Pregnant lab values
Pregnancy: laboratory measurements
Home / ABA Keyword Categories / Obstetric Anesthesia / Pregnancy: laboratory measurements
Definition
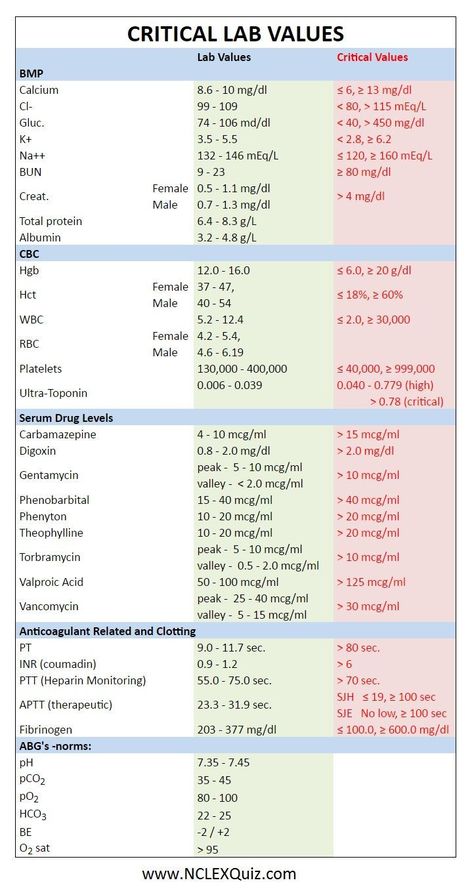
Pregnancy is known to be a state of “physiologic anemia” due to the disproportionate increase in plasma volume relative to red blood cell volume. This increase in blood volume is necessary to supply the fetus and placenta and begins very early in pregnancy. The plasma volume is already increased by 10-15% at 6 weeks of gestation and increases to 30-50% greater than pre-pregnancy volume by term. The red cell volume, in contrast to this, is only increased by 20-30% at term. This increase is prompted by a higher level of erythropoietin. Thus, despite a higher red cell volume, the hematocrit will fall during pregnancy. The greatest time of disproportion between the plasma volume and red cell volume changes will be at 28-36 weeks. Anemia during pregnancy is defined differently than someone who is not pregnant. To be considered anemic during pregnancy the hemoglobin needs to be less than 11g/dL in the 1st or 3rd trimesters.
Other hematologic changes in pregnancy include an increase in white blood cells, particularly neutrophils, and a slight decrease in platelet count. The average white cell count during pregnancy is about 9-15k. It increases up to term, and can go as high as 25k during labor. Platelets, on the other hand, remain in the normal non-pregnant range but mean platelet counts may be slightly lower than in healthy non-pregnant women. The “low normal” range is considered to be about 106-120k.
There are also many changes in blood chemistries during pregnancy as well, mostly by the same dilutional mechanism as the hematocrit. Important among these are albumin, total protein and creatinine. Both albumin and total protein decrease by about 1g/dL by mid-pregnancy and creatinine decreases by about 0.3mg/dL. For other chemistry changes, see chart (below).
| Blood Chemistry | |||
| Albumin | 3.5-4.8 g/dL | 1 g/dL decrease | By midpregnancy |
| Calcium | 9. 0-10.3 mg/dL 0-10.3 mg/dL | 10% decrease | Falls gradually |
| Chloride | 95-105 mEq/L | No change | |
| Cholesterol | 200-240 mg/dL | 50% increase | Rises steadily |
| Creatinine | 0.6–1.1 mg/dL | 0.3 mg/dL increase | By midpregnancy |
| Fibrinogen | 200–400 mg/dL | 1.5-3x increase | By term |
| Glucose, fasting | 65–105 mg/dL | 10% decrease | Gradual fall |
| Potassium (plasma) | 3.5–4.5 mEq/L | 0.2–0.3 mEq/L decrease | By midpregnancy |
| Protein (total) | 6.5–8.5 g/dL | 1 g/dL decrease | By midpregnancy |
| Sodium | 135–145 mEq/L | 2–4 mEq/L decrease | By midpregnancy |
| Urea nitrogen | 12–30 mg/dL | 50% decrease | First trimester |
| Uric acid | 3.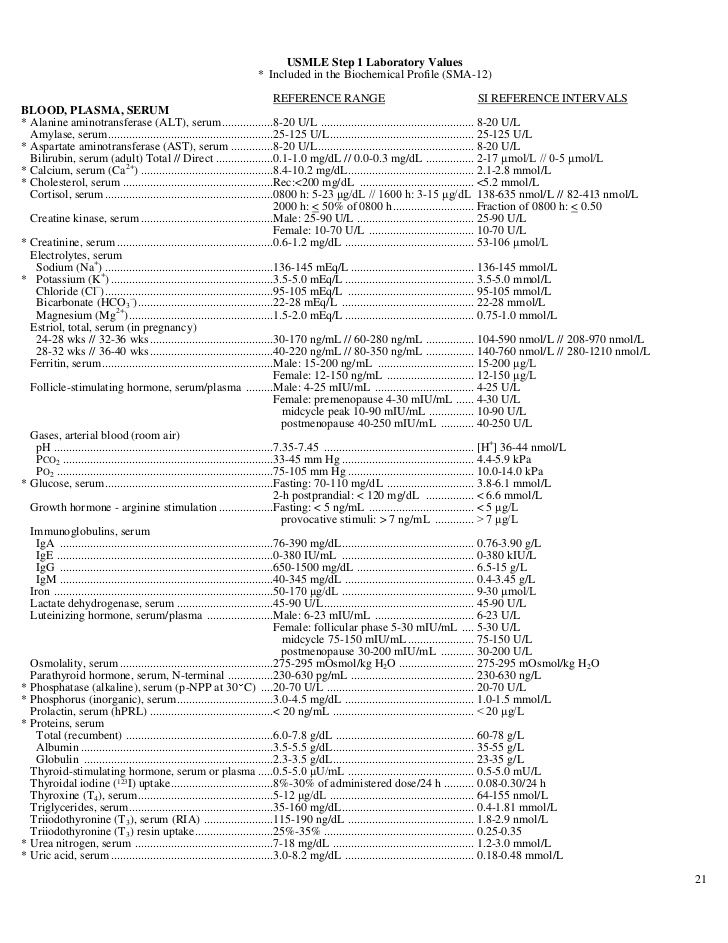 5–8 mg/dL 5–8 mg/dL | 33% decrease | First trimester |
| Urine Chemistry | |||
| Creatinine | 15–25 mg/kg/d | No change | |
| Protein | Up to 150 mg/d | Up to 250–300 mg/day | By midpregnancy |
| Creatinine clearance | 90–130 mL/min/1.73 m2 | 40–50% increase | By 16 weeks |
| Serum Enzymes | |||
| Alkaline phosphatase | 30–120 U/L | 2x to 4x increase | By 20 weeks |
| Amylase | 60–180 U/L | Controversial | |
| Creatinine phosphokinase | 26–140 U/L | 2- to 4-fold increase | After labor (MB bands as well) |
| Lipase | 10–140 U/L | No change | |
| Aspartate aminotransferase (AST) | 5–35 mU/mL | No change | |
| Alanine Aminotransferase (ALT) | 5–35 mU/mL | No change | |
| Formed Elements of Blood | |||
| Hematocrit | 36–46% | 4–7 point decrease | Nadir at 30–34 weeks |
| Hemoglobin | 12–16 g/dL | 1. 4–2.0 g/dL decrease 4–2.0 g/dL decrease | Nadir at 30–34 weeks |
| Leukocyte count | 4.8–10.8 x 103/mm3 | 3.5 x 103/mm3 increase | Gradual increase to term, as high as 25 x 103/mm3 in labor |
| Platelets | 150–400 x 103/mm3 | Slight decrease | Gradual |
Subspecialty
Obstetric Anesthesia
Related Media
Keyword history
71%/2008
See Also:
Pregnancy: Heme and electrolyte changes
Sources
PubMed
Filed Under: Obstetric Anesthesia, Obstetric Anesthesia, P
Routine Tests During Pregnancy | ACOG
Acquired Immunodeficiency Syndrome (AIDS): A group of signs and symptoms, usually of severe infections, in a person who has human immunodeficiency virus (HIV).
Anemia: Abnormally low levels of red blood cells in the bloodstream. Most cases are caused by iron deficiency (lack of iron).
Most cases are caused by iron deficiency (lack of iron).
Antibiotics: Drugs that treat certain types of infections.
Antibodies: Proteins in the blood that the body makes in reaction to foreign substances, such as bacteria and viruses.
Bacteria: One-celled organisms that can cause infections in the human body.
Birth Defects: Physical problems that are present at birth.
Cells: The smallest units of structures in the body.
Cervix: The lower, narrow end of the uterus at the top of the vagina.
Chlamydia: A sexually transmitted infection caused by bacteria. This infection can lead to pelvic inflammatory disease and infertility.
Chromosomes: Structures that are located inside each cell in the body. They contain the genes that determine a person’s physical makeup.
Complications: Diseases or conditions that happen as a result of another disease or condition. An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gene: Segments of DNA that contain instructions for the development of a person’s physical traits and control of the processes in the body. The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
Gestational Diabetes: Diabetes that arises during pregnancy.
Glucose: A sugar in the blood that is the body’s main source of fuel.
Gonorrhea: A sexually transmitted infection that can lead to pelvic inflammatory disease, infertility, and arthritis.
Group B Streptococcus (GBS): A type of bacteria that many people carry normally and can be passed to the fetus at the time of delivery. GBS can cause serious infection in some newborns. Antibiotics are given during labor to women who carry the bacteria to prevent newborn infection.
Hepatitis B: An infection caused by a virus that can be spread through blood, semen, or other body fluid infected with the virus.
Hepatitis C: An infection caused by a virus that can be spread through infected blood.
Human Immunodeficiency Virus (HIV): A virus that attacks certain cells of the body’s immune system. If left untreated, HIV can cause acquired immunodeficiency syndrome (AIDS).
Immune: Protected against infectious disease.
Intravenous (IV) Line: A tube inserted into a vein and used to deliver medication or fluids.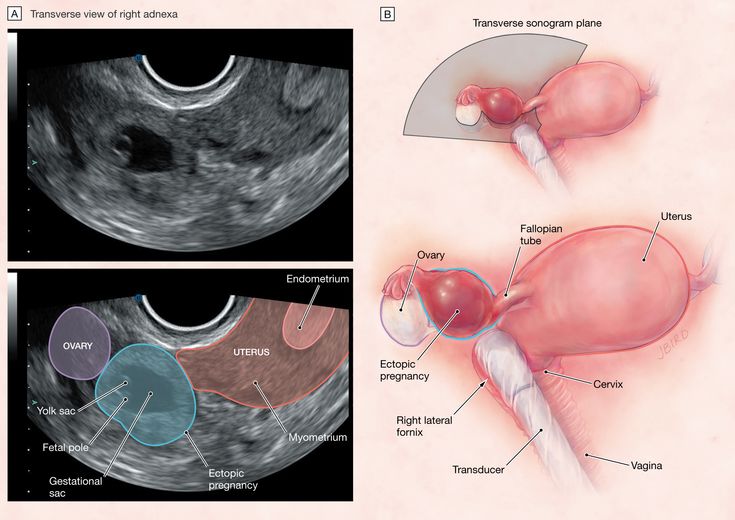
Measles–Mumps–Rubella (MMR) Vaccine: A shot given to protect against measles, mumps, and rubella. The shot contains live viruses that have been changed to not cause disease. The shot is not recommended for pregnant women.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Rectum: The last part of the digestive tract.
Rh Factor: A protein that can be found on the surface of red blood cells.
Rubella: A virus that can be passed to the fetus if a woman becomes infected during pregnancy. The virus can cause miscarriage or severe birth defects.
The virus can cause miscarriage or severe birth defects.
Sexually Transmitted Infections (STIs): Infections that are spread by sexual contact. Infections include chlamydia, gonorrhea, human papillomavirus (HPV), herpes, syphilis, and human immunodeficiency virus (HIV, the cause of acquired immunodeficiency syndrome [AIDS]).
Syphilis: A sexually transmitted infection (STI) that is caused by an organism called Treponema pallidum. This infection may cause major health problems or death in its later stages.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Tuberculosis (TB): A disease that affects the lungs and other organs in the body. TB is caused by bacteria.
Urinary Tract Infection (UTI): An infection in any part of the urinary system, including the kidneys, bladder, or urethra.
Vaccine: A substance that helps the body fight disease. Vaccines are made from very small amounts of weak or dead agents that cause disease (bacteria, toxins, and viruses).
Vaccines are made from very small amounts of weak or dead agents that cause disease (bacteria, toxins, and viruses).
Vagina: A tube-like structure surrounded by muscles. The vagina leads from the uterus to the outside of the body.
Laboratory tests for pregnant women at the IGR clinic (Kyiv)
Pregnancy is a special time in every woman's life. This is an exciting, but at the same time extremely pleasant time waiting for a meeting with a long-awaited baby. It is necessary to prepare properly for such a special event - to visit a doctor in a timely manner and undergo the necessary laboratory tests.
The main task of laboratory diagnostics during pregnancy is prevention, early detection and timely treatment of possible deviations in the development of the fetus and complications that have arisen in a woman. nine0004
About the need to pass tests
Most doctors recommend that you visit a gynecologist in advance and undergo the necessary examination, even before planning a pregnancy. At the same time, ideally, both men and women should be tested and examined by a doctor. In the event that any diseases are detected during the examination, the couple will be able to undergo treatment in advance and plan a pregnancy being absolutely healthy.
At the same time, ideally, both men and women should be tested and examined by a doctor. In the event that any diseases are detected during the examination, the couple will be able to undergo treatment in advance and plan a pregnancy being absolutely healthy.
However, it is worth noting that pregnancy is often unplanned and becomes a real surprise for spouses. How to be in such a case? You don't have to give up having a baby. Indeed, during pregnancy, a woman can also undergo the necessary laboratory tests and a comprehensive examination. nine0004
The capabilities of the current laboratory diagnostics are quite large. The main laboratory tests for pregnant women today are general clinical tests, microbiological blood and urine tests, genital swabs, immunological research methods, PCR diagnostics, and others.
Blood tests
The first analysis, which is given at least four times during pregnancy, is a complete blood count (detailed). In the case of determining pathologies or deviations from the norm, it will have to be taken even more often.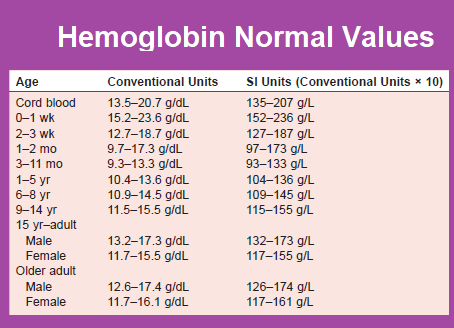 A blood test reveals one of the most common pathologies of pregnant women - iron deficiency anemia, the presence of which is evidenced by reduced hemoglobin. Also, during the analysis, the amount of other important blood components is determined, the deficiency or lack of which may indicate any problems. nine0004
A blood test reveals one of the most common pathologies of pregnant women - iron deficiency anemia, the presence of which is evidenced by reduced hemoglobin. Also, during the analysis, the amount of other important blood components is determined, the deficiency or lack of which may indicate any problems. nine0004
Another extremely important test for a pregnant woman is a blood type and Rh factor test, which avoids possible problems in the event of a so-called Rh conflict (if the woman is negative and the man is Rh positive).
If necessary, a pregnant woman may be prescribed biochemistry - a biochemical blood test. It allows you to assess the condition and efficiency of the functioning of the most important organs - kidneys, liver, pancreas, heart. nine0004
Also, the patient can be prescribed a coagulogram, which determines the main indicators that characterize blood clotting. Any abnormality in this analysis may indicate an increased risk of preterm birth, bleeding, or miscarriage (in the early stages of pregnancy).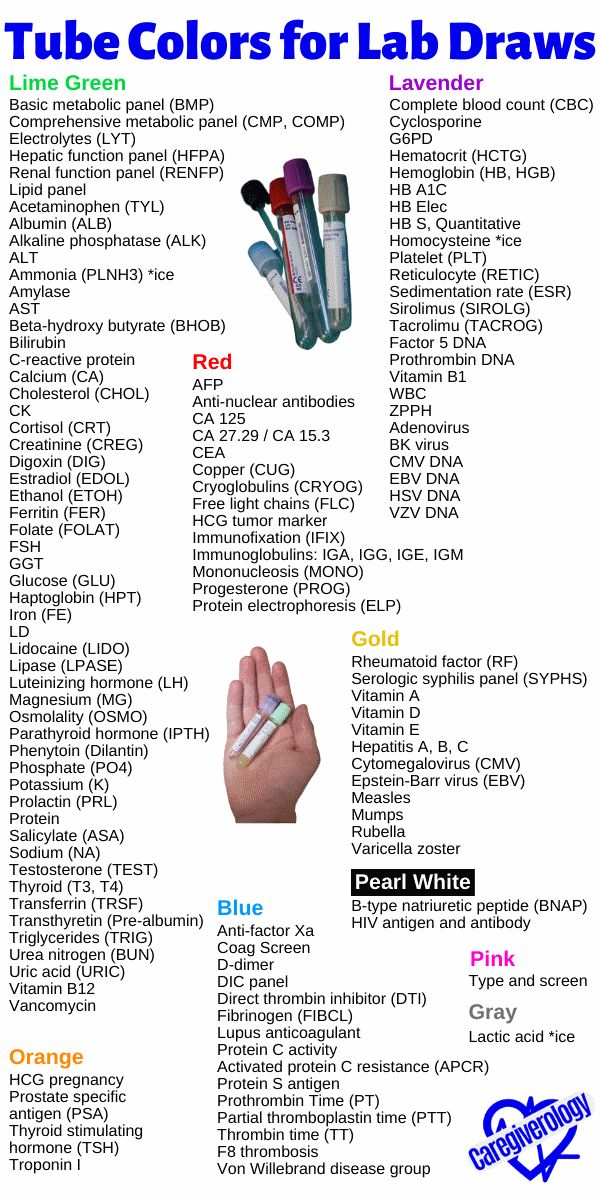
Urinalysis
Just as often in each trimester of pregnancy, a woman will have to take a urinalysis. In the absence of complaints and deviations from the norm, it is given once a month for all three trimesters. If deviations occur, it is given more often (on the recommendation of a doctor). A general urine test allows at an early stage to detect abnormalities in the functioning of the kidneys and the inflammatory process in the bladder. nine0004
Laboratory diagnosis for infection
It is recommended to take tests for infections at the stage of pregnancy planning. Otherwise, they surrender already upon the onset of pregnancy: the sooner the better. The main and mandatory laboratory tests include an analysis of the so-called TORCH infections - toxoplasma, cytomegalovirus, rubella and herpes.
Also, pregnant women are tested several times during pregnancy for HIV, syphilis and hepatitis. nine0004
Hormonal studies
Includes two main prenatal screenings, which are performed in the 1st and 2nd trimester of pregnancy.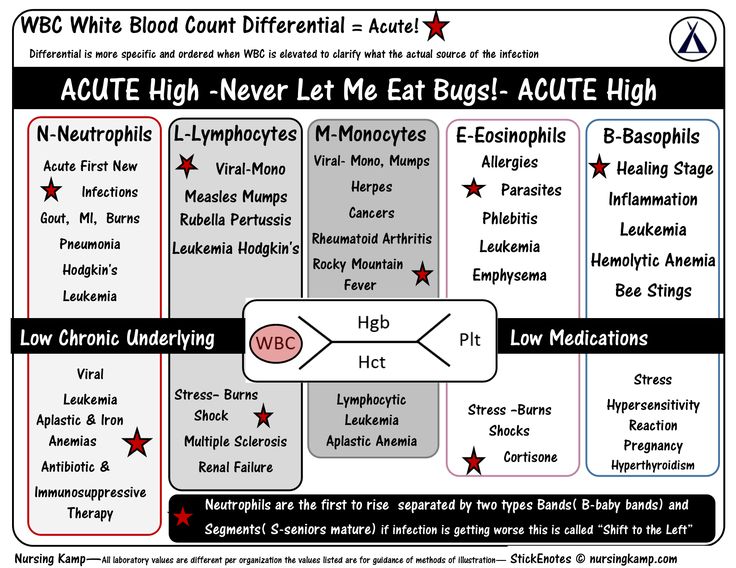 They allow you to assess the risk of congenital malformations and anomalies in the development of the fetus.
They allow you to assess the risk of congenital malformations and anomalies in the development of the fetus.
It is also recommended that a pregnant woman be tested for certain hormones (progesterone and estradiol), which are responsible for maintaining pregnancy and the full development of the fetus.
If there are problems in the functioning of the thyroid gland, a woman will have to be tested for thyroid hormones. nine0004 Make an appointment
Pregnancy: what are the changes in a woman's body, laboratory features
Views: 93174 Published: / Updated:
- Pregnancy
General
Pregnancy is the period of time during which a fetus develops inside a woman's uterus, culminating in the birth of a child. nine0004
During pregnancy, there are numerous physiological changes necessary to meet the needs of the growing fetus and the mother's body, which adapts to them. Most of these changes begin shortly after conception and continue into late pregnancy. Physiological adaptation is reflected in changes in the values of laboratory parameters. Some of the changes are well known, for example, a decrease in hematocrit and hemoglobin, creatinine; others, on the contrary, are known to a lesser extent and therefore their observation in the form of the result of the analysis can lead to misinterpretation. nine0004
Most of these changes begin shortly after conception and continue into late pregnancy. Physiological adaptation is reflected in changes in the values of laboratory parameters. Some of the changes are well known, for example, a decrease in hematocrit and hemoglobin, creatinine; others, on the contrary, are known to a lesser extent and therefore their observation in the form of the result of the analysis can lead to misinterpretation. nine0004
The cardiovascular system
Changes in the work of the cardiovascular system occur among the very first. Their deep restructuring begins already in the early stages of gestation. The main events are physiological vasodilation and fluid retention in the body. Peripheral vasodilation leads to a decrease in vascular resistance and an increase in cardiac output, an increase in heart rate, and an increase in venous pressure. nine0071
Blood pressure decreases in the first and second trimesters, but rises to levels in non-pregnant women in the third trimester.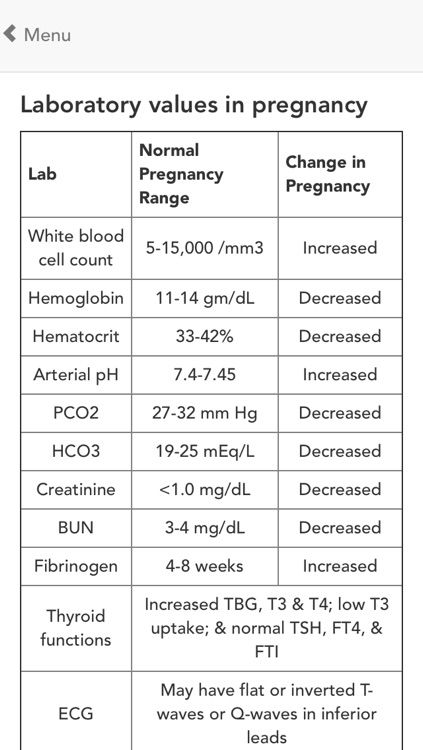
Water balance
Low blood pressure during pregnancy leads to activation of the renin-angiotensin-aldosterone system, resulting in increased secretion of antidiuretic hormone. There is a tendency to retain water and sodium, and the likelihood of edema formation increases. nine0071
Hematological changes
Pregnancy is accompanied by stimulation of hematopoietic processes. There is a general increase in plasma, the number of erythrocytes (RBC) and the total volume of circulating blood. Plasma volume increases during normal pregnancy. An increase of 15% occurs in the first trimester, in the second trimester this trend continues, reaching a maximum by 32 weeks. By this time, the plasma volume is increased exactly by half. nine0071
The number of red blood cells increases, but occurs more slowly compared to plasma, which makes the blood more dilute and leads to the "physiological anemia" of pregnancy. There is a decrease in hemoglobin and hematocrit and mean hemoglobin content in erythrocytes (MCH). The maximum decrease in hemoglobin values is observed at 32-34 weeks of pregnancy.
There is a decrease in hemoglobin and hematocrit and mean hemoglobin content in erythrocytes (MCH). The maximum decrease in hemoglobin values is observed at 32-34 weeks of pregnancy.
During pregnancy, the volume of red blood cells changes. The first 8 weeks of pregnancy, MCV decreases, by 16 weeks it returns to normal values, as in non-pregnant women, and then MCV increases. nine0071
The level of leukocytes (WBC) increases by an average of 20%. The following changes are noted in the leukocyte formula: the absolute number of neutrophils (stab and segmented) increases, the number of lymphocytes decreases.
The number of platelets (PLT) varies ambiguously. Pregnancy is associated with increased platelet turnover.
An increase in blood volume is accompanied by an increase in ESR. In the first trimester, the ESR value is 15 mm/h, in the second - 25 mm/h, in the third - 40 mm/h. nine0071
Hemostasis indicators
Throughout the entire period of pregnancy, the body prepares for the upcoming blood loss, so certain changes occur in the hemostasis system.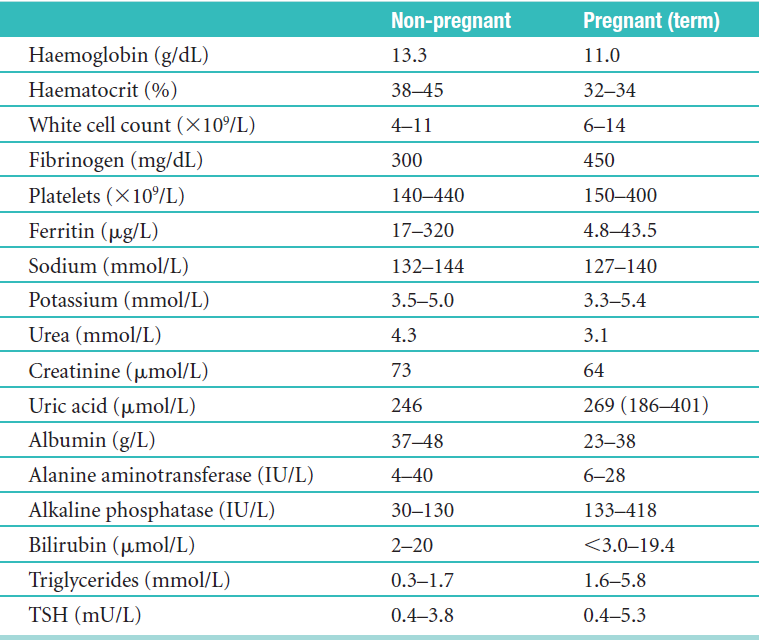
Changes in the blood coagulation system during pregnancy lead to a physiological state of hypercoagulability, or an increased tendency to clot. In the third trimester, coagulation activity is twice as high as normal. The procoagulant activity of the hemostasis system increases, on the other hand, the activity of the fibrinolysis system decreases. nine0071
The concentration of factors VII, VIII, IX, X, XII and the von Willebrand factor increase.
Factor XI values decrease to 60-70% of those in non-pregnant women.
The level of fibrinogen increases significantly - up to 50%.
Levels of protein S, antithrombin III gradually decrease during pregnancy, the activity of protein C remains unchanged.
Plasma fibrinolytic activity decreases throughout pregnancy, but returns to normal within one hour after delivery.
Thrombin is generated as the gestational age increases. The value of D-dimer increases throughout pregnancy. Only 3–5 days after delivery, the D-dimer value returns to its original values.
Only 3–5 days after delivery, the D-dimer value returns to its original values.
Shortening of APTT is observed in the second and third trimester and is associated with an increase in the activity of procoagulants in the blood. In the third trimester, there is a shortening of prothrombin time. nine0071
carbohydrate metabolism
Pregnancy is a diabetogenic condition as it is associated with the development of insulin resistance. An increase in the level of estrogen and progesterone in the initial stages leads to hypertrophy of pancreatic cells that secrete insulin. As a result, insulin secretion and tissue sensitivity to it increase in the early stages.
In the second trimester, insulin resistance begins to appear, reaching a peak in the third trimester. This is the result of the secretion of contrainsular hormones: human placental lactogen, growth hormone, progesterone, cortisol and prolactin. These hormones cause a decrease in the sensitivity of peripheral tissues to insulin, especially in adipose tissue and skeletal muscle, by interfering with insulin receptor signaling.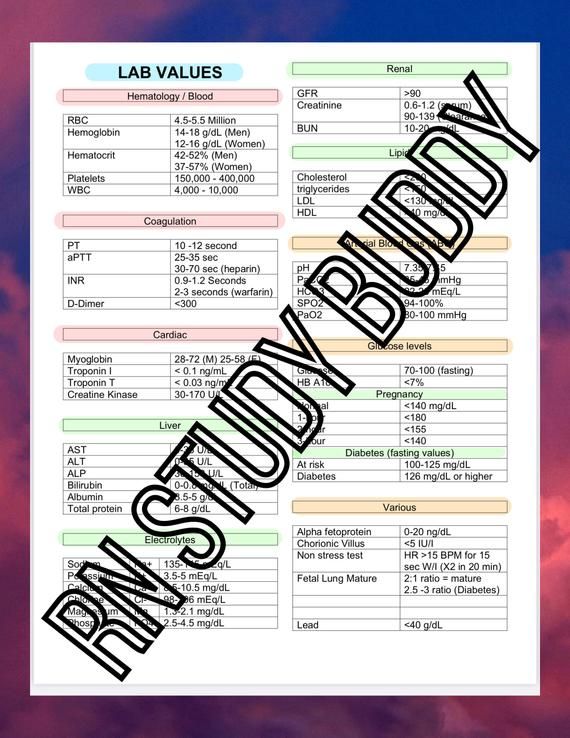 nine0071
nine0071
Insulin levels during pregnancy increase during fasting, after meals.
Fasting glucose often decreases due to:
- increased storage of tissue glycogen stores;
- increased use of peripheral glucose;
- decrease in hepatic glucose production;
- Fetal glucose uptake.
Insulin resistance and relative hypoglycemia lead to an increase in the process of lipolysis - the formation of fats, which mainly allows the use of fat as fuel, saving glucose and amino acids for the fetus. The placenta allows the transfer of glucose, amino acids, and ketones to the fetus, but is impermeable to large lipids. If a woman's endocrine function of the pancreas is impaired and she cannot overcome the insulin resistance associated with pregnancy, then gestational diabetes develops. nine0071
During pregnancy, physiological transient glucosuria is often observed, which is associated with an increase in the glomerular filtration rate and an increase in the permeability of the renal tubular epithelium.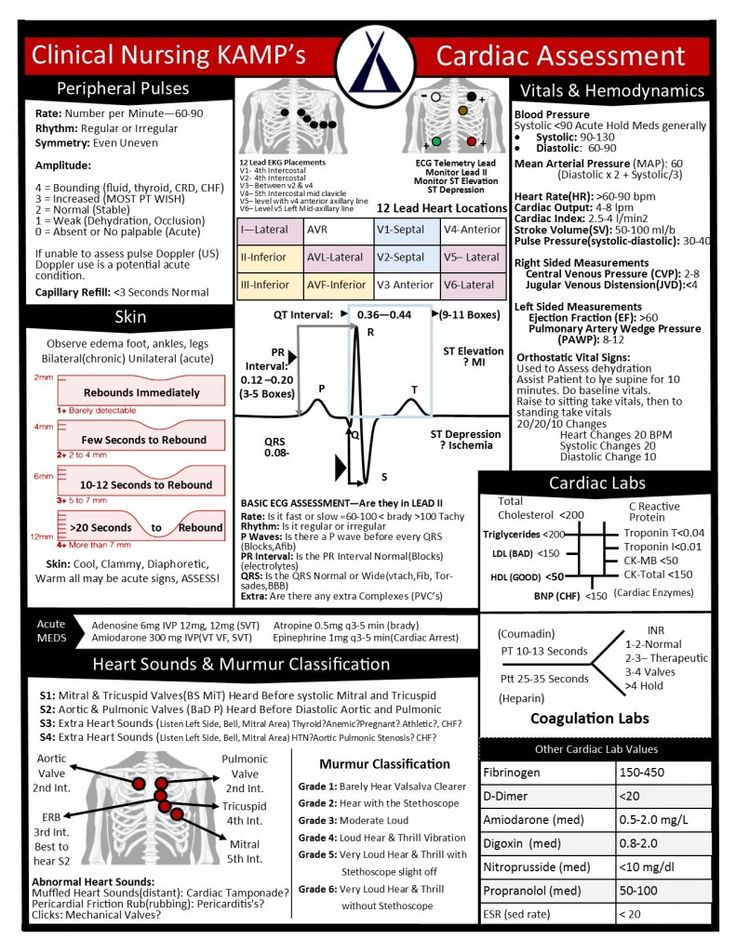
Protein metabolism
During the entire period of pregnancy, a woman needs more protein, since the processes of anabolism prevail over the processes of catabolism. nine0004
There is a physiological decrease in blood albumin, blood dilution also contributes to a decrease in the proportion of albumin.
The proteinogram in the I and II trimester has the following features: a decrease in the level of albumin, a slight increase in a-2 and b-1 globulin fraction. In the III trimester, there is a sharp increase in the a-1 globulin fraction.
Due to increased protein metabolism, a positive nitrogen balance is observed. By increasing GFR by 75%, creatinine and urea levels are reduced. The decrease in creatinine occurs mainly in the I and II trimester, when there is an intensive growth of the uterus. The level of urea falls due to increased protein utilization, especially pronounced in the third trimester.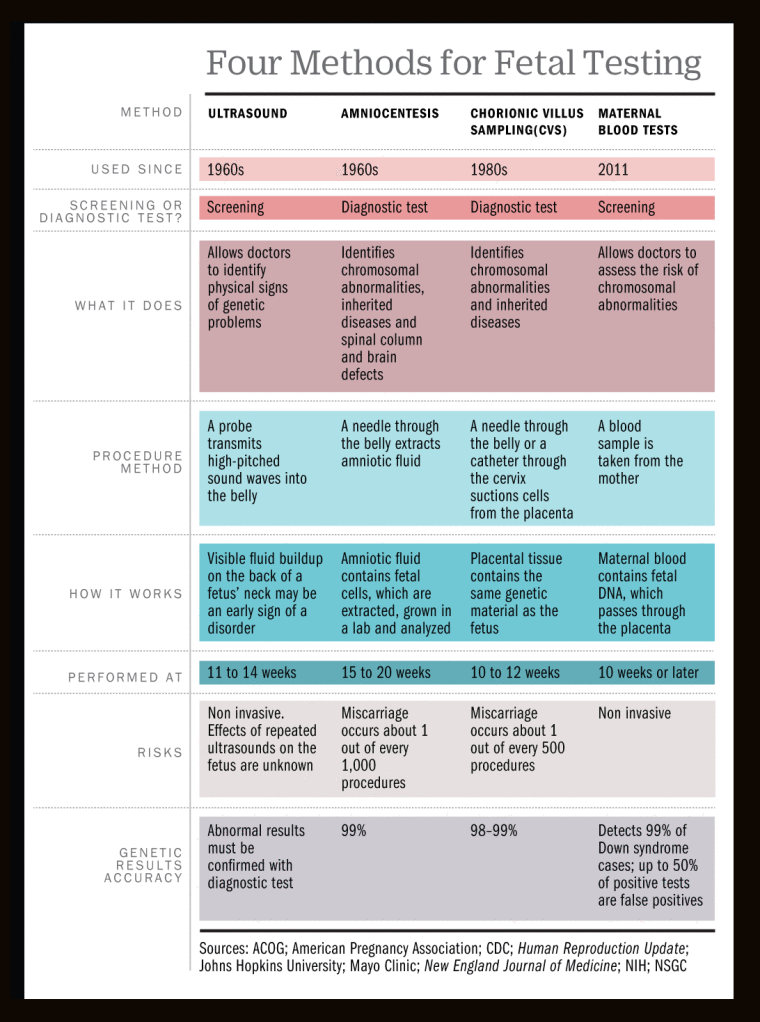 nine0071
nine0071
lipid metabolism
The general effects of altered lipid metabolism during pregnancy are the accumulation of fat reserves in the mother's body in the first half and increased fat mobilization in the second half of pregnancy.
Hypercholesterolemia is due to increased production of sex steroid hormones, changes in metabolism in the liver and adipose tissue. Elevated triglycerides provide the mother's need for energy. An increase in LDL cholesterol is associated with an increase in progesterone, in addition, LDL cholesterol is a source of placental progesterone. The increased concentration of estrogen during pregnancy causes an increase in total cholesterol, LDL cholesterol and triglycerides. nine0071
Regional deposition of fat in the mammary glands and subcutaneous fat is associated with an increase in the transition of carbohydrates into fats under the action of insulin.
Mineral exchange
Pregnancy causes an increase in the need for iron by 2-3 times for the synthesis of hemoglobin, for the production of certain enzymes.