Pregnant warning signs
Pregnancy Warning Signs: Symptoms Not to Ignore
Most of the symptoms women experience during pregnancy are normal, even if they're not exactly comfortable. They are simply the result of being pregnant. Still, it's easy to worry and wonder whether everything is OK and how to know if it’s not. Although true complications are rare, it's always good to know what to look out for. Read on for some pregnancy symptoms you should not ignore that are worth contacting your healthcare provider about.
Vaginal spotting. Early on in the pregnancy, it can be normal to experience spotting that’s known as implantation bleeding; however, in some cases there could be spotting or bleeding due to a more serious condition, like an ectopic pregnancy, a molar pregnancy, or a cervical infection. Contact your healthcare provider if the spotting is heavy and is accompanied by other symptoms like abdominal or pelvic pain, extreme lightheadedness, or shoulder pain.
Persistent or severe vomiting. Vomiting, along with nausea, can be a completely normal first trimester symptom. It’s more commonly known as “morning sickness,” but it doesn’t necessarily appear only in the morning! If, however, your morning sickness is severe (and it’s combined with other symptoms like dizziness or bloody vomit), it may be a rare condition called hyperemesis gravidarum, which requires medical attention. After the first trimester, if you experience vomiting, consult your healthcare provider to rule out anything serious and to treat the nausea.
Urge to pee or burning sensation while you urinate. If you feel an increased urge to pee, but find only a few drops come out, or if you have a burning sensation while you urinate, it may be a sign of a urinary tract infection (UTI). Other symptoms of a UTI can include fever, chills, or blood-tinged urine. Your provider will be able to diagnose your symptoms and treat the bacterial infection to avoid complications. Keep in mind that frequent urination on its own is a common pregnancy symptom during the first trimester and later on in pregnancy, as your baby grows and presses on your bladder.
Dizziness or faintness. Feeling lightheaded can be a normal symptom early in your second trimester. You might also feel dizzy later during pregnancy due to things like circulation problems or low blood sugar levels. However, if this feeling of dizziness persists; if you feel faint or actually do faint; or if your dizziness is combined with other symptoms like blurred vision, vaginal bleeding, headaches, or pain in your abdomen; consult your healthcare provider so that a cause can be identified and treated.
Lower abdominal pain. It’s natural to wonder about abdominal pain during your pregnancy. Keep in mind that discomfort associated with round ligament pain, for example, may be perfectly normal. This will feel like a dull ache or sharp pain on either side of your belly, most noticeable when you cough or sneeze. However, abdominal pain, possibly accompanied by fever or chills, may be a sign that there’s something wrong. In this case, it’s best to contact your healthcare provider.
Racing heart. It’s normal for your heart to beat faster during pregnancy. In fact, your heart pumps up to 30 to 50 percent more blood when you’re pregnant compared to when you’re not pregnant. This is so that your baby receives the appropriate amount of oxygen and nutrients through the placenta. However, if you feel that your heart rate is staying elevated and/or you have shortness of breath, contact your healthcare provider right away.
Severe headache. Headaches during pregnancy can be caused by many factors, including hormonal changes, stress, and fatigue. However, if your headache feels severe, it may be a sign of high blood pressure or the high blood pressure disorder called preeclampsia, which is a serious condition that can occur after 20 weeks of pregnancy or even after childbirth. It requires medical treatment to protect your health and the health of your baby.
Changes in eyesight. Changes in vision, such as temporary loss of vision, blurred vision, or light sensitivity, may be linked to complications like gestational hypertension or preeclampsia.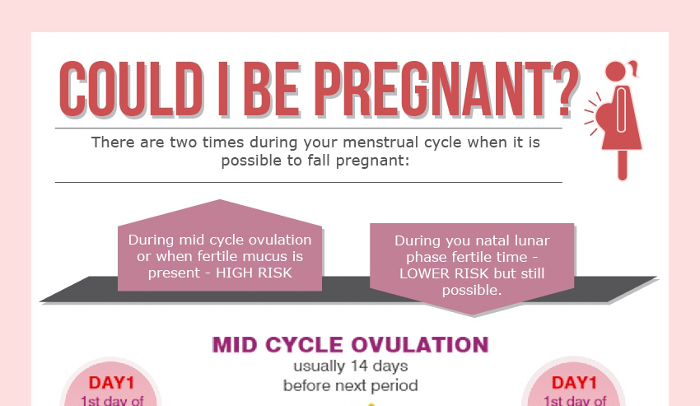
Unusual weight gain, and swelling or puffiness. Sudden, large weight gain (not related to overeating!) is linked to the possibility of preeclampsia. You may notice this weight gain is combined with swelling (edema) of the face and hands. Remember, some swelling of your feet or hands may be normal but should be monitored.
Severe pain above the stomach, under the rib cage. Stomach pain during your pregnancy (especially if it's combined with other symptoms like blurred vision, severe headaches, or nausea) may be a sign of high blood pressure and an associated condition called preeclampsia, mentioned above. Your healthcare provider will monitor your blood pressure during prenatal visits, but if you notice any of the signs of preeclampsia, then contact your provider right away.
Vaginal discharge. You’ll experience more vaginal discharge than you did before you were pregnant. This is usually a sticky, clear, or white discharge caused by changes in your vagina and cervix. However, you could be experiencing a vaginal infection if the color is not clear or white; if it has a bad odor; and if it is accompanied by pain, soreness, or itching. Reach out to your healthcare provider for diagnosis and treatment.
However, you could be experiencing a vaginal infection if the color is not clear or white; if it has a bad odor; and if it is accompanied by pain, soreness, or itching. Reach out to your healthcare provider for diagnosis and treatment.
Lower back pain. It’s normal to experience lower back pain in the later months of your pregnancy. After all, your body is getting closer to delivery, and the ligaments in your pelvis are loosening in order to make the passage of your baby easier. Sciatica can also cause pain in the lower back as your growing uterus puts pressure on your sciatic nerve. In this case, you may feel pain in your lower back, hip, and back of the leg. If you’re also experiencing numb feet or weakness in your leg, or you have severe pain in your calf, contact your healthcare provider.
Feeling your baby move less often. Women often begin to feel the baby fluttering, kicking, or turning sometime between 18 to 25 weeks of pregnancy. Once you’re well into the third trimester, your provider may ask you to monitor your baby's movements by tracking how long it takes to feel 10 kicks, rolls, or flutters. It may take only a few minutes, but if an hour passes without any movement, eat a light snack, lie back down, and try again. You can keep track of these movements in a notebook. If you notice an absence of movement or if your baby isn’t moving as much as usual over several days, call your healthcare provider to double-check everything is progressing well.
Once you’re well into the third trimester, your provider may ask you to monitor your baby's movements by tracking how long it takes to feel 10 kicks, rolls, or flutters. It may take only a few minutes, but if an hour passes without any movement, eat a light snack, lie back down, and try again. You can keep track of these movements in a notebook. If you notice an absence of movement or if your baby isn’t moving as much as usual over several days, call your healthcare provider to double-check everything is progressing well.
Vaginal bleeding. Bleeding during your third trimester can become serious, which is why it’s very important to let your healthcare provider know right away. Bleeding can be a sign of placenta previa, which is when the placenta covers the cervix, or placental abruption, which is when the placenta begins to separate from the wall of the uterus.
Itching all over. Intense itching that isn’t paired with a rash may be a condition commonly known as cholestasis of pregnancy, which is a liver condition that can occur in late pregnancy. Contact your healthcare provider right away if you notice an extreme itchy feeling. Remember, having itchy skin during pregnancy can also be completely normal. This is because as your baby grows, your skin stretches; as your skin stretches it can also become dry, causing areas like your belly, breasts, and thighs to itch.
Contact your healthcare provider right away if you notice an extreme itchy feeling. Remember, having itchy skin during pregnancy can also be completely normal. This is because as your baby grows, your skin stretches; as your skin stretches it can also become dry, causing areas like your belly, breasts, and thighs to itch.
Preterm (before the end of 37 weeks of pregnancy) uterine contractions. These sensations can be perfectly normal Braxton Hicks practice contractions; however, if your contractions persist (i.e., don’t stop when you move or change positions) and become painful or regular, it may be a sign you are in preterm labor. In this case, it’s very important to contact your healthcare provider right away.
Gush or trickle of fluid from your vagina (before the end of 37 weeks of pregnancy). Premature rupture of membranes, also known as your “water breaking,” can show up as a trickle, as steady leaking, or as a gush of fluid from your vagina before your pregnancy is full term. Call your healthcare provider right away if you notice this. Once you’re full term, your water breaking is a sign that labor has started.
Call your healthcare provider right away if you notice this. Once you’re full term, your water breaking is a sign that labor has started.
Vaginal spotting or discharge (between weeks 37 and 40 of pregnancy). You may experience light spotting or a pink or slightly bloody discharge. This may be an early sign of labor, indicating that the cervix has started to dilate and the mucus plug that sealed it off has begun to loosen. If the bleeding is very heavy, however, contact your healthcare provider right away.
Remember, some of these symptoms may be normal symptoms of pregnancy, but they may also be signs of something more serious. Contact your healthcare provider for appropriate guidance.
If you’re in any doubt or you just don’t feel right, it’s always better to consult your provider. This way, you won't worry, and if a problem does exist, it can be taken care of immediately.
Use our Pregnancy Calendar to track your pregnancy week by week.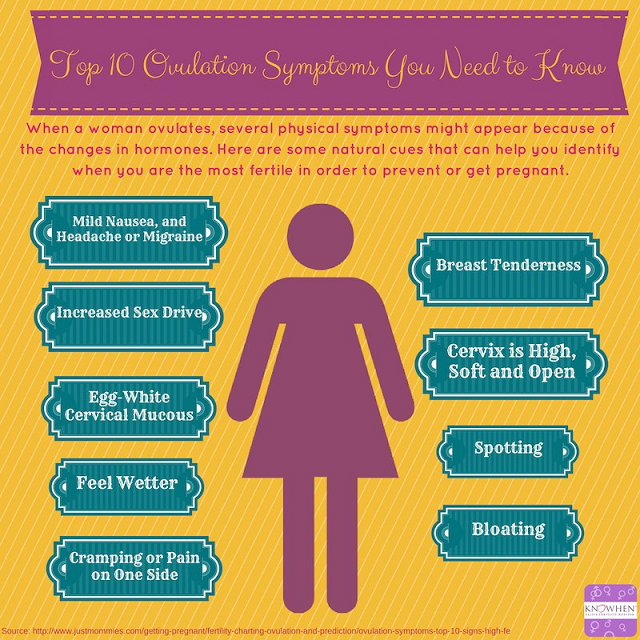 You might also like to start thinking about establishing a birth plan by using our downloadable guide.
To get ready for the arrival of your little one, download the Pampers Club app to start earning rewards for all the diapers and wipes you’ll be purchasing.
You might also like to start thinking about establishing a birth plan by using our downloadable guide.
To get ready for the arrival of your little one, download the Pampers Club app to start earning rewards for all the diapers and wipes you’ll be purchasing.
Warning signs during pregnancy | Pregnancy Birth and Baby
Warning signs during pregnancy | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Pregnancy is a time of great change for your body, and in your life, as you get ready for your baby to arrive. It also can be a time when you may be worried about some of the changes you are experiencing, and you want to know when you should seek help.
Most changes in your body are likely to be a normal part of pregnancy. Most pregnancy health issues are mild and common. However, some signs can indicate that things may not be going well, and could point to a more serious pregnancy complication.
However, some signs can indicate that things may not be going well, and could point to a more serious pregnancy complication.
Some of these symptoms may appear at different stages of your pregnancy; others might occur at any time. Even if you are not sure about your symptoms but think that something just doesn't feel right with your own or your baby's health, it's important to get it checked out.
Contact your doctor, midwife or hospital immediately if you have any of the following symptoms:
Any time during pregnancy
While some signs may only appear at certain times during your pregnancy, many can occur at any stage, including:
- prolonged or severe vomiting
- bleeding from your vagina
- a discharge from your vagina that is unusual, or a lot more than usual
- severe or long-lasting headaches
- dizziness
- continuing weight loss
- fever or chills
- urgency, pain or a burning feeling when urinating (weeing)
- feeling constantly out of breath, dizzy or weak or having a racing heart
- you have had a blow to your stomach (such as from a fall, crash or a family violence incident)
- you are experiencing problems with your emotional health that last longer than 2 weeks, such as feeling depressed, anxious or being unable to do your usual, everyday tasks
Early pregnancy (before 20 weeks)
Certain types of pain in the early stages of pregnancy could be a sign of miscarriage or an ectopic pregnancy:
- persistent or severe pain on one side of your abdomen or pain in the tip of one shoulder
- severe pain or cramping in your lower abdomen (tummy)
Later pregnancy (after 20 weeks)
Although some discomfort is common during the later stages of pregnancy, some signs need to be checked by a doctor immediately, including:
- changes to your vision, flashing lights or blurry eyesight, which are signs of pre-eclampsia
- sudden, severe swelling in your hands, feet or face
- an extreme itchiness of your skin, including hands and feet
- a large amount of swelling in your legs (which is also painful)
- if your baby has stopped moving or is moving differently
What happens next?
When you see your healthcare professional, they may perform some tests to check or maintain the health of you and your baby. These tests may include:
These tests may include:
- a health assessment and investigation
- an ultrasound or blood test
You may also receive a referral to another doctor or specialist, and you can also get emotional support.
How can I avoid pregnancy complications?
It's often not possible to avoid a complication in pregnancy. You may have a higher chance of developing one if you have a health problem before conception, or had one during a previous pregnancy. There may also be a higher chance if you have a family history of pregnancy complications.
It may be possible to lessen the chance of developing a problem, or reduce the chance of a complication becoming worse, by making sure you go to all of your antenatal appointments. If a potential health issue is found, you may need additional antenatal appointments to more closely monitor the health of you and your baby.
Where to get help
- Phone your doctor, midwife or maternity hospital urgently if you have any concerns.

- Visit your hospital or call triple zero (000) and ask for an ambulance.
Other sources of advice
- Call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
- Consider visiting healthdirect's Symptom Checker for pregnancy if you are experiencing discomfort in pregnancy or are worried about any symptoms.
Sources:
NSW Health (Early pregnancy – when things go wrong), BabyCenter (Pregnancy symptoms you should never ignore), Raising Children Network (Health problems in pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Need more information?
Early pregnancy: when things go wrong - Maternal, child and family health
Early pregnancy – when things go wrong is a resource that offers expert advice and support to women experiencing complications in early pregnancy.
Read more on NSW Health website
What is a stillbirth?
The cause of a stillbirth is often unknown, but you can help to lower the risk. Learn about prevention, warning signs and giving birth to a stillborn baby here.
Read more on Pregnancy, Birth & Baby website
Pregnancy: premature labour & birth | Raising Children Network
Are you likely to be having a premature birth? Here’s all you need to know about preparing for and recovering from premature labour and birth.
Read more on raisingchildren.net.au website
Premature babies and birth | Raising Children Network
Premature babies are born before 37 weeks of pregnancy. Our essential guide covers premature birth, babies, development, NICU and more.
Our essential guide covers premature birth, babies, development, NICU and more.
Read more on raisingchildren.net.au website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Bleeding or pain in early pregnancy
One in 4 women will experience bleeding and/or pain during their first 12 weeks of pregnancy. Unfortunately half of these pregnancies may also end in miscarriage, which cannot be prevented.
Read more on WA Health website
What really happens during a miscarriage
Understand what actually happens during a miscarriage and what you might see and feel. Please be warned that this article contains some graphic descriptions.
Please be warned that this article contains some graphic descriptions.
Read more on Pregnancy, Birth & Baby website
Stillbirth and neonatal death | Raising Children Network
Information about pregnancy loss, stillbirth and neonatal death, including grief and getting support.
Read more on raisingchildren.net.au website
Pregnancy - preeclampsia - Better Health Channel
There is no evidence that preeclampsia is caused by emotional stress, working too hard or not getting enough rest.
Read more on Better Health Channel website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
After how many meters prohibition signs begin to operate
Unfortunately, the existence of such a zone of adaptation to the sign is nothing more than a myth. In fact, the action of the prohibition sign begins immediately after it, that is, if you drive at least a couple of centimeters after the 60 km / h sign at a speed of 81 km / h or more, the driver can already be fined.
How the speed limit violation cameras are configured is another matter. First of all, a violation can be recorded as soon as the offending vehicle enters the field of view of the radar and / or video camera. Moreover, it will not necessarily be a complex installed in the direction of travel. Cameras that read rear license plates are also quite common. Therefore, in fact - when the intruder was in the field of view of the camera - from this moment the process of fixing the violation begins.
It is not so important what type of violation fixing is used. For example, the "Avtohuragan" complex calculates the speed of an object using the video image method, analyzing the measurement of the parameters of the observed object in the frame. Or, say, the "Kordon" radar complex during fixing simultaneously recognizes the number of the car, determines its coordinates and calculates the speed.
Another important issue that causes controversy is how long a speed limit sign lasts. According to the legislation, the sign will last:
According to the legislation, the sign will last:
1) Until the next delimiter.
2) To the end of the settlement.
3) To the nearest road intersection.
In the latter case, it should be taken into account that exits from adjacent territories, as well as junctions of unpaved dirt roads, are not considered intersections. In addition, the beginning of the settlement limits the zone of action of the sign. This is a plate 5.23 with the name of a city or town on a white background. After it, the speed limit of 60 km / h begins.
If the speed limit sign is temporary, then again, contrary to popular belief, the driver should slow down ahead of time. Moreover, temporary signs have a special status. In case of their contradiction between hospital and th signs, it is necessary to focus on temporary ones.
It should also be taken into account that temporary speed limit signs are valid until cancellation signs 3.21, which are also made on a yellow background.
At the same time, the corresponding signs on a white background (that is, stationary) also cancel the effect of temporary prohibition signs. And, by the way, the installation of traffic police cars with equipment for photo and video recording of violations in areas where the speed of movement is temporarily limited, contrary to popular belief, is not prohibited, as well as fixing violations in this area in manual mode by a traffic police officer.
A special case should be considered the situation with the passage of signs, where under the designation of the speed limit there are white plates indicating the length of the neutral zone. It can be, for example, the numbers 100 or 200. In this case, the driver has the appropriate number of meters in stock to slow down. As a rule, after such delayed speed limit zones, additional speed limit signs are installed.
We add that if the driver did not notice the speed limiting sign due to a tree covering it or, for example, a truck passing by, then the fact of imposing a fine can then be challenged in court by providing the appropriate video confirmation.
Sports during pregnancy
Russian
In Attesa
Benefits of sports and advice on choosing exercise during pregnancy
It is well known that regular exercise improves physical and mental well-being at all ages and in all stages of life, including during pregnancy and after childbirth. With greater motivation and more frequent medical check-ups, pregnancy can provide an opportunity to maintain or improve your lifestyle and develop good habits (such as eating healthy and not smoking), taking care of yourself and the baby in the womb.
Benefits of exercise during pregnancy
Experimental and randomized studies, as well as a recent review of the literature on the subject, have shown that exercise during pregnancy can:
- Reduce the risk of gestational diabetes
- Reduce the likelihood of excessive weight gain
- Guarantee a lower incidence of gestational hypertension or pre-eclampsia
- Reduce the rate of preterm birth, caesarean section
- Reduce the likelihood of low birth weight and complications associated with pregnancy
- Improve recovery and reduce the risk of postpartum depression
- Reduce the incidence of back pain and sciatica during pregnancy.

What sports should I do while pregnant?
Exercise during pregnancy is associated with minimal risk, but a visit to the doctor is necessary for an in-depth obstetric examination and the elimination of contraindications and complications. In addition, for the safety of both mother and child, it is important that the proposed exercise schedule be personalized based on the athletic performance of each individual patient, as well as physical and anatomical changes that occur during pregnancy, such as weight gain and a shift in the center of gravity. , as well as changes in the lungs and cardiovascular system.
Sedentary women should follow a gradual exercise schedule during pregnancy. Women who were already active before pregnancy can engage in high-intensity activities such as running or aerobic exercise. Professional athletes can continue training under the close supervision of a gynecologist and sports trainer, tracking changes in weight, diet and exercise types. The latest US guidelines recommend at least 150 minutes of moderate-intensity aerobic activity per week during pregnancy and postpartum (aerobic exercise for 30-90 minutes 3-4 times a week is not associated with the risk of preterm pregnancy).
The latest US guidelines recommend at least 150 minutes of moderate-intensity aerobic activity per week during pregnancy and postpartum (aerobic exercise for 30-90 minutes 3-4 times a week is not associated with the risk of preterm pregnancy).
Activities and sports during pregnancy
Here are the preferred and recommended sports for pregnant women:
- Walking
- Exercise bike
- Aerobics
- Dancing
- Hydrotherapy, water aerobics, swimming
- Exercises with resistance (e.g. weights or bands)
- Stretching
Here are some general tips for safe training:
- Keeping your body hydrated
- Balanced, varied and healthy diet
- Suitable clothing and footwear
- Avoidance of hot and poorly ventilated areas
- Avoiding the supine position for extended periods, especially in the last trimester
What to avoid during pregnancy and what to look out for
Contact sports should be avoided throughout pregnancy due to the risk of abdominal injury and loss of balance, as well as scuba diving due to the risk of blistering in the fetal and placental circulation.