Symptoms of an incomplete miscarriage
Incomplete miscarriage | Tommy's
An incomplete miscarriage is when a miscarriage begins, but the pregnancy doesn’t completely come away from the womb.
What is an incomplete miscarriage?
Sometimes not all of the pregnancy comes away after a miscarriage. An incomplete miscarriage is when a miscarriage begins, but some pregnancy tissue stays in the womb.
Signs of an incomplete miscarriage
All women have some bleeding or pain during and after a miscarriage. But if you have an incomplete miscarriage, you may have these symptoms:
- heavy bleeding – get medical help if you’re soaking through a pad in an hour
- bleeding that carries on and doesn’t settle down
- passing blood clots
- increasing tummy pain, which may feel like cramps or contractions
- a raised temperature (fever) and flu-like symptoms.
Get medical help straightaway if you experience any of these warning signs.
Treatment for an incomplete miscarriage
If you have an incomplete miscarriage, you’ll need to have treatment. There are 3 options available:
- waiting for the miscarriage to happen by itself naturally (expectant management)
- taking medicine to help things along (medical management)
- having surgery to remove the pregnancy (surgical management).
Your doctor should talk with you about what may be the best option for you. You should be given some time for the diagnosis to sink in and to think about what you want to do.
“It's OK to take your time over making a decision. You may have a gut feeling about how to manage the miscarriage, you may not. Talk through your options with the medical professionals. I know they are incredibly busy, but we needed and wanted answers. I phoned the number we were given after our second missed miscarriage and asked all the questions I had. This helped us make a decision.”
Catherine
How you are treated is your choice. However, you may be advised to have surgery immediately if there are any problems, such as infections.
Find out more about how your miscarriage will be managed.
Your emotional health
Miscarriage can be devastating. You may be struggling with grief, anxiety and shock, but you do not need to go through this alone. There are lots of organisations that can provide advice and support.
If you’re worried that you or your partner are struggling to cope after losing a baby, please talk to your GP. They will be able to help you get the support you need.
You can also talk to a Tommy’s midwife for free. You can call them Monday-Friday, 9am-5pm on 0800 0147 800 or you can email them at [email protected]. Our midwives are trained in bereavement support so will be able to talk to you about what you’re going through.
Find out more about support after a miscarriage.
Back to top
Miscarriage | Pregnancy Birth and Baby
The loss of a baby through miscarriage can be very distressing. A miscarriage generally occurs for reasons outside your control and nothing can be done to prevent or stop it from happening. Most women who have had a miscarriage will go on to have a healthy pregnancy in the future.
A miscarriage generally occurs for reasons outside your control and nothing can be done to prevent or stop it from happening. Most women who have had a miscarriage will go on to have a healthy pregnancy in the future.
What is a miscarriage?
A miscarriage is the loss of your baby before 20 weeks of pregnancy. The loss of a baby after 20 weeks is called a stillbirth.
Up to 1 in 5 confirmed pregnancies end in miscarriage before 20 weeks, but many other women miscarry without having realised they are pregnant.
Common signs of miscarriage include:
- cramping tummy pain, similar to period pain
- vaginal bleeding
If you think you are having a miscarriage, see your doctor or go to your local emergency department.
Many women experience vaginal spotting in the first trimester that does not result in pregnancy loss.
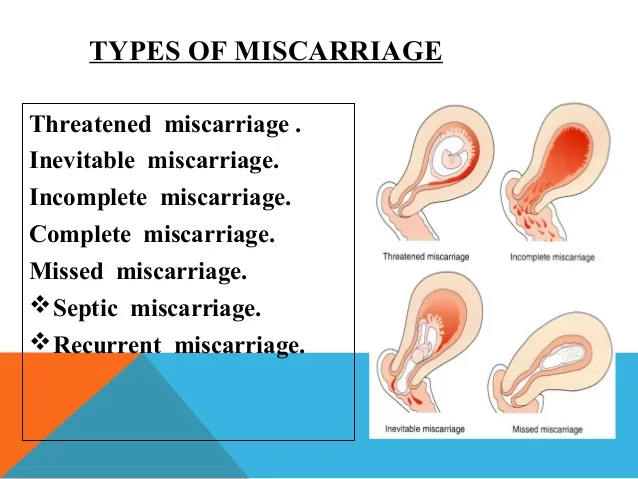
What are the types of miscarriage?
There are several types of miscarriage — threatened, inevitable, complete, incomplete or missed.
Other types of pregnancy loss include an ectopic pregnancy, molar pregnancy and a blighted ovum.
Threatened miscarriage
When your body is showing signs that you might miscarry, that is called a 'threatened miscarriage'. You may have light vaginal bleeding or lower abdominal pain. It can last days or weeks and the cervix is still closed.
The pain and bleeding may resolve and you can go on to have a healthy pregnancy and baby. Or things may get worse and you go on to have a miscarriage.
There is rarely anything a doctor, midwife or you can do to prevent a miscarriage. In the past bed rest was recommended, but there is no scientific proof that this helps at this stage.
Inevitable miscarriage
Inevitable miscarriages can come after a threatened miscarriage or without warning. There is usually a lot more vaginal bleeding and strong lower stomach cramps. During the miscarriage your cervix opens and the developing fetus will come away in the bleeding.
Complete miscarriage
A complete miscarriage has taken place when all the pregnancy tissue has left your uterus. Vaginal bleeding may continue for several days. Cramping pain much like labour or strong period pain is common — this is the uterus contracting to empty.
If you have miscarried at home or somewhere else with no health workers present, you should have a check-up with a doctor or midwife to make sure the miscarriage is complete.
Incomplete miscarriage
Sometimes, some pregnancy tissue will remain in the uterus. Vaginal bleeding and lower abdominal cramping may continue as the uterus continues trying to empty itself. This is known as an 'incomplete miscarriage'.
Your doctor or midwife will need to assess whether or not a short procedure called a ‘dilatation of the cervix and curettage of the uterus’ (often known as a ‘D&C’) is necessary to remove any remaining pregnancy tissue. This is an important medical procedure done in an operating theatre.
Missed miscarriage
Sometimes, the fetus has died but stayed in the uterus. This is known as a 'missed miscarriage'.
If you have a missed miscarriage, you may have a brownish discharge. Some of the symptoms of pregnancy, such as nausea and tiredness, may have faded. You might have noticed nothing unusual. You may be shocked to have a scan and find the fetus has died.
If this happens, you should discuss treatment and support options with your doctor.
Recurrent miscarriage
A small number of women have repeated miscarriages. If this is your third or more miscarriage in a row, it’s best to discuss this with your doctor who may be able to investigate the causes, and refer you to a specialist.
A miscarriage can occur suddenly or over a number of weeks. The symptoms are usually vaginal bleeding and lower tummy pain. It is important to see your doctor or go to the emergency department if you have signs of a miscarriage.
The most common sign of a miscarriage is vaginal bleeding, which can vary from light red or brown spotting to heavy bleeding. If it is very early in the pregnancy, you may think that you have your period.
If it is very early in the pregnancy, you may think that you have your period.
Other signs may include:
- cramping pain in your lower tummy, which can vary from period-like pain to strong labour-like contractions
- passing fluid from your vagina
- passing of blood clots or pregnancy tissue from your vagina
What really happens during a miscarriage?
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
What should I do if I think I’m having a miscarriage?
If you are concerned that you are having a miscarriage, call your doctor or midwife for advice and support.
Keep in mind that many women experience vaginal spotting in the first trimester of pregnancy that does not result in a miscarriage.
If you are alone, consider calling your partner or a friend for help and support.
If you have very heavy bleeding, strong pain or feel unwell, call triple zero (000) or have someone take you to your nearest emergency department.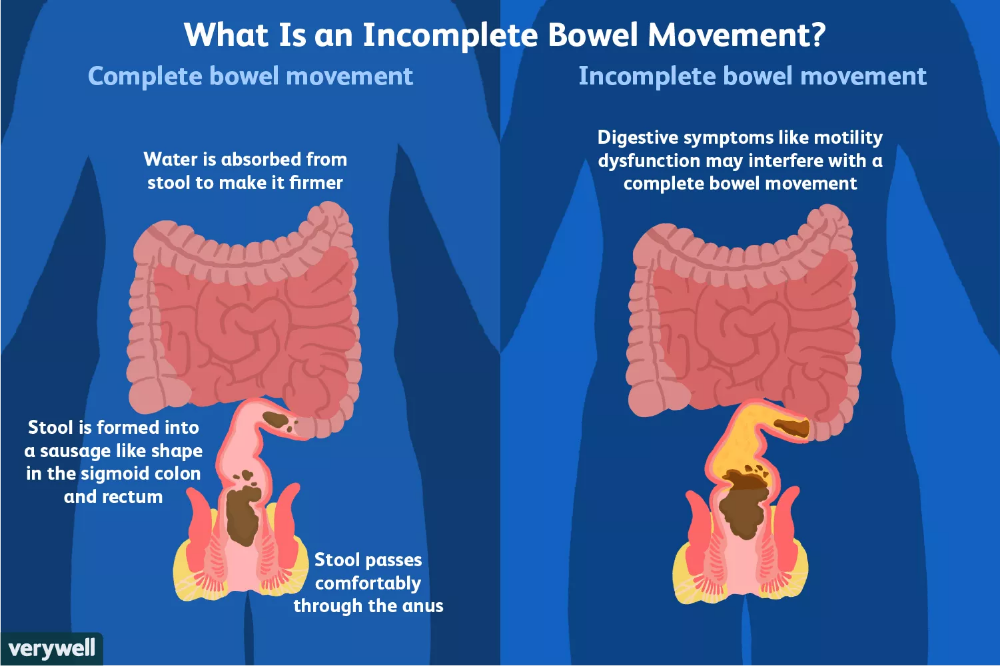
How is a miscarriage managed?
Unfortunately, nothing can prevent a miscarriage from happening once it has begun. What happens now depends on your own health and what is happening to you.
Each approach has benefits and risks. You should discuss these with your doctor.
Expectant or natural management
Also called ‘watch and wait’, expectant management may be recommended in early pregnancy. This involves going home and waiting until the pregnancy tissue has passed from your womb by itself. This can happen quickly, or it may take a few weeks.
Medical management
You may be offered medication that speeds up the passing of the pregnancy tissue. You may be asked to stay in hospital until the tissue has passed, or you may be advised to go home.
Surgical management
You may be advised to have a form of minor surgery called a 'dilatation and curettage' (also called a D&C or a curette). This procedure is often recommended if you have heavy bleeding, significant pain or signs of infection.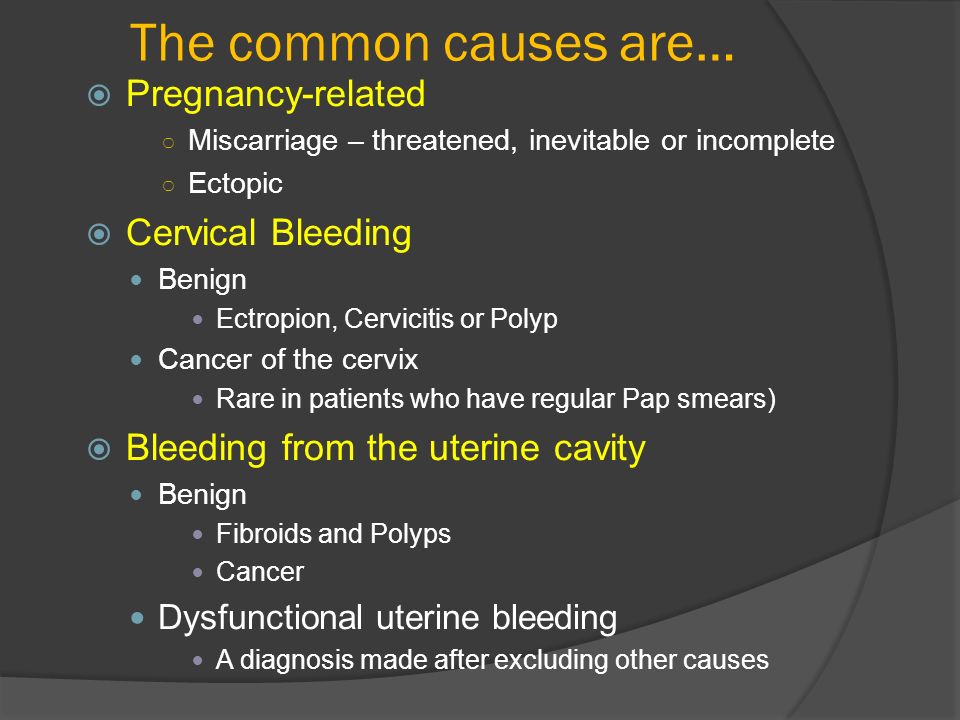 It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
This procedure is done under general anaesthesia in an operating theatre. It takes 5-10 minutes once you are asleep. The doctor opens the cervix and removes the remaining pregnancy tissue.
How is a miscarriage treated?
Once it is confirmed that you are having a miscarriage, your doctor may offer or recommend treatment. There are many options. All have benefits and risks — discuss these with your doctor.
If the miscarriage is complete
If it seems the miscarriage is complete, you should still see your doctor for a check-up. You may be advised to have an ultrasound to make sure your uterus is empty.
If you go to hospital
If you go to your hospital’s emergency department, you will be seen first by a triage nurse, who will assess how urgently you need to be seen by a doctor. Depending on your symptoms, you will either be taken in to see a doctor immediately, or you will be asked to wait.
If you are waiting to be seen and your symptoms become worse or you feel like you need to go to the toilet, let the staff know immediately.
What happens if I miscarry at home?
Some women miscarry at home before they have a chance to see their doctor or get to the hospital.
If this happens, then:
- use pads to manage the bleeding
- if you can, save any pregnancy tissue that you pass, as your doctor may recommend it is tested to see why your miscarriage happened
- take medications such as paracetamol if you have pain
- rest
- call your doctor or midwife
There is a chance you may see your baby in the tissue that you pass, but often the baby is too small to recognise, or may not be found at all. It is normal to want to look at the remains, but you may decide you do not want to. There is no right or wrong thing to do.
Some women miscarry while on the toilet. This can also happen if you are out and about, or in hospital. There is no right or wrong way to handle this.
There is no right or wrong way to handle this.
Why do miscarriages happen?
Many women wonder if their miscarriage was their fault. In most cases, a miscarriage has nothing to do with anything you have or have not done. There is no evidence that exercising, stress, working or having sex causes a miscarriage.
Most parents do not ever find out the exact cause. However, it is known that miscarriages often happen because the baby fails to develop properly, usually due to a chromosomal abnormality that was spontaneous, not inherited.
Occasionally, miscarriage is caused by:
- hormonal abnormalities
- immune system and blood clotting problems
- medical conditions such as thyroid problems or diabetes
- severe infections causing high fevers (not common colds)
- physical problems with your womb or cervix
What are the risk factors for miscarriage?
Women are more likely to have miscarriages if they:
- are older
- smoke
- drink alcohol in the first trimester
- drink too much caffeine in coffee, tea or energy drinks
- have had several previous miscarriages
Can you prevent a miscarriage?
Living healthily — no cigarettes, no alcohol and little to no caffeine — can decrease your risk of miscarriage. It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
Who can I talk to for advice and support?
Talk to your doctor or midwife for information and advice on what do and how to look after yourself if you experience a miscarriage.
Your hospital should be able to provide details of available support services, such as bereavement support.
SANDS is an independent organisation that provides support for miscarriage, stillbirth and newborn death. You can call them on 1300 072 637 or visit www.sands.org.au.
You can also call Pregnancy, Birth and Baby on 1800 882 436, 7am to midnight (AET) to speak to a maternal child health nurse for advice and emotional support.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Incomplete abortion - causes, symptoms, diagnosis and treatment
Incomplete abortion - retention of the fetus or its membranes in the uterine cavity during spontaneous or induced abortion for up to 22 weeks. It is manifested by pulling or intense cramping pain in the lower abdomen, bloody vaginal discharge, in which fragments of the fetal egg may be present. To make a diagnosis, they use an examination on a chair, ultrasound of the uterus, if necessary, prescribe laboratory tests and hysteroscopy. The patient management plan involves the removal of residual abortive material by vacuum aspiration or curettage of the uterine cavity, followed by the appointment of uterotonics, antibiotics, and infusion therapy.
General information
According to studies in the field of obstetrics and gynecology, from 1 to 5% of spontaneous miscarriages, instrumental or drug interruptions of gestation end in incomplete abortion. At this stage, it is not possible to save the fetus, since it has already died.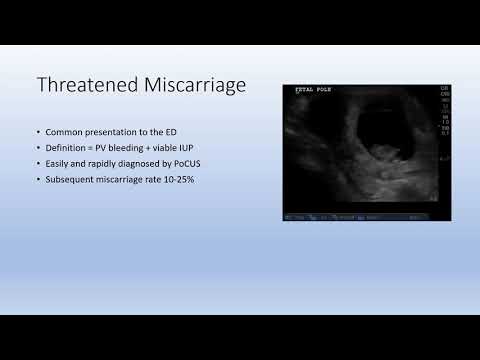 The main task of the doctor when such a pathology is detected is the rapid correction of disorders to exclude possible complications and eliminate threats to the patient's reproductive health. More often, incomplete spontaneous abortion is diagnosed in women over 35 years of age with genital and extragenital pathology. Incomplete induced abortion with late development of clinical symptoms can occur in a patient of any age with a pharmacological method of abortion.
The main task of the doctor when such a pathology is detected is the rapid correction of disorders to exclude possible complications and eliminate threats to the patient's reproductive health. More often, incomplete spontaneous abortion is diagnosed in women over 35 years of age with genital and extragenital pathology. Incomplete induced abortion with late development of clinical symptoms can occur in a patient of any age with a pharmacological method of abortion.
Incomplete abortion
Causes of incomplete abortion
Incomplete is both spontaneous and artificial termination of pregnancy in the early stages. Usually, the complete discharge of the remains of the fetal egg is prevented by the anatomical features of the uterus, insufficient opening of its neck, the presence of a connection between parts of the fetus or its membranes with the uterine wall. The immediate causes of an incomplete abortion are:
- Medical abortion . In most cases, incomplete abortion is observed when taking medications in the early stages of gestation.
 Despite the low invasiveness of the technique, in some patients there is a violation of the contractility of the myometrium and insufficient opening of the cervical canal.
Despite the low invasiveness of the technique, in some patients there is a violation of the contractility of the myometrium and insufficient opening of the cervical canal. - Improper surgical abortion . Part of the fetal egg remains attached to the wall of the uterus when the operation is performed by an inexperienced obstetrician-gynecologist or in the absence of ultrasound guidance before or after the intervention to terminate the pregnancy. The risk of incomplete expulsion of abortive material increases with criminal operations.
- Dishormonal conditions . The degree of cervical opening, the strength and rhythm of myometrial contractions are hormonally regulated. With an imbalance of estrogens, prostaglandins, oxytocin, progesterone, and other mediators, the contractile activity of the muscle layer becomes insufficient for the complete expulsion of the fetal egg.
- Anomalies in the structure of the uterus . In rare cases, anatomical features such as a bicornuate or saddle uterus, submucosal fibroids in the isthmus area are obstacles to the free expulsion of a rejected ovum.
 With hypoplasia of the organ, insufficient contractile activity of its muscles is noted.
With hypoplasia of the organ, insufficient contractile activity of its muscles is noted.
The risk group for the possibility of incomplete abortion are patients with impaired secretion of female sex hormones (polycystic ovaries, depletion or resection of ovarian tissue), extragenital somatic and endocrine pathology (diabetes mellitus, hypothyroidism, adrenal diseases), obesity. The likelihood of incomplete abortion is also increased in women with chronic specific and nonspecific endometritis, abortions and diagnostic curettage.
Pathogenesis
The mechanism of development of incomplete abortion and the formation of its clinical picture is common, despite the difference in etiological factors. Partial separation of the ovum due to technical errors or insufficient contractile activity of the myometrium under the implantation site of the embryo, retention of its parts in the uterus due to the presence of mechanical obstacles (myomatous node, closed cervical canal, etc.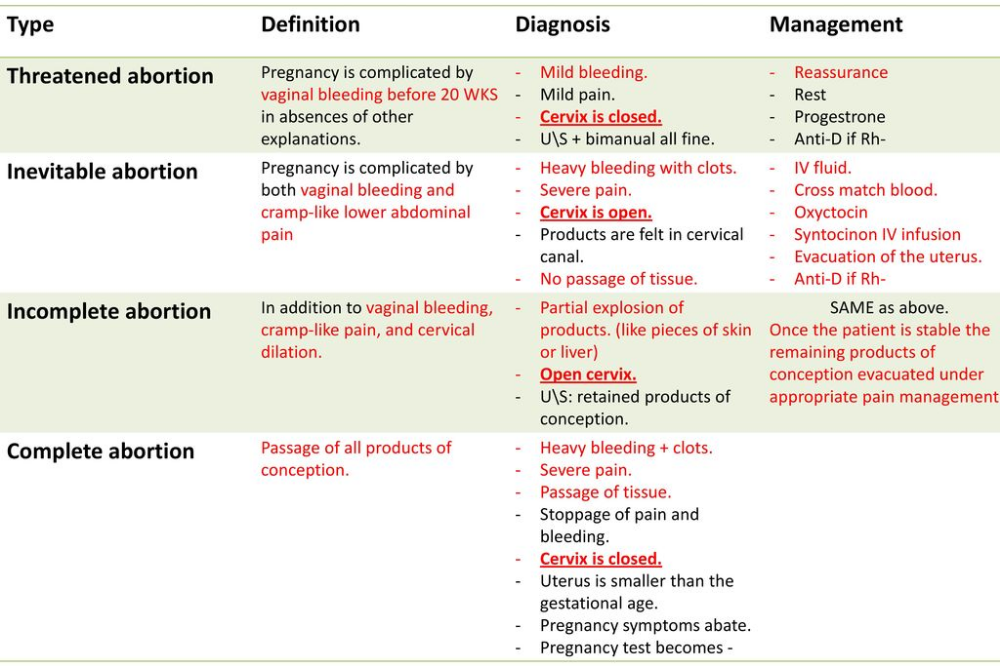 ) makes it impossible to adequately contract the organ wall. As a result, bleeding from gaping vessels continues, characteristic pain occurs and a nutrient substrate is formed for possible infection.
) makes it impossible to adequately contract the organ wall. As a result, bleeding from gaping vessels continues, characteristic pain occurs and a nutrient substrate is formed for possible infection.
Symptoms of incomplete abortion
The clinical picture of the disorder is a continuation of the symptoms of spontaneous miscarriage in the course or gradually develops within a few hours after surgical abortion. With drug interruption of gestation, pathological signs may appear several days and even weeks after taking the medication. An incomplete abortion is manifested by intense cramping pains in the lower abdomen, often radiating to the lower back and sacrum, as well as profuse uterine bleeding with the possible presence of fragments of abortive material in the secretions. Rarely, the pain is excruciating in nature. The appearance of a sharp putrid odor of vaginal discharge, an increase in body temperature to 37.5-38.0 ° C and above indicate the accession of infection. When the pathology worsens, the patients complain of weakness, dizziness, fainting.
When the pathology worsens, the patients complain of weakness, dizziness, fainting.
Complications
In case of late diagnosis, incomplete abortion is complicated by profuse uterine bleeding, hematometra, infection of the abortive material. At first, the inflammation is local in nature and is manifested by the clinical picture of acute endometritis. Subsequently, a generalization of the process is possible with the involvement of the uterine appendages (acute salpingitis or adnexitis), the pelvic peritoneum (pelvioperitonitis), and sepsis. Long-term consequences of an incomplete abortion are chronic inflammatory diseases of the pelvic organs, isthmic-cervical insufficiency, recurrent miscarriage, and infertility. If fragments of the chorion remain in the uterine wall, a placental polyp may form from them in the future, accompanied by heavy and prolonged menstrual bleeding.
Diagnosis
If an incomplete abortion is suspected, tests are prescribed to determine the presence of abortive material in the uterus, confirm the termination of pregnancy, and establish possible causes. For timely detection of complications, monitoring of temperature, heart rate and blood pressure is provided. The most informative in terms of diagnostics are:
For timely detection of complications, monitoring of temperature, heart rate and blood pressure is provided. The most informative in terms of diagnostics are:
- Gynecological examination . During examination, blood clots are found in the mirrors in the vagina, sometimes - abortive material. The cervix is smoothed, blood is released from its canal. On bimanual palpation, the uterus is enlarged, soft, painful. The internal os is ajar or completely open.
- Ultrasound of the uterus . The size of the organ is less than the estimated gestational age. In the cavity, a deformed fetal egg or amorphous inclusions of different sizes, shapes and echogenicity are determined. The fetus shows no signs of life. It is possible to detect anatomical abnormalities.
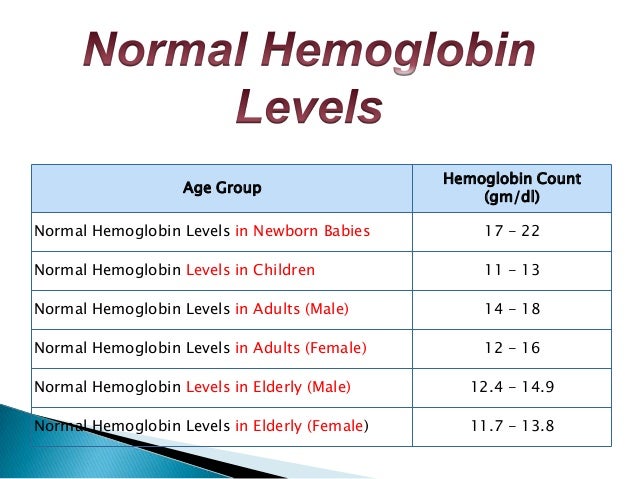
Usually a typical clinical presentation with characteristic ultrasound findings is sufficient to make a diagnosis. In doubtful cases, laboratory methods are prescribed to confirm the interruption of gestation (colpocytology with an assessment of the karyopyknotic index, determination of the levels of chorionic gonadotropin, estradiol, progesterone).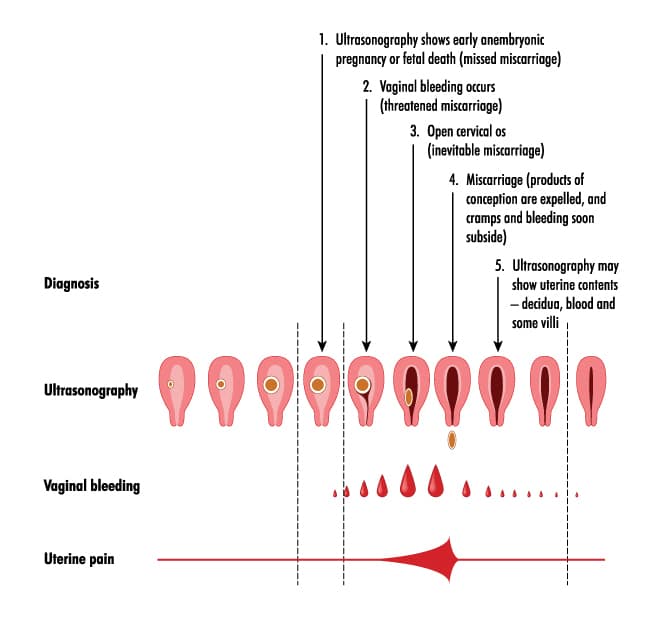 To exclude infectious and hemorrhagic complications, a complete blood count and hemostasis indicators are monitored. Differential diagnosis is carried out with a completed abortion, ectopic pregnancy, missed miscarriage. If necessary, an anesthesiologist-resuscitator, an infectious disease specialist, a hematologist are involved in the examination of the patient.
To exclude infectious and hemorrhagic complications, a complete blood count and hemostasis indicators are monitored. Differential diagnosis is carried out with a completed abortion, ectopic pregnancy, missed miscarriage. If necessary, an anesthesiologist-resuscitator, an infectious disease specialist, a hematologist are involved in the examination of the patient.
Treatment of incomplete abortion
The main tasks are to remove the dead fetus and its parts from the uterine cavity, stop bleeding and prevent possible infectious complications. An attempt to expel the abortive material with uterotonics is, as a rule, rarely effective and only increases the cramping pains. The standard management of a patient with incomplete spontaneous or induced abortion includes the following steps:
- 0004 . To remove the remaining fetal egg, abortsang is used, after which, taking into account the gestational age, vacuum aspiration is performed (up to 12 weeks of pregnancy) or classic curettage of the uterine walls (from 12 weeks onwards).
 Effective management of the patient without a complete cleaning of the uterine cavity is impossible. Hysteroscopy can be used for optical quality control of the intervention.
Effective management of the patient without a complete cleaning of the uterine cavity is impossible. Hysteroscopy can be used for optical quality control of the intervention. - Stopping uterine bleeding . When an incomplete abortion is combined with coagulopathic and hemodynamic disorders, depending on the results of laboratory tests, oxytocin is dripped in Ringer's solution or saline. In exceptional cases, with significant blood loss, hemostatics, transfusion of blood or its components are recommended.
- Antibacterial therapy . The use of broad-spectrum antibiotics is directly indicated for clinical and laboratory signs of an infectious process. For prophylactic purposes, drugs with antimicrobial action are administered with late diagnosis of incomplete discharge of the fetal egg. The course of antibiotic therapy lasts from 7 to 10 days with the simultaneous appointment of eubiotics and antifungal agents.
In the postoperative period, according to indications, non-steroidal anti-inflammatory drugs, iron preparations are used.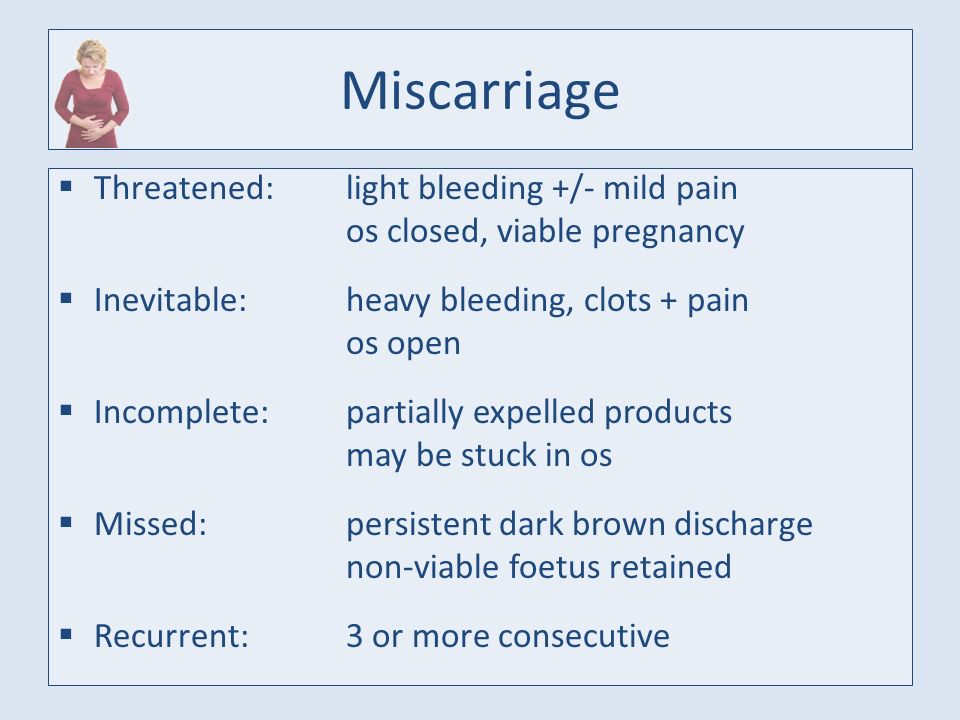 If an incomplete miscarriage or induced abortion is diagnosed in a woman with a negative Rh blood factor, anti-Rh0 (D) immunoglobulin is prescribed. Within 2 weeks after curettage, the patient is recommended to refrain from sexual intercourse, douching, intravaginal administration of tampons, suppositories. In the normal condition of the patient, a follow-up examination is performed after 14 days. An increase in temperature and a deterioration in the general condition are grounds for a more thorough diagnostic search, the appointment of massive antibiotic therapy, and a possible repeated curettage of the uterine cavity. Women with neurotic and subdepressive disorders associated with the unexpected loss of a child are shown mild sedatives, light antidepressants, and psychotherapy.
If an incomplete miscarriage or induced abortion is diagnosed in a woman with a negative Rh blood factor, anti-Rh0 (D) immunoglobulin is prescribed. Within 2 weeks after curettage, the patient is recommended to refrain from sexual intercourse, douching, intravaginal administration of tampons, suppositories. In the normal condition of the patient, a follow-up examination is performed after 14 days. An increase in temperature and a deterioration in the general condition are grounds for a more thorough diagnostic search, the appointment of massive antibiotic therapy, and a possible repeated curettage of the uterine cavity. Women with neurotic and subdepressive disorders associated with the unexpected loss of a child are shown mild sedatives, light antidepressants, and psychotherapy.
Prognosis and prevention
Timely detection of signs of incomplete abortion, adequate treatment can quickly eliminate the symptoms of the disorder and maintain the chances of a normal re-pregnancy in 80-85% of patients. For preventive purposes, women with dyshormonal conditions or anatomical features of the uterus are recommended pregnancy planning, early registration in the antenatal clinic and regular monitoring by an obstetrician-gynecologist. If there is a threat of miscarriage, compliance with the therapeutic and protective regimen and appropriate drug therapy are shown. If the rejection of the fetal egg has occurred, it is necessary to control its complete evacuation from the uterine cavity during ultrasound or hysteroscopy. The control of the discharge of abortive material is especially important after medical interruption of gestation.
For preventive purposes, women with dyshormonal conditions or anatomical features of the uterus are recommended pregnancy planning, early registration in the antenatal clinic and regular monitoring by an obstetrician-gynecologist. If there is a threat of miscarriage, compliance with the therapeutic and protective regimen and appropriate drug therapy are shown. If the rejection of the fetal egg has occurred, it is necessary to control its complete evacuation from the uterine cavity during ultrasound or hysteroscopy. The control of the discharge of abortive material is especially important after medical interruption of gestation.
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy.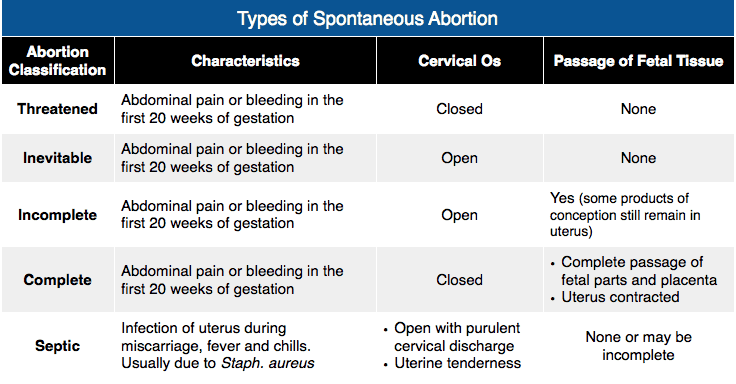 If the pregnancy is terminated in the second half, it is called preterm labor.
If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png)
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy;
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, pulling pains, similar to pain during menstruation.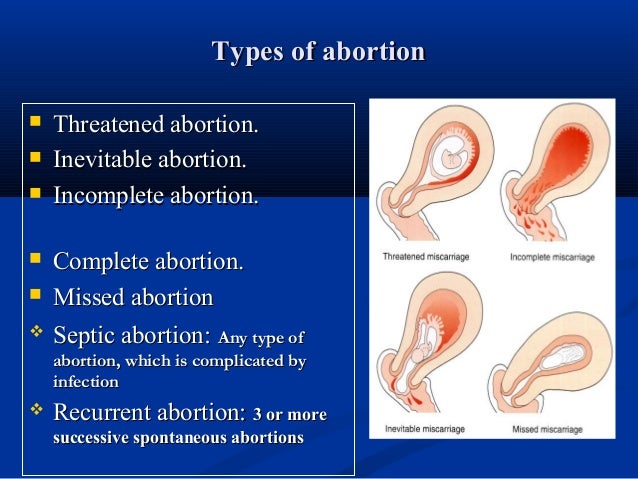 Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the ovum, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization.
Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the ovum, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization.
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin. Pregnancy cannot be saved, cleaning is required;
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a miscarriage, a short break in planning and taking preventive measures is recommended to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them.
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.
2. The second most common cause is disorders in the female genital area: endometritis - inflammation of the uterine mucosa - preventing the implantation of the fetal egg and its development and polycystic ovaries.
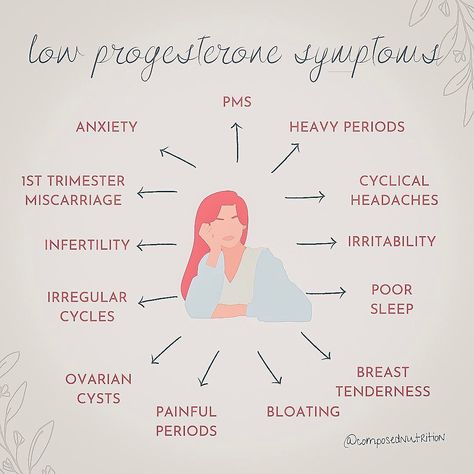
3. Hormonal disorders, namely progesterone deficiency.