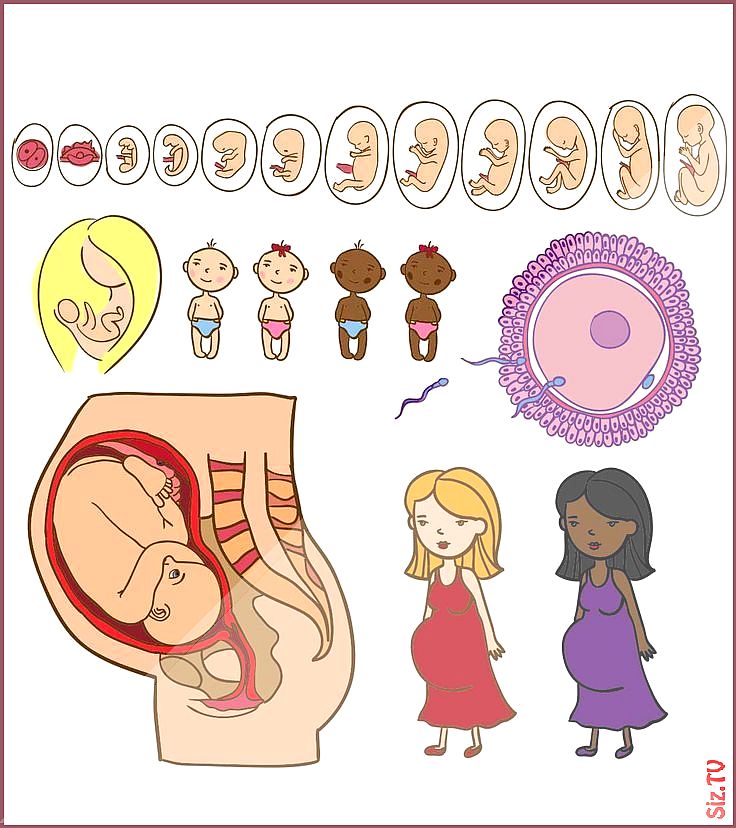
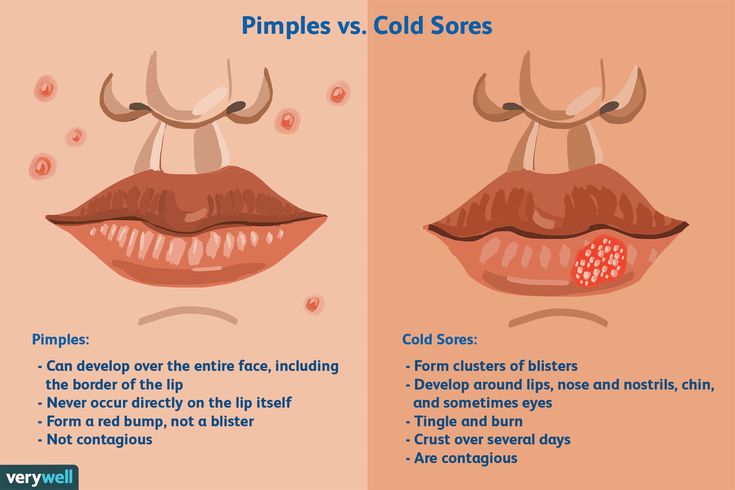
Cold sore locations
Cold sore symptoms & treatments - Illnesses & conditions
Cold sores usually clear up without treatment within 7 to 10 days. Antiviral tablets or cream can be used to ease your symptoms and speed up the healing time.
If you develop a cold sore, some general advice to follow includes:
- drink plenty of fluids to avoid dehydration
- avoid acidic or salty foods and eat cool, soft foods
- if brushing your teeth is painful, use an antiseptic mouthwash
- dab creams on to sores rather than rubbing them in
- wash your hands using soap and water before and after applying cold sore creams
- avoid touching your cold sores, other than to apply cream, and don't share your cold sore cream with others
Antiviral creams and tablets
Antiviral creams such as aciclovir or penciclovir (also known as Fenistil®) may speed up the healing time of a recurrent cold sore infection if used correctly.
Cold sore creams are widely available over the counter from pharmacies without a prescription.
They're only effective if you apply them as soon as the first signs of a cold sore appear, when the herpes simplex virus is spreading and replicating. Using an antiviral cream after this initial period is unlikely to have much effect.
If you have frequently recurring bouts of cold sores, use antiviral medication as soon as you feel the tingling sensation that indicates a cold sore is about to develop. You'll need to apply the cream up to five times a day for four to five days.
Antiviral creams can only help to heal a current outbreak of cold sores. They don't get rid of the herpes simplex virus or prevent future outbreaks of cold sores occurring.
Antiviral tablets are generally more effective than creams at treating cold sores, but are usually only prescribed for more severe cases.
Cold sore patches
Cold sore patches that contain a special gel called hydrocolloid are also available. They're an effective treatment for skin wounds and are placed over the cold sore to hide the sore area while it heals.
Non-antiviral treatments
Several non-antiviral creams are also available over the counter from pharmacies without the need for a prescription.
These creams aren't specifically designed to treat cold sores and won't help them heal faster, but they may help ease any pain or irritation. Ask your pharmacist to recommend a suitable treatment for you.
Pain can also be treated with painkillers such as ibuprofen or paracetamol – both are available in liquid form for young children.
However, don't take ibuprofen if you have asthma or stomach ulcers, or you've had them in the past.
Children under the age of 16 shouldn't be given aspirin.
Speak to your pharmacist if you have cold sores and you're pregnant.
Treating complications
If your cold sores are particularly severe or your immune system is damaged – for example, if you have HIV or you're having chemotherapy treatment – you may be at risk of developing serious complications.
For example, your risk of developing encephalitis or the infection spreading to other parts of your body, such as your eyes, is increased.
Speak to your GP if you're at risk. They may prescribe antiviral tablets and refer you for specialist treatment.
The type of treatment recommended will depend on the severity of your cold sore symptoms and the complication that's causing problems.
For example, if you develop herpetic keratoconjunctivitis – a secondary eye infection – you may need to see an ophthalmologist, a specialist eye doctor.
Gingivostomatitis
Visit your pharmacist if you or your child develops swollen, painful gums (gingivostomatitis) as a result of the primary herpes simplex infection. They'll be able to suggest treatments to help ease your symptoms.
If the infection is painful, your pharmacist may suggest using a preparation that contains benzydamine, which is available as an oral rinse or oral spray, to help relieve any pain in your mouth or throat.
Brushing your teeth may also be painful because of the swelling of your gums. Your pharmacist may suggest using an antiseptic mouthwash.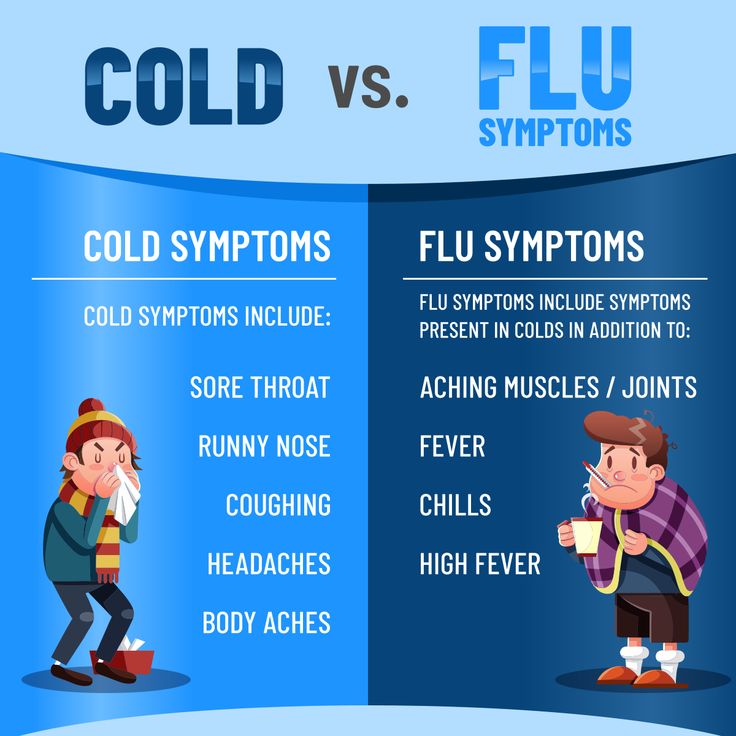 This helps prevent secondary infections and will also control a build-up of plaque if you can't brush your teeth effectively.
This helps prevent secondary infections and will also control a build-up of plaque if you can't brush your teeth effectively.
As with the treatment of cold sores, any pain or fever can be treated using ibuprofen or paracetamol.
In rare cases of gingivostomatitis, it's possible for your lips to become stuck together in places. Using a lip barrier cream available from your local pharmacist will help prevent this.
Dehydration
If you or your child has gingivostomatitis, it's important to drink plenty of fluids to avoid becoming dehydrated. Young children are particularly at risk as they may refuse to eat or drink because of the pain in their mouth.
It's important to watch out for signs of dehydration, such as:
- headaches
- tiredness
- irritability
- lightheadedness
- low urine output
Most cases of gingivostomatitis get better in 7 to 14 days, although it may take up to three weeks for the sores to heal completely.
Specialist treatment
If you or your child still has symptoms of gingivostomatitis after two weeks or the infection is severe your pharmacist may advise you to contact your GP, who may refer you for specialist treatment.
Specialist referral may also be needed for gingivostomatitis if you're pregnant or have a weakened immune system.
Visit your GP if you have a newborn baby who develops gingivostomatitis, as they may also need to be referred for specialist treatment.
Cold sore - Symptoms and causes
Overview
Cold sore
Cold sore
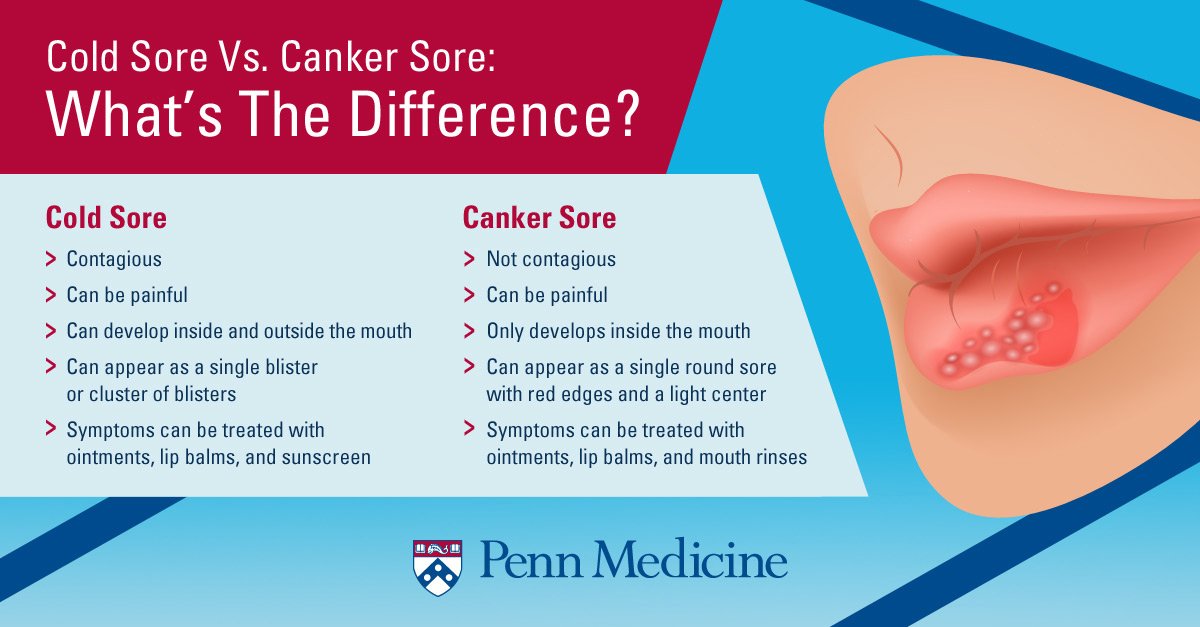
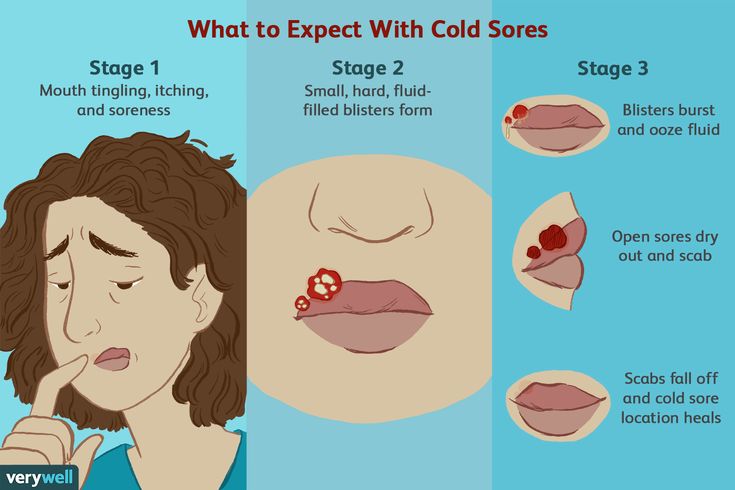
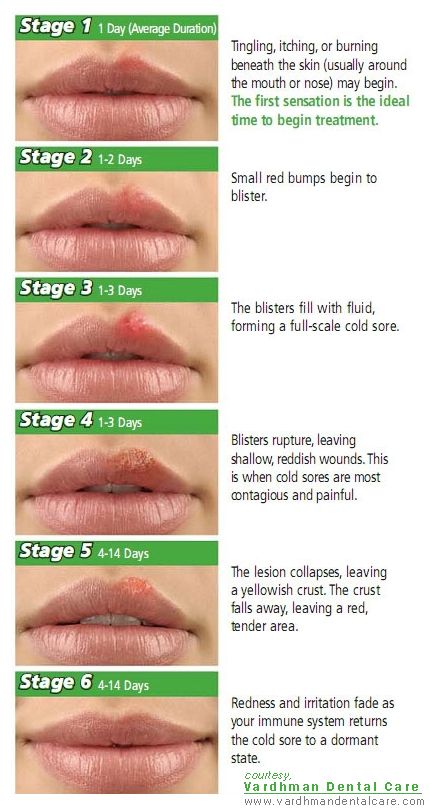
Cold sores, often called fever blisters, are clustered, small, fluid-filled blisters. You may feel a tingling on your lip before a small, hard, painful spot appears (top). In a day or two, blisters form, which later break and ooze (bottom). Healing usually occurs in two to three weeks without scarring.
Cold sores — also called fever blisters — are a common viral infection. They are tiny, fluid-filled blisters on and around your lips. These blisters are often grouped together in patches. After the blisters break, a scab forms that can last several days. Cold sores usually heal in two to three weeks without leaving a scar.
They are tiny, fluid-filled blisters on and around your lips. These blisters are often grouped together in patches. After the blisters break, a scab forms that can last several days. Cold sores usually heal in two to three weeks without leaving a scar.
Cold sores spread from person to person by close contact, such as kissing. They're usually caused by herpes simplex virus type 1 (HSV-1), and less commonly herpes simplex virus type 2 (HSV-2). Both of these viruses can affect your mouth or genitals and can be spread by oral sex. Cold sores are contagious even if you don't see the sores.
There's no cure for cold sores, but treatment can help manage outbreaks. Prescription antiviral pills or creams can help sores heal more quickly. And they may reduce the frequency, length and severity of future outbreaks.
Products & Services
- Book: Mayo Clinic Book of Home Remedies
Symptoms
A cold sore usually passes through several stages:
- Tingling and itching.
 Many people feel itching, burning or tingling around the lips for a day or so before a small, hard, painful spot appears and blisters erupt.
Many people feel itching, burning or tingling around the lips for a day or so before a small, hard, painful spot appears and blisters erupt. - Blisters. Small fluid-filled blisters typically erupt along the border of your lips. Sometimes they appear around the nose or cheeks or inside the mouth.
- Oozing and crusting. The small blisters may merge and then burst, leaving shallow open sores that ooze and crust over.
Signs and symptoms vary, depending on whether this is your first outbreak or a recurrence. The first time you have a cold sore, symptoms may not start for up to 20 days after you were first exposed to the virus. The sores can last several days, and the blisters can take two to three weeks to heal completely. Recurrences typically appear at the same spot each time and tend to be less severe than the first outbreak.
In a first-time outbreak, you also might experience:
- Fever
- Painful gums
- Sore throat
- Headache
- Muscle aches
- Swollen lymph nodes
Children under 5 years old may have cold sores inside their mouths and the lesions are commonly mistaken for canker sores.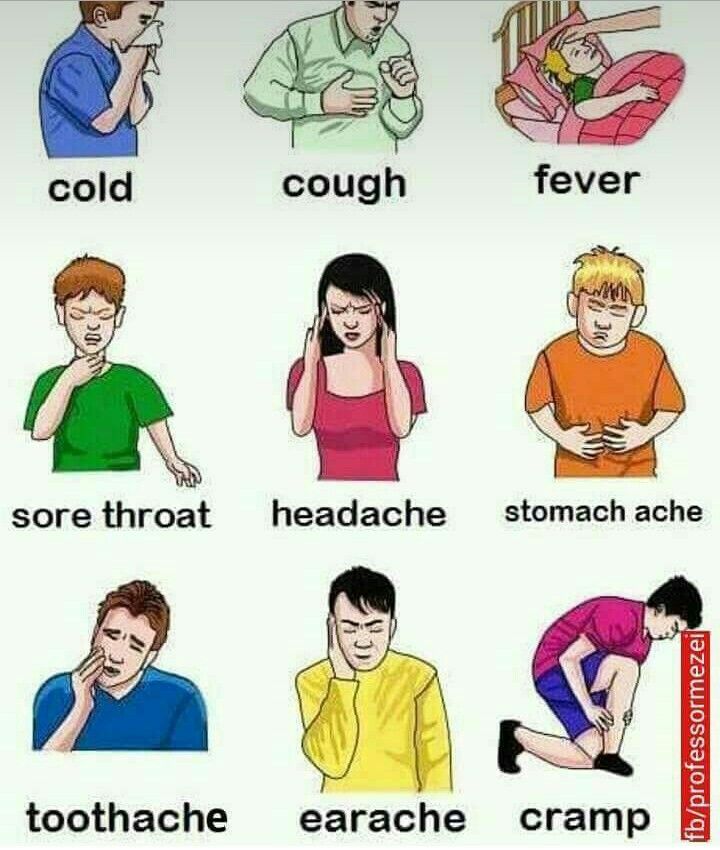 Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
When to see a doctor
Cold sores generally clear up without treatment. See your doctor if:
- You have a weakened immune system
- The cold sores don't heal within two weeks
- Symptoms are severe
- You have frequent recurrences of cold sores
- You experience irritation in your eyes
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Cold sores are caused by certain strains of the herpes simplex virus (HSV). HSV-1 usually causes cold sores. HSV-2 is usually responsible for genital herpes. But either type can spread to the face or genitals through close contact, such as kissing or oral sex. Shared eating utensils, razors and towels might also spread HSV-1.
Cold sores are most contagious when you have oozing blisters because the virus easily spreads through contact with infected body fluids. But you can spread the virus even if you don't have blisters. Many people who are infected with the virus that causes cold sores never develop signs and symptoms.
Once you've had an episode of herpes infection, the virus lies dormant in nerve cells in your skin and may emerge as another cold sore at the same place as before. Recurrence may be triggered by:
- Viral infection or fever
- Hormonal changes, such as those related to menstruation
- Stress
- Fatigue
- Exposure to sunlight and wind
- Changes in the immune system
- Injury to the skin
Video: 3 things you didn't know about cold sores
Cold sores on the lips can be embarrassing and tough to hide. But, turns out, you might not have a reason to be embarrassed.
"About 70-plus percent of the U. S. population has been infected with herpes simplex 1. Now, a very small percentage of those people will actually develop cold sores."
S. population has been infected with herpes simplex 1. Now, a very small percentage of those people will actually develop cold sores."
Dr. Pritish Tosh, an infectious diseases specialist at Mayo Clinic, says, genetics determines whether a person will develop cold sores.
"A proportion of the population, they don't quite have the right immunologic genes and things like that and so they're not able to handle the virus as well as other people in the population."
The problem is people can spread the herpes virus whether they develop cold sores or not. Herpes virus spreads through physical contact like kissing, sharing a toothbrush — even sharing a drinking glass — or through sexual contact.
"Since the number of people who are infected but don't have symptoms vastly outnumber the people who are infected and have symptoms, most new transmissions occur from people who have no idea that they are infected."
For the Mayo Clinic News Network, I'm Ian Roth.
Risk factors
Almost everyone is at risk of cold sores. Most adults carry the virus that causes cold sores, even if they've never had symptoms.
Most adults carry the virus that causes cold sores, even if they've never had symptoms.
You're most at risk of complications from the virus if you have a weakened immune system from conditions and treatments such as:
- HIV/AIDS
- Atopic dermatitis (eczema)
- Cancer chemotherapy
- Anti-rejection drugs for organ transplants
Complications
In some people, the virus that causes cold sores can cause problems in other areas of the body, including:
- Fingertips. Both HSV-1 and HSV-2 can be spread to the fingers. This type of infection is often referred to as herpes whitlow. Children who suck their thumbs may transfer the infection from their mouths to their thumbs.
- Eyes. The virus can sometimes cause eye infection.
 Repeated infections can cause scarring and injury, which may lead to vision problems or loss of vision.
Repeated infections can cause scarring and injury, which may lead to vision problems or loss of vision. - Widespread areas of skin. People who have a skin condition called atopic dermatitis (eczema) are at higher risk of cold sores spreading all across their bodies. This can become a medical emergency.
Prevention
Your doctor may prescribe an antiviral medication for you to take on a regular basis if you develop cold sores more than nine times a year or if you're at high risk of serious complications. If sunlight seems to trigger your recurrences, apply sunblock to the spot where the cold sore tends to erupt. Or talk with your doctor about using an oral antiviral drug as a preventive if you expect to be doing an activity that tends to trigger your condition, such as intense sunlight exposure.
To help avoid spreading cold sores to other people or to other parts of your body, you might try some of the following precautions:
- Avoid kissing and skin contact with people while blisters are present.
 The virus spreads most easily when the blisters leak fluid.
The virus spreads most easily when the blisters leak fluid. - Avoid sharing items. Utensils, towels, lip balm and other personal items can spread the virus when blisters are present.
- Keep your hands clean. When you have a cold sore, wash your hands carefully before touching yourself and other people, especially babies.
By Mayo Clinic Staff
Herpes: symptoms and treatment, doctor's advice
- Home >
- About clinic >
- Publications >
- Herpes: causes, symptoms, and treatment of the virus
"Cold" on the lips is familiar to almost everyone. It is worth catching a runny nose or getting nervous, as an unpleasant harbinger immediately appears - a tingling sensation somewhere near the mouth.
The herpes simplex virus is present in the body of 95% of people. And only a few have immunity, the reasons for which are still not understood.
The virus enters the body in early childhood: at 3-4 years old, when the antibodies against the herpes virus transmitted to the baby by the mother are depleted. Most often, infection occurs if the child is kissed by carriers of the infection. In addition to a kiss, the virus can enter the body, for example, with saliva. It penetrates into the mucous membranes, reaches the nerve endings, rises into the cranial cavity, where it "hides" in the nerve plexus, called the trigeminal ganglion, and "sleeps" there until it is reactivated.
Herpes "wakes up" with a decrease in immunity
Causes of recurrence of herpes on the lips: stress or emotional upset; various other diseases, in particular colds, flu, diabetes, HIV; poisoning or intoxication; alcohol, caffeine and smoking; excessive ultraviolet radiation; hypothermia or overheating; the onset of menstruation; overwork and exhaustion; malnutrition/diet or indigestion; other individual factors for each person.
After "waking up" the virus is sent back to the skin.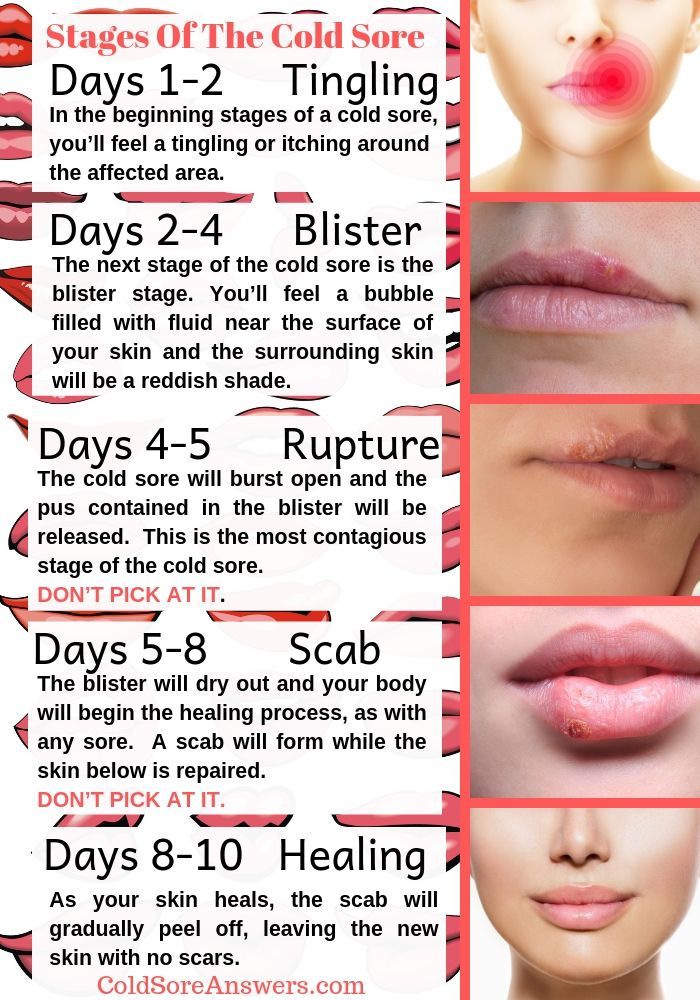 When moving through a nerve, the virus causes inflammation of the nerve tissue.
When moving through a nerve, the virus causes inflammation of the nerve tissue.
The development of herpes can be divided into several stages. At the first stage, the person feels unwell. Pain, tingling appear at the site of the appearance of the "fever", the skin turns red. At the stage of inflammation, a small, painful vesicle filled with fluid forms. After a while, the vial bursts and a colorless liquid containing billions of viral particles flows out of it. An ulcer appears in its place. At the final stage, the sore is covered with a crust.
Most often, herpes appears on the lips, but lesions can also appear on the face, around the ears, or in the oral cavity.
What to do if you have a "cold" on your lips
At the moment, no medicines and treatments have been developed that would completely destroy the herpes simplex virus in the human body. But a few tips for those suffering from herpes can be given.
-
Strictly follow the rules of personal hygiene! Since herpes is contagious, wash your hands with soap and use separate dishes and towels.
-
Don't bring your hands to your eyes! And don't wet your lenses with saliva! Herpes can affect the mucous membrane of the eye.
-
It is not recommended to touch a viral rash, kiss. The virus can be transmitted by wearing one lipstick or smoking one cigarette.
-
If you try to remove a blister or crust over an ulcer, the virus can spread to other parts of the body.
-
Give up oral sex! A virus from affected lips can cause genital herpes in a partner.
-
A young mother must also take certain precautions to protect her baby from contracting herpes. If you have cold sores, wash your hands with soap every time before touching your baby. And in no case should the affected surface come into contact with the skin of the child.
How to minimize discomfort
Starting to use anti-herpes drugs should begin as soon as you feel a tingling sensation. Medications won't get rid of the virus, but they will stop it from progressing and speed up your recovery. There are drugs that prevent the development of the virus: tablets, ointments for external use, which help the healing of blisters and ulcers, reduce discomfort.
When applying the ointment, use cotton swabs to avoid transmitting the virus from the lips to the skin of the fingers.
Herpes requires the attention of specialists! A "cold" on the lips can be a symptom of serious diseases: a sharp decrease in immunity, cancer, HIV infection.
If you suffer from relapses of herpes - consult a doctor. The specialist will not only relieve you of unnecessary worries and eliminate the danger to health, but will also help you choose a comprehensive program for the prevention and treatment of herpes.
To make an appointment with an immunologist or a dermatologist for the program of diagnosis and treatment of herpes, call the Family Doctor clinic +7 (495) 775 75 66 (clinic hours: Mon-Fri from 8.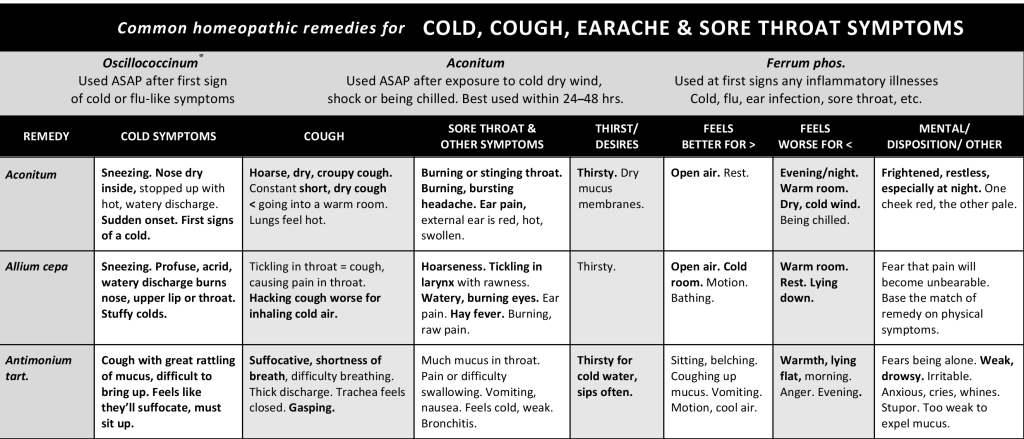 00 to 21.00, Sat-Sun from 9.00 to 20.00), or make an appointment and diagnostics through the online appointment form
00 to 21.00, Sat-Sun from 9.00 to 20.00), or make an appointment and diagnostics through the online appointment form
Return to the list of publications
Physicians
About the doctor Record
Ilyenko Verenika Alexandrovna
allergist-immunologist, Ph.D.
Clinic on Ozerkovskaya
About the doctor Record
Fesenko Irina Davidovna
Children's building on Usacheva
Services
- Demodex analysis
- Dermatologist-oncologist
- Dermatologist
- Calling a dermatologist at home
- Calling a pediatric dermatologist at home
- Toenail fungus in a child
- Dermoscopy of moles
- Facial cryotherapy
- Laser removal of keratomas
- Laser removal of neoplasms
- Laser therapy
- Treatment of allergic dermatitis
- Treatment of allergic dermatosis
- Treatment of atopic dermatitis
- Treatment of warts in children
- Treatment of varicose eczema
- Treatment of vitiligo in children
- Treatment of herpes in children
- Treatment of demodicosis
- Treatment of dyshidrotic eczema
- Treatment of lichen planus
- Treatment of mycoses
- Treatment of pityriasis versicolor
- Treatment of papillomas
- Treatment of flat warts
- Treatment of psoriasis
- Rosacea treatment
- Treatment of seborrheic dermatitis
- Treatment of seborrheic dermatitis in children
- Scabies treatment
- eczema treatment
- Treatment of eczema in children
- Mycosis of the skin, hands and feet
- Pityriasis versicolor in children
- Plantar warts in children
- Scabies
- seborrheic eczema
- Wart removal
- Nitrogen Wart Removal
- Laser wart removal
- Removal of warts in children
- Removal of keratoma with nitrogen
- Removal of keratoma
- Molluscum contagiosum removal
- Removal of genital warts
- Removal of plantar warts
- Laser mole removal
- Removal of moles in children
- Removal of moles surgically
- Facial phototherapy
Herpes - KVD №2
What is a herpetic infection?
Genital herpes is a sexually transmitted infection (STI). The disease is caused by the herpes simplex virus 1 or 2 (HSV - 1.2) type - Herpes Simplex Virus.
The disease is caused by the herpes simplex virus 1 or 2 (HSV - 1.2) type - Herpes Simplex Virus.
Herpes is manifested by the appearance of redness of a small area of the skin, itching, the appearance of one or more vesicles, then the vesicles open with the formation of painful sores that heal with the formation of crusts. The first case of diseases is more acute than repeated ones, and takes from 2 to 4 weeks. HSV-1 most often affects the skin of the face, lips, mouth, cornea of the eye, and less often the genitals. HSV type 2 affects the genitals and anus, and therefore often this virus is called genital herpes. Herpetic infection is a chronic disease, once it enters the body, HSV remains in it, living in the nerve endings, for life. Some people may not have exacerbations of the disease, while others experience exacerbations very often. The latent course of the disease is the cause of the easy spread of infection.
.
Ways of herpes infection
HSV-1 infection occurs mainly in childhood and adolescence by airborne droplets or by contact (kissing, etc. ). Sexual transmission is also possible through oral-genital contact.
). Sexual transmission is also possible through oral-genital contact.
Infection with genital herpes (HSV-2) occurs through direct sexual contact. Infection can occur both with an exacerbation of infection in a sexual partner, and with the carriage of the virus. However, the risk of infection is much higher if one partner has herpetic eruptions on the skin and mucous membranes and there is close contact with the skin and mucous membranes of the other sexual partner.
Exacerbations of genital herpes are provoked by hypothermia, physical and emotional stress, menstruation in women, sexual intercourse, concomitant diseases (flu, etc.) and ultraviolet radiation.
The virus can be transmitted to the fetus from an infected mother during pregnancy or childbirth.
Manifestations of herpes
Most of those infected have no manifestations of the disease. The rest of the signs of herpes appear 2 to 20 days after infection.
Initially, there may be flu-like manifestations - slight fever, chills, weakness, fatigue.
A typical sign of genital herpes is the appearance of small (2-5 mm) fluid-filled blisters on the genitals, buttocks and anus. The rash is accompanied by itching and/or pain. Rashes can be located in the vagina, on the cervix, in the rectum. Within a few days, the blisters burst, turning into painful sores. After 1-2 weeks, the sores, covered with crusts, heal. Other manifestations: pain in the groin or on the inside of the thighs, painful urination, vaginal discharge in women or from the urethra in men.
Primary infection lasts about 3 weeks with severe manifestations.
When symptoms subside, the herpes virus leaves the lesion and enters the nerve cells of the sacral spine. During the next exacerbation, the virus goes through the nerves to the skin or mucous membranes, where it causes typical rashes.
After the initial episode of the disease, exacerbations occur several times (usually 4-5) during the year. In the future, the number of exacerbations decreases, the severity of manifestations decreases.
Complications of infection
Persons with a decrease in the body's defenses experience very frequent prolonged exacerbations that cause both physical suffering and psycho-emotional discomfort.
It is possible to attach a secondary (bacterial) infection, and then the deeper layers of the skin are involved in the inflammatory process, the exacerbation becomes protracted and requires changes in treatment.
Persons with genital herpes in the acute phase are more at risk of contracting HIV infection. HIV-infected people who have genital herpes in the acute stage are more likely to infect their sexual partners with the human immunodeficiency virus.
The effect of the disease on a pregnant woman and her child
Infection of the fetus occurs during pregnancy, a newborn during childbirth through an infected birth canal. Herpetic infection of newborns is very dangerous and can lead to the death of a child. If during childbirth a woman has herpetic eruptions in the genital area (birth canal) - this is an indication for a caesarean section. This dramatically reduces the risk of transmitting herpes to the newborn during childbirth. It is very important for a woman to avoid contracting genital herpes during pregnancy, since it is the initial episode of infection that is most dangerous for the fetus.
This dramatically reduces the risk of transmitting herpes to the newborn during childbirth. It is very important for a woman to avoid contracting genital herpes during pregnancy, since it is the initial episode of infection that is most dangerous for the fetus.
Diagnosis of herpes
The manifestations of genital herpes are varied, it is difficult to detect ulcers and distinguish them from ulcers caused by other diseases.
Diagnosis includes visual examination of the patient's clinical signs if an exacerbation is typical. Scrapings from sores for HSV are being studied by PCR (polymerase chain reaction). It is very important to establish the microorganism that caused the clinical manifestations in order to prescribe the correct and timely treatment. Swabs and scrapings may cause minor discomfort. Additionally, a blood test is performed by ELISA to determine specific antibodies to HSV-2, the duration of the last exacerbation and the amount of antibodies are estimated. The ELISA method allows you to diagnose genital herpes without exacerbation.
The ELISA method allows you to diagnose genital herpes without exacerbation.
Treatment of herpetic infection
Diagnosis and treatment of genital herpes, as well as other STIs, should be carried out in a specialized clinic - KVD, which has all the necessary tools for quick and accurate diagnosis.
Once infected with HSV, it is no longer possible to recover completely. There are no drugs that definitively cure herpes yet. Antiviral antibiotics inhibit the reproduction (replication) of the virus, speed up the healing time of sores and help prevent their reappearance.
To be more effective, antibiotics should be given as early as possible, at the very first sign of an aggravation - hypersensitivity, itching and/or reddening of the skin areas where rashes usually appear.
Herpes Prevention
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner. Latex male condoms, when properly used and provided they cover areas of skin with cold sores, can reduce the risk of transmission.