Full term pregnant with twins
Twin Pregnancy: Answers from an Expert
Twin Pregnancy: Answers from an Expert | Johns Hopkins MedicineReviewed By:
When you’re expecting twins, you know you’ll need two of everything for your registry. But what about staying healthy during your pregnancy? Do you need to double your food intake, weight gain and visits to the doctor? With regard to the babies, are there two placentas and two amniotic sacs, or can they share these?
Johns Hopkins maternal-fetal medicine specialist Jeanne Sheffield answers eight commonly asked questions.
Do twins share a placenta and an amniotic sac?
While some twins may share a placenta and an amniotic sac, that is not the case for the vast majority of pregnancies. Here are three major possibilities that exist:
- Two placentas and two amniotic sacs.
A twin pregnancy with two placentas and two amniotic sacs is the optimal twin pregnancy, as each baby has its own nutritional source and protective membrane.
- One placenta and two amniotic sacs. In pregnancies with one placenta and two amniotic sacs, you will definitely have identical twins. Additionally, when your babies share a placenta, there is a greater risk for complications, such as twin-to-twin transfusion syndrome. Your physician will closely monitor your pregnancy to check for potential problems.
- One placenta and one amniotic sac. This is the riskiest and rarest type of twin pregnancy. Fetal complications can arise due to tangling of the umbilical cords or an imbalance in nutrients, blood or other vital life supporting systems.
- Two placentas and two amniotic sacs.
Do I need to double my caloric intake during a twin pregnancy?
A common misconception surrounding twin pregnancy is that you need to double your caloric intake to provide your babies with enough nutrients.
 However, pregnancy nutrition guidelines aren’t simply based on the number of babies you’re carrying. Instead, they’re based on your body mass index at the time you became pregnant.
However, pregnancy nutrition guidelines aren’t simply based on the number of babies you’re carrying. Instead, they’re based on your body mass index at the time you became pregnant. Your doctor will make individualized recommendations based on your starting weight. On average, it’s estimated that a woman’s caloric requirements will increase about 40 percent for a twin pregnancy. What’s most important, though, is that a woman eats as healthy as possible.
Do I need to take different prenatal vitamins for twins?
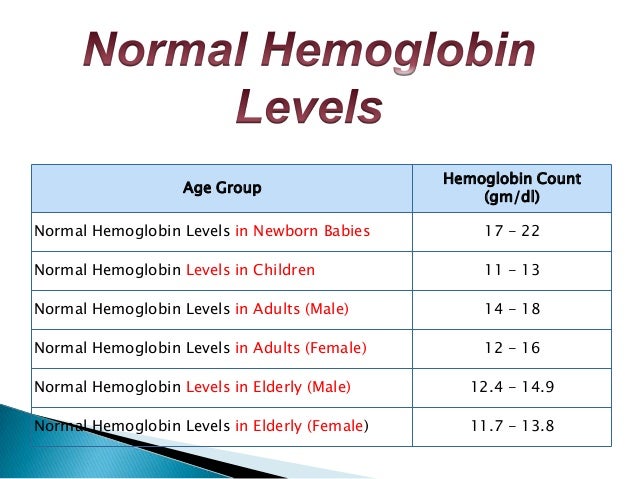
If you’re pregnant with twins, you should take the same prenatal vitamins you would take for any pregnancy, but your physician will recommend extra folic acid and iron. The additional folic acid and extra iron will help ward off iron-deficiency anemia, which is more common when you’re pregnant with multiples.
Will I need to visit my doctor more frequently?
While every pregnancy is different, most women carrying twins will have more frequent prenatal visits than women carrying only one baby.
 If your twins are sharing one placenta, you will automatically have a more frequent monitoring schedule.
If your twins are sharing one placenta, you will automatically have a more frequent monitoring schedule. If your pregnancy doesn’t have complications, your prenatal visits may not differ much from a singleton pregnancy until you get to the end of your second trimester. At that point, you’ll be seen more frequently because there is a higher risk of pre-eclampsia and preterm labor.
Do I have to see a maternal-fetal medicine specialist for a twin pregnancy?
Maternal-fetal medicine specialists see high-risk pregnancies, but not every twin pregnancy will fall into this category.
To find the best care provider for your twins, make sure that the physician is comfortable managing twins, including vaginal delivery of twins rather than only offering a cesarean section (C-section) for delivery.
Are all twin pregnancies delivered preterm?
A little more than half of twin pregnancies end in preterm delivery (before 37 weeks).
 While 40 weeks is the full gestation period of the average pregnancy, most twin pregnancies are delivered at approximately 36 weeks (range 32-38 weeks depending on the type of twin pregnancy).
While 40 weeks is the full gestation period of the average pregnancy, most twin pregnancies are delivered at approximately 36 weeks (range 32-38 weeks depending on the type of twin pregnancy). Unfortunately, preventing preterm labor with multiples is more challenging than with a singleton pregnancy because the interventions used with singleton pregnancies are not as effective with multiples.
Can bed rest reduce the risk of preterm delivery?
Scientific data show that bed rest does not prevent preterm delivery. In fact, bed rest can increase your risk of developing blood clots and have negative financial and social consequences.
Although bed rest is not prescribed as frequently as it once was, your doctor may suggest reducing your activity level if you’re showing signs of early labor at the end of your second trimester or early in your third trimester.
Is labor and delivery significantly different with twins?
Labor is generally the same whether you’re having one baby or two.
 During delivery is when things differ significantly.
During delivery is when things differ significantly. When it’s time to deliver your twins, you will go to an operating room even if you are delivering vaginally. This is a safety precaution known as a double setup. Following the vaginal delivery of the first baby, there is a small risk of an emergency cesarean section for the second baby. There is also the possibility of the second twin being delivered breech, which is a safe form of vaginal delivery if the obstetrician is experienced in this type of delivery.
Of women giving birth to twins over 32 weeks, only about 4 percent who try for a vaginal delivery will have a combined vaginal and cesarean section delivery. While it doesn’t happen very often, by delivering both babies in the operating room, physicians are better prepared to protect the health of the mother and the babies.
Although being pregnant with twins can seem very different, your doctor will treat your pregnancy like any other unless a complication occurs.

Sign Up for Our Free Newsletter
One of the best things you can do to protect and improve your health is to stay informed. Your Health is a FREE e-newsletter that serves as your smart, simple connection to the world-class expertise of Johns Hopkins.
Sign Up
Related
-
Planning a Pregnancy
How to Prepare for Pregnancy
-
Fertility, Pregnancy and Childbirth
Complications of Pregnancy
-
Planning a Pregnancy
Ovarian Tissue Freezing Cryopreservation
Related Topics
What is Full Term for Twins? » TwinStuff
For mothers who are about to give birth to twins, the last trimester is imminently the time to be extra cautious. Because this last stretch can be a bit more stressful, knowing precisely when the full term for twins is will significantly bring a sense of comfort especially when mothers are especially particular about preterm labor and essential preparations.
Because this last stretch can be a bit more stressful, knowing precisely when the full term for twins is will significantly bring a sense of comfort especially when mothers are especially particular about preterm labor and essential preparations.
This article will give helpful insight as to knowing just when your twins are ready to pop out of the oven as well as the essentials to pre and post-natal care.
How Many Weeks is a Full Term Pregnancy for Twins?
Pregnancy Day By Day editor-in-chief Maggie Blott, M.B.,B.S., reports that there are about 1 in 31 twin births in the United since the 80’s. Among those births, more than half of the twins delivered were born at about 37 weeks, which is considered normal and healthy when giving birth to multiples.
Baby Center UK says, the average timeline for twin pregnancies is about 36.4 weeks and doctors consider 37 weeks as the full term pregnancy for twins. Babies born within this time (32 to 37 weeks) have no complications and actually do well.
Preparing for the Arrival of Your Twins
Since multiples are born earlier compared to singletons, it is important to already have a hospital bag packed as early as the 26th week of pregnancy. During the wait time, the Twins and Multiple Births Association (TAMBA) advises thinking about how you would want to feed your babies.
It is important to inquire and attend antenatal classes specifically for twin pregnancies. These classes include sessions on how to breastfeed more than one child. Being able to know the merits of bottle feeding, breastfeeding, or the mixed approach is also very helpful.
How to Take Care of Yourself and Your Twins
When pregnant with twins or multiples, there are a lot of changes that go through until you reach full term. One of which is that weight gain is rapid as early as the first trimester.
The vomiting and nausea can be pretty intense, as well as the pain of breast tenderness. Such physical changes call for extra TLC, so it is important to always have someone with you at home during these times.
Another important thing to note according to The Office on Women’s Health is to visit your doctor. With twins, visits to the doctor will happen more often than those moms who are pregnant with singletons.
Mothers who carry twins have a higher risk of low birth weight, preterm birth, gestational diabetes, preeclampsia and cesarean birth. To avoid complications, frequent prenatal visits are a must. Doing so, allows your doctor to monitor the health of your twins, including your own.
Close monitoring will give you the best chance of having your babies being born full term and at a healthy weight. Plus, you will be able to know the vitamins you need and what activities are unsafe during the pregnancy. In short, your doctor is your best friend at this critical time.
Taking care of yourself as a mom is important to have happy and healthy twins
What if I Give Birth Early? What Should I Know About Pre-Term Labor?
It is important to know the signs of preterm labor in order to avoid complications and be able to get help on time. Since preterm labor is “silent,” being aware of your body is key. The first thing to be keen with is contractions. If you experience these symptoms, be sure to contact your doctor as soon as possible:
Since preterm labor is “silent,” being aware of your body is key. The first thing to be keen with is contractions. If you experience these symptoms, be sure to contact your doctor as soon as possible:
- Having four or five contractions in an hour
- Pressure in the pelvic area that is persistently rhythmic
- An aching back
- Experiencing cramps
There are also other signs of preterm labor like diarrhea and vaginal discharge or bleeding. Any discharge that looks streaked or bloody may mean that the cervix is about to dilate.
If you feel a gush of fluid or a leak from the vagina, this too can mean that the membranes have prematurely ruptured. This fluid is from the amniotic sac and when it breaks, the fluid gushes through the vagina. Finally, another symptom is that certain gut-feel that something is just not right. When things like these happen, go straight to your doctor.
After Giving Birth, What Now?
Although the pregnancy and delivery can be a cause of worry, it is essential to look forward to what happens next- your twins’ arrival! This is a joy for any mom but then, take note that care is still very much needed. Because your body is still recovering, you’d definitely need to do a number of changes at home.
Because your body is still recovering, you’d definitely need to do a number of changes at home.
To allow ample rest, limit the number of visitors at home. Be sure to have some extra hands to help with preparing meals and cleaning up the house. Eat healthily. Drink a lot of water and take in a lot of fiber to avoid constipation. Prevent swelling in your legs by putting your feet up and to avoid vaginal discomfort, sit in a warm bath. Whenever the need arises, apply nipple cream to sore breasts to soothe the pain.
Always be in check with your emotional health. If you feel sad, be sure to open up to your partner and family. If the sadness doesn’t seem to go away, be sure to call your doctor. Take all the rest you can whenever possible. Your babies always need you at your best.
There is nothing like the joy of giving birth and being a mom.
Even if this brings a number of physical and emotional changes, being ready with the essentials throughout the journey of pregnancy to giving birth is a must and will be a source of comfort early on.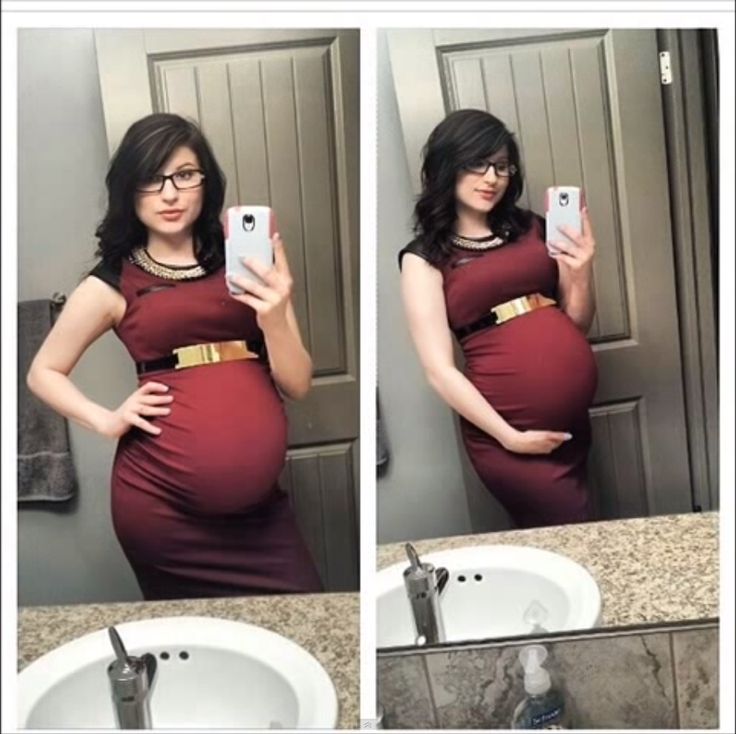 From knowing when the full term for twins is, doing necessary preparations, being emotionally ready, and of course realizing complications and risks, achieving a safe and healthy pregnancy is more than possible.
From knowing when the full term for twins is, doing necessary preparations, being emotionally ready, and of course realizing complications and risks, achieving a safe and healthy pregnancy is more than possible.
Multiple pregnancy
Author: Mikheeva Natalia Grigoryevna, Malyshok magazine
A multiple pregnancy is a pregnancy in which two or more fetuses develop simultaneously in the uterus. Multiple pregnancy occurs in 0.4 - 1.6% of all pregnancies. Recently, there has been an obvious trend towards an increase in the incidence of such pregnancies due to the active use of assisted reproduction technologies, including in vitro fertilization (IVF).
Types of multiple pregnancies
Children born in multiple pregnancies are called TWINS. There are two main types of twins: monozygotic (identical, homologous, identical, similar) and dizygotic (fraternal, heterologous, different). African countries have the highest twin birth rate, Europe and the USA have an average rate, and Asian countries have a low rate.
Dizygotic (fraternal) twins are more common (in 66-75% of all twins). The birth rate of dizygotic twins varies from 4 to 50 per 1000 births. Dizygotic twins occur when two separate eggs are fertilized. The maturation of two or more eggs can occur both in one ovary and in two. The predisposition to develop dizygotic twins may be maternally inherited. Dizygotic twins can be either same-sex or opposite-sex, they look like each other like ordinary brothers and sisters. With fraternal twins, two placentas are always formed, which can be very close, even touching, but they can always be separated. Two fruit spaces (i.e., fetal bladders or two “houses”) are separated from each other by a septum consisting of two chorionic and two amniotic membranes. Such twins are called dizygotic dichorionic diamniotic twins.
Monozygotic (identical) twins are formed as a result of the separation of one fetal egg at various stages of its development. The frequency of birth of monozygotic twins is 3-5 per 1000 births. The division of a fertilized egg into two equal parts can occur as a result of a delay in implantation (immersion of the embryo in the uterine mucosa) and oxygen deficiency, as well as due to a violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. The emergence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. If the separation of the fetal egg occurs in the first 3 days after fertilization, then monozygotic twins have two placentas and two amniotic cavities, and are called monozygotic diamniotic dichoriones (Fig. A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta.
The division of a fertilized egg into two equal parts can occur as a result of a delay in implantation (immersion of the embryo in the uterine mucosa) and oxygen deficiency, as well as due to a violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. The emergence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. If the separation of the fetal egg occurs in the first 3 days after fertilization, then monozygotic twins have two placentas and two amniotic cavities, and are called monozygotic diamniotic dichoriones (Fig. A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta. Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other.
Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other.
Twin births occur once in 87 births, triplets - once in 87 2 (6400) twins, quadruples - once in 87 3 (51200) triplets, etc. (according to the Gallin formula). The origin of triplets, quadruplets, and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be identical and fraternal.
Features of the course of multiple pregnancy
In case of multiple pregnancies, the woman's body is subject to increased requirements. All organs and systems function with great tension. In connection with the displacement of the diaphragm by the enlarged uterus, the activity of the heart becomes difficult, shortness of breath, fatigue occur. Enlargement of the uterus, especially towards the end of pregnancy, leads to compression of the internal organs, which is manifested by impaired bowel function, frequent urination, and heartburn. Almost 4-5 times more often there is the development of preeclampsia, which is characterized by an earlier onset, a protracted and more severe clinical course, often combined with acute pyelonephritis of pregnant women. Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination.
All organs and systems function with great tension. In connection with the displacement of the diaphragm by the enlarged uterus, the activity of the heart becomes difficult, shortness of breath, fatigue occur. Enlargement of the uterus, especially towards the end of pregnancy, leads to compression of the internal organs, which is manifested by impaired bowel function, frequent urination, and heartburn. Almost 4-5 times more often there is the development of preeclampsia, which is characterized by an earlier onset, a protracted and more severe clinical course, often combined with acute pyelonephritis of pregnant women. Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination. Preterm birth is observed in 25-50% of cases of such pregnancies.
Preterm birth is observed in 25-50% of cases of such pregnancies.
The development of term twins is normal in most cases. However, their body weight is usually less (by 10% or more) than in singleton pregnancies. With twins, the weight of children at birth less than 2500 g is observed in 40-60%. The low weight of twins is most often due to insufficiency of the uteroplacental system, which is not able to adequately provide several fetuses with nutrients, trace elements and oxygen. The consequence of this is a delay in the development of the fetus, which is a common occurrence in multiple pregnancies. The mass of twins, respectively, decreases in proportion to their number (triplets, quadruplets, etc.).
With monochorionic twins in the placenta, anastomoses are often formed between the vascular systems of the fetus, which can lead to a serious complication - the syndrome of feto-fetal transfusion. In this case, there is a redistribution of blood from one fetus to another, the so-called "stealing". The severity of feto-fetal transfusion (mild, moderate, severe) depends on the degree of redistribution of blood through the anastomoses, which vary in size, number and direction.
The severity of feto-fetal transfusion (mild, moderate, severe) depends on the degree of redistribution of blood through the anastomoses, which vary in size, number and direction.
Diagnosis in multiple pregnancy
The most reliable method for diagnosing multiple pregnancies is ultrasound, which allows not only early diagnosis of multiple pregnancies, but also to determine the position and presentation of fetuses, localization, structure and number of placentas, the number of amniotic cavities, the volume of amniotic fluid, congenital malformations and antenatal fetal death, the state of the fetus from a functional point of view, the nature of the uteroplacental and fetal-placental blood flow.
In multiple pregnancies, due to the higher risk of complications, ultrasound monitoring is performed more frequently than in singleton pregnancies. With dizygotic twins, about once every 3-4 weeks, with monozygotic twins - once every 2 weeks.
In addition, examinations and control of clinical tests are carried out with great care, and CTG is regularly recorded from 28 weeks of pregnancy.
Birth management
Indications for caesarean section associated with multiple pregnancies are triplets (quadruple), the transverse position of both or one of the fetuses, breech presentation of both fetuses or the first of them, and not associated with multiple pregnancy - fetal hypoxia, anomalies labor activity, prolapse of the umbilical cord, extragenital pathology of the mother, severe gestosis, placenta previa and abruption, etc.
-
ECO
In the department of assisted reproductive technologies of the Maternity Hospital No. 2
, IVF is performed at the expense of the Republican budget for couples
who have received a positive decision from the Minsk city or regional commissions to provide one free IVF attempt.
No drug supply problem. There is no waiting list. -
Farewoman
-
Individual care for patients
-
Ultrasound diagnostics
Curious facts are
0
, how many are the Geminis? up to 80 million pairs of twins.
The number of twins born in relation to the total number of newborns in different countries and on different continents is different, but in general the trend is such that it continues to grow. Compared with the 60s, the percentage of twins has increased from 1.18 to 2.78, that is, almost 2.5 times.
The largest number of children
The largest number of children born to one mother, according to official data, is 69. According to reports made in 1782, between 1725 and 1765. The wife of a Russian peasant Fyodor Vasiliev gave birth 27 times, giving birth to twins 16 times, triplets 7 times and 4 twins 4 times. Of these, only 2 children died in infancy.
The most prolific mother of our contemporaries is considered to be Leontina Albina (or Alvina) of San Antonio, Chile, who at 1943-81 years gave birth to 55 children. As a result of the first 5 pregnancies, she gave birth to triplets, and exclusively male.
Most birthed
The record 38 births are said to be Elizabeth Greenhillies Abbots-Langley, c. Hertfordshire, UK. She had 39 children - 32 daughters and 7 sons.
Hertfordshire, UK. She had 39 children - 32 daughters and 7 sons.
The largest number of multiple births in one family
Maddalena Pomegranate from Italy (b. 1839) had triplets born 15 times.
There is also information about the birth on May 29, 1971 in Philadelphia, Pennsylvania, USA, and in May 1977 in Bagarhat, Bangladesh, 11 twins. In both cases, no child survived.
Most fertile pregnancies
Dr. Gennaro Montanino, Rome, Italy, claimed to have removed, in July 1971, the embryos of 10 girls and 5 boys from the uterus of a 35-year-old woman who was 4 months pregnant. This unique case of 15-fertility was the result of infertility pills.
9 children - the largest number in one pregnancy - were born on June 13, 1971 by Geraldine Broadrick in Sydney, Australia. 5 boys and 4 girls were born: 2 boys were stillborn, and none of the rest survived more than 6 days.
The birth of 10 twins (2 boys and 8 girls) is known from reports from Spain (1924), China (1936) and Brazil (April 1946).
The father with many children
The largest father in the history of Russia is Yakov Kirillov, a peasant from the village of Vvedensky, who in 1755 was presented to the court in connection with this (he was then 60 years old). The first wife of a peasant gave birth to 57 children: 4 times four, 7 times three, 9once twice and 2 times once. The second wife gave birth to 15 children. Thus, Yakov Kirillov had 72 children from two wives.
Longest Birth Intervals for Multiple Pregnancies
Peggy Lynn of Huntington Pennsylvania, USA, gave birth to a girl, Hanna, on November 11, 1995, and the second of the twins, Erika, only 84 days later (February 2, 1996).
Siamese twins
United twins became known as "Siamese" after Chang and Eng Bunkers were born fused in the area of the sternum on May 11, 1811 in the Maeklong region of Siam (Thailand). They married Sarah and Adelaide Yates of pc. North Carolina, USA, and had 10 and 12 children, respectively. They died in 1874, and with a difference of 3 hours.
They died in 1874, and with a difference of 3 hours.
The science of twins - gemellology.
"Secret language"
Twins often talk to each other in a language that others do not understand. This phenomenon is called cryptophasia.
Left-handed twins
18-22% of left-handed twins (for non-twins this percentage is 10).
Parameters of physical development of fetuses and newborns during twin pregnancy
The problem of multiple pregnancy is relevant for modern obstetrics due to a significant increase in the frequency of multiple pregnancy in the last 20 years. To a certain extent, this trend is associated with the development and improvement of assisted reproductive technologies [1].
Perinatal outcomes in multiple pregnancies are highly dependent on chorionality (number of placentas) [2, 6]. The monochorionic type of placentation is the least favorable, which is associated with a greater number of adverse perinatal outcomes compared to dichorionic [4, 7]. The frequency of fetoplacental insufficiency and intrauterine growth retardation of the fetus/fetus in multiple pregnancy is 10 times higher than in singleton [3]. Perinatal mortality in multiple pregnancy is 3-4 times higher than in singleton, and among monozygotic twins - 2.5 times higher than among dizygotic twins. Postnatal losses do not depend on chorionicity and are mainly due to prematurity [8].
The frequency of fetoplacental insufficiency and intrauterine growth retardation of the fetus/fetus in multiple pregnancy is 10 times higher than in singleton [3]. Perinatal mortality in multiple pregnancy is 3-4 times higher than in singleton, and among monozygotic twins - 2.5 times higher than among dizygotic twins. Postnatal losses do not depend on chorionicity and are mainly due to prematurity [8].
Diagnosis of multiple pregnancy on the basis of anamnestic data and the clinical picture presents certain difficulties. The introduction of ultrasound research methods into obstetric practice has radically changed the diagnostic possibilities [5]. Currently, echography is the only real highly informative non-invasive method for diagnosing multiple pregnancies. With its help, it is possible not only to carry out early diagnosis, but also to determine the nature of the development of the fetus by biometric indicators. The parameters of the physical development of newborns with multiple pregnancy differ from those of children with a singleton pregnancy, and therefore they cannot be evaluated according to the same normative tables. At the same time, there are no percentile tables that make it possible to judge the development of fetuses in multiple pregnancies.
At the same time, there are no percentile tables that make it possible to judge the development of fetuses in multiple pregnancies.
The purpose of the study was to assess the parameters of the physical development of fetuses and newborns during pregnancy with twins and the development of percentile evaluation tables.
Material and methods
Examination of 112 patients with spontaneous twin pregnancy (main group) was carried out. All patients of the main group were divided into two subgroups depending on chorion: 26 pregnant women with monochorionic diamniotic twins (1st subgroup) and 86 pregnant women with dichorionic diamniotic twins (2nd subgroup). The comparison group consisted of 20 pregnant women with a spontaneous singleton pregnancy.
All examined patients underwent a thorough history taking, including information on hereditary and extragenital diseases, the number and outcomes of previous pregnancies, the course of this pregnancy, the presence and severity of its complications. In 100% of cases, an ultrasound examination was performed, which included determining the position of the fetus in the uterus, measuring the biparietal size of the head, the circumference of the chest and abdomen of the fetus. In addition, the amount and nature of amniotic fluid, the number of placentas, their localization, thickness, maturity and structural features were assessed. In the 1st subgroup, studies were carried out from 28 weeks of gestation with an interval of 14 days, in the 2nd subgroup - at 28, 32 and 36 weeks. At 30, 34 weeks and before delivery, the resistance of the vessels of the fetoplacental complex was studied using pulsed Doppler.
In 100% of cases, an ultrasound examination was performed, which included determining the position of the fetus in the uterus, measuring the biparietal size of the head, the circumference of the chest and abdomen of the fetus. In addition, the amount and nature of amniotic fluid, the number of placentas, their localization, thickness, maturity and structural features were assessed. In the 1st subgroup, studies were carried out from 28 weeks of gestation with an interval of 14 days, in the 2nd subgroup - at 28, 32 and 36 weeks. At 30, 34 weeks and before delivery, the resistance of the vessels of the fetoplacental complex was studied using pulsed Doppler.
In addition, 221 newborns born in patients of the main group and 20 newborns in the comparison group were examined. At the birth of children, their gender, the main indicators of physical development (body weight, head and chest circumferences), compliance with the gestational age, assessment of the state on the Apgar scale at the 1st and 5th minutes were taken into account.
Comparison of the examined groups of pregnant women was carried out using non-parametric criteria (Wilcoxon-Mann-Whitney, Kolmogorov-Smirnov, c2, Fisher's exact method). The calculations were carried out using the Statistica 7.0 software package.
Results and discussion
Analysis of anamnestic data showed that the average age of the examined patients of the main group was 28 years, while patients with monochorionic type of placentation were younger (median 25.5 years) than patients with dichorionic twins (median 30 years). The significance of the hereditary factor in patients with monochorionic twins was also noted.
Various extragenital diseases were detected in 79 (70.5%), and gynecological diseases - in 44 (39.3%) of patients of the main group. 11 women had a combination of both diseases. Among the surveyed women of the 1st subgroup, there was a high percentage of primiparas (65.4). In the history of pregnant women in the main group, a high number of spontaneous miscarriages (23. 2%) was noted, and the production of caesarean section was 6.3%. Previous pregnancies ended in induced abortions in 42 (37.5%) patients of the main group, while in the 2nd subgroup the frequency of abortions was 2 times higher than in the 1st.
2%) was noted, and the production of caesarean section was 6.3%. Previous pregnancies ended in induced abortions in 42 (37.5%) patients of the main group, while in the 2nd subgroup the frequency of abortions was 2 times higher than in the 1st.
The course of this pregnancy was complicated in all patients of the main group: early toxicosis - in 62 (55.4%), which is 2 times more often than in patients of the comparison group; preeclampsia - in 56 (50.4%), while in 4 (3.6%) cases there was an average degree of severity, and in 3 (2.7%) - a severe degree. The threat of abortion in the I and II trimesters was diagnosed in 73 (65.2%) and 82 (73.2%) patients of the main group, respectively, which is 3 times more often than in the comparison group. In the III trimester, the threat of preterm labor complicated the course of 73 (65.2%) pregnancies in the main group and only 1 (5%) in the comparison group, which confirms the unfavorable course of multiple pregnancy.
The number of spontaneous births in both subgroups did not differ significantly (44-46%). However, it is noteworthy that in the 2nd subgroup, operative vaginal delivery (vacuum extraction of the fetus, extraction of the fetus behind the pelvic end) was most common, and in the 1st subgroup, the number of cases of caesarean section was higher (63.8%). The number of cases of planned and emergency abdominal delivery in the subgroups was the same (35 and 65%, respectively), and the indications for caesarean section were basically similar. But in the 1st subgroup at 29% of cases of caesarean section were performed due to breech presentation of the first fetus, every fifth patient was operated on for weakness of labor, the same number due to placental insufficiency (FPI). In the 2nd subgroup, the main indication for abdominal delivery was the breech presentation of the first fetus (54%), high myopia with changes in the fundus (16%), and 5% of women were delivered by the abdominal route due to the severity of preeclampsia.
However, it is noteworthy that in the 2nd subgroup, operative vaginal delivery (vacuum extraction of the fetus, extraction of the fetus behind the pelvic end) was most common, and in the 1st subgroup, the number of cases of caesarean section was higher (63.8%). The number of cases of planned and emergency abdominal delivery in the subgroups was the same (35 and 65%, respectively), and the indications for caesarean section were basically similar. But in the 1st subgroup at 29% of cases of caesarean section were performed due to breech presentation of the first fetus, every fifth patient was operated on for weakness of labor, the same number due to placental insufficiency (FPI). In the 2nd subgroup, the main indication for abdominal delivery was the breech presentation of the first fetus (54%), high myopia with changes in the fundus (16%), and 5% of women were delivered by the abdominal route due to the severity of preeclampsia.
Premature births occurred in 26 (23.2%) patients of the main group, while spontaneous births in the 1st subgroup were noted in 18 (69. 2%), and in the 2nd subgroup - in 5 (27.8%).
2%), and in the 2nd subgroup - in 5 (27.8%).
Dissociated fetal development (difference in birth weight over 10%) was detected in 26 (23%) patients: in 5 (19.2%) in the 1st subgroup and in 21 (24.4%) in the 2nd subgroup. th.
It should be emphasized that among all those born in the main group, 8 pairs of newborns had a difference in body weight of less than 500 g, i.e. 16 (7.2%) children, 14 pairs of twins - 28 (12.6%) newborns had a difference in body weight from 500 g to 1000 g, 4 pairs - 8 (3.6%) newborns more than 1000 g. In satisfactory 144 (65.1%) children were born. Hypoxia at birth was diagnosed in 77 (34.8%) newborns, 6 (2.7%) children were born in a state of severe asphyxia. Signs of dissociated development were observed in 52 newborns. Discharged home in a satisfactory condition 31 (59.6%) out of 52 children with dissociated development, 19 (36.5%) children of this group were transferred to staged nursing. Two (3.9%) dissociated monochorionic twin fetuses died antenatally. In 12 (46.2%) patients with dissociated fetal development, spontaneous labor occurred, the same number were delivered by caesarean section, in 1 (3.8%), a caesarean section was performed on the second fetus due to acute hypoxia against the background of premature detachment of the placenta, in 1 (3.8%) woman in labor underwent vacuum extraction of the second fetus due to acute hypoxia. With a monochorionic type of placentation and a dissociated type of fetal development, premature births occurred 8 times more often. Vascular anastomoses were found in placentas in 3 (11.5%) patients with monochorionic twins. In 2 (7.6%) patients of the 1st subgroup, sheath attachment of the umbilical cord of the smaller of the fetuses was found, and 2 times less often (3.8%) - marginal attachment of the umbilical cord.
In 12 (46.2%) patients with dissociated fetal development, spontaneous labor occurred, the same number were delivered by caesarean section, in 1 (3.8%), a caesarean section was performed on the second fetus due to acute hypoxia against the background of premature detachment of the placenta, in 1 (3.8%) woman in labor underwent vacuum extraction of the second fetus due to acute hypoxia. With a monochorionic type of placentation and a dissociated type of fetal development, premature births occurred 8 times more often. Vascular anastomoses were found in placentas in 3 (11.5%) patients with monochorionic twins. In 2 (7.6%) patients of the 1st subgroup, sheath attachment of the umbilical cord of the smaller of the fetuses was found, and 2 times less often (3.8%) - marginal attachment of the umbilical cord.
When analyzing weight and height indicators, it turned out that in more than 50% of children in both subgroups, body weight exceeded 2500 g. During full-term pregnancy with low body weight (less than 2500 g), 16% of children in the 1st subgroup and 8% in the 2nd subgroup were born. th subgroup (see figure). Figure 1. Body weight of children of patients of the main group at birth. The second children were 2 times more likely to have a lower birth weight.
th subgroup (see figure). Figure 1. Body weight of children of patients of the main group at birth. The second children were 2 times more likely to have a lower birth weight.
The body weight of newborns in multiple and singleton pregnancies did not differ significantly during the third trimester. The data obtained are consistent with the data of other researchers: the greatest differences were observed at a gestational age of 36 weeks or more.
We made an attempt to develop percentile tables to determine the anthropometric parameters of newborns born in multiple pregnancies at different gestational ages (Table 1).
The circumference of the fetal head in a multiple pregnancy from 32 to 36 weeks of gestation is commensurate with that in a singleton pregnancy, however, from 36 weeks of gestation, it slows down growth by 1-2 cm compared with this parameter in the presence of one fetus (Table 2).
The only indicator that differs throughout the entire third trimester is the fetal chest circumference. The increase in this indicator lags behind by 2-3 cm compared with that in singleton pregnancy (Table 3).
The increase in this indicator lags behind by 2-3 cm compared with that in singleton pregnancy (Table 3).
In 111 patients of the main group, the pregnancy ended in the birth of live children, of which 172 (77.8%) were full-term. In the 1st subgroup, 50 (96.2%) children were born alive, in the 2nd - 171 (99.4%). The number of children born in a satisfactory condition did not differ significantly in both subgroups. However, in the 1st subgroup there were slightly more children born in serious condition (11.5% in the 1st subgroup versus 9.3% in the 2nd). In the 2nd subgroup, children at birth were more likely to have hypoxic syndrome.
Premature in the 1st subgroup were born 16 (30.8%) children, in the 2nd - 36 (20.9%). Among premature babies, 19 (36.5%) were born in a satisfactory condition, hypoxia at birth was diagnosed in 19 (36.5%), severe asphyxia at birth - in 12 (23.2%).
The course of the early neonatal period became complicated in more than 50% of the children of the main group. The most frequent complications were recorded in the monochorionic type of placentation: hypoxic-ischemic damage to the central nervous system, respiratory distress syndrome, intrauterine infection. Intrauterine infection was detected 4.8 times more often in the 1st subgroup. Perinatal losses were represented by two antenatalally dead fetuses and one intranatally dead fetus in the 1st subgroup (monochorial twins), in the 2nd subgroup (dichorionic twins) a postnatally premature newborn died on the 10th day after caesarean section.
The most frequent complications were recorded in the monochorionic type of placentation: hypoxic-ischemic damage to the central nervous system, respiratory distress syndrome, intrauterine infection. Intrauterine infection was detected 4.8 times more often in the 1st subgroup. Perinatal losses were represented by two antenatalally dead fetuses and one intranatally dead fetus in the 1st subgroup (monochorial twins), in the 2nd subgroup (dichorionic twins) a postnatally premature newborn died on the 10th day after caesarean section.
Thus, the number of dead fetuses in the 1st subgroup was 3 times higher than in the 2nd. More children (46.2%) were transferred to the 2nd stage of nursing from the 1st subgroup than from the 2nd (33%).
We have developed fetometric indicators for ultrasonic determination of anthropometric parameters of fetuses from twins (Table 4). When analyzing data on determining the main ultrasonic anthropometric parameters of fetuses from multiple pregnancies, a clear trend towards a decrease in these indicators in relation to those in the comparison group throughout the entire third trimester of pregnancy is obvious.