the functions of the expectant mother's organs.
Women aged 35 years and older have a significantly increased risk of having children with a genetic disorder (eg Down syndrome, Edwards syndrome, Patau syndrome, etc.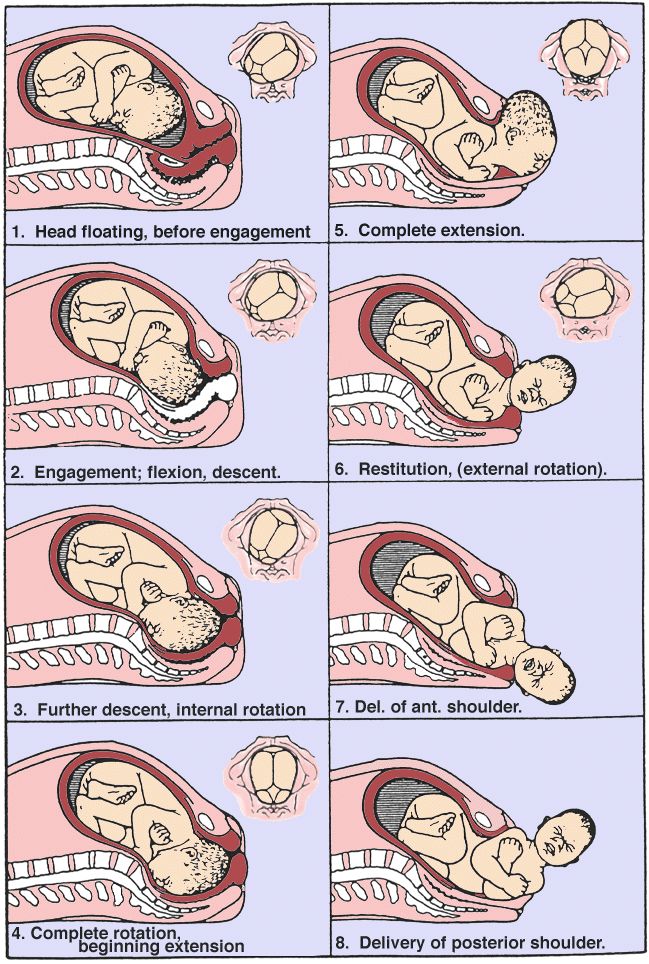 ). However, at the present stage of development of medical genetics, most of these diseases can be diagnosed even in the early stages of pregnancy.
). However, at the present stage of development of medical genetics, most of these diseases can be diagnosed even in the early stages of pregnancy.
Already at 11-12 weeks of pregnancy, ultrasound examination can reveal some malformations and reveal changes that may indicate the presence of a chromosomal pathology of the fetus.
So, the presence of a thickening of the collar zone in the fetus at 11 - 12 weeks of pregnancy in most cases reveals Down's syndrome. The second ultrasound examination is performed at 20-22 weeks of pregnancy. During these periods, it is possible to determine the anatomy of all organs of the fetus, to identify deviations in development.
Biochemical markers of chromosomal pathology are another important method for diagnosing genetic diseases. They are determined in the blood of the expectant mother at 11-12 weeks and at 16-20 weeks of pregnancy.
In the 1st trimester, the concentration in the blood of a protein associated with pregnancy and human chorionic gonadotropin is monitored, in the second trimester - a combination of alphafetoprotein and human chorionic gonadotropin.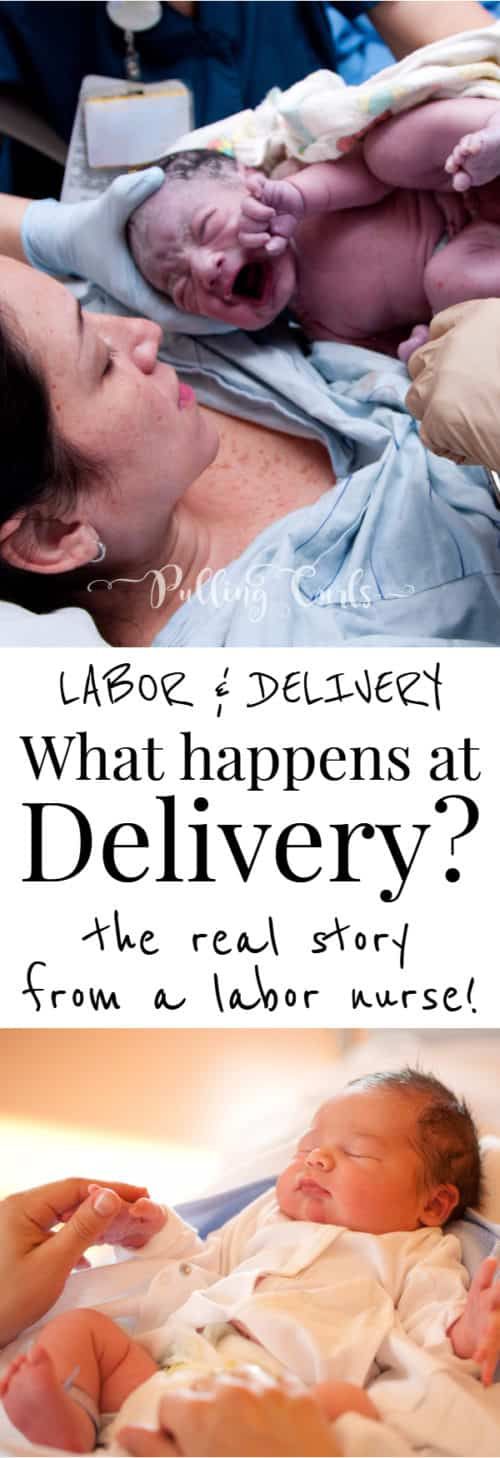 To make sure that the suspicions are correct, so-called invasive diagnostic methods are used.
To make sure that the suspicions are correct, so-called invasive diagnostic methods are used.
This is a chorion biopsy (obtaining cells from the future placenta), which is performed at 8-12 weeks of pregnancy, amniocentesis (aspiration of amniotic fluid at 16-24 weeks), cordocentesis - puncture of the umbilical cord of the fetus (performed at 22-25 weeks of pregnancy).
These methods allow you to accurately determine the chromosome set of the unborn child and speak with confidence about the presence or absence of genetic diseases in him. All studies are carried out under ultrasound control, which allows you to minimize the degree of complications.
It was previously believed that the first birth after the age of 30 years is an indication for caesarean section. Now this position is hopelessly outdated. Most women of mature age give birth on their own. Of course, it should be remembered that in patients of this age category, such complications of childbirth as the development of weakness in labor, acute fetal hypoxia are somewhat more common than in the general population.
In such situations, the doctor in charge of the birth may decide to have an emergency operation. But almost all women who give birth to their first child after 30 years have a chance to give birth on their own.
For a successful course of pregnancy and childbirth, it is more important than for young mothers to monitor their health, carefully follow all the doctor's recommendations. It is also desirable that pregnancy and childbirth be conducted by one doctor who knows in detail all the features of the course of pregnancy and can foresee possible complications of childbirth and prevent them in a timely manner.
Make an appointment
to the doctor - Broitman Evgenia Viktorovna
Clinical Hospital "AVICENNA" Group of Companies "Mother and Child"
Analysis of the binding of spermatozoa with hyaluronic acid (HBA-test)Spermogram analysis and other ejaculate studies and surrogate motherhoodEgg donationFemale infertilityICSIMSIFor out-of-town patientsFor out-of-town patientsArtificial (intrauterine) inseminationHow to become a sperm donor? How to become an egg donor? When is IVF contraindicated? to the IVF program at the expense of compulsory medical insuranceList of examinations before IIList of examinations before IVFIndications for PGDPreimplantation genetic diagnosisPreservation of fertilityOvulation stimulationSurrogacySurgical treatment of infertilityCenter for innovative reproductive technologies0003
By clicking on the send button, I consent to the processing of personal data
Late children bring back youth - articles from specialists of the clinic "Mother and Child"
The number of women who gave birth to their first child between 30 and 40 years has almost tripled in the last 20 years. In addition, the number of first-time mothers after 40 years has increased by almost 50%. And physicians are forced to reckon with it. Gradually, the offensive word “old-timer” disappeared from their vocabulary, and childbirth in adulthood is no longer considered something out of the ordinary.
In addition, the number of first-time mothers after 40 years has increased by almost 50%. And physicians are forced to reckon with it. Gradually, the offensive word “old-timer” disappeared from their vocabulary, and childbirth in adulthood is no longer considered something out of the ordinary.
Increasingly, women are postponing childbirth while studying or moving up the career ladder. The number of early births (up to 20 years old) in all civilized countries is steadily falling (Russia, however, is an exception).
Numerous studies have shown that pregnancy and childbirth after 35 do not pose such a serious danger as previously thought. The average portrait of a woman in her thirties who is preparing to become a mother has changed a lot lately. As a rule, she belongs to the middle class, is well educated, takes care of her health. Her body is not worn out by numerous births.
It has always been believed that later children are more likely to be born prematurely, gain less weight and get sick more in early childhood. Recent research has cast doubt on this.
Recent research has cast doubt on this.
American doctors who observed 4 thousand women in labor in one of the hospitals in New York came to the conclusion that a woman over 35 years old, if she is physically healthy and has not had miscarriages, has a chance to give birth to a normal healthy child (even if this is the first birth) almost the same as a 20-year-old.
For a middle-aged woman who has devoted all her young years to a career, pregnancy is an opportunity to try herself in a completely new way. In addition, she is more likely to find support from her husband, since a mature man is psychologically more prepared for the role of a father than a young one.
As you know, psychological readiness for motherhood comes much later than biological. According to psychologists, pregnancy in adulthood is much more favorable than in early youth. A woman perceives her condition more calmly, less prone to stress, less likely to experience internal conflicts.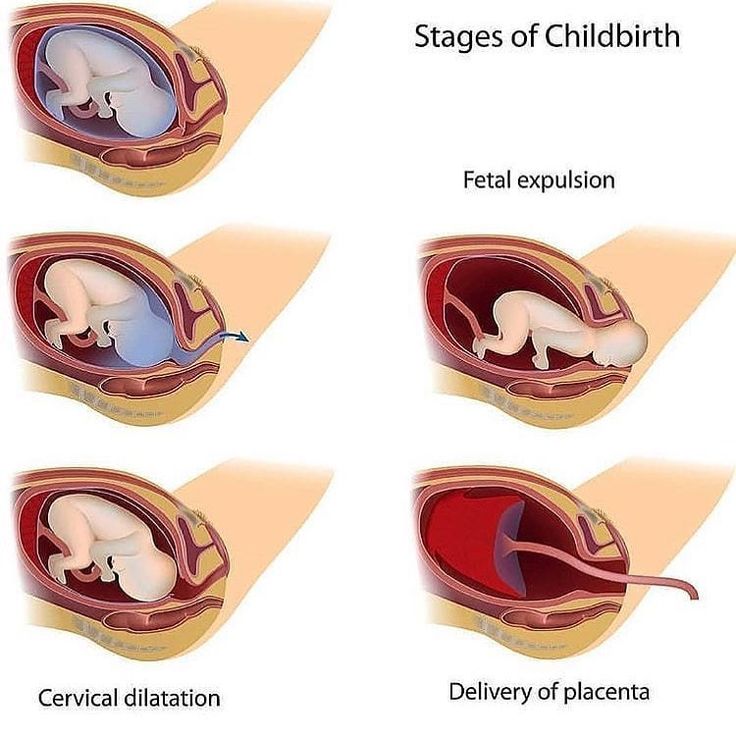 She is more disciplined and lives in harmony with herself. Many consider the birth of a child a gift of fate or a blessing from God.
She is more disciplined and lives in harmony with herself. Many consider the birth of a child a gift of fate or a blessing from God.
Older women, most of whom married late, as a rule, stand firmly on their feet, have reached a certain level in their professional activities, and are confident that they will return to work some time after giving birth. All this allows them to look to the future with great calmness and optimism. A middle-aged woman who has devoted all her young years to a career may look at pregnancy as an opportunity to try herself in a completely new capacity. In addition, she is more likely to find support from her husband, since a mature man is psychologically more prepared for the role of a father than a young one. As a rule, middle-aged parents, unlike young ones, devote more time to raising a child. As a result, many "late" children are ahead of their peers in their intellectual and physical development. The secret here is in the atmosphere of love and mutual understanding in the family where the long-awaited baby appeared.
American psychologists conducted a survey among women who became mothers before the age of 20 and between 30 and 40 years. Both were asked to answer the question of whether they would give birth at the same age if they could make a new decision. More than half of those whose children were born before the age of 20 answered “no”, and the majority of older mothers expressed confidence that they had chosen the optimal time for the birth of a child.
Hollywood star Kim Basinger first became a mother when she was already over 40. Actress Beverly D * Angelo, a friend of Al Pacino, gave birth to his charming twins when she was 49. The famous actress Marina Neelova had a daughter when she was 41 years old. And there are many such examples.
Doctors today can help even those women whose reproductive period has ended. Various methods are used for this: hormone therapy, implantation of a donor egg in the uterus. Muscovite Natalya Alekseevna Surkova got into the Guinness Book of Records, becoming a mother at the age of 57. She already had two adult children. Recently, a 66-year-old woman from Romania gave birth to a child. For many years she taught at the University and wrote books for children, but she had no babies of her own before. True, doctors are not particularly enthusiastic about the increase in the number of mothers-grandmothers: the risk of complications and the responsibility of the doctor who “leads” such a woman in labor are too high.
She already had two adult children. Recently, a 66-year-old woman from Romania gave birth to a child. For many years she taught at the University and wrote books for children, but she had no babies of her own before. True, doctors are not particularly enthusiastic about the increase in the number of mothers-grandmothers: the risk of complications and the responsibility of the doctor who “leads” such a woman in labor are too high.
Of course, late motherhood has its problems. Women over 35 are more likely to experience health complications during pregnancy, especially diabetes and high blood pressure. These complications occur in approximately 6% of women over 35 years of age compared to 1.3% in younger women.
Another problem: the "solid" age of the parents increases the risk of developing anomalies in the fetus, the birth of children with severe hereditary diseases. Therefore, all primiparas over 35 years of age are usually offered an amniocentesis in the second trimester of pregnancy - an analysis of amniotic fluid. This allows you to identify about 200 hereditary diseases associated with a violation of the chromosome set.
You can also find out the degree of risk of such diseases using the "triple" test - it is done around the 16th week of pregnancy. For analysis, blood is taken from a vein. Women of older reproductive age do not recover from childbirth as quickly as younger women. For some of them, after decades of taking care of themselves, it can be difficult to get used to the fact that the baby, especially in the first months, requires constant care and attention.
Another disadvantage of late childbirth is that parents have to limit themselves to one child or have a second one when the first one is still very small - after all, the time allotted by nature for acquiring offspring is not unlimited.
Should I do a Caesarean section?
In women over 30-40 years of age, childbirth can be more difficult and protracted than in younger women - this is the generally accepted opinion. In fact, any experienced obstetrician can testify that in many cases, older mothers do an excellent job with minimal medical help. Often and, by the way, not always justified, at this age they offer a caesarean section. This does not raise questions if there are medical indications for surgery or a woman managed to get pregnant only with the help of doctors. Then, trying to eliminate any risk to the baby and taking into account the aggravating factors, the doctor makes such a decision.
In fact, any experienced obstetrician can testify that in many cases, older mothers do an excellent job with minimal medical help. Often and, by the way, not always justified, at this age they offer a caesarean section. This does not raise questions if there are medical indications for surgery or a woman managed to get pregnant only with the help of doctors. Then, trying to eliminate any risk to the baby and taking into account the aggravating factors, the doctor makes such a decision.
Recent studies have shown that, on average, the duration of labor for older mothers exceeds the duration of labor for young mothers by only 45 minutes. And at 40, you can not be afraid of difficult childbirth if you are well prepared for them physically and psychologically.
Where to start?
If for some reason you put off the birth of your child, you should prepare in advance for his possible birth.
Try to get rid of bad habits if you have them. By the age of 35, we have time to experience a stronger impact of adverse environmental factors than by the age of 20.
Should we add to them the harm from smoking and alcohol? Watch your health, do not start even trifling, at first glance, diseases. If you treat a cold rather than endure it on your feet, you are much more likely to keep your kidneys and heart healthy, organs that take a lot of stress during pregnancy.
Control your weight and maintain muscle tone. Go in for sports or exercise. Excess weight creates additional problems during gestation.
It should be borne in mind that after 35 years, the ability to bear children gradually decreases. Experts believe that at this age it may take 6-12 months to conceive instead of four. Before you decide it's time to start procreation, visit a therapist. Sometimes a woman is being treated for infertility for years, during which time she develops various ailments. These diseases may not cause much concern, but they can interfere with the normal course of pregnancy.
During pregnancy, you will need to be more attentive to yourself than younger women, to strictly monitor your diet and regimen.
It is worth taking seriously the choice of a doctor and a maternity hospital. It is desirable that the clinic be equipped with everything necessary in case you need urgent help for a newborn.
"If you want to preserve beauty, have a child at forty," say the French. If a woman is healthy, during pregnancy she blossoms. In this magical way, estrogens act - female sex hormones, the production of which increases several times. In addition, the eggs of a pregnant woman are not "spent", so aging seems to be suspended. Menopause in women who have become mothers in adulthood may come later. Raising a baby provides a unique opportunity to turn from a middle-aged woman into a young mother.
Such parents usually go through the so-called midlife crisis painlessly - they just don't have time to delve into their problems. Not soon they will have another test, which psychologists call the "empty nest" syndrome - when children grow up and leave their father's house.