Gad and pregnancy
Perinatal Generalized Anxiety Disorder: Assessment and Treatment
1. Freud S. Inhibitions, symptoms and anxiety. In: Strachey J, eds. The standard edition of the complete psychological works of Sigmund Freud, volume 2 London: Hogarth Press, 1959:77–174 [Google Scholar]
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed., text rev. (DSM-IV-TR). Arlington, VA: American Psychiatric Association, 2000 [Google Scholar]
3. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed. (DSM-5). Arlington, VA: American Psychiatric Association, 2013 [Google Scholar]
4. Adewuya AO, Ola BA, Aloba OO, Mapayi BM. Anxiety disorders among Nigerian women in late pregnancy: A controlled study. Arch Womens Ment Health 2006;9:325–328 [PubMed] [Google Scholar]
5. Buist A, Gotman N. Generalized anxiety disorder: Course and risk factors in pregnancy. J Affect Disord 2011;131:277–283 [PMC free article] [PubMed] [Google Scholar]
6. Sutter-Dallay AL, Giaconne-Marcesche V, Glatigny-Dallay E, Verdoux H. Women with anxiety disorders during pregnancy are at increased risk of intense postnatal depressive symptoms: A prospective survey of the MATQUID cohort. Eur Psychiatry 2004;19:459–463 [PubMed] [Google Scholar]
7. Hoge EA, Oppenheimer JE, Simon NM. Generalized anxiety disorder. FOCUS 2004;2:346–359 [Google Scholar]
8. Phillips J, Sharpe L, Matthey S. Rates of depressive and anxiety disorders in a residential mother-infant unit for unsettled infants. Aust N Z J Psychiatry 2007;41:836–842 [PubMed] [Google Scholar]
9. Navarro P, García-Esteve L, Ascaso C, Aguado J, Gelabert E, Martín-Santos R. Non-psychotic psychiatric disorders after childbirth: Prevalence and comorbidity in a community sample. J Affect Disord 2008;109:171–176 [PubMed] [Google Scholar]
10. Wenzel A, Haugen EN, Jackson LC, Robinson K. Prevalence of generalized anxiety at eight weeks postpartum. Arch Womens Ment Health 2003;6:43–49 [PubMed] [Google Scholar]
11. Rowe HJ, Fisher JRW, Loh WM. The Edinburgh Postnatal Depression Scale detects but does not distinguish anxiety disorders from depression in mothers of infants. Arch Womens Ment Health 2008;11:103–108 [PubMed] [Google Scholar]
Rowe HJ, Fisher JRW, Loh WM. The Edinburgh Postnatal Depression Scale detects but does not distinguish anxiety disorders from depression in mothers of infants. Arch Womens Ment Health 2008;11:103–108 [PubMed] [Google Scholar]
12. Weisberg RB, Paquette JA. Screening and treatment of anxiety disorders in pregnant and lactating women. Womens Health Issues 2002;12:32–36 [PubMed] [Google Scholar]
13. Davis EP, Snidman N, Wadhwa PD, Glynn LM, Schetter CD, Sandman CA. Prenatal maternal anxiety and depression predict negative behavioral reactivity in infancy. Infancy 2004;6:319–331 [Google Scholar]
14. Austin MP, Hadzi-Pavlovic D, Leader L, Saint K, Parker G. Maternal trait anxiety, depression and life event stress in pregnancy: Relationships with infant temperament. Early Hum Dev 2005;81:183–190 [PubMed] [Google Scholar]
15. Brouwers EPM, Baar AL. Van, Pop VJM. Maternal anxiety during pregnancy and subsequent infant development. Infant Behav Dev 2001;24:95–106 [Google Scholar]
16. Blair MM, Glynn LM, Sandman CA, Davis EP. Prenatal maternal anxiety and early childhood temperament. Stress 2011;14:644–651 [PubMed] [Google Scholar]
Blair MM, Glynn LM, Sandman CA, Davis EP. Prenatal maternal anxiety and early childhood temperament. Stress 2011;14:644–651 [PubMed] [Google Scholar]
17. Stein A, Craske MG, Lehtonen A, et al.. Maternal cognitions and mother-infant interaction in postnatal depression and generalized anxiety disorder. J Abnorm Psychol 2012;121:795–809 [PMC free article] [PubMed] [Google Scholar]
18. Arteche A, Joormann J, Harvey A, et al.. The effects of postnatal maternal depression and anxiety on the processing of infant faces. J Affect Disord 2011;133:197–203 [PMC free article] [PubMed] [Google Scholar]
19. Wenzel A, Haugen EN, Goyette M. Sexual adjustment in postpartum women with generalized anxiety disorder. J Reprod Infant Psychol 2005;23:365–366 [Google Scholar]
20. Uguz F, Sonmez EO, Sahingoz M, et al.. Maternal generalized anxiety disorder during pregnancy and fetal brain development: A comparative study on cord blood brain-derived neurotrophic factor levels. J Psychosom Res 2013;75:346–350 [PubMed] [Google Scholar]
21. Ding X-X, Wu Y-L, Xu S-J, et al.. Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Disord 2014;159:103–110 [PubMed] [Google Scholar]
Ding X-X, Wu Y-L, Xu S-J, et al.. Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Disord 2014;159:103–110 [PubMed] [Google Scholar]
22. Vasiliadis H-M, Buka SL, Martin LT, Gilman SE. Fetal growth and the lifetime risk of generalized anxiety disorder. Depress Anxiety 2010;27:1066–1072 [PMC free article] [PubMed] [Google Scholar]
23. Mina TH, Reynolds RM. Mechanisms linking in utero stress to altered offspring behaviour. Curr Top Behav Neurosci 2014;18:93–122 [PubMed] [Google Scholar]
24. Buss C, Davis EP, Shahbaba B, Pruessner JC, Head K, Sandman CA. Maternal cortisol over the course of pregnancy and subsequent child amygdala and hippocampus volumes and affective problems. Proc Natl Acad Sci U S A 2012;109:E1312–1329 [PMC free article] [PubMed] [Google Scholar]
25. Grigoriadis S, de Camps Meschino D, Barrons E, et al.. Mood and anxiety disorders in a sample of Canadian perinatal women referred for psychiatric care. Arch Womens Ment Health 2011;14:325–333 [PubMed] [Google Scholar]
Arch Womens Ment Health 2011;14:325–333 [PubMed] [Google Scholar]
26. Wenzel A, Haugen EN, Jackson LC, Brendle JR. Anxiety symptoms and disorders at eight weeks postpartum. Anxiety Disord 2005;19:295–311 [PubMed] [Google Scholar]
27. Reck C, Struben K, Backenstrass M, et al.. Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiatr Scand 2008;118:459–468 [PubMed] [Google Scholar]
28. Van Balkom AJLM, van Boeijen CA, Boeke AJP, van Oppen P, Kempe PT, van Dyck R. Comorbid depression, but not comorbid anxiety disorders, predicts poor outcome in anxiety disorders. Depress Anxiety 2008;25:408–415 [PubMed] [Google Scholar]
29. Bittner A, Goodwin RD, Wittchen H-U, Beesdo K, Höfler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? J Clin Psychiatry 2004;65:618–626, quiz 730 [PubMed] [Google Scholar]
30. Wittchen H-U, Beesdo K, Bittner A, Goodwin RD. Depressive episodes–evidence for a causal role of primary anxiety disorders? Eur Psychiatry 2003;18:384–393 [PubMed] [Google Scholar]
31. Hofmeijer-Sevink MK, Batelaan NM, van Megen HJGM, et al.. Clinical relevance of comorbidity in anxiety disorders: A report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012;137:106–112 [PubMed] [Google Scholar]
Hofmeijer-Sevink MK, Batelaan NM, van Megen HJGM, et al.. Clinical relevance of comorbidity in anxiety disorders: A report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012;137:106–112 [PubMed] [Google Scholar]
32. Coelho HF, Murray L, Royal-Lawson M, Cooper PJ. Antenatal anxiety disorder as a predictor of postnatal depression: A longitudinal study. J Affect Disord 2011;129:348–353 [PubMed] [Google Scholar]
33. Prenoveau J, Craske M, Counsell N, et al.. Postpartum GAD is a risk factor for postpartum MDD: The course and longitudinal relationships of postpartum GAD and MDD. Depress Anxiety 2013;30:506–514 [PMC free article] [PubMed] [Google Scholar]
34. Skouteris H, Wertheim EH, Rallis S, Milgrom J, Paxton SJ. Depression and anxiety through pregnancy and the early postpartum: An examination of prospective relationships. J Affect Disord 2009;113:303–308 [PubMed] [Google Scholar]
35. Arch JJ. Pregnancy-specific anxiety: Which women are highest and what are the alcohol-related risks? Compr Psychiatry 2013;54:217–228 [PubMed] [Google Scholar]
36. Andrews G, Creamer M, Crino R, Hunt C, Lampe L, Page A. treatment of anxiety disorders: Clinician guides and patient manuals, 2nd ed. Cambridge: Cambridge University Press, 2003 [Google Scholar]
Andrews G, Creamer M, Crino R, Hunt C, Lampe L, Page A. treatment of anxiety disorders: Clinician guides and patient manuals, 2nd ed. Cambridge: Cambridge University Press, 2003 [Google Scholar]
37. National Collaborating Centre for Mental Health (NCCMH). Antenatal and postnatal mental health: The NICE guideline on clinical management and service guidance. Leicester and London: The British Psychological Society and the Royal College of Physicians, 2007. [Google Scholar]
38. National Institute for Health and Care Excellence (NICE). Antenatal and postnatal health overview. Manchester: NICE, 2014. [Google Scholar]
39. Argyropoulos SV, Ploubidis GB, Wright TS, et al.. Development and validation of the Generalized Anxiety Disorder Inventory (GADI). J Psychopharmacol 2007;21:145–152 [PubMed] [Google Scholar]
40. Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979;9:139–145 [PubMed] [Google Scholar]
41. Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, 1970. [Google Scholar]
Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, 1970. [Google Scholar]
42. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–370 [PubMed] [Google Scholar]
43. Spitzer R, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine 2006;166:1092–1097 [PubMed] [Google Scholar]
44. Levin JS. The factor structure of the Pregnancy Anxiety Scale. J Heal Soc Behav 1991;32:368–381 [PubMed] [Google Scholar]
45. Somerville S, Dedman K, Hagan R, et al.. The Perinatal Anxiety Screening Scale: Development and preliminary validation. Arch Womens Mental Health 2014;17:443–454 [PubMed] [Google Scholar]
46. Cohen L, Altshuler L. Pharmacologic management of psychiatric illness during pregnancy and the postpartum period. In: Dunner D, Rosenbaum JF, eds. The psychiatric clinics of North America annal of drug therapy. Philadelphia: WB Saunders Company, 1997:21–60 [Google Scholar]
Philadelphia: WB Saunders Company, 1997:21–60 [Google Scholar]
47. Avni-Barron O, Wiegartz PS. Issues in treating anxiety disorders in pregnancy. Psychiatr Times 2011;28 [Google Scholar]
48. Alwan S, Reefhuis J, Rasmussen S a, Olney RS, Friedman JM. Use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. N Engl J Med 2007;356:2684–2692 [PubMed] [Google Scholar]
49. Peretti S, Judge R, Hindmarch I. Safety and tolerability considerations: Tricyclic antidepressants vs. selective serotonin reuptake inhibitors. Acta Psychiatr Scand 2000;101(s403):17–25 [PubMed] [Google Scholar]
50. Einarson A. Studying the safety of drugs in pregnancy: And the gold standard is? J Clin Pharmacol Pharmacoepidemiol 2008;1:3–8 [Google Scholar]
51. Byatt N, Deligiannidis KM, Freeman MP. Antidepressant use in pregnancy: A critical review focused on risks and controversies. Acta Psychiatr Scand 2013;127:94–114 [PMC free article] [PubMed] [Google Scholar]
52. Gentile S. Selective serotonin reuptake inhibitor exposure during early pregnancy and the risk of birth defects. Acta Psychiatr Scand 2011;123:266–275 [PubMed] [Google Scholar]
Gentile S. Selective serotonin reuptake inhibitor exposure during early pregnancy and the risk of birth defects. Acta Psychiatr Scand 2011;123:266–275 [PubMed] [Google Scholar]
53. Grigoriadis S, Vonderporten EH, Mamisashvili L, et al.. Antidepressant exposure during pregnancy and congenital malformations: Is there an association? A systematic review and meta-analysis of the best evidence. J Clin Psychiatry 2013;74:e293–e308 [PubMed] [Google Scholar]
54. GlaxoSmithKline. Use of paroxetine in first trimester of pregnancy may have a small increased risk of birth defects, compared to other antidepressants. Missisauga, ON: GlaxoSmithKline, 2005. [Google Scholar]
55. Bérard A, Ramos E, Rey E, Blais L, St-André M, Oraichi D. First trimester exposure to paroxetine and risk of cardiac malformations in infants: The importance of dosage. Birth Defects Res B Dev Reprod Toxicol 2007;80:18–27 [PubMed] [Google Scholar]
56. Einarson A, Pistelli A, DeSantis M, et al.. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry 2008;165:749–752 [PubMed] [Google Scholar]
Am J Psychiatry 2008;165:749–752 [PubMed] [Google Scholar]
57. Bakker MK, De Walle HEK, Wilffert B, de Jong-Van den Berg LTW. Fluoxetine and infantile hypertrophic pylorus stenosis: A signal from a birth defects-drug exposure surveillance study. Pharmacoepidemiol Drug Saf 2010;19:808–813 [PubMed] [Google Scholar]
58. Malm H, Artama M, Gissler M, Ritvanen A. Selective serotonin reuptake inhibitors and risk for major congenital anomalies. Obstet Gynecol 2011;118:111–120 [PubMed] [Google Scholar]
59. Einarson A, Choi J, Einarson TR, Koren G. Rates of spontaneous and therapeutic abortions following use of antidepressants in pregnancy: Results from a large prospective database. J Obstet Gynaecol Can 2009;31:452–456 [PubMed] [Google Scholar]
60. Hemels MEH, Einarson A, Koren G, Lanctôt KL, Einarson TR. Antidepressant use during pregnancy and the rates of spontaneous abortions: A meta-analysis. Ann Pharmacother 2005;39:803–809 [PubMed] [Google Scholar]
61. Ross LE, Grigoriadis S, Mamisashvili L, et al. . Selected pregnancy and delivery outcomes after exposure to antidepressant medication:A a systematic review and meta-analysis. J Am Med Assoc Psychiatry 2013;70:436–443 [PubMed] [Google Scholar]
. Selected pregnancy and delivery outcomes after exposure to antidepressant medication:A a systematic review and meta-analysis. J Am Med Assoc Psychiatry 2013;70:436–443 [PubMed] [Google Scholar]
62. Chambers CD, Hernandez-Diaz S, Van Marter LJ, et al.. Selective serotonin-reuptake inhibitors and risk of persistent pulmonary hypertension of the newborn. N Engl J Med 2006;354:579–587 [PubMed] [Google Scholar]
63. Grigoriadis S, Vonderporten EH, Mamisashvili L, et al.. Prenatal exposure to antidepressants and persistent pulmonary hypertension of the newborn: Systematic review and meta-analysis. BMJ 2014;348:f6932. [PMC free article] [PubMed] [Google Scholar]
64. Oberlander TF, Misri S, Fitzgerald CE, Kostaras X, Rurak DW, Riggs W. Pharmacologic Factors Associated With Transient Neonatal Symptoms Following Prenatal Psychotropic Medication Exposure. J Clin Psychiatry 2004;65:230–237 [PubMed] [Google Scholar]
65. Sanz EJ, De-las-Cuevas C, Kiuru A, Bate A, Edwards R. Selective serotonin reuptake inhibitors in pregnant women and neonatal withdrawal syndrome: A database analysis. Lancet 2005;365:482–487 [PubMed] [Google Scholar]
Selective serotonin reuptake inhibitors in pregnant women and neonatal withdrawal syndrome: A database analysis. Lancet 2005;365:482–487 [PubMed] [Google Scholar]
66. Wisner KL, Sit DKY, Hanusa BH, et al.. Major depression and antidepressant treatment: Impact on pregnancy and neonatal outcomes. Am J Psychiatry 2009;166:557–566 [PMC free article] [PubMed] [Google Scholar]
67. Misri S, Reebye P, Kendrick K, et al.. Internalizing behaviors in 4-year-old children exposed in utero to psychotropic medications. Am J Psychiatry 2006;163:1026–1032 [PubMed] [Google Scholar]
68. Oberlander TF, Reebye P, Misri S, Papsdorf M, Kim J, Grunau RE. Externalizing and attentional behaviors in children of depressed mothers treated with a selective serotonin reuptake inhibitor antidepressant during pregnancy. Arch Pediatr Adolesc Med 2007;161:22–29 [PubMed] [Google Scholar]
69. Reebye PN, Morison SJ, Panikkar H, Misri S, Grunau RE. Affect expression in prenatally psychotropic exposed and nonexposed mother-infant dyads. Infant Ment Health J 2002;23:403–416 [Google Scholar]
Infant Ment Health J 2002;23:403–416 [Google Scholar]
70. Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry 2011;68:1104–1112 [PubMed] [Google Scholar]
71. Harrington RA, Lee L-C, Crum RM, Zimmerman AW, Hertz-Picciotto I. Prenatal SSRI use and offspring with autism spectrum disorder or developmental delay. Pediatrics 2014;133:e1241–-e1248 [PMC free article] [PubMed] [Google Scholar]
72. Hviid A, Melbye M, Pasternak B. Use of selective serotonin reuptake inhibitors during pregnancy and risk of autism. N Engl J Med 2013;369:2406–2415 [PubMed] [Google Scholar]
73. Sørensen MJ, Grønborg TK, Christensen J, et al.. Antidepressant exposure in pregnancy and risk of autism spectrum disorders. Clin Epidemiol 2013;5:449–459 [PMC free article] [PubMed] [Google Scholar]
74. Gentile S. The safety of newer antidepressants in pregnancy and breastfeeding. Drug Saf 2005;28:137–152 [PubMed] [Google Scholar]
75. Hale TW, Shum S, Grossberg M. Fluoxetine toxicity in a breastfed infant. Clin Pediatr 2001;40:681–684 [PubMed] [Google Scholar]
Hale TW, Shum S, Grossberg M. Fluoxetine toxicity in a breastfed infant. Clin Pediatr 2001;40:681–684 [PubMed] [Google Scholar]
76. Hale TW. Medications and mothers' milk, 15th ed. Amarillo, TX: Hale Publishing, 2012 [Google Scholar]
77. Daw JR, Mintzes B, Law MR, Hanley GE, Morgan SG. Prescription drug use in pregnancy: A retrospective, population-based study in British Columbia, Canada (2001–2006). Clin Ther 2012;34:239–249.e2 [PubMed] [Google Scholar]
78. Hoffman EJ, Mathew SJ. Anxiety disorders: A comprehensive review of pharmacotherapies. Mt Sinai J Med 2008;75:248–262 [PubMed] [Google Scholar]
79. Barker MJ, Greenwood KM, Jackson M, Crowe SF. Cognitive effects of long-term benzodiazepine use. CNS Drugs 2004;18:37–48 [PubMed] [Google Scholar]
80. Baldwin DS, Waldman S, Allgulander C. Evidence-based pharmacological treatment of generalized anxiety disorder. Int J Neuropsychopharmacol 2011;14:697–710 [PubMed] [Google Scholar]
81. NCCMH. Generalised anxiety disorder in adults: The NICE guidelines on clinical management and service guidance. Leicester and London: The British Psychological Society and the Royal College of Physicians, 2011. [Google Scholar]
Leicester and London: The British Psychological Society and the Royal College of Physicians, 2011. [Google Scholar]
82. Dolovich LR, Addis A, Vaillancourt JMR, Power JDB, Koren G, Einarson TR. Benzodiazepine use in pregnancy and major malformations or oral cleft: Meta-analysis of cohort and case-control studies. BMJ 1998;317:839–843 [PMC free article] [PubMed] [Google Scholar]
83. Wikner BN, Stiller C-O, Bergman U, Asker C, Källén B. Use of benzodiazepines and benzodiazepine receptor agonists during pregnancy: Neonatal outcome and congenital malformations. Pharmacoepidemiol Drug Saf 2007;16:1203–1210 [PubMed] [Google Scholar]
84. Gentile S. Anxiety and sleep disorders, psychopharmacology, and pregnancy. In: Galbally M, Snellen M, Lewis A, eds. Psychopharmacology and pregnancy. Heidelberg: Springer; 2014:87–102 [Google Scholar]
85. Iqbal MM, Sobhan T, Ryals T. Effects of commonly used benzodiazepines on the fetus, the neonate, and the nursing infant. Psychiatr Serv 2002;53:39–49 [PubMed] [Google Scholar]
86. Committee on Drugs. Use of psychoactive medication during pregnancy and possible effects on the fetus and newborn. Pediatrics 2000;105:880–887 [PubMed] [Google Scholar]
Committee on Drugs. Use of psychoactive medication during pregnancy and possible effects on the fetus and newborn. Pediatrics 2000;105:880–887 [PubMed] [Google Scholar]
87. Levine RE, Oandasan AP, Primeau L a, Berenson AB. Anxiety disorders during pregnancy and postpartum. Am J Perinatol 2003;20:239–248 [PubMed] [Google Scholar]
88. Katzman MA. Aripiprazole: A clinical review of its use for the treatment of anxiety disorders and anxiety as a comorbidity in mental illness. J Affect Disord 2011;128:S11–S20 [PubMed] [Google Scholar]
89. Stein DJ, Bandelow B, Merideth C, Olausson B, Szamosi J, Eriksson H. Efficacy and tolerability of extended release quetiapine fumarate (quetiapine XR) monotherapy in patients with generalised anxiety disorder: An analysis of pooled data from three 8-week placebo-controlled studies. Hum Psychopharmacol 2011;26:614–628 [PubMed] [Google Scholar]
90. Üçok A, Gaebel W. Side effects of atypical antipsychotics: A brief overview. World Psychiatry 2008;7:58–62 [PMC free article] [PubMed] [Google Scholar]
91. McKenna K, Koren G, Tetelbaum M, et al.. Pregnancy outcome of women using atypical antipsychotic drugs: A prospective comparative study. J Clin Psychiatry 2005;66:444–449 [PubMed] [Google Scholar]
McKenna K, Koren G, Tetelbaum M, et al.. Pregnancy outcome of women using atypical antipsychotic drugs: A prospective comparative study. J Clin Psychiatry 2005;66:444–449 [PubMed] [Google Scholar]
92. Reis M, Källén B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol 2008;28:279–288 [PubMed] [Google Scholar]
93. ACOG Committee on Practice Bulletins; Stowe ZN, Ragan K. ACOG Practice Bulletin No. 92: Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol 2008;111:1001–1020 [PubMed] [Google Scholar]
94. Arch JJ. Cognitive behavioral therapy and pharmacotherapy for anxiety: Treatment preferences and credibility among pregnant and non-pregnant women. Behav Res Ther 2014;52:53–60 [PubMed] [Google Scholar]
95. Goodman J. Women's attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth 2009;36:60–69 [PubMed] [Google Scholar]
96. Covin R, Ouimet AJ, Seeds PM, Dozois DJA. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord 2008;22:108–116 [PubMed] [Google Scholar]
A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord 2008;22:108–116 [PubMed] [Google Scholar]
97. Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G. Psychological treatment of generalized anxiety disorder: A meta-analysis. Clin Psychol Rev 2014;34:130–140 [PubMed] [Google Scholar]
98. Leichsenring F, Salzer S, Jaeger U, et al.. Cognitive-behavioral therapy in generalized anxiety disorder: A randomized, controlled trial. Am J Psychiatry 2009;166:875–881 [PubMed] [Google Scholar]
99. Huppert JD, Rynn M. Generalized anxiety disorder. In: Stein DJ, ed. Clinical manual of anxiety disorders. Arlington, VA: American Psychiatric Publishing; 2004:147–171 [Google Scholar]
100. Austin M-P, Frilingos M, Lumley J, et al.. Brief antenatal cognitive behaviour therapy group intervention for the prevention of postnatal depression and anxiety: A randomised controlled trial. J Affect Disord 2008;105:35–44 [PubMed] [Google Scholar]
101. Duncan LG, Bardacke N. Mindfulness-based childbirth and parenting education: Promoting family mindfulness during the perinatal period. J Child Fam Stud 2010;19:190–202 [PMC free article] [PubMed] [Google Scholar]
Duncan LG, Bardacke N. Mindfulness-based childbirth and parenting education: Promoting family mindfulness during the perinatal period. J Child Fam Stud 2010;19:190–202 [PMC free article] [PubMed] [Google Scholar]
102. Dunn C, Hanieh E, Roberts R, Powrie R. Mindful pregnancy and childbirth: Effects of a mindfulness-based intervention on women's psychological distress and well-being in the perinatal period. Arch Womens Ment Health 2012;15:139–143 [PubMed] [Google Scholar]
103. Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Arch Womens Ment Health 2008;11:67–74 [PubMed] [Google Scholar]
104. Goodman JH, Guarino A, Chenausky K, et al.. CALM Pregnancy: Results of a pilot study of mindfulness-based cognitive therapy for perinatal anxiety. Arch Womens Ment Health 2014;17:373–387 [PMC free article] [PubMed] [Google Scholar]
105. Borkovec BTD, Newman MG, Castonguay LG. Cognitive-behavioral therapy for generalized anxiety disorder with integrations from interpersonal and experiential therapies 2003;8:382–389 [PubMed] [Google Scholar]
106. Bastani F, Hidarnia A, Kazemnejad A, Vafaei M, Kashanian M. A randomized controlled trial of the effects of applied relaxation training on reducing anxiety and perceived stress in pregnant women. J Midwifery Womens Health 2005;50:e36–e40 [PubMed] [Google Scholar]
Bastani F, Hidarnia A, Kazemnejad A, Vafaei M, Kashanian M. A randomized controlled trial of the effects of applied relaxation training on reducing anxiety and perceived stress in pregnant women. J Midwifery Womens Health 2005;50:e36–e40 [PubMed] [Google Scholar]
107. Urech C, Fink NS, Hoesli I, Wilhelm FH, Bitzer J, Alder J. Effects of relaxation on psychobiological wellbeing during pregnancy: A randomized controlled trial. Psychoneuroendocrinology 2010;35:1348–1355 [PubMed] [Google Scholar]
108. Hoyer J, Beesdo K, Gloster AT, Runge J, Höfler M, Becker ES. Worry exposure versus applied relaxation in the treatment of generalized anxiety disorder. Psychother Psychosom 2009;78:106–115 [PubMed] [Google Scholar]
109. Donker T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for depression, anxiety and psychological distress: A meta-analysis. BMC Med 2009;7:79. [PMC free article] [PubMed] [Google Scholar]
110. Cloninger CR, Zohar AH, Hirschmann S, Dahan D. The psychological costs and benefits of being highly persistent: Personality profiles distinguish mood disorders from anxiety disorders.![]() J Affect Disord 2012;136:758–766 [PubMed] [Google Scholar]
J Affect Disord 2012;136:758–766 [PubMed] [Google Scholar]
111. Marcé LV. Traité de la folie des femmes enceintes des nouvelles accouchées et des nourrices et considérations médico-légales qui se rattachent à ce sujet. Paris: Baillière, 1858. [Google Scholar]
How can you manage anxiety during pregnancy?
Pregnancy is an exciting time. You will soon become a parent to an adorable, tiny human. You may expect to experience the rollercoaster of emotions during pregnancy, or emotions may catch you off guard. Some women feel joy at every flutter or kick, marveling at their changing bodies. For other women, pregnancy is hard, giving no reprieve as it brings severe fatigue, mood changes, and constant worries. You may notice that with every passing month, your thoughts are spiraling out of control, affecting your performance at work and your relationships at home. But how do you manage your anxiety, and should you treat it?
What causes anxiety during pregnancy?
Worries during pregnancy are universal. Hormonal changes of pregnancy, prior heartbreaking miscarriages, and sleep difficulties may all contribute to anxiety for mothers-to-be. You may worry about how a baby will affect your relationships with friends or family members, the health of your future child, the delivery experience, or the financial burden of an additional family member. All of these worries are completely normal. For humans, a certain amount of anxiety is protective; how else could we motivate ourselves to complete our work or run away from a bear?
Hormonal changes of pregnancy, prior heartbreaking miscarriages, and sleep difficulties may all contribute to anxiety for mothers-to-be. You may worry about how a baby will affect your relationships with friends or family members, the health of your future child, the delivery experience, or the financial burden of an additional family member. All of these worries are completely normal. For humans, a certain amount of anxiety is protective; how else could we motivate ourselves to complete our work or run away from a bear?
What are the symptoms of anxiety disorders during pregnancy?
Although it’s normal to be worried about the health of your baby, in some cases this worry becomes debilitating and may require further attention. Thoughts about the health of the baby may become obsessive, even when doctors are reassuring. Worries may also appear as physical symptoms, such as a rapid heartbeat, difficulty breathing, or panic attacks. If this is the first time you experience a high level of anxiety, this may be frightening in itself. When anxiety starts to interfere with your day-to-day functioning, relationships, or job performance, it may be classified as an anxiety disorder — if your doctor picks up on it.
When anxiety starts to interfere with your day-to-day functioning, relationships, or job performance, it may be classified as an anxiety disorder — if your doctor picks up on it.
Anxiety can occur at any time during pregnancy, or it may first appear after delivery (perinatal anxiety is the term used for anxiety during pregnancy and after delivery). The rates of generalized anxiety disorder appear to be highest in the first trimester, likely due to hormonal changes. The most common symptoms of anxiety include constant worrying, restlessness, muscle tension, irritability, feeling dread, an inability to concentrate, and difficulties falling asleep due to worries. Some women also experience symptoms as a result of other anxiety disorders, including panic disorder, obsessive-compulsive disorder, or post-traumatic stress disorder.
Unfortunately, two of the most common mental health screening tools in pregnancy (the Edinburgh Postnatal Depression Screen and Generalized Anxiety Disorder 7-item Scale) are not great at detecting anxiety in pregnancy. Although underdiagnosed, anxiety disorders during pregnancy and in the postpartum period are common, and may affect up to one in five women. Many women suffer in silence.
Although underdiagnosed, anxiety disorders during pregnancy and in the postpartum period are common, and may affect up to one in five women. Many women suffer in silence.
What are the effects of untreated anxiety on the fetus?
When thinking about management of anxiety, it is important to consider both the risks of treatment as well as the harms of untreated anxiety. Although less studied than depression, research suggests that anxiety may negatively affect both the mother and the fetus. Anxiety increases the risk for preterm birth, low birthweight, earlier gestational age, and a smaller head circumference (which is related to brain size).
What are some treatments for anxiety during pregnancy?
Fortunately, there are many treatments that can reduce anxiety during pregnancy and help you feel better. For many women, anti-anxiety medication is not an option during pregnancy, as there is little information on the safety of such medication on the fetus. Some women who had previously taken medications for anxiety may wish to discontinue medications during pregnancy for personal reasons.
Therapies such as cognitive behavior therapy (CBT) demonstrate promise in the peripartum period (the period shortly before, during, and after giving birth). CBT focuses on challenging maladaptive thoughts, emotions, and actions, and it uses anxiety management strategies such as diaphragmatic breathing (adapted to pregnancy).
If your anxiety is severe, medications may be an option for you. Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for depression and anxiety during pregnancy and after delivery. It does not appear that SSRIs are associated with an increased risk of major congenital malformations. However, SSRIs may be associated with transient neonatal symptoms such as jitteriness, tremor, crying, and trouble feeding, which resolve on their own in a few days.
The use of benzodiazepines such as lorazepam (Ativan) and alprazolam (Xanax) during pregnancy has long been a controversial topic. Although older studies showed an association between their use and an increased risk for cleft lip and palate, a more recent study looking at benzodiazepine use during pregnancy did not show this link when these medications were used alone (although there may be an increased risk when combined with antidepressants).
What else helps anxiety during pregnancy?
- Engage in regular physical activity. In general, it is safe to engage in physical activity during pregnancy. However, if you are at risk for preterm labor or have pregnancy complications, consult with your doctor first.
- Ensure adequate sleep. Whether it’s a calming bedtime routine, pregnancy pillow, or a few nights in a bed away from your snoring partner, now is the time to learn what works for your sleep.
- Practice mindfulness. Research shows that mindfulness may reduce worries about labor, and it may even prevent postpartum depression.
- Journaling. Writing about your worries may help you brainstorm potential solutions, and it allows you to reflect on your concerns.
- Schedule worry time. We often worry because we do not want to forget something. Setting aside 30 minutes toward the end of the day provides you with a time to worry productively, but it frees you from holding onto your worries the rest of the day (practice reminding yourself "I’ll get to these thoughts later").

- Yoga, massage, meditation, and acupuncture. Finding relaxation techniques that work for you may take some experimentation — but their benefits will continue even after the baby arrives.
It will be possible to decipher the child's genome by the blood of a pregnant woman
Western doctors began to introduce a genetic study of the unborn child by the mother's blood about five years ago. The American College of Obstetricians and Gynecologists has already recommended it for all pregnant women: more than three million such tests have been done. But this study is far from a panacea and can reveal not so many diseases. Why?
There are two types of violations. The first is when all chromosomes are normal, but their number changes. For example, not 46, as it should be, but 47. Because of them, children are born with Down syndrome, Edwards, Patau ... Such pathologies are common, and they can be detected with a probability of 99 percent starting from the 9th week of pregnancy. In Russia, such a study is also being carried out.
In Russia, such a study is also being carried out.
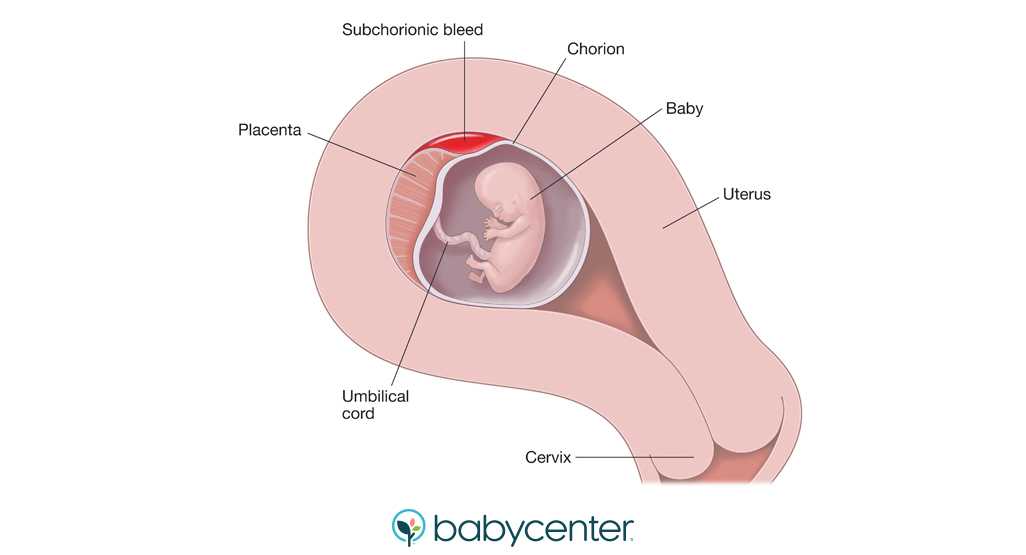
The second type is "breakdowns" in individual genes, of which there are thousands of variants. Such mutations are rare, and it is extremely difficult to identify them from the mother's blood. Judging by the headlines in the media, Western geneticists have successfully coped with the task. But what has been advertised as "full genome sequencing" is actually just an advanced version of a familiar test. We are talking about quantitative violations: the truth is not only of whole chromosomes, but also of their fragments. And full decoding is the ability to determine all the letters in the genome to one.
By the way, even in newborns, doctors have not learned how to diagnose all disorders. There are cases when the DNA of a baby has been "read" by specialists on the most modern equipment. But the exact "breakdown" in the genes, which caused a rare hereditary disease, could not be determined. In prenatal research, which is carried out during pregnancy, it is even more complicated: only incomplete fragments of the baby's DNA enter the mother's blood through the placenta.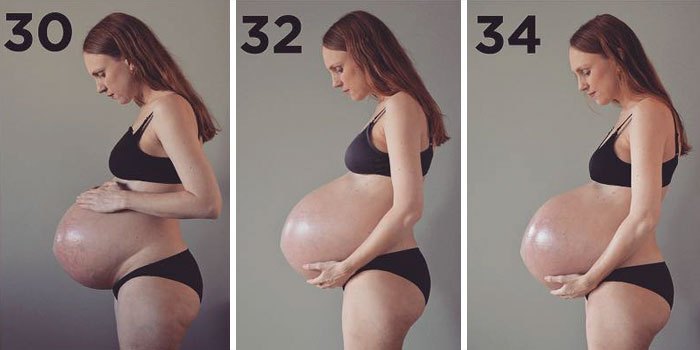 Therefore, when searching for individual "breakdowns" there is a big risk of getting inaccurate results. Or, for example, find a mutation that will not lead to any disease, but will greatly frighten parents. Hence another problem - ethical.
Therefore, when searching for individual "breakdowns" there is a big risk of getting inaccurate results. Or, for example, find a mutation that will not lead to any disease, but will greatly frighten parents. Hence another problem - ethical.
However, experts have no doubt that the future of medicine is determined precisely by DNA methods. And not only diagnostics, but also chromosome editing. Scientists are already working on "repairing" the genome of embryos, trying to cut out DNA copies of the human immunodeficiency virus from there. So the elimination of the child's diseases at the stage of pregnancy planning is already a real prospect, not a fantasy.
Opinion
Ilya Kanivets, Researcher at the Medical Genetic Research Center, Head of the Genetics Department at the Genomed Center:
- Indeed, the study of fetal DNA isolated from the mother's blood already makes it possible to detect not only frequent chromosomal abnormalities, but also to study the entire genome of the unborn child. True, it is still too early to use this method for the clinical diagnosis of diseases caused by mutations in individual genes. To do this, it is necessary not only to improve the research technology, but also to modernize the system for interpreting the data obtained. We still have very few specialists in this area.
True, it is still too early to use this method for the clinical diagnosis of diseases caused by mutations in individual genes. To do this, it is necessary not only to improve the research technology, but also to modernize the system for interpreting the data obtained. We still have very few specialists in this area.
However, such tests will make it possible to prevent the birth of a sick child in spouses carrying dangerous mutations in the near future. They will also be useful to families who already have children with an established hereditary pathology. But as a geneticist, I still cannot recommend conducting a genome-wide DNA analysis of the unborn child during each pregnancy. And the point is not only in complex bioinformatics analysis, but also in ethical and legislative aspects, which, not only in Russia, but all over the world, have not yet been resolved.
Rossiyskaya gazeta - Federal issue: No. 41(6909)
Share:
NaukaNauka
ᐈ Are you pregnant? What to do? — Reproductive medicine, gynecology, pregnancy monitoring, urology
Laser treatment and vaginal rejuvenation
More details
Once again about hormones or a list of must-haves for the week
More details
A visit to a urologist. For or Against?
For or Against?
Read more
Reproductive health care
Read more
Pregnancy with uterine fibroids
Read more
Practical skills when examining barren steam
Read more
Pregnancy with endometriosis: Modern view
more
Contractions of breast cancer
Details
Varico -stake
More details
Secretory and obstructive male infertility
More details
Controlled ovarian stimulation (COS) protocols
More
Miscarriage. What is the reason?
Read more
Hysteroscopy and its role in the treatment of infertility
Read more
Why you can’t get pregnant
more
How to calculate the gender of the child before the conception of
more details
more than
Syndrome of ovary hypertension syndrome. a look at the problem
a look at the problem
More
Pregnancy with endometriosis - a modern view
Read more
Immunological infertility and the role of antisperm antibodies in it
Read more
What is cervical pathology?
More details
IVF in the natural cycle: pros and cons
More details
Practical skills in examining infertile couples
More details
Artificial insemination
More details
More
Unable to get pregnant. Where to run? Where to begin?
Read more
What future parents need to know (most popular questions)
Read more
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
Should I be afraid?
Read more
Obstruction of the fallopian tubes, what to do next?
More
Human papillomavirus. Basic information
Details
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
More details
Infertility and cancer: why men should definitely visit a reproductive specialist chances with IVF
Read more
Portrait of a female doctor: 5 signs of a good gynecologist
Read more
Is sex during IVF a good idea?
Read more
Never say never. Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
Learn more
How to plan for health, longevity and parenthood: practical advice from doctors for 2020
Learn more
From virus to cancer: hidden threats to women's health
Learn more
Threatening abortion
Reproductive health of teenage girls: what children and their parents need to know
Read more
Life is like magic: how to believe in a miracle if you are a pragmatist - a doctor's story
Read more
Beautiful skin in youth is the key to happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
What determines the effectiveness of ART
More
Why do not all eggs become embryos?
More details
Maxim Gapchuk in "Mother and child" ambitious future
More details
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know?
Read more
9 tips for future parents
Read more
Eco: Modern methods and approaches in the treatment of female infertility
Read more
icsi: Men's infertility is not a sentence
more
Laparoscopy: Advantages over traditional surgical
Read more
Uterine examination: what you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: the essence of the method, stages and results
Read more
Infertility Diagnostics in men
Read more
10 reasons to contact a man to andrologist
Read more
Cryototechnology as a way of family planning
more details
How to become a mother: Psychological and physical training
Read more
Monalisa Touch — what is this technology
More
Premature menopause in men: how to recognize and what is dangerous
More
Why visit a gynecologist for preventive examinations
More details
Laser therapy in gynecology: without anesthesia and pain
More details
Outpatient gynecology - timely seeking qualified help
More details
examinationMore details
Causes and prevention of female infertility
More details
One-day surgery: a modern approach to treatment
More details
Pregnancy management: to keep the baby healthy and mother's well-being
More details
Pregnancy after IVF: what future parents need to remember
More details
Anomalies of the uterus and their impact on the onset and carrying of pregnancy.