Pregnant women check up
Prenatal care checkups | March of Dimes
Prenatal care is medical care you get during pregnancy. At each prenatal care visit, your health care provider checks on you and your growing baby.
Call your provider to schedule your first prenatal care checkup as soon as you know you’re pregnant.
Getting early and regular prenatal care can help you have a healthy pregnancy and a full-term baby.
Go to all your prenatal care checkups, even if you’re feeling fine.
What is prenatal care and why is it important?
Prenatal care is medical care you get during pregnancy. At each visit, your health care provider checks on you and your growing baby. Call your provider and go for your first prenatal care checkup as soon as you know you’re pregnant. And go to all your prenatal care checkups, even if you’re feeling fine.
Getting early and regular prenatal care can help you have a healthy pregnancy and a full-term baby. Full term means your baby is born between 39 weeks (1 week before your due date) and 40 weeks, 6 days (1 week after your due date). Being born full term gives your baby the right amount of time he needs in the womb to grow and develop.
Don’t be afraid to talk to your provider about personal things. Your provider needs to know all about you so she can give you and your baby the best care. She asks lots of questions about you, your partner and your families. Your medical information and anything you tell her are confidential. This means she can’t share them with anyone without your permission. So don’t be afraid to tell her about things that may be uncomfortable or embarrassing, like if your partner hurts or scares you or if you smoke, drink alcohol, use street drugs or abuse prescription drugs.
Who can you go to for prenatal care?
You can get prenatal care from different kinds of providers:
- An obstetrician/gynecologist (also called OB/GYN) is a doctor who has education and training to take care of pregnant women and deliver babies.
 The American College of Obstetricians and Gynecologists can help you find an OB in your area.
The American College of Obstetricians and Gynecologists can help you find an OB in your area. - A family practice doctor (also called a family physician) is a doctor who can take care of every member of your family. This doctor can take care of you before, during and after pregnancy. The American Board of Family Medicine can help you find a family practice doctor in your area.
- A maternal-fetal medicine (also called MFM) specialist is an OB with education and training to take care of women who have high-risk pregnancies. If you have health conditions that may cause problems during pregnancy, your provider may want you to see a MFM specialist. The Society for Maternal-Fetal Medicine can help you find a specialist in your area.
- A certified nurse-midwife (also called CNM) is a nurse with education and training to take care of women of all ages, including pregnant women. The American College of Nurse-Midwives can help you find a CNM in your area.
- A family nurse practitioner (also called FNP) or a women’s health nurse practitioner (also called WHNP).
 A FNP is a nurse with education and training to take care of every member of your family. A WHNP is a nurse with education and training to take care of women of all ages, including pregnant women. The American Association of Nurse Practitioners can help you find these kinds of nurse practitioners in your area.
A FNP is a nurse with education and training to take care of every member of your family. A WHNP is a nurse with education and training to take care of women of all ages, including pregnant women. The American Association of Nurse Practitioners can help you find these kinds of nurse practitioners in your area.
Think about these things to help you choose a provider:
- Is the provider licensed and board certified to take care of you during pregnancy, labor and birth? Licensed means the provider can legally practice medicine in a state. To have a license, a provider has to have a certain amount of education and training and pass certain tests to make sure he can safely take care of patients. Board certified means that a provider has had extra training in a certain area (called a specialty).
- Is the provider covered by your health insurance?
- Have you heard good things about the provider? Is she recommended by your friends or family? How does your partner feel about her as your prenatal care provider?
- Would you rather see a man or a woman provider? How old to you want the provider to be? Does he explain things clearly?
- Is the office easy to get to? Do the office hours fit into your schedule? Is the office staff friendly and helpful?
- Who takes care of phone calls during office hours? Who handles them after hours or in an emergency? Do you have to pay if your provider spends time with you on the phone?
- Is the provider in group practice? If yes, will you always see your provider at prenatal care checkups? Or will you see other providers in the practice? Who will deliver your baby if your provider’s not available when you go into labor?
- What hospital or birthing center does the provider use? What do you know about it? Is it easy for you to get to?
How often do you go for prenatal care checkups?
Most pregnant women can follow a schedule like this:
- Weeks 4 to 28 of pregnancy.
 Go for one checkup every 4 weeks (once a month).
Go for one checkup every 4 weeks (once a month). - Weeks 28 to 36 of pregnancy. Go for one checkup every 2 weeks (twice a month).
- Weeks 36 to 41 of pregnancy. Go for one checkup every week (once a week).
If you have complications during pregnancy, your provider may want to see you more often.
Your partner or support person (a friend or someone from your family) is welcome at your prenatal checkups.
How can you get ready for your first prenatal care checkup?
Be ready to talk with your provider about:
- The first day of your last menstrual period (also called LMP). Your provider can use this to help find out your baby’s due date.
- Health conditions you have, like depression, diabetes, high blood pressure, and not being at a healthy weight. Conditions like these can cause problems during pregnancy. Tell your provider about your family health history.
 This is a record of any health conditions and treatments that you, your partner and everyone in your families have had. Use the March of Dimes Family Health History Form and share it with your provider. If you have a record of your vaccinations, take it to your checkup. A vaccination is a shot that contains a vaccine that helps protect you from certain harmful infections.
This is a record of any health conditions and treatments that you, your partner and everyone in your families have had. Use the March of Dimes Family Health History Form and share it with your provider. If you have a record of your vaccinations, take it to your checkup. A vaccination is a shot that contains a vaccine that helps protect you from certain harmful infections. - Medicines you take, including prescription medicine, over-the-counter medicine, supplements and herbal products. Some medicines can hurt your baby if you take them during pregnancy, so you may need to stop taking it or switch to another medicine. Don’t stop or start taking any medicine without talking to your provider first. And tell your provider if you’re allergic to any medicine. You may be allergic to a medicine if it makes you sneeze, itch, get a rash or have trouble breathing when you take it.
- Your pregnancy history. Tell your provider if you’ve been pregnant before or if you’ve had trouble getting pregnant.
 Tell her if you’ve had any pregnancy complications or if you’ve had a premature baby (a baby born before 37 weeks of pregnancy), a miscarriage or stillbirth. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
Tell her if you’ve had any pregnancy complications or if you’ve had a premature baby (a baby born before 37 weeks of pregnancy), a miscarriage or stillbirth. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy. - Smoking, drinking alcohol, using street drugs and abusing prescription drugs. All of these can hurt your baby. Alcohol includes beer, wine and liquor. Street drugs are illegal to use, like heroin and cocaine. Abusing prescription drugs means you use them differently than your provider tells you to. This means you take more than your provider says you can take, you take it with alcohol or other drugs or you use someone else’s prescription drugs.
- Stress you feel. Stress is worry, strain or pressure that you feel in response to things that happen in your life. Talk to your provide about ways to deal with and reduce your stress.
 High levels of stress can cause complications during pregnancy.
High levels of stress can cause complications during pregnancy. - Your safety at home and work. Tell your provider about chemicals you use at home or work and about what kind of job you have. If you’re worried about abuse during pregnancy and ask about ways you can stay healthy and safe at home and work.
What happens at your first prenatal care checkup?
Your first checkup is usually the longest because your provider asks you lots of questions about your health. At your first prenatal care checkup, your provider:
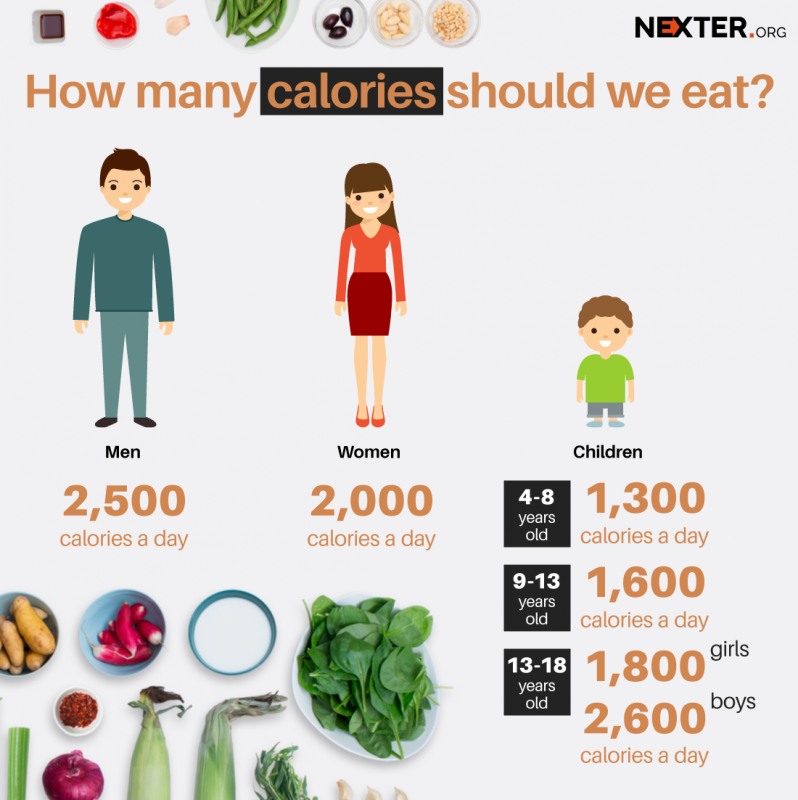
- Gives you a physical exam and checks your overall health. Your provider checks your weight and height to figure out how much weight you should gain during pregnancy.
- Checks your blood, blood pressure and urine. Blood tests can tell your provider if you have certain infections, like syphilis, hepatitis B and HIV. Your provider also uses a blood test to find out your blood type and Rh factor and to check for anemia.
 Anemia is when you don't have enough healthy red blood cells to carry oxygen to the rest of your body. Rh factor is a protein that most people have on their red blood cells. If you don’t have it and your baby does, it can cause Rh disease in your baby. Treatment during pregnancy can prevent Rh disease. Blood pressure and urine tests can help your provider diagnose a serious condition called preeclampsia. This is a kind of high blood pressure that can happen during pregnancy. Having too much protein in your urine may be a sign of preeclampsia. Urine tests also can tell your provider if you have a kidney or bladder infection or other conditions, like diabetes.
Anemia is when you don't have enough healthy red blood cells to carry oxygen to the rest of your body. Rh factor is a protein that most people have on their red blood cells. If you don’t have it and your baby does, it can cause Rh disease in your baby. Treatment during pregnancy can prevent Rh disease. Blood pressure and urine tests can help your provider diagnose a serious condition called preeclampsia. This is a kind of high blood pressure that can happen during pregnancy. Having too much protein in your urine may be a sign of preeclampsia. Urine tests also can tell your provider if you have a kidney or bladder infection or other conditions, like diabetes. - Gives you a pelvic exam and a Pap smear. Your provider checks the pelvic organs (pelvis and womb) to make sure they’re healthy. For the Pap smear, your provider collects cells from your cervix to check for cancer and for infections, like chlamydia and gonorrhea. The cervix is the opening to the uterus (womb) that sits at the top of the vagina.

- May give you vaccinations, like a flu shot. It’s safe to get a flu shot any time during pregnancy. But some vaccinations are best at certain times and some aren’t recommended during pregnancy. Talk to your provider about what’s best and safe for you and your baby.
- Tells you your due date. Your provider usually uses your LMP to figure out your due date. But you may get an early ultrasound to confirm that you’re pregnant and help your provider figure out your baby’s age. An ultrasound uses sound waves and a computer screen to show a picture of your baby inside the womb.
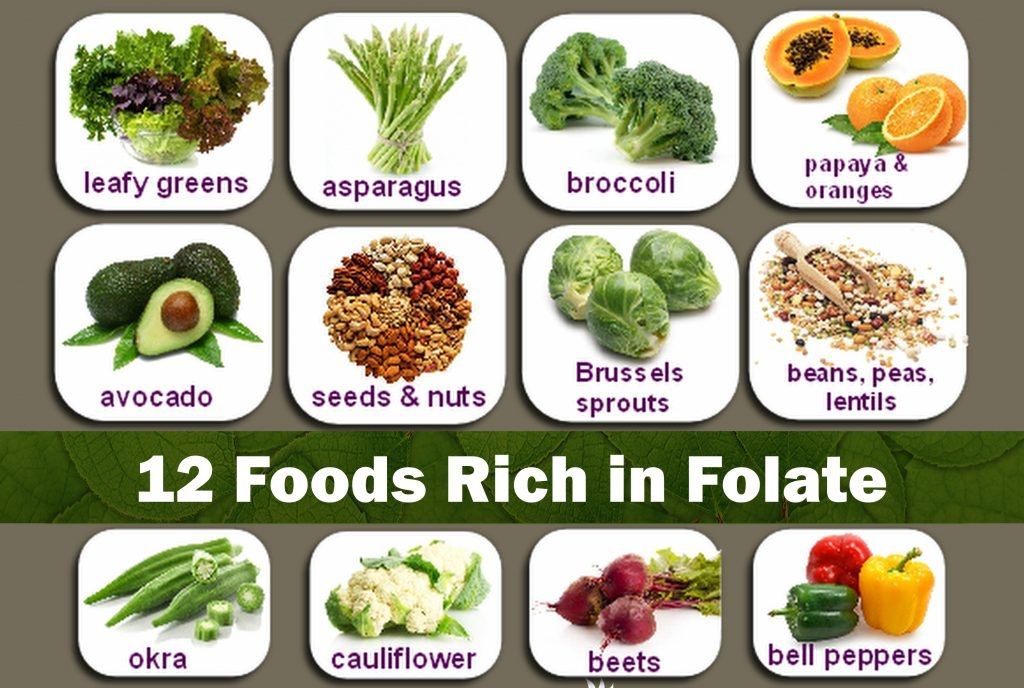
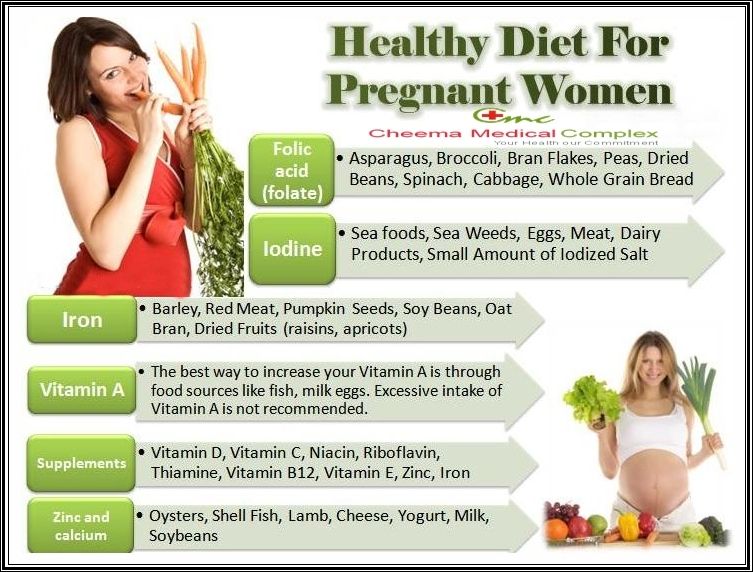
- Prescribes a prenatal vitamin. This is a multivitamin made for pregnant women. Your prenatal vitamin should have 600 micrograms of folic acid in it. Folic acid is a vitamin that every cell in your body needs for healthy growth and development. If you take it before pregnancy and during early pregnancy, it can help protect your baby from birth defects of the brain and spine called neural tube defects (also called NTDs), and birth defects of the mouth called cleft lip and palate.

- Talks to you about prenatal tests. These are medical tests you get during pregnancy. They help your provider find out how you and your baby are doing. You may want to have certain tests only if you have certain problems or if you’re at high risk of having a baby with a genetic or chromosomal condition, like Down syndrome. If your provider thinks you’re at risk for having a baby with one of these conditions, he may recommend that you see a genetic counselor. This person has training to help you understand about genes, birth defects and other medical conditions that run in families, and how they can affect your health and your baby’s health.
What happens at later prenatal care checkups?
Later prenatal care checkups usually are shorter than the first one. At your checkups, tell your provider how you’re feeling. There’s a lot going on inside your body during pregnancy. Your provider can help you understand what’s happening and help you feel better if you’re not feeling well. Between visits, write down questions you have and ask them at your next checkup.
Between visits, write down questions you have and ask them at your next checkup.
At later prenatal care checkups, your health care provider:
- Checks your weight and blood pressure. You also may get urine and blood tests.
- Checks your baby’s heartbeat. This happens after about 10 to 12 weeks of pregnancy. You can listen, too!
- Measures your belly to check your baby’s growth. Your provider starts doing this at about 20 weeks of pregnancy. Later in pregnancy, she also feels your belly to check your baby’s position in the womb.
- Gives you certain prenatal tests to check you and your baby. For example, most women get an ultrasound at 18 to 20 weeks of pregnancy. You may be able to tell if your baby’s a boy or a girl from this ultrasound, so be sure to tell your provider if you don’t want to know! Later in pregnancy, your provider may use ultrasound to check the amount of amniotic fluid around your baby in the womb.
 Between 24 and 28 weeks, you get a glucose screening test to see if you may have gestational diabetes. This is a kind of diabetes that some women get during pregnancy. And at 35 to 37 weeks, you get a test to check for group B strep. This is an infection you can pass to your baby.
Between 24 and 28 weeks, you get a glucose screening test to see if you may have gestational diabetes. This is a kind of diabetes that some women get during pregnancy. And at 35 to 37 weeks, you get a test to check for group B strep. This is an infection you can pass to your baby. - Asks you about your baby’s movement in the womb. If it’s your first pregnancy, you may feel your baby move by about 20 weeks. If you’ve been pregnant before, you may feel your baby move sooner. Your provider may ask you to do kick counts to keep track of how often your baby moves.
- Gives you a Tdap vaccination at 27 to 36 weeks of pregnancy. This vaccination protects both you and your baby against pertussis (also called whooping cough). Pertussis spreads easily and is dangerous for a baby.
- Does a pelvic exam. Your provider may check for changes in your cervix as you get close to your due date.
How can you get free or low-cost prenatal care?
If you don't have health insurance or can't afford prenatal care, find out about free or low-cost prenatal care services in your community:
- Call (800) 311-BABY [(800) 311-2229].
 For information in Spanish, call (800) 504-7081.
For information in Spanish, call (800) 504-7081. - Visit healthcare.gov to find a community health center near you. Community health centers can provide low-cost prenatal care.
Last reviewed: June, 2017
What Happens at a Prenatal Care Check-Up Appointment?
In This Section
- Prenatal Care
- What happens at an appointment?
- What is prenatal testing?
- What’s an ultrasound?
- What’s chorionic villus sampling?
- What’s amniocentesis?
- Where can I get prenatal care?
- What pregnancy complications can happen?
Prenatal services include tests and physical exams to make sure you and your pregnancy are healthy. It’s a good time to ask questions about your pregnancy and the birth of your future baby.
It’s a good time to ask questions about your pregnancy and the birth of your future baby.
What happens during my first prenatal care appointment?
Your first prenatal care visit is usually the longest one. You’ll talk with your doctor about your medical history, the other parent’s medical history, and your family's’ medical history.
Your doctor will give you a complete check-up, usually with a physical exam and blood and urine tests to make sure you’re healthy. This can include:
-
measuring your height, weight, blood pressure, breathing, and pulse
-
a breast exam
-
a pelvic exam
-
a Pap test
-
testing for sexually transmitted infections (like chlamydia, gonorrhea, syphilis, and HIV)
-
screening for diabetes, anemia, hepatitis B, and rubella
Your doctor might also talk with you about your diet and lifestyle, and prenatal vitamins. The most important vitamin you can take is folic acid, which ideally you would start taking before you’re even pregnant. Your doctor can give you advice about any changes you can make to have the healthiest pregnancy possible.
Your doctor can give you advice about any changes you can make to have the healthiest pregnancy possible.
Some types of medicine are dangerous to use during your pregnancy. Tell your doctor about every medicine, supplement, or drug you’re using, and always check with your doctor before starting any new ones.
What will happen during my follow-up prenatal care appointments?
During your follow-up prenatal care visits, your doctor, nurse, or midwife will examine you to make sure your pregnancy is developing well, and that you and the fetus are healthy.
During prenatal care visits, your doctor, nurse, or midwife may:
-
update your medical history
-
check your urine
-
check your weight and blood pressure
-
check for swelling
-
feel your belly to check the position of your fetus
-
measure the growth of your belly
-
listen to the fetal heartbeat
-
give you any genetic testing you decide to do
These prenatal checkups are a great time to talk about any questions or concerns that have come up since your last visit.
What changes to my body can I expect during my pregnancy?
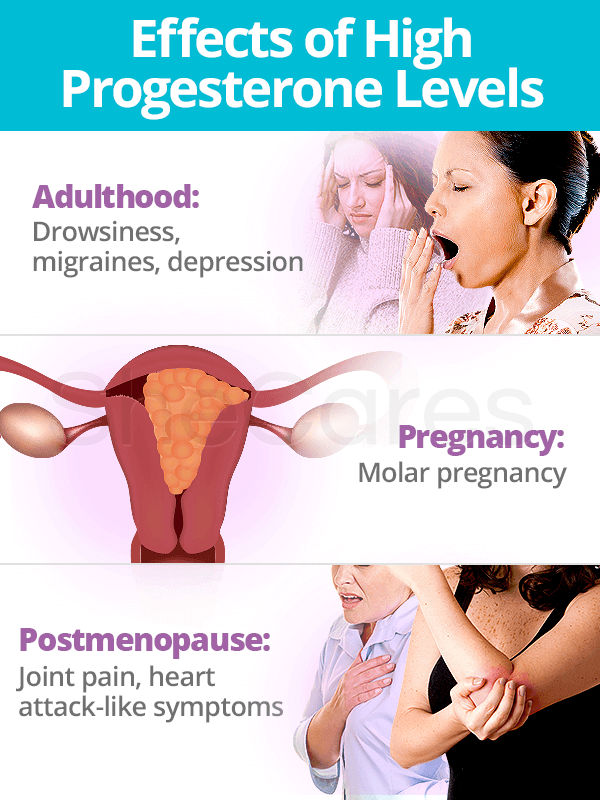
There’s no getting around it — your body will change a lot during your pregnancy. You’ll go through lots of hormonal changes, and you’ll get bigger as the fetus develops. Your uterus will grows up to 18 times its normal size, and your breasts and nipples will probably get larger, too.
It’s normal to gain up to 35 pounds during your pregnancy, and some people may gain more. Your sex drive can increase or decrease throughout your pregnancy. And some people notice changes in the texture and amount of their body hair.
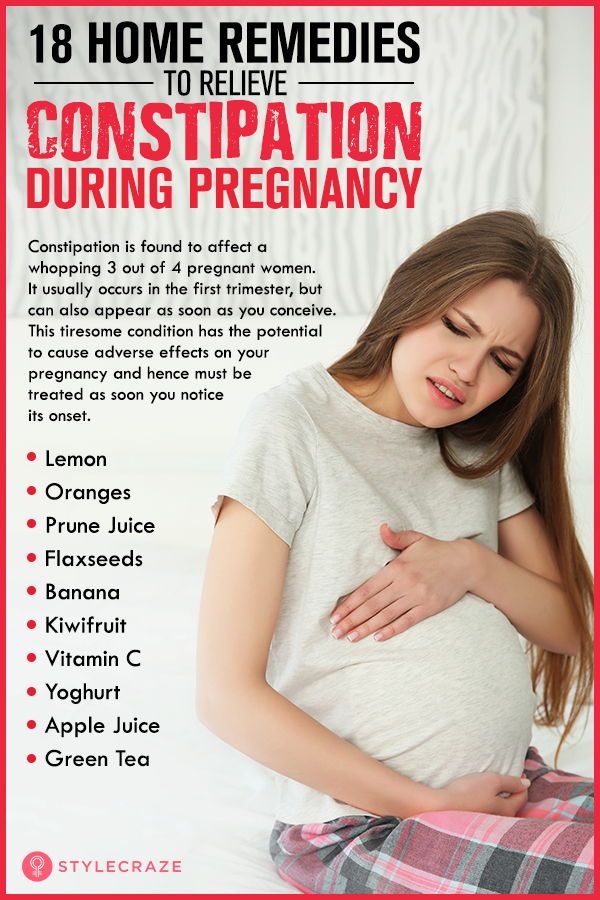
Unfortunately, almost everyone feels uncomfortable at some point in their pregnancy. Some common issues include:
-
nausea or vomiting, especially in the morning
-
swollen and tender breasts
-
heartburn
-
constipation
-
aches and pains in your lower back and hips
-
tiredness and fatigue
-
trouble sleeping
There are things you can do to feel more comfortable, like changing your diet, and doing certain exercises. Your doctor, nurse, or midwife will have tips for feeling better during your pregnancy.
Your doctor, nurse, or midwife will have tips for feeling better during your pregnancy.
How do I relieve common pregnancy discomforts?
For nausea and vomiting:
-
Eat a few bites of food before getting out of bed.
-
Drink ginger or peppermint tea.
-
Eat small meals throughout the day, instead of a few big ones.
-
Drink fluids between meals instead of with your meals.
-
Avoid strong spices, strong odors, and greasy foods.
For heartburn:
-
Eat small meals throughout the day, instead of a few big ones.
-
Chew your food slowly.
-
Don't lie down for at least 1 hour after you eat.
-
Wear clothes that are loose around your waist.
-
Raise your head with pillows when you sleep.
For constipation
Talk with your doctor, nurse, or midwife about getting help for pain or discomfort that doesn’t go away.
- Yes
- No
Help us improve - how could this information be more helpful?
How did this information help you?
Please answer below.
Are you human? (Sorry, we have to ask!)
Please don't check this box if you are a human.
You’re the best! Thanks for your feedback.
Thanks for your feedback.
Back to top
We couldn't access your location, please search for a location.
Zip, City, or State
Please enter a valid 5-digit zip code or city or state.
Please fill out this field.
Service All Services Abortion Abortion Referrals Birth Control COVID-19 Vaccine HIV Services Men's Health Care Mental Health Morning-After Pill (Emergency Contraception) Pregnancy Testing & Services Primary Care STD Testing, Treatment & Vaccines Transgender Hormone Therapy Women's Health Care
Filter By All Telehealth In-person
Please enter your age and the first day of your last period for more accurate abortion options. Your information is private and anonymous.
AGE This field is required.
Or call 1-800-230-7526
10 questions from pregnant women about ultrasonography
10 questions from pregnant women about ultrasonography
The moment when an expectant mother can see her unborn baby on ultrasound is exciting, sometimes to tears. Also important are the quality of the examination and the personality of the doctor, who can both please and, if anything, reassure. Gynecologist Gunars Sergeants , who will soon celebrate his 70th birthday, has been working at Riga 1st Hospital since 1980. Thousands of grateful mothers and born babies! Today, an ultrasound specialist answers the questions that pregnant women ask most often. nine0003
Also important are the quality of the examination and the personality of the doctor, who can both please and, if anything, reassure. Gynecologist Gunars Sergeants , who will soon celebrate his 70th birthday, has been working at Riga 1st Hospital since 1980. Thousands of grateful mothers and born babies! Today, an ultrasound specialist answers the questions that pregnant women ask most often. nine0003
1.When is it necessary to perform ultrasonography?
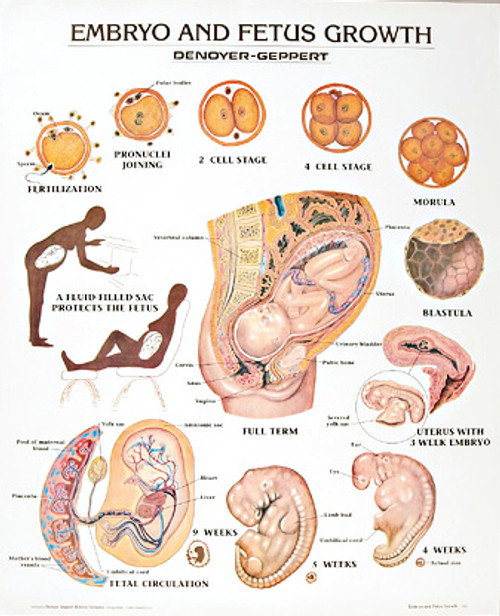
The very first sonography is usually performed between the fourth and sixth weeks of pregnancy, before the mother is registered. The task of the specialist during the examination is to establish whether the pregnancy has occurred, whether there is an ectopic pregnancy that should be terminated, whether the fetus has a heartbeat, or whether the pregnancy is multiple. The parameters of the child are also measured, which allow you to determine the week of pregnancy and the approximate date of birth.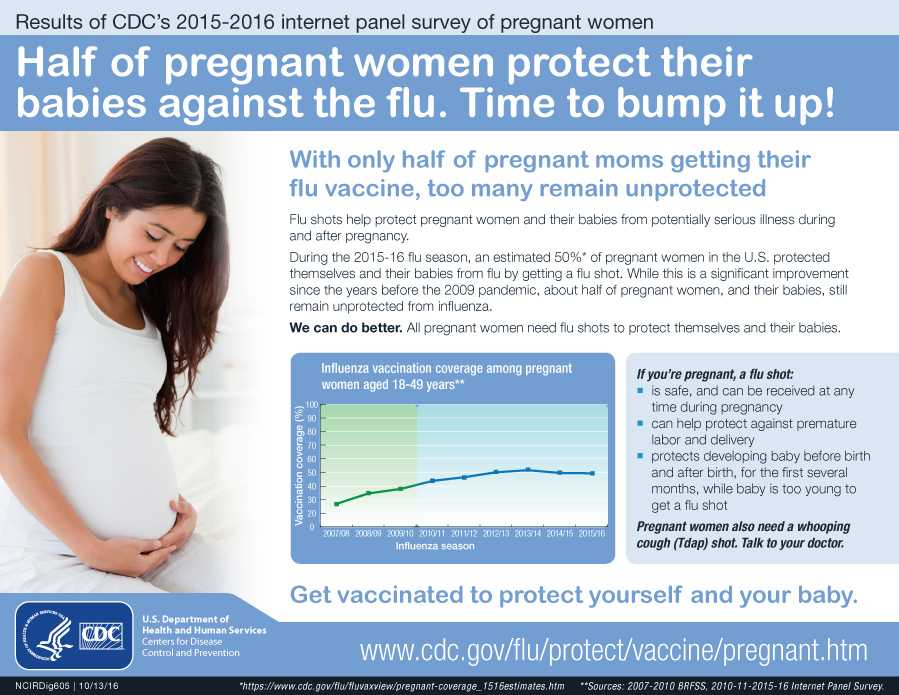 nine0003
nine0003
The next sonography, which is also called the first trimester screening, is carried out at 11-13 weeks, when the fetus is 45-85 mm in size and already looks like a human. The doctor will check if all the internal organs are in order, how the arms and legs look, how the heart beats and the umbilical circulation system works.
Third sonography (second trimester screening) performed at 20-22 weeks. The doctor can see if the fetus has any pathologies. If so, will they be treatable while still in the womb or immediately after birth. Unfortunately, sometimes halfway through the journey, you have to make a decision to terminate the pregnancy. nine0003
2. What is screening? Why does it need to be done multiple times?
Screening and sonography are practically the same thing. The only difference is in the names. But, during screening in the first trimester, in addition to ultrasound, a blood test is done within 24 hours and, taking into account the results of both procedures, it is determined whether the baby has a risk of being born with Down syndrome.
Tests are no longer taken during the second trimester screening. On ultrasound, the doctor examines not only the baby, but also measures the amniotic fluid, looks at the bottom of the uterus, its density, and checks for placental abruption. If a woman has previously had a delivery by caesarean section, then the old suture is also examined during screening. nine0003
3. Why is the state-paid planned ultrasound not carried out in the third trimester as well?
Ultrasound can be performed as many times as needed. If the doctor needs to make sure that everything is in order with the baby, additional ultrasonographic checks are prescribed in both the second and third trimester. They are not prohibited, and, if necessary, the state pays for them. It is possible to carry out an ultrasound in the third trimester if the doctor wants to make sure that the baby is preparing for childbirth. If everything is in order with the child on the second ultrasound, then sonography is usually not prescribed in the third trimester. nine0003
nine0003
After the 36th week, sonography can determine the approximate weight at which the baby will be born. Pay attention to how the child moves. If it seemed to the mother that the activity of the child had decreased, this is a reason for an additional ultrasound. After the 40th week, the doctor looks at how the baby feels, whether he is ready to be born on his own or needs stimulation. There are many situations when a sonographic examination is necessary in the third trimester.
4. At what time can the sex of the child be accurately determined by ultrasound? Are there any mistakes? nine0006 5. Is it possible to determine with the help of ultrasound whether the child is developing correctly? 6. What, unfortunately, cannot be seen on ultrasound? 7. Can the procedure be performed in the presence of the child's father? 8. What does the baby feel in the mother's belly during the ultrasound? 9. If ultrasonography is performed frequently, is it harmful to the child? One can say that sonography can supposedly warm up the amniotic fluid (there are such concerns) if the stomach is heated with the device for more than 40 minutes. But neither at the visit to the gynecologist, nor at the ultrasound specialist, the examination is carried out for such a long time. 10. Ultrasound in 2D, 3D and 4D - a tribute to fashion or a necessity? You can have an ultrasonographic examination with Dr. Gunārs Sergeants at the Riga 1st Hospital by registering at the reception by phone +371 67366323 or via the Internet Gestational age Analyzes Events (registration, medical examinations, doctor visit schedule) nine0003 Up to 12 weeks Early registration in the antenatal clinic Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) At first appearance An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measuring height, body weight, determining body mass index), measuring the size of the pelvis, examining the cervix in the mirrors, bimanual vaginal study nine0003 Not later than 7-10 days after the initial visit to the antenatal clinic Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology nine0003 First trimester (up to 13 weeks) (and at first visit) 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. nine0003 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). nine0003 Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid disease) 1 time per month (up to 28 weeks) Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) nine0003 11-14 weeks Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. After 14 weeks - once Culture of midstream urine To exclude asymptomatic bacteriuria (the presence of bacterial colonies more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. In the second trimester (14-26 weeks) General (clinical) analysis of blood and urine. Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. nine0003 Potassium iodide 200-250 mcg/day 1 time per month (up to 28 weeks) Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) 16-18 weeks Blood test for estriol, alpha-fetoprotein, beta-hCG Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks nine0003 18-21 weeks The second screening ultrasound of the fetus is performed in the antenatal clinic In the third trimester (27-40 weeks) 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). nine0003 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. nine0003 7. A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. nine0003 Potassium iodide 200-250 mcg/day 24-28 weeks Oral glucose tolerance test (OGTT) 28-30weeks In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood Administration of human immunoglobulin antirhesus RHO[D] nine0003 30 weeks A certificate of incapacity for work is issued for maternity leave 30-34 weeks The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. nine0003 After 32 weeks At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), the tone of the uterus, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. After 33 weeks Cardiotocography (hereinafter referred to as CTG) of the fetus is performed nine0003 Throughout pregnancy In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. Over 37 weeks nine0003 Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. 41 weeks Planned hospitalization for delivery No later than 72 hours after delivery All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system nine0003 Re-introduction of human immunoglobulin anti-rhesus RHO[D] postpartum period 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. nine0003 5.
External sexual characteristics of the child begin to appear from the ninth week. But not so clearly to say for sure whether it is a boy or a girl. It can only be guesswork. In boys, the scrotum is not yet clearly visible, and a boy's penis can still be easily confused with a girl's clitoris. The sex of the child is determined after the 16th week of pregnancy. You can see the baby well, provided that the child does not spin and does not cover the “right place” with a pen or leg. The specialist is mistaken in rare cases. nine0003
The specialist is mistaken in rare cases. nine0003
Possible. If the ultrasonography specialist during the screening sees that the development of the baby is normal, then there is no reason to doubt it. If the doctor suspects that the child has some kind of pathology, then additional examinations are carried out by a geneticist. Also, the doctor asks to do an ultrasound again - earlier than it should be. The ultrasound specialist and the attending physician talk to the pregnant woman about the possible pathology in the baby only when this possibility is really very high. The only thing that is difficult to determine one hundred percent is the specific date of birth. During sonography, the latest possible date of delivery is established, when the pregnant woman can already walk over. It is also difficult to determine the exact weight of the child. At a later date, the error can be 200 grams, because the baby is already "donkey" in the pelvic area and it is difficult to accurately measure it. nine0003
nine0003
Any disease or pathology that develops only after the birth of a child. It is impossible to see the child's joints and determine how strong the internal ligaments of the foot will be. In a sonographic image, it is almost impossible to see what is happening with the child's skin, whether he will have birthmarks or moles.
Yes, it is allowed. For a man, this is a wonderful opportunity to meet a baby and the moment when he can realize: I will become a father. The first sonography is carried out at a very early stage, when the baby is not yet visible, and it is performed vaginally, which not all men are ready to look at, and the expectant mother may not feel comfortable. The best time when future parents can come to the ultrasound together is 20-22 weeks of pregnancy. The image of the child is very clear, besides, it is possible to determine its gender, which gives parents great joy. However, there is a request to the accompanying persons - do not stay in the office during the entire time of the inspection. Let the doctor and the expectant mother talk in private. nine0003
However, there is a request to the accompanying persons - do not stay in the office during the entire time of the inspection. Let the doctor and the expectant mother talk in private. nine0003
Most often, the baby sleeps during ultrasonography, which proves that the procedure does not interfere with him. To better examine the baby, it is desirable that he spin. Therefore, it happens that we ask the pregnant woman to move, walk around, turn from side to side so that the child wakes up.
Sonography is not only accurate, but also safe. It is not true that he can somehow harm the child. A visit to an ultrasound specialist takes 40 minutes, but the process of examining a child lasts no more than 10 minutes. With such a duration of the ultrasound procedure, it is not harmful, even if it is done once a month. In addition, even at a monthly examination by a gynecologist, a pregnant woman is not looked at as carefully and for a long time as in an ultrasound room. The observing gynecologist, even if he uses an ultrasound machine, examines the most necessary things - whether the baby’s heart is working well, whether the size of the head corresponds to the size of the abdomen, whether fluid collects in the child’s head, whether the pregnant woman’s cervix opens. nine0003
In addition, even at a monthly examination by a gynecologist, a pregnant woman is not looked at as carefully and for a long time as in an ultrasound room. The observing gynecologist, even if he uses an ultrasound machine, examines the most necessary things - whether the baby’s heart is working well, whether the size of the head corresponds to the size of the abdomen, whether fluid collects in the child’s head, whether the pregnant woman’s cervix opens. nine0003
Most pregnant women are traditionally examined with a two-dimensional image (2D) The picture on the screen is flat, and everything that is in the stomach is visible on it. Everything solid is white, liquid is black. With the help of 2D sonography, the doctor can clearly see both the baby and his organs. 3D sonography does not allow you to see the internal organs so well. It is used in order to better consider the face of the expected child. 3D ultrasonography helps to view the baby's body not in a flat image, but in a three-dimensional one. Usually 3D is used if the mother wants to get a clear photo of the baby in the stomach, close to the real one. In turn, 4D allows you to “catch” the movements of the baby. The image is the same as in 3D, but it is very clearly visible how the baby moves his arms, legs, fingers, how he smiles, and sometimes you can even see how he pees. Such a device is most often used to determine if a child has some kind of facial pathology. nine0003
Everything solid is white, liquid is black. With the help of 2D sonography, the doctor can clearly see both the baby and his organs. 3D sonography does not allow you to see the internal organs so well. It is used in order to better consider the face of the expected child. 3D ultrasonography helps to view the baby's body not in a flat image, but in a three-dimensional one. Usually 3D is used if the mother wants to get a clear photo of the baby in the stomach, close to the real one. In turn, 4D allows you to “catch” the movements of the baby. The image is the same as in 3D, but it is very clearly visible how the baby moves his arms, legs, fingers, how he smiles, and sometimes you can even see how he pees. Such a device is most often used to determine if a child has some kind of facial pathology. nine0003 Citizens | Ministry of Health of the Kaliningrad Region
 General (clinical) blood test.
General (clinical) blood test.  nine0003
nine0003  nine0003
nine0003  General (clinical) blood test.
General (clinical) blood test.  Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.  Inspections and consultations:
Inspections and consultations: