Blood from nipple when breastfeeding
What to Do About Blood in Breast Milk
Written by WebMD Editorial Contributors
Reviewed by Dan Brennan, MD on February 22, 2021
In this Article
- What Causes Blood in Breast Milk?
- What to Do When You Have Blood in Breast Milk
Breast milk looks different over time, ranging from the yellow of colostrum to white, creamy, or clear. Sometimes, blood tinges the milk pink, red, or brown. Seeing blood in breast milk causes alarm, but in most cases, it looks worse than it actually is.
Knowing why this happens and the symptoms that go along with it gives you a better sense for how to respond — and helps you judge whether you need to take any action at all.
What Causes Blood in Breast Milk?
Many situations can lead to blood in breast milk. These range from mild concerns to urgent signs of trouble. Some examples include:
Rusty pipe syndrome. Breast milk that appears reddish-brown sometimes results from a phenomenon called rusty pipe syndrome.
Typically, rusty pipe syndrome happens during the first few days of breastfeeding. A type of breast engorgement, it results from increased blood flow that accompanies an increase in milk production. Some of this blood may seep into the colostrum or breast milk and change its color. This is rarely painful and should disappear after a few days.
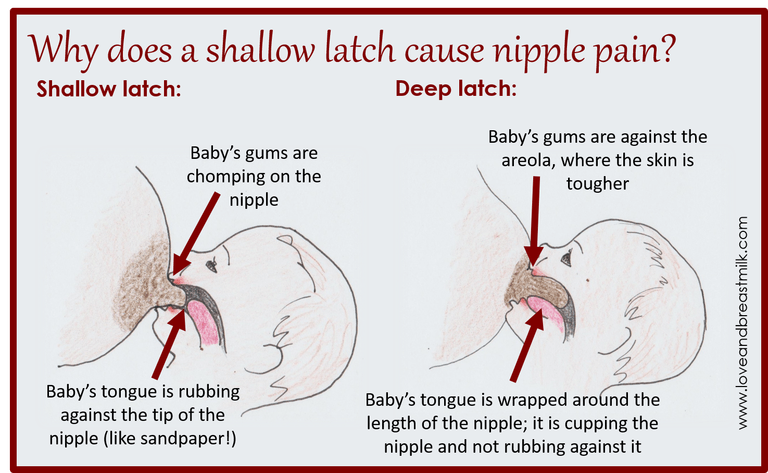
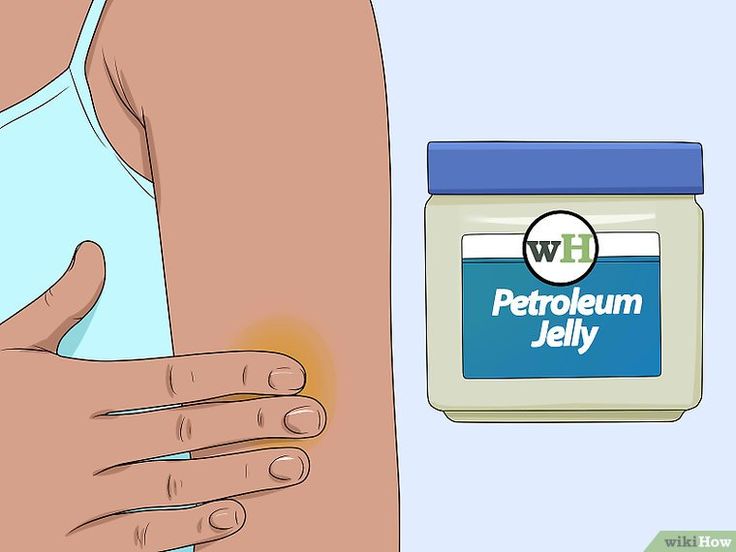
Cracked nipples. Another common source of blood in breast milk, cracked nipples may happen if a baby doesn't attach to the nipple well. Occasionally, issues such as tongue-ties or thrush may be to blame. Breast milk or medical-grade lanolin can be applied to the cracked area to help with healing.
Mastitis. Blood in breast milk is just one of several symptoms associated with mastitis (inflammation of the breast tissue). Typically, nursing mothers with this condition get tender or painful breasts, as well as swelling, lumps, or fever. Bloody nipple discharge can happen during mastitis but is more often a cause of the condition than a symptom.
Breast cancer. Although rare, breast cancer can sometimes cause blood in breast milk. Typically, this results from nipple discharge and includes other symptoms, such as breast thickening or lumps. These issues are often confused with mastitis, but both conditions require medical attention.
What to Do When You Have Blood in Breast Milk
How you respond to blood in breast milk may depend on which symptoms you get and at what point in your breastfeeding journey the problems arrive. For example, small amounts of blood in the first few days of breastfeeding may not need action, especially if there are no other symptoms.
Common responses to blood in breast milk include:
Continue breastfeeding. In most cases, it's safe or even helpful to continue breastfeeding if you see blood in your breast milk. This can sometimes be a sign of health problems for the mother, but it's not dangerous for babies. Some mothers find that blood in the breast milk causes babies to spit up more, but this is rarely cause for concern.
Continue following advice from your doctor and lactation consultant, regardless of the presence of blood in your breast milk. As you and your baby adjust to breastfeeding, the problem may go away on its own.
Wait it out. Waiting for blood to go away is the best solution when only a small amount appears during the first days of breastfeeding. If the blood clearly results from common concerns such as engorgement or rusty pipe syndrome, there’s no need to seek help yet. Instead, focus on resolving the underlying problem.
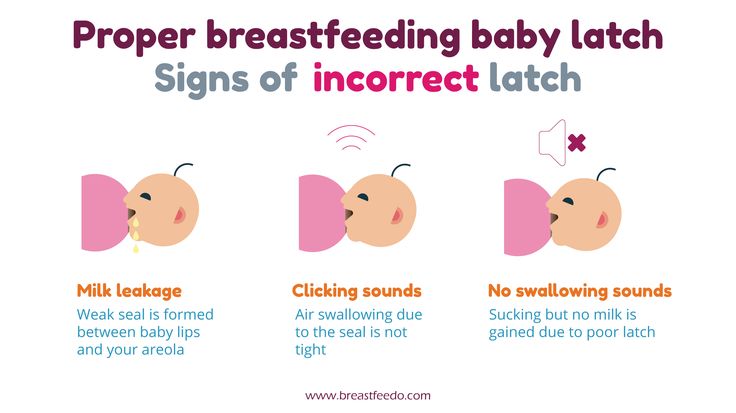
Work on attachment and positioning. If cracked nipples cause blood in breast milk, a better attachment (latch) process could fix the problem. To begin, try different positions until you find one that's comfortable for both you and your baby. No matter which position you prefer, your baby’s head and spine should fully align. The mouth should open wide before attaching, with the chin touching the breast as much as possible.
If you still struggle to get a good latch, make an appointment with a lactation consultant. Mention that you’ve spotted blood in your breast milk. You should receive targeted advice, as well as follow-up attention to make sure that you’re safe and that your breastfeeding efforts are on track.
Ask your doctor. If you’re worried that blood in your breast milk could signal mastitis, cancer, or some other serious problem, contact your doctor as soon as possible. If you have cancer, you may also find lumps in your breasts not related to clogged milk ducts or mastitis.
When you visit your doctor, they'll ask about your medical history and current breastfeeding practices. If the doctor suspects cancer, you may receive a breast exam, a mammogram, or an ultrasound. An official diagnosis can only be made once you have a biopsy.
Sore, cracked or bleeding nipples
Sore, cracked or bleeding nipples | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Sore, cracked or bleeding nipples are common. Some mothers have such trouble with them that they stop breastfeeding early.
Some mothers have such trouble with them that they stop breastfeeding early.
As a new mother, you may find it could take a few days or weeks to adapt to the strong suck of a healthy baby on your breasts.
It is normal for your breasts to become more sensitive in the first weeks after you have given birth. They may sting, burn, ache or feel tender. Over time, the discomfort and sensitivity should resolve.
If you have sore nipples, it may be that your baby isn’t attaching properly to your breast. This pain usually lasts about half a minute while baby first draws your nipple into their mouth.
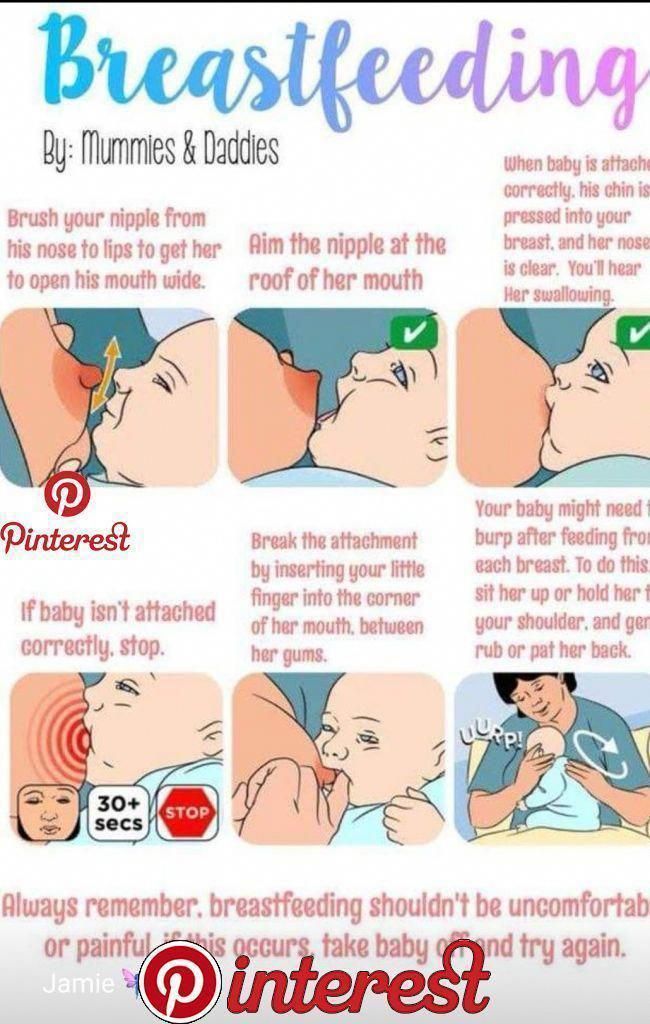
Try to make sure your baby’s mouth is attached correctly for suckling from the very first breastfeed.
If you do not correct your baby’s latch, your nipples could be damaged, which causes problems like mastitis (infections).
How to get baby to attach to your breast correctly
- Make sure you are sitting or lying comfortably. Position your baby’s chest against your chest, with their mouth and nose facing your nipple.

- If you are lying down, let your baby’s cheek rest against your breast. If you are sitting up, lift your breast slightly so it does not press on your baby’s chin.
- Position your baby so the first contact point is their chin on your areola — the coloured area around your nipple.
- Bring your baby’s head to your breast, not the breast to baby’s head. Support your baby to move to where they are trying to go — towards your nipple.
- Ensure the nipple and much (or all) of the areola and some surrounding breast are in your baby’s mouth.
After a few rapid gulps, your baby should start to suck and swallow in a regular rhythm. Once you have got the hang of it, breastfeeding can be enjoyable and should not be painful.
How to manage sore nipples
Before putting baby to the breast
Wash your hands and sit in a comfortable position and try to relax. Apply a warm washer to the breast and gently massage or express to help milk flow. Express some milk to soften the areola to lubricate the nipple.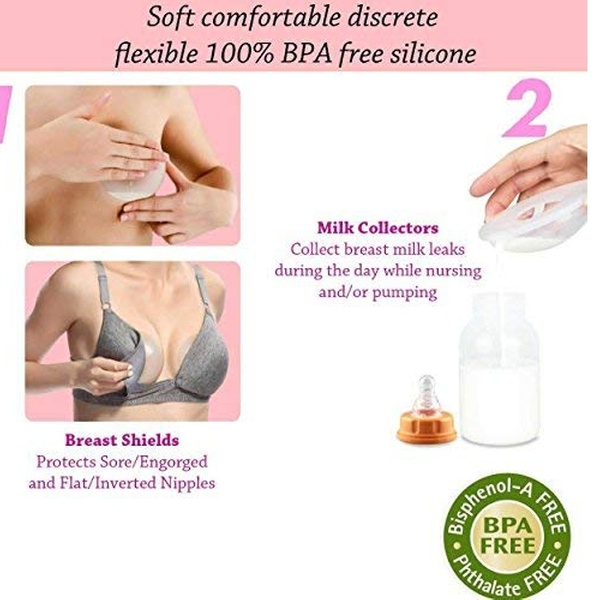
At the breast
Poor attachment is a key cause of sore nipples. Make sure the way your baby latches to your breast is correct. If you are not sure, ask for help from a health professional.
If the attachment feels uncomfortable after 30 seconds, break your baby’s suction by putting your finger in the corner of their mouth. Take your baby off and let them re-latch to your breast. Try different feeding positions. If your nipples are tender, limit your baby’s comfort sucking.
After the breastfeed
Check your nipples for redness and misshapen appearance. Wipe your breasts with clean water and let them dry. It can help to leave your bra off for a while and allow your nipples to air. Make sure your bra fits.
When expressing milk, make sure that the suction on your breast pump is not too strong. If the pain in your nipples increases after the first week, talk to a health professional.
Finding the cause of cracked or bleeding nipples
You will need to work out the source of your nipple problems. The first thing to do is to check if your baby is latching on correctly. You may need to ask a health professional for assistance. They can also check your baby for problems with their lips and tongue and whether you have medical problems like dermatitis or nipple infection. If you use a nipple shield, make sure it is the correct size and if you’re using a breast pump, make sure you’re doing it properly.
The first thing to do is to check if your baby is latching on correctly. You may need to ask a health professional for assistance. They can also check your baby for problems with their lips and tongue and whether you have medical problems like dermatitis or nipple infection. If you use a nipple shield, make sure it is the correct size and if you’re using a breast pump, make sure you’re doing it properly.
How to treat cracked or bleeding nipples
There are a number of things you can do to treat cracked or bleeding nipples.
- Look after your nipples: wash your nipples with water after every feed and clean and sterilise your nipple shield after each feed.
- If you can, continue breastfeeding (it is quite safe for baby to feed on a bleeding nipple). But if it’s too painful, you may need to take your baby off the breast for 24 to 48 hours, rest the nipple and feed your baby expressed breast milk. Gradually reintroduce the breast after resting for a short time and take special care with positioning and attachment.

- If you’re going to take pain-relieving medication, talk to your doctor or pharmacist. Many household remedies are ineffective or harmful.
The Australian Breastfeeding Association has more tips on treating sore or cracked nipples.
If you need further help or are experiencing prolonged abnormal breast pain, contact your doctor, lactation consultant, breast feeding counsellor, child health nurse or Pregnancy Birth and Baby on 1800 882 436.
Sources:
Australian Breastfeeding Association (Sore/cracked nipples), Australian Breastfeeding Association (Mastitis), Australian Breastfeeding Association (Attachment to the breast), Raising Children Network (Breastfeeding attachment techniques), Tresillian (Breastfeeding 0-3 months)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: December 2020
Back To Top
Related pages
- Expressing and storing breast milk
- Breastfeeding your baby
Need more information?
Breastfeeding – mastitis and other nipple and breast problems - Better Health Channel
Mastitis affects some breastfeeding women and may be caused by blocked milk ducts or a bacterial infection.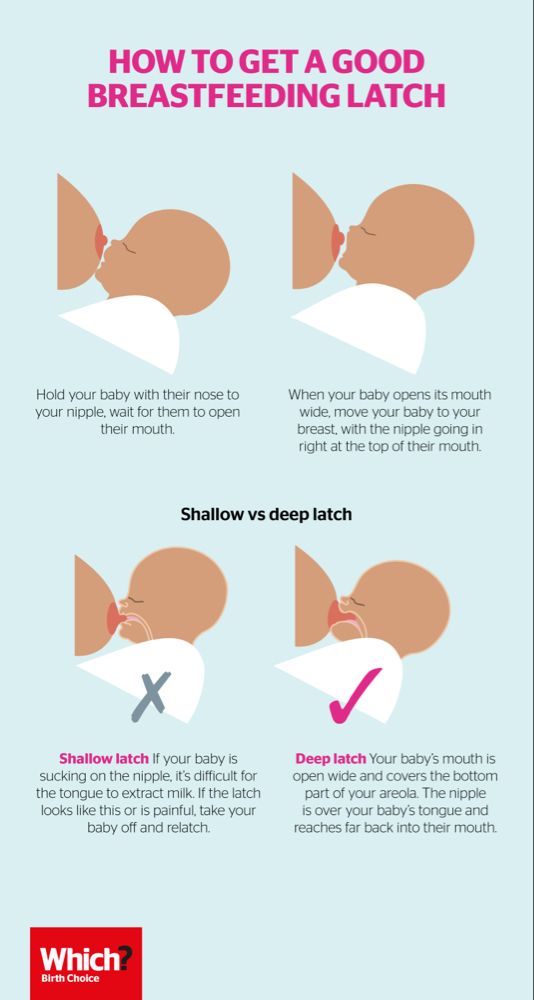
Read more on Better Health Channel website
Breastfeeding | Sydney Children's Hospitals Network
Breastfeeding is not always easy and you may have trouble breastfeeding your baby
Read more on Sydney Children's Hospitals Network website
Breastfeeding Advice For Newborn Babies | Tresillian
When establishing breastfeeding good positioning and attachment are key. Here are some tips from Tresillian to help your breastfeed your newborn.
Read more on Tresillian website
Breastfeeding - expressing breastmilk - Better Health Channel
Expressing breast milk by hand is a cheap and convenient method.
Read more on Better Health Channel website
Vasospasm and breastfeeding
Vasospasm affects the flow of milk from the nipple and can be a painful condition for women breastfeeding.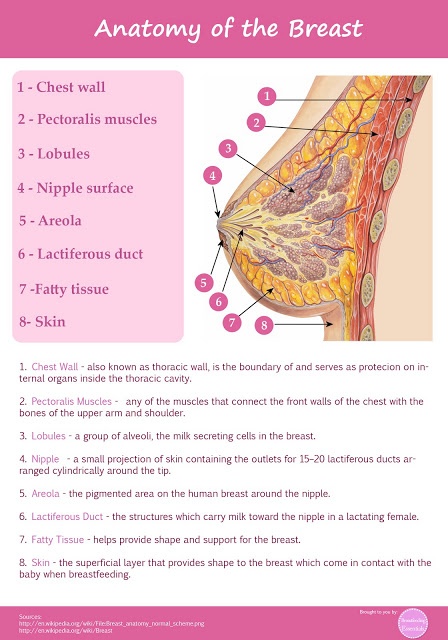 Learn about vasospasm and how to relieve the pain.
Learn about vasospasm and how to relieve the pain.
Read more on Pregnancy, Birth & Baby website
Breastfeeding
Breastfeeding is learnt over the first weeks and months of your child’s life. It is a unique and special experience for families as no two mothers or babies are the same.
Read more on Karitane website
Breast milk expressing - MyDr.com.au
There are a number of reasons why a breast feeding mother might wish to express milk rather than feeding the baby directly from the breast.
Read more on myDr website
Breastfeeding challenges - Ngala
Many new mothers experience breastfeeding challenges
Read more on Ngala website
Breastfeeding your baby
Breastfeeding is the most natural way to feed your baby, providing all the nutrition your baby needs during the first six months of life and a loving bond with your baby.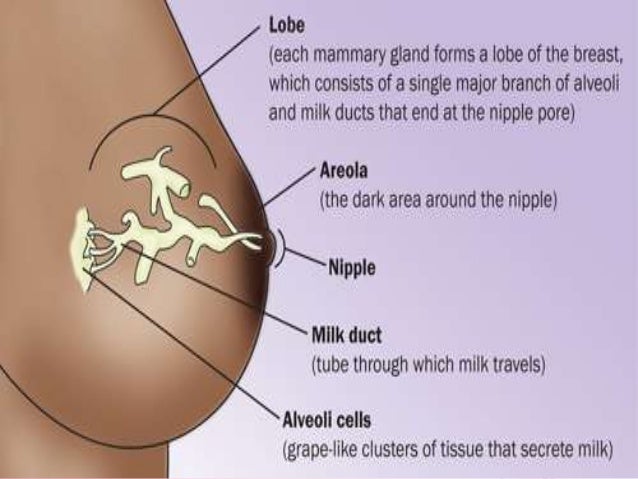
Read more on Pregnancy, Birth & Baby website
Common breastfeeding issues | Health and wellbeing | Queensland Government
Learn about common problems and solutions to help you establish breastfeeding.
Read more on Queensland Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.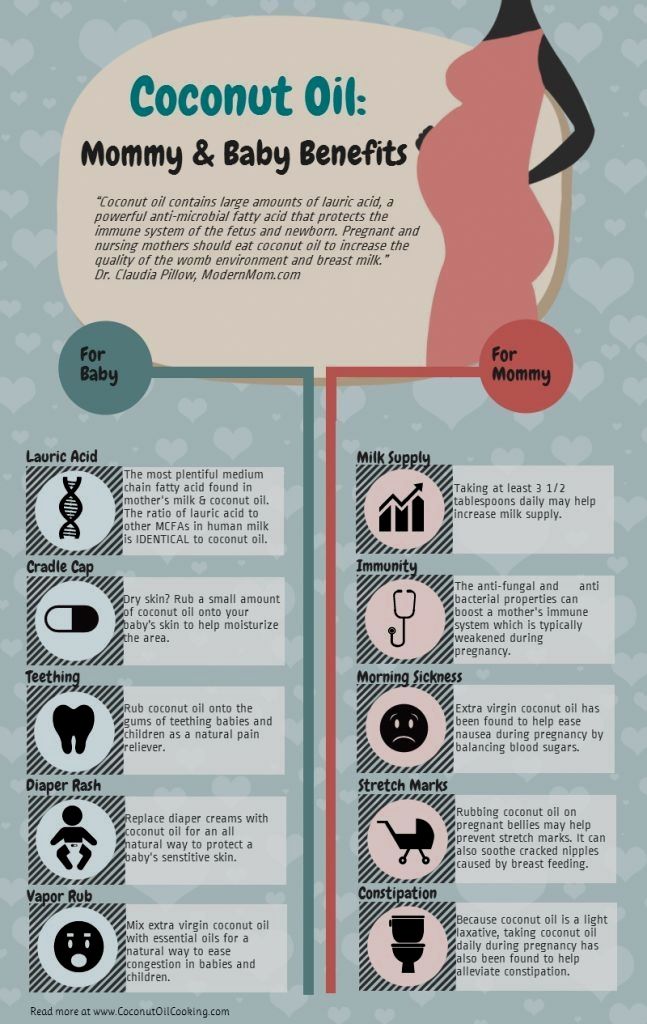
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Blood in breast milk - what could it be?
Sometimes breastfeeding mothers notice unusual discharge from the breast during lactation. Such discharge may have a reddish, pinkish, or rusty tint. You should always pay close attention to such secretions, because. they can be a sign of the presence of blood in the milk.
Most often, blood enters the milk from external injuries of the nipple and areola, for example, with deep cracks or abrasions in the nipple area blood often mixes with milk and turns it pink.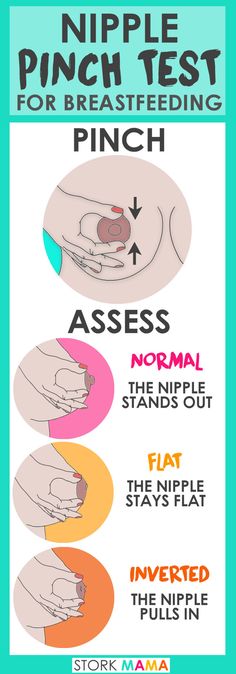 Sometimes mothers can watch a crack in the nipple bleed and the baby spit up milk with blood.
Sometimes mothers can watch a crack in the nipple bleed and the baby spit up milk with blood.
In this case, the cause of the presence of blood in the milk lies on the surface and usually does not raise questions, but only requires correction of the attachment of the child to the breast and additional treatment of the nipples for the speedy healing of cracks.
However, there are less obvious causes of blood in the milk when there are no visible lesions on the breast. Different studies of this problem describe different clinical cases, for example, one mother with severely inverted nipples had painless bleeding from the chest after wearing milk collection pads in late pregnancy. After she reduced the time she wore the braces, the bleeding stopped [2].
Another reason for the appearance of blood in milk can be damage to the capillaries inside the breast tissues due to inaccurate manual expression or improper use of the breast pump [4].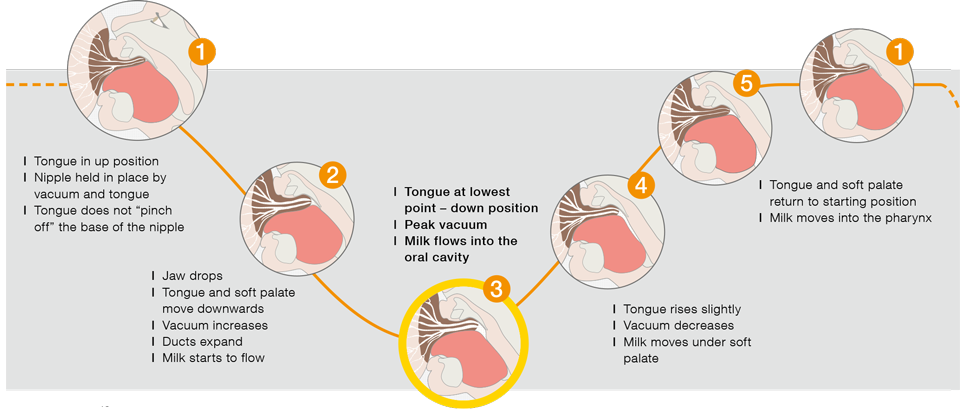
There is also a study that says that the milk of some breastfeeding mothers during the first weeks after childbirth can be similar to rusty water, which can be observed in water pipes that have not been used for a long time. This phenomenon is called "rusty pipe syndrome" . According to researchers, this syndrome occurs more often in primiparous mothers during the early stages of lactogenesis and is most often not associated with any discomfort [3]. In addition, dairy farmers report "rusty" milk from cows that calve for the first time. It is assumed that the reason for this is a slight internal bleeding from edema during the first flush of milk in a cow [4].
O'Callaghan, also a researcher of Rusty Pipe Syndrome, reports 37 clinical cases of its manifestation [5]. The earliest manifestation of the syndrome was noted during the fourth month of pregnancy and in most cases was associated with mechanical compression of the breast during the prenatal period.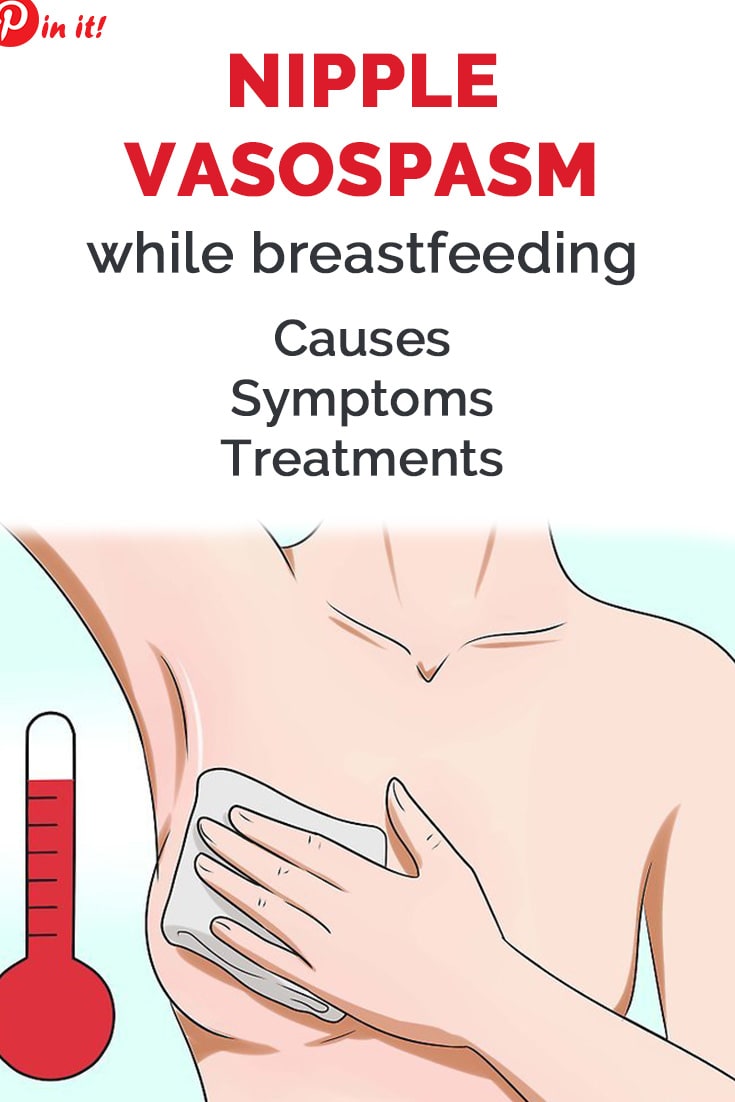 With this syndrome, blood in the milk may appear in both breasts and disappear, as a rule, within 3-7 days after the start of lactation.
With this syndrome, blood in the milk may appear in both breasts and disappear, as a rule, within 3-7 days after the start of lactation.
Bright red breast bleeding without sore or cracked nipples indicates that the nursing mother needs to see a doctor (mammologist or surgeon) as soon as possible. First of all, the study is carried out on the subject of intraductal papilloma.
Intraductal papilloma is a small, benign, wart-like growth on the inner surface of the milk duct that may bleed as it grows or decays. Usually, in this case, neither compaction nor swelling is palpated in the chest, and discomfort may be absent. Usually, with intraductal papilloma, bleeding is observed from only one breast. Often, bleeding stops spontaneously without any treatment [2], but nevertheless, a nursing mother should still consult a doctor to identify its causes.
Cytology, mammography, and ultrasound may be helpful in identifying the cause of blood in the milk in the absence of sore or cracked nipples [1].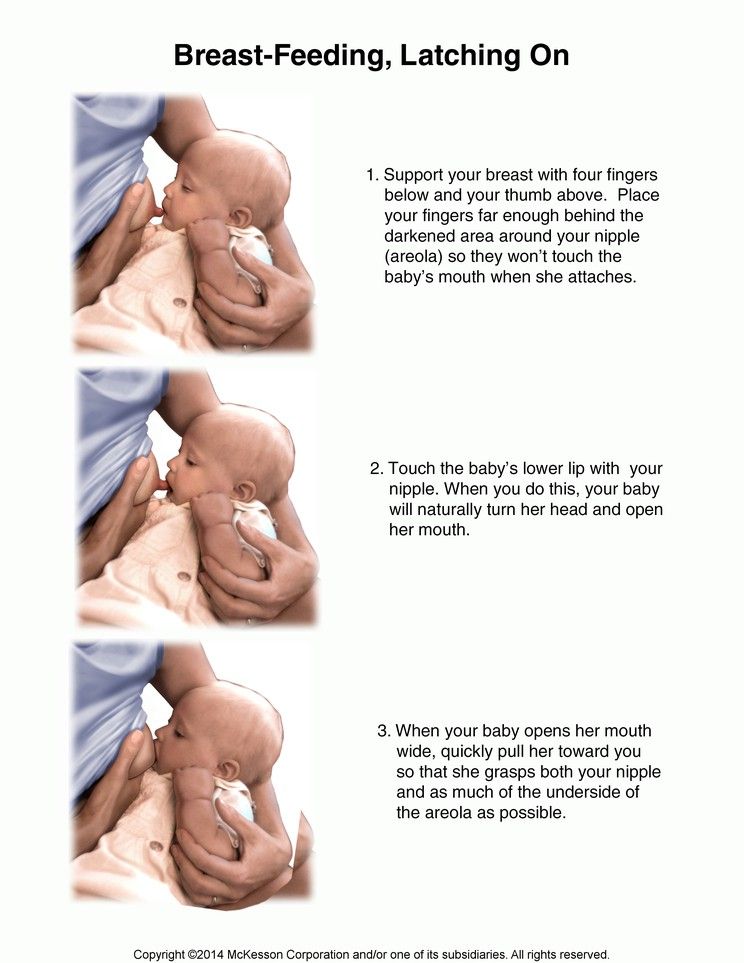 If, according to the results of the study, there is a need for surgical intervention, the doctor will remove the formation inside the duct. The mass will then be histologically examined to confirm that it is an intraductal papilloma and not something more serious such as intraductal malignancy .
If, according to the results of the study, there is a need for surgical intervention, the doctor will remove the formation inside the duct. The mass will then be histologically examined to confirm that it is an intraductal papilloma and not something more serious such as intraductal malignancy .
In a situation of breast bleeding of unknown origin, a breastfeeding mother can gently pump her breast to maintain lactation until the cause of the bleeding is identified. It is advisable to opt for manual pumping and carefully follow the correct gentle pumping technique, as rough pumping or pumping can exacerbate the problem.
In any case, if a mother notices that a child has accidentally received milk with a small amount of blood, do not panic - the baby will not be harmed by small amounts of serous-hemorrhagic discharge [2]. A relatively large amount of blood in the milk can lead to regurgitation of milk with blood in the baby.
Call a consultant Have questions? +7 (812) 956-3-954
Literature:
Literature:
- Berens P.
 D. , Prenatal, intrapartum, and postpartum support of the lactating mother. In: Schanler, RJ, ed. Breastfeeding, Part II: the management of breastfeeding, Pediatric Clin No Americal 48:365–75, 2002.
D. , Prenatal, intrapartum, and postpartum support of the lactating mother. In: Schanler, RJ, ed. Breastfeeding, Part II: the management of breastfeeding, Pediatric Clin No Americal 48:365–75, 2002. - Breastfeeding and Human Lactation (Jones and Bartlett Series in Breastfeeding/Human Lactation) by Jan Riordan Publisher: Jones and Bartlett Publishers, 3rd Edition, 2004. Pages: 819.
- Marmet C., Breast assessment: a model for evaluating breast structure and function. Presented at: La Leche League International Annual Seminar for Physicians, Boston, July 11–13, 1990.
- Mohrbacher N., Stock J., La Leche League International, The Breastfeeding Answer Book, Third Revised Edition, 2008.
- O’Callaghan M.A., Atypical discharge from the breast during pregnancy and/or lactation. Aust NZ J Obstet Gynaecol 21:214–16, 1981.
Alena Lukyanchuk Psychologist, lactation consultant, member of ILCA (The International Lactation Consultant Association)
Alena Korotkova, clinical psychologist, lactation consultant.
Nursing nipple care | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples. Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
Sioned Hilton, mother of three, has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.
In most women during pregnancy, the nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. 1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible. 2
Prevention is better than cure, so check out our tips.
Check your baby's latch on
Correct latch is the key to pain-free breastfeeding.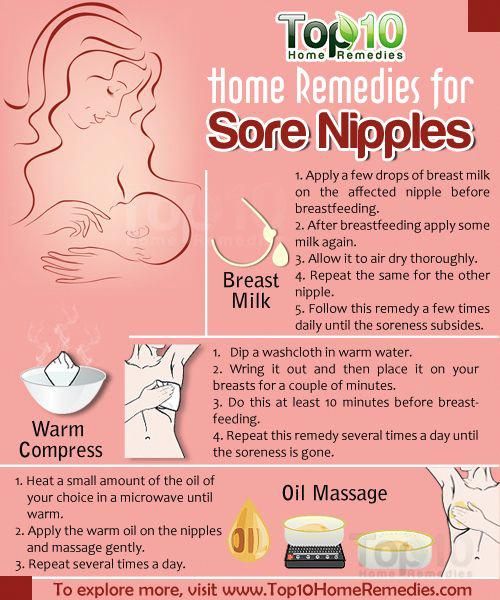 When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby.
Check tongue frenulum
Tongue frenulum (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin with which the tongue is attached at the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.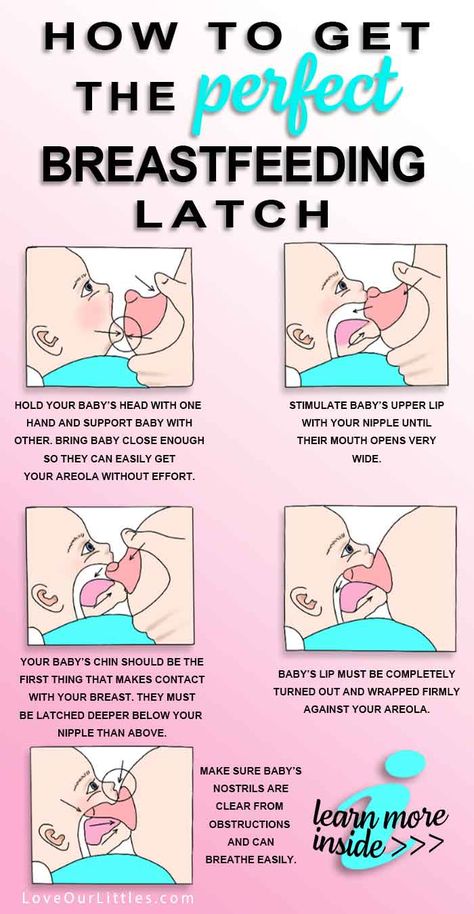
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum. A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding Nipple Tips
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples.
 Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6
Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6 - Pat the nipples gently with a soft towel or simply let them air dry. In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past!
- Do not wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's intestinal microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.
- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain.
 9
9
Healthy teat care products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool. It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding.
- Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit inside the bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.
- Nursing Bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples.
- Nursing pads* are special silicone pads that fit over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer.
 Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.
Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.
When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395.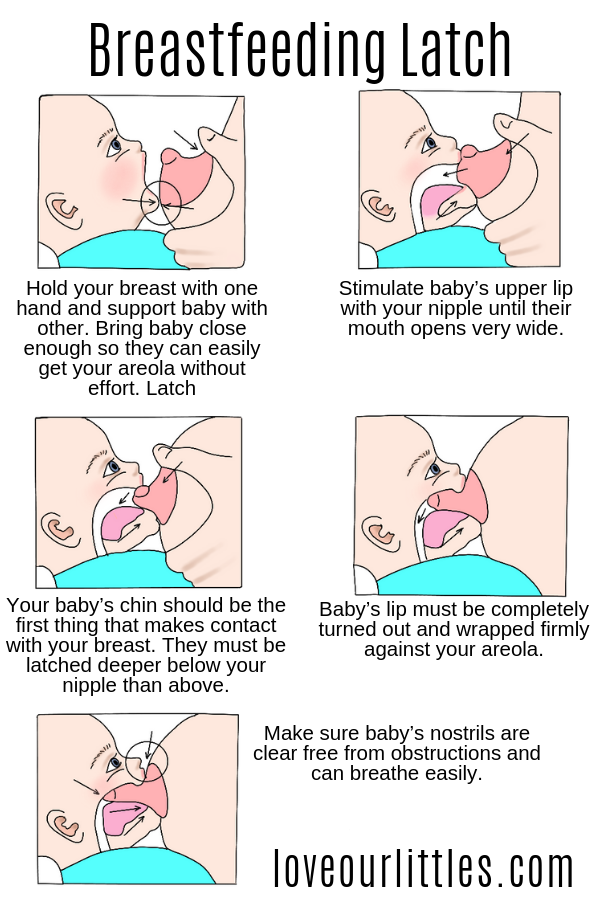 - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
- Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review.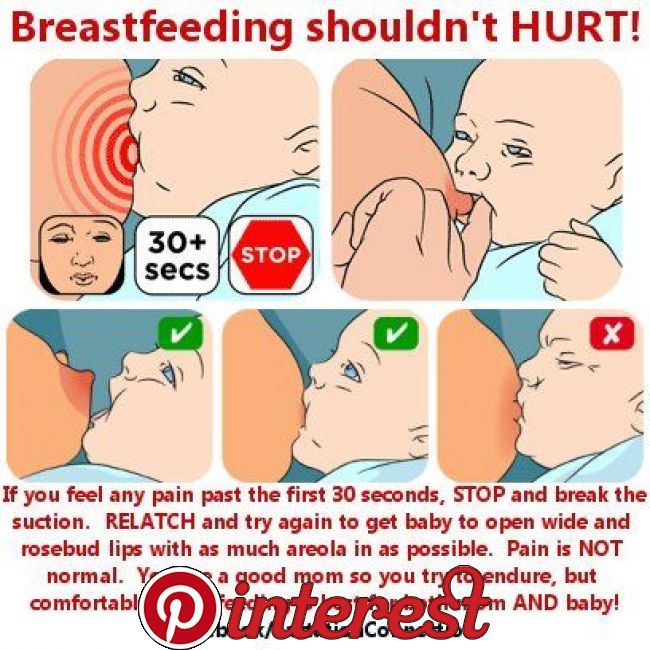 Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P.